Downloaded from bjo.bmj.com on August 10,2012 - Published by group bmj.com Penetrating keratoplasty using femtosecond laser-enabled keratoplasty with zig-zag incisions versus a mechanical trephine in patients with keratoconus Ronald N Gaster, Oanna Dumitrascu, Yaron S Rabinowitz ABSTRAGT Background/aims This paper will compare the visual outcomes of two dffierent penetrating keratoplasty (PKPI techniques in patients with keratoconus. lt is a retrospective comparative surgical case series of 116 keratoconus patients {137 eyes} who had PKP at the Cornea Eye Institute, Bevedy Hills, California, USA. Methods 56 keratoconus patients (66 eyesl underwent femtosecond laser-enabled keratoplasty (FLEKI with a zig-zag incision configuration. Their visual parameters were compared with those of 60 patients (7'l eyes) who had traditional blade mechanical trephination PKP. The range of follow-up was between 3 and 6 months. Jhe main outcome measures included uncorrected visual acuity and best spectacle-corected visual acuity (BSCVA), manifest refractive spherical equivalent and topographically determined astigmatism. Results BSCVA was significantly better as early as 3 months postoperatively (p:0.001) in the FLEK group. Visual recovery to20140 after 3 months was significantly better in the FLEK group (p<0.001). Topographic astigmatism was lower in the FLEK group, but the difference between the two groups reached significance only at 3 months of follow-up (p:0.001 ). Postoperative comolications noted were not different between the two groups Conclusions Faster visual recovery and better long-term outcomes were observed in keratoconus oatients who had FLEK compared with those who had the mechanical PKP procedure with 6 months of postoperative follow-up. INTNODUCTION The femtosecond laser is gaining rapid and wide- spread acceptance for use in corneal surgery. In penetrating keratoplasty (PKP), initial laboratory models demonstrated superior mechanical stabiliry after laser keratoplasty compared with manual keratoplasty,l and the first human full-thickness corneal transplant using femtosecond laser was oerformed in 2005." Preliminarv results on the applicability of laser-enabled keratoplasty in different corneal disorders have been reported on a relatively small number of patients and with- Iimited follow-up. These reports demonstrate a biomechanically stable wound, excellent wound apposition, faster suture removal and faster recovery of best spectacle-corrected visual acuiry (BSCVA), accompanied by moderate astrgmatrsm.- " In 2007 , 50 122 PubMed corneal transplants were performed in the USA (statistics provided by Eye Cornea Eye Institute, Beverly Hills. Califomia. USA Gonespondence to Dr Yaron Habinowitz, Cornea Eye Institute, Cedars Sinai, 50 N. La Cienega Blvd , Suite 340, Bevertv Hills, CA 90211. USA; [email protected] Accepted 9 June 2012 Bank of America). PKP is the standard treatment in advanced keratoconus wlth 72-20/" of patients eventually requiring PKP at a relatively young age." As femtosecond laser-enabled keratoplasty (ILEK) has been reported as a safe and stable procedure,a specifically in this group of young patients, earlier visual rehabilitation and decreased short and long- term complication rates would greatly benefit them. This study presents visual outcomes with up to 6 months of follow-up after femtosecond laser- enabled ig-zag-shaped keratoplasty in keratoconus patients and compares the outcomes with the mechanical trephine keratoplasty (PKP) technique in a similar cohort. METHODS Patient selection This is a retrospective chart review study. The ethics committee of the Eye Surgery Center of Beverly Hills approved this research. Our research adheres to the tenets of che Declaration of Helsinki. We analysed visual outcomes at 3 and 6 months of 116 keratoconus patients (137 eyes) who had corneal transplants at the Cornea Eye Institute, Beverly Hills, California, USA. All procedures were performed by the same surgeon (YSR) using the same surgical technique. Iifty-six keratoconus patients (66 eyes) had ILEK, while 60 keratoconus patients (Zl eyes) had traditional PKP. All conventional PKP surgeries were performed consecutively before acquiring the femtosecond laser. All ILEK surgeries were performed consecutively after the femtosecond laser was obtained. There were no selection criteria other than the need for corneal transplant sur8ery- All patients received a complete ophthalmolog- ical examination preoperatively and post- operatively at 1 month, 3 months and 6 months. All patients were diagnosed with advanced kera- toconus preoperatively and were either contact lens intolerant or had a central comeal scar, with PKP as the only therapeutic option for adequate visual rehabilitation. Deep anterior Iamellar keratoplasty patients were not included in this study. Suture removal was started at 3 months in both groups and was complete by 6 months in the FLEK group and later in the PKP group. The parameters collected for comparative ana-lysis were: uncor- rected visual acuity, BSCVA manifest refractive spherical equivalenr and topographically deter- mined astigmatism. Videokeratography was G'ebFvrq$trnrffcftyrythbttb+frt&PgrttHf,dyerft0?le++dffie0sffuffBm.r puolishins Group Ltd under ticencdj 5

