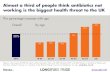
Nachreiner 1 Matthew Nachreiner Dr. Quinn Microeconomic Public Policies 8 December 2016 Pathway to Solve the Antibiotic Resistant Bacteria Problem Introduction to the Problem Figure 1 (Source: Cooper, 2011). Our efforts to address the rise of antibiotic resistant bacteria (ARBs 1 ) have been lackluster. Figure 1 illustrates the increasing level of resistance in just 3 ARBs over a thirty-year period (1980 – 2010) and it seems to continue to rise. If we aren’t able to halt antibiotic resistance bacteria, we will lose antibiotics as an option to cure bacterial infections. More importantly, the lack of antibiotics to address bacterial infections would render modern advances 2 such as surgery, transplants and chemotherapy unviable useless due to the threat of 1 See Appendix to see the abbreviations/acronyms spelled out. (Page 18) 2 “Without effective antimicrobials for prevention and treatment of infections, medical procedures such as organ transplantation, cancer chemotherapy, diabetes management and major surgery (for example, caesarean sections or hip replacements) become very high risk” (World Health Organization).

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Nachreiner 1
Matthew Nachreiner
Dr. Quinn
Microeconomic Public Policies
8 December 2016
Pathway to Solve the Antibiotic Resistant Bacteria Problem
Introduction to the Problem
Figure 1 (Source: Cooper, 2011).
Our efforts to address the rise of antibiotic resistant bacteria (ARBs1) have been
lackluster. Figure 1 illustrates the increasing level of resistance in just 3 ARBs over a thirty-year
period (1980 – 2010) and it seems to continue to rise. If we aren’t able to halt antibiotic
resistance bacteria, we will lose antibiotics as an option to cure bacterial infections. More
importantly, the lack of antibiotics to address bacterial infections would render modern
advances2 such as surgery, transplants and chemotherapy unviable useless due to the threat of
1 See Appendix to see the abbreviations/acronyms spelled out. (Page 18) 2 “Without effective antimicrobials for prevention and treatment of infections, medical procedures such as organ
transplantation, cancer chemotherapy, diabetes management and major surgery (for example, caesarean sections or
hip replacements) become very high risk” (World Health Organization).

Nachreiner 2
infection. This is a major cause for concern as society used roughly 38 million pounds of
antibiotics in the agriculture and healthcare sector combined in 2011 (Philpott). Legislation in
antibiotics is only now starting to be passed as ARBs are relatively new surfacing over the past
60 years. 3 In 2014, the Obama Administration issued the Executive Order on Combating
Antibiotic Resistance Bacteria (CARB) and funds were allocated to the Centers for Disease
Control (CDC) to initiate action only this year. CARB hasn’t been able to implement a strategy
to tackle the core issues: 1) the lack of a protocols and tracking on antibiotic use and negative
externalities of Obamacare’s policies, 2) the widespread use of antibiotics in livestock
production (as a growth supplement) and 3) the lack of antibiotic alternatives due to absence of
research and investment over the last three decades.
Due to the lack of a permanent and cohesive protocol throughout the healthcare sector for
the use of antibiotics and prevention of ARBs, doctors have oversubscribed antibiotics and
administrators in public institutions have failed to contain this growing problem. Figure 2 shows
how ARBs are also passed from animals to humans due to the widespread use of antibiotics in
the food industry to promote growth in food-producing livestock. To solve this issue, the
pharmaceutical industry, which has significantly reduced antibiotics research evident by 4
companies left in the market in Figure 1, has to produce more drugs of increasing strength to
manage the impact of ARBs. While, developing new innovative alternatives to antibiotics. As
stated by Tom Frieden, Director of the CDC: “Every day we don’t act to better protect antibiotics
will make it harder and more expensive to address drug resistance in the future. Drug resistance
can undermine both our ability to fight infectious diseases and much of modern medicine.
3 Case Study: Timeline of an ARB. University of Chicago Medicine developed the timeline of Methicillin-resistant
Staphylococcus aureus (MRSA). General Synopsis: First Outbreak in Boston in 1968, Large Outbreak in 1981,
Epidemic in 1998.

Nachreiner 3
Patients undergoing chemotherapy for cancer, dialysis for renal failure, and increasingly
common treatments for diseases such as arthritis depend on antibiotics so common infectious
complications can be treated effectively” (Dr. Frieden 5).
Figure 2 (Source: Frieden, 2013:15).
Brief History of Antibiotics and How Bacteria Become Antibiotic-Resistant:
Antibiotics were discovered by Sir Alexander Fleming and used to treat infections or
diseases caused by bacteria. Due to their effectiveness, they have increasingly been deployed
beyond human applications such as the agriculture sector where antibiotics are deployed to keep
livestock healthy by inhibiting the growth or destroying microorganisms. Figure 3 depicts how
bacteria become resistant to antibiotics. The antibiotics kill certain strains of bacteria, the
genetics of these strains are selected against and removed from the population. Conversely, the
genetics of the strains of bacteria that survive the antibiotics are selected for and grow in

