Original Article Cortical folding difference between patients with early-onset and patients with intermediate-onset bipolar disorder Recent epidemiologic studies have modelled the distribution of age at onset in bipolar disorder (BD), with the aim of defining genetically more homogeneous subtypes of the illness [1, 2; see also Penttila¨ J, Cachia A, Martinot J-L, Ringuenet D, Wessa M, Houenou J, Galinowski A, Bellivier F, Gallarda T, Duchesnay E, Artiges E, Leboyer M, Olie´ J-P, Mangin J-F, Paille`re-Martinot M-L. Cortical folding difference between patients with early-onset and patients with intermediate-onset bipolar disorder. Bipolar Disord 2009: 11: 361–370. ª 2009 The Authors. Journal compilation ª 2009 Blackwell Munksgaard. Objectives: Cerebral abnormalities have been detected in patients with bipolar disorder (BD). In comparison to BD with a later onset, early- onset BD has been found to have a poorer outcome. However, it is yet unknown whether neuroanatomical abnormalities differ between age- at-onset subgroups of the illness. We searched for cortical folding differences between early-onset (before 25 years) and intermediate-onset (between 25 and 45 years) BD patients. Methods: Magnetic resonance images of 22 early-onset BD patients, 14 intermediate-onset BD patients, and 50 healthy participants were analyzed using a fully automated method to extract, label, and measure the sulcal area in the whole cortex. Cortical folding was assessed by computing global sulcal indices (the ratio between total sulcal area and total outer cortex area) for each hemisphere, and local sulcal indices for 12 predefined regions in both hemispheres. Results: Intermediate-onset BD patients had a significantly reduced local sulcal index in the right dorsolateral prefrontal cortex in comparison to both early-onset BD patients and healthy subjects, and lower global sulcal indices in both hemispheres in comparison to healthy subjects (p < 0.05, Bonferroni corrected). Brain tissue volumes did not differ between groups. Conclusions: This study provided the first evidence of a neuroanatomic difference between intermediate-onset and early-onset BD, which lends further support to the existence of different age-at-onset subgroups of BD. Jani Penttila ¨ a–d , Arnaud Cachia a–d , Jean-Luc Martinot a–d , Damien Ringuenet a–e , Miche ` le Wessa a–d,f , Josselin Houenou g,h , Andre ´ Galinowski i,j , Frank Bellivier g,h , Thierry Gallarda i,j , Edouard Duchesnay a–d,k , Eric Artiges a–d , Marion Leboyer g,h , Jean-Pierre Olie ´ i,j , Jean-Franc ¸ ois Mangin a–d,k and Marie-Laure Paille ` re-Martinot a–d,I a INSERM, U797 Research Unit Neuroimaging and Psychiatry, b CEA, U797 Research Unit Neuroimaging and Psychiatry, Hospital Department Fre ´de ´ ric Joliot and Neurospin, c Universite ´ Paris Sud, Orsay, d Universite ´ Paris Descartes, Paris, e AP-HP, Department of Psychiatry and Addictology, Paul Brousse Hospital, Villejuif, France, f Department of Cognitive and Clinical Neuroscience, University of Heidelberg, Central Institute of Mental Health, Mannheim, Germany, g AP-HP, Department of Psychiatry, Chenevier-Mondor Hospital, Cre ´ teil, h INSERM, U995, IMRB, Genetics Department, Universite ´ Paris 12, Cre ´teil, i INSERM, Physiopathologie des Maladies Psychiatriques, U894-7, Paris, j Universite ´ Paris Descartes, SHU, Department of Psychiatry, Sainte Anne Hospital, Paris, k LNAO, NeuroSpin I 2 BM, Saclay, l AP-HP, Department of Adolescent Medicine, Maison de Solenn, Cochin Hospital, Paris, France Key words: bipolar disorder – magnetic resonance imaging – neurodevelopment – neuroimaging Received 22 July 2008, revised and accepted for publication 27 October 2008 Corresponding author: Jani Penttila ¨, M.D., Ph.D. Adolescent Psychiatry Unit, Pa ¨ija ¨t-Ha ¨me Central Hospital, Vapaudenkatu 6 (5th floor), F1-15110, Lahti, Finland Fax: +358 3 819 2630 e-mail: japepe@utu.fi The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manu- script. Bipolar Disorders 2009: 11: 361–370 ª 2009 The Authors Journal compilation ª 2009 Blackwell Munksgaard BIPOLAR DISORDERS 361

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Original Article
Cortical folding difference between patientswith early-onset and patients withintermediate-onset bipolar disorder
Recent epidemiologic studies have modelled thedistribution of age at onset in bipolar disorder(BD), with the aim of defining genetically morehomogeneous subtypes of the illness [1, 2; see also
Penttila J, Cachia A, Martinot J-L, Ringuenet D, Wessa M, Houenou J,Galinowski A, Bellivier F, Gallarda T, Duchesnay E, Artiges E, LeboyerM, Olie J-P, Mangin J-F, Paillere-Martinot M-L. Cortical foldingdifference between patients with early-onset and patients withintermediate-onset bipolar disorder.Bipolar Disord 2009: 11: 361–370. ª 2009 The Authors.Journal compilation ª 2009 Blackwell Munksgaard.
Objectives: Cerebral abnormalities have been detected in patients withbipolar disorder (BD). In comparison to BD with a later onset, early-onset BD has been found to have a poorer outcome. However, it is yetunknown whether neuroanatomical abnormalities differ between age-at-onset subgroups of the illness. We searched for cortical foldingdifferences between early-onset (before 25 years) and intermediate-onset(between 25 and 45 years) BD patients.
Methods: Magnetic resonance images of 22 early-onset BD patients, 14intermediate-onset BD patients, and 50 healthy participants wereanalyzed using a fully automated method to extract, label, and measurethe sulcal area in the whole cortex. Cortical folding was assessed bycomputing global sulcal indices (the ratio between total sulcal area andtotal outer cortex area) for each hemisphere, and local sulcal indices for12 predefined regions in both hemispheres.
Results: Intermediate-onset BD patients had a significantly reducedlocal sulcal index in the right dorsolateral prefrontal cortex incomparison to both early-onset BD patients and healthy subjects, andlower global sulcal indices in both hemispheres in comparison to healthysubjects (p < 0.05, Bonferroni corrected). Brain tissue volumes did notdiffer between groups.