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Downloaded from bjo.bmj.com on August 10,2012 - Published by group bmj.com
Penetrating keratoplasty using femtosecondlaser-enabled keratoplasty with zig-zag incisionsversus a mechanical trephine in patientswith keratoconusRonald N Gaster, Oanna Dumitrascu, Yaron S Rabinowitz
ABSTRAGTBackground/aims This paper will compare the visualoutcomes of two dffierent penetrating keratoplasty (PKPI
techniques in patients with keratoconus. lt isa retrospective comparative surgical case series of 116keratoconus patients {137 eyes} who had PKP at theCornea Eye Institute, Bevedy Hills, California, USA.Methods 56 keratoconus patients (66 eyesl underwentfemtosecond laser-enabled keratoplasty (FLEKI witha zig-zag incision configuration. Their visual parameterswere compared with those of 60 patients (7'l eyes) whohad traditional blade mechanical trephination PKP. Therange of follow-up was between 3 and 6 months. Jhemain outcome measures included uncorrected visualacuity and best spectacle-corected visual acuity(BSCVA), manifest refractive spherical equivalent andtopographically determined astigmatism.Results BSCVA was significantly better as early as3 months postoperatively (p:0.001) in the FLEK group.Visual recovery to20140 after 3 months was significantlybetter in the FLEK group (p<0.001). Topographicastigmatism was lower in the FLEK group, but thedifference between the two groups reached significanceonly at 3 months of follow-up (p:0.001 ). Postoperativecomolications noted were not different between the twogroupsConclusions Faster visual recovery and better long-termoutcomes were observed in keratoconus oatients whohad FLEK compared with those who had the mechanicalPKP procedure with 6 months of postoperative follow-up.
INTNODUCTIONThe femtosecond laser is gaining rapid and wide-spread acceptance for use in corneal surgery. Inpenetrating keratoplasty (PKP), initial laboratorymodels demonstrated superior mechanical stabiliryafter laser keratoplasty compared with manualkeratoplasty,l and the first human full-thicknesscorneal transplant using femtosecond laser wasoerformed in 2005." Preliminarv results on theapplicability of laser-enabled keratoplasty indifferent corneal disorders have been reported ona relatively small number of patients and with-Iimited follow-up. These reports demonstratea biomechanically stable wound, excellent woundapposition, faster suture removal and fasterrecovery of best spectacle-corrected visualacuiry (BSCVA), accompanied by moderateastrgmatrsm.- "
In 2007 , 50 122 PubMed corneal transplants wereperformed in the USA (statistics provided by Eye
Cornea Eye Institute, BeverlyHills. Califomia. USA
Gonespondence toDr Yaron Habinowitz, CorneaEye Institute, Cedars Sinai, 50N. La Cienega Blvd , Suite 340,Bevertv Hills, CA 90211. USA;[email protected]
Accepted 9 June 2012
Bank of America). PKP is the standard treatment inadvanced keratoconus wlth 72-20/" of patientseventually requiring PKP at a relatively young age."As femtosecond laser-enabled keratoplasty (ILEK)has been reported as a safe and stable procedure,aspecifically in this group of young patients, earliervisual rehabilitation and decreased short and long-term complication rates would greatly benefitthem.
This study presents visual outcomes with up to6 months of follow-up after femtosecond laser-enabled ig-zag-shaped keratoplasty in keratoconuspatients and compares the outcomes with themechanical trephine keratoplasty (PKP) techniquein a similar cohort.
METHODSPatient selectionThis is a retrospective chart review study. Theethics committee of the Eye Surgery Center ofBeverly Hills approved this research. Our researchadheres to the tenets of che Declaration of Helsinki.
We analysed visual outcomes at 3 and 6 monthsof 116 keratoconus patients (137 eyes) who hadcorneal transplants at the Cornea Eye Institute,Beverly Hills, California, USA. All procedures wereperformed by the same surgeon (YSR) using thesame surgical technique.