Nachreiner 4
abundance in the population. The ARBs render the original antibiotic useless and forces
scientists to produce new antibiotics capable of destroying resistant-antibiotic bacterial genes.
The overall theme of this mechanism is evolution and it has started a vicious, endless cycle.4
Figure 3 (Source: Frieden, 2013:15)
Economic Impact to Society:
In 2010, the Obama Administration addressed the impact to society of healthcare costs
with the Affordable Care Act (ACA)5. Still, the overall healthcare spending across the economy
has reached 18.2% of gross domestic product still significantly more than the Organization for
Economic Cooperation and Development (OECD) average (Sussman). ARBs are a prime
contributor to rising healthcare costs because its expensive treatment and readmission of patients.
The health and economic impact of ARBs6 estimated by CDC in the United States (2013): “At
least two million illnesses and 23,000 deaths are caused by antibiotic-resistant bacteria in the
United States alone...Antibiotic resistance adds $20 billion in excess direct health care costs,
4 Case study of an ARB Defensive Mechanism- MRSA. The following sources, RxList and Postgrad Med (Look at
References Section), go into hard science behind the defensive mechanism for MRSA. 5 The following source, United State Department of Health and Services (Look at References Section) has more
information regarding ACA. 6 For in-depth information regarding individual ARBs cost to society look at Dr. Frieden’s article that entails CDC
report about Antibiotics (Page 51-89). For example: Clostridium Difficile: Costs over $1 Billion in excess medical
per year, 14000 deaths, and 250000 hospitalizations.

Nachreiner 5
with additional costs to society for lost productivity as high as $35 billion a year.” (Dr. Frieden
11). On a microscale, there was a case study in Chicago that looked at the impact of ARBs in a
hospital setting where “the cost (of an ARB) per patient ranged from $18588-29069, increased
hospital stays by 6.4-12.7 days, attributable mortality increased by 6.5%, and societal costs were
$10.7-15.0 million” (Roberts).7 Table 1 breaks down every party that is affected by ARBs. All
the costs mentioned above are being distributed across all these parties.
Table 1 (Source: McGowan 2001:1)
Goals of National Strategy for CARB
1. Slow the Emergence of Resistant Bacteria and Prevent the Spread of Resistant Infections
2. Strengthen National One-Health Surveillance Efforts to Combat Resistance
3. Advance the Development and Use of Rapid and Innovative Diagnostic Tests for
Identification and Characterization of Resistant Bacteria
4. Accelerate Basic and Applied Research and Development for New Antibiotics, Other
Therapeutics and Vaccines
5. Improve International Collaboration and Capacities for Antibiotic Resistance Prevention,
Surveillance, Control, and Antibiotic Research and Development (CDC)
The CDC is allocating $160 million to stop ARB in 2016 and $40 million in 2017 against a
total budget of approximately $7 billion (CDC). Prominent Public Health experts agree that
ARBs threaten modern medicine, but the actions to combat them are inadequate. Mae Wu, a
7 The study also looked at the impact if they reduced the ARBs levels by 3.5% in their hospital setting. They found
that the hospital would have saved $910,812, and the societal savings for reduced mortality and lost productivity
would have been $1.8 million.

Nachreiner 6
Natural Resources Defense Council (NRDC) attorney issued the following quote, “It’s great that
the President has elevated [the problem of antibiotic resistance] to this level, and the White
House is really talking about the problem and developing a plan over the next five years about
how to do it,” she says. “But it’s disappointing that they are being so passive on one of the
largest issues – the largest use of antibiotics in this country [in agriculture]” (Parks). In addition,
Venki Ramakrishnan a Nobel prize winner from the Laboratory of Molecular Biology at the
University of Cambridge pushed for a larger governmental role: “So I think that governments
really need to get involved in the development of new antibiotics. They have to think of this as
something generally good for society, the same reason that governments fund education, roads,
police, defense and so on. This is one case where governments need to act” (Moskvitch). Second,
the stated goals of CARB8 are simply too broad to bring solutions in a timely manner. The core
problem is that we must stop, or at least slow, the rate of growth of ARBs and, most critically,
create an alternative to antibiotics. As we finally start to address this problem, we need to over-
emphasize spending and activity on Goals 1 (Slow the Emergence of Resistant Bacteria and
Prevent the Spread of Resistant Infections) and 4 (Accelerate Basic and Applied Research and
Development for New Antibiotics, Other Therapeutics and Vaccines).
Modified National Strategy
In addition to requiring stronger funding, there are three main ways to overcome ARBs
economic and health impact on society:
1) Protocol
- Make Antimicrobial Stewardship Program (ASP) a federal mandate
- Properly educate our patients on antibiotics and look into prevention strategies.
- Remove patient satisfaction rating from the physician payment system formula that was
incorporated under the ACA to increase quality of healthcare
8 For example, one of CARB’s measured outcomes was reducing “inappropriate inpatient antibiotic use for
monitored conditions/agents will be reduced by 20% from 2014 levels” (CARB 9). The CARB failed to mention
how they would be able to measure this outcome.

