Michigan Medicine Quality Improvement Continuity of Care in Stroke Patient Discharge Current State Analysis and Recommendations December 12, 2017 To: Jenevra Foley, Operations Director, Comprehensive Stroke Center, [email protected] Alison Spork, Senior Project Manager, Physical Medicine & Rehabilitation, [email protected] Mark Van Oyen, IOE 481 Professor, [email protected] Mary Duck, Industrial Engineering Expert, [email protected] From: IOE 481 Project Team #8 Christopher Cardoso, IOE 481 Student, [email protected] Joshua Johnston, IOE 481 Student, [email protected] Catherine Samuel, IOE 481 Student, [email protected]

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Michigan Medicine Quality Improvement
Continuity of Care in Stroke Patient Discharge
Current State Analysis and Recommendations
December 12, 2017
To:
Jenevra Foley, Operations Director, Comprehensive Stroke Center, [email protected] Spork, Senior Project Manager, Physical Medicine & Rehabilitation, [email protected] Van Oyen, IOE 481 Professor, [email protected] Duck, Industrial Engineering Expert, [email protected] From:
IOE 481 Project Team #8Christopher Cardoso, IOE 481 Student, [email protected] Johnston, IOE 481 Student, [email protected] Samuel, IOE 481 Student, [email protected]

Table of Contents
EXECUTIVE SUMMARY 1Background 1Key Issues 1Methodology 1
Interviews 1Data Collection 2Data Analysis 2
Summary Statistics 2Current State Flow Map 2
Findings and Conclusions 2Opportunity to Increase Transparency 2Some Aspects of the Process Are Out of the Hospital's Control 3Data Findings for Waiting Times in Process 3Need for Additional Data and Consistency in Data Collection 3
Recommendations 3Future Recommendations 3
INTRODUCTION 1
BACKGROUND 4
KEY ISSUES 5
GOALS AND OBJECTIVES 5
PROJECT SCOPE 6
DATA AND METHODS 6Design Methods, Constraints, and Standards 6Data Collection 6Literature Search 7Interviews 7Data Analysis 8Current State Flow Process Maps with Data 8
FINDINGS AND CONCLUSIONS 9Opportunity to Increase Transparency 11Some Aspects of the Process Are Out of the Hospital's Control 12Quantitative analysis of Discharge/Admission Process Timing Shows High Variability 10Opportunities for Streamlined Data Tracking 12Findings from Literature Provided Context 13
ii

RECOMMENDATIONS 13Immediate Recommendations 13
1. Implement Excel data collection tool for use by stakeholders 132. Use metrics to benchmark process timing and improve performance 133. Improve communication with pages at key decision points. 14
Future Recommendations 141. Create additional Excel tool that can pull data from MiChart reports 142. Use Time Studies to validate in process times. 143. Use additional data collected to complete a full six-sigma analysis 14
EXPECTED IMPACT 15
REFERENCES 16
APPENDIX A: Design Documentation 17Constraints 17Standards 17
APPENDIX B: Current State Process Map and A3 Documentation 20
APPENDIX C: Results from Data Analysis 26
APPENDIX D: Work Instructions for Excel Tool 35
iii

List of Tables and Figures
Table 1: Summary Statistics of Individual Steps in Discharge/Admission Process 8
Table 2: Median and Standard Deviation for Highly Variable Process Data Points 10
Table A-1: Constraints and Standards Matrix 18
Figure 1: Distribution of timing from Stroke Admission to IRF Admission 11
Figure B-1: 4A to IRF Admission Process Flowchart using data without outliers 20
Figure B-2: Orders/Consults Current State Process Flowchart using data without outliers
21
Figure B-3: Insurance Approval Current State Process Flowchart using data without outliers
22
Figure B-4: Transfer from 4A to IRF Current State Process Map with Data using data without outliers
23
Figure B-5: Key to the 4A to IRF Admission Process Flowchart 24
Figure B-6: Project A3 Document 25
Figure C-1: Distribution of Timing from Stroke Admission to PT/OT Order 26
Figure C-2: Distribution of Timing from Stroke Admission to PT/OT Order with Outliers
26
Figure C-3: Distribution of Timing from PT/OT Order to PT Note 27
Figure C-4: Distribution of Timing from PT/OT Order to PT Note with Outliers 27
Figure C-5: Distribution of Timing from PT/OT Order to OT Note 28
Figure C-6: Distribution of Timing from PT/OT Order to OT Note with Outliers 28
Figure C-7: Distribution of Timing from PT Note to PM&R Order 29
Figure C-8: Distribution of Timing from OT Note to PM&R Order 29
Figure C-9: Distribution of Timing from PM&R Consult to PM&R Note 30
Figure C-10: Distribution of Timing from PM&R Consult to PM&R Note with 30
iv