Iifty-six keratoconus patients (66 eyes) hadILEK, while 60 keratoconus patients (Zl eyes) hadtraditional PKP. All conventional PKP surgeries wereperformed consecutively before acquiring thefemtosecond laser. All ILEK surgeries wereperformed consecutively after the femtosecondlaser was obtained. There were no selection criteriaother than the need for corneal transplant sur8ery-
All patients received a complete ophthalmolog-ical examination preoperatively and post-operatively at 1 month, 3 months and 6 months.All patients were diagnosed with advanced kera-toconus preoperatively and were either contact lensintolerant or had a central comeal scar, with PKP asthe only therapeutic option for adequate visualrehabilitation. Deep anterior Iamellar keratoplastypatients were not included in this study. Sutureremoval was started at 3 months in both groupsand was complete by 6 months in the FLEK groupand later in the PKP group. The parameterscollected for comparative ana-lysis were: uncor-rected visual acuity, BSCVA manifest refractivespherical equivalenr and topographically deter-mined astigmatism. Videokeratography was
G'ebFvrq$trnrffcftyrythbttb+frt&PgrttHf,dyerft0?le++dffie0sffuffBm.r puolishins Group Ltd under ticencdj 5
Downloaded from bjo.bmj.com on August 10,2012 - Published by group.bmj.com
performed on all patients with the topographic modellingsystem (TMS 4; Tomey, Japan) using a saggital algorithm andthe absolute scale.
Surgical techniquesAll patients reviewed and signed the informed consent for PKP.
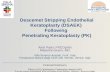
FLEK techniquePatients received 10 cc of marcaine and lidocaine as a combina-tion of rerrobulbar and peribulbar anaesrhesia. The centre of thecornea was marked with a marking pen before the procedure.The Ag-zag ILEK pattern was designed on the Intralase laser(Abbott Medical Optics, Irvine, California, USA) with a 2.9 mmouter diameter and 6.7 mm inner diameter- It was set at a depthof 800 pm to ensure that there was complete perforation of theincision. This is safe in our setting because we have an oPeratingroom with a door leading directly to the Intralase, decreasingthe time from laser trephination to removal of the host buttonto less than 10 min. The rest of the parameters are outlined infigure 7. A same-size donor with the same og-=ag parameterswas pre-ordered from the eye bank before the surgery. Thisallowed for the best postoperative frt o[ donor into recipient.After completion o[ the host cut, the patient was wheeledthrough the door from the femtosecond laser to the operatingroom and the eye was prepped and draped in the usual sterilefashion for intraocular surgery. After a speculum was put in theeye, the wound was opened with a Sinskey hook superiorly andthe button was removed entirely with a 0.12 forceps. The pupilwas constricted with miochol, and healon was put into theanterior chamber to protect the lens. The donor comea was thensutured onto the host with 12 interrupted 10-0 nylon sutures onthe radial marks made by the Intralase. This was followed bya running suture in between the interrupted sutures atapproximately 50% corneal depth. The running suture wasburied within the wound and the knot cut and trimmed. Theviscoelastic was irrigated out of the antedor chamber. Thepatient was given subconjunctival decadron and vancomycin.Erythromycin ointment was put in the eye and a patch andshield were placed on the eye.
Traditional mechanical (PKPI techniqueThe PKP technique was identical to the FLEK technique exceptthat a Barron Hessburg 7.5 mm trephine was used to remove thediseased button and a 7 .5 mm Katena manual trephine was usedto fashion the donor cornea.
Suture removal and measurement of topographic astigmatismIn both groups suture removal was started at 3 months. Allsutures were out by 6 months in the FLEK group and later in thePKP group. Sutures were removed when they became loose orwhen the corneal wound appeared well healed.
Statistical analys€sThis was performed with SAS V9.0. For quantitative traits,comparisons between two SrouPs were tested by the Student's ttest when variables had a normal distribution or by the non-oarametric Wilcoxon rank test when traits deviated trom normaldistribution. fhe A2 test was used to compare proportions ofqualitative traits between groups. As baseline measures werehighly correlated with outcome measures during each technique,we also conducted a linear regression model to compare twogroups by incorporated baseline values of each trait, as well asage and gender, as covariates.