Nachreiner 7
2) Elimination of Antibiotic Use for Growth Promotion in Animals in Agriculture
- The Food and Drug Administration (FDA) should make “Guidance for Industry (GFI)
#152”9 law that clearly that the bans the use of medically human important antibiotics for
growth promotion in agriculture. The law should be implemented over time for the
industry to adjust, although consumers have been demanding more antibiotic free
poultry/meat over the years. Companies that have made that transition could serve as case
studies.
3) New Antibiotics, Antibiotic-Free Alternatives, and Amending Obamacare
- The markets and the government have to restructure regulatory policies and incentivize
the development of new antibiotics.
- Actively develop antibiotic-free alternatives
Protocol on the Usage, Amending Obamacare, Patient Education of Antibiotics,
Prevention:
Public health institutions such as the IDSA (Infections Diseases Society of America)
along with the Obama Administration have started to take steps to cut back the excessive usage
of antibiotics that have led to the antibiotic resistance bacteria. The CDC has estimated: “up to
50 percent of all the antibiotics prescribed for people are not needed or are not prescribed
appropriately” (Dr. Frieden 15). The most significant step is the implementation of the ASP that
wants to coordinate the entire healthcare sector (private or public) to administer proper usage of
antibiotics that maintains its effectiveness and increases efficiency within the sector (Bakken).
The ASP would rely on CDC’s core elements. The core elements involve leadership
commitment, accountability, drug expertise, action, tracking, reporting, and education. The
public health institutes need to look at hospitals that have opted into the program and learn from
them to increase the efficiencies of future programs across the country. By publishing the results
behind these case studies, government agencies would be able to push forth a proposal for a
federal mandate for ASPs across the country.
Pew Trusts analyzed case studies and came away with important guidelines for the
successful implementation of ASP’s: “Someone within the institution who strongly believes in,
9 For more information regarding this GFI, refer to the following source FDA on the references section.

Nachreiner 8
and is committed to, antibiotic stewardship. Shared responsibility for monitoring the program
and implementing new interventions” (Talkington). These characteristics motivated the hospital
to sustain their ASP, along with results that justified the costs of the program. One case study
proved that the cost savings created by the ASP outweighed the initial costs of implementing it.
St. Tammany Parish Hospital in Covington, Louisiana carried out an ASP that required
employees to complete stewardship training and the information technology manager created a
computer-assisted surveillance program that held physicians accountable for their decision
making. Physicians were aided by the installment of ASP recommendations on their medical
software prior to administering antibiotics to their patients. In addition, the hospital held weekly
meetings to discuss appropriate antibiotic selection and dosing. All their efforts culminated in
reducing daily doses per month of all antibiotics by more than 61%. Furthermore, the adjusted
total antimicrobial cost per adjusted patient-day peaked at $25.93 in October 2012 and was
reduced to an average cost of $8.32 per patient-day after ASP implementation. Since its
inception in July 2013, the ASP’s review of antimicrobial use has resulted in a total savings of
$1.3 million through December 2014. The cost savings generated by the ASP in the first year
alone more than offset the staff time devoted to ASP activities (Talkington).
The ACA aimed to improve the quality of healthcare by tying patient satisfaction into the
formula for physician payment. The Obama Administration argued that this portion of the ACA
would hold physicians accountable to their patients. For instance, Dr. Miller from the University
of Utah Hospitals & Clinics in Salt Lake City saw, “A big turnaround for our institution” in
terms of bedside manner to being attentive to basic needs. However, this creates a conflict of
interest in solving the ARB problem. Professor Hoff points out that a “provider giving a patient
an unnecessary antibiotic simply because it will earn him or her a better rating” (Wolinsky).

Nachreiner 9
Unfortunately, the patient satisfaction component of the physician payment system has
created a negative externality by incentivizing physicians to provide antibiotics to a patient
in order to get a better rating and higher pay, even though that isn’t the treatment that patient
needed.10 This leads to the oversubscription of antibiotics and in the long run economic and
health costs to society due to resistance. The next Presidential administration must take patient
satisfaction out of the formula for physician payment to avoid oversubscription of antibiotics.
In addition to the concerted effort from the public health institutions, the physicians need
to educate their patients on antibiotics and the treatment plan. A study published in Society for
Healthcare Epidemiology of America, concluded that complying with the physician’s antibiotic
treatment plan significantly reduces the spread of a particular ARB, MRSA. They looked at 223
households in southeast Pennsylvania, who contracted MRSA and were prescribed antibiotics,
founded that those who stuck to the antibiotic treatment guidance by the physician were able to
completely wipeout MRSA in 4 days faster than non-compliant households11. This study points
out the importance of antibiotic education. For example, many patients stop using antibiotics
once they start to physically and mentally feel better. However, the bacteria aren’t necessarily
eradicated and can come back if the patient fails to carry out the physician’s antibiotic schedule
completely. Furthermore, the patient’s negligence can foster a population of antibiotic-resistant
bacteria that not only renders the original antibiotic useless, but could potentially put their health
in danger (Society for Healthcare Epidemiology of America).
In addition to patient education and protocol on antibiotics, healthcare facilities can also
engage in prevention strategies. For example, the Veteran Affairs Medical Center (VAMC)
10 Hard to find data regarding this claim because the physician would be criticized by public health experts.
However, this is important to point out because in theory it incentives the physician to act against the public good. 11 4 more healthy days to a patient may make them more productive in the workforce, which leads to an increase in
income.

