-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
1/16
Sarah M. | Hezer | Mariz | April | Tsen | Victor UERM 2015B Page 1 of 16
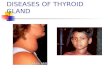
2.8 DISORDERS OF THE THYROIDGLAND
Michael D. Rosario MD, FPSEM August 16, 2013
Legend: Italicized: Recordings
Lecture outline:
-Thyroid anatomy and physiology
-Thyroid work up
-Hypothyroidism
-Hyperthyroidism
-Thyroiditis
-Special situations
-Goiter
-Thyroid cancer
ANATOMY AND PHYSIOLOGY OF THE THYROID
GLAND
Figure 1. Anatomy of the thyroid
ANATOMY
2 lobes + isthmus Between cricoid cartilage and suprasternal notch 12-20 grams, highly vascular and soft 4 parathyroid glands posterior (behind the thyroid
gland)o Removal: Hypocalcemia
Lateral nerves: Recurrent laryngeal nerveso Damage: Vocal cord paralysis
***Thyroidectomy may cause removal of parathyroid gland anddamage to recurrent laryngeal nerves
Medullary C cells
o Neural crest derivativeso Produce Calcitonin
Calcium lowering hormone Minimal role in calcium
homeostasis Clinical significance: Tumor marker
for medullary thyroid cancer
DEVELOPMENT
Orchestrated by coordinated expression of severaldevelopmental factors: TTF1, TTF2 and pairedhomeobox 8 (PAX-8)
o Expressed selectively but not exclusively inthe thyroid gland
o Dictate thyroid cell developmento Induction of thyroid specific genes for the
following proteins Thyroglobulin (Tg) Thyroid peroxidase (TPO) Sodium iodide symporter (NIS) Thyroid stimulating hormone
receptor (TSH-R)o Clinical significance: Mutations in these
transcription factors or their target genesleads to congenital hypothyroidism
CONGENITAL HYPOTHYROIDISM
Figure 2. Congenital hypothyroidism
Occurs in 1/4000 newborns Part of neonatal screening
o Transplacental passage of MATERNALthyroid hormone occurs before the fetalthyroid glands to function (11th week) andprovides partial hormone support to a fetuswith congenital hypothyroidism
o Clinical significance: early detection throughneonatal screening allows early replacementin newborns preventing potentially severedevelopmental abnormalities
*** Thyroid gland of fetus will be fully developed at 11 weeks AOG
before this, supply depends on the transplacental passage of maternalhormone
REGULATION OF THE THYROID AXIS
Figure 3. HPT Axis
Hypothalamus TRH (Thyrotropin releasing hormone) Major positive regulator of TSH synthesis and
secretionPituitary
TSH (Thyroid stimulating hormone)
Stimulates thyroid hormone synthesis secretion 31kDa hormone with alpha and beta sub-units Most useful physiologic marker of thyroid hormone
production
Thyroid stimulating hormone receptor (TSH R)
G protein coupled receptor (GPCR) subunit of stimulatory G protein
o Activates adenylyl cyclase leading toincreased production of cyclic AMP
Recessive loss of function mutation=hypoplasia orhypothyroidism
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
2/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 2 of 16
Dominant gain of function mutation = thyroid cell
hyperplasia, goiter, autonomous function Somatic mutations=clonal expansion of affected
thyroid cell=autonomously functioning thyroidnodules
Thyroid Thyroid hormones Low levels
o Increase basal TSH productiono Enhance TRH mediated stimulation of TSH
High levelso Rapidly and directly suppress TSH gene
expression and secretion
o Inhibit TRH stimulation of TSHIODINE TRANSPORT TO THYROID
Ingested iodine is bound to serum proteins (albumin)o Unbound iodine is excreted in urine
Thyroid glands extracts iodine in the circulation in ahighly efficient manner
Iodine uptake the critical first step; mediated by NIS Clinical significance:
o Iodine deficiency leads to goiter andpossibly hypothyroidism and cretinism
o Iodine oversupply through supplements oriodine enriched foods (kelp, shellfish) is
associated with increased incidence of
autoimmune thyroid disease
CRETINISM
Mental and growth retardation Affects children who:
o Live in iodine deficient regiono Not treated with iodine or thyroid hormone
immediately during early life
oBorn to mothers with iodine deficiencywhich worsens the condition
o Concomitant selenium deficiency Iodine supplementation has markedly reduced the
prevalence of cretinism
IODINE DEFICIENCY
Common sources of dietary iodine:
Breads Cheese, Cows milk
Eggs Frozen yogurt
Ice cream Iodine-containing multivitamins
Iodized table salt Saltwater fish
Seaweed (dulce, nori) Soy sauce
Shellfish Soy milk, Yogurt
FIDEL Fortification for Iodine Deficiency Elimination
**Why salt? Does not spoil easily and consumed by a lot of people so
effective vehicle.
Table 1. Recommended Daily Intake
Recommended intake
Children 90-120 ug/day
Non pregnant adults 150-250 ug/day
Pregnant and lactating women 250 ug/day
IODINE UPTAKE - NIS Expressed at the basolateral membrane of the thyroid
follicular cells
Also present in salivary glands (parotid,submandibular), lactating breast and placenta but a
lower levels (so if radioiodine is given, there will also
be uptake in parotid which is NORMAL)
Affected by dietary iodine intakeo Low levels increased NIS expression and
iodine uptake; increased thyroid blood flow
o High levels decreased NIS expression andiodine uptake
Clinical significanceo Radioactive iodine treatment for
differentiated thyroid cancer
o Mutation leads to a congenitalhypothyroidism
*** Iodine uptake in thyroid cells is secondary to sodium iodide
symporter. Iodide absorption (via NIS) transported out in the apex(via pedrin, a protein Iodide oxidation (through hydrogen
peroxide and TPO/thyroid peroxidase enzyme After iodination,
attached to tyrosine residue found in thyroglobulin converted to 3
mono or 35 di-iodo tyrosine coupled to form T3 or T4 catalyze
by thyroid peroxidase. Thyroglobulin is reabsorbed in follicular cells
(where T3 and T4 are cleaved) released of T3 and T4 in
circulation. Excess MIT and DIT, iodine is removed by dehalogenase
iodine goes back to pool.
