Please cite this article in press as: Rizzo, L.B., et al., The theory of bipolar disorder as an illness of accelerated aging: Implications for clinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.doi.org/10.1016/j.neubiorev.2014.02.004 ARTICLE IN PRESS G Model NBR 1894 1–13 Neuroscience and Biobehavioral Reviews xxx (2014) xxx–xxx Contents lists available at ScienceDirect Neuroscience and Biobehavioral Reviews jou rn al h om epage: www.elsevier.com/locate/neubiorev Review The theory of bipolar disorder as an illness of accelerated aging: Implications for clinical care and research Lucas Bortolotto Rizzo a,b , Leonardo Gazzi Costa a,b , Rodrigo B. Mansur a,b,c , Q1 Walter Swardfager d , Síntia Iole Belangero b,e , Rodrigo Grassi-Oliveira f , Roger S. McIntyre c,d , Moisés E. Bauer f , Elisa Brietzke a,b,∗ a Program for Recognition and Intervention in Individuals in At-Risk Mental States (PRISMA), Department of Psychiatry, Federal University of São Paulo, São Paulo, Brazil b Interdisciplinary Laboratory of Clinical Neuroscience (LINC), Department of Psychiatry, Federal University of São Paulo, São Paulo, Brazil c Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, Ontario, Canada d Sunnybrook Research Institute, University of Toronto, Toronto, Ontario, Canada e Department of Morphology and Genetics, Federal University of São Paulo, São Paulo, Brazil f Institute of Biomedical Research and Faculty of Biosciences, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil a r t i c l e i n f o Article history: Received 29 August 2013 Received in revised form 17 December 2013 Accepted 5 February 2014 Keywords: Bipolar disorder Aging Biomarkers Neuroprogression Telomeres Inflammation Immunosenescence BDNF Oxidative stress Amyloid Cognition Molecular imaging a b s t r a c t Bipolar Disorder (BD) has been conceptualized as both a cyclic and a progressive disorder. Mechanisms involved in neuroprogression in BD remain largely unknown although several non-mutually exclusive models have been proposed as explanatory frameworks. In the present paper, we propose that the pathophysiological Q2 changes observed in BD (e.g. brain structural alterations, cognitive deficits, oxidative stress imbalance, amyloid metabolism, immunological deregulation, immunosenescence, neurotrophic deficiencies and telomere shortening) converge on a model of accelerated aging (AA). Aging can be under- stood as a multidimensional process involving physical, neuropsychological, and social changes, which can be highly variable between individuals. Determinants of successful aging (e.g environmental and genetic factors), may also confer differential vulnerability to components of BD pathophysiology and contribute to the clinical presentation of BD. Herein we discuss how the understanding of aging and senes- cence can contribute to the search for new and promising molecular targets to explain and ameliorate neuroprogression in BD. We also present the strengths and limitations of this concept. © 2014 Published by Elsevier Ltd. Contents 1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2. Neurobiological similarities between neuroprogression in BD and aging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.1. Changes at the structural level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.2. Changes at the functional levels . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.3. Changes at the molecular level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.3.1. Increased oxidative stress . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.3.2. Disturbances in amyloid metabolism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.4. Changes at the cellular level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.4.1. Immunosenescence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.4.2. Reduction in neurotrophins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 2.4.3. Short telomeres . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 ∗ Corresponding author at: R. Pedro de Toledo, 669, 3 ◦ andar Vila Clementino, CEP: 04039-032 São Paulo, Brazil. E-mail address: [email protected] (E. Brietzke). http://dx.doi.org/10.1016/j.neubiorev.2014.02.004 0149-7634/© 2014 Published by Elsevier Ltd. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
N
R
TI
LQ1
WRa
Sb
c
d
e
f
a
ARR1A
KBABNTIIBOACM
Q2
C
h0
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
ARTICLE IN PRESSG ModelBR 1894 1–13
Neuroscience and Biobehavioral Reviews xxx (2014) xxx–xxx
Contents lists available at ScienceDirect
Neuroscience and Biobehavioral Reviews
jou rn al h om epage: www.elsev ier .com/ locate /neubiorev
eview
he theory of bipolar disorder as an illness of accelerated aging:mplications for clinical care and research
ucas Bortolotto Rizzoa,b, Leonardo Gazzi Costaa,b, Rodrigo B. Mansura,b,c,alter Swardfagerd, Síntia Iole Belangerob,e, Rodrigo Grassi-Oliveira f,
oger S. McIntyrec,d, Moisés E. Bauer f, Elisa Brietzkea,b,∗
Program for Recognition and Intervention in Individuals in At-Risk Mental States (PRISMA), Department of Psychiatry, Federal University of São Paulo,ão Paulo, BrazilInterdisciplinary Laboratory of Clinical Neuroscience (LINC), Department of Psychiatry, Federal University of São Paulo, São Paulo, BrazilMood Disorders Psychopharmacology Unit, University Health Network, Toronto, Ontario, CanadaSunnybrook Research Institute, University of Toronto, Toronto, Ontario, CanadaDepartment of Morphology and Genetics, Federal University of São Paulo, São Paulo, BrazilInstitute of Biomedical Research and Faculty of Biosciences, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
r t i c l e i n f o
rticle history:eceived 29 August 2013eceived in revised form7 December 2013ccepted 5 February 2014
eywords:ipolar disordergingiomarkerseuroprogressionelomeres
a b s t r a c t
Bipolar Disorder (BD) has been conceptualized as both a cyclic and a progressive disorder. Mechanismsinvolved in neuroprogression in BD remain largely unknown although several non-mutually exclusivemodels have been proposed as explanatory frameworks. In the present paper, we propose that thepathophysiological changes observed in BD (e.g. brain structural alterations, cognitive deficits, oxidativestress imbalance, amyloid metabolism, immunological deregulation, immunosenescence, neurotrophicdeficiencies and telomere shortening) converge on a model of accelerated aging (AA). Aging can be under-stood as a multidimensional process involving physical, neuropsychological, and social changes, whichcan be highly variable between individuals. Determinants of successful aging (e.g environmental andgenetic factors), may also confer differential vulnerability to components of BD pathophysiology andcontribute to the clinical presentation of BD. Herein we discuss how the understanding of aging and senes-cence can contribute to the search for new and promising molecular targets to explain and ameliorate
nflammationmmunosenescenceDNFxidative stressmyloid
neuroprogression in BD. We also present the strengths and limitations of this concept.© 2014 Published by Elsevier Ltd.
ognitionolecular imaging
ontents
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 002. Neurobiological similarities between neuroprogression in BD and aging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
2.1. Changes at the structural level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 002.2. Changes at the functional levels . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 002.3. Changes at the molecular level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
2.3.1. Increased oxidative stress . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 002.3.2. Disturbances in amyloid metabolism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
2.4. Changes at the cellular level . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
2.4.1. Immunosenescence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2.4.2. Reduction in neurotrophins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2.4.3. Short telomeres . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
∗ Corresponding author at: R. Pedro de Toledo, 669, 3◦ andar Vila Clementino, CEP: 040E-mail address: [email protected] (E. Brietzke).
ttp://dx.doi.org/10.1016/j.neubiorev.2014.02.004149-7634/© 2014 Published by Elsevier Ltd.
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
39-032 São Paulo, Brazil.
ARTICLE IN PRESSG ModelNBR 1894 1–13
2 L.B. Rizzo et al. / Neuroscience and Biobehavioral Reviews xxx (2014) xxx–xxx
3. Implications for research directed to clinical care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 003.1. Pharmacological strategies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
3.1.1. Current pharmacology modulating aging related mechanisms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 003.1.2. Sirtuins as possible new target . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
3.2. Non-pharmacological strategies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 003.2.1. Physical activity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
4. Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00Conflict of interest statement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00Acknowledgements. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
. . . . . .
1
ooretGcnSm(
is2dtdtaavilesepss
uaastoGHoa2
aSdiAota
Normal aging is associated with alterations in brain structures.
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. Introduction
Bipolar Disorder (BD) is a prevalent and often severe mood dis-rder where individuals experience disruptive episodes of maniar hypomania and depression (Anderson et al., 2012). Causes of BDemain largely unknown but probably involve a set of genetic andnvironmental factors, which interact during neurodevelopmento determine vulnerability to the disease (Brietzke et al., 2012a).enetic studies have implicated many chromosomal regions andandidate genes, but results have been inconsistent and oftenot replicable (Sullivan et al., 2012). Genome-wide Associantiontudies (GWAS) studies indicate that genetic susceptibility is deter-ined by a high number of genes, each with a small effect size
Sullivan et al., 2012).Although BD has been understood classically as a cyclic disease,
n the last 10 years evidence has accumulated supporting progres-ive features of BD (Berk et al., 2010; Fries et al., 2012; Mansur et al.,013), reconceptualizing BD as both a cyclic and progressive disor-er. The starting point for this hypothesis was the clinical evidencehat individuals in early and late stages of BD present substantialifferences in the severity of clinical presentation and response toreatment (Berk et al., 2011). There are robust data suggesting that
greater number of episodes, especially those of manic polarity,re associated with a decrease in the length of the euthymic inter-al between episodes, worsening of neurocognitive performance,ncreasing risk of suicide, and poorer response to both pharmaco-ogical and psychosocial treatments (Berk et al., 2010; Magalhaest al., 2012). Nonetheless, evidence has been mixed and progres-ive models of mental illness are not universally accepted (Zipurskyt al., 2012). At present, operationalization of the concept of neuro-rogression in clinical practice manifests mainly in the “staging” ofevere mental disorders, including BD (for a detailed review, pleaseee Kapczinski et al., 2009).
