Working Group 3: Clinical Trials NSAYAO Scientific Update and Workshop Bethesda, MD September 16-17, 2013

Working Group 3: Clinical Trials
Jan 28, 2016
Working Group 3: Clinical Trials. NSAYAO Scientific Update and Workshop Bethesda, MD September 16-17, 2013. Working Group 3: Clinical Trials. WG3: Primary Question. - PowerPoint PPT Presentation
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Working Group 3: Clinical Trials
NSAYAO Scientific Update and Workshop
Bethesda, MD
September 16-17, 2013

Working Group 3: Clinical TrialsName Discipline Affiliation Key Experience
David Freyer (Chair) Pediatric Oncology Children’s Hospital Los Angeles , USC
Chair, COG AYAO Discipline Committee
Charles Blanke (Co-Chair)
Medical Oncology Oregon Health & Sciences University
Group Chair, SWOG
Rashmi Chugh Medical Oncology University of Michigan Sarcoma, SARC
Steve Friedman Informatics/Data Mgt CTEP/NCI NCI Data Analyses
Sally Hunsberger Biostatistics NCI NCI Data Analyses
Danny Indelicato Radiation Oncology University of Florida RTOG, LiveStrong and Critical Mass Alliances
Wolf Lindwasser Brain and Solid Tumor Steering Committees
CTEP/NCI CTEP Study Review and Prioritization
Michael Link Pediatric Oncology Stanford University ASCO Chair, sarcoma
Ann O’Mara Oncology Nursing, Palliative Care
DCP/NCI Cancer Control, CCOP
Nita Seibel Pediatric Oncology CTEP/NCI NCI AYAO Committee
Wendy Stock Medical Oncology University of Chicago Chair, C10403
Eric Tai Pediatrics, Preventive Medicine
CDC AYA Access to Clinical Trials Initiative

WG3: Primary Question
“Since enrollment was recognized as a factor in the lack of progress in AYA Oncology, what has been the clinical trial activity and what are the outstanding obstacles?”

15-19 20-24 25-290-14 35-39
0%
.8%
1.6%
2.4%
3.2%
4.0%
30-34
Ave
. Ann
ual
% C
ha
nge
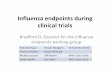
Change in SEER 5-Year Survival from 1985-1992
Age (Years)
Accrual Proportion (log)
r = 0.93, p = 0.006
-1%
0%
1%
2%
3%
4%
1% 10% 50%
Ave
. A
nnua
l % C
hang
e
0%
5%
10%
15%
20%
25%
Acc
rua
l Pro
port
ion
vs. Accrual Proportion on National Treatment Trials, 1990-98
Slide courtesy of Archie Bleyer, MD

On Cooperative Group Trial
60%
2%
33% 29%
11%6%
60%
40%
50%10%
Age (Years)
0-4 5-9 10-14 15-19
Number of Patients
withCancerin the
US
Not at NCI-Sponsored Cooperative Group Institution
At Cooperative Group Institution;not on Cooperative Group Trial
20-30
The Adolescent-
Young Adult Gap
in Cancer Clinical Trials
79%
92%
21%
Sites of Care for Adolescents and Young Adults with Cancer
Bleyer et al, J Adolesc Health 1997; Albritton, Bleyer Eur J Cancer 2003

The Other Side of the Coin: Adult Protocols for “Adult Cancers”
Older adolescents with certain “adult-type” cancers may have better outcomes when treated by medical oncologists
Bleyer A, Pediatr Blood Cancer 2010; 54:238-41

WG3: Approach-1• Five Working Group conference calls
• Many emails
• Search strategy– Largely database- rather than literature-driven– Criteria
• AYA = 15-39 years old• Eligibility criteria inclusive of any AYA age segment• Focus on NCI-funded clinical trials and
mechanisms• Limited to North American experience

WG3: Approach-2• Trends in Clinical Trial Enrollment
– Seibel, Freyer, Friedman, Hunsberger, Lindwasser, Link
• Existing Mechanisms to Improve Accrual– O’Mara, Freyer, Seibel
• Inter-Group Clinical Trials and Initiatives to Improve Accrual– Indelicato, Chugh, Stock
• Clinical Trials Accrual: Barriers and Solutions– Chugh, Blanke, Tai
• Recommendations– Blanke and All

RFA-CA-12-010
COGSWOG

AYAO Participation on NCI Clinical Trials
Objectives:• To compare the number of newly diagnosed AYAO patients enrolled on cooperative groups trials with the population based incidence of the same types of cancer•To compare the relative accrual from academic and community-based sites on these same trials

Methods
Identified studies in the NCI portfolio that met the following criteria:•Newly diagnosed patients between the ages of 15 to 39 years of age•Open to enrollment during 2000-2010•Following disease typesNumber of AYA patients /total participants for disease; Compared to SEER 17 incidence

Clinical Trials Enrollment Project
Shanda FinneganSteve FriedmanSally HunsbergerDenise LewisWolf Lindwasser
Ann O’MaraTroy BuddPamela Maxwell

