2011

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

2011


SEA/TB/332Distribution: General
Tuberculosis in the South-East Asia Region
The Regional Report: 2011

© World Health Organization 2011
All rights reserved.
Requests for publications, or for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – can be obtained from Publishing and Sales, World Health Organization, Regional Office for South-East Asia, Indraprastha Estate, Mahatma Gandhi Marg, New Delhi 110 002, India (fax: +91 11 23370197; e-mail: [email protected]).
The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
This publication does not necessarily represent the decisions or policies of the World Health Organization.
Printed in India

Tuberculosis Control in the South-East Asia Regioniii
ContentsAbbreviations v
Preface viii
1. Introduction 1
2. Epidemiology of Tuberculosis in The SEA Region 4
2.1 Estimated TB incidence, prevalence and mortality 5
2.2 Community-based surveys to estimate prevalence of pulmonary tuberculosis, annual risk of tuberculosis infection (ARTI) and mortality due to TB 10
2.3 Impact of HIV on TB in the Region 13
2.4 Drug-resistant TB 16
3. Achievements 17
3.1 DOTS coverage 17
3.2 Case-notifications 18
3.3 Treatment outcomes 23
3.4 Reporting progress towards global targets 26
4. Key Milestones achieved in 2010 28
4.1 DOTS 28
4.2 Strengthening national laboratory networks 28
4.3 Addressing TB/HIV, MDR-TB and other challenges 29
4.4 Public and private partnerships 33
4.5 Surveillance, monitoring and evaluation 34
4.6 Resources for TB control 35
4.7 Operational research 35
5. WHO Support in the Region 36
5.1 Technical assistance 36
5.2 Strengthening national laboratory networks 37

Tuberculosis Control in the South-East Asia Regioniv
5.3 Capacity-building, information exchange 38
5.4 Resource mobilization 38
5.5 Ensuring regular supplies of drugs and improving procurement and supply management 39
5.6 MDR-TB 39
5.7 Operational research 40
5.8 Coordination, collaboration and partnerships 40
5.9 Advocacy, communication and social mobilization 41
5.10 Monitoring and evaluation 41
Country Profiles 43
Bangladesh 45
Bhutan 51
DPR Korea 56
India 61
Indonesia 68
Maldives 75
Myanmar 79
Nepal 85
Sri Lanka 90
Thailand 95
Timor-Leste 101

Tuberculosis Control in the South-East Asia Regionv
Abbreviations3DF Three Disease FundACSM Advocacy, Communication and Social MobilizationADB Asian Development BankAFB Acid-Fast BacilliAIDS Acquired Immunodeficiency SyndromeART Antiretroviral TreatmentARTI Annual Risk for Tuberculosis InfectionATS American Thoracic SocietyAUSAID Australian Agency for International Development AustraliaBRAC Bangladesh Rural Advancement CommitteeCDR Case Detection RateCFR Case Fatality RateCHC Community Health CentreCIDA Canadian International Development AgencyCO Country OfficeCOD Cause of DeathCPT Cotrimoxazole Preventive TherapyDFID United Kingdom Department for International DevelopmentDOT Directly Observed TreatmentDOTS Directly Observed Treatment, Short CourseDPR Korea Democratic People’s Republic of KoreaDRS Drug Resistance Survey/SurveillanceDST Drug Susceptibility TestingDTCs District TB CoordinatorsEC European CommissionEP Extra-pulmonaryEQA External Quality Assessment/AssuranceERD External Resource DivisionEXPAND-TB Expanding Access to new Diagnostics for TBFDC Fixed Dose CombinationFHI Family Health InternationalFidelis Fund for Innovative DOTS Expansion through Local Initiatives
to Stop TBFIND Foundation for Innovative New DiagnosticsGDF Global (TB) Drug FacilityGF Global Fund to Fight AIDS, Tuberculosis and MalariaGLC Green Light CommitteeGLI Global Laboratory InitiativeHIV Human Immunodeficiency VirusHNPSP Health, Nutrition and Population Sector ProgrammeHQ Headquarters

Tuberculosis Control in the South-East Asia Regionvi
HRD Human Resources DevelopmentICDDRB International Centre for Diarrhoeal Disease Research,
BangladeshICTC Integrated Counselling and Testing CentreIDU Intravenous Drug UserIEC Information, Education and CommunicationIMA Indian Medical AssociationIMPACT Indian Medical Professional Associations Coalition Against TBINGO International Nongovernmental OrganizationIPT Isoniazid Preventive TreatmentISAC Intensified Support and Action CountriesISTC International Standards for Tuberculosis CareIVMS International Centre for Veterinary and Medical Sciences, JATA Japan Anti-TB AssociationJICA Japan International Cooperation AgencyKNCV Royal Dutch Tuberculosis AssociationLED Light Emitting DiodeMDG(s) Millennium Development Goal(s)MDR-TB Multidrug Resistant TuberculosisMIFA Managing Information for ActionMMR Mass Miniature RadiographyMO Medical OfficerMoF Ministry of FinanceMoU Memorandum of UnderstandingNAP National AIDS ProgrammeNEP New Extra-pulmonaryNGO Nongovernmental OrganizationNIDCH National Institute of Diseases of the Chest and Hospital NPO National Professional OfficerNRL National Reference LaboratoryNSN New Smear-NegativeNSP New Smear-Positive (TB cases)NTI National Tuberculosis Institute, Bangalore, IndiaNTP National Tuberculosis ProgrammeNTRL The National Tuberculosis Reference Laboratory OGAC Office of Global AIDS ControlOSE Onsite EvaluationPAL Practical Approach to Lung HealthPHIs Public Health Inspectors PHL Public Health LaboratoryPITC Provider Initiate HIV Testing and CounselingPITC Provider Initiated (HIV) Testing and CounsellingPLHIV People Living with HIV

Tuberculosis Control in the South-East Asia Regionvii
PPM Public-Private, Public-Public or Private-Private MixPPP Public-Private PartnershipPSI Population Services InternationalPTB pulmonary TBQA Quality AssuranceRBRC Random Blinded Re-CheckingRHC Rural Health CentreRNTCP Revised National Tuberculosis Control Programme (India)RO Regional OfficeRTRL Regional TB Reference Laboratory SAARC South-Asian Association for Regional CooperationSEAR WHO South-East Asia RegionSLD Second-Line Drugs (for MDR-TB)SNRL Supranational Reference LaboratorySOP Standard Operating ProceduresSSA Special Services AgreementSTAG Strategic and Technical Advisory Group (for Tuberculosis)STD Sexually Transmitted DiseaseTAD Treatment After DefaultTAF Treatment After FailureTB TuberculosisTB/HIV Tuberculosis and Human Immunodeficiency VirusTBCTA TB Coalition for Technical AssistanceTBREACH An initiative launched by Stop TB Partnership to support
countries in early and universal case detection through proposal submission
TBTEAM TB Technical Assistance MechanismTDR UNICEF-UNDP-World Bank-WHO Special Programme for
Research and Training in Tropical DiseasesThe Union International Union Against Tuberculosis and Lung DiseaseTRC Tuberculosis Research Centre (Chennai, India)TSG Technical Strategic GroupUNDP United Nations Development ProgrammeUNICEF United Nations Children’s Fund UNICERF UN Common Emergency Relief FundUNITAID UNITAID contribute to scaling up access to treatment for
HIV/AIDS, malaria andtuberculosisUSAID United States Agency for International DevelopmentUSD United States dollarVCTC Voluntary Counselling and Testing CentreVR Vital Registration WHO World Health OrganizationXDR-TB Extensively Drug-Resistant Tuberculosis

Preface The WHO South-East Asia Region continues to make a significant contribution to the global efforts towards the elimination of TB. The notified TB cases have been steadily increasing and in 2009 the figure reached in excess of 2.3 million, which is more than a third of all cases notified globally. This has been complemented by an overall treatment success rate of 88% among new smear-positive cases in the Region.
In the year 2010 the WHO South-East Asia Region has also reached an important half-way landmark in its inexorable progress against goals set in the Regional Strategic Plan for TB Control 2006 - 2015 and also towards the Millennium Development Goals (MDGs) 2015.
TB prevalence rates across the Region have declined by more than 25% by 2010. Maldives and Bhutan already show a more than 50% decline while Myanmar and Indonesia have shown a third of reduction. Nepal and India have reduced TB by a quarter of the reported cases. The remaining five member countries have shown a smaller decline. Mortality among TB cases in the Region as a whole has declined by around 44%, which is very close to the target of 50%. Bhutan, Indonesia, Maldives, Myanmar and Nepal have already achieved a 50% reduction in mortality while India is close to achieving the target. However, a slower decline in incidence rates in the countries has been observed.
However, we cannot afford to be complacent. The fight against TB cannot be won without universal access to quality care for all TB patients. This means we need to strengthen the present services and also be innovative to reach out to those who still do not have access to DOTS services. We also need to innovate for rapid diagnosis and quicker treatment which would make service more patient-friendly.
While we intensify our efforts to control TB we also need to confront the epidemic of drug-resistant TB in the Region. Substantial resources will need to be mobilized for organizing services in the Region, that has around 130 000 MDR-TB cases – nearly one third of the global burden. Extensively drug-resistant TB (XDR-TB) has also been reported from five countries - Bangladesh, India, Indonesia, Nepal and Thailand. The strategy will need to focus on prevention of emergence of resistance by strengthening services for basic TB control while
Tuberculosis Control in the South-East Asia Regionviii

Tuberculosis Control in the South-East Asia Regionix
also providing for diagnosis and treatment of such cases. Countries in the Region are in various stages of implementation of programmatic management of drug-resistant TB (PMDT). Nine countries have PMDT guidelines while for the remaining two this is expected to be done in early 2011.
Emergence and spread of drug-resistant TB re-emphasizes the need for involvement of all sectors for providing quality services and also mobilizing the available resources within countries to improve access. While several hundred medical colleges, large hospitals and thousands of private physicians are already working with national TB programmes, this is still only a percentage of the entire expense.
The need for greater collaboration with HIV programmes is already felt. Member States have developed and established national policies and strategies for collaboration and are expanding interventions to detect and care for people co-infected with HIV and TB. The strategies would need to be further adapted for the needs of drug-resistant TB as well.
All Member States have reached out to communities in various ways for supporting the TB programme. We need to map community resources and models of successful involvement from the Region need to be documented to be replicated within and outside the Region. Community support becomes all the more important in case of MDR-TB treatment that requires the social, psychological and financial rehabilitation of the patient.
This annual report is a compilation of regional and country-specific achievements, challenges and plans. WHO will continue to provide technical support to catalyse and accelerate the implementation of TB control services in Member States through a range of activities as detailed in this report. I am sure that with the commitment of ministries of health and support from all partners and stakeholders the Region will achieve the desired targets and lead the global fight against TB.
Dr Samlee PlianbangchangRegional Director


Tuberculosis Control in the South-East Asia Region1
Each year the South-East Asia Region (SEA Region or “the Region”) comes with an annual report that measures the progress towards eliminating TB, within the purview of the given situation of TB and challenges that confront us. The annual report may thus be seen as a status, monitoring and planning document.
Overall the Region continues to bear more than one third of the global burden of tuberculosis, an estimated pool of nearly five million cases to which more than 3 million are added each year. This is despite a more than 25% decrease in prevalence rates since 1990. Decrease in prevalence rates have been achieved due to a good case-notification and treatment success rate of more than 85% for the Region as a whole.
The progress in expansion and strengthening of DOTS services is quite visible from the increasing case-notification and success rates. Mortality rate among TB patients has also decreased by more than 44% for the Region as a whole although absolute mortality figures are still close to half a million.
Good performance of DOTS in the Region has also led to low levels of multidrug-resistance (MDR) among newly detected cases (range: 1.7%–4.2%). Among previously treated cases in the Region, MDR-TB rates range from 10.0%–34.7%. However, given the large numbers of TB cases in the SEA Region, this translates to 130000 MDR-TB cases (110 000–170 000) accounting for nearly one third of the world’s MDR-TB cases. However many of country-specific estimates are based on modelling. Laboratory capacity to undertake drug-resistance surveys needs strengthening.
1
Introduction

Tuberculosis Control in the South-East Asia Region2
Spread of HIV also threatens to reverse the gains already achieved by TB control programmes. It is estimated that there are 3.5 million people living with HIV (PLHIV) in the South-East Asia Region, constituting 11% of the total number of PLHIVs globally. In 2009, there were an estimated 220 000 new HIV infections in the Region and 230 000 people died of AIDS-related illnesses. This calls for further strengthening of the degree of collaboration between TB and HIV programmes and specifically bolstering the availability of ART and cotrimoxazole preventive therapy for all eligible TB patients co-infected with HIV. Intensified case-finding, INH prophylaxis and infection control among all HIV patients is also imperative.
The desired goal of universal access is yet to be achieved and remain a specific challenge for a wide array of service providers in most countries. There have been some efforts made in the Region to establish partnerships with various health sectors and civil society. Good models of partnerships need to be replicated in all countries with the involvement of communities to promote a patient-centric approach.
Recognizing that effective TB control necessarily depends on strong health systems, efforts will also be made to effectively streamline TB services within the primary health care systems, optimize the use of common resources for the delivery of TB services alongside those of other programmes, while at the same time adopting the successful approaches of other programmes to improve TB services.
Respiratory infection control is important to prevent the spread of TB infection and such policy should be part of health system strengthening. Infection control is not just limited to health care facilities. All congregate settings need to be assessed. A regional-level endeavour is required to raise the issue of the need for greater attention to the neglected area of infection control within the national health systems at the highest-level policy forums.
Research has been observed to be a weak area in the Region and in the year ahead efforts will be made to strengthen this through regional training and technical support. Specifically in the context of upcoming newer technologies, countries would need to undertake operations research for quick adoption of such tools and technologies in the local context. Member States will also need to undertake further research on social and behavioural determinants that influence the disease progress and outcome.

Tuberculosis Control in the South-East Asia Region3
Sustaining these efforts will require continued commitment and adequate resources for national TB control programmes for several more years. Increased commitment from donors and funding agencies will also be required not only for strengthening basic DOTS but also for establishing and expanding programmatic management of drug-resistant TB. Like all previous years it is hoped that the Region will show tangibly good progress towards the achievement of TB control goals in the next year.

Tuberculosis Control in the South-East Asia Region4
The WHO South-East Asia (SEA) Region has an estimated 5 million prevalent and about 3.3 million incident case of tuberculosis annually. It carries more than one third of the global burden of tuberculosis (Figure 1). Five of the 11 Member countries in the Region are among the 22 high-burden countries, with India alone accounting for more than 20% of the world’s cases. Most cases continue to occur in the most productive age group of 15–54 years, with males being disproportionately affected. The male-to-female ratio in the Region is 2.0 among
2
Epidemiology of Tuberculosis in the SEA Region
Estimated global TB incidence = 9 400 000 (8 900 000 – 9 900 000) cases (all forms of TB).
Source: Global Tuberculosis Control: WHO Report 2010, World Health Organization, Geneva 2010. WHO/HTM/2010.7
Figure 1: Estimated incidence of all forms of TB, classified by WHO Regions, 2009
20%35%
5%
7%3%
Africa
Western Pacific
South-East Asia
Europe
Eastern Mediterranean
Americas30%

Tuberculosis Control in the South-East Asia Region5
new smear-positive TB cases detected for the year 2009. Though the death rates due to TB have declined after the introduction of DOTS in the Region, there are still about half a million deaths occurring among TB patients each year.
2.1 Estimated TB incidence, prevalence and mortality
2.1.1 Revision of methodology for TB burden estimatesIn 2009, the methodology to obtain estimates of the burden of disease (prevalence, incidence and mortality) has been revised by WHO. Therefore, it is important to note that figures published in this report are likely to be different from those published earlier, and that the new and old estimates cannot be compared. Further details about the methodology used are provided in Annex 1 of the Global Tuberculosis Control: WHO Report 2010.
For all the countries in the Region, the estimates of the total number of incident cases, prevalent cases and deaths due to TB have been obtained based indirectly on estimates of the case-detection rate of all forms of TB . Therefore, TB incidence, prevalence and mortality are published as best estimates with confidence intervals. The confidence intervals provide a range of plausible values and their width is inversely proportional to the accuracy of the estimate, depending on quality and completeness of country data.
The estimates could be improved through systematic assessment of the quality and completeness of surveillance data, strengthening TB surveillance within countries and carrying out an in-depth analysis of available data. Other approaches to improve estimates include operational research, and strengthening vital registration (VR) systems in order to obtain reliable mortality data.
Population-based surveys can provide direct measurement of TB prevalence and information about the reasons and extent to which people with TB are missed in surveillance data.
To improve current estimates, Bangladesh and Myanmar conducted a TB prevalence survey in 2009 and 2010; Indonesia, Nepal and Thailand are planning to conduct a survey by 2015; Sri Lanka conducted an in-depth analysis of TB surveillance data; India will hold a national workshop on TB burden estimates in 2011; and Timor-Leste will explore the best option to improve country estimates.

Tuberculosis Control in the South-East Asia Region6
2.1.2 Estimated TB incidence, prevalence and mortality in the South-East Asia RegionThe TB incidence, prevalence and mortality rates in Member States of the SEA Region, estimated by mathematical and epidemiological modelling of available data, are presented in Table 1.
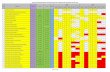
Table 1: Estimates of TB disease incidence, prevalence and mortality in Member States of the South-East Asia Region (rates per 100 000 population), 2009
Country Population* (in thousands)
Incidence rate of all forms of
TB (confidence intervals)
Prevalence rate of all forms of
TB (confidence intervals)
Death rate for all forms of TB,
excluding HIV (confidence intervals)
Bangladesh 162 221 225 (183–270) 426 (198–696) 51 (37–67)
Bhutan 697 158 (132–186) 179 (47–315) 8.4 (4.6–17)
DPR Korea 23 906 345 (293–400) 423 (126–736) 25 (13–44)
India 1 198 003 168 (137–202) 249 (107–417) 23 (14–36)
Indonesia 229 965 189 (153–228) 285 (119–482) 27 (16–41)
Maldives 309 39 (33–45) 47 (14–81) 2.6 (1.4–4.6)
Myanmar 50 020 404 (329–486) 595 (262–994) 59 (36–87)
Nepal 29 331 163 (133–197) 241 (97–408) 21 (12–34)
Sri Lanka 20 238 66 (54–80) 101 (41–170) 9.2 (5.4–14)
Thailand 67 764 137 (111–165) 189 (83–317) 18 (11–27)
Timor-Leste 1 133 498 (406–600) 743 (295–1274) 66 (37–106)
SEA Region 1 783 587 182 (161–206) 278 (186–398) 27 (20–35)
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition. (URL: http://www.un.org/esa/population/publications/wpp2008/wpp2008_text_tables.pdf)
Figure 2 makes a comparison of the estimated TB prevalence rates per 100 000 population between 1990 and 2009 in each of the 11 Member States of the Region. However, this comparison takes into consideration only the best estimate of prevalence rate, and not the uncertainty bounds that have variable width according to the quality of country data used for the estimate. Taking into account this limitation, a decline in the prevalence rates is observed in all Member States, and in some countries this decline is very significant. For Timor-Leste country-specific data did not exist prior to 2002 and comparison of baseline data may be biased.