POSTERIOR SIDE CUTAIVTERIOR DEPTHPOSTERIOR STDE CUTPOS?ERIOR SIDE CTITPOSTERIOR DEtrTHPOSTERIOR SIDE CIITPOSTERIOR SIDE CUTPOSTERIOR SIDE CT'T
ON270
DIAPIETER. 'I .9ENERGY 2.308s0AIVGLE 30
SPOT SEP 4I,AYER SEP 4
RING LAMELI,AR CIIILAII,IBLI.AR DEPTH IN CORNEAIJAMEI'I'AR OIITER DIAMBTERLAII{ELI,AR INNER DTA}iIETERI,AMELLAR START POSITIONLAII{EI,LAR ENERGYI.AI,IELI,AR TA$IG SPOT SEPLAMELLAR RAD SPOT SEP
FUIL LAMELITAR CUT
AI\MERIOR SIDE CTIT ONPOSTERIOR DEHTTI 330AI{TERIOR SIDE CIIT DIAI{ETER 7.8ANTERIOR SIDE CUT BNERGY 2.3OANTERIOR SIDE CUT 1 POS OANTERIOR SIDE CUT 1 AhIGLE 360ANTERIOR STDB CI'T 2 POS 180AIITERIOR SIDE CIIT 2 A}IGLE O
ANTERTOR SIDE CUf ANGI-,E 30A}ITERIOR SIDE EUT SPOT SEP 5AI{TERIOR SIDE CITT I.AYER SEP 5DEPTH IN CONTACT GI,ASS 50
AI,IGNIT{EIIT INEISIONS ONINCISIONS L2INCISIONS DEHIH IN GL,ASS 20INCISIONS POSTERIOR DEPTH ].OOINCISIONS ENERGY 1.50INCISIONS LBNGTH 1OOOINCISIONS WIDTI{ 10INCISIONS SPOT SEP 4INCISIONS I"AYER SEP 4INCISIONS LINE SEP 2
Figure 1 Femtosecond laser parameters used for corneal transplant.
p Values less than 0.05 were considered statisticallysignifrcant.
RESULTSWe included 56 keratoconus patients (66 eyes) who underwentILEK surgery and 60 patients (71 eyes) with PKP surgery in theanalysis. All eyes in the two groups were followed at 3 monthsand most of them were followed at 6 months (54 vs 7l).
There were more men in the ILEK group than in the PKPgroup (74.2% vs 56.31", p:0.03). No statistically significantdifference of age was identifred between the two groups (FLEKgroup: 38.7 years (range 17-75); PKP group: 44-Syears (range13-80); p:0.0n.
ON300'1 .96.?our2.3555
OFF
2of5 Gaster BN, Dumitrascu 0. Rabinowiu YS. Br J ophthalmol ,2012l,. doi:10.1'136/biophthalmol-2012-301662
Donvnloaded from bjo.bmj.com on August 10,2012 - Published by group.bmj.com
Table 1 Baseline characteristics of the two gloups of patients
Fl.Elt (n=65| PKP (n=71| p Value
Logmar UCVA (SD)
Logmar BSCVA (SD)
MBSE {SD}TA (SD}
1.44 {0.57}0.77 (0.52)
-7.67 (3.811
5.s4 (3.77)
1.s1 (0.661
r.11 {0.691
-6.70 (1.471
6.39 13.591
0.760.0020.380.$
BSCVA, best spectaclecorrected visual acuity; FLEK femtosecord lasergnHedkeratoplasty; PKP, penetrating kerdtodasty; TA, topogBphically detemined astigmatism;UCVA, unconected visual acuity.
There were no significant differences for most ocular param-eters, except for BSCVA at baseline between the two SrouPs(table 1).
Three months atter corneal transplantation was performed,BSCVA and topographic astigmatism were significantly betterin che ILEK group compared with the PKP group of Patients(table 2). BSCVA of 20/40 or greater at 3 months was obtainedin 28 cases (42.42%) in the ILEK group compared with 9.7% ofcases in the PKP group (p<0.001).
At the 6-month follow-up time point, the ILEK group showedbetter values for all the parameters studied, but the dlfferencebetween the groups did not reach statistical significance(table 2).
Topographic astigmatism values improved in a time-depen-dent fashion; although they were lower in the ILEK group ateach follow-up time point, they were statistically lower only at3 months of follow-up (fugure 2).
Although there were continuous improvements of the mani-fest refractive spherical equivalent during the follow-up in theILEK group (table2), no statistically significant differences wereidentified between the two groups after adiusting for baselinevalues (all p>0.05).
