INTRODUCTION A total of 100 million patients develop scars in the developed world alone each year as a result of 55 million elective op- erations and 25 million operations after trauma (1). Excessive scars form as a re- sult of aberrations of physiologic wound healing and may develop following any insult to the deep dermis, including burn injury, lacerations, abrasions, surgery, piercings and vaccinations. By causing pruritus, pain and contractures, excessive scarring can dramatically affect a pa- tient’s quality of life, both physically and psychologically. Excessive scarring was first described in the Smith papyrus about 1700 BC (2). Many years later Mancini (in 1962) and Peacock (in 1970) differentiated excessive scarring into hypertrophic and keloid scar formation. Per their definition, both scar types rise above skin level, but while hypertrophic scars do not extend beyond the initial site of injury, keloids typically project beyond the original wound mar- gins (3,4). Nevertheless, clinical differenti- ation between hypertrophic scars and keloids can be problematic. Incorrect identification of scar type may result in inappropriate management of pathologic scar formation, and occasionally con- tribute to inappropriate decision making related to elective or cosmetic surgery (5). Although there are clinical similari- ties between hypertrophic scars and keloids, there are some clinical, histo- logical and epidemiological differences (Table 1 and Figure 1) that indicate that these entities may be distinct from one another (5,6). HYPERTROPHIC SCARS VERSUS KELOIDS Clinical Characteristics Hypertrophic scarring usually occurs within 4 to 8 weeks following wound in- fection, wound closure with excess ten- sion or other traumatic skin injury (7), has a rapid growth phase for up to 6 months, and then gradually regresses over a pe- riod of a few years, eventually leading to flat scars with no further symptoms (8,9). Keloids, in contrast, may develop up to several years after minor injuries and may even form spontaneously on the midchest in the absence of any known injury. Keloids also persist, usually for long peri- ods of time, and do not regress sponta- neously (10). Keloids appear as firm, mildly tender, bosselated tumors with a shiny surface and sometimes telangiecta- sia. The epithelium is thinned and there may be focal areas of ulceration. The color is pink to purple and may be accompa- nied by hyperpigmentation (11). The bor- ders of the tumor are well demarcated but irregular in outline. A hypertrophic scar has a similar appearance, but is usually linear, if following a surgical scar, or papular or nodular, following inflamma- tory and ulcerating lesions (12). Both le- sions are commonly pruritic, but keloids may even be the source of significant pain and hyperesthesia (7,9). In the majority of cases, hypertrophic scarring develops in wounds at anatomic MOL MED 17(1-2)113-125, JANUARY-FEBRUARY 2011 | GAUGLITZ ET AL. | 113 Hypertrophic Scarring and Keloids: Pathomechanisms and Current and Emerging Treatment Strategies Gerd G Gauglitz, 1,2 Hans C Korting, 1 Tatiana Pavicic, 1 Thomas Ruzicka, 1 and Marc G Jeschke 2,3,4,5 1 Department of Dermatology and Allergology, Ludwig Maximilians University, Munich, Germany; 2 Shriners Hospitals for Children, Department of Surgery, University Texas Medical Branch, Galveston, Texas, United States of America; 3 Ross Tilley Burn Centre and 4 Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada; and 5 Department of Surgery, Division of Plastic Surgery, University of Toronto, Toronto, Ontario, Canada Excessive scars form as a result of aberrations of physiologic wound healing and may arise following any insult to the deep der- mis. By causing pain, pruritus and contractures, excessive scarring significantly affects the patient’s quality of life, both physically and psychologically. Multiple studies on hypertrophic scar and keloid formation have been conducted for decades and have led to a plethora of therapeutic strategies to prevent or attenuate excessive scar formation. However, most therapeutic approaches remain clinically unsatisfactory, most likely owing to poor understanding of the complex mechanisms underlying the processes of scarring and wound contraction. In this review we summarize the current understanding of the pathophysiology underlying keloid and hypertrophic scar formation and discuss established treatments and novel therapeutic strategies. © 2011 The Feinstein Institute for Medical Research, www.feinsteininstitute.org Online address: http://www.molmed.org doi: 10.2119/molmed.2009.00153 Address correspondence and reprint requests to Marc Jeschke, Sunnybrook Research Institute, Rm D704, 2075 Bayview Avenue, Toronto, Ontario, Canada M4N 3M5. Phone: 416-480-6703; Fax: 416-480-6763; E-mail: [email protected]. Submitted October 22, 2009; Accepted for publication October 4, 2010; Epub (www.molmed.org) ahead of print October 5, 2010.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

INTRODUCTIONA total of 100 million patients develop
scars in the developed world alone eachyear as a result of 55 million elective op-erations and 25 million operations aftertrauma (1). Excessive scars form as a re-sult of aberrations of physiologic woundhealing and may develop following anyinsult to the deep dermis, including burninjury, lacerations, abrasions, surgery,piercings and vaccinations. By causingpruritus, pain and contractures, excessivescarring can dramatically affect a pa-tient’s quality of life, both physically andpsychologically.
Excessive scarring was first describedin the Smith papyrus about 1700 BC (2).Many years later Mancini (in 1962) andPeacock (in 1970) differentiated excessivescarring into hypertrophic and keloidscar formation. Per their definition, bothscar types rise above skin level, but whilehypertrophic scars do not extend beyond
the initial site of injury, keloids typicallyproject beyond the original wound mar-gins (3,4). Nevertheless, clinical differenti-ation between hypertrophic scars andkeloids can be problematic. Incorrectidentification of scar type may result ininappropriate management of pathologicscar formation, and occasionally con-tribute to inappropriate decision makingrelated to elective or cosmetic surgery (5).
Although there are clinical similari-ties between hypertrophic scars andkeloids, there are some clinical, histo-logical and epidemiological differences(Table 1 and Figure 1) that indicate thatthese entities may be distinct from oneanother (5,6).
HYPERTROPHIC SCARS VERSUS KELOIDS
Clinical CharacteristicsHypertrophic scarring usually occurs
within 4 to 8 weeks following wound in-
fection, wound closure with excess ten-sion or other traumatic skin injury (7), hasa rapid growth phase for up to 6 months,and then gradually regresses over a pe-riod of a few years, eventually leading toflat scars with no further symptoms (8,9).Keloids, in contrast, may develop up toseveral years after minor injuries and mayeven form spontaneously on the midchestin the absence of any known injury.Keloids also persist, usually for long peri-ods of time, and do not regress sponta-neously (10). Keloids appear as firm,mildly tender, bosselated tumors with ashiny surface and sometimes telangiecta-sia. The epithelium is thinned and theremay be focal areas of ulceration. The coloris pink to purple and may be accompa-nied by hyperpigmentation (11). The bor-ders of the tumor are well demarcated butirregular in outline. A hypertrophic scarhas a similar appearance, but is usuallylinear, if following a surgical scar, orpapular or nodular, following inflamma-tory and ulcerating lesions (12). Both le-sions are commonly pruritic, but keloidsmay even be the source of significant painand hyperesthesia (7,9).
In the majority of cases, hypertrophicscarring develops in wounds at anatomic
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 1 3
Hypertrophic Scarring and Keloids: Pathomechanisms andCurrent and Emerging Treatment Strategies
Gerd G Gauglitz,1,2 Hans C Korting,1 Tatiana Pavicic,1 Thomas Ruzicka,1 and Marc G Jeschke2,3,4,5
1Department of Dermatology and Allergology, Ludwig Maximilians University, Munich, Germany; 2Shriners Hospitals for Children,Department of Surgery, University Texas Medical Branch, Galveston, Texas, United States of America; 3Ross Tilley Burn Centre and4Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada; and 5Department of Surgery, Divisionof Plastic Surgery, University of Toronto, Toronto, Ontario, Canada
Excessive scars form as a result of aberrations of physiologic wound healing and may arise following any insult to the deep der-mis. By causing pain, pruritus and contractures, excessive scarring significantly affects the patient’s quality of life, both physicallyand psychologically. Multiple studies on hypertrophic scar and keloid formation have been conducted for decades and have ledto a plethora of therapeutic strategies to prevent or attenuate excessive scar formation. However, most therapeutic approachesremain clinically unsatisfactory, most likely owing to poor understanding of the complex mechanisms underlying the processes ofscarring and wound contraction. In this review we summarize the current understanding of the pathophysiology underlying keloidand hypertrophic scar formation and discuss established treatments and novel therapeutic strategies.© 2011 The Feinstein Institute for Medical Research, www.feinsteininstitute.orgOnline address: http://www.molmed.orgdoi: 10.2119/molmed.2009.00153
Address correspondence and reprint requests to Marc Jeschke, Sunnybrook Research
Institute, Rm D704, 2075 Bayview Avenue, Toronto, Ontario, Canada M4N 3M5. Phone:
416-480-6703; Fax: 416-480-6763; E-mail: [email protected].
Submitted October 22, 2009; Accepted for publication October 4, 2010; Epub
(www.molmed.org) ahead of print October 5, 2010.

locations with high tension, such asshoulders, neck, presternum, knees andankles (9,12,13), whereas anterior chest,shoulders, earlobes, upper arms and
cheeks have a higher predilection forkeloid formation. Eyelids, cornea, palms,mucous membranes, genitalia and solesare generally less affected (14). Keloidstend to recur following excision, whereasnew hypertrophic scar formation is rareafter excision of the original hyper-trophic scar (13,15).
HistologyHistologically, both hypertrophic scars
and keloids contain an overabundance ofdermal collagen. Hypertrophic scars con-tain primarily type III collagen orientedparallel to the epidermal surface withabundant nodules containing myofibrob-lasts, large extracellular collagen filamentsand plentiful acidic mucopolysaccharides(6). Keloid tissue, in contrast, is mostlycomposed of disorganized type I and IIIcollagen, containing pale-staining hypocel-lular collagen bundles with no nodules orexcess myofibroblasts (Table 1) (6,16). Bothscar types demonstrate overproduction ofmultiple fibroblast proteins, including fi-bronectin, suggesting either pathologicalpersistence of wound healing signals or afailure of the appropriate downregulationof wound-healing cells (16).