Outliers
Figure C-11: Distribution of Timing from Being Added to Potential Admit List to Insurance
31
Figure C-12: Distribution of Timing from Insurance Verification to Insurance Approval
31
Figure C-13: Distribution of Timing from PM&R Note to Discharge Order 32
Figure C-14: Distribution of Timing from PM&R Note to Discharge Order with Outliers
32
Figure C-15: Distribution of Timing from 4A Discharge Order to Actual 4A Discharge
33
Figure C-16: Distribution of Timing from 4A Discharge Order to Actual 4A Discharge with Outliers
33
Figure C-17: Distribution of Timing from Actual 4A Discharge to 6A Admission 34
Figure D-1: Excel Tool Work Instructions for Order Sheet 35
Figure D-2: Excel Tool Work Instructions for Summary Sheet 36
v

EXECUTIVE SUMMARY
Michigan Medicine’s Comprehensive Stroke Center treats approximately 700 stroke patients every year [1]. A vast majority of these stroke patients are housed in the Neurology unit (4A). A subset of the stroke population in 4A moves to the Inpatient Rehabilitation Facility (IRF) after their time in 4A is complete, and there is currently a perception that this process takes too long. Therefore, the Comprehensive Stroke Center and the IRF have requested that an IOE 481 student team analyze the process to identify bottlenecks and develop metrics that the units can use to track performance. Through interviews with stakeholders and data analysis regarding timestamp data, the student team created a current state flow map with recommendations for increased communication. Lastly, the team has created recommendations for future analysis and data collection.
Background
This project is a continuation of work that was completed by another IOE 481 student team in the Winter of 2017. The previous students analyzed the current state of the process at a high-level in order to gain an understanding of where future studies should focus their efforts [2]. With an average of ~89% capacity in the stroke unit and 90+% occupancy in the IRF [3], there is pressure on both ends of the process to manage throughput as efficiently as possible. For this project, the student team has taken a deeper look at the discharge/admission process to make recommendations for improvement.
Key Issues
The following key issues are driving the need for this project:● Discharge/admission process between 4A and IRF is complex and not readily visual● Data collection is not currently a standardized process
Methodology
The student team used the following methods throughout the project.
InterviewsThe team conducted 8 interviews of key stakeholders, including the IRF Admissions Coordinator, the 4A Case Manager, a doctor in the Stroke Unit, a Speech Language Pathologist, a Physical Therapist, a doctor in the IRF, a Stroke Unit nurse, and the Insurance Coordinator in the IRF. These interviews were integral for developing a thorough understanding of the current state of the discharge/admission process and helped the team begin to understand the current state of how units communicate with each other.

Data CollectionThe team used two major data collection sources. The first source is from the IRF admissions coordinator, which includes timestamp information for 20 patients between February 2017 - October 2017 regarding each step in the IRF admissions process. The second collection source was manually pulled via MiChart, where the team collected timestamp data for 40 patients between January 2017 - November 2017 regarding each step in the 4A discharge process.
Data AnalysisThe team analyzed the collected data in order to generate summary statistics and create a process flow diagram.
Summary Statistics
Information from both interviews and data collection in MiChart was used to generate summary statistics for the steps within the discharge/admission process. Using timestamps from the collected data, the team calculated the time between process steps, and used this to generate summary statistics regarding the mean, median, standard deviation, 80th percentile, minimum, and maximum, as well as create box plots to better understand the distributions. These figures can be found in Appendix C.
Current State Flow Map
Using the interviews from eight key stakeholders in the process, the team generated a current state process flow map of the discharge/admission process. The map separates the process into three major sections: Orders/Consults, Insurance Verification and Approval, and Admission to IRF. The whole process map and each individual section can be seen in Appendix B. All available data used to generate summary statistics was added to the current state flow map to better quantify the length of the process. For more information, the current state flow map can be found in Appendix B.
Findings and Conclusions
Using the methods outlined above, the team was able to draw the following conclusions.
Opportunity to Increase TransparencyThrough interviewing stakeholders, it became evident that stakeholders were unaware of the complex steps involved in the admission/discharge process, and that there are opportunities to improve communication between the 4A Case Manager and the IRF Utilization Review Coordinator. The team worked to mitigate these issues by creating a Current State Flow Map, which will help stakeholders better understand the overall process, as well as recommendations for standardized communication between unit 4A and the IRF, to reduce communication barriers between units. The map can be found in Appendix B.
2