ORGANIFICATION, COUPLING, STORAGE ANDRELEASE
Iodide is transported to the apical membrane whereto be oxidized in an organification reaction thatinvolves TPO and hydrogen peroxide
The reactive iodine atom is added to selected tyrosylresidues within Tg
The iodotyrosines in Tg are then coupled via an etherlinkage in a reaction that is also catalyzed by TPO
forming either T4 or T3
After coupling, Tg is taken back into the thyroid cell,where it is processed in lysosomes to release T4 and
T3.
Dehalogenase enzymes deiodinate uncoupled monoand diiodotyrosines (MIT, DIT) to recycle iodide
THYROID HORMONE TRANSPORT BINDINGPROTEINS
Purpose of binding proteins:
Increase pool of circulating hormone Delay hormone clearance Modulate hormone delivery
Thyroxine binding globulin (TBG)
Low concentration but high affinity for thyroidhormones = 80%
Albumin
High concentration but low affinity = 10% T4 & 30%T3
Transthyretin (TTR aka TBPA) 10% T4 & little T3
Unbound hormones
Biologically available for tissues T3 less tightly bound than T4 (99.7% T3 vs 99.98% T4) But there is less unbound or Free T3 in the circulation
because it is produced in lesser amounts and is
cleared more rapidly
ABNORMALITIES OF THE THYROID HORMONEBINDING PROTEINS
Disease
condition
Total
T3
&T4
Free T3
and T4
TSH Clinical
X linked TBG
deficiency
Absent TBG
leads to rapid
hormone
clearance
Low Normal Normal Euthyroid
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
3/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 3 of 16
Pregnancy or
OCP use
Increased
estrogen levels
-elevated TBG
High Normal
Normal
or Low Euthyroid
Euthyroid
Hyperthyroxine
mia
Increased
binding affinityfor T4 or T3
High Normal Normal Euthyroid
DEIODINASES
Figure 4. Deiodinases
*** If hormone is in target cell, will be acted upon by deiodinases
(removal of one iodine from T4). Active hormone: T3
Table 2. Types of deiodinases
Type 1 Type 2 Type 3
Location
Thyroid,
Liver,
Kidneys
Pituitary,
Brain,
Brown
Fat, Thyroid
Placenta
Placenta, CNS,
Hemangiomas,
Adult and
Fetal Liver,
Skeletal
Muscle
T4 affinity Low High
Response to
increased T4Increased Decreased Increased
Susceptibility
to PTUHigh Absent Absent
Physiologic
role
Source of
plasma T3
in
thyrotoxic
patients
Provide
intracellular
T3 in specific
tissues,
source of
plasma T3
Inactivate T3
and T4
Most important
source of
Reverse T3
*** in T4 results to type 1 (produces active hormone and source of
plasma T3 in thyrotoxic patient, but susceptible to PTU). Type 2
produces intracellular T3 in specific tissues. Type 3 produces reverse
T3 and inactivating enzyme. Clinical significance: infant with very
big hemangioma (high level of T3) inactivation of T3 and T4
resulting to congenital hypothyroidism
NUCLEAR THYROID HORMONE RECEPTORS
Figure 5. Thyroid hormone receptors
Enter cells by passive diffusion and via themonocarboxylate 8 (MCT8) transporter
High affinity to nuclear thyroid hormone receptors (TRs) & which are expressed in most tissues, but their
relative expression levels vary among organs
o TR is particularly abundant in brain,kidney, gonads, muscle, and heart
o TR expression is relatively high in thepituitary and liver.
o The TR 2 isoform is selectively expressed inthe hypothalamus and pituitary, where it
plays a role in feedback control of the
thyroid axis.
Receptors are occupied mainly by T3, reflecting T4 toT3 conversion by peripheral tissues, greater T3
bioavailability in the plasma, and receptors greater
affinity for T3.
The aporeceptors bind to corepressor proteins thatinhibit gene transcription.
Thyroid hormone binding dissociates these co-repressors and allows the recruitment of coactivators
that enhance transcription.