Clinical Trials Outcomes
Accrual of AYAs to NCI Cancer Trials (out of total accruals, all ages)
2000-2005•Highest enrollment for: Hodgkin , Bone , Cervix , AML , ALL
2006-2010•Highest enrollment for: Hodgkin , Bone (47%), Cervix, AML , ALL

CTSU Background and Objectives
• Established 1999• Primary Focus:
– Provide Centralized Operational Support Activities for NCI Cooperative Group Program
• Provide a wide choice of clinical trial options to the largest possible number of investigators
• Involve a larger number of treating institutions in the clinical trials process
• Increase enrollment to cancer clinical trials

CTSU Scope• Most Phase III treatment trials• Selected Phase II trials• Selected Division of Cancer Prevention Cancer
Control and Prevention Trials• Adolescent/Young Adult (AYA) Trial
collaborations with COG & Adult Groups– AEWS 1031 Ewings Sarcoma trial– Studies under development
• Newly diagnosed non-rhabdomyosarcoma (w/RTOG)• Desmoid (w/Alliance)

Community Clinical Oncology ProgramCCOP
What is a CCOP?
– A Group of Community Hospitals and Physicians
– Funded by a Peer Reviewed Cooperative Agreement
– To Participate In NCI-approved Cancer Prevention, Control, and Treatment Clinical Trials

CCOP Organizational Relationships
CCOPs & [MB-CCOPs]
Accrual to Protocols
Data Management
Quality Control
Research Bases
(Groups/Centers)
Develop Protocols
Data Management and Analysis
Quality Assurance
Members and Affiliates
Accrual to Prevention and Control Protocols

2013
(47)(16)
(395)

Intergroup Collaborations and Initiatives to Improve Accrual
Wendy Stock, MDRashmi Chugh, MD
Danny Indelicato, MD

• Intergroup collaboration will be emphasized as the NCTN evolves
Rationale:• Avoid redundant study objectives• Harmonize study objectives• Minimize redundant costs
• For AYA-based research, this provides a valuable opportunity to address one aspect of the clinical trial “gap”
• Clinical trial participation among oncology patients is valuable, yet accrual of patients age 15-39 to clinical trials is poor
• Reasons are multifactorial, but two barriers may be national availability and local access
Intergroup Collaboration

• C-10403: First US intergroup trial for AYA patients– New diagnosis, untreated, B and T-ALL– Ages 16-39– Completed accrual in September 2012 – 318 patients
enrolled; initial EFS results very promising but longer f/u needed (median survival not reached)
• Good accrual by all three US cooperative groups• Challenges:
– Major challenge: initiation of trial!• From time of initial discussions, more than 5 years before
final trial design and protocol written with approval of CTEP and all cooperative groups
Intergroup CollaborationExample: ALL

C-10403 Challenges/ Insights• Initial steep learning curve for treating teams
– Assessment and management of specific toxicities• Hepatic toxicities during induction, high rates of grades 3-4 hypersensitivity,
prolonged myelosuppression– Unique compliance, medication cost coverage, and psycho social
issues in AYA population – highlighted by patient surveys– Tremendous benefit to monthly (initially every two weeks!) phone
calls available to all investigators• Calls have continued through summer of 2013
• Accrual halted early on for change in protocol due to reports of toxicity from 0232– Switch dex to prednisone – Resulted in slowing of accrual in first year of trial and some loss of
momentum• Widespread efforts to publicize trial with highlights/posters at
cooperative group meetings, webinars, fliers, support in advertising trial by SigmaTau facilitated awareness– During course of trial, enrollment increased from 3-5 patients per
month to a steady rate of 7-9 patients in last 18 months of accrual

C-10403 Initial Attempt: A Success!
• Use of pediatric regimen feasible in the AYA population– Early EFS analysis suggests tremendous improvement in
outcomes (68% 2 year EFS) but longer f/u required• Toxicities not very different than matched population
in AALL0232 (to be presented at ASH 2013)• Enthusiasm, comfort level, commitment grew with
time• Fascinating insights emerging into differences in
disease biology– Slower initial response with more MRD after induction– High rates of activated kinase signature– Provides impetus and direction for the successor study

• COG AEWS0031 (2001-2005) • Randomized controlled trial of interval-compressed chemotherapy• Eligibility: any patient ≤50 years old with non-metastatic Ewing sarcoma
Intergroup Collaboration
Womer et al, JCO, 2012
• Only 12% were ≥18 years old• Limits investigators ability to ascertain
the cause(s)
• AEWS1031/RTOG1172 opened 2010• First COG trial endorsed by RTOG• First COG trial open through CTSU• Currently, 21% of patients are ≥18
years old
Example: Ewing Sarcoma