Tuberculosis Control in the South-East Asia Region7
Figure 3 compares the estimated TB mortality rates per 100 000 population in 1990 and 2009 in each of the 11 Member States of the Region. As said earlier, this comparison takes into consideration only the best estimate
Figure 2: Estimated prevalence rate (all forms of TB, except HIV) in 1990 and 2009, classified by Member State of the SEA Region
Source: Global Tuberculosis Control: WHO Report 2010, World Health Organization, Geneva 2010. WHO/HTM/2010.7
1000
900
800
700
600
500
400
300
200
100
0
Rate
per
100
000
pop
ulat
ion
BAN BHU DPRK IND INO MAl MMR NEP SRL THA TLS
1990 2009
140
120
100
80
60
40
20
0
Rate
per
100
000
pop
ulat
ion
BAN BHU DPRK IND INO MAV MMR NEP SRL THA TLS
1990 2009
* Source: Global Tuberculosis Control: WHO Report 2010, World Health Organization, Geneva 2010. WHO/HTM/2010.7
[The scale used in this graph does not allow visualization of mortality rates for Bhutan, Maldives and Sri Lanka in 2009 due to their very low figures].
Figure 3: Estimated mortality rate (all forms of TB, except HIV) in 1990 and 2009, classified by Member State of SEA Region*

Tuberculosis Control in the South-East Asia Region8
of mortality rate, and not the uncertainty bounds. A significant decline in the mortality rates is observed in all Member States with the exception of Timor-Leste (country data are not available as mentioned above). For some countries decrease in mortality is already beyond 50% of 1990 baseline for achieving the Stop TB Partnership target for 2015.
The trends of estimated prevalence, incidence and mortality rates in the SEA Region as a whole are presented in Figure 4. TB prevalence rates decreased by 25% and mortality rates have nearly halved. The decline in incidence, however, is less perceptible.
This graph is based on the best annual estimates of mortality, prevalence and incidence; the interpretation of the trends should take into account the uncertainty bounds around each value. Figures 5, 6 and 7 are showing the trends of, respectively, incidence, prevalence and mortality as best estimate and upper and lower confidence intervals.
Figure 4: Trends in estimated TB prevalence, incidence and mortality rates from 1990 to 2009 in the SEA Region
Rate
per
100
000
pop
ulat
ion
400
350
300
250
200
150
100
50
01990 2000 2005 2006 2007 2008
Year
Source: Global Tuberculosis Control: WHO Report 2010, World Health Organization, Geneva 2010. WHO/HTM/2010.7
2009
375
183
48
1995
278
182
27
Estimated prevalence all forms
Estimated incidence all forms
Estimated TB mortality

Tuberculosis Control in the South-East Asia Region9
Figure 5: Trend of TB incidence rate (best estimate, upper and lower bounds) from 1990 to 2009 in the SEA Region
Rate
per
100
000
pop
ulat
ion
260
240
220
200
180
160
140
120
1001990 2000 2005 2006 2007 2008
Year
2009
239
183
137
1995
Best EstimateLower bound Upper bound
Estimated TB incidence rate, SEAR, 1990-2009
Figure 6: Trend of TB prevalence rate (best estimate, upper and lower bounds) from 1990 to 2009 in the SEA Region
Rate
per
100
000
pop
ulat
ion
650
550
450
350
350
501990 2000 2005 2006 2007 2008
Year
2009
580
375
227
1995
Best EstimateLower bound Upper bound
398
278
186
206
182
161

Tuberculosis Control in the South-East Asia Region10
Figure 7: Trend of TB mortality rate (best estimate, upper and lower bounds) from 1990 to 2009 in the SEA Region
Rate
per
100
000
pop
ulat
ion
80
70
60
50
40
30
20
10
01990 2000 2005 2006 2007 2008
Year
2009
68
33
1995
Best EstimateLower bound Upper bound
3527
20
48
2.2 Community-based surveys to estimate prevalence of pulmonary tuberculosis, annual risk of tuberculosis infection (ARTI) and mortality due to TBA number of community-based surveys have been carried out in the Region at different times to estimate the prevalence of pulmonary TB (PTB). The results of surveys undertaken since 1990 (the baseline year for the MDGs) are summarized in Table 2 and reveal variable prevalence rates in different countries and between different parts of individual countries.
The surveys carried out in Bangladesh over the period are not comparable, since these were carried out in different areas using different methodologies. The nationwide prevalence survey was conducted in 2009.
Three rounds of surveys in Thiruvallur district in Tamil Nadu, India, between 1999 and 2006 showed a decline of about 12% per year in the prevalence of smear-positive as well as culture-positive PTB. In this area, no decline in prevalence had been observed in the pre-DOTS period through several rounds of surveys carried out between 1968 and 1986. District-subdistrict-level surveys are also currently in progress in five other sites in India.
In Indonesia, the national-level survey during the year 2004 demonstrated a three-fold decline in prevalence rates when compared with the prevalence rates

Tuberculosis Control in the South-East Asia Region11
obtained during a number of district-level surveys carried out during the 1980s. Indonesia is planning to conduct another TB prevalence survey by 2013.
Myanmar conducted a TB prevalence survey in Yangon district in 2006 and a nationwide TB prevalence survey in 2010; the results of both showed higher prevalence compared with previous estimates.
Table 2: Prevalence surveys in Member States of the SEA Region, 1990–2010
Country Area Study period
Age(yrs≥)
Sample size
Screening method
Prevalence of PTB cases/ 100,000 population
Culture +ve
Smear +ve
Culture and/ orsmear+ve
Bangladesh
74 subdistricts
2001 12 223 936 Symptoms - 24 -
Matlab rural area
2001 15 59 395 Symptoms - 95 -
National level
2007–09 15 52 098 No screening*
- 79 -
India
Morena(Madhya Pradesh)
1991–92 15 11 097 Symptoms - - 1270
Delhi 1991 5 27 838 MMR - - 330
Car Nicobar(Andaman & Nicobar)
2000–01 15 10 570 Symptoms - 729 -
Thiruvallur(Tamil Nadu)
1999–012001–032004–06
15 83 42585 47489 413
MMR + symptoms
609451311
326257169
-
Tribal areas (Madhya Pradesh)
2006–07 15 20 000 Symptoms 387
Faridabad (Haryana)
2008–09 15 98 599 Symptoms 126
IndonesiaMyanmar
National level
2004 15 50 134 Symptoms 104 - -
Yangon division
2006 10 20 792 279 537
2010 10 51 368 Symptoms 239 605
*Sputum samples collected from all participants.

Tuberculosis Control in the South-East Asia Region12
Thailand is currently in the preparation phase to carry out a nationwide prevalence survey in late 2011.
Tuberculin surveys to estimate the annual risk of tuberculosis infection (ARTI) among children carried out in the Member States of the Region from 1990 onwards are presented in Table 3.
The trends in ARTI are available from two areas of India. In Thiruvallur, a district in southern India, the trends in ARTI mirrored the decline in prevalence of TB over the same time period. A decline in ARTI rates was also seen in Bangalore city.
Presently, repeat zonal-level tuberculin surveys are in progress in India and will help define trends in ARTI since the first zonal-level surveys carried out during 2000–2003. A consultative meeting is scheduled for early 2011 to arrive at a consensus on epidemiological data for India.
In Indonesia, surveys in five provinces demonstrated a significant decline in ARTI when compared with the ARTI estimates obtained during several district-level surveys carried out in the 1980s.
Table 3: Tuberculin surveys in Member States of the SEA Region, 1990–2010
Country Area Year Sample size Age group (Years)
Estimated ARTI (%)
Bangladesh National level 2007–2009 17585 5–14 Results awaited
Bhutan Thimphu, Mongar and Bumthang dsitricts
1991 1736 6–14 1.9
DPR Korea National-level 2007 11182 7–8 3.0
India
Bangalore city 19982006
4936 3354
5–8 5–8
2.2 1.5
Rural areas, Thiruvallur district, Tamil Nadu
1999–01 12854 0–9 1.6
2004–2005 8668 0–9 1.4
2001–2003 8329 0–9 1.2
Orissa (state level) 2002 10626 1–9 1.7
Andhra Pradesh (state level)
2005–2006 3636 5–9 1.4
Khammam, Andhra Pradesh
2001–2002 5–7 1.5
Zonal level surveys (4 zones)
2000–2003 N. Zone–51 380W. zone–51 733E. Zone–42 836S. Zone–52 300
0–9 N. Zone–1.9W. Zone–1.6E. Zone–1.3S. Zone–1.0

Tuberculosis Control in the South-East Asia Region13
Kerala—(state level) 2006 4821 5–9 Not available**
Chennai city 2006 7008 1–9 2.0
Tribal areas, Madhya Pradesh
2006 4802 1–9 1.3
Indonesia-Provincial Level surveys
West Sumatra 2006 5653 6–9 1–1.3$
Nusa Tenggara 2007 5479 1
Central Java 2007 6943 0.9
North Sulawesi 2008 6557 1.9–2.5$
South Kalimantan 2008 6359 1.8
NepalSub-national surveys in 17 selected areas
1985–1995 Not Available 6–10 2.1
National Level 2006–2007 17 260 5–7 0.9
$Estimates vary depending upon statistical method of estimation.
**ARTI could not be estimated due to low proportion of tuberculin reactors leading to absence of demarcation on the frequency distribution of tuberculin reaction sizes.
National-level baseline tuberculin surveys are also in progress in Bhutan and Sri Lanka.
A limited number of TB mortality studies based on vital registration, and verification of the cause of death (CoD) through verbal autopsies, have been carried out in the Region. A study in Chennai revealed TB mortality rate at 152 per 100 000 population among males and 43 per 100 000 among females. A state-level study in Andhra Pradesh revealed that 5% of deaths among males and 3% among females were caused by TB. In Indonesia, verbal autopsy-based mortality studies carried out at seven sites at the provincial and subprovincial level during 2006–2008, revealed that TB was ranked between first to third among the leading causes of death in the different provinces.
A national-level study to find out the cause of death (CoD) in a sample of one million deaths is under progress in India. Myanmar is planning to conduct a nationwide TB mortality survey in 2015.
2.3 Impact of HIV on TB in the Region The expanding HIV epidemic is a growing concern. It is estimated that there are 3.5 million people living with HIV (PLHIV) in the South-East Asia Region, constituting 11% of PLHIV globally. In 2009, there were an estimated 220 000 new HIV infections in the Region and 230 000 people died of AIDS-related illnesses. Five countries in the Region as shown in Figure 8

Tuberculosis Control in the South-East Asia Region14
Figure 8: HIV prevalence in Member States of the SEA Region, 2009
Source: South-East Asia HIV Report 2010.
account for the majority of HIV cases in the Region, with about 2.4 million PLHIVs in India alone.
The prevalence of HIV in the general population in the South-East Asia Region is estimated to be the highest in Thailand, followed by Myanmar, Nepal and India (Table 4). The Region is distinguished by complex and heterogenous HIV epidemics at different stages both across and within individual countries. While Myanmar and Thailand have more homogenous HIV prevalence among populations living in different geographical areas, the epidemic is more concentrated in some states and districts in India and among high-risk population groups in Bangladesh, Nepal and Indonesia. HIV prevalence is estimated to be low in Bhutan, Maldives, Sri Lanka and Timor-Leste. No HIV cases have been reported from DPR Korea to date.
Nepal64 000
Myanmar240 000
Thailand610 000
Indonesia190 000
India2.4 million
Bhutan(<1000)
Bangladesh(7 000)
Sri Lanka(3 000)
Maldives(<100)
DPR Korea(No cases reported
% of adult population infected with HIV
<0.1%
0.1 – 0.49%
0.5 – 0.99%
≥ 1.0%
Source: Reports of HIV estimates, national AIDS programmesNote: Numbers in parentheses include estimated number of people living with HIV/AIDS, figure are rounded off
Timor-Leste(<100)

Tuberculosis Control in the South-East Asia Region15
Table 4: Estimated HIV prevalence among adult populations and the number of people living with HIV infection in Member States of the SEA Region, 2009
Country Proportion (%) of adult population infected with HIV prevalence
Estimated number of people living with HIV
Bangladesh <0.1 7000
Bhutan 0.1 <1000
DPR Korea No reported HIV positive individual till date
India 0.3 2,400,000
Indonesia 0.2 190,000
Maldives <0.1 <100
Myanmar 0.6 240,000
Nepal 0.4 64,000
Sri Lanka <0.1 3,000
Thailand 1.4 610,000
Timor-Leste <0.1 <1000
Total 0.3 Approx 3.5 million
Source: SEA Region HIV Report, 2010.
A significant proportion of PLHIVs are also infected with tubercle bacilli and are thus at a high risk of developing TB. However, most of the incident TB cases continue to emerge among HIV-negative people.
The estimated prevalence of HIV infection among TB cases in different countries of the Region is presented in Table 5.
Table 5: Estimated HIV prevalence among incident TB cases in Member States of the SEA Region, 2009
Country Estimated HIV prevalence among TB cases
Bangladesh 0.2%
Bhutan <0.1%
DPR Korea NA
India 6.4%
Indonesia 2.8%
Maldives <0.1%
Myanmar 9.2%
Nepal 2.4%
Sri Lanka 0.1%
Thailand 17%
Timor-Leste 1.1%
SEA Region (average) 5.7%
Source: SEA Region HIV Report, 2010.

Tuberculosis Control in the South-East Asia Region16
2.4 Drug-resistant TB Well-functioning national TB control programmes in the Region achieving high treatment success rates has resulted in maintaining the slow but steady decline in TB incidence rates during the past decade. This has also led to low levels (Range: 1.7–4.2%) of multidrug-resistance (MDR) among newly detected cases. Among previously treated cases in the Region, MDR-TB rates range from 10.0–34.7%. However, given the large numbers of TB cases in the SEA Region, this translates to 130 000 MDR-TB cases (110 000–170 000), accounting for nearly one third of the world’s MDR-TB cases. Country-wise estimated burden of MDR-TB is presented in Table 6.
Extensively drug-resistant TB (XDR-TB) has also been reported from five countries of the Region: Bangladesh, India, Indonesia, Nepal and Thailand.
Considerable efforts are required to expand the capacity for quality assured drug susceptibility testing in the Region in order to more accurately estimate the extent of drug-resistant TB. Given the widespread availability and use of second-line drugs, and as laboratory capacity to conduct second-line drugs susceptibility testing increases, additional numbers of patients with XDR-TB are likely to be identified.
Table 6: Estimated MDR-TB cases and rates in SEA Region Member Countries, 2010
Country Source of estimates
% MDR among new TB cases (95% CI)
% MDR among previously treated TB cases (95% CI)
Number of MDR-TB among incident total TB cases (95% CI)
Bangladesh model 2.2 (0.0–5.6) 14.7 (0.0–39.6) 9 800 (1 000–19 000)
Bhutan model 2.2 (0.0–5.6) 14.7 (0.0–39.6) 33 (4–61)
DPR Korea model 2.2 (0.0–5.6) 14.7 (0.0–39.6) 3900 (658–7 200)
India DRS,a 2005 2.3 (1.8–2.8) 17.2 (14.9–19.5) 99 000 (79 000–120 000)
Indonesia DRS,b 2004 2.0 (0.5–6.9) 14.7 (0.0–39.6) 9 300 (0–21 000)
Maldives model 2.2 (0.0–5.6) 14.7 (0.0–39.6) 3 (0–6)
Myanmar DRS, 2007 4.2 (3.2–5.6) 10.0 (7.1–14.0) 9 300 (6 400–12 000)
Nepal DRS, 2007 2.9 (1.9–4.3) 11.7 (7.6–17.6) 1 700 (990–2 300)
Sri Lanka DRS, 2006 0.2 (0.0–1.0) 18-21% 63 (0–130)
Thailand DRS, 2006 1.7 (1.1–2.6) 34.5 (28.2–41.5) 2 900 (2 100–3 800)
Timor-Leste model 2.2 (0.0–5.6) 14.7 (0.0–39.6) 130 (6–260)a Estimates based on subnational drug resistance data. b DRS Survey in Indonesia was completed for Mimika district (2004) and the Central Java province (2006).
Mimika district: MDR-TB in newly diagnosed TB cases: 2.0 %. Central Java province: preliminary result; MDR-TB in newly diagnosed TB cases was: 1.8% and among previously treated TB cases was: 16.7%.
DRS = drug resistance surveillance or survey data; CI = confidence interval; MDR-TB = multidrug-resistant TB

Tuberculosis Control in the South-East Asia Region17
3.1 DOTS coverageDOTS coverage, defined as the proportion of population living in administrative areas with access to DOTS services, increased steadily in the WHO South-East Asia Region from 1995 onwards. Almost the entire population of the Region had access to DOTS by the end of 2007 (Figure 9).
3
Achievements
Figure 9: Population coverage by DOTS services, SEA Region 1997-2010
Source: Tuberculosis control in the South-East Asia Region, Annual Reports 1996-2009, WHO/SEARO
Year
100
90
80
70
60
50
40
30
20
10
0
% o
f pop
ulat
ion
cove
red
19952000
20012002
20032004
20052006
20071999
19981997
19962008
20092010

Tuberculosis Control in the South-East Asia Region18
3.2 Case-notifications
3.2.1 Trends in case-notificationsFigure 10 shows the trends in numbers of cases notified in the Region since 1993 for all forms of TB and new smear-positive (NSP) cases. Notifications continue to rise, reflecting improved case-finding efforts in Member States over time. There is a much sharper increase in notifications of all forms of TB, possibly due to increasing registration of smear-negative and extra-pulmonary cases following the involvement of the private sector and medical teaching institutions.
Figure 10: Trends in TB cases notified, SEA Region 1993-2010
Sources: Tuberculosis control in the South-East Asia Region, Annual Reports 1996–2009, WHO-SEARO; Annual Reports, National TB Programmes, SEA Region Member States, 2010.
The trends in case-notification rates of NSP cases for the five high-burden countries and other (intermediate and low-burden) countries in the Region are presented in Figures 11a and 11b respectively.
In Bangladesh, an increasing trend was observed until 2006 following which notification rates have remained fairly stable. In India, notification rates have continued to rise, primarily due to a tangible increase in case-finding efforts. At the same time, there has been increase in the involvement
Year
Cas
es n
otifi
ed
1995
2000
2001
2002
2003
2004
2005
2006
2007
1999
1998
1997
1996
2008
2.500.000
2.250.000
2.000.000
1.750.000
1.500.000
1.250.000
1.000.000
750.000
500.000
250.000
020
09
All cases NSP

Tuberculosis Control in the South-East Asia Region19
Figure 11a: Trends in annual NSP TB case-notification rates for high-burden countries in the SEA Region, 1995–2009
Sources: Tuberculosis control in the South-East Asia Region, Annual Reports 1996–2009, WHO-SEARO; Annual Reports, National TB Programmes, SEA Region Member States, 2009.
Figure 11b: Trends in annual NSP TB case-notification rates for intermediate and low-burden countries in the SEA Region, 1995–2009
Sources: Tuberculosis Control in the South-East Asia Region, Annual Reports 1996–2009, WHO-SEARO; Annual Reports, National TB programmes, SEA Region Member States, 2010
Note: NSP notification rates for 2008 calculated using revised population estimates for 2008 by Population Division, United Nations.
Year
Cas
es n
otifi
ed p
er 1
00 0
00 p
opul
atio
n
1995
2000
2001
2002
2003
2004
2005
2006
2007
1999
1998
1997
1996
Bhutan
DPRK
2008
140
120
100
80
60
40
20
0
Maldives
Nepal
Sri Lanka
Timor Leste
Year
Cas
es n
otifi
ed p
er 1
00 0
00 p
opul
atio
n
1995
2000
2001
2002
2003
2004
2005
2006
2007
1999
1998
1997
1996
BangladeshIndia
2008
100
90
80
70
60
50
40
30
20
10
0
IndonesiaMyanmar
Thailand
2009
2009

Tuberculosis Control in the South-East Asia Region20
of health-care providers from other sectors in programme case-finding and treatment activities.
In Indonesia, following a period of steady increase there was a drop in NSP notification rates in 2007, attributed to the temporary cessation of Global Fund support for a period of nine months. In Myanmar, a steady increase in notification rates was observed from the year 2000 to 2007; and the decline in 2008 may be related to funding problems. A declining trend has been observed in Thailand since 2006 but it is reversing in 2009.
In DPR Korea, a sharp increase in the notification rates has been observed in the last three years. This was primarily due to the introduction of active case-finding and involvement of other sectors. Active case-finding was adopted as a supplementary strategy since a perceptible gap was observed between case-notification rates and the revised estimates of the incidence of TB in the country, following a national tuberculin survey among children in the year 2007 that revealed a high ARTI. There was also increased availability of drugs through support from GDF and a jump in smear-negative cases registered for treatment. In Sri Lanka, an increase in notifications was recorded since 2006. In Nepal, more or less stable notification rates have been observed. A steady increase has been recorded in Bhutan since 2005. A consistently declining trend has been observed in Maldives. The trends in Timor-Leste have been fluctuating since the creation of the country with significant increase in notification rates in 2009.
3.2.2 Case-notifications in 2009Table 7 shows the absolute numbers of cases notified by type of TB in each Member State of the Region for the year 2009. A total of 2,124,370 notified cases of tuberculosis (new and relapses) were reported, which represents a case-notification rate of 119 per 100 000 population. Of those, 48% were new smear-positive pulmonary cases. Five high-burden countries from the Region (Bangladesh, India, Indonesia, Myanmar and Thailand) notified 95% of all NSP cases in the Region and contributed to 37% of the total notifications globally.
There was an increase of 1.7% in the numbers of cases (of all forms) notified in 2009 as compared with 2008 (Table 7). It is difficult to evaluate the change compared with 2008 for re-treatment cases notified, other than relapses, because Bangladesh did not report re-treatment cases. It is likely that certain types of re-treatment cases are still under-reported in several Member countries.