Mechanisms involved in neuroprogression remain largelynknown and only few explanatory models exist that could justify
neuroprogressive disease course. Among these, one of the mostccepted is the concept of Allostatic Load (AL). AL implicates chronictress in overactivating homeostatic mechanisms that are collec-ively beyond the capability of the organism, leading to progressionf clinical and neurobiological parameters (Brietzke et al., 2011;oldstein et al., 2009b; Grande et al., 2012; Kapczinski et al., 2008).owever, it has been difficult to quantify the impact of stress biol-gy on neuroprogression, in part due to mechanisms of resistancend resilience that can modulate the impact of stress (Brietzke et al.,012b).
Another nascent theoretical framework is the concept of BDs a disorder of accelerated aging (AA) (Simon et al., 2006;odhi et al., 2012). Aging in humans refers to a persistentecline in the age-specific fitness components of an organ-
sm due to internal physiological degeneration (Rose, 1991).ging can also be understood as a multidimensional process
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
f physical, neuropsychological, and social changes. With respecto neuropsychological changes, the effect of aging is non-uniformcross domains. For instance, psychomotor processing speed and
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 00
verbal memory performance decline with age, while knowledgeand wisdom can continue to expand. The rates of change in thesedomains differ between individuals and they can be modified bymany intervening genetic and environmental factors. A comple-mentary concept is the idea of senescence. The phenomenon ofcellular senescence was first described by Leonard Hayflick in 1961,referring to the limited capacity of isolated cells to proliferate inculture (the Hayflick Limit) (Hayflick and Moorhead, 1961), but theconcept can also be applied to whole organisms. For example, aftera period of near perfect renewal (in humans, between 20 and 35years of age), organismal senescence is characterized by the declin-ing ability to respond to stress, increasing homeostatic imbalanceand risk of disease.
Preliminary data suggest that individuals with BD present earlysenescent features consistent with AA. One of the most clinicallyconspicuous corollaries is the high prevalence and earlier age ononset of age related medical conditions e.g. cardiovascular con-ditions, hypertension, metabolic imbalances, autoimmunity andcancer (Crump et al., 2013; Czepielewski et al., 2013; Fagioliniet al., 2008; Goldstein et al., 2009a; McIntyre et al., 2005, 2006;Osby et al., 2001; Padmos et al., 2004; Rege and Hodgkinson, 2013;Soreca et al., 2008). In addition, the association between mooddisorders and dementia has been well recognized. Most studiesinclude individuals with Major Depressive Disorder (MDD), but arecent meta-analysis suggested that the association between BDand dementia might be stronger than that of MDD (da Silva et al.,2013). Although the degree of neurobiological overlap betweenthe two conditions remains a matter of debate, there is evidencethat inflammation, neurotrophic and amyloid cascades are alteredin both conditions (Aprahamian et al., 2013; Modabbernia et al.,2013).
Here we discuss how aging and senescence may contributeto the search for new and promising molecular targets to bet-ter understand neuroprogressive features of BD. Although somefindings are preliminary, we postulate they can be integrated ina new theoretical framework to better explain some elements ofBD pathophysiology.
2. Neurobiological similarities between neuroprogressionin BD and aging
Although there are few studies exploring aging in BD, there is asurprisingly high overlap between neurobiological mechanisms inthe two conditions, including progressive changes at the molecularand cellular levels, and in the structure and function of the centralnervous system (CNS).
2.1. Changes at the structural level
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Post mortem and structural neuroimaging studies indicate thatthe human brain shrinks with age, with selective and differentialchanges that are not uniform or random. CNS volume atrophy is
148
149
150
ING ModelN
iobeha
ialtcti(n0pfdi2J2
dettt2rwFit2dneo2
2
blspshifbahv
ofMibstfovfmfc
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248
249
250
251
252
253
254
255
256
257
258
259
260
261
262
263
264
265
266
267
268
269
270
271
272
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
ndicated by reduced brain weight and volume, ventriculomegalynd sulcal expansion. Microscopic studies documented myelin pal-or, loss of neuronal bodies in the neocortex, the hippocampus andhe cerebellum, loss of myelinated fibers across the subcorticalerebrum, shrinkage and dysmorphology of neurons, accumula-ion of lipofuscin, rarefication of cerebral vasculature, reductionn synaptic density, deafferentation and loss of dendritic spinesRaz and Rodrigue, 2006). The main findings of magnetic reso-ance imaging studies include brain atrophy (total brain volume:.4–0.5% brain tissue loss per year); hippocampal volume loss (1.6%er year in normal individuals); white matter lesions as puncti-orm or early confluent lesions in periventricular or subcorticalistribution and cerebral microbleeds (prevalence more than 20%
n persons older than 60 years) (Allen et al., 2005; DeCarli et al.,005; Enzinger et al., 2005; Fotenos et al., 2005; Ikram et al., 2008;ernigan et al., 2001; van der Lijn et al., 2008; Vernooij and Smits,012).
BD is also associated with alterations in brain structures evi-enced by previous imaging studies that reported findings ofnlargement of the third and lateral ventricles; a reduction inhe gray matter volumes of the orbital and medial prefrontal cor-ex, ventral striatum and mesotemporal cortex and an increase inhe size of the amygdala (Hallahan et al., 2011; Konarski et al.,008; Lisy et al., 2011; Martinez-Aran et al., 2002). These neu-oanatomical changes tend to be more pronounced in patientsith repeated episodes (Lisy et al., 2011; Strakowski et al., 2002).
urthermore, one of the most consistently reported abnormalitiesn BD is an increased number and/or severity of white mat-er hyperintensities (WMH) (Mahon et al., 2010; Mahon et al.,009). The main findings of neuropathogical studies suggesteficits in neuroplasticity, particularly in cell resilience and con-ectivity (Connor et al., 2009; Harrison, 2002; Martinez-Arant al., 2002; Rajkowska, 2002) as well as data showing fewerligodendrocytes in prefrontal white matter (Vostrikov et al.,007).
.2. Changes at the functional levels
The tertiary association cortices, the neostriatum, and the cere-ellum are profoundly affected by aging throughout the adult
ifespan. Regional volumetric decline has been linked with domain-pecific declines in cognitive performance. For example, poorererformance on executive function tasks has been associated withmaller volume of the prefrontal cortex and increased white matteryperintensity burden. Skill acquisition performance is enhanced
n those individuals who show larger volumes of the striatum, pre-rontal cortex and cerebellum. Spatial memory performance haseen linked to hippocampal volume and the concentration of N-cetyl aspartate therein. In addition, entorhinal cortex shrinkageas been found to predict memory decline, even in healthy indi-iduals (Raz and Rodrigue, 2006).
BD is associated with cognitive impairment during acute phasesf illness and euthymia, with greater abnormalities reported asunction of more frequent episodes (Martinez-Aran et al., 2005;
artinez-Aran et al., 2004; Robinson et al., 2006). The most severempairments are seen in verbal working memory, response inhi-ition, sustained attention, psychomotor speed, abstraction andet-shifting (Martinez-Aran et al., 2007). These deficits in execu-ive function and verbal memory have been associated with poorerunctional outcomes (Torrent et al., 2006; Ustun, 1999) and burdenf illness associated with BD (Rosa et al., 2008). It is similar of indi-iduals with mild cognitive impairment and early dementia who
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
requently report impairments in functioning such as poor perfor-ance in household management activities and in more advanced
unctions (Albert et al., 1999). Furthermore, impairments psychoso-ial functioning can take a progressive course (Rosa et al., 2012;
PRESSvioral Reviews xxx (2014) xxx–xxx 3
Rosa et al., 2011) and can be present during euthymia (Swannet al., 1999). Some authors have proposed that individuals with BDpresent an acceleration in age-related cognitive decline, when com-pared with healthy controls (Gualtieri and Johnson, 2008), althoughthere are some contrary data (Samame et al., 2013). Individualswith MDD, especially those who present the disorder in late life,carry a well-documented risk of dementia (Aprahamian et al., 2013;Osorio et al., 2013). The increased risk of dementia associated withmood disorders in epidemiological studies may be due to commonneuropathological changes shared by these disorders. The investi-gation of aging and senescence processes might lead to an improvedunderstanding of these associations (Gualtieri and Johnson, 2008).