All procedures were performed without intraoperativecomplications. Postoperative complications noted were notdifferent between the two groups. We had one case (1.51%) ofgraft failure after ILEK and two cases (2.81%) after PKP. Intra-ocular hypertension or glaucoma was observed in6.04/" of casesafter FLEK vercus 4.22/" after PKP (p:0.4 No cases of wounddehiscence were seen after suture removal and no cases o[postoperative graft rejection.
Drscussr0NDifferent laser types and different procedure shapes are availablefor keratoplasty incisions. Three lasers are approved by the US
Table 2 Visual outcomes at 3 and 6-month time intervals aftertreatment
FIEK ln:661 Pl(P (n=7tl p Value
3 months 6 months
Figure 2 Time dynamic of topographically determined astigmatism(dioptres) (p:0.001 ). FLEK, femtosecond laser-enabled keratoplasty;PKP, penetrating kemtoplasty.
Iood and Drug Administration for corneal cuts: Intralase(lntralase Corp., division of Abbott Medical Optics); Femtec(20/10 Perfect Vision; CmbH, Heidelberg, Cermany) andFemtoLDV (Ziemer Ophthalmic Systems AC, Port,Switzerland).Z 8 Different shapes with different indicationshave been proposed, some of which include: top hat, mushroom,dg-^g, Chrisimas tree, zig-squared, tongue and groove.3 e
We chose the zig-zag technique (figure 3) for keratoconuspatients because the angled incisions from zig-zag-shaped kera-toplasty had been described as being more biomechanicallyfavourable, optical coherence tomography images showingexcellent alignment of the anterior and posterior layers of thetransplant, smooth transition along the anterior surface andexcellent host-graft alignment.'
In a previously reported study with other corneal disorders,the femtosecond laser-generated Ag-zag-shaped incisionsresulted in a more rapid recovery of BSCVA and induced lessastigmatism compared with conventional blade trephinationPKP.10 These data together with the reduced procedure timelinfluenced us to make this our procedure of choice. Similarstudies have reported results on a small number of keratoconuspatients2 10 tt a.td demonstrated faster recovery of BSCVA andless induced astigmatism at 3 months, but they did not reporton visual outcomes at a later time point or make comparisonwith the mechanical techniques.
Farid et allo reported on 49 eyes of 43 patients who underwentig-rag ILEK versus 17 eyes of 14 patients who underwentconventional PKP. AII PKP were closed with an identical 24-biterunning nylon suture technique. The Postoperative follow-upranged from 1 to 12 months. There was a significant differencein average astigmatism between the groups at postoperativemonths 1 (p:0.013) and 3 (p:Q.Ql8). By month 3, the averageastigmatism was 3 dioptres (D) in the ILEK zig-zag group and4-46D in the conventional group. Of the patients with normalmacular and opcic nerve function, a signi&cant difference inBSCVA was seen at month 1 (p:0.0003) and month 3(p:0.ooo, with 81% of the FLEK zig-zag group versus 45% ofthe conventional group achieving BSCVA of 20/40 or greater bymonth 3 (p:0.03). They concluded that the ILEK ig-u9-shaped incision results in a more rapid recovery of BSCVA andinduces less astigmatism compared with conventional PKP.
8
7
6
1
0
3 MonthsLogmar UCVA (SD)
Logmar BSCVA (SD)
MRSE (SD)
TA (SD)
0.9r {0.55}0.46 (0.40)
-2.79 (5.66)5.0s {3.55}
0.e4 (0.37) 0.420.69 (0.381 0.001
-0.64 (5.66) 0.057.33 (4.61) 0.001
Fl"E( (n:5ll PlO (n=7ll p Value
6 MonthslogMar UCVA (SD]
LogMar BSCVA (SDlMRSE (SD}
TA (SD}
0.91 (0.691
0.44 {0.49}3.76 (4.631
4.76 (3.4r I
1.00 (0.70) 0.350.57 (0.58) 0.12
-3.31 (5.5r) 0.525.91 (4.531 0.15
BSCVA, best spectacle-corrected visual acuity; FLEK femtosecond laser-enabledkeratodNty; PKP, penetrating keratodasty; TA, topographic2lly detemined astigmatism;UCVA, unconected visual acuity.
