Nasolacrimal Stents in the Management of Epiphora: Medium-term Results of a Multicenter Prospective Study Carlos Lanciego, MD, Silvia De Miguel, MD, Miguel Perea, MD, Cristo ´ bal Cano, MD, Isaac Ruíz García, MD, Julio Dávila, MD, Cristina Ibarburen, MD, Nicola ´s Toledano, MD, Rufo Rodriguez-Merlo, MD, and Lorenzo García García, MD PURPOSE: To evaluate in a prospective multicenter setting the clinical utility of polyurethane stents in the percuta- neous management of epiphora. MATERIALS AND METHODS: Patients (N 5 163; age range 5 22– 85 y, mean 5 52 y; 29 men, 134 women) with severe epiphora had stents (n 5 183) inserted under fluoroscopic guidance in 180 lacrimal systems (unilateral 5 146; bilateral 5 17) to treat complete (n 5 172) or partial (n 5 8) obstruction of the nasolacrimal duct or sac. The junction between sac and duct was the most frequent location (n 5 102), followed by the sac alone (n 5 48), and the duct alone (n 5 30). The etiology of the obstruction was idiopathic in 113 cases (63%) and chronic dacryocystitis in 67 (37%). The set designed by Song was used in all patients and the original technique was slightly modified by the authors. All patients were treated on an outpatient basis. Average time of the procedure was 14 minutes (range 5 3–70 min). RESULTS: Initial technical success rate of stent placement was 97%. Resolution of epiphora was complete in 175 eyes and partial in five. On follow-up (mean 5 450 d; range 5 8 –730 d), 157 of 183 stents remained patent (85.8%). Of the 24 obstructed, 19 were easily withdrawn and 17 of these patients remained asymptomatic for a mean of 15 months (secondary patency rate 5 89.5%). CONCLUSIONS: The procedure is simple and safe. It can be performed on an outpatient basis and the original technique could be improved with some technical modifications. It is well tolerated by patients and may be considered as a valid alternative technique for the resolution of epiphora. Index terms: Epiphora • Lacrimal gland and duct, stenosis or obstruction • Stents and prostheses J Vasc Interv Radiol 2001; 12:701–710 Abbreviations: DCG 5 dacryocystography, DCP 5 dacryocystoplasty, DCR 5 dacryocystorhinostomy EPIPHORA (also known as tearing or wet eye) can be caused by reflex hy- persecretion of tears as a result of in- fection, irritation of anatomic origin (eg, eyelid malformations, trichiasis), or obstruction of the lacrimal drainage system. Epiphora secondary to lacri- mal obstruction is a common (3% of clinical consultations) ophthalmologic problem (1,2). Although there are many causes of lacrimal outflow ob- struction, most cases are caused by id- iopathic inflammation and scarring of the nasolacrimal system. It is an an- noying disability, and its continuance tends to provoke chronic irritative lac- rimal conjunctivitis and, sometimes, eczematous eyelids (3,4). Most cases of acquired obstructions occur in adult- hood and are not related to trauma, neoplasm, or systemic disease. Involu- tional stenosis is probably the most common cause of nasolacrimal ob- struction in older individuals; women are affected twice as often as men. The histopathologic cause of obstruction remains uncertain, but compression of the duct by inflammatory infiltrates and edema precede development of chronic dacryocystitis accompanied by pain and discomfort (1,5). The appropriate therapy for lacri- mal obstruction depends on its cause and extent. A probe is usually intro- duced in cases of congenital stenosis. Intubation with a silicone tube causes discomfort because the tube needs to be left in situ for protracted periods and could cause complications such as From the Unit of Interventional Radiology (C.L., L.G.G.), Ophthalmology Service (S.D.M., M.P.), and Anatomy-Pathology Service (R.R.M.), Hospital Vir- gen de la Salud, Toledo; Unit of Interventional Ra- diology (C.C.) and Ophthalmology Service (I.R.G.), Hospital General Yagüe, Burgos; and Unit of Inter- ventional Radiology (J.D., C.I.) and Ophthalmology Service (N.T.), Hospital General de Móstoles, Ma- drid, Spain. Received May 26, 2000; revision re- quested July 18; final revision received November 30; accepted December 4. Address correspondence to C.L., Radiología Vascular-Intervencionista, Hos- pital Virgen de la Salud, Avda. de Barber s/n, 45005 Toledo, Spain; E-mail: [email protected] © SCVIR, 2001 Clinical Studies 701

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Nasolacrimal Stents in the Management ofEpiphora: Medium-term Results of aMulticenter Prospective StudyCarlos Lanciego, MD, Silvia De Miguel, MD, Miguel Perea, MD, Cristobal Cano, MD, Isaac Ruíz García, MD,
Julio Dávila, MD, Cristina Ibarburen, MD, Nicolas Toledano, MD, Rufo Rodriguez-Merlo, MD,and Lorenzo García García, MD
PURPOSE: To evaluate in a prospective multicenter setting the clinical utility of polyurethane stents in the percuta-neous management of epiphora.