Tuberculosis Control in the South-East Asia Region21
Tabl
e 7:
Est
imat
ed in
cide
nce
and
case
s no
tifie
d (b
y ty
pe o
f TB
patie
nts)
in th
e M
embe
r cou
ntrie
s, S
EA R
egio
n, 2
009
Cou
ntry
Estim
ated
inci
denc
e of
al
l for
ms
(in th
ousa
nds
with
con
fiden
ce
inte
rval
s)
TB c
ases
not
ified
New
sm
ear-
posit
ive
New
sm
ear-
nega
tive
New
ex
trapu
l-m
onar
y
Rela
pse
Trea
tmen
t af
ter
failu
re
Trea
tmen
t af
ter
defa
ult
Oth
er re
-tre
atm
ent
Type
un
know
nTo
tal
notif
icat
ions
Bang
lade
sh36
0 (
300–
340)
109
311
25 3
37
21 9
77
4 11
0 0
0 0
0 16
0 73
5
Bhut
an1.
1 (0
.9–1
.3)
434
285
355
51
16
9 0
0 1
150
DPR
Kor
ea82
(70
–96)
29 3
66
32 4
91
12 2
32
2 24
7 2
312
1 65
1 8
366
0 88
665
Indi
a2
000
(1 6
00–2
400
)62
4 61
7 38
4 11
3 23
3 02
6 10
8 36
1 18
870
73
549
88
976
1
796
1 53
3 28
6
Indo
nesia
430
(350
–520
)16
9 21
3 10
8 61
6 11
215
3
710
225
723
1 03
0 0
294
732
Mal
dive
s0.
12 (
0.10
–0.1
4)45
13
41
1
0 1
0 0
101
Mya
nmar
200
(160
–240
)41
357
50
919
31
509
4
558
1 33
1 51
8 3
247
0 13
3 43
9
Nep
al48
(39
–58)
15 4
42
9 79
4 7
054
2 59
8 27
9 24
0 0
0 35
407
Sri L
anka
13 (
11–1
6)4
764
1 99
6 2
358
196
89
124
261
0 9
880
Thai
land
93 (
75–1
10)
32 8
10
20 0
58
9 14
3 1
964
575
726
664
0 65
940
Tim
or–L
este
5.6
(4.6
–6.8
)1
206
3 09
5 40
6 41
8
3 0
0 4
759
SEA
Reg
ion
3 30
0 (2
900
–3 7
00)
1 02
8 56
5 63
6 71
7 32
9 31
6 12
7 83
7 23
705
77
544
102
544
1 79
6 2
328
094
SEA
Reg
ion
(200
8)N
/A*
1 00
7 38
5 63
5 94
3 31
0 83
0 12
2 83
6 23
681
82
661
10
2 15
1 1
866
2 28
7 51
2
Perc
enta
ge
chan
ge
2009
ver
sus
2008
2.1%
0.1%
5.6%
3.9%
0.1%
–6.6
%0.
4%–3
.9%
1.7%
*The
met
hod
to c
alcu
late
est
imat
es c
hang
ed in
201
0, th
eref
ore
new
and
old
est
imat
ed s
houl
d no
t be
com
pare
d.
Sour
ces:
Ann
ual R
epor
ts, N
atio
nal T
B Pr
ogra
mm
es, S
EA R
egio
n M
embe
r Sta
tes,
200
9.

Tuberculosis Control in the South-East Asia Region22
About 50% of all notified new cases in the Region were new smear–positive cases (Figure 12). Among all new cases of pulmonary TB (PTB), 62% were smear-positive in the Region as a whole, with a range being from 28% in Timor - Leste to 81% in Bangladesh.
About 17% of all new cases in the Region were extra-pulmonary cases. This proportion varied in different countries, ranging from 4% in Indonesia to 33% in Bhutan and 41% in Maldives (Figure 12).
The proportion of smear-positive re-treatment cases out of all smear - positive cases varied between 3 and 24% (Figure 13). The highest proportions were reported from India (24%), DPR Korea (19%), Nepal (17%) and Bhutan (15%). The proportion of relapses from among all smear-positive cases varied between 2% and 14%, with the highest being from India, DPR Korea, Nepal, Bhutan and Myanmar.
An increasing trend in the proportion of relapse cases was seen over the previous years in Bangladesh, Bhutan and DPR Korea, while the proportion of relapses decreased for India, Nepal and Thailand in 2009.
Figure 12: Proportion of smear–positive pulmonary TB (PTB), smear-negative PTB and extra-pulmonary TB cases out of all new
notified cases in Member States, SEA Region, 2009.
Source: Annual Reports, National TB programmes, SEAR Member states, 2010.
Bang
lade
sh
Bhut
an
DPR
Kor
ea
Indi
a
Indo
nesia
Mal
dive
s
Mya
nmar
Nep
al
Sri L
anka
Thai
land
Tim
or-L
este
SEA
Regi
on
Extra-pulmonary TB
Smear-negative PTB
Smear-positive PTB
0 %10 %20 %30 %40 %50 %60 %70 %80 %90 %
100%

Tuberculosis Control in the South-East Asia Region23
Figure 13: Proportions of different types of smear–positive cases among all smear–positive cases reported in Member States of the
SEA Region, 2009
Source: Annual Reports, National TB Programmes, SEA Region Member States, 2010
0%
20%
40%
60%
80%
100%
Bang
lade
sh
Bhut
an
DPR
Kor
ea
Indi
a
Indo
nesia
Mal
dive
s
Mya
nmar
Nep
a l
Sri L
anka
Thai
land
Tim
or-L
este
SEA
Regi
on
Treatment after defaultTreatment after failureRelapseNSP
3.2.3 Age and sex distribution of notified NSP cases in 2009Figure 14 shows the age and sex distribution of notified new smear–positive cases in 2009 in the Region. Approximately 77% of the cases belonged to the most productive age groups between 15–54 years; 75% being among males and 81% among females. Compared with 2008 there has been a slight increase in the number of cases belonging to >54 years.
The percentage of cases in the age group of 0–14 years is 1.8 for the whole Region, suggesting under reporting of paediatric cases. No breakdown was reported in the age group of 0–4 and 5–14 years by the countries in the Region.
The male-to-female ratio of the numbers of notified NSP cases in 2009 varied from 1.0 in Bhutan to 3.0 in Sri Lanka, and was 2.0 for the Region as a whole.
3.3 Treatment outcomesThe treatment success rate among new smear–positive cases enrolled for treatment during 2008 was 88% for the Region as a whole. It was 85% or more

Tuberculosis Control in the South-East Asia Region24
Figure 14: Age and sex distribution of notified new smear–positive cases in the SEA Region, 2009
Sources: Annual Reports, National TB Programmes, SEAR Member States, 2010.
160 000
140 000
120 000
100 000
80 000
60 000
40 000
20 000
0
NSP
cas
es n
otifi
ed
0-14
Male Female
15-24 25-34 35-44 45-54 55-64 65+
in nine out of eleven countries (Table 8). The overall cure rate in the Region for new smear-positive cases was 84.2% and the treatment completion rate was 3.8% for the cases registered in 2008.
The overall case-fatality rate (CFR), default and failure rates were 4%, 5% and 2% respectively among new smear–positive cases registered for treatment in 2008.
In Thailand, the treatment success among NSP cases was lower than the target due to a CFR of 7%. This is probably due to the higher CFR among co–infected TB/HIV cases.
The treatment success among NSP cases was lower than the target in Maldives, where about 9% of cases were not evaluated for outcomes of treatment.
Default rates among NSP cases were high (>5%) in India, Sri Lanka and Timor - Leste.
The success rate among re–treatment cases is lower than in new cases, being 74% for the Region, ranging from 66% to 82% among the countries. Similarly, while the case-fatality rate and failure rate among new smear-positive cases are low, there are more than double among the re-treatment cases,

Tuberculosis Control in the South-East Asia Region25
Tabl
e 8:
Tre
atm
ent o
utco
mes
am
ong
case
s no
tifie
d in
200
8 by
type
of c
ases
, Mem
ber S
tate
s of
the
SEA
Reg
ion
Cou
ntrie
sN
ew s
mea
r–po
sitiv
e ca
ses
Re–t
reat
men
t cas
es
Not
ified
Succ
ess
rate
Cas
e fa
talit
y ra
te
Failu
re
rate
Def
ault
rate
Not
ev
alua
ted/
trans
fer
out
Not
ified
Succ
ess
rate
Cas
e fa
talit
y ra
te
Failu
re
rate
Def
ault
rate
Not
eva
luat
ed/
trans
fer o
ut
Bang
lade
sh10
6 08
991
41
22
5 09
1–
––
––
Bhut
an35
491
33
03
7079
316
11
DPR
Kor
ea28
026
892
42
214
170
823
103
2
Indi
a61
5 97
787
42
61
289
285
747
413
2
Indo
nesia
166
376
912
14
25
430
724
314
7
Mal
dive
s53
834
04
90
00
00
0
Mya
nmar
41 2
4785
63
52
8 63
173
125
73
Nep
al14
640
894
13
31
954
7610
55
5
Sri L
anka
4 64
685
62
71
393
708
215
5
Thai
land
33 0
7882
72
44
3 46
866
94
714
Tim
or–L
este
867
855
07
335
7111
611
0
SEA
R1
011
353
884
25
132
8 52
774
74
122
Sour
ce: A
nnua
l Rep
orts
, Nat
iona
l TB
Prog
ram
mes
, SEA
R M
embe
r Sta
tes,
201
0.

Tuberculosis Control in the South-East Asia Region26
Figure 15: Estimated TB prevalence, incidence and notification rate, SEA Region, 1990–2009
Notification rate (all forms)
Estimated prevalence all forms
Rate
per
100
000
pop
ulat
ion
400
350
300
250
200
150
100
50
01990 2000 2005 2006 2007 2008
Year
2009
Estimated incidence all forms375
183
48
1995
278
182
27
being respectively 7% and 4% for the whole Region. Default rate among re-treatment cases is also high in the Region (12%), and is particularly in India (13%), Indonesia (14%), Sri Lanka (15%) and Timor–Leste (11%). These high default rates among re-treatment cases are a cause of concern, as well as rates of failure in DPR Korea (10%) and Bhutan (16%), since many of these cases could have multidrug-resistant TB.
3.4. Reporting progress towards global targetsWith the fifteenth annual report, “Global Tuberculosis Control 2010”, WHO ceased publishing data on case-detection rates of new smear–positive TB cases. The CDR of new smear-positive TB >70% is no longer a global target. One of the reasons behind this decision is the difficulty to obtain reliable estimates for the denominator to this indicator that is not routinely directly measurable. Another reason is the current focus on universal case detection. In fact, due to new diagnostics that allow a definite diagnosis of people with smear–negative TB make the focus on the detection of only smear–positive cases increasingly outdated.
To monitor the performance of TB control efforts in a country the focus will be on case-notifications (in absolute numbers and rates) and treatment success rate, which are both directly measurable and an important indicator of the quality of TB management and care.

Tuberculosis Control in the South-East Asia Region27
No target has been set for case-notification. On the other hand, the global target for treatment success rate by 2015 has been increased to 90%.
In 2009, nine countries in the Region achieved or surpassed the 85% treatment success target among new smear-positive cases; the overall treatment success rate in the Region as a whole was 88%, which is close to the current target of 90%, three of the eleven Member States have achieved the new target already.
The case-notification rate of all forms of TB is steadily increasing since 2005 (Figure 15), although it is still far from TB incidence that represents the ideal goal in terms of universal access.

Tuberculosis Control in the South-East Asia Region28
4.1 DOTSComplete geographical coverage with DOTS services has been achieved in the Region since 2007. Considering the extent of DOTS coverage and the continuous increase of cases notified over time, and with over 15 million TB patients treated during past 10 years, the WHO SEA Region is on the move towards universal access.
4.2 Strengthening national laboratory networksQuality-assured smear microscopy services are available through the laboratory networks in all 11 Member States of the Region.
National reference laboratories (NRLs) in all Member countries (with the exception of DPR Korea, Maldives and Timor-Leste) have the capacity for microbacterial culture and DST. Although this capacity is limited in some countries, efforts have been made to strengthen laboratory capacity within countries in accordance with national plans and with the support of supranational reference laboratories (SNRL). All eleven countries have formally established linkages with SNRLs.
The NRLs in Bangladesh, India, Indonesia and Myanmar have been quality-assured for culture and drug susceptibility testing. Sri Lanka is in the process of being quality assured, and capacity for diagnosing MDR-TB is available as per national guidelines. The national reference laboratories in India
4
Key Milestones achieved in 2010

Tuberculosis Control in the South-East Asia Region29
and Thailand are currently undertaking DST for second-line anti-TB drugs to determine the extent of XDR-TB.
Reference laboratories in Bangladesh, Indonesia, Myanmar and Nepal are also engaged in rapid surveys for XDR-TB among microbacterial isolates from patients who have failed re-treatment regimens, through linking with the SRNLs in the global network.
Efforts are also on to introduce the newer molecular and liquid culture technology for the management of MDR-TB in high-burden countries in the Region with assistance through the EXPAND TB project, with assistance from the Global Laboratory Initiative (GLI), FIND and WHO-SEARO.
4.3 Addressing TB/HIV, MDR-TB and other challenges
4.3.1 TB/HIVAn estimated 3.4 million people are estimated to be living with HIV/AIDS in the South-East Asia Region. The Region is distinguished by a complex and heterogeneous HIV epidemic at different stages across different countries and in different geographical areas within individual countries. For example, approximately two thirds of the estimated HIV burden in India is to be found in six states in the South and North-East that make up only a third of the country’s population. In four states in southern India, HIV prevalence appears to be decreasing slowly.
In Indonesia, where the overall prevalence of HIV is low, three provinces have been reported to have higher rates of HIV. In other countries, such as Bangladesh and Nepal, increasing HIV prevalence among high-risk groups such as IDUs has raised concerns about the potential risk of a generalized HIV epidemic.
National TB/HIV guidelines and a comprehensive package of interventions (i.e. incorporating joint advocacy, coordination, training of staff and integrated service delivery), are being implemented in nine countries. TB/HIV activities are widely available in Thailand which continues to lead the Region in implementing the same. Services are being further expanded in 11 high-HIV prevalence states in India, as well as in Myanmar, Nepal and 10 provinces in Indonesia. Currently, the total population having access to a comprehensive package of TB/HIV services in the Region is estimated to be 600 million.

Tuberculosis Control in the South-East Asia Region30
Intensified case-finding is steadily increasing at integrated/HIV counseling, testing and care centres and cross-referrals between the TB and HIV programmes have been strengthened. Integrated management options are becoming more widely available as HIV services continue to expand. Infection control measures have been included in the national plans of Bhutan, India, Indonesia, Myanmar, Nepal and Thailand.
The TB recording and reporting systems in countries have been revised to include information on TB/HIV co-infection. However, the available data on HIV among TB cases remains insufficient and there is an urgent need to scale up and report on the screening of TB cases for HIV infection, and vice versa.
4.3.2 MDR-TBDuring the past two years, steady progress has been made in the Region in initiating MDR-TB cases on treatment. The Green Light Committee had approved the case management of patients with MDR-TB under national programmes in 10 Member countries. Bangladesh, India, Indonesia and Myanmar are in the process of expanding these services, while Nepal has already established ambulatory case management services for MDR-TB throughout the country. Maldives continues to treat the few cases that occur on a case-by-case basis. Bhutan and Sri Lanka have begun enrolling cases in 2010, while DPR Korea will apply to the GLC to establish MDR-TB case management under its national programme in early 2011. Until the end of 2010, more than 5000 patients with MDR-TB had been registered for treatment in the Region. Initial treatment success rates reported are in excess of 55%.
4.3.3 Paediatric TBGuidelines for diagnosis and treatment of paediatric TB have been widely disseminated in India and Indonesia. In India patient-wise drug boxes for children are also available under the programme. National guidelines for the management of childhood TB have also been finalized in Bangladesh and Myanmar. Myanmar, Nepal, DPR Korea and Sri Lanka received grants for anti-TB paediatric formulations through the Global Drug Facility (GDF).
Member States need to revise their national guidelines according to the “Rapid Advice” issued in October 2010 by WHO that provides evidence-based recommendations while considering the risks and benefits, feasibility, and cost and financial implications. National guidelines should be widely disseminated and staff trained on paediatric TB management in all Member States. Notification data for different paediatric age groups should be routinely available.

Tuberculosis Control in the South-East Asia Region31
The “Rapid Advice” issued in October 2010 is the latest revision to the guideline and aims to establish standards for high-quality treatment of tuberculosis in children by providing evidence-based recommendations having factored in risks and benefits, feasibility, and cost and financial implications.
The following ten key recommendations are made in the “Rapid Advice” and should be used by countries to adopt and adapt according to their national requirements:
1. Dosages of anti-TB drugs for the treatment of tuberculosis in children:
Rifampicin (R) – 15 mg/kg (range 10 – 20 mg/kg); max. dose 600 mg/day.
Isoniazid (H) – 10 mg/kg (range 10 – 15 mg/kg); max. dose 300 mg/day.
Pyrazinamide (Z) – 35 mg/kg (range 30 – 40 mg/kg).
Ethambutol (E) – 20 mg/kg (range 15 – 25 mg/kg).
2. Children living in settings where the prevalence of HIV is high or where resistance to isoniazid is high, or both, with suspected or confirmed pulmonary tuberculosis or peripheral lymphadenitis; or children with extensive pulmonary disease living in settings of low HIV prevalence or low isoniazid resistance, should be treated with a four-drug regimen (HRZE) for two months followed by a two-drug regimen (HR) for four months at the following dosages:
Rifampicin (R) – 15 mg/kg (range 10 – 20 mg/kg); max. dose 600 mg/day.
Isoniazid (H) – 10 mg/kg (range 10 – 15 mg/kg); max. dose 300 mg/day.
Pyrazinamide (Z) – 35 mg/kg (range 30 – 40 mg/kg).
Ethambutol (E) – 20 mg/kg (range 15 – 25 mg/kg).
3. Children with suspected or confirmed pulmonary tuberculosis or tuberculosis peripheral lymphadenitis who live in settings with low HIV prevalence or low resistance to isoniazid and children who are HIV-negative can be treated with a three-drug regimen (HRZ) for two months followed by a two-drug (HR) regimen for four months at the following dosages:
Rifampicin (R) – 15 mg/kg (range 10 – 20 mg/kg); max dose 600 mg/day.

