Mechanical and Electrical Events of the Cardiac Cycle

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Mechanical and Electrical Events of the Cardiac Cycle

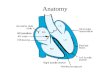
Cardiac CycleCardiac Cycle: the electrical, pressure and
volume changes that occur in a functional heart between successive heart beats.
• Phase of the cardiac cycle when myocardium is relaxed is termed diastole.
• Phase of the cardiac cycle when the myocardium contracts is termed systole.– Atrial systole: when atria contract.– Ventricular systole: when ventricles contract.

Mechanical Events of the Cardiac Cycle
1. Ventricular Filling Period [ventricular diastole, atrial systole]
2. Isovolumetric Contraction Period [ventricular systole]
3. Ventricular Ejection Period [ventricular systole]
4. Isovolumetric Relaxation Period [ventricular diastole]


Cardiac Cycle• Electrical changes in heart tissue cause
mechanical, i.e. muscle contraction, changes.
• Thus, changes in electrical membrane potential of specific parts of the heart tissue represent mechanical events in specific areas of the heart tissue.

Electrical Events of the Cardiac Cycle
• Each wave or interval represents depolarization or repolarization of myocardial tissue.
• P wave represents depolarization of atria which causes atrial contraction.
• QRS complex reflects depolarization of ventricles which causes contraction.
• T wave reflects repolarization of muscle fibers in ventricles.


1. The electrical activity of the heart originates in the sino-atrial node. The impulse then rapidly spreads through the right atrium to the atrioventricular node. It also spreads through the atrial muscle directly from the right atrium to the left atrium. The P-wave is generated by activation of the muscle of both atria.
The impulse travels very slowly through the AV node, then very quickly through the bundle of His, then the bundle branches, the Purkinje network, and finally the ventricular muscle.
2. The first area of the ventricular muscle to be activated is the interventricular septum, which activates from left to right. This generates the Q-wave.
3. Next, the left and right ventricular free walls, which form the bulk of the muscle of both ventricles, gets activated, with the endocardial surface being activated before the epicardial surface. This generates the R-wave.
4. A few small areas of the ventricles are activated at a rather late stage. This generates the S-wave.
5. Finally, the ventricular muscle repolarizes. This generates the T-wave.

Cardiac Cycle
Coordination of :• Electrical Changes• Pressure Changes in Left Atria, Left
Ventricle and Aorta• Ventricular Volume Changes• Cardiac Valves


Electrocardiography
• Two common abbreviations for electrocardiogram: EKG and ECG.
• EKG comes from German language where cardiogram is written as kardiogram.
• The ECG records the electrical activity of the heart.
• Mechanical activity of the heart is sensed by echocardiography.

ElectrocardiographyECG - electrocardiogram
– graphic recording of electrical events– established electrode pattern results in specific
tracing pattern– electrical pattern reveals blood supply problems

Electrophysiology
• If an electrode is placed so that wave of depolarization spreads toward the recording electrode, the ECG records a positive (upward) deflection.
• If wave of depolarization spreads away from recording electrode, a negative (downward) deflection occurs.

Electrophysiology

Cardiac Current Flow

Cardiac Current Flow

ECG Time & Voltage
• ECG machines can run at 50 or 25 mm/sec.• Major grid lines are 5 mm apart, at standard
25 mm/s, 5 mm corresponds to .20 seconds.• Minor lines are 1 mm apart, at standard 25
mm/s, 1 mm corresponds to .04 seconds.• Voltage is measured on vertical axis.• Standard calibration is 0.1 mV per mm of
deflection.

Electrophysiology
• When myocardial muscle is completely polarized or depolarized, the ECG will not record any electrical potential but rather a flat line, isoelectric line.
• After depolarization, myocardial cells undergo repolarization to return to electrical state at rest.

Electrophysiology
• P wave represents depolarization of atria which causes atrial contraction
• Repolarization of atria not normally detectable on an ECG
• Excitation of bundle of His and bundle branches occur in middle of PR interval
• QRS complex reflects depolarization of ventricles
• T wave reflects repolarization of muscle fibers in ventricles

Electrocardiogram• Normal P wave has
amplitude of ≤ 0.25 mV • Q wave is first
downward deflection after P wave; signals start of ventricular depolarization
• R wave is positive deflection after Q wave
• S wave is negative deflection preceded by Q or R waves
• T wave follows QRS


Standard 12-Lead ECG
• Usually performed when person is resting in supine position.
• Composed of three bipolar limb leads: I, II, and III; three augmented voltage leads: aVR, aVL, aVF; and six chest or precordial leads: V1 – V6.
• All limb leads lie in frontal plane.• Chest leads circle heart in transverse plane.

ECG Limb Leads

ECG Augmented Limb Leads


ECG Precordial Leads


Standard 12-Lead ECG
• Each lead provides a different electrical angle or picture of the heart.
• Anterior part of heart by looking at V1 – V4.
• Lateral view of heart: I, aVL, V5 and V6.
• Inferior view of heart: II, III, and aVF.

Exercise 12-Lead ECG

12-Lead ECG• Limb lead II shows
large QRS amplitude because left ventricle vector lies parallel with electrode placement.
• Chest lead V1 has large S wave because left ventricle current vector is directed away from electrode.

12-Lead ECG Strip

Interpretation of ECG
Rate. First measurement to calculate is heart rate. PQRST waves represent one complete cardiac cycle.
• At standard paper speed, divide 1500 by distance between R to R waves.
• Find R wave on heavy line. Count off 300, 150, 100, 75, 60 for each following line. Where next R lands is quick estimate.
• Multiply number of cycles in 6 second marks by 10.

Interpretation of ECG


Interpretation of ECG
• Normal heart rhythm has consistent R-R interval.• Mild variations due to breathing also normal.

Interpretation of ECG
Normal Sinus Rhythm• Rate: 60-100 b/min• Rhythm: regular• P waves: upright in
leads I, II, aVF
• PR interval: < .20 s• QRS: < .10 s



Interpretation of ECG
ST segment depression. • Hallmark of myocardial ischemia.• Reduction of oxygen-rich blood supply alters normal
cellular action causing ST segment displacement ≥ 1 mm below line.
• Upsloping, horizontal, downsloping
Related Documents










![ECG: UNDERSTANDING ACCELERATED CONDUCTION Dr. Krishnendu Maity BHMS [Calcutta] MD (Hom. Repertory) [Pune] Professor & HOD, Dept. of Medicine Teaching.](https://static.cupdf.com/doc/110x72/551be6b6550346c3588b608f/ecg-understanding-accelerated-conduction-dr-krishnendu-maity-bhms-calcutta-md-hom-repertory-pune-professor-hod-dept-of-medicine-teaching.jpg)