MATERIALS AND METHODS: Patients (N 5 163; age range 5 22–85 y, mean 5 52 y; 29 men, 134 women) with severeepiphora had stents (n 5 183) inserted under fluoroscopic guidance in 180 lacrimal systems (unilateral 5 146; bilateral5 17) to treat complete (n 5 172) or partial (n 5 8) obstruction of the nasolacrimal duct or sac. The junction betweensac and duct was the most frequent location (n 5 102), followed by the sac alone (n 5 48), and the duct alone (n 5 30).The etiology of the obstruction was idiopathic in 113 cases (63%) and chronic dacryocystitis in 67 (37%). The setdesigned by Song was used in all patients and the original technique was slightly modified by the authors. Allpatients were treated on an outpatient basis. Average time of the procedure was 14 minutes (range 5 3–70 min).
RESULTS: Initial technical success rate of stent placement was 97%. Resolution of epiphora was complete in 175 eyesand partial in five. On follow-up (mean 5 450 d; range 5 8–730 d), 157 of 183 stents remained patent (85.8%). Of the24 obstructed, 19 were easily withdrawn and 17 of these patients remained asymptomatic for a mean of 15 months(secondary patency rate 5 89.5%).
CONCLUSIONS: The procedure is simple and safe. It can be performed on an outpatient basis and the originaltechnique could be improved with some technical modifications. It is well tolerated by patients and may beconsidered as a valid alternative technique for the resolution of epiphora.
Index terms: Epiphora • Lacrimal gland and duct, stenosis or obstruction • Stents and prostheses
J Vasc Interv Radiol 2001; 12:701–710
Abbreviations: DCG 5 dacryocystography, DCP 5 dacryocystoplasty, DCR 5 dacryocystorhinostomy
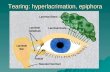
EPIPHORA (also known as tearing orwet eye) can be caused by reflex hy-persecretion of tears as a result of in-
fection, irritation of anatomic origin(eg, eyelid malformations, trichiasis),or obstruction of the lacrimal drainagesystem. Epiphora secondary to lacri-mal obstruction is a common (3% ofclinical consultations) ophthalmologicproblem (1,2). Although there aremany causes of lacrimal outflow ob-struction, most cases are caused by id-iopathic inflammation and scarring ofthe nasolacrimal system. It is an an-noying disability, and its continuancetends to provoke chronic irritative lac-rimal conjunctivitis and, sometimes,eczematous eyelids (3,4). Most cases ofacquired obstructions occur in adult-hood and are not related to trauma,neoplasm, or systemic disease. Involu-
tional stenosis is probably the mostcommon cause of nasolacrimal ob-struction in older individuals; womenare affected twice as often as men. Thehistopathologic cause of obstructionremains uncertain, but compression ofthe duct by inflammatory infiltratesand edema precede development ofchronic dacryocystitis accompaniedby pain and discomfort (1,5).
The appropriate therapy for lacri-mal obstruction depends on its causeand extent. A probe is usually intro-duced in cases of congenital stenosis.Intubation with a silicone tube causesdiscomfort because the tube needs tobe left in situ for protracted periodsand could cause complications such as
From the Unit of Interventional Radiology (C.L.,L.G.G.), Ophthalmology Service (S.D.M., M.P.), andAnatomy-Pathology Service (R.R.M.), Hospital Vir-gen de la Salud, Toledo; Unit of Interventional Ra-diology (C.C.) and Ophthalmology Service (I.R.G.),Hospital General Yagüe, Burgos; and Unit of Inter-ventional Radiology (J.D., C.I.) and OphthalmologyService (N.T.), Hospital General de Móstoles, Ma-drid, Spain. Received May 26, 2000; revision re-quested July 18; final revision received November30; accepted December 4. Address correspondenceto C.L., Radiología Vascular-Intervencionista, Hos-pital Virgen de la Salud, Avda. de Barber s/n, 45005Toledo, Spain; E-mail: [email protected]
© SCVIR, 2001
Clinical Studies
701
recurrent dacryocystitis, granulomaformation, and erosion of the canalic-ulus (6). For the past 70 years, externaldacryocystorhinostomy (DCR) has re-mained the standard treatment of choicefor correction of nasolacrimal obstruc-tion and has yielded success rates of89%–95% in primary repairs (7,8). De-spite its established success (albeit onlyin experienced hands), dacryocystorhi-nostomy continues to be approachedwith reluctance by many ophthalmo-logic surgeons and their patients. Inmany institutions, the procedure is per-formed under general anesthesia, withthe patient often in controlled hypoten-sion to provide better control ofbleeding. Complications of this surgicalprocedure include partial or completereobstruction of the fistulous tract, hy-pertrophy of the facial scar, and growthof the mucus membrane over the naso-lacrimal opening.
