Web Annex C. Estimates of the coverage of diagnosis and treatment for hepatitis B and C virus infection, by WHO region and income group, 2015 Centre for Disease Analysis In: Global hepatitis report 2017

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Web Annex C. Estimates of the coverage of diagnosis
and treatment for hepatitis B and C virus infection, by
WHO region and income group, 2015
Centre for Disease Analysis
In: Global hepatitis report 2017

WHO/CDS/HIV/18.47
© World Health Organization 2018
Some rights reserved. This work is available under the Creative Commons AttributionNonCommercial-
ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo).
Under the terms of this l icence, you may copy, redistribute and adapt the work for non-commercial purposes,
provided the work is appropriately cited, as indicated below. In any use of this work, there should be no
suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not
permitted. If you adapt the work, then you must l icense your work under the same or equivalent Creative
Commons licence. If you create a translation of this work, you should add the following disclaimer along with
the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not
responsible for the content or accuracy of this translation. The original English edition shall be the binding and
authentic edition”.
Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization.
Suggested citation. Centre for Disease Analysis. Web Annex C. Estimates of the coverage of diagnosis and
treatment for hepatitis B and C virus infection, by WHO region and income group, 2015. In: Global hepatitis report 2017.Geneva: World Health Organization; 2018 (WHO/CDS/HIV/18.47). Licence: CC BY-NC-SA 3.0 IGO.
Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris.
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit
requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing.
General disclaimers. The designations employed and the presentation of the material in this publication do
not imply the expression of any opinion whatsoever on the part of WHO concerning the legal status of any
country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries.
Dotted and dashed lines on maps represent approximate border l ines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are
endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this publication.
However, the published material is being distributed without warranty of any kind, either expressed or
implied. The responsibility for the interpretation and use of the material l ies with the reader. In no event shall
WHO be liable for damages arising from its use.
This publication forms part of the WHO guideline entitled Global hepatitis report 2017. It is being made
publicly available as supplied by those responsible for its development for transparency purposes and information, as required by WHO (see the WHO handbook for guideline development, 2nd edition (2014)).
The named institution alone is responsible for the views expressed in this publication.

CONTENTS
1. Background
2. Methods
2.1 Country-level estimates
2.2 Extrapolations to generate regional estimates
2.3 Stratifications
2.4 Sensitivity analysis
3. Results
3.1 Cascade of care for HBV infection
3.2 Cascade of care for HCV infection
4. Discussion
5. Acknowledgements
6. Cascades
7. Tables
8. Figures
References

Page 1 of 21
ESTIMATES OF THE COVERAGE OF DIAGNOSIS AND TREATMENT FOR HBV
AND HCV INFECTION, BY WHO REGION AND INCOME GROUP, 2015
Online annex # 3 to the 2017 WHO Global Hepatitis Report on the cascade of care – Version: 20 April 2017
Report prepared by the Center for Disease Analysis for the World Health Organization
BACKGROUND
The global health sector strategy (GHSS) on viral hepatitis calls for elimination of viral hepatitis as a public
health threat by 2030 (reduction of 90% in incidence and of 65% in mortality). Chronic sequelae of HBV and
HCV infection account for 95% of the mortality from viral hepatitis [1]. The monitoring and evaluation
framework of the GHSS includes indicators for the five core interventions [2]. The four prevention
interventions are already implemented and data are available to monitor coverage. For testing and treatment,
data systems to generate information are not yet in place and estimates are not available to determine how
far the world is from the 2030 target. By 2030, the proportion of persons living with HBV or HCV who have
been diagnosed should reach 90% (30% in 2020), and among those diagnosed, 80% of eligible persons should
be treated (5 million for HBV and 3 million for HCV in 2020) [3].
The cascade of care concept originates from HIV and quantifies the series of steps that occur between testing
and the achievement of viral suppression or sustained virological response (SVR) [4]. The cascade of care for
HBV and HCV infection [5, 6] addresses diagnosis, treatment and viral suppression (for HBV) and eventual cure
(for HCV) [5, 7, 8]. Reports that address the cascade for HCV [9, 10 , 11, 12 , 13, 14] are mostly from high-
income countries. Monitoring the cascade facilitates the identification of gaps in access to and engagement in
care and treatment [15]. New direct-acting antivirals for HCV have already improved adherence and SVR rates.
Reports quantifying the cascade of care for HBV are also mostly from high-income countries [16–22]. Among
antinucleos(t)ides with a high barrier to resistance recommended by WHO for the treatment of chronic
hepatitis B, tenofovir has been the most widely used. With full adherence to antinucleos(t)ides with a high
barrier to resistance, viral suppression occurs at 48 weeks in 83–97% of patients. Disease progression stops in
patients who respond to treatment [23–26]. However, older therapies such as lamivudine are still in use, even
though they are not recommended by WHO as they induce resistances.
Before implementing the GHSS on viral hepatitis, a baseline quantification of the cascade of care for HBV and
HCV was necessary to (a) identify priorities for action, and (b) compare regions in terms of access to diagnosis
and treatment. We therefore abstracted the available data to estimate the number of patients infected with
HBV and HCV who were (a) diagnosed, (b) treated and (c) virologically suppressed or cured at the regional and
global levels, using 2015 as the reference year. WHO regions included the African Region, Region of the
Americas, Eastern Mediterranean Region, European Region, South-East Asia Region and Western Pacific
Region.