2.3. Changes at the molecular level
2.3.1. Increased oxidative stressIncreased generation of reactive oxygen species (ROS) or dys-
regulation of anti-oxidant mechanisms can lead to the damage ofcellular components such as DNA, proteins and lipids (Andreazzaet al., 2009). Possible sources of ROS include changes in energygeneration and ATP production, for instance free radicals can begenerated during mitochondrial electron transport (Steckert et al.,2010). Other cell process can also generate ROS, including exces-sive dopaminergic transmission (due reductive potential of thisneurotransmitter and its metabolites) and increases in levels of glu-tamate leading to increases in levels of intracellular calcium andcytotoxicity (Berk et al., 2011). Under physiological conditions, theharmful potential of ROS is kept under control by enzymatic andnon-enzymatic antioxidant defense systems (Steckert et al., 2010).
As oxidative stress has been considered a major source of molec-ular and cellular damage, and aging can be understood as a lifelongprocess of cell damage, these two phenomena are presumablylinked. Key pathophysiological elements of several diseases relatedto aging cause end-organ damage through oxidative mechanisms,including chronic obstructive pulmonary disease (Ito et al., 2012),cancer (Ito et al., 2012), type II diabetes (Stadler, 2012), cardio-vascular disease (Penna et al., 2013), Parkinson’s disease (Torraoet al., 2012), and Alzheimer’s disease (Torrao et al., 2012). Thesedata initially lead to “the free radical theory of aging” supportedextensively by numerous in vivo and in vitro studies (Harman,2009). Cumulative oxidative stress causes DNA damage, reducesmechanisms of DNA repair, stimulates inflammatory activation andmodulates redox-sensitive transcriptional factors, such as activatorprotein (AP)-1 and nuclear factor-kappa B (NF-�B), which alter thetranscription of numerous genes, both adaptive and maladaptive,consequently disrupting homeostasis.
Increased oxidative stress and its cellular and molecular con-sequences have been found extensively in BD. In animal modelsof mania, increases in oxidative mediators such as thiobarbituricacid reactive substances (TBARS) are well documented (Ghedimet al., 2012). Studies that focused on individuals in manic episodesobserved increases in nitric oxide (NO) and TBARS, as well asdecreases in antioxidant enzymes, including superoxide dismutase(SOD) and catalase (CAT) (Gergerlioglu et al., 2007; Machado-Vieiraet al., 2007; Savas et al., 2002). Acute treatment with lithiumappears to have an antioxidant effect, as it was shown to affectTBARS, SOD and CAT levels (Machado-Vieira et al., 2007). The onlystudy that evaluated BD individuals in depressive episodes reportedhigher levels of NO and lower levels of SOD, which were alsoresponsive to pharmacological treatment (Selek et al., 2008).
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
While imbalances in oxidative stress can be detected in earlystages of disease, they tend to be more pronounced with increasingduration of illness or number of episodes, suggesting that oxidativestress might be a mechanism of neuroprogression and a source of
273
274
275
276
ING ModelN
4 iobeha
pe
2
smadbrapddptsomnAc
paaettJec2fntde
ediSBse(l(t2dVrborJTtoiibt
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
296
297
298
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
323
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
348
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
371
372
373
374
375
376
377
378
379
380
381
382
383
384
385
386
387
388
389
390
391
392
393
394
395
396
397
398
399
400
401
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
lasma biomarkers to monitor the course of the disease (Andreazzat al., 2009; Berk et al., 2011; Magalhaes et al., 2012).
.3.2. Disturbances in amyloid metabolismAmyloid � (A�) peptides of 40 or 42 amino acids are formed after
equential cleavage of the amyloid precursor protein (APP), a transembrane glycoprotein of undetermined function, by successive
ction of the � and � secretases (Zhang et al., 2011). Alzheimer’sisease (AD) is characterized, from a neuropathological standpoint,y the extracellular deposition of the A� and by the intraneu-onal generation of neurofibrillary tangles, neuropil threads, andbnormal material in dystrophic nerve cell processes of neuriticlaques. These changes are also found in a large number of non-emented elderly people post-mortem. One difference betweenemented AD patients and nondemented elderly with AD-relatedathology is reflected by the distribution pattern of neurofibrillaryangles and A� deposits. The AD patients who manifest clinicalymptoms of dementia present a pattern of widespread lesionsccurring in many areas of the brain (all areas affected in nonde-ented patients plus in the brain stem and cerebellum) whereas
ondemented elderly people showed neurofibrillary tangles and� deposits restricted to distinct predilection sites (neocortex, allo-ortex, basal ganglia, and diencephalic nuclei) (Thal et al., 2004).
Alterations of A� peptides concentration in plasma from ADatients (i.e. reduced A� 42 and an increased A� 40/A� 42 ratio)re common findings in recent studies, and this alteration waslso found in patients suffering from MDD (Kita et al., 2009; Qiut al., 2007; Sun et al., 2007). The risk for dementia and for cogni-ive decline seems to be greater in patients with mood disordershan in the general population (Geerlings et al., 2008; Gualtieri andohnson, 2008). In BD, the number of affective episodes (Geerlingst al., 2008; Kessing and Andersen, 2004) and the presence of psy-hotic symptoms (Kessing and Andersen, 2004; Robinson et al.,006; Torres et al., 2007) have been implicated as additional riskactor. Another study on bipolar depressed patients, found a sig-ificant negative correlation between A� 42 plasma levels andhe duration of the illness, whereas a positive correlation wasetected between the A� 40/A� 42 ratio and the number of affectivepisodes (Piccinni et al., 2012).
Direct cytotoxic effects of A�, negative effects on monoamin-rgic transmission, and functional antagonism between brain-erived neurotrophic factor (BDNF) and A�, suggest the potential
nvolvement of A� in the pathophysiology of BD and cellular aging.tudies suggest that A� may exhibit functional interference withDNF actions, because BDNF stimulates glutamatergic transmis-ion and long-term potentiation (LTP) (Korte et al., 1995; Levinet al., 1998; Lue et al., 1999) whereas A� inhibits these phenomenaSnyder et al., 2005). Furthermore, A� can block the phosphory-ation of the transcription factor cAMP response element-bindingCREB) (Tong et al., 2001) and its nuclear translocation, inhibitinghe synthesis of BDNF (Arancio and Chao, 2007; Arvanitis et al.,007). The hypothesized increase in glutamatergic transmissionuring mood episodes (Kugaya and Sanacora, 2005; Machado-ieira et al., 2009; Yildiz-Yesiloglu and Ankerst, 2006) may play aole in the A�-mediated neurotoxicity, explaining the relationshipetween cognitive decline and the severity of the clinical coursef mood disorders, and the greater risk of developing dementiaeported in mood disorders (Geerlings et al., 2008; Gualtieri andohnson, 2008; Kessing and Andersen, 2004; Robinson et al., 2006;orres et al., 2007). It has been suggested that some presenta-ions may represent a prodromal manifestation of AD, or a subtypef amyloid-associate mood disorder characterized by cognitive
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
mpairment and risk of dementia (Sun et al., 2007). More generally,ndividuals who present with considerable Alzheimer’s pathologyut who do not develop clinical dementia may be less suscep-ible to dementia due to greater “cognitive reserve” (i.e. greater
PRESSvioral Reviews xxx (2014) xxx–xxx
resilience to neuropathological processes by virtue of greater neu-ral substrate, higher premorbid IQ, extensive education, exercise,other lifestyle factors, etc.), which may be eroded by BD pathologyresulting in greater susceptibility to dementia in the presence ofthe same neuropathological burden.
2.4. Changes at the cellular level
2.4.1. ImmunosenescenceImmunosenescence refers to the decline of immunological func-
tion that occurs with aging. During aging, sustained low-gradeinflammatory activity gradually evolves and this is sometimesreferred to as “inflammaging” (Franceschi et al., 2007). In this con-text, healthy aging and longevity are likely result not only froma lower propensity to mount inflammatory responses but alsomaintenance of efficient anti-inflammatory networks (Franceschiet al., 2007). During aging, regulatory processes may fail to coun-teract the inflammatory responses consequent to exposure todamaging agents or to the lifelong acquired antigenic burden.Intriguing data from a large multi-ethnic cohort study suggeststhat cumulative pathogen exposure, particularly viral pathogenssuch as cytomegalovirus (CMV) and other herpes virus, can lead toincreased risks of vascular aging, and cognitive decline in later-life(Elkind et al.; Katan et al.; Swardfager and Black). Further investi-gation is needed, but it is possible that these infections, overwhelmthe diminishing capacity for immunoregulation/immunotoleracethat occurs with age, resulting in increased tissue damage. In ani-mal models, the inflammatory response to experimental infectionresolves more slowly in aged mice than in adult mice, which isassociated with prolonged depressive-like behavior in aged mice(Kelley et al.). According to this perspective, one key to successfulphysical, psychological and cognitive aging is decreased inflamma-tory activity without compromising an effective acute response tonew pathogens (Franceschi et al., 2007).