EpidemiologyThe occurrence of keloids and hyper-
trophic scars has equal sex distributionand the highest incidence in the second tothird decade (17,18). Incidence rates of hy-pertrophic scarring vary from 40% to 70%following surgery to up to 91% followingburn injury, depending on the depth ofthe wound (19,20). Keloid formation isseen in individuals of all races, except al-binos, but dark-skinned individuals havebeen found to be more susceptible tokeloid formation, with an incidence of 6%to 16% in African populations (14,21). Theconcept of a genetic predisposition tokeloids has long been suggested, becausepatients with keloids often report a posi-tive family history, unlike patients suffer-ing from hypertrophic scarring. Bayat andcolleagues (22) compared the profiles ofpatients of Afro-Caribbean origin withkeloid scars at single versus multipleanatomical site and found the latter to bemore common in younger age groups andin females. An important finding was thatmore than 50% of all keloid patients had apositive family history of keloid scarring,and family history was strongly associ-ated with the formation of keloid scars in
1 1 4 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S
Table 1. Hypertrophic scars and keloids: epidemiological, clinical and histological differences.
Hypertrophic scarring Keloids
Incidence 40% to 70% following surgery, up to 91% following 6% to 16% In African populationsburn injury
Equal in sex distribution with highest incidence in the second to third decade
Predilection sites Shoulders, neck, presternum, knees and ankles Anterior chest, shoulders, earlobes, upper arms and cheeks
Less affected: eyelids, cornea, palms, mucous membranes, genitalia and soles
Time course Within 4 to 8 weeks following wounding, rapid Within years after minor injuries or spontaneous growth phase for up to 6 months, then regression formation on the midchest in the absence of any over a period of a few years known injury. Persistence for long periods of time.
No spontaneous regression
Low recurrence rates after excision of the original High recurrence rates following excisionhypertrophic scar
Appearance Do not extend beyond the initial site of injury Projects beyond the original wound margins
Histological characteristics Primarily fine, well-organized, wavy type III collagen Disorganized, large, thick, type I and III hypocellular bundles oriented parallel to epidermis surface with collagen bundles with no nodules or excess abundant nodules containing myofibroblasts and myofibroblasts. Poor vascularization with widely plentiful acidic mucopolysaccharide. Proliferating scattered dilated blood vessels. PCNA/p53-level/ATPcell nuclear antigen (PCNA)/p53-level/ATP expression highexpression low
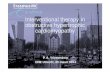
Figure 1. Clinical appearance of hyper-trophic scars and keloids. Development ofhypertrophic scars after a scald burn (A);hypertrophic scar on lower leg 4 monthsafter surgical procedure (B); keloid onchest after two minor operations (C); keloidon right ear, no history of trauma (D).

multiple sites as opposed to a singleanatomical site. Marneros and colleagues(23) studied two families with an autoso-mal-dominant inheritance pattern ofkeloids and identified linkage to chromo-some 7p11 and chromosome 2q23 for theAfrican and Japanese family, respectively.Brown and colleagues (24) found a ge-netic association between HLA-DRB1*15status and the risk of developing keloidscarring in white individuals. Also, carri-ers of HLA-DQA1*0104, DQB1*0501 andDQB1*0503 have been reported to be havean increased risk of developing keloidscarring (24). Keloid growth may also bestimulated by various hormones, as indi-cated by some studies in which resultshave suggested a higher incidence ofkeloid formation during puberty andpregnancy, with a decrease in size aftermenopause (18,25,26). Also, immunologicassociations of keloids have been pro-posed. A study by Placik and Lewis (27)revealed a direct correlation between theincidence of keloid formation and levelsof serum immunoglobulin E, and Smith etal. (28) found a higher incidence of aller-gic symptoms in keloid-afflicted patientscompared with individuals with hyper-trophic scars, suggesting a possible role ofmast cells in the pathophysiology ofkeloid formation. Other investigatorshave reported an association between theformation of keloids and blood type A(14,29).
PATHOPHYSIOLOGY OF EXCESSIVESCAR FORMATION
The physiologic response to wound-ing in adult tissue is the formation of ascar, a process that can be temporallygrouped into three distinct phases (Fig-ure 2): inflammation, proliferation andremodeling (14).
Immediately following wounding,platelet degranulation and activation ofthe complement and clotting cascadesform a fibrin clot for hemostasis, whichacts as a scaffold for wound repair (30).Platelet degranulation is responsible forthe release and activation of an array ofpotent cytokines, such as epidermalgrowth factor (EGF), insulinlike growth
factor (IGF-I), platelet-derived growthfactor (PDGF) and transforming growthfactor β (TGF-β), which serve as chemo-tactic agents for the recruitment of neu-trophils, macrophages, epithelial cells,mast cells, endothelial cells and fibrob-lasts (14,30). Within 48 to 72 hours afterthe initial event, the healing process tran-sitions into the proliferation phase, whichmay last for up to 3 to 6 weeks (6). Re-cruited fibroblasts synthesize a scaffold ofreparative tissue, the so-called extracellu-lar matrix (ECM). This granulation tissueis made of procollagen, elastin, proteogly-cans and hyaluronic acid and forms astructural repair framework to bridge thewound and allow vascular ingrowth (6).Modified fibroblasts, so-called myofi-broblasts, which contain actin filaments,help to initiate wound contraction. Once
the wound is closed, the immature scarcan transition into the final maturationphase, which may last several months.The abundant ECM is then degraded andthe immature type III collagen of theearly wound can be modified into maturetype I collagen (6).
The transformation of a wound clotinto granulation tissue thus requires adelicate balance between ECM proteindeposition and degradation, and whenthis process is disrupted, abnormalitiesin scarring appear, resulting in eitherkeloid or hypertrophic scar formation.
Both lesions represent aberrations inthe fundamental processes of woundhealing, in which there is an obvious im-balance between the anabolic and cata-bolic phases; however, keloids seem tobe a more sustained and aggressive fi-
R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 1 5
Figure 2. Differences between normal wound healing and excessive scar formation overtime. Processes of wound repair follow a specific time sequence and can be temporallygrouped into three distinct phases: inflammation (I), proliferation (II) and remodeling (III).Platelet degranulation is responsible for the release and activation of an array of potentcytokines, which serve as chemotactic agents for the recruitment of, for example,macrophages, neutrophils, epithelial cells and fibroblasts. In normal wounds, a balance isachieved between new tissue biosynthesis and degradation mediated by apoptosis andremodeling of ECM (A). During excessive scar formation, a dysfunction of the underlyingregulatory mechanisms may lead to persistent inflammation, excessive collagen synthesisor deficient matrix degradation and remodeling (B).

brotic disorder than hypertrophic scars(31). Evidence to date strongly suggests amore prolonged inflammatory period,with immune cell infiltrate present in thescar tissue of keloids, the consequence ofwhich may contribute to increased fi-broblast activity with greater and moresustained ECM deposition (31). The elu-cidation of this process may help to ex-plain why keloid scars spread beyondthe margins of the original wound, whilehypertrophic scars, in which the immunecell infiltrate decreases over time, remainwithin the original wound margins andoften regress over time. However, only afew published studies on the pathophys-iology of keloid and hypertrophic scarformation have included direct compari-son of the two entities.
InflammationRecent evidence suggests that it is not
simply the severity of inflammation thatpredisposes individuals to hypertrophicand keloid scarring, but also the type ofimmune response (31). T-helper (Th)CD41 cells have been implicated asmajor immunoregulators in wound heal-ing. The characteristic cytokine expres-sion profile of the CD41 T cells repre-sents the basis for describing either apredominantly Th1 or Th2 response to aspecific or unspecific stimulus (32).While the development of a Th2 re-sponse (with production of interleukin[IL]-4, IL-5, IL-10 and IL-13) has beenstrongly linked to fibrogenesis, a pre-dominance of Th1 CD41 cells has beenshown to almost completely attenuatethe formation of tissue fibrosis via pro-duction of interferon-γ (IFN-γ) and IL-12(33,34).
Secretion and activation of these medi-ators during the inflammatory phase ofhealing are prerequisites for subsequentprocesses, such as angiogenesis, reepithe-lialization, recruitment and proliferationof fibroblasts and matrix deposition (30).Angiogenesis is stimulated by endothe-lial chemoattractants and mitogens suchas heparin, fibroblast growth factor(FGF)-β, IL-8 and IGF-I. Wound reepithe-lialization occurs following the migration
of epithelial cells from the wound mar-gin and epidermal appendages withinthe wound bed and has been shown tobe enhanced by EGF, TGF-α and IGF-I(30). Fibroblast recruitment and prolifera-tion, and production of ECM, as well asinhibition of production of proteases re-quired to maintain the balance betweenproduction and degradation, are influ-enced predominantly by the fibrogenicgrowth factors PDGF, IGF-I and FGF-β,as well as TGF-β (14).
Fibrogenic ResponseInflammation is not the only critical
step in the development of the fibroticresponse. One reason for this hypothesisis the failure of current antiinflammatorytherapies, even in combination with po-tent immunosuppressives, to improveoutcomes in fibroproliferative diseasessuch as pulmonary fibrosis (35). Currentresearch thus focuses on direct inhibitionof specific fibrogenic events such as cy-tokine elaboration, fibroblast prolifera-tion and ECM deposition (36). Central tothe formation of hypertrophic scar andkeloid scar tissue is an alteration of thefibroblast phenotype (36,37). Indeed,when compared with normal fibroblasts,keloid fibroblasts show increased num-bers of growth-factor receptors and re-spond more briskly to growth factorslike PDGF and TGF-β, which may up-regulate these abnormal cells from thebeginning of wound healing (38,39).Using Affymetrix-chip analysis to iden-tify pathways critical to keloid patho-genesis, Smith and colleagues found increased expression of several IGF-binding and IGF-binding–related pro-teins and decreased expression of a sub-set of Wnt-pathway inhibitors andmultiple IL-1–inducible genes, providingpreliminary evidence for epigenetic si-lencing of a subset of genes in the al-tered program of keloid fibroblasts (40).