Recently, two interventional proce-dures have come into use: dacryocysto-plasty (DCP) with balloon dilation, andplacement of metal, plastic-nylon, orpolyurethane stents. The purposes ofthis report of our prospective study areto (i) evaluate the clinical utility of poly-urethane stents in the interventionalmanagement of epiphora; (ii) summa-rize our experience gained in a prospec-tive multicenter trial with a large seriesof patients and follow-up, to date, of 2years; (iii) report new technical detailsarising from our experience; and (iv)present the short- to medium-term com-plications observed, together with theirmanagement.
MATERIALS AND METHODS
Patient Population
Over a period of 2 years, 183 softpolyurethane stents were inserted in 180lacrimal systems of 163 patients (29 men
and 134 women; age range 5 22–85 y,mean 5 52 y) with severe epiphora(Grade III-IV on Munk’s score; Table).They were recruited consecutively fromamong the patients attending the oph-thalmologic outpatient clinics of thethree hospitals involved in the study.Dacryocystography (DCG) indicatedcomplete obstruction in 172 lacrimalsystems and partial obstruction in eight.The junction between sac and duct wasthe most frequent location (n 5 102),followed by the sac alone (n 5 48) andthe duct alone (n 5 30) (Figs 1,2). Partialocclusions or simple stenosis occurredfar less frequently than did complete oc-clusions (n 5 8). Obstruction was bilat-
eral in 17 cases and unilateral in 146. Theetiology of the obstruction was idio-pathic in 113 cases (63%) and chronicinfection (chronic dacryocystitis) in 67(37%). Patient selection was based onclinical history and followed ophthal-mologic assessment including canaliza-tion of both lacrimal ducts and irrigationwith physiologic saline. Inclusion crite-ria excluded patients with activedacryocystitis because the proposedprocedure, when conducted in an in-fected lacrimal sac, could result inspread of infection to surrounding tis-sues and produce periorbital or orbitalcellulitis. Also excluded were those pa-tients who had obstruction of the cana-
Figure 1. (a) Dacryocystography (frontal view) showing normal anatomy of the leftnasolacrimal system. (b) Superior (ccs) and inferior (cci) lacrimal canaliculi; commoncanaliculus (cmc); lacrimal sac (ls); nasolacrimal duct (d); inferior meatus in the nasal fossa(im); valve of Hasner (VH).
Figure 2. Obstructions suitable for nasolacrimal stent placement: (a) complete obstruc-tion at the junction between the lacrimal sac and the nasolacrimal duct (arrow); (b)complete obstruction at the outlet of the duct near the valve of Hasner (arrow).
Clinical Classification of EpiphoraBased on Munk’s Score
Grade Description
0 No epiphora: eye cleaning notnecessary
1 Occasional epiphora once or twice aday
2 Epiphora two to four times a day3 Epiphora five to ten times a day4 Epiphora more than ten times a day
702 • Nasolacrimal Stents in the Management of Epiphora June 2001 JVIR
liculi (superior and/or inferior) or of thecommon canaliculus on anteroposteriorand lateral projection DCG (Fig 4). Allpatients provided written consent afterbeing informed of the nature of theprocedure.
Technique of Stent Placement
The Song Nasolacrimal Duct StentSet (Cook, Queensland, Australia) was
used in all patients (Fig 3). The stent andthe original technique have been widelyused. However, we have introducedsome modifications to simplify the tech-nique, reduce the mean procedure time,and improve the effectiveness andsafety of the intervention. Preoperativesedation is not used. Local anesthesia isapplied to the nasal mucosa with cottonpledgets moistened in cocaine hydro-chloride (10%) and epinephrine and in-
troduced into the nasal fossa for 3–5minutes. Topical proparacaine hydro-chloride is applied to the eyes, and thenthe periorbital area is cleaned with io-dinated solution. Infratrochlear nerveblock is not routinely used; this is a mi-nor improvement of the originaltechnique.