The paradigm of inflammaging has been largely accepted toexplain why age is an important risk factor for diseases such astype-2 diabetes, cardiovascular diseases and some types of can-cer (Macaulay et al., 2013). In addition, inflammaging has beenpostulated as an explanation for some neurobiological characteris-tics of Alzheimer’s disease. Patients with Alzheimer’s disease showincreased inflammatory activity compared to controls (Swardfageret al., 2010b) as do patients in the clinical mild cognitive impair-ment prodromal phase of the illness (Fuchs et al., 2013). There isevidence that IFN-� and other pro-inflammatory cytokines inter-act with processing and production of A� peptide, suggesting thatthe increased inflammatory activity that accompanies aging couldprecipitate, accelerate or exacerbate AD pathology (Giunta, 2008).Some treatments that counteract inflammaging have been pro-posed to prevent or treat AD, including celecoxib, naproxen, trifusaland indomethacin although limitations in trial design or uncer-tainty in these results limit their readiness for clinical application(de Jong et al., 2008; Gomez-Isla et al., 2008).
There is a consistent body of evidence suggesting that BD isassociated with a persistent and low intensity pro-inflammatorystates, which are more intense during mood episodes, especiallymanic episodes, and less intense in depressive episodes (Brietzkeet al., 2009b; Modabbernia et al., 2013). Even euthymia has beenassociated with detectable peripheral pro-inflammatory activity(Brietzke et al., 2009a). In the context of aging, blood cytokineconcentrations have been correlated with immune-stimulatedcatabolism of tryptophan and tyrosine, necessary precursors in thesynthesis of serotonin and dopamine, and this has been associ-
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
ated with affective and neurovegetative symptoms, respectively(Capuron et al., 2011). This mechanism may apply to BD patientsearlier in life. For instance, the enzymes and final products of thekynurenine pathway, which catabolizes tryptophan, are increased
402
403
404
405
ING ModelN
iobeha
iaaS
iC2eccsstpqrw2iiltci2incir2
2
ctora12Pnd
mthiaBeBtBa2
alaip6e
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444
445
446
447
448
449
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464
465
466
467
468
469
470
471
472
473
474
475
476
477
478
479
480
481
482
483
484
485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504
505
506
507
508
509
510
511
512
513
514
515
516
517
518
519
520
521
522
523
524
525
526
527
528
529
530
531
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
n the cingulate cortex in BD (Miller et al., 2006, 2008). This has beenssociated with cognitive symptoms in mood disorders patientsnd proposed as a modifiable target for therapy (Wonodi andchwarcz, 2010).
BD patients exhibit other immunological alterations commonn elderly people; for instance higher proportions of circulatingD8+CD28− cells (do Prado et al., 2013; Wieck and Grassi-Oliveira,013), and lower proportions of regulatory T cells (do Pradot al., 2013; Wieck and Grassi-Oliveira, 2013) and increasedytomegalovirus (CMV) infection (Rizzo et al., 2013). CD8+CD28−
ells have lost the expression of the CD28 protein, which is neces-ary for their complete stimulation and clonal expansion. They havehort telomeres, impaired cytotoxic function, and they are resistanto apoptosis (Derhovanessian et al., 2009; Weng et al., 2009). Theroportion of CD8+CD28− cells increases with aging and a high fre-uency of CD28− cells in the elderly correlates with a less effectiveesponse to influenza virus vaccination (Goronzy et al., 2001) andith a higher risk of mortality (Olsson et al., 2000; Wikby et al.,
002). The main cause for the expansion of these senescent cellss related to infectious burden, particularly CMV infection. Afternfection with CMV, the body is not able to promote virus clearance,eading to chronic albeit asymptomatic infection. The long course ofhe infection promotes chronic immunological stimulation of spe-ific cells for CMV epitopes, and consequently restriction of themmunological repertoire (Almanzar et al., 2005; Ouyang et al.,003). Intriguingly, this effect is less pronounced other chronic
nfections (Pawelec and Derhovanessian, 2011). The motive is untilow not completely understood, but it is possible that CMV has aloser relation with the immunological system compared to othernfections, since dendritic and endothelial cells function as viraleservoirs (Benedict et al., 2008; Bentz et al., 2006; Tabata et al.,008).
.4.2. Reduction in neurotrophinsImpaired capacity for neuroplasticity has been proposed as a
ore-underlying feature of mood disorders, which may be relatedo both affective and cognitive symptoms as they affect the integrityf nodal brain structures and connectivity between them. Neu-oplasticity can be impaired by pro-inflammatory cytokines (Dasnd Basu, 2007; Goshen et al., 2007), normal aging (Kuhn et al.,996) and activation of the stress-response systems (Joca et al.,007; Karten et al., 2005). On the other hand, physical activity (vanraag et al., 1999) and mood stabilizers such as lithium can promoteeurogenesis (Chen et al.). Many treatment benefits are thought toepend on the release of neurotrophic factors.
Neurotrophins, notably BDNF, have been considered one of theost important mediators of synaptic plasticity and apoptosis con-
rol in mood disorders. Individuals with BD, when compared withealthy controls, have lower peripheral levels of BDNF in mania and
n depressive episodes, as described by a systematic review, with meta-regression analysis (Fernandes et al., 2011). In that study,DNF levels in euthymia were unaltered, although they were influ-nced by age and length of illness. A separate study reported thatDNF levels were decreased in euthymic individuals, but only inhe latter stages of illness (Kauer-Sant’Anna et al., 2009). Therefore,DNF has been considered both a marker of clinical symptoms and
mechanism underlying neuroprogression (Berk, 2009; Berk et al.,010).
Interestingly, reduced BDNF levels have also been found inging (Perovic et al., 2012). In non-demented elderly individuals,ower BDNF plasma levels have been correlated with white-mattertrophy (Driscoll et al., 2012). The age-related decline in BDNF
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
s probably due to epigenetic changes. In one rodent study, hip-ocampal BDNF mRNA was lower in 12-month-old compared with
months old animals. In addition, there was a decrease in thexpression of TrkB, the BDNF receptor mediating neuroprotection
PRESSvioral Reviews xxx (2014) xxx–xxx 5
and structural plasticity, which was accompanied by lower levelsof the two main downstream effector kinases, pAkt and proteinkinase C (Perovic et al., 2012). Recently, a post-mortem studyshowed an age-related decrease in BDNF transcripts in amygdalaof both healthy and MDD individuals as well as in BDNF-dependentgene expression. Interestingly, most genes that are age-dependentin control subjects display greater age effects in MDD subjects(Douillard-Guilloux et al., 2013).
A second neurotrophin likely to be of importance to mood dis-orders, and particularly in senescence processes, is insulin-likegrowth factor 1 (IGF-1). In mouse behavioral studies, experimen-tal IGF-1 deficiency induces depressive-like symptoms (Mitschelenet al.), and in an inflammatory depression model, IGF-1 reduceddepression-like behavior (Park et al.). Polymorphisms in the IGF-1gene have been associated with BD, suggesting that genomic vari-ants may increase susceptibility (Pereira et al.). Insulin-like growthfactor-1 (IGF-1) can increase neural stem cell proliferation in thedentate gyrus of the hippocampus and increase CA1 pyramidalneuron dendritic spine density (Glasper et al.). IGF-1 activates anti-apoptotic signaling, protecting neurons against oxidative stress(Floratou et al.; Wang et al.). Moreover, a recent study found that BDpatients who respond to lithium express greater amounts of IGF-1(Squassina et al.) compared to non-responders. The IGF-1 systemis a well-known regulator of aging; however, the relationship maybe complex and the overall effect on lifespan may depend on theperiod of reduced IGF-1 signaling (Kenyon). In animals, the IGF-1receptor determines lifespan based on a neuroendocrine mecha-nism during normal development that increases metabolic functionand reduces longevity (Holzenberger et al.). In humans, mutationsthat decrease the function of the IGF-1 receptor or of signalingmolecules downstream of the IGF-1 receptor are associated withlongevity (Kenyon). However, plasma IGF-1 concentrations declinewith age and they are negatively associated with cardiometabolicrisk factors such as BMI, insulin resistance and blood pressure, sug-gesting that concentrations of IGF-1 may be a marker of metabolicdisease rendering patients with BD more susceptible to neuralinsult and impaired resilience (Sesti et al.). In later-life and in mooddisorders, increases in oxidative stress, apoptosis, inflammation,and declining endothelial function may be ameliorated by IGF-1(Higashi et al.). Further investigation into the relationships betweenBD, aging and the IGF-1 system are warranted.