ACTION OF THYROID HORMONES (TH)
Child
Brain development Growth and development in latter stages of
childhood
Adult
Primarily metabolismo Carbohydrate, lipid, protein and vitamin
metabolism
o Regulation of oxygen consumption Other actions on mood, cognition, heart, bone and
muscle
NON- GENOMIC ACTION OF TH
Major effects of T3 are mediated by nuclear ThyroidHormone Receptor regulation of target gene
transcription
However, it has some non genomic actiono Vasculature reduced systemic vascular
resistance which rapidly occurso Acts on glucose transporters in certain
tissues allowing increased uptake of glucose
THYROID HORMONES RESISTANCE
Autosomal dominanto Similar hormonal abnormalities found other
family members
Mutation leading to loss of thyroid hormone receptorfunction
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
4/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 4 of 16
o They also function as antagonists of theremaining normal thyroid hormone
receptors
Elevated unbound thyroid hormone levels Inappropriately normal or elevated TSH The resistance is partial hence signs and symptoms of
hypothyroidism are not full blown
o Goiter, attention deficit, mild IQ reduction,delayed skeletal maturation
THYROID WORK UPTHYROID FUNCTION TESTS
TSH Total T3 and Total T4
o Highly protein bound which can be affectedby numerous factors (refer to abnormalities
of thyroid hormone binding proteins)
o Elevated when TBG is high (increasedestrogen conditions)
o Decreased when TBG is low (Androgens,Nephrotic syndrome)
Free T3 and Free T4 (unbound)
o Represents the biologically availablehormonal pool
o Isolated Free T3 elevation occurs in 2-5% ofpatients (T3 toxicosis)
o Normal FT3 may occur in 25% of patientswith Hypothyroidism
*** TSH and unbound hormones (total hormones are highly protein
bound so affected by various factors)
Table 3. Match the following
Thyroid Function Thyroid Condition
1. High TSH, Low FT4,
Low FT32. Normal TSH, Low FT4,
Low FT3
3. Low TSH, Normal FT4,
Normal
FT3
4. Low TSH, High FT4,
High FT3
5. Normal TSH and FT4,
Low FT3
A. Central Hypothyroidism
B. Subclinical Hyperthyroidism
C. Autoimmune
Hypothyroidism
D. Sick Euthyroid Syndrome
E. Hyperthyroidism
***Answer:
1: C (Autoimmune hypothyroidism) low production, compensatory
action of pituitary2: A (Central hypothyroidism)
3: B (Subclinical hyperthyroidism) - asymptomatic
4: E (Hyperthyroidism)
5: D (Sick euthyroid syndrome)
(See Thyroid Patterns in Appendix)
THYROID PROTEINS AND ANTIBODIES
Thyroglobulin (Tg)o Follow up of thyroid cancero To rule out thyrotoxicosis factitiao Elevated in thyroiditis
Antibodies to thyroid proteinso Anti thyroglobulin (Anti Tg)
Follow up of thyroid cancerpatients
Autoimmune thyroid illness (notroutinely included)
o Anti Thyroid Peroxidase (Anti TPO) Autoimmune thyroid illness
o Anti TSH receptor (TRAB) TSH stimulating
Hyperthyroidism
TSH blocking Hypothyroidism
*** Tg = sign of thyroid cancer recurrence and to rule out
Thyrotoxicosis factitia (Thyrotoxicosis factitia: Tg is normal but px
has symptoms of thyrotoxicosis, either faking it or taking thyroid
medication). Among Ab, the best is TPO (best indicator of
autoimmune thyroid illness).
Table 4. Thyroid Antibodies in subset of population (%)
Patient Group
TSH
receptorAntibody
Thyroglobulin
(TG) Antibody
Thyroid
Peroxidase
(TPO)
antibody
General
Population0% 5-20% 8-27%
Graves
Disease80-95% 50-70% 50-80%
Autoimmune
thyroiditis10-20% 80-90% 90-100%
RADIONUCLIDE IMAGING
The thyroid gland selectively transports radioisotopes of
iodine (123I, 125I, 131I) and 99mTc pertechnetate, allowing
thyroid imaging and quantitation of radioactive tracerfractional uptake.
Iodine uptake measures thyroid function High in Graves Disease Low in thyroiditis (hyperthyroid phase)
Figure 6. Thyroid Scan Imaging
Figure 7. Radionuclide Imaging: Whole Body Scan
***Whole body scan done after thyroid cancer treatment to check for
metastasis. Notice pick-up in salivary gland (normal)
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
5/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 5 of 16
ULTRASOUND OF THE THYROID
Figure 8. Ultrasound of the Thyroid
***Nodule: hypoechoic compared to thyroid tissues, regular/defined
border, no calcification. Only does Biopsy if there are suspicious
features
Micro calcification Increased vascularity especially in the center Irregular/ill-defined border
HYPOTHYROIDISM
Figure 9. Classifications of Hypothyroidism
*** Most common worldwide: iodine deficiency. In iodine sufficient
areas: autoimmune or iatrogenic(See appendix for algorithmevaluation of hypothyroidism)
***Request for the complete panel (TSH, FT3, FT4) if suspecting
thyroid disease (to avoid delay and multiple blood extraction)
AUTOIMMUNE HYPOTHYROIDISM
HistologyHashimotos or
GoitrousThyroiditis
AtrophicThyroiditis
Lymphocyticinfiltration
Markedlymphocytic
infiltration with
germinal cellformation
Less pronounced
Thyroid folliclesAtrophy of thyroid
follicles withabsent colloid
Almost completelyabsent
Fibrosis Mild to moderate Extensive
***Autoimmune hypothyroidism- 2nd most common, can present as
atrophy or a goiter, subclinical, overt/clinical
Genetic Factorso HLA-DR and CTLA-4 polymorphisms account for
approximately half of the genetic susceptibility to
autoimmune hypothyroidism.
o Both of these genetic associations are shared by otherautoimmune diseases(type 1 diabetes mellitus,
Addisons disease, pernicious anemia, and vitiligo)
Sexo Female preponderance: sex steroid effect on immune
response vs X chromosome-related genetic factor Diet
o A high iodine intake may increase the risk ofautoimmune hypothyroidism by immunologic effects
or direct thyroid toxicity
Infectiono Congenital Rubella syndrome associated with high
frequency of autoimmune hypothyroidism
o Viral thyroiditis does not induce subsequentautoimmune thyroid disease.