We begin the procedure by prepar-ing the guide wire by cutting the 0.8-mm ball with wire cutters and pre-mounting the guide wire through thecannula that has been manually pre-formed into a slight curve (a useful ad-dition to the original procedure). The0.018-inch guide wire is then introducedthrough the superior punctum into thecanaliculus. The superior punctum is di-lated if and when necessary. With lat-eral tension on the eyelid to preventkinking of the canaliculus, the guidewire is advanced until it makes contactwith bone, which indicates that it hasreached the nasal wall of the lacrimalsac. It is then withdrawn slightly and itsdirection vertically changed by 90° so asto point the ball tip caudally at a poste-rior angle of 15°–20°. Working continu-ously with lateral fluoroscopic guid-ance, and with the aid of a preliminarydacryocystogram to localize the sac, theguide wire is advanced gently across theobstruction into the inferior meatus ofthe nasal cavity. The cannula needlefrom the set (with a slight curvature pre-formed manually) is used to support theguide wire during recanalization. Ahook is placed in the nasal cavity andaimed laterally toward the inferior me-atus to grasp the guide wire. The oper-ator can feel metallic contact and hear asoft sound at this point. The guide wireis grasped with the hook (we prefer touse the hook as a channel to support theguide wire) and, at this stage, the guidewire is advanced gently toward the ex-ternal nares so as not to induce traumato the nasal mucosa (an important devi-ation from the original Song technique).At this point, the 0.6-mm end ball of theguide wire is cut. The 6-F sheath (withdilator) from the set is advanced retro-gradely through the nose across the le-sion until the distal tip of the dilator is inthe sac. To place the tip of the sheathproperly in the lacrimal sac and confirmits location (one of the main steps of theprocedure), contrast medium and airare introduced through the sheath via aTuohy-Borst adapter and visualized flu-oroscopically (a critical stage in themodified procedure). The dilator is
Figure 3. (a) Anatomic drawing of the nasolacrimal system before and after the recana-lization procedure; (b) photograph of the stent with a drawing of its placement. (c) Allother parts of the recanalization apparatus.
Lanciego et al • 703Volume 12 Number 6
withdrawn from the sheath, and thestent is introduced over the guide wireinto the sheath and then advanced bymeans of a pusher catheter until the ra-diopaque tip of the stent is located at thesheath tip. The pusher is held in placewhile the sheath is withdrawn, therebyfreeing the stent, which then assumes amushroom shape. Visual confirmationof the stent’s expansion is important toconfirm that it is properly located in the
sac. The sheath and the pusher are with-drawn via the nasal fossa and the guidewire through the superior punctum.
Immediately after the procedure(equally applicable in the placement asin the withdrawal of a stent), a pro-phylactic regimen of ocular topic anti-biotic collyrium is administered (To-brex; tobramycin, 3 drops every 8 h for7 d). Neither oral antibiotics nor ste-roids are used.
Technique of Stent Removal
Occasionally, some stents need tobe removed because of recurrence ofepiphora, which would suggest an ob-structed stent. In these cases, and toconfirm the condition, DCG is per-formed before device removal, which,when conducted under fluoroscopicguidance, is easier than stent place-ment and can be done by any of threesimple techniques:
1. The “standard” removal technique,in which the distal tip of the stent inthe nasal fossa is grasped withcurved-tip tweezers and the stent isteased out.
2. The Song’s hook technique can beemployed, in which the tip of thehook is introduced into one of thetwo small round holes (1 mm indiameter) in the beveled portionof the stent and gently pulledthrough to the external nares. Aprocedure for the removal ofblocked stents with use of a mod-ified hook has been described bySong et al recently (9).
3. In difficult situations, a reason-able alternative is the recanaliza-tion of the obstructed stent withthe guide wire in a similar man-ner to the original procedure forstent placement.
Anesthetic Guidelines
Different anesthesia protocols wereused in the three hospitals involved in the
Figure 4. Obstructions not suitable for nasolacrimal stent placement: DCG showing obstructions in the union of the superior andinferior canaliculi (arrows) (a), and in the common canaliculus (arrows) (b). The anatomic line drawing of the axis of the nasolacrimalsystem is for the reader’s orientation.
Figure 5. Dacryocystogram after implantation of a stent in anteroposterior (a) and lateral(b) views. Note good passage of contrast medium to the nasal fossa.
704 • Nasolacrimal Stents in the Management of Epiphora June 2001 JVIR
study and reflected local preferences. Inone hospital (111 patients), the first 12 pa-tients underwent conventional anesthesiaas described by Song et al (10). Thereafter(99 patients), only local anesthesia was ap-plied to the nasal mucosa with a cottonpledget soaked in epinephrine (1%) plustopical anesthesia collyrium of 0.5% pro-paracaine hydrochloride applied to theeyes. There was no need for nerveblockage. In another of the hospitals (31patients), the standard procedure was lo-cal nasal anesthesia plus topical eye anes-thetic collyrium and infratrochlear nerveblock. In the third hospital involved in thestudy (21 patients), the same standardprocedures were used together with in-tracanalicular anesthesia with lidocaine(2%) through the introducer sheath afterremoval of the dilator, in addition to pre-operative sedation with 2 mg midazolam.Patient compliance and comfort was as-sessed by directly questioning the patientand scaling the response as: 0 5 no pain, 15 distress or slight pain that spontane-ously ceased, and 2 5 moderate pain re-quiring conventional oral analgesics.
Follow-up
A close follow-up is the key to thesuccess of this treatment. Stent pa-tency is maintained only if the devicereceives periodic care by means of sa-
line irrigation by the ophthalmologist.Our protocol included a clinicalcheck-up (including irrigation) in thefirst week, at months 1, 3, and 6, andevery 6 months thereafter. Follow-upcare by the ophthalmologist consists ofirrigation of both lacrimal points withphysiologic saline. Flushing is per-formed once or twice with 2 mL saline,which is used cold by some investiga-tors so the patient notes the sensationat the back of the throat.