Tuberculosis Control in the South-East Asia Region32
Isoniazid (H) – 10 mg/kg (range 10 – 15 mg/kg); max dose 300 mg/day.
Pyrazinamide (Z) –35 mg/kg (range 30 – 40 mg/kg).
4. Children with suspected or confirmed pulmonary tuberculosis or tuberculosis peripheral lymphadenitis living in settings with a high HIV prevalence (or with confirmed HIV infection) should not be treated with intermittent regimens (twice-weekly or thrice-weekly doses).
5. During the continuation phase of treatment, thrice-weekly regimens can be considered for children known to be HIV-uninfected and living in settings with well established directly-observed therapy (DOT).
6. Infants (aged 0–3 months) with suspected or confirmed pulmonary tuberculosis or tuberculosis peripheral lymphadenitis should be promptly treated with the standard treatment regimens as described above.
7. Streptomycin should not be used as part of first-line treatment regimens for children with pulmonary tuberculosis or tuberculosis peripheral lymphadenitis.
8. Children with suspected or confirmed tuberculosis meningitis should be treated with a four-drug regimen (HRZE) for two months, followed by a two-drug regimen (HR) for 10 months; the total duration of treatment being 12 months. The doses recommended for the treatment of tuberculosis meningitis are the same as those described for pulmonary tuberculosis.
9. Children with suspected or confirmed osteoarticular tuberculosis should be treated with a four-drug regimen (HRZE) for 2 months followed by a two-drug regimen (HR) for 10 months; the total duration of treatment being 12 months. The doses recommended for the treatment of osteoarticular tuberculosis are the same as those described for pulmonary tuberculosis.
10. Children with proven or suspected pulmonary tuberculosis or tuberculosis meningitis caused by multiple drug-resistant bacilli can be treated with a fluoroquinolone in the context of a well-functioning MDR-TB control programme and within an appropriate MDR-TB regimen. The decision to treat should be taken by a clinician experienced in managing paediatric tuberculosis. (for more information visit http://www.who.int/tb/challenges/children/en/).

Tuberculosis Control in the South-East Asia Region33
4.3.4 Other challengesNational plans for TB control in 11 Member States of the SEA Region are addressing the needs of populations at higher risk and those living in cross-border areas according to the specification for each country. Higher rates of case detection and quality case management are also addressed in national plans of Member Countries.
Infection control measures have been included in the national plans in Bhutan, India, Indonesia, Myanmar, Nepal, Sri Lanka and Thailand.
4.4 Public and private partnershipsA major strategy towards improving case detection and treatment success rates has been the inclusion of public health-care providers operating outside the ministry of health, such as the railways, military and prison health services, as well as private providers in all Member States where patients seek services through the private health sector. Nine Member countries have clear policies and strategies that envisage the involvement of other sectors.
Universities and medical schools are contributing to evidence-based policies and strategies through technical advisory groups at the national level.
The International Standards of TB Care have been endorsed by professional bodies such as medical associations in Bangladesh, DPR Korea, India, Indonesia, Maldives, Myanmar and Nepal. Intersectoral collaboration and public-private partnerships for delivery of services have been further scaled up in eight Member countries—Bangladesh, India, Indonesia, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste. Nearly 500 medical colleges, 25 000 private practitioners, 1500 large public and private hospitals, 200 corporate institutions, 2500 nongovernmental organizations, nearly 100 faith-based organizations and 900 prisons are now working with national TB control programmes.
Other recent initiatives have been the formal inclusion of the principles and practices of TB control in pre-service training and the establishing of referral mechanisms through providing lists of DOTS centres to teaching institutes. Nearly 1000 private laboratories are now included in national diagnostic networks and quality assurance mechanisms are being extended to these laboratories. Indonesia has intensified the training of staff private and public hospitals and laboratories. The country has also introduced coordination meetings between community health facilities and hospitals to improve transfer

Tuberculosis Control in the South-East Asia Region34
mechanisms between lung clinics and puskesmas. In Myanmar, services have been resumed throughout the network of Sun Quality clinics and the NTP plans further expansion of public-private mix services through the Myanmar Medical Association.
A large number of international and national NGOs form the bulwark of services in remote areas and among marginalized populations in several countries of the Region. The work of BRAC and Damien through MoUs with the Government in Bangladesh is an outstanding example of large-scale services delivery by NGOs that are contributing significantly towards achieving national targets for TB control.
A number of community-based approaches are also being incorporated into routine services delivery by national programmes. However, these need to be systematically documented and the experiences used to more widely replicate successful models in countries.
Business alliances in the Region such as the Thai Business Coalition in Thailand and the Business Alliance in India are emerging as players from the non-health private sector to have introduced TB services into their work places
4.5 Surveillance, monitoring and evaluationEfforts are being made to strengthen national TB surveillance systems focusing on the quality of data through focused attention paid to ensuring completeness of case reporting and accurate compilation and reporting of data.
In-depth analysis of several years of programme data to determine trends were undertaken in India, Nepal and Sri Lanka in 2010.
However, with the exception of the Maldives and Bhutan inferences on the incidence of TB cannot yet be estimated from the trends in case-notification rates in most countries. Population-based surveys, therefore, continue to serve as independent tools for evaluating the impact of TB control interventions and estimating the trends in the TB epidemic in most countries. Efforts were made to improve data on notification and monitoring of treatment outcomes of MDR-TB cases.
Joint monitoring missions on TB control were conducted in Bangladesh, Bhutan and Sri Lanka in 2010.

Tuberculosis Control in the South-East Asia Region35
4.6 Resources for TB controlDomestic funding for TB control continues to account for over half of the funding for national TB control programmes. Nine Member countries currently benefit from funds mobilized through the Global Fund over the previous nine rounds of GF grants. Applications to the Global Fund from Myanmar and DPR Korea have been approved during Round 8 and 9 respectively, and funding support is expected to commence in 2011.
By the end of 2009, a total of 26 proposals were approved by the Global Fund in support of TB control programmes in the Region. In addition, nine Member States benefit from funds from other development partners and donor governments with the exception of Bhutan and Maldives, where the only external funds are provided through WHO country budgets.
All eleven Member countries continue to access quality-assured affordable anti-TB drugs on a regular basis through grants or direct procurement services of the Global Drug Facility.
Five countries continue to benefit from GDF grants of first-line adult and paediatric anti-TB drugs. At the same time, nine countries are transitioning from being supported through GDF grants to utilizing the GDF direct procurement services using domestic sources, the Global Fund, World Bank, or other sources of bilateral funding. An exceptional 7th year of GDF grant of drugs was secured for DPR Korea and Myanmar.
4.7 Operational researchNational TB programmes and partners are engaged in carrying forward several operational research projects. Research proposals in the area of TB are being supported through the SEA Regional Office and TDR funding. Several other research projects are supported by WHO country offices through funds available at the country levels. Examples are KAP studies in Bangladesh, Bhutan, Indonesia, Myanmar and Sri Lanka; public-private mix (PPM) models in Bangladesh and Myanmar; hospital DOTS in Indonesia; seasonality in TB notifications, ambulatory management and outcome from MDR TB case management in Nepal; use of IPT and outcomes from cross-border TB control in Thailand; mortality studies in India, Indonesia and Myanmar; and approaches to community-based TB care in several countries. National workshops on operations research, priority setting and dissemination are held regularly in India. Nepal applied for funds through TBREACH (an initiative for early and improved case detection) in 2010 and was approved.

Tuberculosis Control in the South-East Asia Region36
5.1 Technical assistance All 11 Member States of the Region continue to receive technical assistance through the WHO Regional Office and country offices, in coordination and collaboration with international technical partners, namely the Centres for Disease Control, USA, the International Centre for Veterinary and Medical Sciences in Australia, the Royal Foundation for Tuberculosis in the Netherlands (KNCV), the Tuberculosis Coalition for Technical Assistance (TBCTA), the U.S. Agency for International Development (USAID), Foundation for Innovative New Diagnostics (FIND), PATH, the Institute of Tropical Medicine in Belgium, and The Union. The three WHO collaborating centres, namely the National TB Institute (NTI) and TB Research Centre (TRC) in India, and the SAARC TB and HIV/AIDS Centre in Nepal, and technical partners based in countries in the Region have also actively provided technical assistance to national TB programmes during the year 2010.
Technical missions were undertaken in all 11 Member countries during the year to provide support to national programmes in various areas, to review and update 5-year national plans, to undertake laboratory assessments and build laboratory capacity, to develop and implement guidelines for MDR-TB, TB-HIV and infection control, to improve drug procurement and supply management, data management and use, and to undertake impact assessments. Bhutan was supported to undertake assessment of ARTI survey; Myanmar supported in dissemination of prevalence survey; Indonesia, Nepal and Thailand were provided support to develop a protocol for the prevalence survey in 2011.
5
WHO Support in the Region

Tuberculosis Control in the South-East Asia Region37
Bangladesh, DPR Korea, India and Sri Lanka were assisted in undertaking drug resistance surveys. Bhutan, Sri Lanka and Thailand were assisted in 2010 to obtain approval from the WHO Green Light Committee and in developing guidelines for the management of MDR-TB cases. Nepal was supported to receive funds through Wave 1 of the TBREACH project. Assistance for health facility assessment and revision of action plan for implementation of PAL (Practical Approach to Lung Health) was also provided to Nepal. Countries were also assisted in developing and implementing measures to address the needs of vulnerable populations at higher risk, including those residing in cross-border areas, through the national plans for TB control.
The TB Technical Assistance Mechanism (TBTEAM) has been utilized to provide technical assistance to countries. The SEA Regional TBTEAM Focal Point identified the DPR Korea, Maldives, Nepal and Thailand national TBTEAM focal point(s) in collaboration with all national and external partners involved in respective countries in 2010. The regional roster of experts was further expanded and all proposed technical assistance missions to countries mapped. This helped in deploying suitable consultants to meet country requirements and facilitate the mobilization of additional resources from the Global Fund, TBREACH and other partners to support the countries.
5.2 Strengthening national laboratory networksTechnical assistance, coordinated through WHO, is being provided through the supranational reference laboratories (SNRLs) based at the Institute of Medical and Veterinary Science (Australia), Institute of Tropical Medicine (Belgium), Central Reference Laboratory, Gauting (Germany), the Tuberculosis Research Centre (India) and at the Bureau of TB at Bangkok, Thailand, to help establish culture and drug susceptibility testing (DST) facilities in countries in a phased manner in line with national plans. All 11 countries have formally established linkages with SNRLs.
Laboratory staff from several Member States were trained in the management of TB laboratories, quality assurance, microbacterial culture techniques, and drug susceptibility testing at an inter country workshop held at the SNRL at Bangkok in 2010, and through the ongoing Fellowships programme of WHO.
Bangladesh, Bhutan, India, Indonesia, Myanmar, Sri Lanka and Timor - Leste were provided with in country assistance in strengthening laboratory capacity for quality assurance, culture and DST. India was provided assistance in further expanding laboratory services for the rapidly expanding MDR-TB treatment programme.

Tuberculosis Control in the South-East Asia Region38
5.3 Capacity-building, information exchangeTraining, exchange of information and in country technical support for policy formulation, guideline development and monitoring have been the key areas of work for WHO-SEARO and country office staff during the past year. A meeting of the Regional TB Technical Working Group was organized in April 2010 in SEARO, New Delhi, to provide guidance to countries on adopting the updated WHO Guidelines on TB Treatment. An informal consultation on expanding laboratory services for TB control was held in May 2010 in New Delhi to assess current capacity, provide inputs required for expanding laboratory capacity for TB diagnosis in the SEA Region, and to provide guidance on the scope and feasibility of introducing newer TB diagnostics in countries of the Region.
A Regional Workshop on Advocacy, Communication and Social Mobilization (ACSM) on TB Care and Control was organized in Colombo in September 2010. Another 2 workshop was held on programmatic management on drug-resistant TB in Kathmandu in September 2010, followed by a Regional Workshop on Laboratory Diagnosis of Multidrug-Resistant TB in Bangkok in November 2010. Study tours and exchange visits between countries to learn from best practices were also supported. The regional and country offices have also supported the facilitation of several national-level trainings as well as trainings held at the three WHO collaborating centres in the Region.
5.4 Resource mobilizationSeveral Member States were assisted in mobilizing resources from development partners and bilateral donors during the year. Bangladesh, Bhutan, Indonesia, Sri Lanka, Thailand and Timor-Leste were supported to develop proposals for the GFATM Round 10. Countries were also supported in grant negotiations, developing work plans, conducting evaluations and preparing the necessary documentation required for continued funding.
The activities undertaken and coordinated by the TB unit at the Regional Office are supported mostly through USAID regional funding. Additional funds for technical assistance to countries are being sourced through the OGAC funded through USAID. Some funding continued to come through the Stop TB department at WHO/HQ for organizing regional workshops.

Tuberculosis Control in the South-East Asia Region39
5.5 Ensuring regular supplies of drugs and improving procurement and supply management Assistance continued to be provided for timely procurement of anti-TB drugs through grants and direct procurement mechanisms. All 11 countries in the Region embarked upon using Global Drug Facility services and products in one or the other way and accessed the low-cost and quality-assured fixed dosage combination drugs. Despite the fact that no stock-outs were reported from any country at the point of treatment delivery, Timor-Leste and Maldives announced zero stock of streptomycin at the central level and considered other arrangements for treatment of re-treatment cases. Due to the global shortage of streptomycin, GDF was not in a position to fulfil the emergency needs of Timor-Leste and Maldives. In addition delays in replenishing stocks of streptomycin in other countries of the Region were also anticipated, countries were alerted in advance about this. Additional support from WHO is planned for addressing the delays in port clearances reported from Bangladesh, Indonesia and Thailand, which led to loss of shelf life of drugs. Advocacy at the country level will be stepped up to increase government funding and timely disbursements of funds for the procurement of anti-TB drugs.
India, Nepal, Myanmar and Timor-Leste were assisted to receive support through UNITAID for the diagnosis and treatment of MDR-TB cases. All other countries in the Region were provided with paediatric anti-TB formulations through UNITAID. In country technical support and training to strengthen procurement and supply management systems were undertaken in Bangladesh, DPR Korea, Myanmar, Nepal and Thailand. A resource mobilization meeting held at Stanford University to help resolve the acute crisis in funding of first-line drugs in DPR Korea was also supported earlier in 2010.
5.6 MDR-TBAssistance to all countries (except Maldives, given the very few cases, and DPR Korea, which is scheduled for early 2011) was provided in preparation of applications for submission to the Green Light Committee (GLC) to establish sound programmes and access to concessionally-priced second-line drugs.
Missions were undertaken together with the GLC in countries that have commenced MDR-TB case management (Bangladesh, Bhutan, India, Indonesia, Myanmar, Sri Lanka, Thailand and Timor-Leste).

Tuberculosis Control in the South-East Asia Region40
The Regional Office also supported training of staff of national programmes and participating NGOs in the management of drug-resistant tuberculosis and provided assistance in evaluating and deploying newer diagnostics (such as liquid culture and molecular tests for rapid diagnosis of MDR-TB) together with FIND (Foundation for Innovative New Diagnostics) and UNITAID.
5.7 Operational research Countries were provided guidelines for submission of research proposals through the newly launched TBREACH initiative. Seven Member countries applied and one proposal from Nepal was approved in 2010.
India and Myanmar are being supported in deploying newer TB diagnostics through collaboration with the Foundation for Innovative New Diagnostics (FIND) to field-test the use of newer diagnostics such as line probe assays, liquid cultures and light emitting diode (LED) microscopes. Plans for supporting this initiative in Bangladesh and Indonesia in 2011 have been initiated. Myanmar, Thailand and India were assisted in developing protocols for initiating isoniazid preventive therapy (IPT) at selected sites and will have evidence for the implementation of IPT among people living with HIV/AIDS by early 2011.
5.8 Coordination, collaboration and partnershipsTo mobilize greater commitment for TB control in the Region, WHO at the country, regional and headquarters levels continued to interact with donors and development partners. The Region is represented on the Stop TB Coordinating Board and the Board of the Global Fund.
Staff from the Regional Office and country offices participated in and contributed to workshops and meetings held by WHO headquarters and partner agencies, namely:
The TB/HIV Technical Meeting on Global Consensus on Intensified Case-Finding and IPT (January 2010);
Sixth Meeting of the Subgroup on Public-Private Mix for TB Care and Control: Strengthening Health Systems through Engaging all Care Providers (February 2010);
Joint Operational Planning for WHO/SEARO and the Global Fund (March 2010);

Tuberculosis Control in the South-East Asia Region41
Meeting of Focal Points of WHO TB Laboratory and Supranational Reference Laboratory (April 2010);
Health System Strengthening Tool Assessment (April 2010);
Meeting of the Global TB STAG and Regional Advisers (June 2010); Global Laboratory Initiative Consultants Workshop to support TB Laboratory Strengthening efforts through Global Fund Round 10 Proposals (July 2010); and
The Regional Seminar on Decentralized Services on Primary Health Care (July 2010).
5.9 Advocacy, communication and social mobilization Bangladesh and Indonesia were supported to develop advocacy and communication road maps. During the Mock Technical Review Panel (TRP) for the GFATM Round 10 proposal, Bangladesh, Bhutan, Indonesia, Sri Lanka, Thailand and Timor-Leste were supported to strengthen the ACSM component. Many community-based initiatives have been established through the active involvement of NGOs in Bangladesh, India, Indonesia, Myanmar and Thailand. A framework for ACSM activities at the country levels has been finalized. Ongoing ACSM activities need to be properly documented, analysed for cost-effectiveness, and best practices emanating from these utilized for wider replication.
5.10 Monitoring and evaluationImpact assessments were supported in six Members States in the form of prevalence or annual risk of infection (ARI) surveys in Bangladesh, Bhutan, India, Indonesia, Myanmar and Thailand. Mortality surveys were supported in India, Indonesia and Myanmar. In-depth analysis of several years’ programme data to determine trends were undertaken in India, Nepal and Sri Lanka in 2010.
In country support and training on data management (updating of recording and reporting forms and software) were completed in Bangladesh, Bhutan and Nepal. Countries were also assisted in further improving supervision and monitoring of programme performance.
Joint monitoring missions on TB control were conducted in Bangladesh, Bhutan, and Sri Lanka in 2010.