Gaster RN, Dumitrascu 0, Rabinowitz YS. Br J 1phthalnol 120121. doi:10 1 136/bjophthalmol-2012-301662 3of5
Downloaded from bjo.bmj.com on August 10,2012 - Published by group.bmj,com
Figure 3 Diagram of femtosecondlaser-enabled keratoplasty zig-zagrncrsron.
Bahar et ala compared 23 eyes that had top-hat ILEK with 35eyes that had conventional PKP At 12 months postoperatively,the mean cylinder was similar between the two groups: 3.6 D(SD 1.9) in the ILEK group and 4.1 D (SD 1.8) in the PKP group.The mean endothelial cell loss was significantly lower at12 months in the FLEK group compared with the PKP group(32.4% vs 408%). The mean time to suture removal was4.1 months (SD 1.2) in the ILEK Sroup versus 9.7 months (SD1.1) in the traditional PKP group.
Huer et all2 analysed eight eyes that underwent FLEK andconcluded that long-term control of postoperative astigmatismremains an issue after ILEK, and that suture technique still playsan important role in postoperative astigmatism magnitude.Chamberlain et al'' compared postoperative outcomes inzig-zagILEK with conventional PKP with 2years of postoperativefollow-up. The authors found a significant improvement inastigmatism before but not after the 6-month postoperativefollow-up period. However, they did not find sigruficant visualimprovement of BSCVA in the ILEK group compared with theconventional PKP group.
Our results on a larger number of keratoconus patientsshowed a signifrcant improvement of BSCVA and astigmatismearly on. Iaster visual recovery to the level of being able toobtain a driver's licence and allowing patients to return tofunctional work earlier represents a great benefit, especially inthis young group of patients who are in the most productiveperiod of their lives.
Despite the fact that there was no statistically significantdifference between the ILEK and the PKP groups in terms oftopographically induced astigmatism at 6 months, the FLEKprocedure has become our procedure of choice. There are severalreasons for this: (1) visual acuity is better at both postoperativetime intervals (3 and 6 months) in our study, which is critical ina young group of patients who are in their actively productivephase of bfe; (2) the procedure produces a stronger and morestable wound because of its larger surface area, making the eyeless prone to corneal rupture; (3) the procedure is much fasterwith the eye being open for a very short period of time, whenthe laser is in or very near the operating room, making thisa much safer procedure and significantly reducing the chance o[
intra-operative complications. An added benefit, as suggested bythe study by Bahar et al,a is that there is less endothelial cell lossin the FLEK group versus the PKP group, suggesting that thegrafts may survive longer in this group of patients.
Even though PKP has been the standard treatment foradvanced keratoconus, the incidence of cases with keratoconusthat need a PKP has reduced in recent years due to alternativetreatments, such as corneal crossJinking, and a major trend todeep anterior lamellar keratoplasty, in order to preserve thepatient's own endothelium.
Iuture research with different pattern types geared toimproving donor-host alignment might also ultimately allowus to achieve our goal of an astigmatism-free or at leastsignificantly reduced astigmatic result in the FLEK procedure.
G0ilctusl0NIaster visual rehabilitation and better long-term visual acuity,earlier suture removal, a biomechanically stronger cornealwound, safety, rapidity of the procedure and less endothelial cellloss, make ILEK our procedure of choice in patients withadvanced keratoconus whose only option is a corneal transplant.One of the limits of this paper is the retrospective nature of thestudy. A future randomised, prospective clinical trial will be ableto clarify further the true benefits of the ILEK procedure overconventional PKP.
Gontibutors All authors contributed t0 the writing, editing and data collection for thispaper
Funding This work was supported by Eye Defects Research Foundation grant 005.
Gompeting interests None
Ethics apployal Ethrcs approval was provided by the ethics committee of the Eye
Surgery Center of Beverly Hills
Pationt consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed
REFEBENCES1 Steineft BF, lgnacio TS, Sarayba MA "Top hal'-shaped penetrating keratoplastyusing the femtosecond laser, Am J 0phthalmol 2007;113:689-912 Slade SG, Applications Jor the femtosecond laser ln corneal surgery Curr 0pin1phthalnol 2007;18:338-41
4of5 Gaster RN, Dumitrascu 0, Rabinowrtz YS Br J 0phthalmol i2012). doi:10 1136/bjophthalmol-2012-301662
Dovvnfoaded fiom bjo.bmj.com on August 10,2012 - Published by group.bmj.com
L
10.
11.
12.