Follow-up DCG was performedonly in the event of stent failure. Thesame clinical checks performed forstent placement were performed afterstent removal.
RESULTS
The technical success rate was 97%,with six cases of initial failure in whichwe were unable to continue with theprocedure. Of these, four were causedby incorrect passage of the guide wirewhich slipped off the guide (perforat-ing the canaliculus in one case) andfollowed a suborbital posterior trajec-tory (as viewed on the lateralprojection). This was accompanied bypalpebral edema and pain in two casesand the procedure was discontinued.In the other two cases, we decided notto continue when the manipulation
seemed protracted. A second success-ful attempt was made 1 week later. Ofthe four cases in which the procedurefailed initially, one resulted in a perfo-rated sac, two patients refused a sub-sequent attempt (one of whom pre-sented with an extreme nasal septumdeviation), and the other is awaitinganother attempt.
Initially, we obtained complete res-olution of epiphora in 175 eyes andpartial resolution (Grade 2 of Munk’sclassification) in five. There were nodifferences in compliance and patientscomfort reported between the threedifferent anesthetic regimens. Themean time of the procedure was 14minutes (range 5 3–70 min).
After a mean of 15 months of fol-low-up (range 5 8–730 d), 157 stentswere patent according to clinical andDCG checks. The primary patency ratewas 85.8% (Fig 5). This level is re-duced to 80% if the initial failures areentered into the life-table calculations(Fig 6).
Complications
In the course of follow-up, we ob-served various complications. Somewere immediate and related to theprocedure and others presented muchlater in the follow-up. Of the immedi-ate complications, eight patients hadmoderate pain which was relievedwith oral analgesics. One patient re-ported a “foreign body” sensation.The stent was withdrawn on the re-quest of the patient despite the pa-tency of the device. Epistaxis (n 5 29)was minimal and self-limited by thepatient and needed no treatment. Pal-pebral edema (n 5 7) and hematoma(n 5 2) were treated with topical ap-plication of ice packs over a period ofless than 1 week. There was one caseof acute or active dacryocystitis afterintervention and three cases of incor-rect positioning of the stent (below thesac) with recurrence of the epiphora.In these three cases, the stent waswithdrawn and the patients are cur-rently awaiting replacements.
In one of the latest stent withdraw-als, the material contained in the inte-rior of the stent was cultured (not astandard part of the study protocol) inthe microbiology department of ourhospital and was shown positive forProteus mirabilis and Streptococcusviridans.
Figure 6. Life-table analysis of patency.
Lanciego et al • 705Volume 12 Number 6
In the medium to long term, the prin-cipal problem or technical failure was ob-struction (blockage) of the stent (Fig 7)and resultant recurrence of epiphora. Wedid not have any cases of stent migration.Of the 24 blocked stents (13%), 19 wereeasily removed by the attending radiolo-gist, one could not be withdrawn with useof the conventional technique and wasscheduled for surgery, another was surgi-cally removed under general anesthesia,and the remaining four are awaiting with-drawal by the radiologist. Of the 19 lacri-mal systems from which stents were re-moved, 17 had remained patent onfollow-up without the necessity of a re-placement stent. In two cases, because ofepisodes of reobstruction, a second stentwas introduced, and the stents remainedpatent. Hence, over the follow-up periodof 15 months (range 5 15–540 d), 17 of 19eyes remained asymptomatic. The rate ofsecondary patency (ie, a period of goodstent function interpreted as the absenceof clinical symptoms of epiphora whetheror not a second stent had been inserted, orfollow-up DCG showing adequate pas-sage of contrast medium to the nasal fossaand, as such, the clinical result coincidingwith the anatomic) was 89.5%.
All stents that needed to be re-moved were examined by a patholo-gist at the hospital. The material foundaround the “mushroom” and in the
inner lumen of the stent was granula-tion tissue with inflammatory infil-trates (Figs 8–9).
DISCUSSION
Treatment of epiphora, the imper-fect drainage of tears through the lac-rimal system, constitutes an importantportion of the practice of the clinicalophthalmologist. Dacryocystitis usu-ally results secondarily from obstruc-tion of the lacrimal sac or nasolacrimalduct. It is a constant source of annoy-ance to the patient and is frequentlyaccompanied by pain and discomfortin addition to the persistent tearing(11).
Traditionally, epiphora caused byobstruction of the lacrimal duct hadbeen treated surgically by DCR, whichinvolves the removal of bone betweenthe lacrimal sac and nasal mucosa.Lately, the preferred technique hasbeen for the lacrimal sac and nasalmucosa to be opened up and suturedto each other so as to bypass the lacri-mal duct (12). Dacryocystorhinos-tomy, with or without silicone intuba-tion, remains the treatment of choicebut it requires general anesthesia andoften leaves a permanent facial scar,and the failure rate is still approxi-mately 6%–21% (13). In experienced
hands, DCR has a success rate of 90%,but possible complications include or-bital emphysema, hemorrhage, infec-tion, cerebrospinal fluid leakage, par-tial or complete obstruction of thefistulous tract, and growth of mucosaltissue over the nasolacrimal opening.