Nachreiner 10
wanted to prevent hospital acquired MRSA. They implemented a national initiative to prevent
MRSA. The VAMC took on a bundled approach: “screening every patient for MRSA, use of
gowns and gloves when caring for patients colonized or infected with MRSA, hand hygiene, and
an institutional culture change focusing on individual responsibility for infection control. It also
created the new position of MRSA Prevention Coordinator at each center” (Evans). After four
years of the national initiative, the VA saw a 36% decrease in MRSA infection rate (Evans).12
All hospitals can learn from the Veteran Affairs Medical Center’s case study that utilized a
prevention strategy that significantly reduced the spread of ARB diseases in a healthcare facility
setting13.
Eliminate Antibiotics for Growth Promotion for Animals
The food industry accounts for close to 80% of all antibiotic usage in the US and has
been slow to accept responsibility for their contribution to the ARB problem (ConsumerUnion).
The industry argues that the use of antibiotics on livestock only contributes to the ARB problem
in livestock-essentially it is isolated to their own community. The CDC, Food and Drug
Administration (FDA), World Health Organization (WHO), and other reputable scientific
organizations have testified that antibiotic usage in animals leads to antibiotic resistance in
humans. Dr. Thomas R. Frieden, Director of the CDC, noted that “there is strong scientific
evidence of a link between antibiotic use in food animals and antibiotic resistance in humans”
(ConsumerUnion).
12 The article didn’t give any CBA analysis of the national initiative. It is safe to assume that the benefits
outweighed the costs because the VAMC expanded the strategy to 133 long-term care facilities across the US. 13 Sherwin Williams has created a product, Paint Shield Microbicidal Interior Latex paint, that can kill ARBs that
comes into contact with the painted surfaces. This product is EPA-registered. (Look at References Section)

Nachreiner 11
Figure 2 clearly shows the ARB’s can enter humans through direct consumption of
contaminated meat and environmentally from the agriculture employees and facilities. In fact, 14
Consumer Reports tested retail poultry and found that more than ⅔ of the samples were
contaminated with more than 60% of the bacteria resistant to one or more antibiotics
(ConsumerUnion). The counterargument from industry is that people know how to thoroughly
cook poultry to avoid this threat. While this is a valid argument, we have seen 2 outbreaks
serious enough to involve the CDC - one that required that 36 million pounds of turkey15 to be
recalled (ConsumerUnion).
Given the high stakes involved in stopping ARB and strong scientific evidence showing
the links between animals and humans, we have to take stronger action to eliminate the use of
antibiotics medically important to humans for growth promotion in animals. This means that the
US government should make FDA’s GFI #152 not a recommendation that results in voluntary
cooperation by the companies, but rather a law that allows time for these companies to transition.
The argument from the agriculture and pharmaceutical community is that antibiotics are
needed to prevent disease. The GFI addresses this issue by allowing antibiotics by prescription
from a veterinarian. 16GFI #152 will not have a major impact on the agriculture industry as firms
have been in tune with consumer trends over the years. A case study done by the non-profit
organization, NRDC, looked at this phenomenon in greater detail. A Consumer Reports survey17
revealed that 86% of consumers wanted antibiotic-free meat and poultry in their local
14 White examined the impact and cases of meat that contains ARBs consumed by the population in the following
article, “The Isolation of Antibiotic-Resistant Salmonella from Retail Ground Meats”. 15 Cargill’s ground turkey contained multi-resistant salmonella that caused 77 illnesses. Bottemiller goes into more
detail about this incident in the following article, “Cargill Recalls 36 million pounds of ground turkey”. 16 In Nordrum and Whitman’s article, they estimated that Pharmaceutical companies spent at least $14.3 million
lobbying Congress in 2013 and 2014 against proposed bills against antibiotics in the agriculture industry.
Agricultural groups spent another $9.2 million on the same proposed bills. 17 The following article, “Meat on Drugs”, provides Consumer Reports Survey and takeaways from its research.