2.4.3. Short telomeresIn humans and other animals, cellular senescence has been
attributed mainly to the shortening of telomeres. Telomeres arespecialized structures present at the end of chromosomes com-posed by DNA tandem repeats of (TTAGGG/CCCTAA)n ranging5–15 kbp (Aubert and Lansdorp, 2008) and proteins such as TRFs,POT, TIN2, which stabilize the region (Amiard et al., 2007; Teixeiraet al., 2004). Telomeres are believed to have evolved to “cap” chro-mosomal termini and prevent end-to-end recombination and thusserve a critical role in the maintenance of chromosomal integrity(Blackburn, 2001; Blackburn et al., 2000; Simon et al., 2006). Sincetelomerase levels are insufficient in normal human cells, in each celldivision telomeres get shorter due to the “end replication problem”.When telomeres become too short, the cell ceases to proliferate andenters a state known as “replicative senescence”. Thus, meteredloss of telomeres can serve as a cellular “mitotic clock” that ulti-mately limits the number of cell divisions and cellular life span.For instance, telomere length declines in stem cells, affecting theirfunctionality and capability to generate new cells (Vaziri et al.,1994). Interestingly, shorter telomeres have been associated with
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
higher risk of mortality due to cardiovascular and infection-relateddiseases (Cawthon et al., 2003). Although the replicative problemplay a role in telomere shortening, other mechanisms are involvedlike oxidative stress (von Zglinicki, 2000).
532
533
534
535
ARTICLE IN PRESSG ModelNBR 1894 1–13
6 L.B. Rizzo et al. / Neuroscience and Biobehavioral Reviews xxx (2014) xxx–xxx
Fig. 1. Biological findings linking bipolar disorder and aging. White matter hyperintensities (WMH), T regulatory cells (Treg), cytomegalovirus (CMV), nitric Oxide (NO),t ase (C
fihsMnlotavtpe
gcspg(opItwl(
gm
536
537
538
539
540
541
542
543
544
545
546
547
548
549
550
551
552
553
554
555
556
557
558
559
560
561
562
563
564
565
566
567
568
569
570
571
572
573
574
575
576
577
578
579
580
581
582
583
584
585
586
587
588
589
590
591
592
593
594
595
hiobarbituric acid reactive substances, (TBARS), superoxide dismutase (SOD), catal
A preliminary study conducted by Simon and collaboratorsound reduction of telomere length from peripheral leukocytes inndividuals with mood disorders (MDD and BD) compared withealthy controls (Simon et al., 2006). Hartman et al. also foundhorter mean telomere length in leukocytes of individuals withDD compared to healthy controls, although the duration of ill-
ess and depression severity were not associated with telomereength (Hartmann et al., 2010). On the other hand, the numberf previous depressive episodes was an important determinant ofelomere shortening in another study (Wolkowitz et al., 2011). Inddition, pre-treatment telomerase activity was significantly ele-ated in depressed individuals compared with healthy controls andelomerase activity was correlated with depression severity andredicticting response to antidepressant treatment (Wolkowitzt al., 2012).
Telomere shortening is less investigated in BD than in MDD. In aroup of individuals with BD type 2, short telomeres were moreommon among the affected group that among healthy controlubjects (15.04% vs. 13.48%; p = 0.04). Mean telomere length in theatient group was 552 base pairs (bp) shorter than in the controlroup; however, the difference did not reach statistical significanceElvsashagen et al., 2011). The effect of lithium in telomere lengthf individuals with BD was also investigated. Lithium-treated BDatients had 35% longer telomeres compared with healthy controls.
n this study, telomere length correlated positively with lithiumreatment duration of >30 months and was negatively associatedith increasing number of depressive episodes. Thus, response to
ithium in BD patients may also be associated with longer telomeres
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
Martinsson et al., 2013).Possible causes for shortening of telomeres have been investi-
ated. One study assessing telomere length in the cerebellar grayatter of patients diagnosed with MDD, BD and schizophrenia
AT).
found no difference in mean telomere length between the threegroups and controls. Since mean telomere length has been reportedto be a heritable quantitative trait, the authors also carried outgenome-wide mapping of genetic factors for telomere length andno association survived correction of multiple comparisons for thenumber of SNPs studied. This suggests that genetic predispositionto shorter telomere length could be determined by multiple lociwith small effect sizes (Zhang et al., 2010).
Although a cause-effect relationship cannot be definitivelyestablished, stress and its impact in the organism have been postu-lated as an important factor. In subjects with MDD, telomere lengthwas inversely correlated with oxidative stress and with inflamma-tion in depressed individuals (Wolkowitz et al., 2011). In addition,stress is implicated as a crucial causal mechanism for mood disor-ders, as well as for aging. In one study of individuals with MDD,short telomere length was associated with Perceived Stress Ques-tionnaire scores, and with a hypocortisolemic state, which wasespecially prevalent among patients with a high familial loadingof affective disorders and high levels of C-reactive protein levels(Wikgren et al., 2012).
A possible limitation of current research investigating telom-eres in mood disorders is the possibility of tissue-specific changes.It is possible that premature senescence may occur particularly inrapidly dividing tissues such as leukocytes, sparing others such asthe cerebellar gray matter, as suggested by Zhang and collaborators.Analyses that include other brain regions, particularly the sub-granular zone of the dentate gyrus or the subventrical zone whereneurogenesis continues into adulthood may be more appropriate.
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Additionally, analyses that seek to identify correlations betweenother peripheral senescence-related biomarkers with telomerelength and clinical symptoms or staging in BD are also warranted Q3(Fig. 1).
596
597
598
599
ARTICLE ING ModelNBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and Biobeha
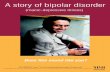
Fig. 2. The relation between Allostatic Load (AL) and Accelerated Aging (AA)hypotheses. Both hypotheses are complementary, the higher the allostatic loadexperienced by BD patients, the higher will the demand of mechanisms to recoverhomeostasis. This leads to an exhaustion of the entire system and promotes theaccelerated aging. The AA paradigm expands the AL hypothesis to its long termconsequences, but also offers new insights into the etiopathology of BD, putting inperspective some of the current knowledge and indicating new areas for furtherrg
3
pwtaadt
Afcmtcbpstrhp
rstOoa(astEsssto2
and interaction with GSK-3 and Bcl-2 (Lai et al., 2006).
600
601
602
603
604
605
606
607
608
609
610
611
612
613
614
615
616
617
618
619
620
621
622
623
624
625
626
627
628
629
630
631
632
633
634
635
636
637
638
639
640
641
642
643
644
645
646
647
648
649
650
651
652
653
654
655
656
657
658
659
660
661
662
663
664
665
666
667
668
669
670
671
672
673
674
675
676
677
678
679
680
681
682
683
684
685
686
687
688
689
690
691
692
693
694
695
696
697
698
699
700
701
esearch. AA hypothesis also opens the field on thinking BD as not just a neuropro-ressive, but a somatoprogressive disorder.
. Implications for research directed to clinical care
Bipolar disorder is a complex disease, accumulating evidenceoints to the involvement of a myriad of pathophysiological path-ays that are dynamic and interact with each other and with
he environment. Notwithstanding these foraging observations, unitary disease model is still unavailable, necessitating furtherdvancement of our understanding of this multifaceted mentalisorder, and the development and refinement of comprehensiveheoretical frameworks.
One integrative hypothesis for neuroprogression in BD is thellostatic Load (AL) which says that BD patients are under stress-
ul conditions (cyclic mood episodes, drug addiction and otheromorbidities) and struggle to restore homeostasis by allostaticechanisms. In the same way, aging can be thought as a loss in
he capability to reattain homeostasis (O’Neill, 1997). In this con-ept, the AA and AL hypotheses are complementary (Fig. 2), theurden of BD promotes exhaustion of allostatic mechanisms thatromote homeostasis. The AA paradigm expands the AL hypothe-is to its long term consequences, but also offer new insights intohe etiopathology of BD, putting in perspective some of the cur-ent knowledge and indicating new areas for further research. AAypothesis also opens the field on thinking BD as not just a neuro-rogressive, but a somatoprogressive disorder.
Although the most explored models for progression of BD areelated to stress, it is intuitive that, even organisms that are notubmitted to chronic stress will age. In addition to environmen-al agents, there is also a strong genetic component in aging.ne interesting insight about genetic component in aging can bebtained from diseases marked by a highly accelerated aging, suchs Hutchinson-Gilford Progeria (HGP) and Werner syndrome (WS)Hegele, 2003; Heyn et al., 2013). As naturally aged individuals, HGPnd WS patients present hair graying, skin thinning, atherosclero-is and osteopenia. Genetically, the disease could be traced backo mutations in lamin A (LMNA) (De Sandre-Giovannoli et al., 2003;riksson et al., 2003; Worman and Bonne, 2007) and the Werneryndrome RecQ helicase like (WRN) (Yu et al., 1996) genes. Althoughimilarities between these conditions and BD were never explored,chizophrenia was conceptualized by some authors as a segmen-
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
al Progeria, due to similarities in genetic and epigenetic controlf CNS senescence between the disorders (Papanastasiou et al.,011).