Conclusions: This study provided the first evidence of a neuroanatomicdifference between intermediate-onset and early-onset BD, which lendsfurther support to the existence of different age-at-onset subgroups ofBD.
Jani Penttilaa–d, Arnaud Cachiaa–d,Jean-Luc Martinota–d, DamienRingueneta–e, Michele Wessaa–d,f,Josselin Houenoug,h, AndreGalinowskii,j, Frank Bellivierg,h,Thierry Gallardai,j, EdouardDuchesnaya–d,k, Eric Artigesa–d,Marion Leboyerg,h, Jean-PierreOliei,j, Jean-Francois Mangina–d,k andMarie-Laure Paillere-Martinota–d,I
aINSERM, U797 Research Unit Neuroimaging and
Psychiatry, bCEA, U797 Research Unit
Neuroimaging and Psychiatry, Hospital Department
Frederic Joliot and Neurospin, cUniversite Paris Sud,
Orsay, dUniversite Paris Descartes, Paris, eAP-HP,
Department of Psychiatry and Addictology, Paul
Brousse Hospital, Villejuif, France, fDepartment of
Cognitive and Clinical Neuroscience, University of
Heidelberg, Central Institute of Mental Health,
Mannheim, Germany, gAP-HP, Department of
Psychiatry, Chenevier-Mondor Hospital, Creteil,hINSERM, U995, IMRB, Genetics Department,
Universite Paris 12, Creteil, iINSERM,
Physiopathologie des Maladies Psychiatriques,
U894-7, Paris, jUniversite Paris Descartes, SHU,
Department of Psychiatry, Sainte Anne Hospital,
Paris, kLNAO, NeuroSpin I2BM, Saclay, lAP-HP,
Department of Adolescent Medicine, Maison de
Solenn, Cochin Hospital, Paris, France
Key words: bipolar disorder – magnetic resonance
imaging – neurodevelopment – neuroimaging
Received 22 July 2008, revised and accepted for
publication 27 October 2008
Corresponding author:
Jani Penttila, M.D., Ph.D.
Adolescent Psychiatry Unit, Paijat-Hame Central
Hospital, Vapaudenkatu 6 (5th floor), F1-15110,
Lahti, Finland
Fax: +358 3 819 2630
e-mail: [email protected]
The authors of this paper do not have any commercial associations
that might pose a conflict of interest in connection with this manu-
script.
Bipolar Disorders 2009: 11: 361–370ª 2009 The Authors
Journal compilation ª 2009 Blackwell Munksgaard
BIPOLAR DISORDERS
361
review by Leboyer et al. (3)]. In BD, age-at-onsetdistribution seems to consist of a mixture ofthree (partially overlapping) Gaussian distribu-tions, which suggests the existence of three BDsubgroups, based on age at onset (1, 2).The most commonly used definition for early-
onset BD is the beginning of clinical illness beforethe age of 25 years (1, 2, 4–7). The peak occurrenceof early-onset BD has been estimated to be around17 years (1, 2). Patients whose illness manifestsafter the age of 45 years are considered to have alate-onset form of BD (1, 2, 8). In between theseearly- and late-onset groups, there appears to be athird group, which Bellivier et al. (1, 2) havenamed the intermediate-onset group.The age-at-onset subgroups of BD have been
proposed to differ from each other with respect togenetic vulnerability factors and transmission of thedisease in families (1, 2, 5). An early onset has beenconsidered to involve a poorer outcome (9, 10) anda marked psychosocial component (11), whereasorganic factors might be more important in BDwith a later onset (12). However, it is still unknownwhether neuroanatomical abnormalities differbetween these age-at-onset subgroups of BD (3).Brain imaging studies have demonstrated BD-
associated alterations in the brain cortex structure,especially in frontal regions (13–17). Some of thesealterations may be neurodevelopmental (14), whileothers appear to develop with repeated affectiveepisodes (15). In adult-onset BD, both increased(16) and decreased (17) prefrontal cortex volumeshave been reported. In contrast, Chang et al. (18)detected no gray or white matter alterations inchildren and adolescents with BD, which gave riseto a proposition that pediatric BD might beneurobiologically distinct from adult-onset BD.In the human brain, the mature sulco-gyral
pattern is considered to result from fetal andchildhood processes that have shaped the cortexanatomy from a smooth lissencephalic structure toa highly convoluted surface (19–21). Systematicchanges in cortical folding patterns may arise fromneurodevelopmental factors, which, in turn, arethought to play an important role in the patho-genesis of bipolar illness (22). As an example,Fornito et al. (14) have recently demonstrated anearly neurodevelopmental anomaly of the anteriorcingulate cortex in patients with BD.In the current study, we aimed to find out
whether there is a link between cortical foldingsurface and the age at onset in BD patients.Therefore, we analyzed global and regional corticalfolding surfaces in early-onset (before 25 years)and intermediate-onset (between 25 and 45 years)BD patients, and in healthy participants.