Nachreiner 12
supermarket, 60% were willing to pay at least $0.05 cents per pound more, and 40% said they
would pay $1 or more per pound. In terms of the market for these products, they found that the
sales for meats without antibiotics had grown 25% over a three-year window (2009-2012) and
have been the fastest grower in the organic industry. Sales of antibiotic-free chicken had grown
over 34% in value in 2013, with consumer spending reaching over $1 billion in 2014 which
excluded restaurants and commercial purchasing. This growing demand from consumers has
forced chicken buyers and chicken producers to alter their production lines. The two biggest
chicken producers, Tyson Chickens and Pilgrim’s Pride, along with one of the biggest chicken
buyers, Chick-fil-A, are leading the charge and represent the tipping point for the industry. A
Pilgrim’s Pride’s representative said that “We’re seeing quite a big growth in antibiotic-free
product. As consumers and the population are looking more for that, the industry needs to
follow” (NRDC). Experts have quelled the worry about the transitional costs for many
companies by pointing towards Denmark18 who phased out the routine use of antibiotics in
animal feed and found no net cost changes because money saved by not purchasing these drugs
offset any costs associated with animals growing fatter on less feed. In addition, research from
the Economic Research Service19 provides evidence that cost of these products wouldn’t result in
significantly higher costs to consumers estimating that wholesale prices of pork and poultry
would increase by less than 5 percent, and retail prices would increase by even less (NRDC).
Alternatives:
Pew Charitable Trust has conducted extensive research showing that the discovery of
new antibiotics has diminished completely in the last half century due to multiple factors. In fact,
18 Following article “Impacts of Antimicrobial Growth Promoter Termination in Denmark”, contains the Denmark
Case Study. 19 The economist, Sneeringer, has piles of research that back this claim. (Look Sneeringer under the References
Section).

Nachreiner 13
Figure 4 shows that there hasn’t been a new type of antibiotic in the past 30 years. The primary
reasons are: “scientific barriers to drug discovery, regulatory challenges, and diminishing returns
on investment have led major drug companies to scale back or abandon their antibiotic research”
(Antibiotic Resistance Project).
Figure 4 (Source: Silver, 2011)
In other words, the markets haven’t incentivized the major players in drug development to solve
the antibiotic resistance problem. Nor has the market made it enticing for healthcare investors to
put their money into anti-bacterial research versus oncology research.
The numbers behind this claim were analyzed via a cost-benefit analysis from the Office
of Health Economics in London, where they calculated the net present value (NPV) of a new
antibiotic is only about $50 million, compared to approximately $1 billion for a drug used to

Nachreiner 14
treat a neuromuscular disease” (Ventola). In addition, the pricing of new antibiotics is
economically unappealing compared to new chemotherapy treatments: “Newer antibiotics are
priced at a maximum of $1,000 to $3,000 per course, while cancer chemotherapy that costs tens
of thousands of dollars” (Ventola). The reason behind this rationale is that “to keep resistance
levels down and maintain effectiveness, doctors often hold new drugs in reserve and use them
only when needed and with limited patient populations” (Thayer). Thus, there is a reduced use of
new antibiotics limiting revenue, and then generics are introduced lowering prices as patents
expire. “Hospitals are constrained in how they reimburse for drugs, so it’s difficult to convince
doctors to look at a new therapy, especially if cheaper generics are available” (Thayer). As a
result, the cheaper generics reduce the return on investment for the original supplier.
Furthermore, “many payers expect all antibiotics to be priced similarly—even new agents that
target multidrug-resistant (MDR) pathogens”. This has led the majority of the major
pharmaceutical players to abandon the antibiotic field. Figure 5 shows that all these factors have
led to the reduction over time in antibacterial new drug application approvals that are still being
processed in Phase II and Phase III of FDA Approval20.
As a result, Pew Charitable Trust has recommended changes to regulatory policies and
providing economic incentives to promote drug development. In addition, they suggest major
agents that are involved in the problem develop plans to share information on developing a better
understanding on the science behind ARBs, innovating new solutions that deviate from
antibiotics, and tackling the basic scientific barriers impeding antibiotic discovery and
development (Antibiotic Resistance Project).
20 For more information regarding the different phases, refer to USFDA on the references section.

Nachreiner 15
Figure 5 (Source: Ventola 2015).
Over the past 2 decades, the FDA has introduced changes in clinical trials that has made
antibiotic clinical trials very challenging. Basically, the changes require large sample populations
driving higher costs making the development of antibiotics uneconomical and unattractive. In the
article, “The United States Food and Drug Administration and the End of Antibiotics”, Shlaes
and Moellering discussed how altering the requirements for trial designs can have a significant
impact on the size, and hence cost, of conducting clinical trials. Although more work in this area
needs to be done, the FDA issued guidance in 2013 that changed the required clinical trial for
acute bacterial skin and skin-structure infections. While these minor changes are encouraging,
we need to support the new limited-population antibiotic drug (LAPD)21 regulatory approval
pathway to enable smaller, less-expensive and faster clinical trials.
21 For more information regarding (LAPD), refer to Infectious Diseases Society of America under the references
section.