Country Profiles


Tuberculosis Control in the South-East Asia Region45
With a population of about 162 million, Bangladesh is among the 22 countries with the highest burden of TB. The estimated prevalence and incidence rates of all forms of tuberculosis in 2009 were 426 and 225 per 100 000 population respectively. Bangladesh completed a survey of the prevalence of TB disease in 2009. A reassessment of the epidemiological burden of TB, using data from the survey combined with an in-depth analysis of surveillance and programmatic data, will be undertaken in 2011. The number of peripheral laboratories, sputum collection or smearing centres was increased to extend greater access to TB diagnostic services. The notification rate of all forms of TB and new smear-positive cases were 99 and 68 respectively, showing an increase compared with previous years. Treatment success rate among new smear-positive cases was 91% for the cohort of patients registered in 2008.
Data from drug resistance surveys indicate low levels of MDR-TB. Isolated surveys have indicated that MDR-TB rates among newly diagnosed cases range between 0.4% and 3% and between 3% and 15.4% among previously treated cases. A limited survey of drug susceptibility among patients failing category II regimens showed that 88% had MDR-TB. A nationally representative population-based survey has been initiated in 2010 to better assess the magnitude of drug resistance nationwide. The National Tuberculosis Reference Laboratory (NTRL) was set up in 2007. Upgrading and renovation of the National TB Reference Laboratory at National Institute of Diseases of the Chest and Hospital (NIDCH) in Dhaka were conducted in 2010. Establishment of three additional regional reference laboratories for culture and drug susceptibility testing in a phase-wise manner is planned for 2011.
Bangladesh

Tuberculosis Control in the South-East Asia Region46
In a GLC-approved project for the management of MDR-TB cases at the National Institute of Diseases of Chest and Hospital, Dhaka that was started in August 2008 enrolled 469 cases till the end of December 2010. The Damien Foundation extended its support for MDR-TB case management to an additional 30 million population.
HIV prevalence in the adult population (15–49 years) has been estimated to be low at 0.02%. A recent survey revealed an HIV prevalence of 7% among injecting drug users. This has raised concerns regarding the potential for transmission of HIV to other population groups. The National HIV Prevalence Survey among TB patients is planned to be undertaken in 2011. While a National TB/HIV Committee is now functional, collaboration between the National AIDS and STI Programme and the National TB Programme for TB/HIV activities need to be strengthened. A limited number of NGOs provide HIV counselling, prevention and care for TB-HIV co-infected individuals; capacity-building for wider implementation of TB/HIV interventions is planned for 2011.
TB services are part of an essential services package under the Health, Nutrition and Population Sector Programme (HNPSP) which is implemented through the primary health care system of the country. Bangladesh is an outstanding example of implementing TB control in partnership with NGOs. Community-based DOTS implemented through village doctors and the network of shasthya shebikas (community health volunteers) is the most common mechanism for supervising drug intake. Collaboration with garment manufacturers, who account for three million employees and are one of the largest industrial sectors, was formalized and plans developed for providing TB services in these companies.
Several private and corporate sectors are involved in TB control and in rendering services in line with international standards for TB care. Thirty seven public hospitals, including medical college hospitals and military hospitals, were involved till 2010. Services have also been established within the prison system. The data management software has been upgraded and a financial management software has been installed. The International Standards of TB Care (ISTC) have been sensitized to professional associations. An HRD plan has been developed and a Focal Point for HR designated at the central level. NTP guidelines have been included in the curricula for basic training of different categories of health staff and the curriculum for undergraduate/ postgraduate medical, paramedical and nursing students on DOTS, TB/HIV, MDR-TB is due to be prepared. The fifth Joint Monitoring Mission was conducted in October 2010.

Tuberculosis Control in the South-East Asia Region47
The TB programme benefits from Global Fund support through Rounds 5 and 8. This support is channelled through two principal recipients: the External Resource Division (ERD) of the Ministry of Finance (MoF) and BRAC. Bangladesh was also approved Round 10. WHO provides strong technical and operational support to the programme. In addition, USAID provides financial assistance to the NTP directly while several other donors are funding TB activities through NGOs. Some support for TB control is also made available through the HNPSP.
Major achievements Budgeting and costing of the National Strategic Plan.
Initiation of the Drug Resistance Survey (DRS) in 2010.
Preparation of 5-year National Strategic Plan for Infection Control.
National TB Prevalence Survey completed and disseminated.
MDR-TB pilot successfully ongoing on in NIDCH with plan for scale-up in place.
Upgradation and renovation of NTRL at NIDCH, Dhaka.
External quality assessment/assurance (EQA) systems for acid-fast bacilli (AFB) microscopy upgraded and standard operating procedures (SOP) developed.
Regional TB Reference Laboratory (RTRL) Chittagong is made operational.
Further expansion of public-private mix in TB control activities and involving the work place, e.g. BGMEA, achieved.
Drug storage capacity strengthened by establishing a separate store in the newly constructed hospital at Shyamoli, Dhaka.
Installation of financial management software.
Selection of international procurement agent.
Major challenges Ensuring uninterrupted supply of drug and logistics.
Ensuring sustainability of skilled and trained staff at different levels.
Scaling up the management of MDR-TB.

Tuberculosis Control in the South-East Asia Region48
Strengthening linkages with the National AIDS and STI programme for TB/HIV.
Further scaling up and strengthening of private-public collaborative interventions.
Ensuring quality control of and sustaining the quality of DOTS is a major issue.
Strengthening the diagnosis system of smear-negative, extra-pulmonary and child TB cases.
Activities planned for 2011 Establishment of the regional reference laboratories at Khulna, Barisal
and Sylhet for culture and drug susceptibility testing in a phase-wise manner.
Implementation of the Practical Approach to Lung Health (PAL).
Phase-wise expansion of TB/HIV collaborative activities.
Undertaking the national HIV prevalence survey among TB patients.
Developing capacity for wider implementation of TB/HIV, MDR-TB and PPM DOTS interventions.
Further expanding private-public collaborative activities.
Strengthening the procurement and supply management system.
Strengthening supervision and monitoring.
Scaling up of comprehensive advocacy, communication and social mobilization (ACSM) activities.
Developing appropriate curriculum for undergraduate/postgraduate medical, paramedical and nursing students on DOTS, TB/HIV, MDR-TB.
Conducting an assessment of the impact of the ACSM campaigns on the population and service recipients.
Capacity-building for diagnosis and management of smear-negative, extra-pulmonary and childhood TB.
Establishing a competent pharmacovigilance system.

Tuberculosis Control in the South-East Asia Region49
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Case-notifications by type of patients, 2009 Trends in TB case-notifications, 2000-2009
Trends in notified new smear-positive TB cases by age group among females, 2000-2009
0
20
10
40
50
30
70
80
90
60
Year
Cas
es n
otifi
ed p
er 1
00 0
00 p
opul
atio
n
2000 2001 2002 2003 2004 2005 2006 2007 20082009
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
20002001
20022003
20042005
20062007
20082009
0
20
40
80
100
120
60
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
nTrends in notified new smear-positive TB cases
by age group among males, 2000-2009
0
100
50
200
250
150
350
400
300
Year
Cas
es n
otifi
ed p
er 1
00 0
00 p
opul
atio
n
20002001
20022003
20042005
20062007
2008
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
2009
Treatment outcomes of new smear-positive cases, 2008 cohort
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t suc
cess
rate
(%)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Died 4%
Other 9%
Cured 89%
Completed 2%
Failed 1%
Transferred out 2%
Defaulted 2%
New smear-negative 16%
New extra-pulmonary 14%
Relapse 3%
New smear-positive 67%

Tuberculosis Control in the South-East Asia Region50
Estimates and notification rates for 2009, Bangladesh
Population* 162 220 768
Incidence of all forms of TB 360 000 (300 000–440 000)
Incidence rate of all forms of TB (per 100 000 population per year) 225 (183–270)
Prevalence of all forms of TB 690 000 (320 000–1 100 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 426 (198–696)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
51 (37–67)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
99
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
68
Case-detection rate (all forms of TB) 44 (37–54)
Treatment success rate (%) of new smear-positive cases for 2008 cohort
91
* Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition.

Tuberculosis Control in the South-East Asia Region51
With a population of approximately 697 335, Bhutan had an estimated TB prevalence and incidence rate of all forms of TB in 2009 of 179 and 158 per 100 000 population respectively. The notification rate of all forms of TB and new smear-positive cases were 161 and 62 respectively, showing a steady increase against previous years. The treatment success for the cohort of new smear-positive cases registered during 2008 was 91%. The TB control programme is fully integrated into the general health services with the majority of activities decentralized to the districts.
There is no representative data on the levels of anti-TB drug resistance in the country. However, it is estimated that 0.6% of newly diagnosed smear-positive TB cases have MDR-TB. A drug resistance survey is ongoing to better assess the levels of drug - resistant TB in the country. The Public Health Laboratory (PHL) has been linked to the Regional Supranational Reference Laboratory in Bangladesh and accredited for culture and first-line DST. Culture and DST facilities are provided at the Public Health Laboratory at the central level, while the culture facilities are being upgraded at the two regional referral hospitals. Additional laboratory staff are being trained to undertake quality-assured culture and DST.
It is proposed that DST will be done for all re-treatment cases through assistance from the designated SNRL until the national laboratory is fully set up, by which time DST may be extended to all smear-positive cases initiated on treatment. GLC approval for the management of MDR-TB cases has been
Bhutan

Tuberculosis Control in the South-East Asia Region52
obtained, guidelines for MDR-TB management have been finalized and second-line drugs are being procured through the Global Drug Facility (GDF).
Fixed-dose combination drugs (FDCs) have been procured through the Global Drug Facility (GDF) and introduced in the programme, replacing single drug formulations for first-line treatment for both adult and paediatric cases.
The prevalence of HIV infection among the general population is low. HIV sentinel surveillance carried out annually has also revealed low level of HIV infection. A national body responsible for coordinating TB-HIV activities was formed in 2007 and a national plan for collaborative TB-HIV activities has been developed.
A comprehensive HRD plan is in place and a Focal Point for HR designated at the central level. A monitoring mission was conducted in 2010.
Collaboration between NTP and partners, including the military and the bigger employment sectors, has been established. Two military hospitals are involved in delivering TB services. The National TB Control Programme is financially supported through both Rounds 4 and 6 of the Global Fund.
Major achievements ARTI survey data validation and analysis completed.
Drug resistance survey is ongoing.
Culture and DST established at the central reference laboratory.
Development of policy guidelines for management of MDR-TB and an infection control plan have been put in place.
Quality control of smear microscopy expanded to the subnational level.
Transfer referral mechanisms for TB cases in prisons developed.
Advocacy, communication and asocial mobilization on TB strengthened.
External review of TB programme completed.
Training of trainers on electronic reporting system for TB completed.
Training of TB in-charges on electronic reporting system for TB completed.
Guidelines for TB revised.

Tuberculosis Control in the South-East Asia Region53
Guidelines for MDR-TB management developed.
Fixed-drugs combinations of anti-TB drugs introduced.
Major challenges Inadequate human resources.
Frequent change of TB focal persons.
Inadequate monitoring and supervision.
Inadequate contact tracing and follow-up.
MDR-TB and TB/HIV collaborative activities.
Extent of DOT implementation.
Technical and managerial capacity for implementation of additional planned interventions.
Sustainability of financial resources.
TB surveillance and improvement of data management.
Activities Planned for 2011 Developing a manual for the training of trainers on comprehensive
TB control.
Improving data management, monitoring and supervision of programme implementation.
Strengthening TB/HIV collaborative activities.
Addressing TB control among cross-border and vulnerable populations.
Undertaking an external review of the National TB Control Programme.
Training of medical doctors on MDR-TB management.
Refurbishment of MDR-TB hospitalization room in two regional referral hospitals.
Preparation and printing of IEC materials on TB.
Procurement of second-line drugs through GLC.
Training of laboratory technicians.
Annual TB laboratory and annual TB review meeting.
Advocacy, communication and social mobilization.

Tuberculosis Control in the South-East Asia Region54
International training for laboratory technicians on DST in SNRL.
Procurement of DST reagents for the Public Health Laboratory.
Procurement of health products for 31 district hospitals and the PHL.
Quality assessment visit to the PHL by the SNRL.
Introduction of electronic reporting system for TB in all 30 reporting centres.
Training of medical doctors on the management of TB as per revised TB guidelines.
Notified new smear-positive TB cases by age group and sex, 2009
Notification rate of new smear-positive TB cases by age group and sex, 2009
Trends in TB case-notifications, 2000-2009
20002001
20022003
20042005
20062007
20082009
0
50
100
200
250
150
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
n
Case-notifications by type of patients, 2009
Relapse4%
Year
Male Female
0-14 15-24 25-34 35-44 45-54 55-64 65+
Num
ber o
f cas
es
0
20
40
60
80
100
120
140
160
New extra-pulmonary
31%
New smear-negative
25% New smear-positive
38%
Treatment after failure
1%
Treatment after default
1%
Other2%
Year
0-14 15-24 25-34 35-44 45-54 55-64 65+0
20
40
60
80
100
120
140
160
Male Female
Cas
es p
er 1
00 0
00 p
opul
atio
n

Tuberculosis Control in the South-East Asia Region55
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t suc
cess
rate
(%)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Treatment outcomes of new smear-positive cases, cohort of 2007
Cured89%
Completed2%
Other9%
Died 3%
Failed 3%
Defaulted 0%
Transferred 3%
Estimates and notification rates for 2009, Bhutan
Population* 697 335
Incidence of all forms of TB 1 100 (920–1 300)
Incidence rate of all forms of TB (per 100 000 population per year) 158 (132–186)
Prevalence of all forms of TB 1 300 (330–2 200)
Prevalence rate of all forms of TB (per 100 000 population per year) 179 (47–315)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
8.4 (4.6–17)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
161
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
62
Case-detection rate (all forms of TB) 102 (87–123)
Treatment success rate (%) of new smear-positive cases for 2008 cohort
91
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition

Tuberculosis Control in the South-East Asia Region56
With a population of nearly 24 million, the Democratic People’s Republic of Korea (DPR Korea) has an annual incidence and prevalence of all forms of TB of, respectively, 345 and 423 per 100 000 population. The notification rate of all forms of TB and new smear-positive cases were respectively 369 and 122, showing a steady increase compared with previous years, and particularly since 2007. The expected incidence was revised upwards significantly in 2007 following a national ARTI survey.
Given the significant gap between the estimated incidence and actual case-notifications, intensified and active case-finding in the community was adopted as a supplementary method for case-finding. The more active case-finding campaign and integration of previously non-DOTS sectors such as health facilities under the ministries of the military, security and railways has led to an increase in case-notifications. The treatment success rate for the cohort of patients registered in 2008 was 90%.
Patients with possible drug resistance were not being diagnosed and second-line regimens are not available through the programme. However, a national reference laboratory for culture and DST has been established at the Central TB Institute in Pyongyang. Guidelines for MDR-TB Management are due to be developed and a proposal will be submitted to the GLC to address drug-resistant TB in the country. There is no reliable data on the extent of MDR-TB in the country. However, re-treatment cases comprised 14% of all notified cases during 2009. A drug resistance survey is planned for 2011.
DPR Korea

Tuberculosis Control in the South-East Asia Region57
HIV has not been reported in the country. There is, however, a plan to establish HIV prevention activities.
A strategic plan has been developed for 2008–2015, in line with the Global Plan to Stop TB and the Regional Plan for TB Control 2008–2015. The government provides for over half of the programmes’ funding requirements in terms of staffing, infrastructure, drugs and surveillance. WHO continues to provide support to the programme in terms of technical assistance, training health staff, strengthening laboratory services, upgrading infrastructure, and monitoring and evaluation.
Regular supplies of anti-TB drugs have been ensured through the GDF grant mechanism from 2003 and the current grant has been extended until 2009. WHO-SEARO secured funds on an exceptional basis to provide up to 90% of funding for a further one year’s supply of drugs to cover the needs of 2010. Supplementary support is also received through the Eugene Bell Foundation and the Christian Friends of Korea. A proposal submitted to the Global Fund was approved during Round 8 although the negotiation have been protracted. A comprehensive HRD plan for the Ministry of Health as a whole and a GAVI HSS proposal for strengthening health services have been developed.
Major achievements DOTS is firmly in place with service delivery extending to even the
most peripheral level.
A national TB reference laboratory for culture and DST has been established.
M&E and supervision of DOTS implementation has been strengthened.
Logistic management system for drug supply and management strengthened.
TB estimates revised on the basis of ARTI survey.
Health facilities in other sectors involved in TB control and management.
Involvement of household doctors in DOTS institutionalized.
Standardized laboratory kits introduced.
Patient-wise kits introduced.
Global Fund-supported project initiated.

Tuberculosis Control in the South-East Asia Region58
Major challenges Sustaining funding to implement basic DOTS, shortages of laboratory
reagents and first-line drugs being a consequence.
Low level of documentation of DOTS by household doctors.
Inadequate laboratory capacity for undertaking laboratory QA.
Diagnosis of TB in children is not widely undertaken.
Lack of adequate information on pattern of MDR-TB in the country and non-availability of guidelines and drugs for MDR-TB.
Activities planned for 2011 Strengthening partnerships with donor agencies to expand of the
resource pool.
Strengthening of coordination with other sectors.
Undertaking systematic supervision of TB control and management activities.
Expansion of microscopic centres for TB.
Training on approaches to ACSM at all levels.
Printing and dissemination of IEC materials on TB prevention and control.
Undertaking second ARTI survey.
Undertaking the first MDR-TB survey and development of MDR-TB guidelines.
Submission of GLC application.
Providing technical support to the National TB Reference Laboratory for competently undertaking culture and DST activities.
Training paediatricians and TB staff on paediatric TB case management.

Tuberculosis Control in the South-East Asia Region59
Trends in TB case-notifications, 2000-2009
All cases New smear-positive
0
50
100
150
200
250
300
350
400
1999 2000 2001 2002 2003 2004 2005 2006 2007
Cas
es p
er 1
00 0
00 p
opul
atio
n
Year
2008
Case-notifications by type of patients, 2009
Treatment after failure 3%
Other re-treatment9%
New extra-pulmonary 14%New smear-negative 36%
Relapse 3%
Other 14%New smear
- positive 33% Treatment after default 2%
Trends in notified new smear-positive TB cases by age group among males, 2000-2009
Trends in notified new smear-positive TB cases by age group among females, 2000-2009
Treatment outcomes of new smear-positive cases, 2008 cohort
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Completed 6%
Cured 84%
Died 2%
Failed 4%
Defaulted 2%
Transferred2%
Other9%
Not evaluated Defaulted FailedDied Success rate
0%
20%
40%
60%
80%
100%
2000 2001 2002 2003 2004 2005 2006 2007 2008
Trea
tmen
t o
utco
mes
(%)
Year
0
50
100
150
200
250
300
350
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
0
20
40
60
80
100
120
140
160
180
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years

Tuberculosis Control in the South-East Asia Region60
Estimates and notification rates for 2009, DPR Korea
Population* 23 906 070
Incidence of all forms of TB 82 000 (70 000–96 000)
Incidence rate of all forms of TB (per 100 000 population per year) 345 (293–400)
Prevalence of all forms of TB 100 000 (30 000–180 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 423 (126–736)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
25 (13–44)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
369
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
122
Case-detection rate (all forms of TB) 93 (80–109)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 90
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition

Tuberculosis Control in the South-East Asia Region61
With a population of about 1198 million, India is the largest country in the Region. It ranks first among countries with the highest burdens of TB in the world and contributed over one fifth of the global incident TB cases in 2009.
The estimated prevalence and incidence rates of all forms of tuberculosis in 2009 were 249 and 168 per 100 000 population respectively. However, the WHO estimates for TB incidence, prevalence and mortality are provisional, pending the outcome of national consultations in 2011 to re-evaluate the TB burden. The notification rate of all forms of TB and new smear-positive cases were 128 and 52 respectively.
Since its inception, the programme, Revised National Tuberculosis Control Programme (RNTCP) has initiated almost 12 million patients on treatment. The programme, RNTCP has consistently achieved the global target of 85% treatment success rate among new smear-positive cases, with 88% achieved for the cohort of patients registered in 2008.
By the end of 2010, more than 19 laboratories were accredited by the Government of India’s (GoI) Revised National TB Control Programme (RNTCP) to undertake culture and drug susceptibility testing for the programme, among which four are from non-public sector providers. By the end of 2010, treatment services for MDR-TB patients were available at sites in 12 states, with a cumulative total of 2985 patients having been placed on RNTCP Category-IV treatment since August–September 2007. The RNTCP has developed an ambitious plan to scale up MDR-TB services in order to treat at least 9000 MDRTB patients
India

Tuberculosis Control in the South-East Asia Region62
annually in the country, and has garnered support under Round 9 of the Global Fund and from UNITAID to enable a rapid expansion of MDR-TB services in the next few years. In collaboration with FIND and WHO, RNTCP has completed a validation study on line probe assay (LPA) and has initiated a demonstration study of LPA.
It is estimated that around 2.3 million Indians are currently living with HIV. Recent country-level data shows that 4.85% of TB patients are HIV-positive. National surveillance has shown that the distribution of HIV among TB patients is highly heterogeneous, and is closely correlated with the distribution of HIV infection. Implementation of the revised “National Framework of Joint TB/HIV Collaborative Activities” began in early 2008 and interventions now cover the entire country. An “intensified TB/HIV package” was rolled out in 11 states and was expanded to 18 states in 2010, covering a population of over 600 million. By 2012, it is planned that all states will have implemented the “intensified TB/HIV package”.
Intensified TB case-finding has been implemented nationwide at all 5000 HIV testing centres (known as integrated counselling and testing centres, or ICTCs), with better reporting coming from states implementing the intensified TB-HIV package. During 2009, in states implementing the intensified TB-HIV package, more than 315 000 TB suspects were referred from ICTCs to RNTCP. Of them, 33 509 were diagnosed as having TB, 257 631 TB patients (55% of total TB patients registered in the states implementing the intensified TB-HIV package) were tested for HIV, and 31 047 (12%) were diagnosed as HIV positive. Based on pilot-testing of decentralized delivery of co-trimoxazole preventive therapy (CPT) for HIV-infected TB patients in three high-HIV prevalence districts, CPT has been incorporated into national policies.
Following a consultative meeting held in early 2008, the revised guidelines and schemes to operationalize RNTCP activities with NGOs and the private sector were implemented from October 2008. The RNTCP training material specifically designed for private practitioners has been revised and updated. Utilizing support received under the Global Fund’s Rolling Continuation Channel (RCC), RNTCP has further expanded its collaborative public-private mix (PPM) TB activities. The PPM project with the Indian Medical Association (IMA) is being expanded from six states to sixteen, and that with the Catholic Bishops’ Conference of India (CBCI) from eleven to nineteen states across the country. The RNTCP is progressively and successfully involving an ever greater number of medical colleges, NGOs, private practitioners and members of the corporate sector in its activities.