A new surgical approach to naso-lacrimal duct obstruction has beenproposal by Massaro et al (8), whoused a sophisticated argon laser tominimize the main bleeding complica-tions of conventional DCR. Termedendonasal laser (ENL) DCR, this newtechnique needs to be further vali-dated with more cases and increasedexperience of the users before its wide-spread use as a routine method in thetreatment of nasolacrimal obstructionmay be recommended. Recently, arandomized trial (14) comparing theefficacy of external DCR with ENLDCR indicated, at 1 year of follow-up,the superiority of external DCR. Thiswas confirmed not only by the practi-tioners but also by the patients in theirperiodic visits to the ophthalmologist.
In recent years, there has been a ten-dency to use less invasive techniques suchas balloon DCP, and the placement of anexpandable stent (metallic or plastic) hasbeen advocated for the treatment ofepiphora. Both procedures are easy andsafe when performed under fluoroscopicguidance.
Since 1990, several studies (5–7,13)have demonstrated the feasibility offluoroscopically guided balloon DCP,which is the passage of a guide wirethrough the lacrimal ducts followedby balloon dilation at the site of theobstruction. Technical and clinical suc-cess rates between 59% and 90% havebeen reported. However, most pa-tients experienced pain while the bal-loon was being inflated, and the rate ofrecurrence was as high as 45% at 2months (4). Lee et al (5), leaders in thedevelopment of tear duct intervention,were the first to publish rather disap-pointing results: technical failure ratesof DCP between 29% and 41% andeven higher recurrence rates of 45%and 80% at 2-year follow-up. Conse-quently, the investigators from thatgroup proposed primary stent place-ment for tear duct obstructions as analternative to balloon dilation.
Berkefeld et al (15), Ilgit et al (16),and Janssen et al (12) tried to improvethe recanalization procedure’s successrate and reduce trauma to the ductal
Figure 7. Obstructed stents. Near complete blockage of the lacrimal sac, as indicated bythe failure of contrast medium to pass through the prosthesis (arrows). Partial filling (a),sac nearly intact (b), totally occluded sac (c).
706 • Nasolacrimal Stents in the Management of Epiphora June 2001 JVIR
Figure 8. Removal of obstructed stents with use of standard technique with curvedtweezers and Song’s hook.
Lanciego et al • 707Volume 12 Number 6
structures by using flexible, steerableguide wires instead of the rigid instru-ments previously used. Clinical long-term success rates of more than 80%have been reported but have beenachieved by narrowly selecting patienttypes (focal lesions, partial junctionalobstructions, and short-distance distallesions) and restricting the indicationsfor the technique.
The very limited success and highrecurrence rates with DCP have per-suaded the majority of investigatorstoward the next logical step: the use ofdifferent stent types.
Initially, Song et al (4) attempted todemonstrate the value of an expand-able metallic stent in the lacrimal sys-tem, but the metallic stent had somelimitations. First, when in place, itcould be removed only by surgery.Second, it lacked longitudinal flexibil-ity, and, third, it was easily obstructedby granulation tissue. To overcomethese disadvantages, plastic-nylonstents gained favor. However, previ-ous balloon dilation is required withthese stents and, in many cases, thestent needs to be cut or shortened be-cause its rigidity causes discomfort
when resting on the base of the nasalfossa.
These limitations induced Song etal (10) to design the new, soft, poly-urethane stent that we have used inthis study. A high rate of patency hasbeen claimed. Pulido et al (17) re-ported, in a group of 35 patients with40 stents in 40 lacrimonasal systems, aprimary patency rate of 93%, which issimilar to that reported by Song et al(11) but with a mean follow-up time of123 days (range 5 15–240 d). In ourstudy, the primary patency rate was85.8% (80% if initial technical failuresare included) in 163 patients in whom183 stents were placed in 180 lacrimalsystems and with a mean follow-uptime of 450 days (range 5 8–730 d)and which, to our knowledge, is themost extensive in the literature to date.
With respect to failures, obstructionor blockage of the stent appeared to bethe main problem. Over the follow-upperiod, 24 stents (13%) became ob-structed and epiphora recurred. Ofthese, 19 were removed without theneed of repeat stent placement tomaintain the patency of the nasolacri-mal system (Fig 10). At the latest clin-
ical assessment, complete resolution ofthe epiphora was noted in 17 of thesecases and reobstruction was noted intwo (after 1 and 3 months, respective-ly); both necessitated repeat stentplacement, yielding a secondary pa-tency of approximately 90%.