Nachreiner 16
In addition, we will have to consider investment and economic incentives for large
pharmaceutical companies to encourage research and development in this area. The current
CARB program relies almost exclusively on government agencies, BARDA22, FDA and others,
to develop antibiotic alternatives. We need to include private industry solutions. In January, 80
drugmakers and diagnostic companies, which included the market leaders, signed a request for
companies and government to cooperate to develop incentives for research and development of
new antibiotics (Berkrot). They proposed a new business model where profits would not be
linked to higher sales instead lump sum payments23 would be awarded to companies, or groups
of companies, that develop effective new antibiotics and antibiotic alternatives. We must have
engagement and leadership from the strongest players in the pharmaceutical industry to develop
alternatives, a group should be formed to include this structure in the CARB action plan.
The following paragraph describe a new alternative24 that has a high potential in solving
specific ARB such as MRSA or a broad range of ARBs.
A future treatment that revolves around antibacterial technology with creams has started
to surface under the tutelage of a Dutch Biotechnology Firm, Micreos Human Health B.V. They
have been recently awarded a large sum of equity to further their development of Staphefekt. The
product specifically targets S. aureus and its resistant strains such as MRSA. Additionally, the
product utilizes an enzyme called endolysins that kills off bacteria at a high rate and extremely
unlikely for an emergence of resistance to the enzyme. This alternative has long way to go before
22 BARDA (Biomedical Advanced Research and Development Authority) 23 From the article, “New Incentives Needed to Develop Antibiotics to Fight Superbugs”, a lump-sum payment
would look like what the British Government panel suggested “drug companies be offered up to $1.5 billion for
successful development of a new antibiotic”. 24 There are two interesting alternatives (Phage Therapy and ADEP) that are still in its initial stages, but have
encouraging results. For more information regarding Phage Therapy refer to Górski and ADEP refer to Herring
under the references section.

Nachreiner 17
the product can be introduced to the market, however the initial results have been promising and
gives the pharmaceutical industry and society hope that we can solve this problem (Micreos).
Final Thoughts
ARBs are a serious threat to our society and the healthcare system. Even though the US
government has been late to address this problem, it is encouraging that we are now taking steps
to address it. However, I believe the national strategy lacks funding and focus. My modified
national strategy narrows down the focus to the major components that are integral to solving
this problem in the short and long-term. Once, we are able to solve this issue in the United
States, we have to help the World conquer this problem and put into place a system that will
track and control ARBs worldwide.

Nachreiner 18
Appendix
ACA- Affordable Care Act
ARBs- Antibiotic Resistant Bacteria
ASP- Antimicrobial Stewardship Program
CARB- Combating Antibiotic Resistant Bacteria (Obama Administration Plan)
CDC- Center for Disease Control and Prevention
FDA- Federal Drug Administration
GFI- Guidance for Industry
HHS- Health and Human Services
IDSA- Infectious Diseases Society for America
LAPD- Limited Population Antibiotic Drug
MRSA- Methicillin-resistant Staphylococcus aureus
NCBI- National Center for Biotechnology Information
NRDC- Natural Resources Defense Council
OECD- Organization for Economic Cooperation and Development
USFDA- United States Food and Drug Administration
VAMC- Veteran Affairs Medical Center
WHO- World Health Organization
WSJ- Wall Street Journal

Nachreiner 19
References:
Antibiotic Prescriptions per 1000 Persons of All Ages According to State, 2010 [Model]. (2010).
Retrieved from https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats
-2013-508.pdf#page=13
Antibiotic Resistance Project. (2016, May 11). Retrieved October 12, 2016, from The Pew
Charitable Trusts website: A Scientific Roadmap for Antibiotic Discovery
Bakken, J. S. (2016, January 4). IDSA Comments to PACCARB on Antibiotic Resistance Data
Collection. Retrieved from IDSA website:
https://www.idsociety.org/uploadedFiles/IDSA/Policy_and_Advocacy/Current_Topics_a
nd_Issues/Advancing_Product_Research_and_Development/STAAR_Act/Letters/IDSA
%20Comments%20to%20PACCARB%20on%20Antibiotic%20Resistance%20Data%20
Collection_01042016.pdf
Berkrot, Bill. "New Incentives Needed to Develop Antibiotics to Fight Superbugs." Reuters, 27
May 2016. www.reuters.com/article/us-health-superbug-antibiotics-idUSKCN0YI2MZ.
Bottemiller, Helena. "Cargill Recalls 36 Million Pounds of Ground Turkey." Food Safety News,
4 Aug. 2011. www.foodsafetynews.com/2011/08/cargill-recalls-36-million-pounds-of-
ground-turkey/#.WEh_eIWcHIV.
CARB. (2014). National Strategy For Combating Antibiotic Resistant Bacteria. WH, 37.
Retrieved from
file:///C:/Users/Matt/AppData/Local/Microsoft/Windows/INetCache/IE/ZIG9C
YW6/carb_national_strategy.pdf
Carrillo, C. L., & Abedon, S. T. (2011, April). pros and cons of phage therapy. NCBI, 1(2), 112-
114. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278648/pdf/bact0102_0111.pdf
CDC. "National Strategy for Combating Antibiotic Resistant Bacteria."
www.cdc.gov/drugresistance/pdf/carb_national_strategy.pdf. Sept. 2014.
ConsumerUnion. (2016). The Overuse of Antibiotics in Food Animals Threatens Public Health.
ConsumerUnion. Retrieved from http://consumersunion.org/news/the-overuse-of-
antibiotics-in-food-animals-threatens-public-health-2/
Cooper, Matthew A., and David Shlaes. "Fix the antibiotics pipeline." Nature, 7 Apr. 2011.
www.nature.com/nature/journal/v472/n7341/full/472032a.html.