PRESSvioral Reviews xxx (2014) xxx–xxx 7
From a clinical point of view, based on the evidence of the pro-gressive nature of BD, some authors propose that the notion ofclinical staging can be applied to BD (Kapczinski et al., 2009; Scottet al., 2013). The main benefits are allowing better prognosis andmore personalized treatments. The use of biomarkers, includingneurotrophins, inflammatory markers and oxidative stress mark-ers have been proposed as auxiliary tools to refine the descriptionof the stages (Kapczinski et al., 2009). In this sense, age-relatedfeatures, such as the presence of medical comorbidities, cognitiveimpairment and shortened telomere length could be useful in thecharacterization of clinical stages. Also, investigation of the pro-gression of these features along the course of the disease may allowearly interventions aimed at better management and prognoses forpatients.
Finally, the recognition of aging processes as part of the BD puz-zle leads to the possibility of treatments targeting specifically thesepathways the so-called “anti-aging” strategies, including nutri-tional approaches and pharmacological and non-pharmacologicalinterventions
3.1. Pharmacological strategies
3.1.1. Current pharmacology modulating aging relatedmechanisms
The mechanisms of action of drugs currently used to treat BD isnot completely understood, but there are some data showing theircapability to modulate pathways related to aging. Patients in treat-ment with lithium show reduced neuronal loss and higher level ofN-acetyl-aspartate (NAA) (marker of neuronal viability) (Beardenet al., 2007; Moore et al., 2000), suggesting a neuroprotectionaleffect by lithium which is already known to be partially mediatedby several mechanisms, its capability to reduce glutamate-inducedexcitotoxicity by NMDA receptors (Hashimoto et al., 2002), directand indirect inhibittion of the pro-apoptotic protein Glycogen syn-thase kinase 3 (GSK-3) (Chiu and Chuang, 2011; Stambolic et al.,1996), induction the antiapoptotic protein B-cell lymphoma 2 (Bcl-2) (Chen and Chuang, 1999) and induction of the growth factorsBDNF (Fukumoto et al., 2001) and vascular endothelial growth fac-tor (VEGF) (Guo et al., 2009).
Over the last years, GSK-3 was also identified as a regulator ofmany components of the immune system. GSK-3 plays an impor-tant role in the signal transmission to promote production of thepro-inflammatory cytokines IL-6, IL-1�, IL-12p40, IFN� and TNF-�and inhibition of the anti-inflammatory cytokine IL-10 and IL1-RA(Beurel et al., 2010). The inhibition of GSK-3 by lithium and itsconsequent impact in the immune system may be one of the ther-apeutic mechanisms of lithium. Recently, the recognition that BDpatients that were lithium intakers had longer telomeres raised thequestion by which means lithium could promote telomere exten-sion. It seems to be also related to the inhibition of GSK-3 andconsequently promoting the transcription hTERT the catalytic sub-unit bearing the enzymatic activity of telomerase (Martinsson et al.,2013).
Lithium also seems to plays a role in the reduction of oxida-tive stress, since lithium treated patients present lower peripherallevels of oxidative stress makers like TBARS, SOD and CAT com-pared to unmedicated patients (Machado-Vieira et al., 2007). Also,lithium pré-treatment was able to protect human neuroblastoma(SH-SY5Y) cell line from rotenone and H2O2-induced cytotoxicity(Lai et al., 2006). The mechanism by which the medication medi-ates oxidative protection is not yet completely understood, but itis partly due to induction of antioxidant proteins like CAT and SOD,
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Valproic acid (VPA) also inhibits GSK-3 activity, although itis now clear yet if it shares the same direct effect as lithiumor other mechanism are involved (Chen et al., 1999; Rosenberg,
702
703
704
ING ModelN
8 iobeha
2iecebc3eias(u
3
eir1rlc2iliohn2
fae(cmtBrt2tB
lcaVad2aptbpsagdg
705
706
707
708
709
710
711
712
713
714
715
716
717
718
719
720
721
722
723
724
725
726
727
728
729
730
731
732
733
734
735
736
737
738
739
740
741
742
743
744
745
746
747
748
749
750
751
752
753
754
755
756
757
758
759
760
761
762
763
764
765
766
767
768
769
770
771
772
773
774
775
776
777
778
779
780
781
782
783
784
785
786
787
788
789
790
791
792
793
794
795
796
797
798
799
800
801
802
803
804
805
806
807
808
809
810
811
812
813
814
815
816
817
818
819
820
821
822
823
824
825
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
007). VPA also impacts in the immunological system promot-ng anti-inflammatory effects in different models as ischemia andxperimental auto-immune neuritis reducing pro-inflammatoryytokines IFN-�, TNF-�, IL-1, IL-6 and IL-17, and also elevating lev-ls of Treg cell (Zhang et al., 2008; Zhang et al., 2012). Mechanismsy which VPA promotes the anti-inflammatory effect needs to belarified, but it seems to be partly mediated by inhibition of GSK-
and histone deacetylase inhibition (Beurel et al., 2010; Grabiect al., 2011). The relation between GSK-3 inhibition by VPA andnduction of hTERT transcription still needs to be investigated. VPAnd atypical antipsychotics also seems to promote effect on cellurvival by elevating levels BDNF and fibroblast growth factor 1FGF1)(Bai et al., 2003; Kao et al., 2013; Yasuda et al., 2009) andpregulating Bcl-2 (Bai et al., 2004).
.1.2. Sirtuins as possible new targetThe sirtuins are a family of ribosyltransferase or deacylase
nzymes that influence a plethora of processes involved in aging,ncluding apoptosis, DNA repair, the inflammatory response andesistance to stress. The mammalian sirtuin homologues, SIRTs–7, are also involved in energy metabolism, with a particularole in metabolic efficiency and maintenance of function duringow energy situations. The sirtuin genes can be upregulated byalorie restriction, with longevity promoting effects (Kanfi et al.,012). For example, SIRT6 is expressed in the nucleus where it
s involved in DNA repair, regulating cell metabolism, and regu-ating the secretion of TNF. In male mice, over-expression of Sirt6ncreases lifespan and alters IGF-1 signaling, consistent with a rolef IGF-1 in determining longevity (Kanfi et al., 2012). On the otherand, SIRT6 deficiency leads to enhanced NF-�B dependent sig-aling, apoptosis and accelerated cell senescence (Kawahara et al.,009).
Recently, decreased expression of SIRT1, SIRT2 and SIRT6 wasound in white blood cells collected from BD patients in states ofcute depression compared to controls. In contrast, SIRT mRNA lev-ls in euthymic BD patients were different from those of controlsAbe et al., 2011), suggesting that sirtuin genes may be defi-iently expressed in BD, and that sirtuin expression may be a statearker of illness. Previously, differences have been described in
he response of white blood cells to glucose deprivation betweenD subjects and controls – whereas healthy controls showed up-egulated transcripts related to mitochondrial energy metabolism,hese transcripts were down-regulated in BD (Naydenov et al.,007). Sirtuin expression would seem to be a compensatory pro-ective measure, and this resilience pathway may be defective inD.
These observations suggest the possibility for novel pharmaco-ogical interventions. For instance, in animal models, resveratrolan activate SIRT1, prolonging the lifespan in obese animalsnd reversing age-related cardiovascular dysfunction (Alcain andillalba, 2009; Barger et al., 2008). More potent pharmacologicalctivators of SIRT1 are under development. These agents can moreramatically increase mitochondrial activity (Alcain and Villalba,009). Interestingly, sirtuin activity is inhibited by nictotinamide,
final product of the kynurenine pathway and an important com-onent of NAD and NADPH involved in the mitochondrial electronransport chain. It has been suggested that blocking nicotinamideinding to its cognate receptors could enhance sirtuin activity andrevent tissue damage caused by age-related degenerative diseasesuch as diabetes, Alzheimers and atherosclerosis (David Adams
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
nd Lori, 2007; Milne et al., 2007). These pharmacological strate-ies might be useful to mitigate the cellular damage that occursuring depressive episodes, and prevent the associated neuropro-ression.