Patients and methods
Participants
Thirty-six patients were recruited from consecutiveadmissions at psychiatric units of university hos-pitals in the Paris, France area. Their diagnoses(DSM-IV) (23) were established by experiencedsenior psychiatrists, using the Mini-InternationalNeuropsychiatric Interview (24). Age at onset wasdefined as the age at which the patient first met theDSM-IV criteria for a thymic episode. Age at onsetwas assessed by the interviewer and then blindlyrated by an independent psychiatrist according tomedical case notes and the Diagnostic Interviewfor Genetic Studies (25). Some of the patients alsoparticipated in a functional magnetic resonanceimaging (MRI) study, the results of which arereported elsewhere (26).Two patient subgroups were defined: the early-
onset group (onset before 25 years; n = 22) andthe intermediate-onset group (onset between 25 and45 years; n = 14). The cutoff point of 25 yearsbetween these two subgroups was based on previ-ous studies (1, 2, 4–7). The subgroups were verysimilar with respect to the sex ratio, age, handed-ness, and current and preceding mood state(s) (seeTable 1).Mood-stabilizing agents were prescribed for 10
early-onset patients (45%) and for 12 intermediate-onset patients (86%) (v2 = 5.8, p = 0.02). In theearly-onset group, 5 patients were treated withlithium (mean dose 1100 mg ⁄day), 3 with valpro-ate (mean dose 1500 mg ⁄day), 3 with carbamaze-pine, 1 with oxcarbazepine, and 1 with topiramate.In the intermediate-onset group, 6 patients weretreated with lithium (mean dose 850 mg ⁄day), 6with valproate (mean dose 1142 mg ⁄day), 1 withcarbamazepine, and 1 with lamotrigine.Antidepressants were prescribed to 8 early-onset
patients (36%) and to 5 intermediate-onset patients(36%) (v2 = 0.002, p = 0.97). In the early-onsetgroup, 2 patients were treated with citalopram(10 mg ⁄day), 1 with escitalopram (20 mg ⁄day), 1with paroxetine (20 mg ⁄day), and 4 with venlafax-ine (mean dose 188 mg ⁄day). In the intermediate-onset group, 1 patient was treated with citalopram(40 mg ⁄day) and clomipramine (225 mg ⁄day)combination, 1 with citalopram alone (60 mg ⁄day),1 with sertraline (50 mg ⁄day), 1 with venlafaxine(225 mg ⁄day), and 1 with mianserine (30 mg ⁄day).Antipsychotic medications were prescribed to 7
early-onset patients (32%) and to 4 intermediate-onset patients (29%) (v2 = 0.04, p = 0.84). In theearly-onset group, 1 patient was treated with acombination of aripiprazole (10 mg ⁄day), cloza-pine (300 mg ⁄day), and amisulpride (150 mg ⁄day),
Penttila et al.
362
2 with olanzapine (2.5 mg ⁄day), 1 with risperidone(1 mg ⁄day), 1 with cyamemazine (100 mg ⁄day),and 2 with levomepromazine (20 and 50 mg ⁄day).In the intermediate-onset group, 2 patients weretreated with olanzapine (10 mg ⁄day), 1 with ris-peridone (3 mg ⁄day), and 1 with levomepromazine(50 mg ⁄day).Seven early-onset patients and two intermediate-
onset patients received no psychotropic medica-tions. At the time of the study, the patients wereeither euthymic or depressed; no manic or hypo-manic patients were enrolled. Exclusion criteriawere electroconvulsive therapy during the past sixmonths, alcohol or substance dependence ⁄abuse,any serious medical condition, or history ofneurological disorders.The comparison group comprised 50 healthy
volunteers who were recruited by word of mouth.They had no personal history of psychiatric orneurological disorder, confirmed by a medicalexamination. The healthy subjects did not statisti-cally significantly differ from patients with respectto sex ratio, age, or handedness (see Table 1 andStatistical analyses). The study was carried out inaccordance with the Declaration of Helsinki. Theprotocol was approved by the local ethics commit-tee, and, after complete description of the studies,each subject gave a written informed consent.
Image acquisition and analysis
All three-dimensional (3D) high-resolution ana-tomical images were acquired with the same 1.5Tesla General Electric Signa System scanner (GEMedical Systems, Milwaukee, WI, USA) and thesame 3D T1-weighted fast spoiled gradient-echosequence [124 contiguous slices of 1.3-mm thick-ness, field of view 24 · 24 cm, matrix 256 · 256,
voxel size: 0.94 · 0.94 · 1.3 mm; echo time(TE) = 2.2 ms, inversion time (TI) = 600 ms,repetition time (TR) = 12.5 ms, two excitations].In order to assess both overall (global) and local
cortex gyrification, the raw MRI data were sub-jected to automatized estimation of sulcus areas(27) by means of a three-step procedure. The 3Dsurface-based sulcal indices (see below) can accu-rately capture the complex shapes of the corticalfolds and they are independent of the brainorientation and the direction of slicing (27–29).This method has recently revealed sulcus abnor-malities in schizophrenia patients (28, 29).Briefly, gray matter (GM), white matter (WM),
and cerebrospinal fluid (CSF) were segmented andtheir hemispheric volumes were calculated fromnon-normalized raw MRI data, using a fullyautomatic procedure (27). The raw MRI data werethen subjected to automatized 3D cortical foldsegmentation (27). No spatial normalization wasapplied, to overcome potential bias due to thesulcus shape deformations induced by the warpingprocess (30). Cortical folds were automaticallysegmented throughout the cortex from the skeletonof the GM ⁄CSF mask, and converted to a graph-based representation of the cortex, containinginformation related to morphology (area, depth,and length) and spatial organization (relativeposition, relative orientation) (27) (see Fig. 1A).An automatic recognition algorithm labelled eachcortical fold (31).Global sulcal index (g-SI) for each hemisphere
was measured as the ratio between the total sulcalarea (sum of the areas of all segmented corticalfolds) and the outer cortex area. Hemispheric outercortex area was defined as the area of a smoothenvelope of the brain mask that wrapped aroundthe hemisphere but did not encroach into sulci.
Table 1. Demographic and clinical characteristics of the study subjects
Characteristic ⁄ sulcal indexEarly-onset bipolarpatients (n = 22)
Intermediate-onsetbipolar patients (n = 14)
Healthy subjects(n = 50)
Groupdifference
Sex ratio (male ⁄ female) 11 ⁄ 11 8 ⁄ 6 25 ⁄ 25 p = 0.89Age (years) 48 (8) 51 (7) 49 (8) p = 0.58Handedness (% right) 82% 93% 94% p = 0.11Age at illness onset (years) 19 (3), range [14–24] 36 (5), range [30–43] – p < 0.001Duration of illness (years) 30 (8) 15 (8) – p < 0.001Number of major depressive episodes 4.4 (2.1) 3.4 (2.0) – p = 0.19Number of manic episodes 2.0 (1.9) 2.0 (2.9) – p = 0.95Time since last affective episode (years) 2.5 (4.5) 3.0 (6.8) – p = 0.64Current mood state (euthymica ⁄ depressed) 13 ⁄ 9 7 ⁄ 7 – p = 0.5921-item HAM-D score 10.1 (10.7), range [0–31] 14.4 (12.8), range [0–31] – p = 0.28
Data are presented as means (SD), except for the sex ratio, handedness, mood state, and treatments. Between-group differences indemographic and clinical data were evaluated using chi-square test (sex ratio, handedness, mood state), analysis of variance (age),Wilcoxon�s test (time since last affective episode) and Student�s t-test (other clinical data).aEuthymia was defined by a 21-item Hamilton Depression Rating Scale (HAM-D) score £ 5.