With these encouraging results, webelieve that there is no urgency to re-move the stent provided that the stentdoes not cause major complicationsand continues to function. However, ifthe stent needs to be removed becauseof blockage or malfunction, the proce-dure is very easy because the distal tipprotruding into the inferior meatuscan be grasped with simple tweezers(curved tip) so the stent can be pulledout. Upon removal of the stent, weprefer not to replace it immediatelybut to maintain the patency of the re-opened nasolacrimal system by meansof saline irrigation and regular clinicalchecks; we would consider replacingthe stent only in case of reobstruction.After removing the failed stents (ex-cept the five that are currently await-ing removal), all but two patients re-main asymptomatic. After a meanfollow-up time of 10 months (range 5
Figure 9. Removal of obstructed stents with use of Song’s hook. Specimen withdrawn with hook (a). Micro- (b) and macro-photographs(c,d,e) showing granulation tissue in the inner lumen of the stent and around the edges of the “mushroom” of the stent (d).
708 • Nasolacrimal Stents in the Management of Epiphora June 2001 JVIR
1–18 mo), nasolacrimal systems arepatent as assessed by clinical and DCGcheck-ups. Seventeen have not re-quired replacement of stents and onlytwo cases have required introductionof another stent, yielding a secondarypatency rate of 89.5%.
In 14 of 24 (58%) of the obstructedstents, the etiology of the epiphora waschronic dacryocystitis and there may be acausal relationship between this observa-tion and incidence of malfunction of thestent. Further clinical trials with extendedfollow-up would be necessary to evaluatethis relationship. The concept of chronicinfection as a promoting factor in obstruc-tion and, consequently, poor long-termpatency results has been suggested byother investigators. Based on culturestaken from the lacrimal sac of patientswith chronic dacryocystitis and those af-fected by simple epiphora (18), poorer re-sults of balloon DCP are to be expected inpatients with signs of chronic infectionthan in those with idiopathic obstructions.As such, DCP treatment may be recom-mended perhaps only if patients were se-lected to exclude candidates with an infec-tious etiology and, better still, to include
only candidates with partial obstructions(19).
In our study, there were no other ma-jor complications such as migration of thestent, excessive pain, stent breakage, etc.,as has been reported by others (11,17).Eight patients described pain; one of thoseeight felt a “foreign body” sensation. Afterstent removal, clinical manifestations dis-appeared and, to date, the nasolacrimalsystems remain open. Epistaxis waspresent in 16% of cases, but it was mini-mal, controlled by the patient, and did notrequire treatment. Eyelid edema (in sevencases: 4%) and eyelid hematoma (in twocases) were encountered in our series, buthave not been reported by other users ofthe technique. The causes remain uncer-tain but may have resulted from excessivemanipulation of the lacrimal canaliculi orperforation and/or extravasation of con-trast medium. However, the edema andhematoma spontaneously resolved in1–10 days.
Patient comfort and acceptance of theprocedure was, in general, very good.This is of particular importance whenworking without standard anesthesiaguidelines for this procedure. We believethat topical anesthesia of the eyes and lo-cal anesthesia and decongestion of the na-sal mucosa with cotton pledgets moist-ened with epinephrine (1%) is sufficientand obviates the use of more invasive an-esthetic procedures such as infratrochlearnerve block. All procedures were per-formed on an outpatient basis. The meantime of the procedure was reduced to ap-proximately 14 minutes and continues todecrease with increasing experience. Thereduction of anesthesia requirements andsome of the technical variations that wehave introduced reduces the mean time ofthe procedure without a loss in safety andeffectiveness of the procedure and com-fort of the patient. However, a close clini-cal surveillance by the ophthalmologist iscrucial for the success of the treatment.Periodic check-ups and saline irrigationare essential if obstruction is to beavoided.
Only in cases of obstruction and recur-rence of the epiphora did we performDCG. Other investigators advocate theuse of computed tomography (CT) for thecontrol of stent placement and its subse-quent monitoring (20). We believe thismay be useful in isolated difficult casesrequiring protracted manipulation for theplacement of the stent but is not necessaryfor routine use. A good knowledge of theanatomy of the lacrimal system, together
with the technical improvements we havedescribed, reduces the possibilities of er-rors in the procedures. However, CT for arepeat attempt at stent placement doeshave its use in ascertaining anatomic ab-normalities or variants that would indi-cate whether to modify or terminate theprocedure. In such cases, it would be use-ful to employ helical CT with topical wa-ter-soluble contrast media, as proposed byMoran et al (21), for clear visualization ofthe lacrimal system.
In conclusion, our medium-term re-sults with polyurethane soft nasolacri-mal stents are encouraging. We be-lieve that the treatment of epiphorawith polyurethane stents minimizesthe problems associated with metallicand other plastic stents and, being lessaggressive, contributes to greater pa-tient comfort. Its simplicity, safety, re-producibility, and effectiveness, andthe fact that it can be performed on anoutpatient basis, could make it an at-tractive alternative to other methodsof epiphora management.
