Thyroid gland Dr.S ara Al-Ghanem – intern from KFU

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Thyroid glandDr.Sara Al-Ghanem – intern from KFU

Objectives

SIZE of Thyroid gland
The thyroid gland weighs 10 to 20 grams in normal adults.
Thyroid volume measured by ultrasonography (US) is slightly greater in men than women
it increases with age and body weight. it decreases with increasing iodine intake. The thyroid is one of the most vascular organs in the
body. Thus, US measurements of thyroid volume and even nodule size can differ markedly from the size after devascularization and resection.


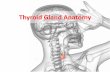
Its location & relations
The normal thyroid gland is immediately caudal to the larynx and encircles the anterolateral portion of the trachea.
The thyroid is bordered by the trachea and esophagus medially and the carotid sheath laterally.
The sternocleidomastoid muscle and the three strap muscles (sternohyoid, sternothyroid, and the superior belly of the omohyoid) border the thyroid gland anteriorly and laterally

Shape
It consists of two lobes connected by a narrow isthmus.
Each lobe is pyramidal in shape, with its apex directed upward and its base directed downward.
The isthmus is the narrow part of the gland connecting the two lobes.
A small pyramidal lobe projecting upward from the isthmus is often present to the left of the midline.


BLOOD SUPPLY
The arterial blood supply to the thyroid gland is primarily from the right and left superior and inferior thyroid arteries, derived from the external carotid arteries and thyrocervical trunk, respectively.
The venous drainage consists of the superior, middle, and inferior thyroid veins that drain into the internal jugular vein and innominate vein

Superior thyroid artery is the first branch off the external carotid artery. It extends inferiorly to the superior pole of the thyroid lobe.
In addition to supplying the thyroid, the superior thyroid artery is the primary blood supply to approximately 15 percent of superior parathyroid glands.
The superior thyroid artery is a landmark for identification of the superior laryngeal nerve, which courses with the artery until approximately 1 cm from the superior thyroid pole

Inferior thyroid artery is a branch of the thyrocervical trunk which arises from the subclavian artery.
The inferior thyroid artery courses posterior to the carotid artery to enter the lateral thyroid. The point of entry can extend from superior to inferior thyroid poles.
The inferior thyroid artery also supplies the inferior parathyroid glands and approximately 85 percent of superior parathyroid glands.
The RLN may course anterior or posterior to the inferior thyroid artery. In some cases, the RLN may branch into both an anterior and posterior position.

Thyroidea ima artery is found in approximately 3 percent of individuals and arises from the aortic arch or innominate artery and courses to the inferior portion of the isthmus or inferior thyroid poles.
Surgical control of the thyroidea ima artery is essential during thyroidectomy.
The thyroidea ima artery can be quite enlarged in patients with thyroid disease such as goiter or hyperthyroidism

Venous drainageSuperior thyroid vein: It arises from the upper part of the lobe. It ends into the internal jugular vein.
Middle thyroid vein: It arises from the middle of the lobe. It ends into the internal jugular vein.
Inferior thyroid veins: Arise from the isthmus and lower parts of the lobes. Descend in front of the trachea. End into the left brachiocephalic vein.

Lymphatic drainage
The lymphatic vessels of the thyroid gland drain into:
1) Pretracheal lymph nodes. 2) Paratracheal lymph nodes.
- The efferent of these nodes drain into the deep cervical lymph nodes.

Thyroid PhysiologySynthesis of the thyroid hormone
Trapping of inorganic iodide from the bloodOxidation of iodide to iodine.
Binding of iodine with tyrosine to form iodotyrosines.
Coupling of mono-iodotyrosines and di-iodotyrosine to form T3, T4

Synthesis of the thyroid hormone
The metabolic effects of the thyroid hormones are due to unbound T4 and T3.
T3 is the more important and is also produced in the periphery by conversion from T4.
T3 is quick acting (within a few hours) whereasT4 acts more slowly (4-14 days)

REGULATION OF THYROID HORMONE PRODUCTION

Thyrotropin-releasing hormone (TRH) increases the secretion of thyrotropin (TSH), which stimulates the synthesis and secretion of trioiodothyronine (T3) and thyroxine (T4) by the thyroid gland. T3 and T4 inhibit the secretion of TSH, both directly and indirectly by suppressing the release of TRH. T4 is converted to T3 in the liver and many other tissues by the action of T4 monodeiodinases. Some T4 and T3 is conjugated with glucuronide and sulfate in the liver, excreted in the bile, and partially hydrolyzed in the intestine. Some T4 and T3 formed in the intestine may be reabsorbed. Drug interactions may occur at any of these sites.

Effects of Thyroid Hormone
Fetal brain and skeletal maturation Increase in basal metabolic rate Increases sensitivity to catecholamines Stimulates gut motility Increase bone turnover Increase in serum glucose, decrease in serum
cholesterol

Parathyroid gland

Normal parathyroid glands are approximately the size of a grain of rice or a lentil. Normal glands are usually about 5 by 4 by 2 millimeters in size and weigh 35 to 50 milligrams. Enlarged parathyroid glands can be 50 milligrams to 20 grams in weight, most typically weighing about 1 gram and 1 centimeter in size
SIZE AND LOCATION

Normal superior parathyroid glands are usually located on the posterior-lateral surface of the middle to superior thyroid lobe. They lie under the thyroid superficial fascia, posterior to the recurrent laryngeal nerve and can be visualized by carefully dissecting the thyroid capsule in this region.
Superior parathyroid glands

The two inferior parathyroid glands reside in the anterior mediastinal compartment, anterior to the recurrent laryngeal nerve. They are most often found in the thyrothymic tract, or just inside the thyroid capsule on the inferior portion of the thyroid lobes
Inferior parathyroid glands

The superior parathyroid glands receive most of their blood supply from the inferior thyroid artery and also are supplied by branches of the superior thyroid artery in 15 to 20 percent of patients.
The inferior parathyroid glands receive their end-arterial blood supply from the inferior thyroid artery.

References

THANK YOU
Related Documents