Some Aspects of the Process Are Out of the Hospital's ControlTwo of the largest barriers for a smooth and timely transition from 4A to the IRF are insurance approval and high bed demand. There are 32 beds available and the hospital is not able to control the strong demand. These are the major bottlenecks that were identified in the discharge/admission process.
Data Findings for Waiting Times in ProcessWith the data that the student team was able to extract from MiChart, many different metrics were developed. These metrics were then analyzed using statistical analysis to determine a quantitative average state. With this data the team created box plots to show the spread and variation of the data. The team also created an Excel tool that will standardize data collection by automatically generating timestamps. The 4A Case Manager, the IRF Admissions Coordinator, and the IRF Utilization Review Coordinator will no longer use manual data entry, which will standardize format and therefore assist stakeholders in future reporting and analysis.
Need for Additional Data and Consistency in Data CollectionIn order to conduct a more thorough analysis of the process, more data will be required. While the team was able to pull enough data points for each statistic to meet hospital standards for statistical significance, much of the data that the team was presented with was either invalid, incomplete, or considered an extreme outlier when compared to the other values.
Recommendations
The team has made the following recommendations for improving the discharge/admission process.
Immediate Recommendations1. Implement Excel data collection tool to assist 4A Case Manager, IRF Admissions Coordinator, and IRF Utilization Review Coordinator with data collection and analysis2. Use determined data metrics to create benchmarks for process timing that stakeholders can use to improve performance3. Improve communication by sending pages at key decision points to the 4A Case Manager denoted on the current state process map in Appendix B
Future Recommendations1. Create additional Excel tool that can pull data from MiChart reports to remove the need for manual data collection2. Conduct Time Studies to validate the in-process times for each step3. Use additional data collected to complete a full six-sigma analysis on the process
3

INTRODUCTION
Michigan Medicine’s Comprehensive Stroke Center treats approximately 700 stroke patients every year [1], many of which begin their stay at the hospital in the Neurology Unit (4A). After stroke patients receive the care they need, there are a variety of pathways for patients to continue their care, including admission to Michigan Medicine’s Inpatient Rehabilitation Facility (IRF). Currently, there is a perception that patients are waiting in 4A longer than necessary while tasks that allow their discharge to the IRF are being completed. This perception is due to a disconnect in communication and knowledge of the process among stakeholders. There is also limited data regarding the time it takes to perform the activities required before a patient can be discharged from 4A or admitted to the IRF. Consequently, the 4A and IRF units requested a team of IOE 481 students to analyze the process of discharge from 4A to the admission into IRF. This information was then used to identify and document the bottlenecks in the patient discharge process, as well as develop metrics that the units can use to track their performance. The team has also created a tool to help stakeholders track the amount of time they take in a uniform way and made recommendations to increase communication in the future. The purpose of this report is to document the work completed by the team as well as the expected outcomes of that work.
BACKGROUND
This project is a continuation of work that was completed by another IOE 481 student team in the Winter of 2017. The previous students generated a high-level process map and A3 documents in order to gain an understanding of where future studies should focus their efforts [2]. For this project, the student team will be focusing on discharge from 4A to an admission to the IRF on a much deeper-level. This newfound information will be added to the previous project’s existingA3 document. After a patient is deemed appropriate for acute rehabilitation by the Physical Medicine and Rehabilitation (PM&R) consult physician, several steps must occur before that patient can be discharged and admitted to the IRF. First, the 4A case manager must be notified of the patient’s planned disposition so that appropriate discharge planning can take place. The IRF Admissions Coordinator must also be notified to initiate the admissions process, which involved several sequential processes. For example, proper insurance benefits must be verified, and the admission must be authorized by the insurer, which requires that specific documentation from the patient's stay on 4A is complete and available. Currently there is a perception of breakdowns in the communication between 4A and the IRF, and unnecessary delays. This leads to stakeholders believing that patients staying in 4A for extended periods of time while they wait for their discharge to the IRF. With an average of ~89% capacity filled in the stroke unit and 90+% occupancy in the IRF [3], there is pressure on both ends of the process to manage throughput as efficiently as possible. Currently there are no standard metrics that are tracked in this process to determine current performance. In addition, there are no tools to assist in data tracking and analysis.
4

KEY ISSUES
The following key issues are driving the need for this project:● Inadequate levels of transparency in the discharge/admission process between 4A and the
IRF○ There is a perception that the process takes too long○ Current communication practices leave some stakeholders with insufficient
information● Opportunities for standardized data collection
○ Data is being collected for most of the steps in the process, but it is manually inputted and there is an opportunity for human error
GOALS AND OBJECTIVES
In order to best increase transparency regarding this process, the team was tasked with the following goals:
● Interview stakeholders involved in the process of discharging a patient from 4A and admitting to the IRF
● Analyze collected timestamp data for the discharge/admission process
With this collected information, the team delivered the following objectives:● Recommended trackable quality metrics
○ Metrics will be selected by prioritizing their urgency based on high variability and importance to stakeholders
● Developed an Excel tool that standardizes data collection● Created a detailed current state process map that lays out each step in the
discharge/admission process to improve transparency○ Data will be added to this where possible
● Added details to existing A3 diagram that documents the current state of the dischargeprocess
● Generated recommendations for future communication between stakeholders in the process
● Identify bottlenecks in the discharge/admission process that may be causing unnecessarily long wait times
PROJECT SCOPE
5