Cortical folding in bipolar disorder
363
This envelope was obtained with a morphologicclosing of the brain mask (27, 32); an isotropicclosing of 5 mm was used to ensure the boundarysmoothness. The g-SI reflects the burying of thecortex (28), but it does not directly measure sulcalopening or cortical thickness as the standardgyrification index does (33, 34). A high g-SI valuedenotes highly convoluted sulci, while a low g-SIindicates a lower degree of sulcation.
Local sulcal indices (l-SIs) were computed for thesulci pooled within 12 predefined regions in eachhemisphere: dorsolateral prefrontal cortex, precen-tral cortex, medial frontal cortex, Sylvian fissure,insula, lateral temporal cortex, medial temporalcortex, parietal cortex, intraparietal sulcus, medialparieto-occipital cortex, occipital cortex, and cal-carine complex (35). The l-SI was defined as theratio between the sum of areas of the labelled sulciin the corresponding region and the total outercortex area in that hemisphere. Thus, the sum of allthe 12 l-SIs in each hemisphere is equal to the g-SIof that hemisphere.All the image processing steps were visually
checked and no gross segmentation or sulcuslabelling error was detected. Some minor segmen-tation errors (poorly defined margin between occip-ital lobes and cerebellum) were corrected manually.Automated brain segmentations and manual
corrections were performed with Brainvisa 3.1 soft-ware (freely available online at http://brainvisa.info).
Statistical analyses
Between-group differences in demographic andclinical factors were evaluated using chi-squaretest (sex ratio, handedness, mood state), analysis ofvariance (age), and Student�s t-test (other clinicalvariables). Differences in �time since last affectiveepisode� were assessed with Wilcoxon�s test as thedata were not normally distributed due to thepresence of currently depressed patients with a zerovalue (Table 1).Between-group differences in brain tissue vol-
umes and sulcal indices were assessed usingunivariate multiple regression analyses within theframework of the linear model, with group and sexas factors and age as a numeric covariate, to takeinto account the possible influence of sex and ageon cortical folding (36–39). Normal distributionassumption underlying the linear model approachwas verified by testing the normality of the linearmodel residuals (Shapiro test). When a significantmain effect of group was detected, analysis wascontinued by post hoc paired comparisons usingTukey�s HSD test with Bonferroni correction.Statistical significance was probed with F-tests inthe linear model and with t-tests in the paired posthoc analyses. In brain tissue and g-SI analyses, atwo-sided p-value < 0.05 was considered statis-tically significant. For the l-SI analyses of the12 predefined regions in each hemisphere, weperformed Bonferroni correction for multiplecomparisons, and two-tailed a level was set at0.002 (i.e., 0.05 ⁄24).
A
B
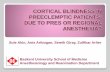
Fig. 1. (A) Sulcal morphometry method. Three-dimensionalreconstruction of a healthy subject�s right hemisphere, wherethe cortical folds (prefrontal sulci in red, other sulci in blue) areshown on a background of white matter mesh. For illustrativepurposes, gray matter ribbon has been removed. In this sub-ject, the global sulcal index (g-SI) for the right hemisphere was1.591 and the local sulcal index (l-SI) for the right dorsolateralprefrontal cortex was 0.197. (B) Local sulcal indices (l-SIs) inthe right dorsolateral prefrontal cortex in patients with early-onset or intermediate-onset bipolar disorder and in healthycomparison subjects. Circles indicate individual values andhorizontal lines indicate the averages of these raw l-SI values ineach group.
Penttila et al.
364
Among patients (n = 36), we searched forpossible drug effects by adding the type of medi-cation (mood stabilizers, antipsychotics, anti-depressants, one at a time) as a factor in thelinear models, parallel with group, sex, and age. Inaddition, we computed the Pearson�s correlationcoefficient (r) between illness duration and sulcalindices.All the statistical analyses were carried out with
R 2.5 software (http://www.r-project.org), usingdedicated libraries (�car�, �effects�, and �multtest�)for the analysis of linear models with unbalanceddesign (40).
Results
The subject groups did not significantly differ fromeach other with respect to hemispheric brain tissuevolumes, even at a lower statistical threshold(p < 0.10) (Table 2).The analyses of hemispheric g-SI revealed sta-
tistically significant main group effects in left andright hemispheres (Table 3). In the post hocanalyses, patients with intermediate-onset BDshowed 5% smaller g-SI in the left hemisphere(t = )2.7, p = 0.02) and 7% smaller g-SI in theright hemisphere (t = )4.1, p < 0.001) in com-parison to healthy subjects, and 5% smaller g-SI inthe right hemisphere (t = )2.8, p = 0.02) incomparison to patients with early-onset BD.In the l-SI analyses of the 12 predefined regions
in each hemisphere, the only between-group dif-ference that was statistically significant after Bon-ferroni correction was detected in the rightdorsolateral prefrontal cortex (Table 4 andFig. 1B). In that region, the l-SI in patients withintermediate-onset BD was 16% lower than inearly-onset BD (t = )3.8, p < 0.001), and 12%
lower than in healthy subjects (t = )3.2,p = 0.006).In addition, nonsignificant group effects (uncor-
rected p < 0.05) were observed in the right medialtemporal cortex and in the right calcarine complex(Table 4). Paired post hoc comparisons showed areduced right medial temporal cortex l-SI inpatients with intermediate-onset BD, in compari-son to patients with early-onset BD ()21%,t = )2.6, p = 0.03) and to healthy subjects()20%, t = )2.8, p = 0.02). In the right calcarinecomplex, l-SI was decreased in patients with early-onset BD, in comparison to healthy subjects()30%, t = )3.1, p = 0.008).Among patients, the use of mood stabilizers,
antipsychotics, or antidepressants had no signifi-cant effect on g-SIs (p > 0.29) or dorsolateralprefrontal cortex l-SIs (p > 0.48). We found nosignificant correlation between the duration ofillness and g-SIs or dorsolateral prefrontal cortexl-SIs (r values ranged from)0.03 to 0.18, p > 0.29).