Intergroup CollaborationExample: Soft Tissue Sarcoma

• ARST1321-RTOG1313 Pazopanib Neoadjuvant Trial In Non-Rhabdomyosarcoma Soft Tissue Sarcomas (PAZNTIS): A Phase II/III Randomized Trial of Preoperative Chemoradiation or Preoperative Radiation Plus or Minus Pazopanib
Intergroup Collaboration
Hypotheses: 1. The addition of a multitargeted receptor tyrosine kinase inhibitor, pazopanib, to preoperative radiation is feasible and will improve pathologic response in adult and pediatric patients with newly diagnosed intermediate and high risk NRSTS
2. If sufficient pathologic necrosis is demonstrated, pazopanib will improve event-free survivalPALETTE results (Lancet 2012)
3-fold increase in PFS vs placebo
• Study will be offered through CTSU and any age STS patient will be eligible• Intended to accelerate and unify therapeutic research into this rare family of AYA tumors• Compliments efforts by Sarcoma Alliance for Research through Collaboration (SARC)
Example: Soft Tissue Sarcoma

Clinical Trials Enrollment: Barriers and Potential Solutions
Charles BlankeRashmi Chugh
Eric Tai
Next Steps in Adolescent and Young Adult OncologyWorking Group 3

Barriers: Location of TreatmentPediatric vs. Adult Hospitals
• More likely to enroll in studies at pediatric hospitals
• Pediatric hospitals more likely to have clinical trials available for typical AYA cancers
• Medical oncologists may not be aware of trials available at their counterpart pediatric hospitals
• Hospital age limits may hinder enrollment• Reimbursement/clinical trial credit for providers
enrolling on counterpart studies

Barriers: Location of TreatmentAcademic vs. Community Hospitals
• Older teens/younger adults more often treated in community– More convenient for most during time of life full of
critical daily life obligations
• Medical oncologists in community not be aware of trials available– May be reluctant to refer to not complicate life of pt
• Academic oncologists may not look beyond own institution for rare cancers

Barriers: Regulatory
• Separate IRBs at pediatric and adult institutions– More difficult to participate in cross-age studies
• Central IRBs – Still under-utilized but improving

Barriers: Logistics
• Limited trials available– $$$– Included diseases too rare
• Patients with psychosocial barriers• Poor consent readability• Low health literacy• Financial limitations

Barriers: AYAs AYA Decision-making to participate in trial
• Primary Factors affecting decision-making:– ?Direct treatment benefit– Perceived harm due to mistrust of researchers– Logistics
Barakat et al, 2013

• Ayas with cancer declining participation– 18% -Thought it would not help– 36% -Had too much else to think about– 45% -Added too much time– 18% -Added too much discomfort– 0% - too risky
Read et al, 2010
Barriers: AYAsAYA Decision-making to participate in trial

Learning from our Northern NeighborsThe Canadian Experience
• Similar obstacles:– Lack of centralized IRB– Lack of knowledge within local IRBs– Difficult requirements for CTAs– Resource limitations
• Plans to establish AYA Committee within NCIC-CTG

Potential Solutions
• Increased recognition of “AYAs” as specific entity– Patients unaware of this identifier, resources– Increase trial availability, funding, access– Utilize social media to disperse information
• Facebook• Mobile phone-based interventions• Virtual support group
– AYA specific clinics/interest groups/meetings

Potential Solutions
• Mandated use of Central IRB by participating institutions– Increase cross-age enrollment

Working Group 3 (Clinical Trials)
Recommendations
Charles D. Blanke, MD, FACP, FASCO
Chair, SWOG
Professor, Department of Medicine/Knight Cancer Institute, OHSU
Co-Chair, NSAYAO WG3
NSAYAO WorkshopNSAYAO WorkshopSeptember 16-17, 2013September 16-17, 2013

Improve Utilization, Data Collection, and Reporting
• Develop national mechanisms to capture # AYA pts with cancer
• Require NCI-funded organizations to report # AYA pts with cancer and capture reasons for non-participation in trials
• Develop mechanisms to capture AYA activity arising on pharma-sponsored oncology studies
• Develop disease-targeted efforts to increase accrual onto cooperative group studies

Optimize Existing Mechanisms to Enhance
Accrual• Expand CTSU use through operationalizing
the NCTN
• Encourage NCORP members to increase accrual– Increase awareness of trials– Resource community outreach– Provide institutional incentives

Expand Intergroup Research
• Strengthen collaboration of COG with adult Groups
• Modify COG and adult Group trial age eligibility • Co-develop intergroup studies of common AYA
cancers• Consider developing an AYA “Super-Committee”• Ensure AYA experts attend adult and pediatric
disease-focused Clinical Trials Planning Meetings

Lower Barriers to Trials Participation
• Increase use of Central IRB• Increase awareness among pts and allied health care
professionals– Have AYA presentations at national nursing, primary care
mtgs– Effectively utilize social media
• Decrease barriers in gettings pts to Specialty Centers– Identify/develop transportation options for isolated patients– But, have AYA Centers help develop local delivery of
sophisticated care and administration of trials

OPEN DISCUSSION
Related Documents