Page 2 of 21
METHODS
General approach
To estimate the indicators that reflect the cascade of care regionally and globally, we proceeded through four
steps (Fig. 1). First, we reviewed the data to estimate the indicators along the cascade by country. Second, we
compiled data from countries that had data available and extrapolated these results to generate regional and
global estimates. Third, we stratified results by WHO region and income level. Fourth, we calculated
uncertainty intervals around the estimates.
Operational definitions
We estimated the indicators selected by WHO to quantify the various steps of the cascade of care [2].
Proportion of infected persons diagnosed (WHO core indicator C6)
We defined persons diagnosed (C.6) as persons living with chronic HBV (C.6.a) or HCV (C.6.b) infection who
had been diagnosed through in vitro diagnostic methods. The proportion of diagnosed individuals was
calculated as the number of persons with chronic infection diagnosed out of the total number of persons with
chronic infection.
Treatment coverage (HBV) or initiation (HCV, WHO core indicator C7)
For HBV, we defined persons on treatment (C.7.a) as persons living with chronic HBV infection who were on
treatment in 2015. For HCV, we defined persons initiating treatment (C.7.b) as persons living with chronic HCV
infection who started any HCV antiviral treatment (including direct-acting antiviral regimens and non-direct-
acting antiviral regimens) in the past 12 months. We calculated the treatment initiation rate for 2015 as the
number of persons initiating treatment during that year out of the total number diagnosed.
Viral suppression (HBV) or sustained virological response (HCV, WHO core indicator C8)
For HBV, we defined the proportion of persons virally suppressed (for C.8.a) as the number of persons with
undetectable HBV DNA in the past 12 months out of the number of persons on HBV treatment in the past 12
months who were tested. For HCV, we defined the proportion of cure (for C.8.b.) as the number of persons
with documented SVR out of the number of persons initiating treatment (within the past 12 months).
Time period
We estimated cascade indicators for the year 2015. Our literature search considered available published
studies and ministry of health reports between January 1990 and November 2016 (HBV), and published studies
and national databases between January 1950 and March 2016 (HCV).
Geographical scope
We considered all countries for the development of our global and regional cascade of care estimates. We
included countries with prevalence data, as well as those without prevalence data but with a population of 1
million or more (HBV) and 1.5 million or more (HCV).

Page 3 of 21
1. Country-level estimates
Number of infected persons
We used the 2015 WHO estimates of the total number of persons infected with HBV and HCV. The estimates
for HBV were generated by the London School of Hygiene &Tropical Medicine for the WHO department of
Immunization, Vaccines and Biologicals. The estimates for HCV were generated by the Center for Disease
Analysis for the WHO Global Hepatitis Programme.
Proportion of infected persons diagnosed (WHO core indicator C6)
HBV
Methods to estimate the size of the population diagnosed included (in order of priority): (a) national
notification or registry data; (b) studies that included estimates or data on the number of persons known to be
living with HBV in a country and published in the peer-reviewed literature; (c) the number of people found to
be infected through blood donation screening programmes; (d) extrapolations from other countries in the
same region.
HCV
In countries where notifications led to a reliable number of newly diagnosed infections, we added all
notifications by year and subtracted mortality. In countries without surveillance data, we used national reports
or expert panel input (in that order). We also considered blood donor data (when available), under the
assumption that the total number of diagnosed patients would at a minimum include those testing positive at
a blood transfusion centre. We assumed that the proportion of anti-HCV-positive persons with viraemia was
identical among persons diagnosed and in the total infected population, and that the newly diagnosed cases
remained constant after the last reporting.
Treatment coverage (HBV) or initiation (HCV) (WHO core indicator C7)
HBV
We estimated the number of individuals treated annually for HBV through (in order of priority): (a) national
databases or government reports; (b) sales audit data of generic tenofovir; (c) published data on the number
of treated patients in the country; or (d) estimates provided by national experts. To use medicine sales audit
data, we converted the annual number of units of treatment sold into the number of treated patients using
the average number of units per patient.
HCV
We estimated the number of individuals initiating treatment for HCV each year through (in order of priority):
(a) national databases or government reports; (b) medicine sales audit data; (c) publications or reports from
major treatment centres; or (d) estimates provided by experts. We considered all therapies available in 2015,
including older regimens containing interferon as well as newer direct-acting antiviral combinations (with or
without ribavirin). To use medicine sales audit data, we converted the annual number of units of each

Page 4 of 21
treatment sold into the number of treated patients using the average number of units per patient. To estimate
the average number of units per patient, we considered several factors that affect the speed and probability of
achieving an SVR, particularly when patients are treated with pegylated interferon. As the average SVR varies
by genotype, we considered the genotype distribution and the duration of treatment by genotype. We also
included the number of treatment units used per week and the proportion of treatment effectively completed.
We further adjusted the annual number of units to account for uses other than for treatment of HCV and for
any underreporting, using inputs from the expert panel in each country when possible. When reports from
individual treatment centres were used, experts provided input on the number and size of other treatment
centres in the country so that the numbers could be extrapolated to determine a countrywide estimate. We
assumed the annual number of patients initiating treatment was constant after the last year of reported data.
Projected treatment effectiveness (WHO core indicator C8)
HBV
We assumed that with full adherence to treatment, viral suppression would occur in 90% of individuals with
chronic hepatitis B [23, 27]. Assuming that 80% of those undergoing treatment were adherent, we assumed
that globally, 72% had effective viral suppression [16, 28–32].
HCV
We used the proportion of treated patients with SVR by genotype to estimate the number of patients with SVR
per year. In the absence of better information, we assumed that the genotype distribution of the treated
population was the same as the one of the total infected population. We interviewed national experts to
estimate the actual proportion of SVR for the different treatment regimens (with or without direct-acting
antivirals). Experts took into consideration the proportion of patients with prior treatment experience, disease
stage and reduced compliance.
2. Extrapolations to generate regional and global estimates
We estimated the proportion of patients diagnosed and treated for the Global Burden of Disease (GBD)
regions, weighted by the sizes of the populations infected and diagnosed, respectively. We used GBD regional
diagnosis and treatment estimates for countries without estimates. If a GBD region did not have any countries
with data, we used the weighted average of neighbouring GBD regions as a surrogate. All GBD regions were
then added to generate a global estimate.
3. Stratifications
We stratified our outputs based on the six WHO-defined regions and four World Bank income groups.
4. Uncertainty analysis
We conducted a sensitivity analysis and developed 95% uncertainty intervals (UI) for our regional and global
outcomes. To this effect, we ran a Monte Carlo analysis that turned off and on the inclusion of each country in
the regional and global estimates. After completing the Monte Carlo analysis, we used the resulting
uncertainty ranges by country to calculate the regional and global levels. This allowed us to determine the