PRESSvioral Reviews xxx (2014) xxx–xxx
3.2. Non-pharmacological strategies
3.2.1. Physical activityPhysical activity and cardiopulmonary fitness are well-
documented neuroprotective strategies that can increase brainvolumes (Colcombe et al., 2006; Colcombe et al., 2006) and pre-serve cognitive function later in life (Barnes et al., 2003) evenin groups of patients with concomitant cardiovascular morbidity(Swardfager et al., 2010a) or clinical mild cognitive impairment(Baker et al., 2010). It has been suggested that these effects may bemediated, in part by augmentation of neurotrophin concentrations(e.g. BDNF and IGF-1) (Erickson et al., 2011; Llorens-Martin et al.,2010; Swardfager et al., 2011) but improvements in other aspects ofphysiological function may also ameliorate neurocognitive decline,including improvements in vascular endothelial function (Banket al., 1998; Fuchsjager-Mayrl et al., 2002; Xiang et al., 2009). Vas-cular endothelial dysfunction is related to increased generationof oxidative species, which can irreversibly damage intracellularcomponents of the cerebral neurovascular unit and compromiseregulation of cerebral blood flow and thus brain function. Vascu-lar endothelial cell senescence and changes in vascular endothelialfunction occur with aging, favoring pro-inflammatory and pro-oxidant processes that may contribute substantially to age-relatedneurological decline (Yildiz, 2007), particularly since these pro-cesses are exacerbated by age-related cognitive risk factors suchas diabetes and hypertension.
Physical activity is also known to increase telomerase activityboth in human and animal models (Ludlow et al., 2012; Werneret al., 2008; Wolf et al., 2011). Telomerase has not yet been eval-uated in BD, but there are reports of decreased activity in majordepression and schizophrenia (Porton et al., 2008; Wolkowitz et al.,2012). These data suggest that BD may follow the same direction,and other mechanism by which patients could be benefited by exer-cise.
The extant literature suggests that BD, and manic or hypo-manic symptoms in particular, may be associated with prematureincreases in vascular endothelial dysfunction (Fiedorowicz et al.,2012; Rybakowski et al., 2006). Physical activity as a means to pro-mote vascular endothelial health or telomere length in BD has notyet been assessed; however, poorer physical fitness can confer anincreased risk of affective disorders including BD (Aberg et al., 2012)and exercise has been suggested as a strategy to improve cognitionin BD (Ng et al., 2007). Prospective controlled studies are needed,and related mechanisms require further investigation (Kucyi et al.,2010).
4. Conclusions
There is considerable overlap between neurobiological charac-teristics of BD and processes of both normal and pathological aging,which is evident in clinical, physiological, neurostructural, cellular,and molecular studies. The strengths of the AA integrative view ofBD progression are that the hypothesis comprises and also expendsthe neuroprogression and allostatic load view, also expands thefield of possible biological mechanisms involved in the pathophys-iology of the disease. The AA hypothesis also creates a theoreticalframework that encompasses not only neurological but also sys-temic alterations involved in the pathophysiology of BD.
Although AA hypothesis integrates the current knowledgeregarding progression of BD, it does not provide direct answersabout the mechanisms that generate mood cyclicity. Yet, in
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
our concept, mood cyclicity generates stressful conditions thatdemand the action of biological mechanisms to reattain homeo-stasis, the chronicity of this conditions could promote acceleratedaging (Fig. 2). Other limitation is that albeit there are compelling
826
827
828
829
ING ModelN
iobeha
dm
fstsoae
aptii
C
e
UQ4
eePe
A
dN(
HT
R
A
A
AA
A
A
A
AA
A
830
831
832
833
834
835
836
837
838
839
840
841
842
843
844
845
846
847
848
849
850
851
852
853
854
855
856
857
858
859
860
861
862
863
864
865
866
867
868
869
870
871
872
873
874
875
876
877
878
879
880
881
882
883
884
885
886
887
888
889
890
891
892
893
894
895
896
897
898
899
900
901
902
903
904
905
906
907
908
909
910
911
912
913
914
915
916
917
918
919
920
921
922
923
924
925
926
927
928
929
930
931
932
933
934
935
936
937
938
939
940
941
942
943
944
945
946
947
948
949
950
951
952
953
954
955
956
957
958
959
960
961
962
963
964
965
966
967
968
969
970
971
972
973
974
975
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
ata supporting AA hypothesis, most studies use cross-sectionalethodology which are more susceptible to bias.The present work, creates the basis for new prospective studies
ocusing on AA framework and consequently bring more under-tanding about BD etiology and physiology. Although the scope ofhe present work made an in deep analysis of AA in BD, there areome data suggesting that this concept could be extrapolated forther psychiatric disorders like major depression, schizophreniand posttraumatic stress disorder (Simon et al., 2006; Wolkowitzt al., 2010).
Finally, the exploration of physiological processes involved inging provides useful insights into the biology of BD, and newotential to suggest new avenues of treatment. Notwithstanding,he associated of controversy and practical challenges, anti-agingnterventions could be beneficial in subpopulations of BD warrant-ng further investigation.
onflict of interest statement
The authors declare that they have no competing financial inter-sts.
ncited references
Chen et al., 2000, Elkind et al., 2010, Floratou et al., 2012, Glaspert al., 2010, Higashi et al., 2012, Holzenberger et al., 2003, Katant al., 2013, Kelley et al., 2013, Kenyon, 2010, Mitschelen et al., 2011,ark et al., 2011, Pereira et al., 2011, Sesti et al., 2005, Squassinat al., 2013, Swardfager and Black, 2013 and Wang et al., 2010.
cknowledgements
The authors acknowledge support by fellowships from Coor-ination of Improvement of Higher Education Personnel (CAPES),ational Counsel of Technological and Scientific Development
CNPq) and São Paulo Research Foundation (Fapesp).Dr. Swardfager acknowledges support by fellowships from the
eart & Stroke Foundation Centre for Stroke Recovery and theoronto Rehabilitation Institute.
eferences
be, N., Uchida, S., Otsuki, K., Hobara, T., Yamagata, H., Higuchi, F., Shibata, T., Watan-abe, Y., 2011. Altered sirtuin deacetylase gene expression in patients with amood disorder. J. Psychiatr. Res. 45, 1106–1112.
berg, M.A., Waern, M., Nyberg, J., Pedersen, N.L., Bergh, Y., Aberg, N.D., Nilsson, M.,Kuhn, H.G., Toren, K., 2012. Cardiovascular fitness in males at age 18 and risk ofserious depression in adulthood: Swedish prospective population-based study.Br. J. Psychiatry 201, 352–359.
lcain, F.J., Villalba, J.M., 2009. Sirtuin activators. Expert Opin. Ther. Pat. 19, 403–414.lbert, S.M., Michaels, K., Padilla, M., Pelton, G., Bell, K., Marder, K., Stern, Y.,
Devanand, D.P., 1999. Functional significance of mild cognitive impairmentin elderly patients without a dementia diagnosis. Am. J. Geriatr. Psychiatry 7,213–220.
llen, J.S., Bruss, J., Brown, C.K., Damasio, H., 2005. Normal neuroanatomical variationdue to age: the major lobes and a parcellation of the temporal region. Neurobiol.Aging 26, 1245–1260, discussion 1279-1282.
lmanzar, G., Schwaiger, S., Jenewein, B., Keller, M., Herndler-Brandstetter,D., Wurzner, R., Schonitzer, D., Grubeck-Loebenstein, B., 2005. Long-termcytomegalovirus infection leads to significant changes in the composition of theCD8+ T-cell repertoire, which may be the basis for an imbalance in the cytokineproduction profile in elderly persons. J. Virol. 79, 3675–3683.
miard, S., Doudeau, M., Pinte, S., Poulet, A., Lenain, C., Faivre-Moskalenko, C.,Angelov, D., Hug, N., Vindigni, A., Bouvet, P., Paoletti, J., Gilson, E., Giraud-Panis,M.J., 2007. A topological mechanism for TRF2-enhanced strand invasion. Nat.Struct. Mol. Biol. 14, 147–154.
nderson, I.M., Haddad, P.M., Scott, J., 2012. Bipolar disorder. BMJ 345, e8508.ndreazza, A.C., Kapczinski, F., Kauer-Sant’Anna, M., Walz, J.C., Bond, D.J., Goncalves,
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
C.A., Young, L.T., Yatham, L.N., 2009. 3-Nitrotyrosine and glutathione antioxidantsystem in patients in the early and late stages of bipolar disorder. J. PsychiatryNeurosci. 34, 263–271.
prahamian, I., Nunes, P.V., Forlenza, O.V., 2013. Cognitive impairment and dementiain late-life bipolar disorder. Curr. Opin. Psychiatry 26, 120–123.
PRESSvioral Reviews xxx (2014) xxx–xxx 9
Arancio, O., Chao, M.V., 2007. Neurotrophins, synaptic plasticity and dementia. Curr.Opin. Neurobiol. 17, 325–330.
Arvanitis, D.N., Ducatenzeiler, A., Ou, J.N., Grodstein, E., Andrews, S.D., Tendulkar,S.R., Ribeiro-da-Silva, A., Szyf, M., Cuello, A.C., 2007. High intracellular concen-trations of amyloid-beta block nuclear translocation of phosphorylated CREB. J.Neurochem. 103, 216–228.
Aubert, G., Lansdorp, P.M., 2008. Telomeres and aging. Physiol. Rev. 88, 557–579.Bai, O., Chlan-Fourney, J., Bowen, R., Keegan, D., Li, X.M., 2003. Expression of brain-
derived neurotrophic factor mRNA in rat hippocampus after treatment withantipsychotic drugs. J. Neurosci. Res. 71, 127–131.