TGF-β. Many of the biologic actions ofTGF-β contribute to the normal wound-healing process and have been impli-cated in a wide variety of fibrotic disor-ders. Early after injury, high levels ofTGF-β are being released from degranu-
lating platelets at the site of injury, wherethey act as chemoattractants for lympho-cytes, fibroblasts, monocytes and neu-trophils (41).
The TGF-β family consists of at leastfive highly conserved polypeptides, withTGF-β1, -β2 and -β3 being the principalmammalian forms. TGF-β1 and -β2 areamong the most important stimulators ofcollagen and proteoglycan synthesis, andthey affect the ECM not only by stimulat-ing collagen synthesis but also by pre-venting its breakdown (42,43). In con-trast, TGF-β3, which is predominantlyinduced in the later stages of woundhealing, has been found to reduce con-nective tissue deposition (44). TGF-β hasbeen linked to hypertrophic scar andkeloid formation in a number of ways.Strong and persistent expression of TGF-βand its receptors has been shown in fibroblasts of post-burn hypertrophicscars (45). Also, overexpression of TGF-β1and -β2 has been found in keloid andkeloid-derived fibroblasts, with signifi-cantly lower TGF-β3 mRNA expression(46,47). Comparing the expression pro-files of TGF-β1, -β2 and -β3 and their re-ceptors in keloids, hypertrophic scar andnormal skin derived fibroblasts, Bockand colleagues found significantly lowerTGF-β2 mRNA expression in hyper-trophic scar fibroblasts compared with fibroblasts derived from keloids and nor-mal skin, while TGF-β3 mRNA expres-sion was significantly lower in keloid fi-broblasts in comparison with fibroblastsderived from hypertrophic scar and nor-mal skin (44). Thus, specifically, beyond1 week, differential expression of TGF-βisoforms, receptors and activity modula-tors, rather than the mere presence or ab-sence of TGF-β, may have a major role inthe development of both keloids and hy-pertrophic scarring (48).
Indeed, antisense phosphorothioateoligonucleotides against TGF-β1 and -β2have been used in vivo to significantly re-duce postoperative scarring in rabbit andmouse models of glaucoma surgery (49).In two studies, Shah and colleagues(50,51) found that dermal wounds ofadult rats healed without scar-tissue for-
1 1 6 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S

mation after injection of a neutralizingantibody to TGF-β1 and -β2 into thewound margins, compared with controls.
The SMAD signal-transduction pathway as a downstream mediator ofTGF-β action. The SMADs are a familyof intracellular regulatory proteins thatact downstream of the TGF-β type I re-ceptor in the cell’s response to a specificTGF-β (Figure 3). Once these SMADs arephosphorylated, they form a complexwith the common mediator Co-SMAD 4.This SMAD complex translocates to thenucleus, where it is recruited to DNA bysite-specific inhibitors, activators or coac-tivators to regulate the transcription ofspecific genes (52).
SMAD intracellular signaling proteinscan be categorized into receptor-regulatedSMADs (R-SMADs), common-mediatorSMADs, and inhibitory SMADs (53). R-SMADs 3 and 4 have been identified asthe predominant mediators of autocrinestimulation by TGF-β in hypertrophic-scar–derived fibroblasts (54). The poten-tial importance of SMAD3 and its rela-tionship with TGF-β in keloid etiologyhas been demonstrated by Wang et al.,who showed that downregulation ofSMAD3 expression can significantly de-crease procollagen gene expression andreduce ECM deposition by keloid fibrob-lasts (55). Inhibitory SMAD 7 preventsphosphorylation of R-SMADs by formingstable associations with activated type ITGF-β receptors and thus provides nega-tive feedback to the actions of TGF-β (56).Indeed, a potential therapeutic benefit ofSMAD 7 overexpression has already beenshown in bleomycin-induced lung fibro-sis, postobstructive renal fibrosis and ex-cessive cutaneous scar formation (57–59).SMAD 3 inhibition and SMAD 7 overex-pression may thus be potential therapeu-tic targets to improve excessive scarring.
Interactions between keratinocytesand fibroblasts. Keratinocytes have beenshown to mediate the behavior of fibrob-lasts during wound healing throughtheir secretion, activation or inhibition ofgrowth factors such as TGF-β (32). Inparticular, the release of IL-1 from ker-atinocytes at the wound site seems to
represent the initial trigger for the in-flammatory reaction and serves as an au-tocrine signal to fibroblasts and endothe-lial cells, resulting in a pleiotropic effecton them (60,61). Greater thickness ofneodermis production was seen in fi-broblast-seeded skin models when ker-atinocytes from hypertrophic scars wereadded in culture (32). Similar resultswere detected with coculturing of keloid-derived keratinocytes and fibroblasts(62), suggesting that keratinocytes mighthave an important role in keloid and hy-pertrophic scar pathogenesis by produc-ing signals that stimulate the fibroblastsin the underlying dermis to proliferate orproduce more ECM. The basis for an in-herent abnormality among hypertrophicscar and keloid-derived keratinocytes re-mains elusive, however.
Mast cells. Our understanding of therole of the mast cell in scar formation isexpanding with new discoveries regard-ing cell–cell communication. Mast cellsare an additional leukocyte subset pres-
ent in the skin, and they are an importantsource of a variety of proinflammatorymediators that can promote inflammationand vascular changes (63). Mediated bythe release of soluble mediators such ashistamine, heparin and cytokines, mastcells have been shown to promote fibrob-last proliferation (64). Increased numbersof mast cells have been reported duringthe active period of hypertrophic andkeloid scar formation (28,65). Clinically,the release of histamine by these cellslikely contributes to the common patientcomplaint of itchiness. In addition, thevasodilatory effect of histamine may pro-mote erythema and leakage of plasmaproteins into the regional tissues (30).
Matrix Remodeling/Maturation PhaseMatrix metalloproteinases (MMPs).
The major effectors of ECM degradationand remodeling belong to a family ofstructurally related enzymes calledMMPs. The MMP family consists ofabout 25 zinc-dependent and calcium-
R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 1 7
Figure 3. The SMAD signal-transduction pathway as a downstream mediator of TGF-β ac-tion. The TGF-β receptor consists of type I and type II subunits that are serine-threonine ki-nases that signal through the SMAD family of proteins. Binding of TGF-β to its cell-surfacereceptor type II causes phosphorylation of the type I receptor by type II. The type I recep-tor is then able to phosphorylate and activate the R-SMAD proteins. Once these SMADsare phosphorylated, they form a complex with the common mediator Co-SMAD 4. ThisSMAD complex translocates to the nucleus, where the activated SMAD complex recruitsother transcription factors (TF) that together activate the expression of target genes me-diating the biological effects of TGF-β. Inhibitory SMAD 7 is able to prevent phosphoryla-tion of R-SMADs by forming stable associations with activated type I TGF-β receptors andthus provides negative feedback to the actions of TGF-β.

dependent proteinases in the mammaliansystem (66). The levels of MMP expres-sion in normal cells are low and allowhealthy connective tissue remodeling. Animbalance in expression of MMPs hasbeen implicated in a number of patholog-ical conditions such as dermal fibrosis(67) and tumor invasion and metastasis(68). In both conditions, cell interactionsbetween either fibroblasts and ker-atinocytes or fibroblasts and tumor cellsresult in increased MMP production. Inparticular, secreted cytokines and growthfactors, including IL-1β, PDGF, EGF andTNF-α, seem to play important roles incontrolling the signal mechanism in-volved in regulation of MMP expressionin fibroblasts (69). Several MMPs havebeen shown to mediate the breakdown oftype I and III collagen, the most abun-dant types of collagen in the skin ECM(66). Specifically, MMP-2 and MMP-9 ac-tivity persists after wound closure andseems to play a potent role in the remod-eling process (70). Interestingly, hyper-trophic scars and keloids were found tohave high levels of MMP-2 and low lev-els of MMP-9 (71). MMP-2 was shown tohave major effects on matrix remodelinglater in wound healing via degrading de-natured collagen, and MMP-9 was foundto be typically involved in early woundrepair by degrading native types IV andV collagen, elastin and fibronectin (72,73).Also, recent in vitro data suggested thatMMPs may downregulate inflammationvia cleavage of chemokines, which thenact as antagonists (74,75).
Decorin. Decorin, a small proteoglycanwith one dermatan sulfate sugar chain, isnormally prevalent in the dermal ECM.Decorin regulates collagen fibril, fiberand fiber-bundle organization and hasbeen shown to be decreased by about75% in hypertrophic scars (76). Decorin isable to bind and neutralize TGF-β, thusminimizing the stimulatory effects of thiscytokine on collagen, fibronectin and gly-cosaminoglycan production (32). The lowlevels of decorin found in hypertrophicscarring may thus account for their irreg-ular collagen organization, as well as in-creased ECM production (77). Zhang and
colleagues (78) showed similar results,with decorin inhibiting both the basaland TGF-β1–enhanced contraction of col-lagen gel by both normal and hyper-trophic scar fibroblasts, suggesting thatdecorin may have therapeutic potentialfor excessive skin contraction as observedin hypertrophic scarring. Mukhopadhyayand colleagues (79) examined the role ofdecorin in keloid tissue and found thatdecorin was able to decrease extracellularmatrix proteins, highlighting its impor-tance as an antifibrotic agent.