Because of the complexity of this process, there was a need to define a project scope as shown below.
In ScopeThe project scope includes the time at which a patient is admitted to 4A with a stroke until the patient arrives in an IRF bed.
Out of ScopeAny clinical decision or treatment planning completed in 4A and IRF are excluded from the scope of this project. In addition, any patients who get discharged from any other Michigan Medicine unit and home is outside of scope. Lastly, this project is focused only on ischemic stroke patients.
DATA AND METHODS
In order to complete the goals of the project, the team has worked to analyze the qualitative and quantitative information that has been provided through interviews and from MiChart data. The analysis has been used to create the process flow map that will be used in to increase transparency of the current process.
Design Methods, Constraints, and StandardsA primary deliverable of the project is to give the stakeholders a better idea of the process a patient goes through from 4A to the IRF unit. The team has achieved this through the use of the engineering design process. The constraints and standards are located in Appendix A - Design Documentation to further explain the team’s key considerations when designing our final deliverables.
Data CollectionTo determine timing information between each step in the process, the team concluded that data collected directly from the hospital is the best method. Completing time studies to collect this information proved to be an inferior method because the process happens sporadically, and the team wished to use previous data in order to gather large enough sample sizes for a robust data analysis. Therefore, the team used two main avenues for data collection: information collected by the IRF Utilization Review Coordinator and MiChart timestamps. The information provided by the IRF Utilization Review Coordinator included timestamps for when patients were placed on the potential admit list, insurance verification, insurance approval, able to admit notification, and actual admit time. The data provided on this set was directly related to the insurance verification and approval as well as actual admission to the IRF. The data however did not explain much about the orders and consults side of the discharge/admission process. Therefore, timestamp data was pulled either manually in MiChart or through MiChart Reports for physical
6

therapist (PT) and occupational therapist (OT) order, PM&R order, PT Note, OT note, PM&R Note, discharge order, and official discharge time.
Literature SearchThe student team conducted a literature search to see if there were already any healthcare standards or best practices regarding the quality metrics and data collection. The team researched a study that discussed the realization of the leadership of the Mayo Clinic Outpatient Procedures Department that their current performance indicators were almost exclusively financial [4]. While this worked during the early years of the clinic to make sure that they were meeting their KPIs, it was now time to improve. These current metrics were not working for them because while they explained the outcome of the process of the department, they did not track performance from within different stages of the process. One of the major notes of the article was the importance of determining the method by which the data is analyzed. In general, the article spoke to the importance of integrating data collection into the major information systems used by the institution in order to make it simple and efficient for stakeholders.
A second article discussed how lean-six sigma methodologies could be applied to hospital discharge times. This article explains that in the prior state of the American University of Beirut Medical Center, the discharge times were too long [5]. The study was used to determine if six sigma methodologies could be applied to a hospital discharge. Many of the methodologies included in the article included the use of a variety of summary statistics to track performance. A few useful statistics included the use of means, medians, and standard deviations, as well as the use of box plots to represent distributions. In addition, the literature noted that sample sizes of size 30 are required in order for a sample to be statistically significant.
InterviewsIn order to create the current state process map for the discharge/admission process, the student team has interviewed eight stakeholders directly related in the discharge process: the IRF Admissions Coordinator, the 4A Case Manager, a doctor in the Stroke Unit, a Speech Language Pathologist, a Physical Therapist, a PM&R doctor, a Stroke Unit nurse, and the Insurance Coordinator in the IRF.
The student team asked interviewees questions relating to their job function and the role they played in the overall discharge/admission process. While the list of questions for each interviewee was customized for the individual, typical questions that were asked included: “please describe your job function and responsibilities within the scope of the stroke unit,” “is there a standard that is used for this process,” and “please describe your job function and responsibilities within the scope of the stroke unit.”
7

Data AnalysisIn addition to the interviews, the team has obtained data regarding the timing for each step in the process from a data set collected by the IRF Utilization Review Coordinator, as well as information that the team has pulled manually from MiChart, and through MiChart reports. This dataset has a timestamp that was collected by staff in the IRF regarding the time that each step is completed. This dataset includes patient information for 44 patients between January 2017 - November 2017.
Information from both interviews and data collection was used to generate summary statistics for the steps within the discharge/admission process. First, using timestamps from the collected data, the team calculated the time between process steps. Then the team, using data collected through interviews, determined how much of the time in between process steps was spent completing each task. Lastly, the team generated summary statistics of mean, median, standard deviation, 80th percentile, minimum, and maximum, and box plots were created to better understand the distributions. Table 1 shows an overview of the statistics that the team was able to generate from the collected data.
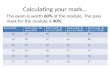
Table 1: Summary Statistics of Individual Steps in Discharge/Admission ProcessMiChart, 1/2/17 - 11/08/2017
Current State Flow Process Maps with DataUsing the interviews from eight key stakeholders in the process, the team generated a process flow map of the discharge/admission process. The process map provides an overview of what happens when a neurology doctor orders a consult for the PT and OT, to the time that a patient sits in their bed in the IRF.
Currently, there exists a process map which was created by the previous IOE 481 team. A deliverable of this team has been to identify areas on the previous map that can be expanded in order to further increase transparency in the process. The interviews have identified that the insurance verification and approval process had the most room for expansion. Through information gathered from the IRF Admissions Coordinator, and IRF Utilization Review Coordinator, the steps in the process were determined and then added to the final map.
8