Discussion
Patients with intermediate-onset BD had adecreased global cortical folding surface (g-SI) inboth hemispheres in comparison to healthy subjects.In addition, a reduced local folding surface (l-SI) inthe right dorsolateral prefrontal cortex differen-tiated intermediate-onset BD from early-onset BD.No difference in global brain tissue volumes wasdetected between early-onset BD patients, interme-diate-onset BD patients, and healthy subjects.Several mechanisms may account for these
BD-associated alterations in cortical foldingsurface. According to the mechanic theory ofmorphogenesis, the cortical folding process whichultimately produces the mature sulco-gyral pattern
Table 2. Brain tissue volumes
VolumeEarly-onset bipolarpatients (n = 22)
Intermediate-onsetbipolar patients(n = 14)
Healthy subjects(n = 50)
Groupdifference
Total intracranial volume (cm3)
Left hemisphere 608 (47) 593 (47) 591 (47) p = 0.36Right hemisphere 608 (45) 594 (46) 590 (46) p = 0.31
Gray matter volume (cm3)
Left hemisphere 245 (23) 234 (23) 242 (23) p = 0.35Right hemisphere 244 (23) 232 (23) 241 (24) p = 0.30
White matter volume (cm3)
Left hemisphere 241 (28) 231 (28) 231 (28) p = 0.37Right hemisphere 240 (27) 231 (27) 230 (27) p = 0.34
Cerebrospinal fluid volume (cm3)
Left hemisphere 122 (21) 128 (21) 119 (22) p = 0.37Right hemisphere 123 (20) 131 (20) 120 (20) p = 0.17
Data are presented as means (SD), which are linearly adjusted on age and sex.
Cortical folding in bipolar disorder
365
Table 3. Results of global sulcal index analyses
Hemisphere
Global sulcal index (g-SI)
Group difference
Early-onsetbipolar patients(n = 22)
Intermediate-onsetbipolar patients(n = 14) Healthy subjects (n = 50)
Left 1.434 (0.091) 1.377 (0.092) 1.453 (0.091) p = 0.03a
Right 1.459 (0.084) 1.379 (0.085) 1.485 (0.084) p < 0.001b
Data are presented as means (SD), which are linearly adjusted on age and sex. Statistically significant paired post hoc comparisons:aIntermediate-onset bipolar patients versus healthy subjects (p = 0.02).bIntermediate-onset bipolar patients versus healthy subjects (p < 0.001) and early-onset versus intermediate-onset bipolar patients(p = 0.02).
Table 4. Results of local sulcal index analyses
Region
Local sulcal index (l-SI)
Group differenceEarly-onset bipolarpatients (n = 22)
Intermediate-onset bipolarpatients (n = 14)
Healthy subjects(n = 50)
Dorsolateral prefrontal cortex
L 0.178 (0.020) 0.167 (0.020) 0.179 (0.020) p = 0.16R 0.188 (0.023) 0.158 (0.023) 0.180 (0.023) p = 0.001a
Precentral cortexL 0.061 (0.016) 0.060 (0.016) 0.058 (0.016) p = 0.79R 0.069 (0.015) 0.069 (0.015) 0.069 (0.015) p = 0.99
Medial frontal cortexL 0.120 (0.017) 0.122 (0.017) 0.118 (0.017) p = 0.71R 0.128 (0.019) 0.124 (0.019) 0.127 (0.019) p = 0.77
Sylvian fissureL 0.139 (0.023) 0.138 (0.023) 0.149 (0.023) p = 0.12R 0.144 (0.018) 0.142 (0.018) 0.151 (0.018) p = 0.11
InsulaL 0.072 (0.019) 0.062 (0.019) 0.068 (0.019) p = 0.32R 0.065 (0.015) 0.059 (0.015) 0.064 (0.015) p = 0.49
Lateral temporal cortexL 0.178 (0.026) 0.179 (0.027) 0.182 (0.026) p = 0.83R 0.193 (0.028) 0.183 (0.028) 0.184 (0.028) p = 0.43
Medial temporal cortex
L 0.093 (0.028) 0.101 (0.029) 0.103 (0.028) p = 0.40R 0.091 (0.021) 0.072 (0.021) 0.090 (0.021) p = 0.02
Parietal cortexL 0.035 (0.012) 0.034 (0.012) 0.032 (0.012) p = 0.53R 0.028 (0.012) 0.026 (0.012) 0.030 (0.012) p = 0.58
Intraparietal sulcusL 0.130 (0.021) 0.117 (0.021) 0.129 (0.021) p = 0.14R 0.129 (0.024) 0.130 (0.024) 0.133 (0.024) p = 0.76
Medial parieto-occipital cortexL 0.069 (0.016) 0.071 (0.016) 0.074 (0.016) p = 0.50R 0.090 (0.016) 0.080 (0.016) 0.090 (0.016) p = 0.15
Occipital cortexL 0.056 (0.024) 0.054 (0.024) 0.055 (0.024) p = 0.97R 0.071 (0.020) 0.072 (0.020) 0.068 (0.020) p = 0.68
Calcarine complex
L 0.042 (0.015) 0.048 (0.015) 0.049 (0.015) p = 0.17R 0.036 (0.020) 0.045 (0.020) 0.052 (0.020) p = 0.01
Data are presented as means (SD), which are linearly adjusted on age and sex. L = left; R = right.Bold font indicates the regions where (uncorrected) p was less than 0.05 for the main effect of group.aRight dorsolateral prefrontal cortex was the only region where the main effect of group reached statistical significance after Bonferronicorrection for multiple comparisons (two-tailed a was set at 0.002, i.e., 0.05 ⁄ 24).
Penttila et al.