Apoptosis. Recently, apoptosis hasbeen shown to play a critical role in thetransition from granulation tissue intoscar formation after tissue injury (43). Asdescribed by Amour and others (32),wound epithelialization and scar colla-gen formation are accompanied by agradual decrease in cellularity on cross-sectional histology. Early immature hy-pertrophic scars are hypercellular; andduring the process of remodeling andmaturing, fibroblast cell density reducesto resemble normal skin, partly due toinduction of apoptosis. In particular,apoptosis of myofibroblasts can be de-tected 12 days after wounding, and is be-lieved to peak on day 20 in normal scarformation (32). In hypertrophic scar tis-sue of severely burned patients, however,the authors found that maximal apopto-sis occurred much later (19–30 monthsfollowing injury). The percentage of my-ofibroblasts was also higher in hyper-trophic scars compared with normalscars or in normal skin, and was foundto correlate with the size of the originalburn (80).
Scar maturation. Scar maturation isthe least recognized phase in the processof wound healing, and this process is rel-atively underresearched in regard to thealterations in the clinical and histologicappearance of a scar over time. In astudy of incisional scars in patients with-out any history of excessive scarring,Bond and colleagues (81) found progres-sive changes in relation to the dermalstructure but persistent fibroblastic den-sity at 4 months, indicating the existenceof a continuing high-turnover state simi-
lar to the proliferative phase, with sub-jects younger than 30 years displaying aprolonged longitudinal progression ofscar maturation compared with subjectsolder than 55 years (82). In another studyin which they examined the natural his-tory of scar redness and maturation inincisional and excisional wounds, thesame authors found that the majority ofscars fade at approximately 7 months.These investigators also showed that aconsiderable proportion of scars dis-played persistent redness at 12 months,in the absence of features suggestive ofhypertrophic or keloid scarring, and theyadvocated the term “rubor perseverans”to describe the physiologic redness of anormal scar as it matures beyond thefirst month (82).
CURRENT AND EMERGING TREATMENTSTRATEGIES
Multiple studies on hypertrophic scarand keloid formation have led to aplethora of therapeutic strategies to pre-vent or attenuate keloid and hyper-trophic scar formation. In 2002, Mustoeet al. published the “international clinicalrecommendations on scar management,”which serve as an outline for most of thecurrently published reviews (83). In a re-cently published work, Durani andBayat (84) evaluated for the first timeprimary clinical studies on keloid dis-ease therapy over the last 25 years andlevels of evidence for the treatmentmodalities assigned. These authors con-cluded that high-quality research inevaluating keloid therapy is still lacking.Within this review we critically discussthe techniques currently used toavoid/treat keloid and hypertrophic scarformation based on our experience froma dermatological and surgical perspec-tive (Table 2).
It is critical to note that generally mostof the therapeutic approaches we men-tion may be used for both hypertrophicscarring and keloids. Nevertheless, clini-cal differentiation between hypertrophicand keloid scars is of central importancebefore the initiation of any treatment,particularly before starting any surgical
1 1 8 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S

R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 1 9
Table 2. Hypertrophic scars and keloids: current therapeutic strategies.
Treatment Use Indications, efficiency and comments
Prophylaxis
Pressure therapy Continuous pressure (15–40 mmHg) for at least •Prophylaxis of hypertrophic burn scars, ear keloids 23 h/d ≥6 months of scar healing (postexcision)
•Controversial success•Reduced compliance due to frequent patient discomfort
Silicone gel sheeting ≥12 h/d for ≥2 months beginning 2 weeks after wound •Prophylaxis for the development of hypertrophic scars healing and keloids
•No effects on mature keloids and hypertrophic scars
Silicone gel Twice daily for 2 months beginning 2 weeks after wound closure
Flavonoids For example, Contractubex gel (Merz Pharma, •Limited to prophylaxis of hypertrophic scar and keloid Frankfurt, Germany), Mederma Skin Care Gel (Merz, developmentPharmaceuticals, Greensboro, NC, USA). Twice daily for 4 to 6 months beginning 2 weeks after wound closure
Current therapies
Corticosteroids Intralesional injections of TAC (10–40 mg/mL), several •First-line therapy for keloids, second-line therapy fortreatments once or twice a month hypertrophic scars
•Combination with surgery, PDL and cryotherapy•Common adverse effects: skin and subcutaneous fat atrophy, telangiectasias
Cryotherapy Contact/spray freezing with liquid nitrogen using •Overall effective for hypertrophic scars, for keloids 10–20 s freeze-thaw cycles combination with triamcinolone acetonide injections
recommended•Limited to management of smaller scars•Common adverse effects: blistering and pain
Scar revision Excision with linear, tension-free closure, split- or •Efficacious for therapy of hypertrophic scarringfull-thickness skin grafting, z-plasty, w-plasty •Recurrence rates of 45-100% after keloid excision
without adjuvant therapy
Radiotherapy Superficial x-rays, dosages 15–20 Gy, overall limit 40 Gy. •Overall good efficiency rates of adjuvant radiotherapyOver 5-6 sessions in the early postoperative period after keloid excision
•Common adverse effects: potential risk of malignant change/carcinogenesis
Laser therapy Short-pulsed dye laser (585-nm PDL) with doses ranging •Excellent therapeutic option for the treatment of from 6.0 to 7.5 J/cm2 (7-mm spot) or from 4.5 to primarily keloids and younger hypertrophic scars5.5 J/cm2 (10-mm spot), 2 to 6 treatments every •High recurrence rates with other (ablative) laser2 to 6 weeks techniques for the treatment of keloids
Emerging Therapies
Interferon Intralesional injection of INF-α2b (1.5–2 × 106 IU) •Clinical studies report overall effectivenesstwice daily over 4 days •Common adverse effects: flu-like symptoms on
injection5-FU Intralesional injection of 5-FU 50 mg/mL •Overall effective for the treatment of keloids and
hypertrophic scars•Common adverse effects: anemia, leucopenia, thrombocytopenia; blood-count monitoring is needed No therapy in pregnant women or patients with bonemarrow suppression

or laser related manipulations as speci-fied below.
ProphylaxisPrevention of pathologic scarring is
undoubtedly more effective than treat-ment. Thus, avoiding all unnecessarywounds in any patient, whether or notthe patient is prone to keloid/hyper-trophic scars, remains an obvious but im-perfect solution (6). Because delayed ep-ithelialization beyond 10 to 14 daysincreases the incidence of hypertrophicscarring dramatically (83), achievementof rapid epithelialization is mandatoryfor avoiding excessive scar formation. Inparticular, wounds subjected to tensiondue to motion, body location or loss oftissue are at increased risk of scar hyper-trophy and spreading (85). Thus, in caseof cutaneous injury, the importance ofrapid primary closure of wounds underlittle to no tension cannot be overstated.It is also crucial to adequately debridecontaminated wounds, obtain good he-mostasis, handle tissues gently and limitforeign bodies in the form of debris andbraided polyfilamentous suture material,such as polyglactin or silk (6).
Pressure therapy. Pressure therapyhas been the preferred conservativemanagement for both the prophylaxisand treatment of hypertrophic scars andkeloids since the 1970s. Currently, pres-sure garments are predominantly usedfor the prophylaxis of hypertrophic burnscar formation, despite controversialdata regarding their value in reducingexcessive scarring and little scientific ev-idence supporting their use (5). Themechanism of action of pressure therapyremains poorly understood; however,possible mechanisms are decreased col-lagen synthesis attributable to limitingof the supply of blood, oxygen and nu-trients to the scar tissue (86–88) and in-creased apoptosis (89).
Recommendations for the amount ofpressure and the duration of the therapyare based merely on empirical observa-tions and advocate continuous pressureof 15–40 mmHg for at least 23 hoursand/or 1 day for more than 6 months
while the scar is still active (87,90). How-ever, compression therapy is ultimatelylimited by inability to adequately fit thegarment to the wounded area and by pa-tient discomfort, which frequently re-duces compliance.
Silicone gel sheeting. Topical siliconegel sheeting has been a well-establishedtreatment for management of scars sinceits introduction in the early 1980s, and itstherapeutic effects on predominantly hy-pertrophic scars have been well docu-mented in the literature (91,92). Currentopinion suggests that occlusion and hy-dration are likely the mechanisms of thetherapeutic action of silicone gel sheetingrather than an inherent antiscarringproperty of silicone (93). Silicone sheetsare recommended to be worn for≥12 hours and/or 1 day for at least2 months beginning 2 weeks after woundhealing. Silicone gel is favored for areasof consistent movement, where sheetingwill not conform, and should be appliedtwice daily (6).
Flavonoids. Flavonoids (quercetin andkaempferol) are found in well-known top-ical scar creams, such as Mederma skincare gel (Merz Pharmaceuticals, Greens-boro, NC, USA) and Contractubex gel(Merz Pharma, Frankfurt, Germany). Sofar, efficacy studies testing the ultimatebenefit of these flavonoid-containing topi-cal scar creams have provided controver-sial data (94–98). Interestingly however,quercetin, a dietary bioflavonoid, hasbeen recently shown to inhibit fibroblastproliferation, collagen production andcontraction of keloid and hypertrophicscar-derived fibroblasts. A study by Phanand others (94) suggested that these in-hibitory effects may be mediated throughinhibition of the above discussed SMAD2, 3, and 4 expression by quercetin.
Emerging Prophylactic ApproachesImiquimod 5% cream. Imiquimod
5% cream, a topical immune-responsemodifier, is approved for the treatmentof genital warts, basal cell carcinomaand actinic keratoses (99). Imiquimodstimulates interferon, a proinflammatorycytokine, which increases collagen break-
down. In addition, imiquimod alters theexpression of apoptosis-associatedgenes (100). Therefore, it has been usedin an attempt to reduce keloid recur-rence after excision and was reported tohave positive effects on the recurrencerate of keloids after postoperative appli-cation (101). However, in a prospective,double-blind, placebo-controlled pilotstudy in which imiquimod 5% creamwas applied nightly for 2 weeks beforebeing given 3 times/week under occlu-sion for 1 month postoperatively, no sig-nificant difference in keloid recurrencerates between groups could be detected(102). The role of imiquimod in the pre-vention of postsurgical keloid recur-rence thus remains questionable. In apreliminary, small, randomized, pro-spective clinical trial, imiquimod wasshown to improve hypertrophic scarquality after surgery (103), but addi-tional studies with a larger sample sizeand longer follow-up are necessary todetermine the role of imiquimod 5%cream in hypertrophic scar therapy.