Tuberculosis Control in the South-East Asia Region63
Health services are administered in a decentralized manner at the level of the states and Union Territories (UT) through diverse public and private sector facilities. Policies for TB control activities are formulated at the central level in consultation with other stake holders, with the Central TB Division in the Ministry of Health and Family Welfare having the overall responsibility for the Revised National TB Control Programme (RNTCP).
The RNTCP plan and budgets are aligned with the National Health Plan. The National Rural Health Mission provides an opportunity for strengthening TB service delivery at the grass-root level. A Focal Point for HRD has been designated at the central level. The EPI centre software has been successfully transitioned to a Windows-based system. The last three-yearly joint Government of India-WHO monitoring mission of RNTCP was successfully conducted in April 2009. A wide range of experts, national and international, from many different partner agencies visited 17 districts in five states and one UT. The mission’s findings were presented to the Government of India in April 2009.
The Government of India supports around half of the central-level budget for RNTCP activities, including a World Bank credit. The RNTCP additionally benefits from donor funding and support from DFID, the Global Fund and USAID.
Major achievements National objectives outlined as providing universal access to quality
TB diagnosis and treatment for all TB patients in the community, with specific objectives encompassing early detection, scale-up of services for drug-resistant TB, detection of TB in HIV-infected persons, and extension of RNTCP services to patients diagnosed and treated in the private sector.
Decentralized diagnosis provided through a network of about 13000 quality assured sputum microscopy laboratories.
Treatment services decentralized through a network of hundreds of thousands of DOT centres/providers that use patient-wise boxes both for adults and paediatric patients.
Uninterrupted supply of first-line anti-TB drugs, with no stock-outs nationwide in any district.
Successful application under Round 9 of the Global Fund for additional financing for accelerated MDR scale-up and for the civil society response to TB.

Tuberculosis Control in the South-East Asia Region64
Inclusion in the UNITAID EXPAND-TB project, allowing the accelerated introduction of rapid diagnostics for MDR-TB in 43 laboratories nationwide.
Successful involvement in RNTCP of over 275 medical colleges, 2700 NGOs, 26 000 private practitioners and over 150 corporate sector health units.
Basic national framework for TB-HIV collaborative activities implemented nationwide, with an “intensified TB/HIV package” launched in 18 states covering a population of over 600 million.
More than 315 000 persons referred from HIV testing centres for TB diagnosis, and over 33 500 TB cases diagnosed.
Since RTNCP MDR-TB services were initiated in 2007, over 15 700 MDR suspects have been examined and 2985 patients initiated on treatment cumulatively.
Nineteen laboratories have been accredited for culture and DST for MDR diagnosis and treatment follow-up. Among these, four are from non-public sector service providers.
Line probe assay evaluated, demonstrated and incorporated as standard of care for MDR TB diagnosis, with systems in place for training, accreditation, external quality assurance, and routine reporting on quality of services.
Global Fund supported IMA and Catholic Bishops, Conference of India (CBCI) projects for enhancing the involvement of private practitioners and NGO services in RNTCP scaled up to 19 states.
National guidelines for Airborne Infection Control in health care and other settings and initiation of pilot-testing of guidelines in selected health care facilities across three states.
Major challenges Achieving universal access while maintaining and continuing to improve
the quality of services across the country.
Ensuring adequate staffing at all levels through improved human resource development, and further integration with the ongoing health systems strengthening efforts.

Tuberculosis Control in the South-East Asia Region65
Alleviating weaknesses in supervision capacity and quality, as well as in planning, monitoring and evaluation.
Enforcement of regulations for prescribing and sale of anti-TB drugs; and promoting rational use of first - and second-line anti-TB drugs outside the programme to prevent MDR and XDR-TB.
Scaling up culture, DST and treatment services for drug-resistant TB.
Developing effective models for the engagement of private providers at scale.
Scaling up TB-HIV collaborative activities effectively in areas where HIV services are dispersed and scarce.
Effectively promoting operational research to address local challenges.
Activities planned for 2011 Supporting the development of a National Strategic Plan to control
TB 2012–2017, with the planned and budgeted activities necessary to achieve the country’s goal of universal access.
Widening the network of quality assured laboratories and strengthening capacity of all the state-level culture and DST laboratories to undertake second-line DST.
Expanding the delivery of services for MDR-TB cases to all states.
Monitoring the implementation of the revised schemes for the involvement of NGOs and private practitioners across the country.
Phased scale-up of the implementation of the intensified TB/HIV package for nationwide coverage by 2012.
Review of all available studies and information on the TB burden, and re-estimation of TB incidence, prevalence, and mortality in cooperation with the Ministry of Health and national experts.
Evaluating, revising and disseminating airborne infection control measures in health facilities.
Developing and rolling out an integrated information system for MDR-TB services nationwide, and integrating laboratory results and patient management with outcome analysis and reporting.

Tuberculosis Control in the South-East Asia Region66
Trends in TB case-notifications, 2000-2009Case-notifications by type of patients, 2009
Trends in notified new smear-positive TB cases by age group among males, 2000-2009
Treatment outcomes of new smear-positive cases, 2008 cohort
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Trends in notified new smear-positive TB cases by age group among females, 2000-2009
New smear-positive41%
New smear-negative
25%
New extra-pulmonary
15%
RelapseOther new cases 0%
7% Treatment after failure 1%
Treatment after default
5%
Other retreatment
6%
Other12%
0
20
40
60
80
100
120
140
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Cas
es p
er 1
00 0
00 p
opul
atio
n
YearNew and relapse New smear-positive
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
0
20
40
60
80
100
120
140
160
180
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
0
10
20
30
40
50
60
1 2 3 4 5 6 7 8 9 10Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
Cured86%
Completed2% Died
4%
Failed2%
Defaulted6%
Transferred0%
Other14%
Success rates Unfavorable outcome
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
2000 2001 2002 2003 2004 2005 2006 2007 2008Year
Trea
tmen
t suc
cess
rate
(%)

Tuberculosis Control in the South-East Asia Region67
Estimates and notification rates for 2009, India
Population* 1 198 003 328
Incidence of all forms of TB 2 000 000 (1 600 000–2 400 000)
Incidence rate of all forms of TB (per 100 000 population per year) 168 (137–202)
Prevalence of all forms of TB 3 000 000 (1 300 000–5 000 000)
Prevalence rate of all forms of TB (per 100 000 population per year)
249 (107–417)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
23 (14–36)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
128
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
74
Case-detection rate (all forms of TB) 67 (56–83)
Treatment success rate (%) of new smear-positive cases for 2008 cohort
88
*Source: Global TB Report 2010.

Tuberculosis Control in the South-East Asia Region68
With a population of 227 million, Indonesia carries the fourth highest TB burden in the world.
The estimated prevalence and incidence rates of all forms of tuberculosis in 2009 were 285 and 189 respectively per 100 000 population. Tuberculin surveys and mortality studies were conducted successfully during 2006–2008 and data indicate that there continues to be a significant decline in TB prevalence in Indonesia.
Indonesia is planning to implement a nationwide TB prevalence survey to improve TB burden estimates and trends assessment. The notification rate of all forms of TB and new smear-positive cases were 128 and 74 respectively. Treatment success rate among new smear-positive cases was 91% for the cohort of patients registered in 2008.
The proportion of sputum smear-positive cases increased slightly from 53% in 2007 to 58% in 2009. The number of sputum smear-negative cases is also consistently rising over the last few years. This is most likely the result of increased notification by hospitals, since more and more hospitals and clinics are being linked to the national TB programme. The number of relapses and failures is still low at around 2%, suggesting that the overall rate of TB drug resistance is still relatively low. However, most of these data are from health centres where DOTS has been well established. Data from the private sector are not yet captured by the NTP while TB data from hospitals are only available for about 30% of the facilities that are currently linked to the NTP.
Indonesia

Tuberculosis Control in the South-East Asia Region69
Following the rapid expansion of DOTS over the last decade with significant improvement in case detection and treatment success, the National TB Programme implemented the second Strategic Plan for 2006–2010, built on a solid DOTS foundation in the public sector. It is and aimed to strengthen the quality of services delivery and increase the participation of hospitals in both the public and private sectors. The new TB Control National Strategy 2010–2014 is been finalized and the flagship theme is “Breakthrough toward Universal Access”.
Strategies such as hospital DOTS linkages, MDR-TB treatment, laboratory network improvement and strengthening of a quality assurance system, and HIV collaborative activities are currently being scaled up.
It is estimated that the prevalence of HIV among the adult population is 0.2% nationally, and there are about 293 000 people living with HIV in the country. The estimated number of people co-infected with TB/HIV is 12 000 (ranging between 7200 and 19 000). While HIV is characterized as a concentrated epidemic in Indonesia, it is at the stage of a generalized epidemic in Papua province, with an HIV prevalence of 2.5% in the general population. Twelve provinces have been identified as priority areas for HIV interventions, The estimated prevalence of HIV among incident TB cases is 3% nationally. In some provinces the reported TB/HIV co-infection rate is reported to be much higher, e.g. in DKI Jakarta (95%), Papua (68%), and East-Java (38.6%).
The national policy for TB-HIV collaboration activities is in place and guidelines and training materials have been developed. The NTP has revised the recording and reporting system, to include the information on TB-HIV. TB-HIV collaborative activities are being implemented in 10 high-HIV prevalence provinces. In these provinces, about 20 hospitals are involved in delivery of ART, VCT and DOTS services, while 10 centres are involved in VCT and DOTS services. Facilities for CD4 counts are available in a total of 26 hospitals in the country.
The drug resistance survey (DRS) was completed for Mimika District (2004), showing 2% MDR-TB cases among newly diagnosed TB cases. DRS in Central Java province has been completed and preliminary data suggest an MDR rate of 1.8% among the new cases and 16.7% among re-treatment cases. Another DRS survey is ongoing for East Java and a DRS plan was developed with the aim to ensure geographical representation within the country.
Efforts to expand and strengthen the national laboratory network are underway with assistance from the Supranational Reference Laboratory in

Tuberculosis Control in the South-East Asia Region70
Adelaide, Australia. Reference laboratories are being established in seven provinces. Five regional reference laboratories are being accredited for culture and DST.
GLC approval for the management of MDR-TB cases was obtained in 2008. Preparation for implementation of MDR-TB case management is in progress and 24 patients have been reported to have started on treatment by 2009. National programmatic and treatment guidelines for the management of MDR-TB have been developed and MDR-TB diagnostic and treatment services have commenced at two sites: in Jakarta at the Persahabatan hospital and in Surabaya city. Programmatic management of drug-resistant TB has been expanded to other three sites.
The TB programme is scaling up public-public and public-private partnerships and especially linkages with public hospitals; 560 public and medical college hospitals are in the process of being engaged in the programme. In addition, 408 prisons and 119 military hospitals are being involved. Teaching of the principles and practices of DOTS have been integrated into the medical school curriculum. The ISTC has been endorsed by the professional associations and is currently being widely disseminated among members of professional organizations. Advocacy, communication and social mobilization activities are being scaled up in different provinces of the country.
A comprehensive HRD plan is in place and a Focal Point for HR has been designated at the central level. Drug management remains suboptimal and needs strengthening. The NTP’s plan and budget are aligned with the national health sector development plan. However, there are challenges due to the decentralization of health services down to the level of each district in the country, and because of cuts in overall government budgets.
The Indonesian programme received support from several sources including the Global Fund Round 8, USAID (Tuberculosis Coalition for Technical Assistance), KNCV and DFID. Technical assistance is being provided by WHO, KNCV Tuberculosis Foundation, MSH Management Sciences for Health, FHI, JICA, ATS and IMVS.
Major achievements TB control has been included in the National Development Plan
2010–2014 with secure budget lines.
TB is a priority in the Strategic Plan of MoH.

Tuberculosis Control in the South-East Asia Region71
TB/HIV interventions were included in the Ministerial Decree of December 2009.
The new TB Control National Strategy 2010–2014 is being finalized with the theme “Breakthrough toward Universal Access”.
Hospital DOTS expansion covered 30% of the public and private hospitals.
Microscopic reference laboratories are operational in seven new provinces.
PMDT expansion from two sites to three more sites and a 5-year expansion plan developed.
Five laboratories were quality assured for culture and DST of FLD and second-line drugs (SLD) and linkage with the supranational reference laboratory established.
DRS was completed in Central Java and in the data collection stage in East Java.
DRS plan was developed and planned for sentinel sites according to the PMDT expansion plan and aimed to ensure geographical representation across the country.
TB/HIV collaborative activities covered high HIV prevalence provinces.
NTP worked in collaboration with the Human Resource Department of the MoH to strengthen HRD on TB and standardized the training curricula and materials.
Indonesian Medical Association is fully involved in improving medical professionals on ISTC, including private practitioners.
Major challenges Degree of commitment and contribution of local governments towards
TB control.
There are still unreached populations in remote areas (eastern part of the country in particular) such as migrants in big cities, inmates in prisons and high-risk populations vulnerable to HIV.
Expanding quality DOTS in hospitals, both government (under the MoH and other ministries) and private, including private practitioners.

Tuberculosis Control in the South-East Asia Region72
Rapid expansion of PMDT and maintaining a consistent degree of high quality.
Expansion of laboratory networks for culture and DST in islands other than Java and external quality assessment/assurance (EQA).
Introduction of new diagnostics (LPA, Xpert MTB/RIF) and their integration into the system.
Expansion of TB/HIV collaborative activities to cover more provinces.
Maintaining the capacity of TB-related staff amidst their high turnover.
Preventing the problem of stock-out of FLD, SLD and commodities.
Activities planned for 2011 Advocacy to increase commitment and contribution from local
governments to support TB control.
Support a comprehensive approach to increase the performance of DOTS in low-performance areas such as (unreached, under served populations).
Support the quality of DOTS expansion in hospitals, both government and private, and among private practitioners.
Support PMDT expansion and quality improvement, and the implementation of DRS.
Support laboratory network expansion and EQA for DST and microscopy.
Facilitate EXPAND-TB collaboration with NTP and the introduction/integration of new diagnostics into the system.
Support the expansion of TB/HIV collaborative activities.
Support the initiation of TB and diabetes collaborative activities (as per the recommendation of Round 10 of the Global Fund).
Support capacity strengthening of TB staff on DOTS, PMDT, TB/HIV and in other key areas.
Collaborate with all partners to prevent the problem of drug and commodity stock-outs.

Tuberculosis Control in the South-East Asia Region73
Trends in TB case-notifications, 2000-2009Case-notifications by type of patients, 2009
Treatment outcomes of new smear-positive cases, 2008 cohort
Trends in treatment outcomes of new smear-positive cases, 2000–2008
New smear-negative
37%
New extra-pulmonary
4%Relapse
1%
Other0%
New smear-positive58%
Treatment after failure 0%
Treatment after default 0%
Other retreatment
0%
New and relapse New smear-positive
0
20
40
60
80
100
120
140
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
New smear-positiveCured
83%
Completed8% Died
2%
Failed1%
Defaulted4%
Transferred2%
Other9%
Not evaluated Defaulted FailedDied Success rate
75%
80%
85%
90%
95%
100%
2000 2001 2002 2003 2004 2005 2006 2007 2008
Trea
tmen
t out
com
es (%
)
Year
Trends in notified new smear-positive TB cases by age group among males, 2001-2009
Trends in notified new smear-positive TB cases by age group among females, 2001-2009
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
0
50
100
150
200
250
2001 2002 2003 2004 2005 2006 2007 2008 2009Year
Cas
es p
er 1
00 0
00 p
opul
atio
n
15-24 years 25-34 years0-14 years 35-44 years45-54 years 55-64 years 65+ years
0
20
40
60
80
100
120
140
2001 2002 2003 2004 2005 2006 2007 2008 2009Year
Cas
es p
er 1
00 0
00 p
opul
atio
n

Tuberculosis Control in the South-East Asia Region74
Estimates and notification rates for 2009, Indonesia
Population* 227 345 088
Incidence of all forms of TB 430 000 (350 000–520 000)
Incidence rate of all forms of TB (per 100 000 population per year) 189 (153–228)
Prevalence of all forms of TB 660 000 (270 000–1 100 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 285 (119–482)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
27 (16–41)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
128
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
74
Case-detection rate (all forms of TB) 67 (56–83)
Treatment success rate (%) of new smear-positive cases for 2008 cohort
91
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition

Tuberculosis Control in the South-East Asia Region75
With a population of about 300 000, Maldives has an estimated prevalence and incidence rate of all forms of TB of 47 and 39 per 100 000 population respectively. The notification rate of all forms of TB and new smear-positive cases were 34 and 15 respectively. Treatment success rate among new smear-positive cases was 83% for the cohort of patients registered in 2008.
The National TB Control Programme (NTP) at the Centre for Community Health and Disease Control, Ministry of Health and Family, Maldives, is the central body for registration, planning, monitoring, training and evaluation of TB control activities since its establishment in 1976. TB is a notifiable disease and DOTS remains the core element of the National TB Control Programme. Coordination and collaboration with other health-care institutions, especially private health-care institutions, in identifying and accurately reporting identified cases has been established. All anti-TB drugs are available only through the government-run National TB Control Programme.
The main objectives of the NTP are to effectively improve and strengthen TB preventive activities, in addition to diagnosis and treatment of TB cases. In this regard, establishment of critical infrastructure and human resource development for intensified case-finding, early case detection and strengthening the microscopy network are critical. At the same time, social mobilization for increased community involvement, and utilization of available services and strengthening NTP management have also been identified as key areas.
Maldives

Tuberculosis Control in the South-East Asia Region76
Available data suggest that TB is relatively uncommon in Maldives and TB/HIV is not a major problem yet. Screening of all HIV-positive cases for active TB has taken place in collaboration with the HIV programme since 2003.
Drug susceptibility testing, if deemed clinically necessary for a particular patient, is undertaken by shipment of samples to TRC, Chennai, which is also the designated supranational reference laboratory for the country. Patients diagnosed with MDR-TB are managed clinically at the tertiary care hospital – the Indira Gandhi Memorial Hospital (IGMH) in Malé – and treatment is based on individualized regimens. Second-line drugs for the management of these cases are procured by the Ministry of Health and Family on a case-by-case basis.
The NTP is technically supported by WHO and benefits from an ongoing grant from the Global Drug Facility for first-line drugs.
Major achievements Development of a Health Master Plan for 2005–2015, which accords
high priority and adequate funding for TB control.
Collaboration with the HIV/AIDS programme.
Total ban on selling anti-TB drugs at local pharmacies and elsewhere in the country.
Development of MDR-TB national guidelines for managing MDR-TB.
Health system providing TB diagnosis and treatment free of cost.
Major challenges Strengthening and sustaining the laboratory EQA system.
Ensuring adequate supervision and monitoring of DOTS centre in the regions and atolls.
Lack of trained health workers for DOTS centres.
Lack of skilled staff at all levels of the programme.
Need of proper ventilation for infection control the main DOTS centres and laboratory at the Indira Gandhi Memorial Hospital.
Strengthen supervisory mechanism on quality assurance of smear microscopy.
Inadequate collaboration between care-providers and the National TB Programme.