Acknowledgments: The authors thankDr. Peter R. Turner of t-SciMed (Reus,Spain) for editorial assistance.
References1. Linberg JV, McCormick SA. Primary
acquired nasolacrimal duct obstruc-tion: a clinicopathologic report and bi-opsy technique. Ophthalmology 1986;93:1055–1063.
2. Traquair HM. Chronic dacryocystitis:its causation and treatment. Arch Oph-thalmol 1941; 26:165–180.
3. Duke-Elder S. System of ophthalmol-ogy: In: Duke-Elder S, ed. The ocularadnexa, Vol 13. London: Henry Kimp-ton 1974; 675–693.
4. Song HY, Ahn HS, Park CK, Kwon SH,Kim CS, Choi KC. Complete obstruc-tion of the nasolacrimal system. Part II:treatment with expandable metallicstents. Radiology 1993; 186:372–376.
5. Lee JM, Song HY, Han YM, et al. Bal-loon dacryocystoplasty: results in thetreatment of complete and partial ob-structions of the nasolacrimal system.Radiology 1994; 192:503–508.
6. Munk PL, Lin DTC, Morris DC. Epi-phora: treatment by means of dacryo-cystoplasty with balloon dilation of thenasolacrimal drainage apparatus. Ra-diology 1990; 177:687–690.
7. Becker BB, Berry FD. Balloon catheterdilatation in lacrimal surgery. Ophthal-mic Surg 1989; 20:193–198.
8. Massaro BM, Gonnering RS, Harris GJ.Endonasal laser dacryocystorhinosto-my: a new approach to nasolacrimal
Figure 10. Dacryocystogram (lateral view)immediately after stent withdrawal. The fill-ing defects that can be observed (arrows) areblood clots that are easily removed on wash-ing with saline. Lacrimal sac (ls); nasolacri-mal duct (d); nasal fossa (nf).
Lanciego et al • 709Volume 12 Number 6
duct obstruction. Arch Opthalmol1990; 108:1172–1176.
9. Kim HS, Song HY, Kim TH, et al. Useof a lacrimal stent retrieval hook in theremoval of occluded plastic and ex-pandable metallic lacrimal stents. JVasc Interv Radiol 2000; 11:762–766.
10. Song HY, Jin YH, Kim JH, et al. Non-surgical placement of a nasolacrimalpolyurethane stent. Radiology 1995;194:233–237.
11. Song HY, Jin YH, Kim JH, Sung KB,Han YM, Cho NC. Nasolacrimal ductobstruction treated nonsurgically withuse of plastic stents. Radiology 1994;190:535–539.
12. Janssen AG, Mansour K, Bos JJ. Ob-structed nasolacrimal duct system inepiphora: Long-term results of dacryo-cystoplasty by means of balloondilation. Radiology 1997; 205:791–796.
13. Song HY, Ahn HS, Park CK, Kwon SH,Kim CS, Choi KC. Complete obstruc-
tion of the nasolacrimal system: Part I:treatment with balloon dilation. Radi-ology 1993; 186:367–371.
14. Hartikainen J, Grenman R, Puukha P,Seppä H. Prospective randomizedcomparison of external dacryocystorhi-nostomy and endonasal laser dacryo-cystorhinostomy. Ophthalmology 1998;105:1106–1113.
15. Berkefeld J, Kirchner J, Müller HM, FriesU, Kollath J. Balloon dacryocystoplasty:indications and contraindications. Radiol-ogy 1997; 205:785–790.
16. Ilgit ET, Yüksel D, Ünal M, Akpek S,Isik S, Hsanreisoglu B. Transluminalballoon dilation of the lacrimal drain-age system for the treatment ofepiphora. AJR Am J Roentgenol 1995;165:1517–1524.
17. Pulido-Duque JM, Reyes R, CarreiraJM, et al. Treatment of complete andpartial obstruction of the nasolacrimalsystem with polyurethane stents: ini-
tial experience. Cardiovasc InterventRadiol 1998; 21:41–45.
18. Hartikainen J, Lethonen OP, SaariKM. Bacteriology of lacrimal ob-struction in adults. Br J Ophthalmol1997; 81:37– 40.
19. Perry JD, Maus M, Nowinski TS, PenneRB. Balloon catheter dilation fortreatment of adults with partial naso-lacrimal duct obstruction: A prelimi-nary report. Am J Ophthalmol 1998;126:811–816.
20. Pinto IT, Paul L, Grande C. Nasolac-rimal polyurethane stent: complica-tions with CT correlation. CardiovascIntervent Radiol 1998; 21:450–453.
21. Moran CC, Buckwalter K, CaldemeyerKS, Smith RR. Helical CT with topicalwater-soluble contrast media for imag-ing of the lacrimal drainage apparatus.AJR Am J Roentgenol 1995; 164:995–996.
710 • Nasolacrimal Stents in the Management of Epiphora June 2001 JVIR
Related Documents