Recombinant TGF-β3 and mannose-6-phosphate. A recently published mile-stone study by Ferguson and colleagues(104) on the prophylactic effects ofTGF-β3 on skin scarring has further in-creased the current interest in the TGF-βfamily. In three double-blind, placebo-controlled studies, intradermal avoter-min (recombinant, active human TGF-β3at concentrations ranging from 0.25 to500 ng/100 μL per linear centimeterwound margin) was administered toboth margins of 1-cm, full-thickness skinincisions before wounding and 24 hourslater, in healthy subjects. In both youngand old participants, only one dose regi-men, 50 ng per 100 μL per linear cen-timeter, achieved more than 10% scar im-provement in nearly two-thirds ofwounds. However, in the final phase IIstudy, each of three doses was judged tobe effective by lay observers and by clini-cians (105). Although the investigatorsacknowledged their commercial interestsin TGF-β3, adherence to established stan-dards in this translational investigationand the rigorous nature of the statistical
1 2 0 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S

analysis in a well-powered series of stud-ies provided strong evidence for the ben-efits of avotermin in this setting.
In March 2009, the company Renovoreported the results of a double-blind,placebo-controlled, randomized phase 2efficacy trial in 195 male and female sub-jects to investigate the safety and efficacyof inhibition by TGF-β1 and -β2 usingtwo dose levels of mannose-6-phosphate(Juvidex®, 300 mmol/L and 600 mmol/L)via two routes of administration (intra-dermal and topical in combination andtopical alone) in the acceleration of heal-ing of split-thickness skin-graft donorsites. Although the trial did not meet itsprimary endpoint, which was demon-stration of a statistically significant dif-ference in the time to complete woundclosure at the skin-graft site as assessedby the investigating physician, it didmeet some of the specified secondaryendpoints with statistical significance.These included a between-patient com-parison performed by an external panelof clinical experts who assessed photo-graphs of the donor sites, where the300 mmol/L Juvidex topical-alone appli-cation versus standard care showed astatistically significant acceleration ofhealing in favor of Juvidex.
Current Treatment StrategiesIntralesional corticosteroid injections.
Since the mid-1960s intralesional steroidinjections have gained popularity as oneof the most common approaches to atten-uate hypertrophic scar and keloid forma-tion (106), while topical administration ofcorticosteroid-containing creams has beenused with only varying success. Most ofthe known effects of corticosteroids arethought to result primarily from its sup-pressive effects on the inflammatory process in the wound (93), and secondar-ily from diminished collagen and gly-cosaminoglycan synthesis, inhibition offibroblast growth (107) and enhanced col-lagen and fibroblast degeneration (108).Two or three injections of triamcinoloneacetonide (TAC, 10 to 40 mg/mL) areusually sufficient, although occasionallyinjections are continued for 6 months or
more (106). Response rates have beenhighly variable, with figures rangingfrom 50% to 100%, and a recurrence rateof 9% to 50% (109). An important findingwas that intralesional corticosteroid injec-tions, when used alone, have the most ef-fect on younger keloids, which can be-come completely flattened. In older scarsand keloids, corticosteroids can softenand flatten the scars only to some extentand can provide symptomatic relief (5).Injections may be used alone or com-bined with other therapies (10), of whichthe combination with cryotherapy or sur-gery are the most widely used modalitiesin clinical practice (110). Side effects in-clude dermal atrophy, telangiectasia andpain at the site of injection. The latter canbe averted by topical anesthesia and/orregional injections of local anestheticaround the scars to be injected (30). De-spite relatively few randomized, prospec-tive studies, TAC remains a first-line ther-apy for the treatment of early keloids anda second-line therapy for the treatment ofearly hypertrophic scars if other easiertreatments have not been efficacious (83).
Cryotherapy. Cryotherapy has beenused as monotherapy and in conjunctionwith other forms of treatment for exces-sive scars. In particular, the combinationof cryotherapy with intralesional TAC in-jections seems to yield marked improve-ment of hypertrophic scars and keloids(111–113). We recommend cryotherapydirectly before the administration of in-tralesional TAC injections, because suc-cess rates seem to be increased with thissequence.
Cryotherapy is believed to induce vas-cular damage that may lead to anoxiaand ultimately tissue necrosis (114). Suc-cess rates in studies in which contact orspray cryosurgery with liquid nitrogenwas used varied between 32% and 74%after two or more sessions, with higherresponse rates of hypertrophic scars com-pared with keloids (83,115,116). The use-fulness of cryotherapy, however, is lim-ited to the management of small scars. Adelay of several weeks between sessionsis usually required for postoperativehealing, and the commonly occurring
side effects, including permanent hypo-and hyperpigmentation, moderate skinatrophy, blistering and postoperativepain, are major handicaps (5,116). Re-cently, the intralesional-needle cryoprobemethod has been assessed in the treat-ment of hypertrophic scars and keloids(117), and has been demonstrated to haveincreased efficacy compared with that ob-tained with contact/ spray probes andshorter reepithelialization periods (117).
Surgical manipulation. Surgical exci-sion remains the traditional treatment forkeloids and hypertrophic scars (6). How-ever, it is imperative to clearly differenti-ate between hypertrophic scars andkeloids before starting any surgical ma-nipulations.
In case of hypertrophic scars, timing ofsurgical treatment is an important con-sideration in the treatment protocol ofstrategies for scar revision. Scars matureduring a period of at least 1 year and canshow decreased contractures along withflattening, softening, and repigmentationwithout any physical manipulation (93).Surgical excision thus might not beneeded, even though postexcisional re-currence rates of the original hyper-trophic scar are usually low (13,15).
Recurrence rates of keloids after exci-sion, in contrast, range between 45% and100% (83). Given this high recurrencerate, surgical intervention without adju-vant therapy, such as postexcisional cor-ticosteroid injections or radiation, shouldbe considered with caution. Excisionmay frequently result in a longer scarthan the original keloid, and recurrencein this new area of trauma may lead toan even larger keloid (109,118). Surgicalrepair (core excision with low-tensionwound closure, or shave excision) of ear-lobe keloids with corticosteroid injectionsand postoperative pressure on the inci-sion site, however, usually providesgood cosmetic results (119).
Radiotherapy. Superficial x-rays, electron-beam therapy and low- or high-dose–rate brachytherapy have been usedwith good results in scar reduction pro-tocols, primarily as adjuncts to surgicalremoval of keloids (120). The effects of
R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 2 1

radiation on keloids are thought to bemediated through inhibition of neovas-cular buds and proliferating fibroblasts,which result in decreased collagen pro-duction (93). Electron beam irradiation isusually started 24 to 48 h after keloid ex-cision, and the total dose is limited to 40Gy over the course of several administra-tions to prevent side effects such ashypo- and hyperpigmentation, erythema,telangiectasia and atrophy (121). How-ever, because radiation entails a risk ofcarcinogenesis, particularly in areas suchas the breast and thyroid, its use shouldbe handled with caution (5,15).
Laser therapy. Since the introductionof laser treatment for keloids in themid-1980s (122), the therapeutic use ofmore and more lasers with differentwavelengths has been investigated, andsuccess has varied. Until today, themost encouraging results have been ob-tained with the 585-nm pulsed-dyelaser (PDL), which has been recognizedas an excellent therapeutic option forthe treatment of younger hypertrophicscars and primarily keloids (123).Nonoverlapping laser pulses at fluencesranging from 6.0 to 7.5 J/cm2 (7-mmspot) or from 4.5 to 5.5 J/cm2 (10-mmspot) have been recommended for thetreatment of hypertrophic scars andkeloids (124). Two to six treatmentsmay be necessary to successfully im-prove scar resolution, including scarcolor, height, pliability and texture(123). By causing local ischemia via de-stroying blood vessels, 585-nm PDLtherapy is believed to induce neocolla-genesis, collagen-fiber heating with dis-sociation of disulfide bonds and subse-quent collagen-fiber realignment, anddecreased fibroblast proliferation aswell as release of histamine and otherfactors that influence fibroblast activity(125–127). Adverse effects include tran-sient hyper- or hypopigmentation andblistering (125,128). Hyperpigmentationhas been reported with a frequency of1–24% (129,130). The most common ad-verse side effect of 585-nm PDL treat-ment is postoperative purpura, whichcan persist for 7–10 days.
Emerging TherapiesIFN injections. IFN therapy, which
has potential therapeutic benefit in thetreatment of abnormal scars, is based onthe effect of IFN in decreasing the syn-thesis of collagen types I and III(15,131). Specifically, IFN-α2b has beenproposed to have antiproliferative prop-erties, and it may improve the patho-logic features of dermal fibrosis directlyor by antagonizing the effects of TGF-βand histamine (132). In vivo, systemicadministration of IFN-α2b in severelyburned patients resulted in improvedclinical appearance of the hypertrophicscars and a lower Vancouver Burn ScarAssessment score (133). IFN-α2b admin-istered intralesionally (1.5 × 106 IU,given twice daily over 4 days) wasfound to result in a 50% reduction ofkeloid size by 9 days and thus wasmuch more effective than intralesionallyinjected corticosteroid (132). Hyper-trophic scars injected three times weeklywith IFN-α2b showed significant meanrates of improvement and sustained re-duced serum TGF-β levels (134). Unfor-tunately, adverse effects are commonwith IFN treatment and include flu-likesymptoms and pain on injection (15).Although IFN is an expensive form oftherapy, it remains a promising thera-peutic approach in the management ofexcessive scars.