After, additional steps gathered from interviews regarding the Orders and Consults and IRF Admission were added to the process map. Then, once all steps were added, the team worked to quantify the time that each step took from estimates provided by stakeholders, and from the data analysis. The team was only able to assign numerical time values to the steps in the patient transfer process due to a lack of quantitative information regarding the insurance verification and approval process. Given that the most robust data was available for orders/consults and admission to IRF, that data was added to the current state flow map. This diagram can be seen in Appendix B.
FINDINGS AND CONCLUSIONS
Using the methods explained above, the team was able to draw the following conclusions. These conclusions show where current gaps in the discharge/admission process exist and where potential for future improvements may lie.
Preliminary Consult Team InterviewAll stroke patients who enter the 4A receive physical therapy (PT) and occupational therapy (OT). These physicians are the ones who make the initial recommendation for PM&R consults to the 4A physician. The PTs and OTs cannot put in a request for a PM&R consult, but the 4A doctors use those recommendations to decide if they should request the consult. Once contacted, the PM&R physician determines the ultimate candidacy of the patient. The preliminary consult team (PT, OT, doctor and PM&R physician) is relatively unaware of the steps in the process that come after the PM&R consult.
IRF Admissions Coordinator InterviewAfter interviewing the IRF Admissions coordinator, they noted that once the PM&R physician determines if a patient is a candidate for the IRF, they generate an “encounter” in MiChart which indicates a new hospital stay. Once the “encounter” has been created, the IRF Admissions coordinator notifies the business office to verify insurance benefits and the IRF Utilization Review coordinator for insurance verification. Once insurance has been approved, the IRF Admissions Coordinator places the candidate in a bed based on their diagnosis, length of stay, gender and overall room availability. In the current state, this person must track all steps in the process using manual data collection.
IRF Utilization Review Coordinator InterviewThe IRF Utilization Review Coordinator will receive notification from the IRF Admissions Coordinator to begin their insurance verification process. First, they confirm whether or not the patient is InterQual qualified. This is required by insurance agencies to determine whether or not
9

a patient can withstand intensive rehabilitation. Approximately 85% of patients pass the InterQual review. The remaining 15% that fail are sent through a secondary review process with the IRF Medical Director. Out of all the data the team collected in the past year, only one patient failed the secondary review.
The team also learned that the approval times vary greatly for different insurance companies. At this time, timestamp data regarding individual steps are not tracked.
4A Case Manager InterviewThe 4A Case Manager is in charge of overseeing the process for the patient. They mentioned that they were not satisfied with the amount of communication they receive from other people in the process. It is difficult to track the process of a patient when not receiving any updates. The team has decided to indicate three stages in the process map where the 4A Case Manager will receive updates on their patient. These can be seen in green shapes in Figure B-3. The selected stages are the InterQual review results, the secondary review (if applicable) and the bed availability once approved.
Quantitative Analysis of Discharge/Admission Process Timing Shows High VariabilityWith the data that the team extracted from MiChart, and the timestamps from data collected by the IRF Admissions Coordinator, many different metrics were studied. These metrics were then analyzed in order to determine basic statistics associated with each stage in the process. After analysis, the most highly variable steps in the process were determined to be the Stroke Admission to PT/OT Order, PT/OT Order to PT Note, PT/OT Order to OT Note, and PM&R Consult to PM&R Note. The medians and standard deviations for these step timings is shown in Table 2 below.
Table 2: Median and Standard Deviation for Highly Variable Process Data Points
Process Step Median Standard Deviation
Stroke admission to PT/OT Order 0:04:33 1:03:47
PT/OT Order to PT Note 1:16:14 3:04:53
PT/OT Order to OT Note 2:17:06 3:17:01
PM&R Consult to PM&R Note 1:08:13 4:01:38
Figure 1 represents the time between admission to the hospital to IRF arrival. The findings from this data assisted the team in creating the process flow diagram. Please see Appendix C for similar graphs representing each of the times between stages in the process.
10