PATHOGENESIS
Figure 10. Pathogenesis of Hashimotos thyroiditis and Graves
disease
CD8 + cytotoxic T cellso Primary mediatoro Perforin-induced cell necrosiso Granzyme B induced apoptosis
Local production of Cytokineso TNF, IFN, IL-1o Impair thyroid cell function directlyo Induce thyroid cells to express pro-inflammatory
molecules
o Renders thyroid cells more susceptible to apoptosis B cells
o Secondary role; merely amplifies ongoingautoimmune response
o TPO ab:-Useful marker for autoimmunity
- Complement fixation
- Transplacental passage does not damage fetal
thyroid
o TSH receptor Ab:-Seen in 20% of patients with autoimmunehypothyroidism
-Blocking antibodies which block TSH binding
-Hypothyroidism and atrophy
-Transplacental passage=neonatal hypothyroidism
***Autoimmune hypothyroidism: blocking antibodies leading to
hypothyroidism and atrophy (remember there are 2 types of TSH-
receptor antibodies; in autoimmune hypothyroidism it is the blocking
type). Can be passed on the fetus resulting to neonatal
hypothyroidism
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
6/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 6 of 16
SIGNS AND SYMPTOMS
Symptoms:o Tiredness, weaknesso Dry skino Feeling coldo Hair loss; thinning of outer third of eyebrows (Queen
Annes sign)
o Difficulty concentrating and poor memoryo Constipationo Weight gain with poor appetiteo Dyspneao Hoarse voiceo Menorrhagiao Paresthesiao Impaired hearing
Signso Dry coarse skino Cool peripheral extremitieso Puffy face, hands and feet(myxedema)o Diffuse alopeciao Bradycardiao Peripheral edemao Delayed tendon reflex relaxationo Carpal tunnel syndromeo Serous cavity effusions***Decreased in metabolism (patient slows down literally)
TREATMENT
Levothyroxine Replacement1. Start levothyroxine replacement 1.6-1.8ucg/kg BW(100-
150ucg/day)
2. Check TSH every 6-8 weeks
3. Adjust dose by 12.5 to 25 ucg until TSH goal of Lower
half of Normal range is achieved
Special situations:
o Pregnancy: higher requirements; need to increase dose by50 % and reduce after delivery
o Elderly, coronary artery disease patients: starting dose12.5-25 ug/day
*** Taken 30 minutes before breakfast (if taken incorrectly can results
to poor absorption and patient may need higher dose). ONLY request
for TSH every 6-8 weeks (FT3 and FT4=unnecessary). If TSH is
within target (lower half of normal range) no need to adjust (if high
or low, adjust in this range: 12.5 to 25 ucg)
Non-levothyroxine Replacemento Dessicated animal thyroid prepations (thyroid extract
USP) are not recommended as the ratio of T3-T4 is
nonphysiologic.
o Benefit of using levothyroxine combined withliothyronine (triiodothyronine, T3) has not been
confirmed in several prospective studies.
o There is no place for liothyronine alone as long-termreplacement, because the short half-life necessitates
three or four daily doses and is associated with
fluctuating T3 levels.
***For replacement, levothyroxine is preferred over liothyronine
(since levothyroxine only required less dosage and can be taken oncea day unlike liothyronine which required multiple dosages).
Liothyronine is usually indicated for 1). preparing the patient for
radioactive iodine uptake and 2). if allergic to levothyroxine (based
on Dr. Rosarios practice)
MYXEDEMA COMA
Clinical manifestations: Reduced level of consciousness,seizures, hypothermia
History of treated hypothyroidism with poor compliance,or the patient may be previously undiagnosed.
Almost always occurs in the elderly Hypothermia also a risk factor Hypoventilation, leading to hypoxia and hypercapnia,
plays a major role in pathogenesis.
o Factors that impair respiration may precipitatemyxedema coma: drug(sedative, anesthetics,
antidepressants), pneumonia, congestive heart failure,
myocardial infarction or cerebrovascular accidents.
***Most severe form of hypothyroidism/ an endocrine emergency
TREATMENT
Levothyroxineo Loading dose: 500 ucgo Maintenance dose: 50-100 ucg g/do Route: Intravenous(preferred) or nasogastric tube
(though aborption may be impaired in myxedema)
Liothyronine(T3)o Dose: 10 to 25 ucg every 8-12 hour intravenously or
via nasogastric tube.
o Advocated because T4-T3 conversion is impaired inmyxedema coma.
o Excess liothyronine has the potential to provokearrhythmias.
o advocated due to T4 to T3 impaired conversion in cases ofMyxedema coma; may be given in combination.
Combined levothyroxine (200ucg) and liothyronine(25ucg)
o Loading: levothyroxine(200ucg) andliothyronine(25ucg)
o Maintenance: levothyroxine(50-100ucg/d) andliothyronine (10ucg every 8 hour)
***Use of liothyronine is advocated since in Myxedema coma,
there is impairment in the conversion of T4 to T3.