366
is mediated by forces that stem from GM thicknessand WM connectivity (20, 41–43). It has also beensuggested that an increase in the number ofneurons results in surface expansion, rather thanin a thicker cortex (44–46). This mechanism mightbe consistent with our observations of g-SI reduc-tions without statistically significant alterations inhemispheric GM volumes.Based on epidemiological data on age at onset,
Bellivier et al. (1, 2) have divided BD into early-onset, intermediate-onset, and late-onset sub-groups. To our knowledge, our present study isthe first to describe a neuroanatomic differencebetween intermediate-onset and early-onset BD.Separate investigation of these subgroups mayreduce the underlying genetic heterogeneity (3, 47),as each of these subgroups may have specificvulnerability factors (2). Interestingly, it was notthe early-onset but the intermediate-onset BDgroup which showed significant sulcal alterationsin comparison to healthy controls. This finding is,however, in line with the proposed role of organicfactors in BD with a later onset (12, 48). Early-onset BD that begins in adolescence or in earlyadulthood has been suggested to be more depend-ent on psychosocial factors (12, 18), but somestudies have also described early abnormalities inlimbic structures in these patients (49).Localization of the cortical folding alteration to
prefrontal area is consistent with previous studiesthat have demonstrated prefrontal GM and WMdeviations in BD (16, 17, 50). BD-associated WMhyperintensities have been reported especially inthe right fronto-parietal area (50). Patients withBD have also shown abnormal prefrontal activa-tion asymmetry in electroencephalography (51).We also observed a similar trend of l-SI reduc-
tion in intermediate-onset BD in the right medialtemporal cortex. This finding is in line withprevious reports that patients with BD may expe-rience a progressive GM loss in medial temporallobe structures, the hippocampus, and the fusiformgyrus (52, 53).In addition to early developmental factors, later
neurodegenerative processes may also contributeto the pathophysiology of BD (13). From thispoint of view, the reduced sulcal indices in theintermediate-onset BD patients might reflect amore severe form of illness (in fact, these patientshad had a similar number of episodes in 15 years asthe early-onset patients had had in 30 years, cf.Table 1). Nevertheless, we consider it unlikely thatthe sulcal index reductions in intermediate-onsetBD patients could merely be explained by neuro-degeneration, since we found no correlation withBD duration, and the number of affective episodes
and gap between last episode and scanning werevery similar in both groups (Table 1).
Methodological issues
Cortex gyrification was assessed by 3D analysis ofcortical folds, which revealed new findings thatwould have been difficult to detect by mere visualinspection (cf. Fig. 1A) or by using planimetryindices based on a two-dimensional approach (54).A fully automated method is thought to be morereliable and less time consuming than manualanalysis (54), which makes it applicable to largedatabases. Sulcus-based morphometry can provideinformation on cortical surface anatomy in affec-tive disorders, which complements the reporteddeviations in local brain tissue volume (17), corticalthickness (55), and WM connectivity (56). Thedefinition of g-SI and l-SI does not depend onsulcus opening or thickness. In addition, ourmethod is original in using the skeleton of theGM ⁄CSF mask, with the cortical folds corre-sponding to the crevasse bottoms of the �land-scape�, the altitude of which is defined by intensityon MRI (27). This definition is supposed toprovide a stable sulcus localization that is notaffected by variation in the GM ⁄WM contrast dueto, e.g., age-related changes in regional vasculari-sation or intra-cortical myelination (57, 58). More-over, the present g-SIs and l-SIs can be used toinvestigate both hemispheric and local gyrification,while the previous indices were limited to MRIslices.It is possible that slight between-group differ-
ences in brain tissue volumes may have remainedundetected in this study because of statistical powerissues (n = 14 in the intermediate-onset group). Incomparison to hemispheric volume measurements,g-SI may be more sensitive in detecting subtlecortical alterations. As described in the statisticalmethods, the unbalanced design (i.e., the unequalnumber of participants in the three subject groups)was taken into account in the estimation of thelinear model parameters, and thus it is notsupposed to have biased the analyses (40).
Limitations
Gender (36, 38) and age (37, 39) have beenreported to have an effect on sulcal anatomy.Thus, we matched the study subject groups withrespect to age and sex ratio, and we used age andsex as covariates in the statistical analyses, tominimize these effects. Therefore, it is assumed thatage and sex should not have any marked influenceson the main findings.
Cortical folding in bipolar disorder
367
Due to the cross-sectional design of this study,the sulcal index changes cannot be ascribed specif-ically to developmental factors or to tissue loss.In addition, previous brain imaging studies haveshown that lithium (59, 60) and valproate (61) mayproduce measurable increases in regional GMvolumes, which may reflect a neurotrophic effect.If the reduced sulcal indices in the intermediate-onset BD patients were caused by illness-associatedneurodegeneration (13), then the lack of sulcalindex reductions in the early-onset group couldpossibly be explained by a longer duration ofillness and, correspondingly, a longer duration ofmood-stabilizing treatments and their neurotroph-ic effects, which may have counteracted neuro-degenerative processes in this group. However, thisexplanation is unlikely, because the proportion ofpatients receiving mood-stabilizing medicationswas twice as high as in the intermediate-onsetgroup (86% versus 45%).The late-onset form of BD in particular has been
associated with WM hyperintensities (62). Accord-ing to Gulseren et al. (50), these hyperintensitiesmay be particularly frequent in the right fronto-parietal area. However, as we did not acquirefluid-attenuated inversion recovery MRIs fromour subjects, we cannot further evaluate thepossible role of WM hyperintensities behind thereduced right dorsolateral prefrontal cortex l-SI inintermediate-onset BD.The brain abnormalities that we detected in the
intermediate-onset BD subgroup could be relatedto the apparent greater severity of the clinicalcourse in these patients, since they had twice asmany episodes as the patients in the early-onsetgroup. It could be speculated that within theintermediate-onset group, some patients mightpresent with a more severe form of the disease.Indeed, as a complementary analysis, we found anegative association (t = )2.2, p = 0.03) betweenthe right dorsolateral prefrontal cortex l-SI and theepisode frequency (total number of manic ordepressive episodes divided by illness duration)using a linear model with episode frequency andage as numeric covariates and gender as factor.
Conclusions
Even though there is no consensus of the interpre-tation of sulcal deviations, our results provide thefirst evidence of a neuroanatomic differencebetween intermediate-onset and early-onset BD,which lends further support to the existence ofdifferent subgroups of BD. The finding thatpatients with intermediate-onset (instead of early-onset) BD showed reduced sulcal indices is in line
with the presumed role of organic factors in BDwith a later onset.
Acknowledgements
This study was supported in part by grants from the FrenchNational Agency for Research (ANP Neurosciences 2005;Psymarker project) and from the Programme Hospitalier deRecherche Clinique, Delegation a la Recherche Clinique del�Assistance Publique-Hopitaux de Paris and the HealthMinistry of France (PHRC ⁄AOM-98099). JP received per-sonal grants from the Finnish Cultural Foundation and theSigrid Juselius Foundation, Finland. AC received post-doc-toral grants from the INSERM. DR was supported by theFondation pour la Recherche Medicale and by the AtomicEnergy Commission of France. MW was supported by a grantfrom the Deutsche Forschungsgemeinschaft, Germany(We3638 ⁄ 1-1). JH was supported by a grant from the FrenchNational Academy of Medicine. MLPM was supported byan APHP-INSERM interface grant and an INSERM-PROGRESS grant.We acknowledge Dr. Pascale Bruguiere for her support.