Page 5 of 21
impact of including each country’s forecast in the regional cascade of care estimate, which in turn estimated
the numbers diagnosed, treated and suppressed/cured for all countries with missing data in the same region.
We conducted these analyses using Crystal Ball®, an Excel® add-in by Oracle® with a binomial distribution to
include or exclude countries [33].
RESULTS
Cascade of care for HBV infection (see Cascade 1)
Data availability
Data on diagnosis were available for 163 countries (94% of the population) with 46% coming from blood donor
data, 31% from registries or published data, 10% from WHO registries (particularly in the European Region and
Western Pacific Region), and 7% utilizing a combination of registry and blood donor data (Fig. 2). Data on
diagnosis accounted for >99% of the population in the Western Pacific, European and American regions. The
South-East Asia Region (94% of the population with data on diagnosis, 98% of which was from blood donations)
and African Region (85% of the population with data on diagnosis, 91% from blood donor donations) had
intermediate data availability. The Eastern Mediterranean Region had the lowest proportion of the population
with data on diagnosis (69%, with 71% of the information coming from blood donations).
Treatment data were available for 59 countries, representing 43% of the global population, ranging from 90%
in the South-East Asia Region to 10% in the European Region. In all but six countries, we used sales data of
generic tenofovir to estimate the number of treated patients. In New Zealand, Poland, Slovakia and Viet Nam,
experts estimated the total number of those treated. These estimates include non-tenofovir treatments. For
Greece and China, previously published estimates were utilized and also include non-tenofovir treatments [19,
34].
No data were available regarding treatment in the Andean Latin America, Southern Latin America and tropical
Latin America; nor were they available for the high-income Asia Pacific subregions. The weighted average of
the proportion treated in a neighbouring region was extrapolated and applied. Sufficient diagnosis and
treatment data for inclusion were available for countries in all the other subregions.
Diagnosis of chronic HBV infection
Overall, in 2015, of the 257 million persons with HBV infection, we estimated that 21 million persons (95% UI:
20–22 million, 9% of the infected population) had been diagnosed (Table 1). The proportion of those infected
who were diagnosed was highest in the Western Pacific Region (25%, 17 million diagnosed) and lowest in the
African Region (0.3%, 153 000 diagnosed). The highest number of diagnosed individuals was in the upper–
middle-income group (2 million, with the lowest in the low-income group, with 312 000 diagnosed. Upper–
middle-income countries also had the highest proportion diagnosed (18.7%), while low-income countries had
the lowest (0.8%).

Page 6 of 21
Treatment coverage for chronic HBV infection
Overall, in 2015, 1.7 million (95% UI: 1.5–1.7 million) persons (8% of those diagnosed) were on treatment for
chronic hepatitis B (Table 1). This proportion varied from 0.5% to 18% by region. Treatment coverage was the
highest in high-income countries (14%) and the lowest in lower–middle-income countries (3%).
Projected viral suppression for chronic HBV infection
Of the 1.7 million on treatment in 2015, an estimated 1.2 million individuals (95% UI: 1.2–1.6 million) achieved
viral suppression globally.
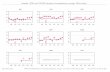
Sensitivity analysis
Globally, 97% of the variation in the total number diagnosed was due to the Western Pacific, South-East Asia
and European regions, with 75% being due to the Western Pacific Region alone. With respect to treatment, 76%
of the variation in the total number treated was due to the Western Pacific Region, followed by the European
and South-East Asia regions, which together account for 94% of the variation (Fig. 4).
Cascade of care for HCV (see Cascade 2)
Data availability
Expert panels approved estimates of the HCV cascade in 59 countries. Published and unpublished data were
available for another 41 countries. For 74 countries (79% of the world population), we estimated the number
of patients diagnosed through expert consensus (39 countries, 36% of the population), published studies (10
countries, 8% of the population) and surveillance (25 countries, 35% of the population, Fig. 3). Surveillance
accounted for >50% of the population in the Region of the Americas and Western Pacific Region (Fig. 3).
We were able to estimate the number of patients with hepatitis C treated in 76 countries (81% of the global
population) through the use of expert consensus (29 countries, 16% of the population), published studies (6
countries, 3% of the population), medicine sales audit data (34 countries, 41% of the population) and
surveillance (7 countries, 22% of the population, Fig. 3). In two regions (Eastern Mediterranean and European),
more than 50% of estimates came from medicine sales audit data or national treatment databases (5% of the
population). National treatment databases were available in the European and the Western Pacific regions (Fig.
3).
Three GBD regions (Latin America, Andean; Oceania; sub-Saharan Africa, central) lacked country data for
diagnosis and two (Oceania; sub-Saharan Africa, central) lacked country data for treatment and SVR. We
estimated the data for the Andean Latin America region using the population-weighted averages from Latin
America, central/southern/tropical; sub-Saharan Africa, central was estimated using the population-weighted
average from sub-Saharan Africa, east/south/west; and Oceania was assumed to have the same proportion
diagnosed and treated as Australasia.