HYPERTHYROIDISM Thyrotoxicosis
o State of thyroid hormone excesso Ex. Excessive intake of levothyroxine
Hyperthyroidismo Thyrotoxicosis due to excessive thyroid functiono Ex. Graves Disease
THYROTOXICOSIS
Figure 11. Classification of thyrotoxicosis
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
7/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 7 of 16
PATHOGENESIS
Thyroid Stimulating Immunoglobulins (TSI)o Synthesized in the thyroid gland, bone marrow and
lymph node
o Aka TRABRISK FACTORS
Polymorphism in HLA-DR, CTLA-4, CD25, PTPN22, TSH-R
Stress via the Neuroendocrine system Smoking
o Minor risk: Graves diseaseo Major risk: TAO
Postpartum Increased iodine uptake After use of HAART tx or alemtuzumab txSIGNS AND SYMPTOMS
Signso Tachycardia; atrial fibrillation in the elderlyo Tremorso Goitero Warm, moist skino Muscle weakness, proximal myopathyo Lid retraction or labo Gynecomastia
Symptomso Hyperactivity, irritability, dysphoriao Heat intolerance and sweatingo Palpitationso Fatigue and weaknesso Weight loss despite increased appetiteo Diarrheao
Polyuriao Oligomenorrhea, loss of libido
THYROID ASSOCIATED OPHTHALMOPATHY (TAO)
Pathogenesis of TAOo TSH-R may be a shared autoantigen expressed in the
orbit
o Infiltration of the EOMs by activated T cells withrelease of cytokines: Orbital fibroblasts become
activated with increased synthesis of
glycosaminoglycans that trap water leading to ocular
muscle swelling.
***risk factor associated with opthalmopathy: Genetics, Stress,
smoking, after delivery, increased iodine intake, after used of anti-
retroviral drugs/therapy (HIV). Patients are very difficult to
interview because of severe anxiousness, agitation, tachycardia.
Euthyroid ophthalmopathy - may occur in the absence ofGraves disease(10%)
Usually occurs 1 year (+/- years) before or after dx ofthyrotoxicosis in 75%
Unilateral only in 10 % of patients Earliest symptoms: gritiness, eye discomfort, excessive
tearing
1/3 have proptosis; may progress to corneal damage ifsevere
5-10 % severe EOM swelling leading diplopia
Most serious manifestation: Optic nerve compression-papilledema-loss of vision.
Course dose not follow thyroid diseaseo Worsens first 3-6mos.o Plateaus next 12-18mos.o Spontaneous improvement in soft tissue changes
Fulminant in 5% of patients Intervention in the acute phase if there is optic nerve
compression or corneal ulceration
General measures
o Achieve euthyroid statuso Smoking cessationo Reassurance
Mild-moderateo Artificial tears, eye ointment and use of dark glasseso Periorbital edema-upright sleeping position or
diuretic
o Eye patches when sleeping to avoid corneal exposure***Elderly may have Apathetic Thyrotoxicosis: weight loss (somedont rather increases appetite), hyperdefecation, palpitation, heat
intolerance, muscle weakness (proximal mostly affected)
Severe ophthalmopathyo First line: high dose oral steroids or pulse steroids
followed by oral steroids
o Orbital decompression: removal of bone from anywall of the orbit
o External beam radiotherapy***Management is mostly supportive ; if severe: use High dose of
Steroids (oral/IV) if not decompress by surgeryremoving bone wallor radiotherapy.
THYROID DERMOPATHY
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
8/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 8 of 16
Thyroid Gland Sizeo Decrease 1/3-1/2o Unchanged or enlarged remaining half
TSH may remain subnormal for 6 months Maximum remission rates (30-50%) are achieved by
18-24 months
o Relapse likely if severe hyperthyroidism orwith large goiters
***PTUhas additional blocking in the T4-T3 peripheral conversion
Deiodenized enzyme TYPE 1; dosage 450-600mg/day- each tab is50mg3-4x a day; may have poor compliance. Methimazole more
potent; thyroid peroxidase action: starting 40-60mgonce or twice a
day
Figure 14. Monitoring thionamide use
(See Appendix for Comparison of Methimazole vs
Propylthiouracil )
Lithium
Alternative to thionamidesIodine
Saturated solution of Potassium Iodide (SSKI),ipodate, iopanoic acid
Wolff- Chaikoff effect Thyroid storm (give 1 hour after thionamides) Decrease vascularity pre-op
Steroids
Thyroid stormBeta Blockers
Adjunct to treatment To control adrenergic symptoms, especially in theearly stages before anti-thyroid drugs take effect Useful in patients with hypokalemic paralysis
***PTU in selected cases usually given in the first 3 months of
pregnancy (organogenesis)
Methimazolerecommended Latest guidelines in most cases
Doc Rosario: Give the meds up to 1 year assuring that the TSH is
normal, then stop gradually. If no recurrence good, but if does:
proceed to definitive treatmentSurgery, RAI.
Radioactive Iodine- -avoid pregnancy within Six months
HOW TO START:
Starts 1st 3months (check-up every month)
Hypothyroidism monitor TSH Hyperthyroidism monitor FT4, FT3 - why not TSH?
= TSH may resume abnormal for 6months:
o Note: as long as the FT4 and FT3 goingdown and has clinically signs of improving
theres no need to increase the dose.
***Doc Rosario: Starts the meds and followed up patient after 2
weekscheck for possible Side effects (because in 2 weeksmay have
already a clinical improvement; Dec palpitation, tachycardia)
specially with propanolol and inderal.
THYROID STORM
A rare endocrine emergency Life-threatening exacerbation of hyperthyroidism,
accompanied by fever, delirium, seizures, coma,vomiting, diarrhea, and jaundice.
Mortality rate due to cardiac failure, arrhythmia, orhyperthermia is as high as 30%, even with treatment.
Precipitants: acute illness (e.g., stroke, infection,trauma, diabetic ketoacidosis), surgery (especially on
the thyroid), or radioiodine treatment of a patient
with partially treated or untreated hyperthyroidism.
BURCH WARTOFSKY SCORE
The scoring includes the following variables:
Temperature CNS GIT- Hepatic Dysfunction CVS
o Tachycardiao CHFo Atrial Fibrillation
Greater than 45 points is highly suggestive of aThyroid Storm
25 to 44 points is Impending Less than 25 is Unlikely(See appendix for corresponding points and scoring)
TREATMENT
Management requires intensive monitoring andsupportive care, identification and treatment of theprecipitating cause, and measures that reduce thyroid
hormone synthesis.