Nachreiner 20
Core Elements of Hospital Antibiotic Stewardship Programs. (2016, May 25). Retrieved October
8, 2016, from CDC website:
http://www.cdc.gov/getsmart/healthcare/implementation/core-elements.html
Examples of How Antibiotic Resistance Spreads [Model]. (2013). Retrieved from
https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-
508.pdf#page=13
Evans, Martin E., et al. "MRSA Infection Rates Drop in Veterans Affairs Long-Term Care
Facilities." American Journal of Infection Control. www.elsevier.com/about/press
-releases/research-and-journals/mrsa-infection-rates-drop-in-veterans-affairs-long-term
-care-facilities.
FDA. (2013, December). U.S. Department of Health and Human Services Food and Drug
Administration Center for Veterinary Medicine. FDA, Retrieved from
http://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/Gui
danceforIndustry/UCM299624.pdf
Frieden Dr. (2013, April 23). Antibiotic Resistance Threats in the United States, 2013.CDC
-Central Disease Control, 114. Retrieved from
https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-
508.pdf#page=13
Górski, A., & Hirszfeld, L. (2007, August 3). Phage therapy of staphylococcal infections
(including MRSA) may be less expensive than antibiotic treatment. Postępy Higieny I
Medycyny Doświadczalnej, Retrieved from
http://www.phmd.pl/fulltxthtml.php?ICID=495359
Guidos, Robert J. "Combating Antimicrobial Resistance: Policy Recommendations to Save
Lives." NCBI, May 2011. www.ncbi.nlm.nih.gov/pmc/articles/PMC3738230/.
Herring, A. (2013, November 13). http://www.northeastern.edu/news/2013/11/lewis-mrsa/.
Northeastern News (Research).
How Antibiotic Resistance Happens [Model]. (2013). Retrieved from
https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-
508.pdf#page=13
Impacts of Antimicrobial Growth Promoter Termination in Denmark, Word Health Organization,
November 6, 2002, www. iatp.org/documents/impacts-of-antimicrobial-growth-

Nachreiner 21
promoter-termination-indenmark-0.
Infectious Diseases Society of America. "Limited Population Antibacterial Drug (LPAD)
Approval Mechanism Frequently Asked Questions."
www.idsociety.org/uploadedFiles/IDSA/News_and_Publications/IDSA_News_Releases/
2012/LPAD%20FAQs.pdf.
McGowan, John E. "Economic Impact of Antimicrobial Resistance." NCBI (National Center for
Biotechnology Information), Mar. 2001.
www.ncbi.nlm.nih.gov/pmc/articles/PMC2631707/pdf/11294725.pdf.
"Meat On Drugs." Consumer Report, June 2012.
www.consumerreports.org/content/dam/cro/news_articles/health/CR%20Meat%20On%2
0Drugs%20Report%2006-12.pdf.
Micreos secures €12M for antibiotic alternative. (2016, February 23). Holland (Connecting you
with Netherlands). Retrieved from http://nlintheusa.com/micreossecures-
e12millionfornewproductscontaining-staphefekt/
Moskvitch, Katia. "How to Solve the Problem of Antibiotic Resistance." Scientific American, 28
Jan. 2015. www.scientificamerican.com/article/how-to-solve-the-problem-of-antibiotic-
resistance/.
Nordrum, Amy, and Elizabeth Whitman. "Antibiotic Resistance: How Livestock Lobbyists and
Drug Companies Hinder The US Fight Against Superbugs." International BusinessTimes,
29 Apr. 2015. www.ibtimes.com/antibiotic-resistance-how-livestock-lobbyists-drug-
companies-hinder-us-fight-against-1901499.
NRDC. "Going Mainstream: Meat and Poultry Raised Without Routine Antibiotics Use." Dec.
2015, www.nrdc.org/sites/default/files/antibiotic-free-meats-CS.pdf.
Paint Shield® Microbicidal Interior Latex Paint. (n.d.). Retrieved October 5, 2016, from
Sherwin Williams website: http://www.sherwin-
williams.com/homeowners/products/catalog/paint-shield-microbicidal-interior-latex/
Park, Alice. "Obama Plan to Fight Antibiotics Resistance 'Disappointing,' Critics Say." Times, 18
Sept. 2014. time.com/3399231/obama-antibiotic-resistance.