3
i
5
o
7
I
Steinort RF. Femtosecond laser enabled keratoplasty IFLEKI Ann 0phhalnol/Sko/nel 2009;11:6-9Bahar l, Kaiserman l, Lange A, ef a/ Femtosecond laser versus manual dissecti0nfor top hat penetrating keratoplasty Br J 0phhalnol 2009;93:73-8Fadd M, Kim M, Steinert RF. Besults 0f penetrating keratoplasty performed witha femtosecond laser zigzag incision: initial rcpoft 1phthalnolow2007:l1l:,2208-12Pramanik S, Musch DC, Sutphin JE, et a/ Extended long-term outcomes 0fpenetrating keratoplasty for keratoconus 1phthalnohgy 2006;1 t 3:1 633-8Holzer MP, Rabsilber TM, Auffarth GU Penetnting kentopbsty using fernt0secondlaser Am J 0phthalmol 2UJ7:113:524-EPor YM, Cheng JY, Parthasanthy A, et a/. outcomes oi ferntosecond laser-assistedpenetrating keratoplasty An J ophthalnol 2ffi8:145:112-4
Price FW Jr, Price M0. Femtosecond laser shaped penetrating keratoplasty: on+year results utilizing a top-hat configuratim. Arn J 0plrthalnol 2t[8;ll5:210-14Fadd M, Steinert RF, Gaster HN, a a/ Comparison of penetratlng keratoplastyperformed with a femtosecond laser zig-zag incisim versus conventional bladetrephination 0phthalmolqgv 2$9;1 16:1 638-43Burato L Btihm E lhe use of the femtosecond laser in penetrating keratoplastykn J 0phthalnol 2007',141:137-42Heur t, Tang M. Vu S. at a/. Inwstigation of femtosecond laser-enabledkeratoplasty wound geunetry using optical coherence tomography Cornea201 1;3ll:889-94Ghambodain WD, Rush SW, Mathen WD. ef a/ Comparison of femtosecond laser-assisted keratoplasty versus conventional penetrating keratoplasty. qphthalnology201 1;118:486-91
Gaster BN, Dumitrascu 0, Rabinowitz YS. Br J 0phttnlnol (20121. doi:10.l13Vbjophthalmol-20l2-301662 5of5
Downfoaded from bjo bmj.com on August 10,2012 - Published by group.bmj.com
Penetrating keratoplasty using femtosecondf aser+nabled keratoplasty with zig-zagincisions versus a mechanical trephine inpatients with keratoconusRonald N Gaster, Oanna Dumitrascu and Yaron S Rabinowitz
Br J Ophthalmol published online July 11,2012doi : 1 0. 1 1 36/bjophthalmol-201 2-301 662
Updated information and services can be found at:http://bjo.bmj.com/contenUearly/2Ol2lOT ll0lbrophthalmol-2012-301662.full.html
References
P<P
Emailalertingservice
Ihese include:
This article cites 13 articles, 1 of which can be accessed free at:http://bio.bmj.com/contenUearly/2O12l07l'lOlUfophthalmol-2012-30l662.full.html#reflist-1
Published online July 11 ,2012 in advance of the print journal.
Receive free email alerts when new articles cite this article. Sign up inthe box at the top right corner of the online article.
TopicCollections
Articles on similar topics can be found in the following collections
Ophthalmologic surgical procedures (989 articles)Cornea (397 articles)Ocular surface (472 articles)Optic nerve (569 articles)Optics and refraction (396 articles)
Advance online articles have been peer reviewed, accepted for publication, edited andtypeset, but have not not yet appeared in the paper joumal. Advance online articles arecitable and establish publication priority;they are indexed by PubMed from initialpublication. Citations to Advance online articles must include the digital object identifier(DOls) and date of initial publication.
To request permissions go to:http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:http J/group.bmj.com/subscribe/
Domfoaded from bjo.bmj.com on August '10,2012 - Published by group.bmj.com
Notes
Advance online articles have been peer reviewed, acc€pted for publication, edited andtypeset, but have not not yet appeared in the paper joumal. Advance online articles arecitable and establish publication priority;they are indexed by PubMed from initialpublication. Citations to Advane online articles must include the digital object identifier(DOls) and date of initial publication.
To request permissions go to:http://group.bmJ.com/grou p/rlght3-licenslngrpermisslons
To order reprints go to:http:/iou mals.bmj.com/cgi/r6printform
To subscribe to BMJ go to:http://group.bmJ.com/subscrlbe/
Related Documents