Large doses of propylthiouracil (600 mg loading doseand 200300 mg every 6 h)per orem, NGT or per
rectum
o Has inhibitory action on T4 to T3 conversion Stable Iodide given one hour after the first dose of
propylthiouracil
o Wolff-Chaikoff effecto The one hour delay allows the antithyroid
drug to prevent the excess iodine from being
incorporated into new hormones.
o A saturated solution of potassium iodide (5drops SSKI every 6 h), or ipodate or iopanoic
acid (0.5 mg every 12 h), may be given
orally.
Propranolol should also be given to reducetachycardia and other adrenergic manifestations (40
60 mg orally every 4 h; or 2 mg intravenously every 4
h)
o High doses of propranolol decrease T4 to T3conversion, and the doses can be easily
adjusted.
Additional therapeutic measures includeglucocorticoids (e.g., dexamethasone, 2mg every 6 h),
antibiotics if infection is present, cooling, oxygen, and
intravenous fluids.
THYROIDITIS
Classification based on duration:
1. Acute Bacterial Fungal Radiation (Iodine 131 treatment)
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
9/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 9 of 16
Amiodarone2. Subacute
Viral or Granulomatous thyroiditis Silent and Postpartum Throiditis Mycobacterial Infection
3. Chronic Autoimmune
o Hashimotos Thyroiditiso Atrophic Thyroiditis
Riedels Thyroiditis Parasitic Thyroiditis Traumatic (after palpation) Thyroiditis
ACUTE INFECTIOUS THYROIDITIS
Rare suppurative infection with an abruptpresentation
Predisposing factorso Piriform sinus seen in children and young
adults
o Long standing goiter or degeneration in athyroid malignancy in older adults
Signs and Symptomso Thyroid pain referred to throat or ears, fever
and dysphagia
o Small tender goiter, lymphadenopathy Lab Tests
o Elevated ESR and WBC counto Normal Thyroid Function
Treatmento Antibiotic treatmento Surgery for abscess
Uncommon Complicationso Tracheal obstruction, septicemia,
retropharyngeal abscess, mediastinitis,
jugular venous thrombosis
SUBACUTE VIRAL THYROIDITIS
Aka granulomatous, de Quervains thyroiditis Many viruses implicated Common in Females ages 30-50 yrs than males There is patchy inflammatory infiltrate with
disruption of thyroid follicles and presence of
multinucleated giant cells
May progress to granulomas with accompanyingfibrosis
Figure 15. Clinical phases of Subacute viral thyroiditis
a. Thyrotoxic Phase: 6 weeks ;. Increased FT4, decreased TSH
b. Hypothyroid phase: decreased FT3, FT4,
c. Recovery Phase: Increased TSH eventually due to thyroid recovery.
Signs and symptomso May initial present with URTI like
symptoms
o Painful thyroid referred to jaw and ear;exquisitely tender
o Fevero Thyrotoxic symptoms appear abruptly
Lab Testso Elevated ESR and WBC counto Thyroid Function depends on phaseo May present with a low radioiodine
uptake initially
o Thyroid antibodies are low Treatment
o First Line: Large doses of Aspirin &NSAIDS
o Second Line/Alternative: Steroidso Monitor TSH and FT4 every 2 weeks
Thyrotoxic phaseo Propranolol to ameliorate symptomso Antithyroid drugs no role
Hypothyroid phaseo Levothyroxine
For a prolonged phase Low doses to allow TSH
mediated recovery
SILENT THYROIDITIS
Aka Painless Occurs in patients with underlying autoimmune
thyroid disease.
Post-partum thyroiditiso Occurs in 5% of women 3-6 months after
pregnancy
o May recur in subsequent pregnancies Lab tests
o Low ESR and WBC counto Thyroid function depends on phaseo May present with a low radioiodine uptake
initiallyo THYROID ANTIBODIES ARE PRESENT.
Treatmento Anti inflammatory agents (steroids) not
necessary
o Thyrotoxic phase Propranolol to ameliorate
symptoms
Antithyroid drugs no roleo Hypothyroid phase
LevothyroxineCHRONIC THYROIDITIS
Focal Thyroiditiso 20-40% of euthyroid autopsy caseso Associated with autoimmunity; TPO
antibodies are present
Hashimotos thyroiditis Riedels thyroiditis
o Rare; occurs in middle aged womeno Dense extensive fibrosis with no thyroid
dysfunction
o Maybe associated with idiopathic fibrosis atother anatomic sites
o Presents with painless goiter andcompressive symptoms
o Treatment: Surgical relief of compressivesymptoms.
SICK EUTHYROID SYNDROME
Any acute, severe illness can cause abnormalities ofcirculating TSH or thyroid hormone levels in the
absence of underlying thyroid disease.
Unless a thyroid disorder is strongly suspected, theroutine testing of thyroid function should be avoided
in acutely ill patients.
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
10/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 10 of 16
The major cause of these hormonal changes is therelease of cytokines such as IL-6.
The diagnosis of SES is frequently presumptive, giventhe clinical context and pattern of laboratory values;
only resolution of the test results with clinical
recovery can clearly establish this disorder.