Nachreiner 22
Pew Charitable Trusts. (2016). Scientific Barriers Impede Antibiotic Discovery [Drawing].
Retrieved from http://www.pewtrusts.org/en/research-and-analysis/reports/2016/05/a-
scientific-roadmap-for-antibiotic-discovery
Philpott, Tom. "The Meat Industry Now Consumes Four-Fifths of All Antibiotics." Mother
Jones, 8 Feb. 2013. www.motherjones.com/tom-philpott/2013/02/meat-industry-still-
gorging-antibiotics.
Postgrad Med (UCSF). (2001). Methicillin-resistant Staphylococcus aureus. Mechanisms of
resistance and implications for treatment. NCBI, Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/19667557
Roberts, Rebecca R., et al. "Hospital and Societal Costs of Antimicrobial-Resistant Infections in
a Chicago Teaching Hospital: Implications for Antibiotic Stewardship." 9 Sept. 2009.
cid.oxfordjournals.org/content/49/8/1175.full.pdf+html.
RxList. (2010). Antibiotic Resistance: Questions & Answers. RxList , Retrieved from
http://www.rxlist.com/antibiotic_resistance-page3/drugs-condition.htm
Shlaes, David M., and Robert C. Moellering. "The United States Food and Drug Administration
and the End of Antibiotics." Oxford Journals-Clinical Infectious Diseases, 2002.
cid.oxfordjournals.org/content/34/3/420.2.long.
Silver, L. L. (2011). More than 30 Year Void in Discovery of New Types of Antibiotics
[Diagram]. Retrieved from http://www.pewtrusts.org/en/research-and-
analysis/reports/2016/05/a-scientific-roadmap-for-antibiotic-discovery
Society for Healthcare Epidemiology of America. (2016, July 28). Household MRSA controlled
through treatment compliance, patient education: New research shows that patient
education and compliance are just as important as the treatment itself in household
MRSA decolonization after infection. ScienceDaily. Retrieved October 11, 2016 from
www.sciencedaily.com/releases/2016/07/160728125302.htm
Sneeringer, S., Economic research Service, USDA. (presentation, Antibiotic resistance at the
Animal Human Interface Workshop, Princeton, NJ, May 13, 2014).
Sumairi, H. (2012). MRSA-Mechanism [Diagram]. Retrieved from
http://image.slidesharecdn.com/mrsaseminarfinaldraft2642012-121230115249-
phpapp01/95/mrsa-seminar-final-draft-2642012-19-638.jpg?cb=1356868842
Sussman, A. L. (2016, August 16). Burden of Health-Care Costs Moves to the Middle Class.
WSJ. Retrieved from http://www.wsj.com/articles/burden-of-health-care-costs-moves-to-
the-middle-class-1472166246

Nachreiner 23
Talkington, Kathy, et al. "A Path to Better Antibiotic Stewardship in Inpatient Settings 10 case
studies map how to improve antibiotic use in acute and long-term care facilities." The
Pew Charitable Trusts, Apr. 2016.
www.pewtrusts.org/~/media/assets/2016/04/apathtobetterantibioticstewardshipininpatient
settings.pdf.
Thayer, A. M. (2016, September 5). Antibiotics: Will the bugs always win? Chemical and
Engineering News. Retrieved from http://cen.acs.org/articles/94/i35/Antibiotics-bugs-
always-win.html
United States Department of Health & Human Services. "Read the Law." HHS.Gov,
www.hhs.gov/healthcare/about-the-law/read-the-law/. Accessed 2 Dec. 2016.
University of Chicago Medicine. (n.d.). MRSA History Timeline: 1959–2016. Retrieved 2014,
from The University of Chicago Medicine website: http://mrsa-research-
center.bsd.uchicago.edu/timeline.html
USFDA. "The FDA's Drug Review Process: Ensuring Drugs Are Safe and Effective." 6 Nov.
2014, www.fda.gov/drugs/resourcesforyou/consumers/ucm143534.htm.
Ventola, C. Lee. "The Antibiotic Resistance Crisis Part 1: Causes and Threats." NCBI, Apr.
2015. www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/.
White, David G., et al. "The Isolation of Antibiotic-Resistant Salmonella from Retail Ground
Meats." The New England Journal of Medicine.
www.nejm.org/doi/full/10.1056/NEJMoa010315#t=article.
Wolinsky, Howard. "Survey dissatisfaction." Modern Healthcare, 2015.
www.modernhealthcare.com/article/20160903/MAGAZINE/309039981?template=print.
World Health Organization. "Antimicrobial Resistance." WHO, Sept. 2016,
www.who.int/mediacentre/factsheets/fs194/en/.
Related Documents