Bleomycin. Bleomycin sulfate, an-other antineoplastic agent that wasfound to directly inhibit collagen syn-thesis via decreased stimulation byTGF-β1 (135), was first investigated inthe mid-1990s as a scar-reducing agent(136). After administering three to fiveintralesional injections of bleomycinwithin a 1-month period, the authorsobserved complete regression in 69.4%of the keloids. Subsequent studies re-vealed similar results, with significantimprovement in hypertrophic scar andkeloid height and pliability as well asreduction in erythema, pruritus andpain (135,137,138). Occasionally, devel-opment of hyperpigmentation and der-mal atrophy may occur with bleomycintreatment. Because of bleomycin’s toxic-
ity, clinicians are encouraged to beaware of associated potential problems.However, systemic toxic effects of in-tralesionally administered bleomycinseem to be uncommon (15). Bleomycinmay thus be a promising agent for thetherapy of keloids and hypertrophicscars; however, further investigationand efficacy trials are needed before thisagent is included in future treatmentprotocols.
5-Fluorouracil (5-FU). 5-FU is apyrimidine analog that is used as an an-timetabolite in cancer chemotherapy(109). 5-FU is converted intracellularlyto its active version, which was sug-gested to directly increase fibroblastapoptosis via inhibiting DNA synthesispreferentially in rapidly proliferatingand metabolizing cells (58,139). In 1999,Fitzpatrick (140) was the first to reportthe use of 5-FU to effectively reducescars during his 9-year experience, inwhich he administered more than 5000injections to more than 1000 patients.Ever since, the use of intralesional 5-FUin combination or as a sole agent fortreatment of keloids has been shown tobe effective. In a prospective, random-ized trial including 28 consecutive pa-tients with keloids of varying size andduration, weekly intralesional 5-FU in-jections (50 mg/mL) for 12 weeks re-sulted in reduction in scar size of atleast 50% in the majority of the patients,with no patient showing failure to re-spond to therapy or recurrence of symp-toms within the follow-up period of 24months (141). Adverse side effects in-cluded pain, ulceration and burningsensations. Intralesional 5-FU treatmenthas also been used for the treatment ofinflamed hypertrophic scars and seemsto be both effective and safe (140).
CONCLUSIONSScarring following surgery or injury is
difficult to predict, and both physiciansand their patients are highly concernedwith minimizing scar appearance andvalue as clinically meaningful even smallimprovements in scarring. Despite aplethora of various in vivo and in vitro
1 2 2 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S

studies, to date only limited informationis available on the exact cause of hyper-trophic scar and keloid formation.Knowledge of the cellular and molecularmechanisms implicated in the develop-ment of these fibroproliferative disordersremains relatively poor because of thelack of representative and well- recognized animal models of human hypertrophic scar formation. Instead,scar tissue for study is usually obtainedfrom humans undergoing scar revision—usually months after the scar first devel-oped. Therefore, early alterations inwound repair mechanisms that likely de-termine the development of hypertrophicscars may be missed.
Existing prophylactic and therapeuticstrategies include pressure therapy, sili-cone gel sheeting, intralesional TAC,cryosurgery, radiation, laser therapy, INF,5-FU and surgical excision as well as amultitude of extracts and topical agents.Many of these treatments have beenproven to be effective through extensiveuse, but few have been supported bywell-designed prospective studies withadequate control groups.
Emerging therapies for patients proneto excessive scars support earlier interven-tions aimed at modulating single celltypes, inflammatory metabolites, cy-tokines or signaling receptors. Encourag-ing results obtained with the use of recom-binant human TGF-β3 and anti–TGF-β1and -β2 support substantial optimism re-garding the future discovery of new solu-tions to difficult fibrotic disorders.
DISCLOSUREThe authors declare that they have no
competing interests as defined by Molecu-lar Medicine, or other interests that mightbe perceived to influence the results anddiscussion reported in this paper.
REFERENCES1. Sund B. (2000) New Developments in Wound Care.
PJB Publications, London, pp. 1–255.2. Berman B, Bieley HC. (1995) Keloids. J. Am. Acad.
Dermatol. 33:117–23.3. Peacock EE Jr, Madden JW, Trier WC. (1970) Bio-
logic basis for the treatment of keloids and hy-pertrophic scars. South. Med. J. 63:755–60.
4. Mancini RE, Quaife JV. (1962) Histogenesis of ex-perimentally produced keloids. J. Invest. Derma-tol. 38:143–81.
5. Atiyeh BS. (2007) Nonsurgical management ofhypertrophic scars: evidence-based therapies,standard practices, and emerging methods. Aes-thetic. Plast. Surg. 31:468–94.
6. Slemp AE, Kirschner RE. (2006) Keloids andscars: a review of keloids and scars, their patho-genesis, risk factors, and management. Curr.Opin. Pediatr. 18:396–402.
7. Wheeland RG. (1996) Keloids and hypertrphicscars. In: Cutaneous Medicine and Surgery. ArndtKA, Robinson JK, Leboit PE, Wintroub BU (eds.).Saunders Elsevier, Philadelphia, pp. 900–5.
8. Alster TS, West TB. (1997) Treatment of scars: areview. Ann. Plast. Surg. 39:418–32.
9. Hawkins HK. (2007) Pathophysiology of theburn scar. In: Total Burn Care. Herndon DN (ed.)Saunders Elsevier, Philadelphia, pp. 608–19.
10. Murray JC. (1994) Keloids and hypertrophicscars. Clin. Dermatol. 12:27–37.
11. Al-Attar A, et al. (2006) Keloid pathogenesis andtreatment. Plast. Reconstr. Surg. 117:286–300.
12. From L, Assad D. (1993) Neoplasms, pseudoneo-plasms, and hyperplasia of supporting tissue ori-gin. In: Dermatology in General Medicine. JeffersJD, Englis MR (eds.). McGraw-Hill, New York,pp. 1198–99.
13. Muir IF. (1990) On the nature of keloid and hy-pertrophic scars. Br. J. Plast. Surg. 43:61–9.
14. Niessen FB, Spauwen PH, Schalkwijk J, Kon M.(1999) On the nature of hypertrophic scars andkeloids: a review. Plast. Reconstr. Surg. 104:1435–58.
15. Leventhal D, Furr M, Reiter D. (2006) Treatmentof keloids and hypertrophic scars: a meta-analy-sis and review of the literature. Arch. Facial. Plast.Surg. 8:362–8.
16. Sephel GC, Woodward SC. (2001) Repair, regener-ation, and fibrosis. In: Rubin’s Pathology. Rubin E(ed.). Lippincott, Williams & Wilkins, Baltimore,pp. 84–117.
17. Oluwasanmi JO. (1974) Keloids in the African.Clin. Plast. Surg. 1:179–95.
18. Moustafa MF, Abdel-Fattah MA, Abdel-FattahDC. (1975) Presumptive evidence of the effect ofpregnancy estrogens on keloid growth: case re-port. Plast. Reconstr. Surg. 56:450–3.
19. Deitch EA, et al. (1983) Hypertrophic burn scars:analysis of variables. J. Trauma. 23:895–8.
20. Lewis WH, Sun KK. (1990) Hypertrophic scar: agenetic hypothesis. Burns. 16:176–8.
21. Murray CJ, Pinnel SR. (1992) Keloids and exces-sive dermal scarring. In: Woundhealing, Biochemi-cal and Clinical Aspects. Cohen IK, DiegelmannRF, Lindblad WJ (eds.). Saunders Elsevier, Phila-delphia, pp. 500–9.
22. Bayat A, et al. (2005) Keloid disease: clinical rele-vance of single versus multiple site scars. Br. J.Plast. Surg. 58:28–37.
23. Marneros AG, et al. (2004) Genome scans pro-vide evidence for keloid susceptibility loci onchromosomes 2q23 and 7p11. J. Invest. Dermatol.122:1126–32.
24. Brown JJ, Ollier WE, Thomson W, Bayat A. (2008)Positive association of HLA-DRB1*15 with keloiddisease in Caucasians. Int. J. Immunogenet. 35:303–7.
25. Ford LC, King DF, Lagasse LD, Newcomer V.(1983) Increased androgen binding in keloids: apreliminary communication. J. Dermatol. Surg.Oncol. 9:545–7.
26. Schierle HP, Scholz D, Lemperle G. (1997) Ele-vated levels of testosterone receptors in keloidtissue: an experimental investigation. Plast. Re-constr. Surg. 100:390–6.
27. Placik OJ, Lewis VL Jr. (1992) Immunologic asso-ciations of keloids. Surg. Gynecol. Obstet.175:185–93.
28. Smith CJ, Smith JC, Finn MC. (1987) The possiblerole of mast cells (allergy) in the production ofkeloid and hypertrophic scarring. J. Burn Care Re-habil. 8:126–31.
29. Ramakrishnan KM, Thomas KP, SundararajanCR. (1974) Study of 1,000 patients with keloids inSouth India. Plast. Reconstr. Surg. 53:276–80.
30. Tredget EE, Nedelec B, Scott PG, Ghahary A.(1997) Hypertrophic scars, keloids, and contrac-tures: the cellular and molecular basis for ther-apy. Surg. Clin. North Am. 77:701–30.
31. Brown JJ, Bayat A. (2009) Genetic susceptibilityto raised dermal scarring. Br. J. Dermatol.161:8–18.
32. Armour A, Scott PG, Tredget EE. (2007) Cellularand molecular pathology of HTS: basis for treat-ment. Wound Repair Regen. 15 Suppl 1:S6–17.
33. Wynn TA. (2004) Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat. Rev. Immunol. 4:583–94.
34. Doucet C, et al. (1998) Interleukin (IL) 4 and IL-13act on human lung fibroblasts. Implication inasthma. J. Clin. Invest. 101:2129–39.
35. Kamp DW. (2003) Idiopathic pulmonary fibrosis:the inflammation hypothesis revisited. Chest.124:1187–90.
36. Ladak A, Tredget EE. (2009) Pathophysiologyand management of the burn scar. Clin. Plast.Surg. 36:661–74.
37. Butler PD, Longaker MT, Yang GP. (2008) Currentprogress in keloid research and treatment. J. Am.Coll. Surg. 206:731–41.