Tuberculosis Control in the South-East Asia Region77
Activities planned for 2011 Continuation of postgraduate training in MD chest medicine/respiratory
medicine.
Develop, print and disseminate IEC information package on transmission and prevention of TB for schoolchildren.
Training workshop for community health workers on TB case management.
Awareness programme for expatriates recruiting agents on TB prevention and control.
Celebration of World TB Day 2011.
Notified smear-positive cases by age group and sex, 2009
Notification rate of new smear-positive TB cases by age group and sex, 2009
Year
0-14 15-24 25-34 35-44 45-54 55-64 65+
Num
ber o
f cas
es
0
2
4
6
8
10
12
14
18
Male Female
16
Year
0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
0
10
20
30
40
50
60
80
Male Female
70
Trends in TB case-notifications, 2000-2009Case-notifications by type of patients, 2009
Treatment after default
1%
New smear-negative 13%
New extra-pulmonary 41%
Other 1%
Relapse 1%
Year
All cases New smear-positive
0
10
20
30
40
50
60
20002001
20022003
20042005
20062007
20082009
Cas
es p
er 1
00 0
00 p
opul
atio
n
New smear-positive 44%

Tuberculosis Control in the South-East Asia Region78
Trends in Treatment outcomes of new smear-positive cases, 2000-2008
Treatment outcomes of new smear-positive cases, 2008 cohort
Cured 83%
Other 17%
Died4%
Defaulted 4%
Transferred 9%
Estimates and notification rates for 2009, Maldives
Population* 309 430
Incidence of all forms of TB 120 (100–140)
Incidence rate of all forms of TB (per 100 000 population per year) 39 (33–45)
Prevalence of all forms of TB 150 (42–250)
Prevalence rate of all forms of TB (per 100 000 population per year) 47 (14–81)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
2.6 (1.4–4.6)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
34
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
15
Case-detection rate (all forms of TB) 83 (72–97)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 83
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition.
YearNot evaluated Defaulted FailedDied Success rate
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
2000 2001 2002 2003 2004 2005 2006 2007 2008
Trea
tmen
t out
com
es (%
)

Tuberculosis Control in the South-East Asia Region79
With an estimated population of 50 million, Myanmar is among the 22 countries of the world with the highest burdens of TB. TB control is a priority in the country’s National Health Plan. DOTS was introduced in 1997 and was expanded to cover the entire country by 2003.
According to WHO, the estimated prevalence and incidence rates of all forms of tuberculosis were 595 and 404 respectively per 100 000 population in 2009, which is much higher than previous estimates. Results from a TB prevalence survey completed in both rural and urban areas in the Yangon Division in 2006 showed that the incidence of TB was 2.3 times higher than the previous WHO estimates for the country, and that TB affects mainly the younger age groups, which is characteristic of a growing epidemic.
To better assess the burden of TB in the country, a nationwide prevalence survey was conducted in 2009–2010. The National TB Programme has screened more than 51 000 people living in 70 geographical areas of the country. The survey has been one of the highest quality TB prevalence surveys WHO has ever been involved in. It was made possible with technical and financial support from the Japan International Cooperation Agency, Population Services International, Three Diseases Fund, Research Institute of Tuberculosis of Japan, United States Agency for International Development, and WHO. The prevalence survey confirmed a prevalence of around 597 TB cases per 100 000 population.
The notification rate of all forms of TB and new smear-positive cases were 267 and 83 respectively. The treatment success rate among new smear-positive cases was 84% for the cohort of patients registered in 2008.
Myanmar

Tuberculosis Control in the South-East Asia Region80
The National Reference Laboratory in Yangon and Mandalay perform cultures and first-line DST. Second-line DST is being undertaken at the SNRL in Bangkok. With support from EXPAND-TB (Expanding Access to New Diagnostics for TB) new TB diagnostic tools have been implemented in the two national reference laboratories, including liquid culture, first-line drug susceptibility testing, rapid immunoassay for species identification and line probe assay for rapid diagnosis of MDR-TB. With the upgraded laboratory capacity, MDR-TB diagnosis can be confirmed within three days compared with 2–3 months in the past.
A nationwide drug resistance survey carried out in 2008 had shown an MDR-TB prevalence of 4.2% among newly diagnosed and 10% among previously treated cases. The Ministry of Health has established a national committee on drug-resistant TB with numbers including specialists from hospitals, the NTP, WHO and NGOs to oversee the national response. A GLC approved project is in place and patient enrolment commenced in July 2009. A total of 64 cases have been enrolled for treatment of MDR-TB by the end of 2009.
While the national prevalence of HIV infection is estimated at 0.6%, the prevalence of HIV among TB patients was reported to be 10.9% based on data from annual HIV sentinel surveillance. TB/HIV collaborative activities are being implemented jointly by the NTP and the national AIDS programmes in 11 townships covering a population of 2.5 million. HIV screening for TB patients is currently available through 45 VCCT sites in the country. CD4 facilities are available at 12 sites.
A new five-year Strategic Plan 2011–2015 has been finalized with all partners. A comprehensive HRD plan has been drafted and a focal point for HR designated at the central level. The NTP’s plan and budget are aligned with the national health sector development plan. The programme has established a national PPM DOTS sub-group and involved general practitioners through the PSI Sun Quality clinics and private practitioners through the Myanmar Medical Association. As result, close to 20% of all TB notifications are contributed from non-NTP providers. The ISTC has been endorsed by specialists and the professional associations in the country. Data management software has been implemented and central, state and divisional staff trained in data management and its use. A pilot project to provide IPT to PLHIV has been started and 333 PLHIV were provided with IPT by 2009.
The NTP is being supported by increased funding from the government, supplemented significantly by funding from external sources such as GDF, the

Tuberculosis Control in the South-East Asia Region81
Union/Yadana project, WHO, the Japan International Cooperation Agency (JICA) and the Japan Anti-TB Association (JATA). After the Global Fund unilaterally withdrew support to Myanmar, a new three Diseases Fund to fight AIDS, TB and Malaria in Myanmar was established in 206 as a multi-donor trust fund by DFID, EC, AusAID, Norway, the Netherlands and Sweden.
The Global Fund Round 9 grant for TB control was signed in November 2010. About US$ 65 million will be available for TB control in the country during the next five years. The Three Diseases Fund agreed to continue supporting TB control efforts during the whole of 2011 to ensure coverage of essential activities not covered by the Global Fund.
Major achievements The nationwide survey of the prevalence of TB disease was successfully
finalized.
The Global Fund to Fight AIDS, Tuberculosis and Malaria grant for TB control (2011–2015) was signed in November 2010.
The Three Diseases Fund will support TB control efforts during 2011 to ensure coverage of essential activities.
The Tuberculosis National Strategic Plan for 2011–2015 was developed in collaboration with partners and was approved by the Ministry of Health.
Upgrading and implementation of newer diagnostic tools in national reference laboratories in Yangon and Mandalay has been conducted.
The MDR-TB pilot projects in Yangon and Mandalay, implemented by the NTP and MSF-Holland in collaboration with WHO, were launched in mid-2009 and were successfully continued in 2010.
The involvement of private practitioners to fight TB is increasing continuously with support from Population Services International and the Myanmar Medical Association.
TB/HIV collaborative activities continued successfully and the need to scale up activities was acknowledged by all partners working on TB and HIV/AIDS control in the country.
Guidelines on community involvement in TB prevention, care and control were developed with national and international partner organizations.

Tuberculosis Control in the South-East Asia Region82
Major challenges Despite significant resources from the Global Fund to Fight AIDS,
Tuberculosis and Malaria, the funding gap from 2011–2015 is about US$ 10 million to US$ 19 million per year. Moreover, additional funding will be needed to find the unreached TB cases and to improve diagnostic capacities to detect smear-negative TB cases.
Resource mobilization needs to continue not only to ensure sustainability of the progress achieved by the NTP but also to expand TB control activities to newer areas.
The national TB prevalence survey showed that the majority of TB patients had still remained undetected. Significant efforts will be needed to increase activities to reach out to all the unreached.
The MDR-TB pilot project is only treating a small fraction of the MDR-TB cases in the country. Major challenges are expected when efforts to decentralize MDR-TB management to areas other than Yangon and Mandalay are undertaken.
TB/HIV collaborative activities are only implemented in 11 out of the 325 townships in the country. It is estimated that 11% of TB patients are living with HIV/AIDS.
Activities planned for 2011 Global Fund support will commence in 2011. With Global Fund
support, more than 65 officers will be hired to support monitoring and evaluation and supervision of TB control activities.
An international review of the NTP is planned to take place at the end of March 2011 to assess the progress in implementing the Stop TB Strategy and in reaching the TB-related Millennium Development Goals.
The third nationwide drug resistance survey will be conducted along with a survey on the prevalence of HIV among TB patients.
The two new molecular laboratories will start performing clinical MDR-TB diagnosis and as such MDR-TB management can be scaled up.
An MDR-TB scale-up plan will be developed.

Tuberculosis Control in the South-East Asia Region83
Trends in TB case-notifications, 2000-2009Case-notifications by type of patients, 2009
New smear-negative
39%
New smear-positive 31%
New extra-pulmonary 24%
Relapse 3%
Other 3%
Treatment after failure
1%
Treatment after default 0%
Other re-treatment
2%
Trends in notified new smear-positive TB cases by age group among male, 2000-2009
Treatment outcomes of new smear-positive cases, 2008 cohort
Cured 77%
Other 16%Failed
3%
Died6%
Completed7%
Transferred 2%
Defaulted5%
Trends in treatment outcomes of new smear-positive cases, 2000-2008
YearNot evaluated Defaulted FailedDied Success rate
0%
20%
40%
60%
80%
100%
2000 2001 2002 2003 2004 2005 2006 2007 2008
Trea
tmen
t out
com
es (%
)
YearAll cases New smear-positive
0
50
100
150
200
250
300
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Cas
es p
er 1
00 0
00 p
opul
atio
n
Year15-24 years 25-34 years0-14 years 35-44 years
45-54 years 55-64 years 65+ years
50
100
150
200
250
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Cas
es p
er 1
00 0
00 p
opul
atio
n
0
Year15-24 years 25-34 years0-14 years 35-44 years
45-54 years 55-64 years 65+ years
0
20
40
60
80
100
120
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009
Cas
es p
er 1
00 0
00 p
opul
atio
nTrends in notified new smear-positive TB cases
by age group among females, 2000-2009

Tuberculosis Control in the South-East Asia Region84
Estimates and notification rates for 2009, Myanmar
Population* 50 000 000
Incidence of all forms of TB 200 000 (160 000–240 000)
Incidence rate of all forms of TB (per 100 000 population per year) 404 (329–486)
Prevalence of all forms of TB 300 000 (130 000–500 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 595 (262–994)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
59 (36–87)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
267
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
83
Case-detection rate (all forms of TB) 64 (53–78)
Treatment success rate (%) of new smear-positive cases for 2008 cohort
84
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition.

Tuberculosis Control in the South-East Asia Region85
With a population of about 29 million, Nepal has an estimated incidence and prevalence of all forms of TB of 163 and 241 respectively per 100 000 population. The notification rate of all forms of TB and new smear-positive cases were 122 and 53 respectively, showing slight but steady increase compared with previous years. Treatment success rates among new smear-positive cases were 89% for the cohort of patients registered in 2008. A six month treatment regimen has been introduced throughout the country.
Tuberculosis control is identified as a priority programme within the Ministry of Health and Population.
Since 2001 there has been a slight shift to the older age group, indicating a possible decline in TB burden in Nepal in recent years. The national ARTI survey completed in 2007 was also indicative of a declining trend. However, according to evidences available TB incidence is currently considered “frozen” at 163 per 100 000 population since 1990. Nepal is considering the conduct of a prevalence survey to better assess the burden of TB and trends in the country.
Culture and DST facilities are being provided through a unique public private partnership with an NGO-run laboratory – GENETUP, which is actively supported by the SNRL at Gauting, Germany. Four drug resistance surveys have been carried out since 1996. MDR-TB rates of 2.9% (1.9%–4.3%) among new cases and 11.7% (7.6%–17.6%) among re-treatment cases were reported at the
Nepal

Tuberculosis Control in the South-East Asia Region86
end of the latest survey in 2007. Nepal was one of the first countries globally to introduce ambulatory MDR-TB case management in 2005, diagnosing and treating Category-II failures and other culture-demonstrated MDR-TB cases under a GLC-approved project. The management of MDR-TB on an ambulatory basis has been expanded to all five regions in the country. Currently there are 10 treatment and 34 sub-treatment centres offering MDR-TB treatment services through primary health care services and health facilities managed by other sectors. Further improvement of MDR-TB management is planned through the establishment of hostels for drug-resistant TB cases, introduction of shortened treatment regimen for MDR-TB, and introduction of an electronic database for programme and cohort analysis for MDR-TB cases on treatment.
Sentinel surveys of HIV among TB patients conducted in 2006–2007 showed an HIV prevalence of 2.4%. The country has established a National Working Group on TB/HIV and a National TB/HIV Coordination Committee. The National Strategy for TB/HIV has been officially endorsed by the Ministry of Health and Population. Joint planning, evaluation and logistics management, information sharing, advocacy and operational research have been planned by the two programmes.
A National Infection Control Plan and guidelines on the same have been developed. An assessment of needs to introduce infection control measures at selected facilities has been undertaken.
The NTP’s plan and budget are aligned with the National Health Sector Development Plan. The programme has successfully involved private practitioners in Kathmandu and Lalitpur, several NGOs, public hospitals, all 13 medical college hospitals (both in the public and private sectors) and two major prisons in the country. The Military Hospital is also collaborating with the NTP in providing TB services.
Data management is presently paper-based; the programme is now introducing Windows-based EPI centre software. The Practical Approach to Lung Health (PAL) was introduced in two districts in 2007 and the NTP has expanded PAL to a total of four districts in the country.
The NTP is heavily dependent on donor funding. The programme also continues to receive support through Rounds 4 and 7 of the Global Fund has and successfully applied for National Standards Association (NSA) grant.

Tuberculosis Control in the South-East Asia Region87
Major achievements Full implementation of all six components of the Stop TB Strategy.
Successful implementation and nationwide coverage of MDR/XDR-TB management programme.
Full DOTS health institutional coverage in the primary health system including 100% coverage in primary health care centres, health posts and 99% of the sub-health posts in the country.
Successful resource mobilization through the Global Fund (Rounds 4 and 7 and NSA grant) and LHL, Norway.
Nationwide introduction of the six-month treatment regimen.
Establishment of PAL in four districts in the country.
Development of an Infection control policy, strategy, plan and guidelines and resource mobilization for implementation.
Major challenges Programme sustainability at risk due to heavy dependence on external
funding.
Addressing operational issues of accommodation and inadequate socioeconomic support for MDR-TB cases.
Expansion of DOTS in urban areas.
Introducing infection control in TB programme setting.
Activities planned for 2011 Establishment of hostels for drug resistant TB cases.
Expansion of DOTS in urban areas.
Introduction of infection control in TB programme settings.
Expansion of PAL initiative in additional five districts.
Introduction of shortened (18 months) treatment regimen for MDR-TB management.
Expansion of TB/HIV collaborative activities.
Introducing an electronic database for the programme and cohort analysis for MDR-TB cases enrolled for treatment.

Tuberculosis Control in the South-East Asia Region88
Treatment outcomes of new smear-positive cases, 2008 cohort
News smear- negative 28%
New extra-pulmonary20% Relapse 7%
Treatment afterfailure 1%
Treatment afterdefault 1%
New smear-positive 43%
Other 14%
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t out
com
es (%
)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Trends in notified new smear-positive TB cases by age group among males, 2000–2009
Trends in notified new smear-positive TB cases by age group among females, 2000–2009
Completed3%
Other11%
Died 4%
Defaulted 3%
Transferred 3%
Case-notifications by type of patients, 2009 Trends in TB case-notifications, 2000-2009
20002001
20022003
20042005
20062007
20082009
140
120
100
80
60
40
20
0
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
n
Failed 1%
20002001
20022003
20042005
20062007
20082009
350
300
250
200
150
100
50
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
20002001
20022003
20042005
20062007
20082009
90
80
70
60
50
40
30
20
10
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
Cured86%

Tuberculosis Control in the South-East Asia Region89
Estimates and notification rates for 2009, Nepal
Population* 29 330 504
Incidence of all forms of TB 48 000 (39 000–58 000)
Incidence rate of all forms of TB (per 100 000 population per year) 163 (133–197)
Prevalence of all forms of TB 71 000 (29 000–120 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 241 (97–408)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year) 21 (12–34)
Notification rate of all forms of TB (per 100 000 population for the year 2009) 122
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
53
Case-detection rate (all forms of TB) 73 (60–90)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 89
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition

Tuberculosis Control in the South-East Asia Region90
Sri Lanka has a population of about 20 million and is among the low TB prevalence countries in the Region.
The estimated prevalence and incidence rates of all forms of tuberculosis in 2009 were 101 and 66 per 100 000 population respectively. The notification rate of all forms of TB and new smear-positive cases were 49 and 24 respectively, showing a slight but steady increase compared with previous years. Treatment success rates among new smear-positive cases were 84% for the cohort of patients registered in 2008. The overall default rate has dropped to 7% from over 12% six years ago due to intensified default tracing efforts involving the field Public Health Inspectors (PHIs) and other categories of health staff at the field level. Innovative case-finding strategy is being implemented through TB/diabetes collaborative activities the (so called PEN-PAL project).
A national drug resistance survey was completed in 2006, and this confirmed the very low levels of drug resistance of 0.2% among new patients and 18%–21% among re-treatment cases in the country. Culture and DST is performed for all patients who fail Category I regimens, at the time of initiation of treatment for all patients commencing Category II regimens, contacts of MDR-TB cases, all patients commencing re-treatment regimens, HIV-infected TB cases, migrants and prisoners. MDR-TB is low, only eight cases were detected in 2008. MDR-TB is diagnosed at the national reference laboratory which is supported by the Supranational Laboratory at TRC, Chennai, India. Patients are treated initially at the Central Chest Hospital after which they are referred for treatment at chest clinics in their respective districts. Second-line anti-TB
Sri Lanka

Tuberculosis Control in the South-East Asia Region91
drugs for treatment of MDR-TB cases are procured by the government from the open market. Periodic stock-outs have been reported. The success rate among MDR-TB cases is not yet known. National guidelines for the treatment of MDR-TB have been developed. The programme initiated MDR-TB case management under GLC approval with support through the Global Fund in 2010.
HIV co-infection rates among TB patients are currently estimated at less than 0.1%. TB patients have been included under the annual surveillance for HIV since 1993. Only eight cases have been detected from among 13 993 TB patients tested so far. A national policy for the provision of CPT and ART to HIV-positive TB patients is in place.
The NTP’s plan and budget are aligned with the National Health Sector Development Plan. Public-private collaborative projects have been initiated on a limited scale. Forty two public hospitals including teaching hospitals and five military hospitals have been involved by NTP. The ISTC will be used as a tool for establishing effective TB services within other sectors. There is a plan for the initiation of Practical Approach to Lung Health (PAL). A joint monitoring mission was conducted in 2010.
The government provides the major part of funding for the TB programme, with additional resources secured from the Global Fund (Rounds 1 and 6), the World Bank and WHO.
Major achievements Reaching and sustaining the global targets.
Further reduction in default rates.
Re-introduction and scaling up of the TB control activities for internally displaced people and the population in resettled areas of the North and Eastern provinces.
Strengthening TB control in prisons.
Expansion of TB culture facilities to the district level.
Improved quality assurance of all chest clinic smear microscopy centres.
Strengthening of private-public collaborative activities.
Further improvement of TB/HIV collaborative activities.
Establishment of TB/diabetes collaborative activities.