References
1. Bellivier F, Golmard JL, Henry C, Leboyer M, SchurhoffF. Admixture analysis of age at onset in bipolar I affectivedisorder. Arch Gen Psychiatry 2001; 58: 510–512.
2. Bellivier F, Golmard JL, Rietschel M et al. Age at onset inbipolar I affective disorder: further evidence for threesubgroups. Am J Psychiatry 2003; 160: 999–1001.
3. Leboyer M, Henry C, Paillere-Martinot ML, Bellivier F.Age at onset in bipolar affective disorders: a review.Bipolar Disord 2005; 7: 111–118.
4. Fujiwara Y, Honda T, Tanaka Y, Aoki S, Kuroda S.Comparison of early- and late-onset rapid cycling affectivedisorders: clinical course and response to pharmacother-apy. J Clin Psychopharmacol 1998; 18: 282–288.
5. Grigoroiu-Serbanescu M, Martinez M, Nothen MM et al.Different familial transmission patterns in bipolar I disor-der with onset before and after age 25. Am J Med Genet2001; 105: 765–773.
6. Somanath CP, Jain S, Reddy YC. A family study ofearly-onset bipolar I disorder. J Affect Disord 2002; 70:91–94.
7. Kiejna A, Rymaszewska J, Hadrys T, Suwalska A, LojkoD, Rybakowski JK. Bipolar or unipolar? – the question forclinicians and researchers. J Affect Disord 2006; 93: 177–183.
8. Carlson GA, Davenport YB, Jamison K. A comparison ofoutcome in adolescent- and later-onset bipolar manic-depressive illness. Am J Psychiatry 1977; 134: 919–922.
9. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ,Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescentbipolar disorder phenotype. Am J Psychiatry 2002; 159:927–933.
10. Birmaher B, Axelson D, Strober M et al. Clinical course ofchildren and adolescents with bipolar spectrum disorders.Arch Gen Psychiatry 2006; 63: 175–183.
11. Post RM, Leverich GS. The role of psychosocial stress inthe onset and progression of bipolar disorder and itscomorbidities: the need for earlier and alternative modes oftherapeutic intervention. Dev Psychopathol 2006; 18:1181–1211.
Penttila et al.
368
12. Hays JC, Krishnan KR, George LK, Blazer DG. Age offirst onset of bipolar disorder: demographic, family history,and psychosocial correlates. Depress Anxiety 1998; 7: 76–82.
13. Monkul ES, Malhi GS, Soares JC. Anatomical MRIabnormalities in bipolar disorder: do they exist and do theyprogress? Aust N Z J Psychiatry 2005; 39: 222–226.
14. Fornito A, Malhi GS, Lagopoulos J et al. In vivo evidencefor early neurodevelopmental anomaly of the anteriorcingulate cortex in bipolar disorder. Acta Psychiatr Scand2007; 116: 467–472.
15. Strakowski SM, Delbello MP, Adler CM. The functionalneuroanatomy of bipolar disorder: a review of neuro-imaging findings. Mol Psychiatry 2005; 10: 105–116.
16. Adler CM, Levine AD, DelBello MP, Strakowski SM.Changes in gray matter volume in patients with bipolardisorder. Biol Psychiatry 2005; 58: 151–157.
17. Lopez-Larson MP, DelBello MP, Zimmerman ME, Schw-iers ML, Strakowski SM. Regional prefrontal gray andwhite matter abnormalities in bipolar disorder. BiolPsychiatry 2002; 52: 93–100.
18. Chang K, Barnea-Goraly N, Karchemskiy A et al. Corti-cal magnetic resonance imaging findings in familial pedi-atric bipolar disorder. Biol Psychiatry 2005; 58: 197–203.
19. Dubois J, Benders M, Cachia A et al. Mapping the earlycortical folding process in the preterm newborn brain.Cereb Cortex 2007; 12: 12.
20. Van Essen DC. A tension-based theory of morphogenesisand compact wiring in the central nervous system. Nature1997; 385: 313–318.
21. Welker W. Why does cerebral cortex fissure and fold?Cereb Cortex 1988; 8B: 3–135.
22. Sanches M, Keshavan MS, Brambilla P, Soares JC.Neurodevelopmental basis of bipolar disorder: a criticalappraisal. Prog Neuropsychopharmacol Biol Psychiatry2008; 7: 7.
23. American Psychiatric Association. Diagnostic and Statis-tical Manual of Mental Disorders, Fourth Edition. Wash-ington, DC: American Psychiatric Association; 1994.
24. Lecrubier Y, Sheehan D, Weiller E et al. The MiniInternational Neuropsychiatric Interview (MINI). Ashort diagnostic structured interview: reliability andvalidity according to the CIDI. Eur Psychiatry 1997;12: 224–231.
25. Nurnberger JI Jr, Blehar MC, Kaufmann CA et al.Diagnostic interview for genetic studies: rationale, uniquefeatures, and training. NIMH genetics initiative. Arch GenPsychiatry 1994; 51: 849–859.
26. Wessa M, Houenou J, Paillere-Martinot ML et al. Fronto-striatal overactivation in euthymic bipolar patients duringan emotional go ⁄nogo task. Am J Psychiatry 2007; 164:638–646.
27. Mangin JF, Riviere D, Cachia A et al. A framework tostudy the cortical folding patterns. Neuroimage 2004;23(Suppl. 1): S129–S138.
28. Cachia A, Paillere-Martinot M-L, Galinowski A et al.Cortical folding abnormalities in schizophrenia patientswith resistant auditory hallucinations. NeuroImage 2008;39: 927–935.
29. Penttila J, Martinot J-L, Paillere-Martinot M-L et al.Altered global and temporal cortical folding in patientswith early-onset schizophrenia. J Am Acad Child AdolescPsychiatry 2008; 47: 1125–1132.