Figure 1: Distribution of timing from Stroke Admission to IRF AdmissionMiChart, 1/2/17 - 11/08/2017, n=36
Opportunity to Increase TransparencyA common theme throughout the team’s interviews was that individuals in the discharge/admission process understood their responsibilities and contributions to the process well, but did not understand all of the parts associated with the process and could not identify many stakeholders involved in processes outside of their respective unit (4A or IRF).
The previous IOE 481 student team created a map that provided a high-level understanding of the steps within the process. With this map, the team looked for ways to expand upon the previous student team’s map in order to increase transparency. The clearest opportunity to expand the map was through the insurance verification and approval process. Given that the team detected that this was a major bottleneck in the process, the team believed it would be useful to explain everything involved to better depict the process as a whole. The detail of the insurance verification and approval process can be found in Appendix B.
Through interviews, it was noticed by the team that there were opportunities for more standardized communication to improve transparency. After speaking with the 4A Case Manager regarding the information required to complete work regarding discharge planning, it appears that there are three key decision points in the insurance approval and verification process where pages regarding patient status would benefit transparency among units. These points include status updates regarding InterQual review, secondary review, and IRF bed availability.
Using the new current state process map, the team developed and A3 document to show the current state process, background, objectives, findings and recommendations. This document is in Appendix B, Figure B-6.
11

Some Aspects of the Process Are Out of the Hospital's ControlTwo of the largest bottlenecks that cannot be controlled by the hospital are insurance approval and bed demand in the IRF, which has been determined through data analysis as well as interviews. The team determined that insurance approval is a large bottleneck since on average it takes 13:23 hrs. to complete, and unfortunately, this process of approval is done externally through the individual insurance agencies and therefore there is little the hospital can do to shorten this timing. Additionally, bed demand at the IRF is high, which the hospital cannot unfortunately control. With 32 beds, there are challenges that the IRF faces to make beds available to the demanded population. Without a bed available to a 4A patient, not much can be done to expedite the process of admitting a 4A patient into the IRF. Opportunities for Streamlined Data Tracking The team has identified that, in order to conduct a six-sigma analysis, more data will be required. The team determined that the root causes of missing data are empty or incorrectly formatted entries, which the team saw as an opportunity to implementing a streamlined process that accurately captures timing data. Currently data is either captured using MiChart, or manually in Excel. To streamline manual collection, the team used VBA Macros in Excel to create a button that generates a timestamp when clicked. The goal of this tool is to make it easier for stakeholders to input data while eliminating human error.
The current Excel tool helps track six highly variable steps within the discharge/admission process. These steps are: Hospital Admission to PT/OT Order, PT/OT Order to PT Note, PT/OT Order to OT Note, PM&R Order to PM&R Note, Addition of Patient to IRF Potential Admit List to Insurance Verification, Insurance Verification to Insurance Approval. For each tracked step, summary statistics regarding average, standard deviation, maximum, minimum, and the amount of entries above and below the average are shown. In addition, boxplots are created for each step in order to best summarize the distributions of the data. As a result, this will assist with further analysis as it will provide an updated picture of current operations, and assist with root cause analysis as outliers will be easily identified. Given that these steps in the process are most actively viewed by the 4A Case Manager, the IRF Admissions Coordinator, and IRF Utilization Review Coordinator, the team believes that these stakeholders will be the best resource for tracking.
To avoid manual data collection in the future, the team recognizes that there is an opportunity to use more of MiChart’s reporting capabilities with Excel. MiChart contains a variety of data, most of which can be pulled from the system using reports. Being able to create a tool that uses the data available in MiChart to pull timestamp information into Excel will further automate the data collection, which will help prevent stakeholders from completing extra tasks.
12

Findings from Literature Provided ContextThe student team gained valuable insight on healthcare optimization from the literature search, most of the information presented in the sources provided context for our analysis. With regard to completing an entire six sigma analysis, the team realized that this was infeasible due to the sample sizes and currently collected data. However, the literature search provided context regarding information systems and their use to track data metrics, which has assisted in the creation of some of our recommendations.
RECOMMENDATIONS
The following section contains the immediate and future recommendations to improve the 4A discharge to IRF admission process. These recommendations are based on quantitative data and qualitative findings.
Immediate Recommendations
1. Implement Excel data collection tool for use by stakeholdersTo assist with current data collection, the team has designed an Excel tool that will automatically generate timestamps by clicking a VBA Macro button for certain steps within the discharge/admission process. The team recommends that the 4A Case Manager, IRF Admissions Coordinator, and the IRF Utilization Review Coordinator use this tool to generate timestamps. Therefore, we recommend training for the use of this tool, as well as systems be put in place to analyze and report this data, in order to best use the tool’s functionality.
2. Use metrics to benchmark process timing and improve performanceThe team has determined that the most useful information to be tracked are the Stroke Admission to PT/OT Order, PT/OT Order to PT Note, PT/OT Order to OT Note, PM&R Consult to PM&R Note, Addition of Patient to Admit List to Insurance Verification, and Insurance Verification to Insurance Approval. These metrics have been determined due high variation, and urgency based on stakeholder interviews. These metrics have been integrated into the Excel data collection tool, which will help consistently benchmark the performance of these steps within the process. Showing the shortest, longest, and average time tasks take to complete can help provide stakeholders with goals that can be used to improve performance. If all stakeholders can work to these goals, then any additional decrease in process time will compound among stakeholders to significantly reduce total time within the discharge/admission process. In addition, currently updated data points will provide stakeholders with an
13