Tuberculosis Control in the South-East Asia Region92
Improvement of data management at the district level.
Operational research on the prison community and general practitioners.
Major challenges Maintaining adequate human resources in the face of the high turnover
of trained staff.
Reaching the unreached population groups (e.g. population groups with limited access to services, urban slums, the prison population, population in tea and rubber estates.
Scaling up TB control services among migrants and the resettled population in the North and Eastern provinces.
Addressing the high disease burden and high defaulter rate in Colombo city.
Overcoming the stigma attached to TB.
Activities planned for 2011 Screening of tuberculosis among diabetics and diabetes among
tuberculosis patients, and the diagnosis and management of those diseases in respective clinics.
Mobilizing funding assistance to meet the gaps created due to non-availability of Global Fund Round 6 Phase 2 funding.
Improving laboratory capacity and scaling up of culture and DST facilities.
Improving procurement and supply management by the training of key staff.
Further improving the infrastructure at facilities for the delivery of quality TB services.
Strengthening interventions to address HIV-related TB (TB/HIV) and drug-resistant TB.
Developing a five-year advocacy, communication and social mobilization strategy with work plan and lost estimates.

Tuberculosis Control in the South-East Asia Region93
Strengthening public-private mix in TB control by establishing DOTS centres in private hospitals, linking private institutions to the programme data management system, and improving the proficiency of private laboratories.
Updating the patient information software package and introducing online data transmission, networking among District Chest Clinics, the national reference laboratory, the central Drug Stores and the Directorate.
Further integrating TB control with the existing primary health care network.
Initiating PEN-PAL as a pilot project in 2011.
Printing and distribution of the revised/newly designed General Manual of TB Control, Management Guidelines of Extra-pulmonary TB, Programmatic Management of MDR-TB, Management Guidelines of TB/HIV Co-infection, and the Laboratory Manual.
Revision and printing of TB management and laboratory training.
Development of an infection control plan for chest clinics, TB wards and other health-care institutions.
Basic and operational research on TB epidemiology, bacteriology and TB control.
Development of grant applications for GFATM Round 11, TB Reach Wave 2, and second wave of the National Strategy Application.
News smear- negative 20%
New extra-pulmonary24% Relapse 2%
Treatment afterfailure 1%
Otherretreatment 3%
Treatment afterdefault 1%
New smear-positive 49%
Altro 5%
Case-notifications by type of patients, 2009 Trends in TB case-notifications, 2000-2009
20002001
20022003
20042005
20062007
20082009
0
10
20
40
60
50
30
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
n

Tuberculosis Control in the South-East Asia Region94
Trends in notified new smear-positive TB cases by age group among males, 2000–2009
Trends in notified new smear-positive TB cases by age group among females, 2000–2009
20002001
20022003
20042005
20062007
20082009
90
80
70
60
50
40
30
20
10
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
20002001
20022003
20042005
20062007
20082009
25
20
15
10
5
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
Other16%
Treatment outcomes of new smear-positive cases, 2008 cohort
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t suc
cess
rate
(%)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Trends in treatment outcomes of new smear-positive cases, 2000–2008
Completed4%
Died 6%
Defaulted 7%
Transferred 1%
Cured80% Failed
2%
Estimates and notification rates for 2009, Sri Lanka
Population* 20 237 730
Incidence of all forms of TB 13 000 (11 000–16 000)
Incidence rate of all forms of TB (per 100 000 population per year) 66 (54–80)
Prevalence of all forms of TB 20 000 (8 400–34 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 101 (41–170)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year) 9.2 (5.4–14)
Notification rate of all forms of TB (per 100 000 population for the year 2009) 49
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
24
Case-detection rate (all forms of TB) 69 (58–85)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 84
*Source: United Nations, Department of Economic and Social Affairs, Population division (2009), World Population Prospects: The 2008 Revision. CD-rom edition

Tuberculosis Control in the South-East Asia Region95
With a population of approximately 68 million, Thailand ranks 18th in the list of 22 high-burden countries for TB. The estimated prevalence and incidence rates of all forms of tuberculosis in 2009 were 189 and 137 respectively per 100 000 population. The country is currently conducting a national TB prevalence survey whose data will be used to improve current estimates. The country has achieved full DOTS coverage and the notification rate of all forms of TB and new smear-positive cases were 97 and 48 respectively in 2009, showing an increase compared to previous years. Treatment success rates among new smear-positive cases were 83% for the cohort of patients registered in 2008. The low treatment success rate is attributed to high default and mortality rates and incomplete reporting, particularly from the city of Bangkok.
Based on a national drug resistance survey in 2006, MDR-TB rates were reported to be 1.65% among newly diagnosed cases and 34.5% among previously treated cases. Thailand has an extensive and well developed laboratory network. The capacity for first-line DST is being expanded through the establishment of culture facilities at selected regional laboratories. However, due to the decentralized nature of laboratory services and the presence of several private sector laboratories also undertaking TB diagnosis, maintaining quality assurance is one of the major challenges faced by the NTP.
Laboratory strengthening is being supported through the Global Fund Round 6. The national reference laboratory has the capacity for second-line DST, and has recently been formally designated as the second SNRL in the South-East Asia Region. Culture, DST and second-line drugs are available free of
Thailand

Tuberculosis Control in the South-East Asia Region96
cost for Thai citizens through the National Health Security Office. Most patients with drug-resistant tuberculosis are diagnosed and managed by university, regional/provincial and some private hospitals, which procure second-line anti-TB drugs using local resources. The Chest Institute in Bangkok is identifying rather large numbers of MDR-TB cases (40 to 50 yearly) and initiating treatment for the same. Many patients transferred to the provinces outside Bangkok are lost for follow-up and treatment outcomes for them are unknown. MDR-TB cases are currently not reported to the TB programme, although 296 are known to have started treatment by end-2009. National guidelines for MDR-TB, in line with international recommendations, have been developed and adopted by national experts. Culture and DST is recommended for all patients who fail Category I and II regimens, all contacts of MDR-TB cases, all patients commencing re-treatment regimens, HIV-infected TB cases, migrants and prisoners.
Model facilities for MDR-TB case management have been selected based on their performance in DOTS implementation, the presence of a good referral system and measures for infection control. Enrolment of patients is being carried on in three sites supported by the GLC through funds of the Global Fund Round 8.
Substantial progress has been made in implementing TB/HIV collaborative activities throughout the country. A national working group for TB/HIV has been established and the NTP provides guidance for collaborative TB/HIV activities. Provider initiate HIV testing and counselling (PITC) of TB patients has been incorporated into national guidelines and is being increasingly implemented throughout the country. TB/HIV collaborative activities are monitored and supervised mainly by TB programme staff. Routine HIV screening is recommended nationally for all registered TB patients; in 2009 the HIV counselling and testing rate among TB patients was 76%, and 16% of all those tested were found to be HIV-infected.
Care and treatment for HIV-infected persons is highly subsidized and widely available. Cotrimoxazole preventive therapy and antiretroviral treatment was provided to, respectively, 72% and 51% of HIV-positive TB patients, showing an increase over previous years, particularly with regard to the provision of ART. Engagement of all care-providers would be necessary to achieve further significant progress towards the national targets of 60% and 80% respectively for CPT and ART. Improved identification of HIV-infected TB patients, together with effective linkage to care and treatment will be required to significantly reduce TB mortality rates.

Tuberculosis Control in the South-East Asia Region97
IPT had been introduced in some health facilities but has been largely discontinued. Intensified case-finding about newly detected patients with HIV has been initiated. Routine and periodic symptomatic screening for TB among HIV infected patients is undertaken at some hospitals during the initial diagnosis, on follow-up visits and when the decision to initiate antiretroviral therapy is made. In 2008, the proportion of those newly diagnosed HIV patients screened for TB was 93% and the proportion of those diagnosed with TB was 14%.
An HRD plan has been developed and a Focal Point for HR designated at the central level. TB services are fully integrated within the corpus of primary health care. Thailand has made remarkable progress in involving NGOs and the private sector. Recently, the memoranda of understanding were signed with the National Health Security Office, the Ministry of Labour and Médecins Sans Frontières (MSF) for implementation of TB in workplaces, prisons and among migrants. The programme has involved private hospital associations, NGOs (World Vision Foundation, American Refugee Committee, and Thailand Business Coalition on AIDS to Control TB) to provide TB care according to the International Standards for Tuberculosis Care (ISTC).
The country’s TB programme is supported mainly by the government budget through the National Health Security Office. Additional support has been provided by the Global Fund and other bilateral Partners.
Major achievements Funding has been provided from the National Health Security Office
to support TB activities at the provincial and local levels.
TB/HIV collaborative activities are available country wide and have a high utilization rate.
Sustained TB services among marginalized populations, such as migrants and cross-border populations, through NGOs supported through the Global Fund.
Establishing TB services in about 150 prisons.
Greater commitment from the Ministry of Public Health including the designation of a “Mr/Ms TB” at all hospitals and provisional health offices for improved coordination and oversight.
Managing Information for Action (MIFA) course introduced.
Global Fund support secured through Rounds 6 and 8.

Tuberculosis Control in the South-East Asia Region98
Major challenges Improving the quality of DOTS under the decentralized health system
and in big cities.
Further strengthening of TB/HIV integrated activities.
Better managing systematic and regular supervision of programme activities.
Ensuring systematic MDR-TB care, and recording and reporting on these cases.
Effectively involving private hospitals in TB control.
Obtaining adequate commitment for implementing TB control activities in Bangkok.
Addressing human resource constraints at the central and regional levels.
Activities planned for 2011 Capacity-building of village health-care volunteers in decentralized
settings and in big cities to ensure treatment adherence.
Strengthening of regular supervision, monitoring and evaluation of the programme.
Implementing IPT service for HIV-infected persons, after successfully implementing pilot and demonstration projects.
Piloting MDR-TB treatment under the programme; and the procurement of second-line drugs through GLC.
Conducting TB prevalence survey.
Increasing the involvement of private hospitals and ensuring that practices are in line with the national guidelines.
Advocating with the Bangkok Metropolitan Administration for greater commitment to address fragmented service delivery.
Updating the database of health staff and developing a strategic HR plan.

Tuberculosis Control in the South-East Asia Region99
News smear- negative 30%
New extra-pulmonary14% Relapse 3%
Treatment afterfailure 1%
Otherretreatment 1%
Treatment afterdefault 1%
New smear-positive 50%
Other 3%
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t suc
cess
rate
(%)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Trends in treatment outcomes of new smear-positive cases
Trends in notified new smear-positive TB cases by age group among males, 2000–2009
Trends in notified new smear-positive TB cases by age group among females, 2000–2009
Case-notifications by type of patients, 2009 Trends in TB case-notifications, 2000-2009
20002001
20022003
20042005
20062007
20082009
0
20
40
80
120
100
60
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
n
20002001
20022003
20042005
20062007
20082009
200
180
160
140
120
100
80
60
40
20
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
20002001
20022003
20042005
20062007
20082009
90
80
70
60
50
40
30
20
10
0
Year0-14 15-24 25-34 35-44 45-54 55-64 65+
Cas
es p
er 1
00 0
00 p
opul
atio
n
Treatment outcomes of new smear-positive cases, 2008 cohort
Completed7%
Other17%
Died 7%
Defaulted 4%
Transferred 4%
Cured76% Failed
2%

Tuberculosis Control in the South-East Asia Region100
Estimates and notification rates for 2009, Thailand
Population* 68 000 000
Incidence of all forms of TB 93 000 (75 000–110 000)
Incidence rate of all forms of TB (per 100 000 population per year) 137 (111–165)
Prevalence of all forms of TB 130 000 (57 000– 210 000)
Prevalence rate of all forms of TB (per 100 000 population per year) 189 (83–317)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year)
18 (11–27)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
97
Notification rate of new smear-positive cases (per 100 000 population for the year 2009)
48
Case-detection rate (all forms of TB) 69 (57–85)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 83
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition.

Tuberculosis Control in the South-East Asia Region101
With a population of about 1.1 million, Timor-Leste is a low-burden country for TB. However, the estimated prevalence and incidence rates of all forms of tuberculosis were considerable in 209, being 743 and 498 respectively per 100 000 population. The new WHO estimates for TB in the country are significantly higher than the previous ones and are characterized by large confidence intervals, resulting from uncertainty about information to base the estimates on. Current estimates need to be further revised in order to better reflect the current burden of disease in the country and trends in incidence, prevalence and mortality.
Information to improve burden estimates may come from in-depth analysis of TB case-notifications over-time, better application of the “onion model”, research, data from the house-to-house survey of pulmonary TB carried out in 2006–2007 in the sub-district of Bazartette and the district Liquica and additional evidence from recent prevalence studies carried out in Indonesia.
The notification rates of all forms of TB and new smear-positive cases were respectively 420 and 106, showing a perceptible increase compared to previous years. This is indicating of efforts made in TB control over the last few years. Treatment success rate among new smear-positive cases was 85% for the cohort of patients registered in 2008.
The NTP has established services in all 13 districts and 65 subdistricts of the country, with the district TB coordinators (DTCs) working with the district health management teams in all districts and with the 65 community health
Timor-Leste

Tuberculosis Control in the South-East Asia Region102
centres (CHCs) at the sub-district level. Community health centres (CHCs) have been strengthened with funding including support for conducting outreach activities at the village level through the servisu integradu da saúde communitária (SISCa) initiative. Currently, 19 microscopy centres are based in public and NGO facilities.
The Ministry of Health supports all staff costs, infrastructure and basic resources. In 2009 additional resources were mobilized through the Global Fund Round 7.
Four NGO facilities are providing ambulatory care and one is providing in-patient MDR-TB management. There are five other NGOs which support the NTP in identifying TB suspects and referring them to DOTS facilities for diagnosis and treatment. Civil society participation is expected to improve and expand with additional funding from the Global Fund through Round 7.
It is estimated that MDR-TB rates are 2.9% among newly diagnosed patients and 20% among previously treated TB cases. A Green Light Committee approved MDR-TB case management project is in place. A small number of patients with MDR-TB have been identified through culture and DST conducted at the Institute of Medical and Veterinary Sciences (IVMS), Adelaide, Australia. The treatment of such cases is initiated through an NGO, Klibur Domin in the district of Liquica. The GDF has provided necessary second-line anti-TB drugs, with funding supported through UNITAID.
HIV remains relatively uncommon in Timor-Leste. However, the country reported 94 cases of HIV infection, among whom four were confirmed to have active TB. A TB/HIV coordinating body at the national level is in the process of being established. Sentinel surveillance of HIV in TB patients has been initiated. Initial training for staff at VCTs has been completed and a formal mechanism for referral from VCTs to DOTS centres has been initiated.
Major achievements National Stop TB Strategy Plan 2011–2015 developed.
Continued funding under the Global Fund Round 7 Phase II has been secured.
Laboratory manual on smear microscopy translated in tetum, and printed and disseminated.

Tuberculosis Control in the South-East Asia Region103
Two rounds of laboratory technicians’ training conducted by the supranational reference laboratory (SNRL) conducted.
Sample transportation to SNRL for culture and sensitivity testing strengthened.
TB/HIV collaboration established at the national level and key staff trained.
Local and Cuban doctors are working in various health facilities trained on TB control.
Interpersonal communication training conducted for peripheral TB staff.
Joint NTP and WHO supervision of the districts enhanced.
Availability of adequate quantities of first-and second-line anti-TB drugs in the country has been ensured.
Major challenges Improving the low case-detection rates and quality of DOTS
implementation.
Ensuring adequate access to health-care services in many remote and hilly areas.
Overcoming high default rates, particularly in the two major towns of the country.
Increasing community awareness about TB as well as available services.
Improving effective collaboration between the NACP and NTP at the facility level.
Promoting adherence to standard diagnostic and treatment practices by all levels of health staff.
Improving drug logistics and management.
Improving data management.
Building adequate capacity and improving commitment of health staff at the district and subdistrict level.

Tuberculosis Control in the South-East Asia Region104
News smear- negative 65%
New extra-pulmonary9% Relapse 1%
Treatment afterfailure 0%
Treatment afterdefault 0%
New smear-positive 25%
Other 0%
Trends in TB case-notifications, 2000-2009
20002001
20022003
20042005
20062007
20082009
0
50
150
100
350
300
450
400
250
200
YearAll cases New smear-positive
Cas
es p
er 1
00 0
00 p
opul
atio
n
Case-notifications by type of patients, 2009
Activities planned for 2011 Developing training modules based on the NTP guidelines.
Training and refresher training of District TB Coordinators and Regional Supervisors.
Training and retraining of laboratory technicians in smear microscopy and EQA.
Implementing the external quality assurance system for all microscopy centres.
Improving the involvement of community volunteers in TB suspect referral and DOT provision.
Improving routine programme data recording and reporting, and providing feedback to the districts.
Streamlining regular supervision from the national to the district level and from the district level to the subdistrict level.
Improving drug management through logistics and drug management training for DTCs.
Improving programme management capacity at the national and district level.

Tuberculosis Control in the South-East Asia Region105
Notification rate of new smear-positive TB cases by age group and sex, 2009
Year
0-14 15-24 25-34 35-44 45-54 55-64 65+
Num
ber o
f cas
es
0
100
200
300
400
500
600
700
Male Female
Notified new smear-positive TB cases by age group and sex, 2009
Year
Male Female
0-14 15-24 25-34 35-44 45-54 55-64 65+
Num
ber o
f cas
es
0
20
40
60
80
100
120
140
180
0
20
10
40
50
30
70
80
90
100
60
Year
Trea
tmen
t suc
cess
rate
(%)
2000 2001 2002 2003 2004 2005 2006 2007
Not evaluated Defaulted FailedDied Success rate
2008
Treatment outcomes of new smear-positive cases, 2008 cohort
Completed12%
Other15%
Died 5%
Defaulted 7%
Transferred 3%
Cured73%
Trends in treatment outcomes of new smear-positive cases, 2000-2008
Estimates and notification rates for 2009, Timor Leste
Population* 1 133 594
Incidence of all forms of TB 5 600 (4 600–6 800)
Incidence rate of all forms of TB (per 100 000 population per year) 498 (406–600)
Prevalence of all forms of TB 8 400 (3 300–1 400)
Prevalence rate of all forms of TB (per 100 000 population per year) 743 (295–1274)
TB death rate (of all forms of TB, excluding HIV per 100 000 population per year) 66 (37–106)
Notification rate of all forms of TB (per 100 000 population for the year 2009)
420
Notification rate of new smear-positive cases (per 100 000 population for the year 2009) 106
Case-detection rate (all forms of TB) 84 (70–103)
Treatment success rate (%) of new smear-positive cases for 2008 cohort 85
*Source: United Nations, Department of Economic and Social Affairs, Population Division (2009), World Population Prospects: The 2008 Revision. CD-rom edition.



2011
Related Documents