Page 7 of 21
Diagnosis of chronic HCV infection
Of the 71 million persons with chronic HCV infection in 2015, 20% (95% UI: 19–21%) had been diagnosed (14
million, 95% UI: 13–15, Table 2). The European Region had the largest total diagnosed population (4.3 million)
and the African Region had the smallest (582 000). The Region of the Americas had the highest proportion of
infected persons diagnosed (36%). The high-income group had the largest number of persons diagnosed (6
million, 43% of all). In the high-income group, 46% of infections were diagnosed, compared with 17% in the
upper–middle-income and 14% in the lower–middle-income groups.
Treatment initiation rate for chronic HCV infection
In 2015, of 14 million diagnosed with HCV infection, an estimated 7% (95% UI: 7–8%) initiated treatment in
2015 (1 million, 95% UI: 1.0–1.1, Table 2). The Eastern Mediterranean Region had the largest number of
persons initiating treatment (326 000) and the highest treatment initiation rate (12%), followed by the Region
of the Americas (11%). The high-income group accounted for the largest number of patients initiating
treatment (483 000), followed by the lower–middle-income group (398 000). Globally, a cumulative 5 million
persons (95% UI: 5.4–5.6) have initiated treatment since 2004.
Projected sustained virological response for HCV infection
The SVR among patients treated in 2015 was 80% overall (95%UI: 76–82%), highest in the Region of the
Americas (88%) and lowest in the Western Pacific Region (63%, Table 2). The high-income group had the
highest SVR (88%) and the upper–middle-income group the lowest (62%).
Sensitivity analysis
For the proportion diagnosed, the European, South-East Asia and African regions accounted for 95% of
variation (Fig. 5). The Western Pacific and Eastern Mediterranean regions accounted for less than 1% of
individuals diagnosed globally. By income, the lower–middle-income and lower-income groups accounted for
approximately 95% of uncertainty. For treatment initiation rate, the European, Eastern Mediterranean and
South-East Asia regions accounted for more than 98% of variation (Fig. 5). The Region of the Americas and
Western Pacific Region accounted for less than 1% of treatment initiation globally. By income, the lower–
middle-income and upper–middle-income groups accounted for 99% of uncertainty. Lower–middle-income
countries alone accounted for about 94% of the uncertainty. For SVR, the European, Eastern Mediterranean
and South-East Asia regions accounted for 95% of variation (Fig. 5). The American and Western Pacific regions
accounted for less than 1% of variation. By income, the lower–middle-income and upper–middle-income
groups accounted for 99% of uncertainty.
DISCUSSION
Globally, we estimated that in 2015, 9% of the 257 million infected with HBV had been diagnosed, a 21% gap
from the GHSS 2020 target of 30%. With widespread diagnosis campaigns documented with registries, the
Region of the Americas, European and Western Pacific regions could meet the 2020 target for diagnosis.
However, given the difficulties in documentation in the African, Eastern Mediterranean and South-East Asia

Page 8 of 21
regions, meeting the 2020 and 2030 targets would be difficult, even with a massive increase in the number of
individuals diagnosed. Registries often suffer from limitations. They do not operate at the national level, do
not differentiate between acute and chronic cases, and exclude the private sector. In addition, a registry would
need to link diagnosis to treatment and continue follow up for patients not yet eligible for treatment until they
are suppressed. With regard to treatment, in 2015, we estimated that 1.7 million individuals (8% of those
diagnosed) were being treated (34% of the 5 million targeted to be on treatment by 2020). However, given the
absence of population-based estimates of the proportion of infected individuals eligible for treatment [35, 36],
it is difficult to determine how far the world is from the 2020 target [16]. As treatment is limited by the
number of individuals diagnosed, the regions that will require the largest scale up of diagnosis will also require
large scale up of treatment. Thus, the African, Eastern Mediterranean and South-East Asia regions have the
greatest need for focused strategies to diagnose and treat chronic HBV. The Western Pacific Region has made
progress in diagnosis, but needs to follow up diagnosis with treatment.
Globally, we estimated that in 2015, 20% of the 71 million infected with HCV had been diagnosed. This
presents a 10% gap from the 30% targeted for 2020. However, the degree of effort necessary to achieve these
targets varies by region. In the African Region, only 6% of HCV infections are diagnosed. Laboratory facilities
equipped to test for HCV are sparse in the Region, and many countries send specimens abroad for testing. This
is both expensive and inefficient for large-scale screening programmes. Although the proportion diagnosed
varies by WHO region, it varies even more by income group. The high-income group has already achieved or
exceeded the 2020 targets. Lack of quality data in low-income and lower–middle-income groups may explain
the variation by income group. While the low-income group had the smallest number of data sources for those
diagnosed, the lower–middle-income group accounted for the largest variation in diagnosis estimates due to
the limited sources available for a large number of included countries. With respect to treatment, worldwide in
2015, 7.4% of diagnosed patients initiated any kind of treatment. Given the 2020 GHSS target for treatment (3
million people have received treatment) [3], these results suggest that at a global level, diagnosis and
treatment must be scaled up. Cumulatively, an estimated 5.5 million patients initiated treatment between
2004 and 2015, which means that 20% of these patients were treated in 2015 alone. In the low-income group,
this proportion was much higher at 88% due to emerging treatment efforts in the African Region where 81% of
patients who cumulatively initiated treatment since 2004 did so in 2015. Overall, 80% of those who started
treatment in 2015 were cured. This proportion of those cured is expected to continue to rise as countries
switch to direct-acting antiviral therapies. Although we are unable to provide quantifiable estimates of
patients treated by therapy type at a regional level, approximately 50% of patients treated globally in 2015 and
approximately 10–15% of the cumulative number of patients treated globally from 2004 to 2015 were treated
with direct-acting antivirals. The annual proportion of cure reflects the uptake of direct-acting antiviral
therapies across regions, as well as the change in treatment over time. More than 80% of treated patients
were cured in the Region of the Americas, African, Eastern Mediterranean and South-East Asia regions, while
less than 80% were cured among those treated in the Western Pacific and European regions. The high
proportion of cure in the Region of the Americas (88%) is largely due to access to direct-acting antivirals in the