Treatment of SES with thyroid hormone (T4 and/orT3) is controversial
***In sick euthyroid T4 is shunted to T3 (reversed) Decreased
FT3increased reversed T3; bodies way of adapting illness, to lessencatabolic rate: Findings: Low TSH, slightly high FT4, low FT 3
Figure 16. Clinical phases of sick euthyroid syndrome
AMIODARONE EFFECTS ON THYROID FUNCTION
Type III antiarrhythmic agent Structural relation to thyroid hormone; 39% iodine by
weight
Stored in adipose tissues; high iodine levels persist for6 months after discontinuation of the drug
Initial effect
Inhibit thyroid hormone release Decreased T4 Wolff Chaikoff Follow up effect Inhibits Deiodinase activity Metabolites function as weak antagonists of thyroid
hormone action
Increased T4, Decreased T3, Increased rT3 andtransient TSH increase (20mIU/L)
TSH normalize in 1-3 months***Hyperthyroidism (thyrotoxicosis)provide antithyroid drugs and
anti-inflammation
Amiodarone Effects HYPOTHYROIDISM
Correlated to iodine intake Higher incidence in iodine replete countries Pathogenesis: inability to escape from the Wolff
Chaikoff effect in autoimmune thyroiditis
More common in women and those with positiveTPO antibodies
Treatment: May continue amiodarone and just startlevothyroxine replacement
Amiodarone Effects THYROTOXICOSISType 1 AIT
With underlying thyroid problems (subclinicalHyperthyroidism/Nodular goiter)
Jod Basedow phenomenon leads to excessive thyroidhormone synthesis
Doppler shows increased vascularity Tx: Anti-Thyroid drugs
Type 2 AIT
No underlying thyroid problems
Drug induced lysosomal activation leading todestructive thyroiditis
Doppler shows decreased vascularity Tx: oral contrast agents, steroids
THYROID AND PREGNANCY
Five factors alter thyroid function in pregnancy
1. Transient increase in hCG during the first trimester,which stimulates the TSH-R and decreases TSH
2. Estrogen-induced rise in TBG during the firsttrimester, which is sustained during pregnancy
3. Alterations in the immune system, leading to theonset, exacerbation, or amelioration of an underlying
autoimmune thyroid disease
4. Increased thyroid hormone metabolism by theplacenta
5. Increased urinary iodide excretion Maternal hypothyroidism occurs in 23% of women of
child-bearing age and is associated with increased risk of
developmental delay in the offspring.
Women with a precarious iodine intake are most at risk ofdeveloping a goiter during pregnancy, and iodine
supplementation should be considered to prevent
maternal and fetal hypothyroidism and neonatal goiter.
TSH screening for hypothyroidism is indicated in earlypregnancy and should be considered in women who are
planning pregnancy, particularly if they have a goiter or
strong family history of autoimmune thyroid disease.
Thyroid hormone requirements are increased by 2550ucg/d during pregnancy.
GOITERDIFFUSE NONTOXIC GOITER
Simple goitero Most commonly caused by iodine deficiencyo Compensatory effort to trap iodideo Endemic goiter if it affects > 5% of the populationo Women>Meno Greater prevalence of autoimmune thyroid
disease
o Increased iodine demands during pregnancyo TSH levels normal to slight increase onlyo But probably there is increased sensitivity to its
effects
o Patient will present OBSTRUCTIVE SYMPTOMSGoitrogens Cassava root thiocyanate
Cruciferous vegetables brussels sprouts, cabbage,cauliflower
Milk from areas where goitrogens are present in grass S/Sxs
o Obstructive symptomso Tracheal obstruction esp substernal goitero dysphagiao External jugular vein - Pembertons sign
Treatment:
Iodine replacement Levothyroxine replacement Young pxs: 100 mcg/day targeting low to normal TSH Elderly: 50 mcg/day Efficacy greater for younger pxs, soft goiters Significant regression: within 3-6 months Surgery: Near total thyroidectomy Radioiodine: reduced goiter size by about 50% in the
majority of pxs in 6-12 months
NONTOXIC MULTINODULAR GOITER
Most nodules are polyclonal in origin TSH usually not elevated
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
11/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 11 of 16
Most are asymptomatic and euthyroid; Obstructivesymptoms
Ultrasound: Look for characteristics suggestive ofmalignancy
Levothyroxine replacement rarely effective to reducegoiter size
Radioiodine treatment may decrease goiter size by 40-50%
TOXIC MULTINODULAR GOITER Presence of autonomously functioning nodules Subclinical or mild thyrotoxicosis Elderly patient: tremors, atrial fibrillation or weight
loss
Aggravated by recent exposure to iodine Anti thyroid drugs
o May stimulate growth of goitero Spontaneous remission does not occur lifelong
tx
Radioiodineo Treat areas of autonomy and decrease goiter sizeo Treated areas may be replaced by other new
autonomous nodules
Surgery
Figure 17. Findings on thyroid scan: heterogenous uptake with areas of
increased and decreased uptake
HYPERFUNCTIONING SOLITARY NODULE
Solitary autonomously functioning thyroid nodule Mild thyrotoxicosis Medical treatment is not an optimal long term
treatment
Radioiodine ablation Surgery: Enuceation or lobectomy Ethanol injections or percutaneous radiofrequency
thermal ablation
Figure 18. Findings on thyroid scan: Focal uptake with diminished
uptake in the remainder (normal tissue) as activity in those areas are
suppressed
***Check TSH: if Decreased do thyroid scan if INCREASED
uptake no need for BIOPSY, but if DECREASED uptake- do
Biopsy, If purely cysticno need for biopsy.