opportunity to determine the root cause of any outliers in data, and work towards improving each case individually in real time.
3. Improve communication with pages at key decision points.To improve discharge planning and increase transparency, the team has indicated three main decision points where the IRF should page the 4A Case Manager. These points include the status regarding InterQual review, secondary review, and bed availability. This information flow will allow the 4A Case Manager to better communicate patient status with stakeholders in 4A and patients in order to improve the patient experience.
Future Recommendations
1. Create additional Excel tool that can pull data from MiChart reportsCurrently, MiChart has a variety of data that can be accessed through reports. There are opportunities to integrate this data with Excel in order to best report available data. Being able to create a tool that directly pulls timestamp information from MiChart reports will further automate the data collection, which will help prevent stakeholders from completing extra tasks. We recommend using MiChart specialists to understand how data for steps in the process is reported, and use Excel tools such as VBA Macros to integrate this information into a spreadsheet that can assist with data analysis.
2. Use Time Studies to validate in process times.Each stakeholder within the discharge/admission process has a rough idea of how long their step in the process takes. These perceived times have been placed into the current state process map in order to more accurately represent the process. There is an opportunity to make this map more robust by completing time studies to validate these in process times to get a better picture of exactly how long each step takes.
3. Use additional data collected to complete a full six-sigma analysisBy collecting more data, there are opportunities to complete a full six-sigma analysis on the current state of the discharge/admission process. Larger sample sizes will help provide a better understanding of the current state, and flag areas that require significant improvement.
EXPECTED IMPACT
The team has identified and mapped out the entire process that a patient goes through from the 4A stroke unit to the IRF. Using this process and the associated data, the team has developed a
14

method to track the amount of time it takes for different steps in the future. The impact of this project is summarized below with their corresponding issue:
● Discharge/admission process between 4A and IRF is complex and not readily visual○ Creation of In Depth Process Map○ Identification of Bottlenecks○ Recommendations for better communication practices
● Data collection for bottlenecks is not currently standardized ○ Development of Quality Metrics○ Building of Excel Tool
15

REFERENCES
[1] Foley, Jenevra and Alison Spork. Personal Interview. 2017.
[2] Farmer, William, et al. Improving the Discharge and Post-Discharge Process Flow. 2017.
[3] Roberts, Jessica and Alison Spork. Personal Interview. 2017.
[4] Curtwright, J., Stolp-Smith, S. and Edell, E. (2000). Strategic Performance Management: Development of a Performance Measurement System at the Mayo Clinic. [online] Biomedsearch.com. Available at: http://www.biomedsearch.com/article/Strategic-Performance-Management-Development-Measurement/61837280.html [Accessed 22 Oct. 2017].
[5] El-Eid, Ghada R. et al. "Improving Hospital Discharge Time". Medicine 94.12 (2015): 1-8. Web. 30 Oct. 2017.
16

APPENDIX A: Design Documentation
ConstraintsTo make this process map and data metric usable for the clients, the team identified constraints they felt it necessary to adhere to.
Current State Process Map Constraints1. The map must remain on one page as it will be widely distributed and printed out.2. Limited access to University of Michigan Health databases because we are not hospital
stakeholders and we can only gain access with a hospital employee present.3. The patient population in scope is only discharges once every 9.125 days. They are not
scheduled at set times and therefore could not be planned for in-person observations.
Data Metric Constraints1. In order for a data metric to be significant, it must be created with at least 40 valid data
points.2. Data in the database had multiple errors—making 200 out of 400 data points unusable—
including:a. Inconsistent formattingb. Words in the place of timestampsc. Times with no datesd. Dates with no timese. No entry
3. All data collection methods must be free.
StandardsTo make this process map and data metric at the highest quality for the clients, the team determined certain standards they felt it necessary to adhere to.
1. University of Michigan Policy: The team will not reveal any names. Titles will be used to give validity to the findings.
2. HIPAA: For data reporting, there will be absolutely no patient information used. The team is interested in timing.
3. The process map will meet the University of Michigan Process Improvement Department and the standards set forth in the IOE 481 course.
4. There were no standards that matched the project on OSHA, MiOSHA, NIOSH, ASTM, ANSI, SAE, Mil-Specs, etc. Multiple web searches using the UM library online resources were performed from 11/12/2017 to 11/14/2017.
17