Page 9 of 21
USA and Brazil, which account for a majority of treatment in the Region. The scarcity of data and small number
of treated patients in the African Region may indicate that prior to the launch of direct-acting antivirals, there
was very little treatment available in that Region. Variations in treatment onset rates and cure rates by income
group highlighted the need for expanded treatment and improved access to direct-acting antivirals in middle-
income and low-income countries.
These estimates suffer from a number of limitations. First, the number of individuals diagnosed may have been
underestimated. Underreporting may occur in public health-care facilities. Some countries do not include data
from the private sector. Second, the number of patients treated could be overestimates. For HBV, in 53
countries with available data, we estimated the number of individuals on treatment based on generic
tenofovir sales. In low-income countries that account for the largest proportion of infected persons and where
most of the tenofovir used is from generic manufacturers, this may have led to an overestimation of treatment
coverage, as some tenofovir could have been used for the prevention or treatment of HIV infection. In contrast,
in upper–middle-income and high-income countries, data on the sales of generic tenofovir may not represent
all the sales of tenofovir, which could have led to an underestimation of the number on treatment. In addition,
we were not able to capture the use of other types of treatment that are not recommended by WHO, such as
lamivudine. Use of these treatments can lead to resistance and wastage of resources. As a consequence of
these limitations of the treatment data for HBV, WHO decided not to consider the regional breakdown in the
indicator reflecting treatment coverage for HBV (Core indicator C.7.a) but only the global aggregated data. For
HCV, we were unable to provide specific estimates of breakdown according to the type of treatment, such as
the use of interferon-based regimens versus direct-acting antivirals. Where the exact proportion of patients
treated with direct-acting antivirals was available in a country, it was reflected in the average SVR by genotype,
as described above. Third, our data on viral suppression for HBV and SVR for HCV were not based on national
systems to monitor patients from diagnosis through evaluation of treatment effectiveness. Instead, we used
multiple sources to project an estimate of the viral suppression or SVR indirectly, through published studies of
the efficacy and observance that can be expected (HBV) or in-country expert opinions based on their own case
series (HCV). Finally, as the situation is developing fast, 2015 estimates reflected a situation that has evolved
substantially since. Unfortunately, as of March 2017, 2016 estimates were not yet available for all countries,
even though preliminary data suggest that there is increasing availability of direct-acting antivirals in many
countries, and that the number of patients treated is increasing [37]. For example, Egypt started 500 000
patients on treatment in the first nine months of 2016 (an increase from October 2014 to December 2015
when 170 000 patients were treated) [37]. These patients are not reflected in these 2015 estimates. The
recent WHO report on access to hepatitis C treatment suggests that 1 million patients have been treated with
direct-acting antivirals since these drugs were first released in 2014 [37]. This is generally compatible with our
estimate that half a million patients were treated in 2015, with between 550 000 and 825 000 patients treated
with direct-acting antivirals in 2014 and 2015 combined. However, once we include data from 2016, our
estimates are likely to exceed 1.1 million treated with direct-acting antivirals between 2014 and 2016.

Page 10 of 21
In conclusion, in 2015, some information is available to provide initial baseline estimates of the cascade of care.
Only 9% and 20% of those with chronic HBV and HCV infection, respectively, have been diagnosed. Of those
infected with HBV, 8% are on treatment. Of those infected with HCV, 7% initiated treatment in 2015. Based on
what is known of the effectiveness of these treatments, we estimate that the majority of those treated are
virally supressed (in the case of HBV) or cured (in the case of HCV). However, most countries do not monitor
the effectiveness of treatment. To achieve the GHSS impact targets of reduced mortality and incidence, scaling
up testing and treatment will be necessary in all regions. In some cases, a switch is needed from older and less
safe therapies such as lamivudine for HBV and pegylated interferon for HCV, and further research required to
develop therapies for chronic HBV infection that would lead to a functional cure. A test-and-treat policy may
avoid post-diagnosis attrition in the future as it is estimated that up to 30% of people who are not eligible
when they are first diagnosed will become treatment eligible within three years [38]. Despite the availability of
surveillance systems and registries in many countries, more work is needed to identify best practices that lead
to improved accuracy and reliability of data systems to monitor the cascade of care. The implementation of
patient registries, especially in the African and South-East Asia regions, will be a necessary consideration in the
development of national strategies as countries move toward eliminating HBV and HCV. In the absence of such
registries, countries may want to consider other mechanisms that will provide preliminary estimates of the
indicators that reflect the cascade of care. Finally, to document SVR or viral suppression, effective systems of
follow up to assess and document the effectiveness of treatment are needed in order to replace estimates
with empirical data collected in-country.
ACKNOWLEDGEMENTS
We would like to acknowledge the 400+ country collaborators who provided and analysed data, participated in
meetings, provided guidance on methodology, and/or critically reviewed the model.
Country-level analyses were funded by industry research grants, the John C. Martin Foundation, and/or the
World Health Organization regional offices through the Center for Disease Analysis and the Polaris Observatory.
The development of WHO regional estimates, and the analysis to ensure adherence to the Guidelines for
Accurate and Transparent Health Estimates Reporting (GATHER) process were funded by the World Health
Organization through the Polaris Observatory.
The unit data for medicine sales audit data were reported by QuintilesIMS, which is a vendor of de-identified
prescription sales data.