30. Allen JS, Bruss J, Mehta S, Grabowski T, Brown CK,Damasio H. Effects of spatial transformation on regionalbrain volume estimates. NeuroImage 2008; 42: 535–547.
31. Riviere D, Mangin JF, Papadopoulos-Orfanos D, Marti-nez JM, Frouin V, Regis J. Automatic recognition ofcortical sulci of the human brain using a congregation ofneural networks. Med Image Anal 2002; 6: 77–92.
32. Mangin JF, Frouin V, Bloch I, Regis J, Lopez-Krahe J.From 3D magnetic resonance images to structural repre-sentations of the cortex topography using topologypreserving deformations. J Math Imaging Vis 1995; 5:297–318.
33. Armstrong E, Schleicher A, Omran H, Curtis M, Zilles K.The ontogeny of human gyrification. Cereb Cortex 1995; 5:56–63.
34. Moorhead TW, Harris JM, Stanfield AC et al. Automatedcomputation of the Gyrification Index in prefrontal lobes:methods and comparison with manual implementation.Neuroimage 2006; 31: 1560–1566.
35. Ono M, Kubik S, Abarnathey CD. Atlas of the CerebralSulci. New York: Georg Thieme, 1990.
36. Duchesnay E, Cachia A, Roche A et al. Classificationbased on cortical folding patterns. IEEE Trans MedImaging 2007; 26: 553–565.
37. Kochunov P, Mangin JF, Coyle T et al. Age-relatedmorphology trends of cortical sulci. Hum Brain Mapp2005; 26: 210–220.
38. Luders E, Narr KL, Thompson PM et al. Gender differ-ences in cortical complexity. Nat Neurosci 2004; 7: 799–800.
39. Rettmann ME, Kraut MA, Prince JL, Resnick SM. Cross-sectional and longitudinal analyses of anatomical sulcalchanges associated with aging. Cereb Cortex 2006; 16:1584–1594.
40. Fox J. An R and S-Plus Companion to Applied Regres-sion. Thousand Oaks, CA: Sage Publications, Inc., 2002.
41. Regis J, Mangin JF, Ochiai T et al. ‘‘Sulcal root’’ genericmodel: a hypothesis to overcome the variability of thehuman cortex folding patterns. Neurol Med Chir 2005; 45:1–17.
42. Hilgetag CC, Barbas H. Role of mechanical factors in themorphology of the primate cerebral cortex. PLoS ComputBiol 2006; 2: e22.
43. Toro R, Burnod Y. A morphogenetic model for thedevelopment of cortical convolutions. Cereb Cortex 2005;15: 1900–1913.
44. Rakic P. Specification of cerebral cortical areas. Science1988; 241: 170–176.
45. Rakic P. Neuroscience. Genetic control of cortical convo-lutions. Science 2004; 303: 1983–1984.
46. Im K, Lee JM, Lyttelton O, Kim SH, Evans AC, Kim SI.Brain size and cortical structure in the adult human brain.Cereb Cortex 2008; 18: 2181–2191.
47. Lenox RH, Gould TD, Manji HK. Endophenotypes inbipolar disorder. Am J Med Genet 2002; 114: 391–406.
48. Zanetti MV, Cordeiro Q, Busatto GF. Late onset bipolardisorder associated with white matter hyperintensities: apathophysiological hypothesis. Prog Neuropsychopharma-col Biol Psychiatry 2007; 31: 551–556.
49. Gogtay N, Ordonez A, Herman DH et al. Dynamicmapping of cortical development before and after theonset of pediatric bipolar illness. J Child Psychol Psychi-atry 2007; 48: 852–862.
50. Gulseren S, Gurcan M, Gulseren L, Gelal F, Erol A. T2hyperintensities in bipolar patients and their healthysiblings. Arch Med Res 2006; 37: 79–85.
51. Miller A, Fox NA, Cohn JF, Forbes EE, Sherrill JT,Kovacs M. Regional patterns of brain activity in adultswith a history of childhood-onset depression: gender
Cortical folding in bipolar disorder
369
differences and clinical variability. Am J Psychiatry 2002;159: 934–940.
52. Moorhead TW, McKirdy J, Sussmann JE et al. Progres-sive gray matter loss in patients with bipolar disorder. BiolPsychiatry 2007; 62: 894–900.
53. Blumberg HP, Kaufman J, Martin A et al. Amygdala andhippocampal volumes in adolescents and adults withbipolar disorder. Arch Gen Psychiatry 2003; 60: 1201–1208.
54. Zilles K, Armstrong E, Schleicher A, Kretschmann HJ.The human pattern of gyrification in the cerebral cortex.Anat Embryol 1988; 179: 173–179.
55. Lyoo IK, Sung YH, Dager SR et al. Regional cerebralcortical thinning in bipolar disorder. Bipolar Disord 2006;8: 65–74.
56. Houenou J, Wessa M, Douaud G et al. Increased whitematter connectivity in euthymic bipolar patients: diffusiontensor tractography between the subgenual cingulate andthe amygdalo-hippocampal complex. Mol Psychiatry 2007;12: 1001–1010.
57. Gogtay N, Giedd JN, Lusk L et al. Dynamic mapping ofhuman cortical development during childhood through
early adulthood. Proc Natl Acad Sci U S A 2004; 101:8174–8179.
58. Paus T. Mapping brain maturation and cognitive devel-opment during adolescence. Trends Cogn Sci 2005; 9: 60–68.
59. Monkul ES, Matsuo K, Nicoletti MA et al. Prefrontalgray matter increases in healthy individuals after lithiumtreatment: a voxel-based morphometry study. NeurosciLett 2007; 429: 7–11.
60. Yucel K, Taylor VH, McKinnon MC et al. Bilateralhippocampal volume increase in patients with bipolardisorder and short-term lithium treatment. Neuropsycho-pharmacology 2008; 33: 361–367.
61. Atmaca M, Ozdemir H, Cetinkaya S et al. Cingulate gyrusvolumetry in drug free bipolar patients and patients treatedwith valproate or valproate and quetiapine. J Psychiatr Res2007; 41: 821–827.
62. Takahashi K, Oshima A, Ida I et al. Relationship betweenage at onset and magnetic resonance image-defined hyper-intensities in mood disorders. J Psychiatr Res 2008; 42:443–450.
Penttila et al.
370
Related Documents