38. Ishihara H, et al. (2000) Keloid fibroblasts resistceramide-induced apoptosis by overexpressionof insulin-like growth factor I receptor. J. Invest.Dermatol. 115:1065–71.
39. Tuan TL, Nichter LS. (1998) The molecular basisof keloid and hypertrophic scar formation. Mol.Med. Today. 4:19–24.
40. Smith JC, et al. (2008) Gene profiling of keloid fi-broblasts shows altered expression in multiple fi-brosis-associated pathways. J. Invest. Dermatol.128:1298–310.
41. Bullard KM, Longaker MT, Lorenz HP. (2003)Fetal wound healing: current biology. World J.Surg. 27:54–61.
42. Szulgit G, et al. (2002) Alterations in fibroblastalpha1beta1 integrin collagen receptor expressionin keloids and hypertrophic scars. J. Invest. Der-matol. 118:409–15.
R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 2 3

43. Kose O, Waseem A. (2008) Keloids and hyper-trophic scars: are they two different sides of thesame coin? Dermatol. Surg. 34:336–46.
44. Bock O, et al. (2005) Studies of transforminggrowth factors beta 1–3 and their receptors I andII in fibroblast of keloids and hypertrophic scars.Acta. Derm. Venereol. 85:216–20.
45. Schmid P, et al. (1998) Enhanced expression oftransforming growth factor-beta type I and typeII receptors in wound granulation tissue and hy-pertrophic scar. Am. J. Pathol. 152:485–93.
46. Lee TY, et al. (1999) Expression of transforminggrowth factor beta 1, 2, and 3 proteins in keloids.Ann. Plast. Surg. 43:179–84.
47. Xia W, et al. (2004) Complex epithelial-mesenchymalinteractions modulate transforming growth factor-beta expression in keloid-derived cells. Wound Re-pair Regen. 12:546–56.
48. Lu L, et al. (2005) The temporal effects of anti-TGF-beta1, 2, and 3 monoclonal antibody onwound healing and hypertrophic scar formation.J. Am. Coll. Surg. 201:391–7.
49. Cordeiro MF, et al. (2003) Novel antisenseoligonucleotides targeting TGF-beta inhibit invivo scarring and improve surgical outcome.Gene Ther. 10:59–71.
50. Shah M, Foreman DM, Ferguson MW. (1992)Control of scarring in adult wounds by neutralis-ing antibody to transforming growth factor beta.Lancet. 339:213–4.
51. Shah M, Foreman DM, Ferguson MW. (1995)Neutralisation of TGF-beta 1 and TGF-beta 2or exogenous addition of TGF-beta 3 to cuta-neous rat wounds reduces scarring. J. Cell. Sci.108(Pt 3): 985–1002.
52. Cutroneo KR. (2007) TGF-beta-induced fibrosisand SMAD signaling: oligo decoys as naturaltherapeutics for inhibition of tissue fibrosis andscarring. Wound Repair Regen. 15 Suppl 1: S54–60.
53. ten Dijke P, Hill CS. (2004) New insights intoTGF-beta-Smad signalling. Trends Biochem. Sci.29:265–73.
54. Kopp J, et al. (2005) Abrogation of transforminggrowth factor-beta signaling by SMAD7 inhibitscollagen gel contraction of human dermal fibrob-lasts. J. Biol. Chem. 280:21570–6.
55. Wang Z, et al. (2007) Inhibition of Smad3 expres-sion decreases collagen synthesis in keloid dis-ease fibroblasts. J. Plast. Reconstr. Aesthet. Surg.60:1193–9.
56. Nakao A, et al. (1997) Identification of Smad7, aTGFbeta-inducible antagonist of TGF-beta sig-nalling. Nature. 389:631–5.
57. Dooley S, et al. (2003) Smad7 prevents activationof hepatic stellate cells and liver fibrosis in rats.Gastroenterology. 125:178–91.
58. Chen MA, Davidson TM. (2005) Scar manage-ment: prevention and treatment strategies. Curr.Opin. Otolaryngol. Head Neck Surg. 13:242–7.
59. Terada Y, et al. (2002) Gene transfer of Smad7using electroporation of adenovirus preventsrenal fibrosis in post-obstructed kidney. KidneyInt. 61: S94–8.
60. Niessen FB, Schalkwijk J, Vos H, Timens W.(2004) Hypertrophic scar formation is associatedwith an increased number of epidermal Langer-hans cells. J. Pathol. 202:121–9.
61. Andriessen MP, Niessen FB, Van de Kerkhof PC,Schalkwijk J. (1998) Hypertrophic scarring is as-sociated with epidermal abnormalities: an im-munohistochemical study. J. Pathol. 186:192–200.
62. Lim IJ, et al. (2001) Investigation of the influenceof keloid-derived keratinocytes on fibroblastgrowth and proliferation in vitro. Plast. Reconstr.Surg. 107:797–808.
63. Eming SA, Krieg T, Davidson JM. (2007) Inflam-mation in wound repair: molecular and cellularmechanisms. J. Invest. Dermatol. 127:514–25.
64. Moyer KE, Saggers GC, Ehrlich HP. (2004) Mastcells promote fibroblast populated collagen latticecontraction through gap junction intercellularcommunication. Wound Repair. Regen. 12:269–75.
65. Noli C, Miolo A. (2001) The mast cell in woundhealing. Vet. Dermatol. 12:303–13.
66. Ghahary A, Ghaffari A. (2007) Role of keratinocyte-fibroblast cross-talk in development of hyper-trophic scar. Wound Repair Regen. 15 Suppl 1:S46–53.
67. Ghahary A, et al. (1996) Collagenase productionis lower in post-burn hypertrophic scar fibrob-lasts than in normal fibroblasts and is reduced byinsulin-like growth factor-1. J. Invest. Dermatol.106:476–81.
68. Birkedal-Hansen H, et al. (1993) Matrix metallo-proteinases: a review. Crit. Rev. Oral. Biol. Med.4:197–250.
69. Johnson-Wint B. (1988) Do keratinocytes regulatefibroblast collagenase activities during morpho-genesis? Ann. N. Y. Acad. Sci. 548:167–73.
70. Fujiwara M, Muragaki Y, Ooshima A. (2005)Keloid-derived fibroblasts show increased secre-tion of factors involved in collagen turnover anddepend on matrix metalloproteinase for migra-tion. Br. J. Dermatol. 153:295–300.
71. Neely AN, et al. (1999) Gelatinase activity inkeloids and hypertrophic scars. Wound RepairRegen. 7:166–71.
72. Mauviel A. (1993) Cytokine regulation of metal-loproteinase gene expression. J. Cell. Biochem.53:288–95.
73. Zhang Y, McCluskey K, Fujii K, Wahl LM. (1998)Differential regulation of monocyte matrix metal-loproteinase and TIMP-1 production by TNF-alpha, granulocyte-macrophage CSF, and IL-1beta through prostaglandin-dependent and -independent mechanisms. J. Immunol. 161:3071–6.
74. McQuibban GA, et al. (2002) Matrix metallopro-teinase processing of monocyte chemoattractantproteins generates CC chemokine receptor antag-onists with anti-inflammatory properties in vivo.Blood. 100:1160–7.
75. McQuibban GA, et al. (2000) Inflammationdampened by gelatinase A cleavage of monocytechemoattractant protein-3. Science. 289:1202–6.
76. Scott PG, et al. (1996) Chemical characterizationand quantification of proteoglycans in human
post-burn hypertrophic and mature scars. Clin.Sci. (Lond). 90:417–25.
77. Sayani K, et al. (2000) Delayed appearance ofdecorin in healing burn scars. Histopathology.36:262–72.
78. Zhang Z, et al. (2009) Recombinant humandecorin inhibits TGF-beta1-induced contractionof collagen lattice by hypertrophic scar fibrob-lasts. Burns. 35:527–37.
79. Mukhopadhyay A, et al. (2010) Syndecan-2and decorin: proteoglycans with a difference—implications in keloid pathogenesis. J. Trauma.68:999–1008.
80. Nedelec B, et al. (2001) Myofibroblasts and apo-ptosis in human hypertrophic scars: the effect ofinterferon-alpha2b. Surgery. 130:798–808.
81. Bond JS, et al. (2008) Maturation of the humanscar: an observational study. Plast. Reconstr. Surg.121:1650–8.
82. Bond JS, et al. (2008) Scar redness in humans:how long does it persist after incisional and exci-sional wounding? Plast. Reconstr. Surg.121:487–96.
83. Mustoe TA, et al. (2002) International clinical rec-ommendations on scar management. Plast. Re-constr. Surg. 110:560–71.
84. Durani P, Bayat A. (2008) Levels of evidence forthe treatment of keloid disease. J. Plast. Reconstr.Aesthet. Surg. 61:4–17.
85. Mutalik S. (2005) Treatment of keloids and hy-pertrophic scars. Indian J. Dermatol. Venereol. Lep-rol. 71:3–8.
86. Baur PS, et al. (1976) Ultrastructural analysis ofpressure-treated human hypertrophic scars. J. Trauma. 16:958–67.
87. Macintyre L, Baird M. (2006) Pressure garmentsfor use in the treatment of hypertrophic scars—areview of the problems associated with their use.Burns. 32:10–5.
88. Kelly AP. (2004) Medical and surgical therapiesfor keloids. Dermatol. Ther. 17:212–8.
89. Reno F, et al. (2003) In vitro mechanical compres-sion induces apoptosis and regulates cytokinesrelease in hypertrophic scars. Wound RepairRegen. 11:331–6.
90. Van den Kerckhove E, et al. (2005) The assess-ment of erythema and thickness on burn relatedscars during pressure garment therapy as a pre-ventive measure for hypertrophic scarring.Burns. 31:696–702.
91. Sawada Y, Sone K. (1992) Hydration and occlu-sion treatment for hypertrophic scars andkeloids. Br. J. Plast. Surg. 45:599–603.