Page 11 of 21
CASCADES
Cascade 1. HBV cascade of care estimates by WHO region, 2015

Page 12 of 21
Cascade 2. HCV cascade of care estimates by WHO region, 2015

Page 13 of 21
TABLES
Table 1. HBV cascade of care estimates by WHO region and income categories, 2015
Region
Chronic HBV infections
Total number (000) Diagnosed (000) Treated (000) Viral suppression (000)
Best estimate Range Best estimate Range
C.6.
Proportion
of infection
diagnosed Best
estimate * Range *
C.7.
Proportion
of
diagnosed
treated *
Best
estimate Range
WH
O r
egi
on
African 60 000 45 000–84 000 153 110–200 0.3% (28) (19–30) (18.4%) 20 20–27
The Americas 7 000 4 000–16 000 669 589–743 9.6% (110) (94–125) (16.4%) 79 79–107
Eastern Mediterranean 21 000 17 000–28 000 351 173–486 1.7% (2) (0.6–2) (0.5%) 1 1–2
European 15 000 11 000–23 000 1 965 1 728–2 218 13.1% (98) (52–98) (5.0%) 71 70–95
South-East Asia 39 000 29 000–77 000 888 848–1 552 2.6% (55) (48–78) (6.2%) 40 39–53
Western Pacific 115 000 93 000–160 000 17 484 15 975–17 621 2.3% (1 382) (1 290–1 395) (7.9%) 995 986–1 340
Wo
rld
Ban
k
inco
me
gro
up
High 10 000 8 000–15 000 1 874 1 664–2 375 18.7% (255) (189–256) (13.6%) 184 182-249
Upper–middle 119 000 95 000–153 000 16 132 15 452–16 295 13.5% (1 334) (1 269–1 333) (8.3%) 961 948-1 295
Lower–middle 87 000 67 000–133 000 3 195 2 265–3 920 3.7% (85) (52–118) (2.7%) 61 61-83
Low 40 000 30 000–66 000 312 273–333 0.8% (28) (27–29) (8.9%) 20 20-27
Global 257 000 199 000–367 000 21 513 19 887–22 285 8.4% (1 702) (1 537–1 703) (7.9%) 1,226 1 196–1 624
* Given the limitations of the estimates of HBV treatment, WHO decided not to use the estimates at the regional level but to only use the worldwide, aggregated estimates

Page 14 of 21
Table 2. HCV cascade of care estimates by WHO region and income categories, 2015
Region
Total
cases
(000)
Diagnosed Treatment initiation (annual) Cumulative number of
persons started on
treatment (000)
Sustained virological response (annual)
Total number (000) Proportion (%) Number (000) Rate (%) Number (000) SVR (%)
Best
estimate Range
Best
estimate Range
Best
estimate Range
Best
estimate Range
Best
estimate Range
Best
estimate Range
Best
estimate Range
WH
O r
egi
on
African 10 284 582 399–718 5.7 3.9–7.0 13 315 2.2 0.6–3.0 16 6–17 11 2–13 84.6 48.3–87.6
The Americas 7 237 2 625 2 446–2 707 36.3 33.8–37.4 290 286–290 11.1 10.7–11.8 1 252 1 248–1 251 255 253–255 87.9 87.7–88.2
Eastern Mediterranean 15 190 2 686 2 644–2 732 17.7 17.4–18.0 326 302–331 12.1 11.2 –12.4 1 576 1 553–1 581 264 242–269 81.1 79.5–81.5
European 13 641 4 250 3 443–4 735 31.2 25.2–34.7 208 186–302 4.9 4.2–7.2 1 157 1 136–1 251 162 156–207 77.9 62.1–85.0
South-East Asia 10 391 906 627–1 016 8.7 6.0–9.8 64 45–69 7.1 4.9–8.4 235 216–240 54 41–55 84.0 79.8–90.5
Western Pacific 13 898 2 985 2 815–2 998 21.5 20.3–21.6 144 141–145 4.8 4.7–5.0 1 169 1 166–1 171 91 88–92 63.1 62.6–63.4
Non-WHO 506 221 221–223 43.8 43.7–44.0 8 8–8 3.8 3.7–3.8 90 90–90 6 6–6 69.9 69.0–70.1
Wo
rld
Ban
k
inco
me
gro
up
High 13 499 6 242 6 169–6 257 46.2 45.7–46.4 483 479–483 7.7 7.7–7.8 2 650 2 647–2 650 423 420–423 87.6 87.6–87.7
Upper–middle 18 439 3 053 2 885–3 139 16.6 15.6–17.0 164 148–176 5.4 4.9–5.9 1 060 1 044–1 072 101 88–109 61.7 55.7–63.9
Lower–middle 33 341 4 599 3 792–4 913 13.8 11.4–14.7 398 354–461 8.7 7.7–10.6 1 776 1 732–1 839 313 284–350 78.7 69.8–82.0
Low 5 846 357 182–445 6.1 3.1–7.6 7 1–9 2.1 0.2–3.2 8 1–9 4.7 0.3–5.7 64.7 41.6–85.9
Other 20 4.4 1.8–5.0 21.5 8.6–24.5 0.3 0.0–0.4 7.7 2.1–17.2 0.3 0.0–0.4 0.3 0.0–0.3 86.0 55.1–89.9
Global 71 146 14 255 13 166–14 638 20.0 18.5–20.6 1 053 987–1 116 7.4 7.0–8.1 5 495 5 429–5 558 843 795–886 80.0 75.6 - 81.6