Table A-1: Constraints and Standards Matrix
Entry # 1 2
Constraints A. Organizational Policy (A-1)
B. Health & Safety N.A.
C. Implementability (C-1) (C-2)
D. Patient Acceptance N.A
E. Project Duration (E-1)
Standards S1. HIPPA (S1-1)
S2. Organization's Std. (S2-1) (S2-2)
S3. Best Practice (S3-1)
Standards that are not of consequence ASTM, SAE, Mil-Spec, IEEE, OSHA
(A-1) Organizational policies constrict our time that the team can spend interviewing stakeholders in the process. Since, most stakeholders work between 9-5, which can be difficult for finding interview times as a full-time student.(C-1) If the team creates a data collection tool, this tool must be implementable in a variety of ways, considering that HIPAA must not be violated, as well as University policy.(C-2) The collection tool must be easy to use by the stakeholders in the process. Anything too clunky or inconvenient will be shrugged off by stakeholders in the process, which will continue to create the issue of lack of data and transparency in the process.(E-1) The project must be completed between September and December. Therefore, as a team the team are unable to verify and make changes once the team create a system. As a result, the team must have confidence that the system the team create is effective.(S1-1) Patient information must not be placed in jeopardy at any time
18

(S2-1) There are organizational standards in place to ensure that names of any workers are not placed on any formal communication. Therefore, title of employee will be used instead.(S2-2) There are Performance Improvement standards in place that must be considered when creating the standards for designing the data metrics to be tracked as well as creating the current state map. As a group, the team wish to uphold the standards provided by the Performance Improvement department and generate a quality of work that aligns with the University of Michigan.(S3-1) The team will use best practices that are shared by the hospital staff and administration in order to make sure that the team are upholding their standards of quality and compliance.
19

APPENDIX B: Current State Process Map and A3 Documentation
Figure B-1: 4A to IRF Admission Process Flowchart using data without outliers
20

Figure B-2: Orders/Consults Current State Process Flowchart using data without outliers
21

Figure B-3: Insurance Approval Current State Process Flowchart using data without outliers
22

Figure B-4: Transfer from 4A to IRF Current State Process Map with Data using data without outliers
23

Figure B-5: Key to the 4A to IRF Admission Process Flowchart
24

Figure B-6: Project A3 Document
25

APPENDIX C: Results from Data Analysis
Figure C-1: Distribution of Timing from Stroke Admission to PT/OT Order MiChart, 1/2/17 - 11/08/2017, n=36
Figure C-2: Distribution of Timing from Stroke Admission to PT/OT Order with OutliersMiChart, 1/2/17 - 11/08/2017, n=39
26

Figure C-3: Distribution of Timing from PT/OT Order to PT Note MiChart, 1/2/17 - 11/08/2017, n=36
Figure C-4: Distribution of Timing from PT/OT Order to PT Note with OutliersMiChart, 1/2/17 - 11/08/2017, n=39
27

Figure C-5: Distribution of Timing from PT/OT Order to OT Note MiChart, 1/2/17 - 11/08/2017, n=36
Figure C-6: Distribution of Timing from PT/OT Order to OT Note with Outliers MiChart, 1/2/17 - 11/08/2017, n=40
28

Figure C-7: Distribution of Timing from PT Note to PM&R OrderMiChart, 1/2/17 - 11/08/2017, n=19
Figure C-8: Distribution of Timing from OT Note to PM&R Order MiChart, 1/2/17 - 11/08/2017, n=13
29

Figure C-9: Distribution of Timing from PM&R Consult to PM&R NoteMiChart, 1/2/17 - 11/08/2017, n=34
Figure C-10: Distribution of Timing from PM&R Consult to PM&R Note with OutliersMiChart, 1/2/17 - 11/08/2017, n=36
30

Figure C-11: Distribution of Timing from Being Added to Potential Admit List to Insurance Verification
MiChart, 1/2/17 - 11/08/2017, n=12
Figure C-12: Distribution of Timing from Insurance Verification to Insurance ApprovalIRF Admissions Coordinator, 1/2/17 - 11/08/2017, n=12
31

Figure C-13: Distribution of Timing from PM&R Note to Discharge Order MiChart, 1/2/17 - 11/08/2017, n=35
Figure C-14: Distribution of Timing from PM&R Note to Discharge Order with OutliersMiChart, 1/2/17 - 11/08/2017, n=37
32

Figure C-15: Distribution of Timing from 4A Discharge Order to Actual 4A DischargeMiChart, 1/2/17 - 11/08/2017, n=38
Figure C-16: Distribution of Timing from 4A Discharge Order to Actual 4A Discharge with Outliers
MiChart, 1/2/17 - 11/08/2017, n=39
33

Figure C-17: Distribution of Timing from Actual 4A Discharge to 6A Admission MiChart, 1/2/17 - 11/08/2017, n=38
34

APPENDIX D: Work Instructions for Excel Tool
Figure D-1: Excel Tool Work Instructions for Order Sheet
35

Figure D-2: Excel Tool Work Instructions for Summary Sheet
36
Related Documents