92. Fulton JE, Jr. (1995) Silicone gel sheeting for the pre-vention and management of evolving hypertrophicand keloid scars. Dermatol. Surg. 21:947–51.
93. Reish RG, Eriksson E. (2008) Scar treatments:preclinical and clinical studies. J. Am. Coll. Surg.206:719–30.
94. Phan TT, et al. (2003) Quercetin inhibits fibronectinproduction by keloid-derived fibroblasts. Implica-tion for the treatment of excessive scars. J. Derma-tol. Sci. 33:192–4.
1 2 4 | G A U G L I T Z E T A L . | M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1
H Y P E R T R O P H I C S C A R S A N D K E L O I D S

95. Jackson BA, Shelton AJ. (1999) Pilot study eval-uating topical onion extract as treatment forpostsurgical scars. Dermatol. Surg. 25:267–9.
96. Chung VQ, Kelley L, Marra D, Jiang SB. (2006)Onion extract gel versus petrolatum emollienton new surgical scars: prospective double-blinded study. Dermatol. Surg. 32:193–7.
97. Beuth J, et al. (2006) Safety and efficacy of local ad-ministration of contractubex to hypertrophic scarsin comparison to corticosteroid treatment. Resultsof a multicenter, comparative epidemiological co-hort study in Germany. In Vivo. 20:277–83.
98. Ho WS, Ying SY, Chan PC, Chan HH. (2006) Useof onion extract, heparin, allantoin gel in pre-vention of scarring in Chinese patients havinglaser removal of tattoos: a prospective random-ized controlled trial. Dermatol. Surg. 32:891–6.
99. Asilian A, Darougheh A, Shariati F. (2006) Newcombination of triamcinolone, 5-fluorouracil,and pulsed-dye laser for treatment of keloid andhypertrophic scars. Dermatol. Surg. 32:907–15.
100. Zurada JM, Kriegel D, Davis IC. (2006) Topicaltreatments for hypertrophic scars. J. Am. Acad.Dermatol. 55:1024–31.
101. Berman B, Kaufman J. (2002) Pilot study of theeffect of postoperative imiquimod 5% cream onthe recurrence rate of excised keloids. J. Am.Acad. Dermatol. 47:S209–11.
102. Berman B, et al. (2009) Treatment of keloid scarspost-shave excision with imiquimod 5% cream:A prospective, double-blind, placebo-controlledpilot study. J. Drugs Dermatol. 8:455–8.
103. Prado A, Andrades P, Benitez S, Umana M.(2005) Scar management after breast surgery:preliminary results of a prospective, random-ized, and double-blind clinical study with al-dara cream 5% (imiquimod). Plast. Reconstr.Surg. 115:966–72.
104. Ferguson MW, et al. (2009) Prophylactic admin-istration of avotermin for improvement of skinscarring: three double-blind, placebo-controlled,phase I/II studies. Lancet. 373:1264–74.
105. Bush J, et al. (2010) Therapies with emerging evi-dence of efficacy: avotermin for the improve-ment of scarring. Dermatol Res Pract 2010:690613.
106. Jalali M, Bayat A. (2007) Current use of steroidsin management of abnormal raised skin scars.Surgeon. 5:175–80.
107. Cruz NI, Korchin L. (1994) Inhibition of humankeloid fibroblast growth by isotretinoin and tri-amcinolone acetonide in vitro. Ann. Plast. Surg.33:401–5.
108. Boyadjiev C, Popchristova E, Mazgalova J.(1995) Histomorphologic changes in keloidstreated with Kenacort. J. Trauma. 38:299–302.
109. Robles DT, Berg D. (2007) Abnormal woundhealing: keloids. Clin. Dermatol. 25:26–32.
110. Lawrence WT. (1991) In search of the optimaltreatment of keloids: report of a series and areview of the literature. Ann. Plast. Surg.27:164–78.
111. Boutli-Kasapidou F, Tsakiri A, Anagnostou E,Mourellou O. (2005) Hypertrophic and keloidal
scars: an approach to polytherapy. Int. J. Derma-tol. 44:324–7.
112. Jaros E, Priborsky J, Klein L. (1999) Treatment ofkeloids and hypertrophic scars with cryother-apy [in Czech]. Acta Medica (Hradec Kralove).Suppl. 42:61–3.
113. Yosipovitch G, et al. (2001) A comparison of thecombined effect of cryotherapy and corticos-teroid injections versus corticosteroids andcryotherapy alone on keloids: a controlledstudy. J. Dermatolog. Treat. 12:87–90.
114. Sharpe D. (1997) Of apples and oranges, filedrawers and garbage: why validity issues inmeta-analysis will not go away. Clin. Psychol.Rev. 17:881–901.
115. Rusciani L, Rossi G, Bono R. (1993) Use ofcryotherapy in the treatment of keloids. J. Der-matol. Surg. Oncol. 19:529–34.
116. Zouboulis CC, Blume U, Buttner P, Orfanos CE.(1993) Outcomes of cryosurgery in keloids andhypertrophic scars: a prospective consecutivetrial of case series. Arch. Dermatol. 129:1146–51.
117. Har-Shai Y, Amar M, Sabo E. (2003) Intrale-sional cryotherapy for enhancing the involutionof hypertrophic scars and keloids. Plast. Recon-str. Surg. 111:1841–52.
118. Poochareon VN, Berman B. (2003) New thera-pies for the management of keloids. J. Craniofac.Surg. 14:654–7.
119. Zuber TJ, DeWitt DE. (1994) Earlobe keloids.Am. Fam. Physician. 49:1835–41.
120. Guix B, et al. (2001) Treatment of keloids byhigh-dose-rate brachytherapy: a seven-yearstudy. Int. J. Radiat. Oncol. Biol. Phys. 50:167–72.
121. Ogawa R, Mitsuhashi K, Hyakusoku H,Miyashita T. (2003) Postoperative electron-beamirradiation therapy for keloids and hyper-trophic scars: retrospective study of 147 casesfollowed for more than 18 months. Plast. Recon-str. Surg. 111:547–55.
122. Apfelberg DB, et al. (1984) Preliminary results ofargon and carbon dioxide laser treatment ofkeloid scars. Lasers Surg. Med. 4:283–90.
123. Alster TS, Handrick C. (2000) Laser treatment ofhypertrophic scars, keloids, and striae. Semin.Cutan. Med. Surg. 19:287–92.
124. Tanzi EL, Alster TS. (2004) Laser treatment ofscars. Skin Therapy Lett. 9:4–7.
125. Alster T. (2003) Laser scar revision: comparisonstudy of 585-nm pulsed dye laser with andwithout intralesional corticosteroids. Dermatol.Surg. 29:25–9.
126. Alster TS, Williams CM. (1995) Treatment ofkeloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet. 345:1198–200.
127. Dierickx C, Goldman MP, Fitzpatrick RE. (1995)Laser treatment of erythematous/hypertrophicand pigmented scars in 26 patients. Plast. Recon-str. Surg. 95:84–92.
128. Chan HH, et al. (2004) The use of pulsed dyelaser for the prevention and treatment of hyper-trophic scars in Chinese persons. Dermatol.Surg. 30:987–94.
129. Fiskerstrand EJ, Svaasand LO, Volden G. (1998)Pigmentary changes after pulsed dye lasertreatment in 125 northern European patientswith port wine stains. Br. J. Dermatol. 138:477–9.
130. Hermanns JF, Petit L, Hermanns-Le T, PierardGE. (2001) Analytic quantification of phototype-related regional skin complexion. Skin. Res.Technol. 7:168–71.
131. Jimenez SA, Freundlich B, Rosenbloom J. (1984)Selective inhibition of human diploid fibroblastcollagen synthesis by interferons. J. Clin. Invest.74:1112–6.
132. Berman B, Duncan MR. (1989) Short-termkeloid treatment in vivo with human interferonalfa-2b results in a selective and persistent nor-malization of keloidal fibroblast collagen, gly-cosaminoglycan, and collagenase production invitro. J. Am. Acad. Dermatol. 21:694–702.
133. Tredget EE, et al. (1998) Transforming growth fac-tor-beta in thermally injured patients with hyper-trophic scars: effects of interferon alpha-2b. Plast.Reconstr. Surg. 102:1317–28; discussion 1329–30.
134. Tredget EE, et al. (1998) Transforming growthfactor-beta in thermally injured patients withhypertrophic scars: effects of interferon alpha-2b. Plast. Reconstr. Surg. 102:1317–30.
135. Espana A, Solano T, Quintanilla E. (2001)Bleomycin in the treatment of keloids and hy-pertrophic scars by multiple needle punctures.Dermatol. Surg. 27:23–7.
136. Bodokh I, Brun P. (1996) Treatment of keloidwith intralesional bleomycin [in French]. Ann.Dermatol. Venereol. 123:791–4.
137. Naeini FF, Najafian J, Ahmadpour K. (2006)Bleomycin tattooing as a promising therapeuticmodality in large keloids and hypertrophicscars. Dermatol. Surg. 32:1023–30.
138. Saray Y, Gulec AT. (2005) Treatment of keloidsand hypertrophic scars with dermojet injectionsof bleomycin: a preliminary study. Int. J. Derma-tol. 44:777–84.
139. Apikian M, Goodman G. (2004) Intralesional 5-fluorouracil in the treatment of keloid scars.Australas. J. Dermatol. 45:140–3.
140. Fitzpatrick RE. (1999) Treatment of inflamed hy-pertrophic scars using intralesional 5-FU. Der-matol. Surg. 25:224–32.
141. Nanda S, Reddy BS. (2004) Intralesional 5-fluo-rouracil as a treatment modality of keloids. Der-matol. Surg. 30:54–7.
R E V I E W A R T I C L E
M O L M E D 1 7 ( 1 - 2 ) 1 1 3 - 1 2 5 , J A N U A R Y - F E B R U A R Y 2 0 1 1 | G A U G L I T Z E T A L . | 1 2 5
Related Documents