Page 15 of 21
FIGURES
Fig. 1. Conceptual framework to extrapolate country-level estimates to regions for the cascade of care for HBV and HCV infection
Estimated Disease Burden ModelsStrong input data that have not yet
been approved by countries(N=41)
Compilation of country modelsModels underwent a second
independent review and were compiled for analysis
(N=100)
Cascade of Care Database2015 diagnosed, treated and cured
were extracted from models and analyzed to generate regional
estimates
Cascade of Care DatabaseGBD regional cascade of care
estimates were used as surrogates for countries without models
Approved Disease Burden ModelsModels that have been approved by
local expert panels(N=59)
PubMed + EmbasePrevalenceGenotype
Age distributionRisk factors
Grey LiteratureMOH, UN databasesTreatment databasesTransplant databases
Diagnosed
HCV Disease Burden ModelCountry models were developed
using input from the literature
Global EstimatesCascade indicators for all countries were compiled and divided by the global population to estimate the
global cascade of care
Stratification by WHO and WB region Data were stratified by WHO region
and World Bank Income Group
Syst
emat
ic
Sear
chN
atio
nal
m
od
els
Ext
rap
ola
tio
ns
to g
ener
ate
reg
ion
al e
stim
ate
s
In c
oun
try
revi
ew
Co
un
try-
leve
l E
stim
ates
GB
D re
gio
nal
est
imat
es fo
r co
un
trie
s w
ith
dat
a
Str
ati
fica
tio
ns
GB
D e
xtra
po
lati
on
s to
co
un
trie
s w
itho
ut
dat
a an
d d
evel
op
men
t o
f gl
ob
al e
stim
ates
Sensitivity and Uncertainty AnalysisSensitivity and uncertainty analysis were conducted to generate 95%
uncertainty intervalsUn
cert
ain
ty

Page 16 of 21
Fig. 2. Data available on diagnosis and treatment of HBV infection, by region, adjusted for population size, 2015
AFR: African Region; AMR: Region of the Americas; EMR: Eastern Mediterranean Region; EUR: European Region; SEAR: South-East Asia Region; and WPR: Western Pacific
Region.

Page 17 of 21
Fig. 3. Data available on diagnosis and treatment of HCV infection, by region, adjusted for population sizes
AFR: African Region; AMR: Region of the Americas; EMR: Eastern Mediterranean Region; EUR: European Region; SEAR: South-East Asia Region; and WPR: Western Pacific
Region.
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
AMR (989 million)
AFR (1,000 million)
EMR (654 million)
EUR (914 million)
SEAR (1,945 million)
WPR (1,867 million)
Non-WHO (25 million)
High (1,408 million)
Upper middle (2,393 million)
Lower middle (2,946 million)
Low (644 million)
Other (3 million)
Global (7,394 million)
WH
O R
eg
ion
WB
Inco
me
Gro
up
Diagnosis data distribution, by region (Regional population)
No Data Expert Consensus Published Study National Surveillance
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
AMR (989 million)
AFR (1,000 million)
EMR (654 million)
EUR (914 million)
SEAR (1,945 million)
WPR (1,867 million)
Non-WHO (25 million)
High (1,408 million)
Upper middle (2,393 million)
Lower middle (2,946 million)
Low (644 million)
Other (3 million)
Global (7,394 million)
WH
O R
eg
ion
WB
Inco
me
Gro
up
Treatment data distribution, by region (Regional population)
No Data Expert Consensus Published Study IMS data National Surveillance

Page 18 of 21
Fig. 4. Sensitivity analysis to estimate the impact of regional uncertainties on the global cascade of care for HBV infection, by region, 2015
AFRO: Regional office for the African Region; AMRO: Regional office for the Region of the Americas; EMRO: Regional office for the Eastern Mediterranean Region; EURO:
Regional office for the European Region; SEARO: Regional office for the South-East Asia Region; and WPRO: Regional office for the Western Pacific Region.

Page 19 of 21
Fig. 5. Sensitivity analysis to estimate the impact of regional uncertainties on the global cascade of care for HCV infection, 2015
AFR: African Region; AMR: Region of the Americas; EMR: Eastern Mediterranean Region; EUR: European Region; SEAR: South-East Asia Region; and WPR: Western Pacific
Region.
WH
O R
eg
ion
WB
Inc
om
e G
rou
p
Total Diagnosed Patients Cured, 2015Initiating Treatment, 2015
102%
101%
101%
100%
100%
100%
97%
99%
99%
99%
99%
100%
95% 100% 105%
EUR
SEAR
AFR
AMR
WPR
EMR
102%
100%
100%
100%
97%
99%
99%
100%
95% 100% 105%
Lower middle income
Low income
Upper middle income
High income
104%
100%
100%
100%
100%
100%
98%
99%
99%
99%
100%
100%
95% 100% 105%
EUR
EMR
SEAR
AFR
AMR
WPR
103%
101%
100%
100%
97%
99%
100%
100%
95% 100% 105%
Lower middle income
Upper middle income
Low income
High income
103%
100%
100%
100%
100%
100%
100%
99%
99%
99%
100%
100%
95% 100% 105%
EUR
EMR
SEAR
AFR
AMR
WPR
103%
101%
100%
100%
98%
99%
100%
100%
95% 100% 105%
Lower middle income
Upper middle income
Low income
High income