THYROID CANCER
Most common malignancy of the endocrine system
Figure 19. Findings on thyroid scan
WELL DIFFERENTIATED
***Classified according to histologic features
Papillary
Most common 70-90% Histology: Psammoma bodies, cleaved nuclei with an
orphan-Annie appearance caused by large nucleoli,
and the formation of papillary structures
Locally invasiveFollicular
More common in iodine-deficient regions. Difficult to diagnose by FNA because the distinction
between benign and malignant follicular neoplasms
rests largely on evidence of invasion into vessels,
nerves, or adjacent structures
Hematogenous spread
Figure 20. Treatment of Well Differentiated
**Treatment: Surgery the RAI to destroy remaining tissues not
removed by surgery, e.g. on Lymph nodes. Provided suppressive
levothyroxine Decreased TSH (note: TSH stimulates growth of
thyroid cells) then monitor by blood test.
POORLY DIFFERENTIATED
Anaplastic
Poor prognosis Poor response to radioiodine treatment Chemotherapy ineffective
Others:
Medullary
Association with Multiple Endocrine Neoplasia 2 Serum calcitonin is a marker of residual or recurrent
disease
Lymphoma
Rapidly expanding thyroid mass Highly sensitive to external radiation (rapidly
expanding!)
SAMPLE CASES
Case 1: Mr. Gollum. What is his
problem (aside from losing thering)?
Appears anxious, keepsmuttering my precious
HR elevated BMI: 17 Neck mass with bruit Irregularly irregular bruit TSH low FT4 and FT3 are high
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
12/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 12 of 16
Case 2: Patient A at ICU bed 3 presents with palpitations on his
3rd HD (hospital day). TSH was requested which showed asuppressed TSH. Which of the following medications beinggiven to him could explain this findings?
a. Dobutamineb. Hydrocortisone
c. Simvastatind. Levothyroxine
Anwer: both b&d Dopamine, glucocorticoids and somastatin
suppress TSH when these agents are administered in
pharmacological doses.
Case 3: Patient A came in for screening for thyroid disease.
Which of the following times is the best time to perform the
TSH?
a. 8 am after overnight fastb. 12 noonc. 6 pm
d. 12 mn
Answer: any of the following is correct; since TSH has
relatively long half-life and no need to undergo fasting. TSH is
released in a pulsatile manner and exhibits a diurnal rhythm highest level at night. However, TSH excursions are modest
compared to other pituitary hormones because of TSH has a
relatively long plasma half-life. Consequently, single
measurements of TSH are adequate for assessing its circulating
level.
Case 4: Patient I came in for her prenatal check-up. She asks
you, what is the recommended daily intake of iodine for a
pregnant like her?
a. Less than 90 ug/day
b. 90-120 ug/dayc. 150-250 ug dayd. 250 ug/day
Answer: D, refer to table of recommended daily intake
Case: 5. Px F, a 34 yr old female came in with the following
thyroid function results. Low T4 and T3 but normal Free T4
and TSH. What is your explanation for the thyroid function
pattern?a. X linked TBG Deficiency
b. Pregnancy
c. OCP used. Euthyroid Hyperthyroxinemia
Answer: A
Case 6 : SE is a 64/F admitted at the ICU for Heart Failure forthe past 14 days referred for further evaluation of palpitations.She has no prior history of thyroid illness. No other signs orsymptoms of thyroid dysfunction. Thyroid function tests
showed low TSH, slightly high FT4, and low FT 3. Yourimpression is:
A. Secondary hypothyroidismB. HyperthyroidismC. Subacute Thyroiditis
D. Sick Euthyroid Syndrome
Answer: D
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
13/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 13 of 16
APPENDIX
Figure 21. Evaluation of Hypothyroidism
Figure 22. Evaluation of Thyrotoxicosis
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
14/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 14 of 16
Table 4. Thyroid Patterns
THYROID
DISORDERTSH FRE T4 TOTAL T4
SIGNS AND
SYMPTOMS
Hyperthyroidism Low High High Present
Subclinical
HyperthyroidismLow Normal Normal Absent
Primary
HypothyroidismHigh Low Low Present
Secondary
Hypothyroidism
Low or
InappropriatelyNormal
Low Low Absent/Present
Subclinical
HypothyroidismHigh Normal Normal Absent
Increased TBG Normal Normal Increased Absent
Decreased TBG Normal Normal Decreased Absent
***Primary hypothyroidism: TSH, pituitary is compensating, in secondary: problem is in pituitary or hypothalamus so TSH (inadequate
elevation in TSH or remain inappropriately normal since normal response is high and normal response means abnormal)
*** or TBG and total T4, but NORMAL, TSH and FT4, patient is asymptomatic
Figure 23. Methimazole vs Propylthiouracil
Table 5. Comparison of drugs used to treat hyperthyroidismINHIBIT
ORGANIFIC
ATION
IMPAIR
CONVERSION OF
T4 TO T3 BY D1
IODIDE
TRANSPORT
INHIBITORS (NIS)
INHIBIT
HORMONE
RELEASE
ADDITIONAL INFO
PTU Yes Yes (600mg)
Methimazole Yes
Thiocyanate Yes
Iodine (SSKI) Yes
3 drops BID with 7-10 day
preop to decrease
vascularity
IpodateIopanoate Yes Yes
Lithium Yes Target Lithium: 1meq/L
DexamethasoneYes (additive to
PTU)
With addition of PTU andSSKI will produce rapid T3
decrease in 48 hours
Propanolol Weakly
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
15/16
Sarah M. | Hezer| Mariz| April| Tsen |Victor UERM 2015B Page 15 of 16
Figure 25. Burch Wartofsky Scoring
Figure 27. Approach to patient with thyroid nodule (ATA 2009 Guidelines for Thyroid Nodules & DTC)
-
7/27/2019 2MEDICINE8 Thyroid Gland Disorders UERM2015B.pdf
16/16