Page 20 of 21
Reference List
1. Stanaway, J.D., et al., The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet, 2016.
2. WHO, Monitoring and Evaluation for Viral Hepatitis B and C: Recommended Indicators and Framework, in Technical Report. 2016, World Health Organization: http://apps.who.int/iris/bitstream/10665/204790/1/9789241510288_eng.pdf. p. 17.
3. Assembly, W.H.O.S.-N.W.H., Global Health Sector Strategies Viral Hepatitis 2016-2021, W.H. Organization, Editor. 2016.
4. Gardner, E.M., et al., The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis, 2011. 52(6): p. 793-800.
5. Linas, B.P., et al., The hepatitis C cascade of care: identifying priorities to improve clinical outcomes. PLoS One, 2014. 9(5): p. e97317.
6. Holmberg, S.D., et al., Hepatitis C in the United States. N Engl J Med, 2013. 368(20): p. 1859-61. 7. Assoumou, S.A., et al., Relationship between hepatitis C clinical testing site and linkage to care. Open
Forum Infect Dis, 2014. 1(1): p. ofu009. 8. Aghemo, A. and S. De Nicola, [Chronic hepatitis C: standard of care and perspective]. Recenti Prog
Med, 2016. 107(7): p. 349-54. 9. Cachay, E.R., et al., The hepatitis C cascade of care among HIV infected patients: a call to address
ongoing barriers to care. PLoS One, 2014. 9(7): p. e102883. 10. Geboy, A., et al., Hepatitis C virus birth cohort testing and linkage to care (HepTLC) in a large
Washington DC medical center. Hepatology, 2013. 58(4): p. 1290A. 11. Hawks, L., et al., The Hepatitis C virus treatment cascade at an urban postincarceration transitions
clinic. J Viral Hepat, 2016. 23(6): p. 473-8. 12. Maier, M.M., et al., Cascade of Care for Hepatitis C Virus Infection Within the US Veterans Health
Administration. Am J Public Health, 2016. 106(2): p. 353-8. 13. Norton, B.L., et al., No Differences in Achieving Hepatitis C Virus Care Milestones Between Patients
Identified by Birth Cohort or Risk-Based Screening. Clin Gastroenterol Hepatol, 2016. 14(9): p. 1356-60.
14. Rodriguez-Diaz, C.E., et al., Health care practices and associated service needs in a sample of HIV-positive incarcerated men in Puerto Rico: implications for retention in care. J Int Assoc Provid AIDS Care, 2014. 13(6): p. 492-6.
15. Janjua, N.Z., et al., The Population Level Cascade of Care for Hepatitis C in British Columbia, Canada: The BC Hepatitis Testers Cohort (BC-HTC). EBioMedicine, 2016. 12: p. 189-195.
16. Lemoine, M., et al., Acceptability and feasibility of a screen-and-treat programme for hepatitis B virus infection in The Gambia: the Prevention of Liver Fibrosis and Cancer in Africa (PROLIFICA) study. Lancet Glob Health, 2016. 4(8): p. e559-67.
17. Allard, N.L., J.H. MacLachlan, and B.C. Cowie, The cascade of care for Australians living with chronic hepatitis B: measuring access to diagnosis, management and treatment. Aust N Z J Public Health, 2015. 39(3): p. 255-9.
18. Byrne, D.D., et al., Prevalence of diagnosed chronic hepatitis B infection among U.S. Medicaid enrollees, 2000-2007. Ann Epidemiol, 2014. 24(6): p. 418-23.
19. Papatheodoridis, G., et al., Estimating the treatment cascade of chronic hepatitis B and C in Greece using a telephone survey. J Viral Hepat, 2015. 22(4): p. 409-15.
20. Cohen C., H.S., McMahon BJ., BLock JM., Brosgart CL., Gish RG., London WT., Block TM., Is chronic hepatitis B being undertreated in the United States? J Viral Hepat., 2011. 18(6): p. 377-83.
21. Shankar, H., et al., Novel community-based hepatitis B and C screening program among African immigrants with linkage to care by a culturally-targeted patient navigator. Hepatology, 2013. 58(4): p. 613A-614A.
22. Papatheodoridis, G., et al., Addressing barriers to the prevention, diagnosis and treatment of hepatitis B and C in the face of persisting fiscal constraints in Europe: report from a high level conference. J Viral Hepat, 2016. 23 Suppl 1: p. 1-12.
23. Marcellin, P., et al., Tenofovir disoproxil fumarate versus adefovir dipivoxil for chronic hepatitis B. N Engl J Med, 2008. 359(23): p. 2442-55.
24. Lok, A.S., et al., Antiviral therapy for chronic hepatitis B viral infection in adults: A systematic review and meta-analysis. Hepatology, 2016. 63(1): p. 284-306.

Page 21 of 21
25. Zoulim, F., F. Lebosse, and M. Levrero, Current treatments for chronic hepatitis B virus infections. Curr Opin Virol, 2016. 18: p. 109-16.
26. Terrault, N.A., et al., AASLD guidelines for treatment of chronic hepatitis B. Hepatology, 2016. 63(1): p. 261-83.
27. Marcellin, P., et al., Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study. Lancet, 2013. 381(9865): p. 468-75.
28. Allard, N., et al., Factors associated with poor adherence to antiviral treatment for hepatitis B. J Viral Hepat, 2017. 24(1): p. 53-58.
29. Romero Diaz-Maroto, V., et al., [Adherence to entecavir for chronic hepatitis B and correlation with effectiveness]. Farm Hosp, 2015. 39(6): p. 378-81.
30. van Vlerken, L.G., et al., Real life adherence of chronic hepatitis B patients to entecavir treatment. Dig Liver Dis, 2015. 47(7): p. 577-83.
31. Wojcik, K., A. Piekarska, and E. Jablonowska, Adherence to antiviral therapy in HIV or HBV-infected patients. Przegl Epidemiol, 2016. 70(1): p. 27-32, 115-8.
32. Ha, N.B., et al., Treatment Outcomes With First-line Therapies With Entecavir and Tenofovir in Treatment-Naive Chronic Hepatitis B Patients in a Routine Clinical Practice. J Clin Gastroenterol, 2016. 50(2): p. 169-74.
33. Malcolm, D.G., et al., Application of a Technique for Research and Development Program Evaluation. Operations Research, 1959. 7(5): p. 646-669.
34. hepatitis, C.i.c.i., Hepatitis in China: Disease Burden and Economic Analysis. 2016: STAC Hepatitis WPRO, Viet Nam.
35. Toy, M., et al., The cost-effectiveness of treating chronic hepatitis B patients in a median endemic and middle income country. Eur J Health Econ, 2012. 13(5): p. 663-76.
36. in Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. 2015: Geneva.
37. Organization, W.H. Global report on access to hepatitis C treatment. Focus on overcoming barriers. 2016 [cited 2016; Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R6-en.pdf.
38. Nguyen, N.H., et al., Treatment eligibility of patients with chronic hepatitis B initially ineligible for therapy. Clin Gastroenterol Hepatol, 2013. 11(5): p. 565-71.
Related Documents