Bai, O., Zhang, H., Li, X.M., 2004. Antipsychotic drugs clozapine and olanzapine upreg-ulate bcl-2 mRNA and protein in rat frontal cortex and hippocampus. Brain Res.1010, 81–86.
Baker, L.D., Frank, L.L., Foster-Schubert, K., Green, P.S., Wilkinson, C.W., McTiernan,A., Plymate, S.R., Fishel, M.A., Watson, G.S., Cholerton, B.A., Duncan, G.E., Mehta,P.D., Craft, S., 2010. Effects of aerobic exercise on mild cognitive impairment: acontrolled trial. Arch. Neurol. 67, 71–79.
Bank, A.J., Shammas, R.A., Mullen, K., Chuang, P.P., 1998. Effects of short-termforearm exercise training on resistance vessel endothelial function in normalsubjects and patients with heart failure. J. Card. Fail. 4, 193–201.
Barger, J.L., Kayo, T., Vann, J.M., Arias, E.B., Wang, J., Hacker, T.A., Wang, Y., Raed-erstorff, D., Morrow, J.D., Leeuwenburgh, C., Allison, D.B., Saupe, K.W., Cartee,G.D., Weindruch, R., Prolla, T.A., 2008. A low dose of dietary resveratrol partiallymimics caloric restriction and retards aging parameters in mice. PLoS ONE 3,e2264.
Barnes, D.E., Yaffe, K., Satariano, W.A., Tager, I.B., 2003. A longitudinal study ofcardiorespiratory fitness and cognitive function in healthy older adults. J. Am.Geriatr. Soc. 51, 459–465.
Bearden, C.E., Thompson, P.M., Dalwani, M., Hayashi, K.M., Lee, A.D., Nicoletti, M.,Trakhtenbroit, M., Glahn, D.C., Brambilla, P., Sassi, R.B., Mallinger, A.G., Frank, E.,Kupfer, D.J., Soares, J.C., 2007. Greater cortical gray matter density in lithium-treated patients with bipolar disorder. Biol. Psychiatry 62, 7–16.
Benedict, C.A., Loewendorf, A., Garcia, Z., Blazar, B.R., Janssen, E.M., 2008. Dendriticcell programming by cytomegalovirus stunts naive T cell responses via the PD-L1/PD-1 pathway. J. Immunol. 180, 4836–4847.
Bentz, G.L., Jarquin-Pardo, M., Chan, G., Smith, M.S., Sinzger, C., Yurochko, A.D., 2006.Human cytomegalovirus (HCMV) infection of endothelial cells promotes naivemonocyte extravasation and transfer of productive virus to enhance hematoge-nous dissemination of HCMV. J. Virol. 80, 11539–11555.
Berk, M., 2009. Neuroprogression: pathways to progressive brain changes in bipolardisorder. Int. J. Neuropsychopharmacol. 12, 441–445.
Berk, M., Conus, P., Kapczinski, F., Andreazza, A.C., Yucel, M., Wood, S.J., Pantelis,C., Malhi, G.S., Dodd, S., Bechdolf, A., Amminger, G.P., Hickie, I.B., McGorry, P.D.,2010. From neuroprogression to neuroprotection: implications for clinical care.Med. J. Aust. 193, S36–S40.
Berk, M., Kapczinski, F., Andreazza, A.C., Dean, O.M., Giorlando, F., Maes, M., Yucel, M.,Gama, C.S., Dodd, S., Dean, B., Magalhaes, P.V., Amminger, P., McGorry, P., Malhi,G.S., 2011. Pathways underlying neuroprogression in bipolar disorder: focus oninflammation, oxidative stress and neurotrophic factors. Neurosci. Biobehav.Rev. 35, 804–817.
Beurel, E., Michalek, S.M., Jope, R.S., 2010. Innate and adaptive immune responsesregulated by glycogen synthase kinase-3 (GSK3). Trends Immunol. 31, 24–31.
Blackburn, E.H., 2001. Switching and signaling at the telomere. Cell 106, 661–673.Blackburn, E.H., Chan, S., Chang, J., Fulton, T.B., Krauskopf, A., McEachern, M., Prescott,
J., Roy, J., Smith, C., Wang, H., 2000. Molecular manifestations and moleculardeterminants of telomere capping. Cold Spring Harb. Symp. Quant. Biol. 65,253–263.
Brietzke, E., Kapczinski, F., Grassi-Oliveira, R., Grande, I., Vieta, E., McIntyre, R.S.,2011. Insulin dysfunction and allostatic load in bipolar disorder. Expert Rev.Neurother. 11, 1017–1028.
Brietzke, E., Kauer-Sant’Anna, M., Teixeira, A.L., Kapczinski, F., 2009a. Abnormalitiesin serum chemokine levels in euthymic patients with bipolar disorder. BrainBehav. Immun. 23, 1079–1082.
Brietzke, E., Kauer Sant’anna, M., Jackowski, A., Grassi-Oliveira, R., Bucker, J., Zug-man, A., Mansur, R.B., Bressan, R.A., 2012a. Impact of childhood stress onpsychopathology. Rev. Bras. Psiquiatr. 34, 480–488.
Brietzke, E., Mansur, R.B., Soczynska, J., Powell, A.M., McIntyre, R.S., 2012b. Atheoretical framework informing research about the role of stress in the patho-physiology of bipolar disorder. Prog. Neuro-Psychopharmacol. Biol. Psychiatry39, 1–8.
Brietzke, E., Stertz, L., Fernandes, B.S., Kauer-Sant’anna, M., Mascarenhas, M.,Escosteguy Vargas, A., Chies, J.A., Kapczinski, F., 2009b. Comparison of cytokinelevels in depressed, manic and euthymic patients with bipolar disorder. J. Affect.Disord. 116, 214–217.
Capuron, L., Schroecksnadel, S., Feart, C., Aubert, A., Higueret, D., Barberger-Gateau,P., Laye, S., Fuchs, D., 2011. Chronic low-grade inflammation in elderly per-sons is associated with altered tryptophan and tyrosine metabolism: role inneuropsychiatric symptoms. Biol. Psychiatry 70, 175–182.
Cawthon, R.M., Smith, K.R., O’Brien, E., Sivatchenko, A., Kerber, R.A., 2003. Associationbetween telomere length in blood and mortality in people aged 60 years or older.Lancet 361, 393–395.
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Chen, G., Huang, L.D., Jiang, Y.M., Manji, H.K., 1999. The mood-stabilizing agent val-proate inhibits the activity of glycogen synthase kinase-3. J. Neurochem. 72,1327–1330.
Chen, G., Rajkowska, G., Du, F., Seraji-Bozorgzad, N., Manji, H.K., 2000. Enhancementof hippocampal neurogenesis by lithium. J. Neurochem. 75, 1729–1734.
976
977
978
979
980
ING ModelN
1 iobeha
C
C
C
C
CQ5
C
d
D
D
d
D
D
D
d
D
D
E
E
E
E
E
F
F
F
F
F
F
F
981
982
983
984
985
986
987
988
989
990
991
992
993
994
995
996
997
998
999
1000
1001
1002
1003
1004
1005
1006
1007
1008
1009
1010
1011
1012
1013
1014
1015
1016
1017
1018
1019
1020
1021
1022
1023
1024
1025
1026
1027
1028
1029
1030
1031
1032
1033
1034
1035
1036
1037
1038
1039
1040
1041
1042
1043
1044
1045
1046
1047
1048
1049
1050
1051
1052
1053
1054
1055
1056
1057
1058
1059
1060
1061
1062
1063
1064
1065
1066
1067
1068
1069
1070
1071
1072
1073
1074
1075
1076
1077
1078
1079
1080
1081
1082
1083
1084
1085
1086
1087
1088
1089
1090
1091
1092
1093
1094
1095
1096
1097
1098
1099
1100
1101
1102
1103
1104
1105
1106
1107
1108
1109
1110
1111
1112
1113
1114
1115
1116
1117
1118
1119
1120
1121
1122
1123
1124
1125
1126
1127
1128
1129
1130
1131
1132
1133
1134
1135
1136
1137
1138
1139
1140
1141
1142
1143
1144
1145
1146
1147
ARTICLEBR 1894 1–13
0 L.B. Rizzo et al. / Neuroscience and B
hen, R.W., Chuang, D.M., 1999. Long term lithium treatment suppresses p53 andBax expression but increases Bcl-2 expression. A prominent role in neuropro-tection against excitotoxicity. J. Biol. Chem. 274, 6039–6042.
hiu, C.T., Chuang, D.M., 2011. Neuroprotective action of lithium in disorders of thecentral nervous system. Zhong Nan Da Xue Xue Bao Yi Xue Ban 36, 461–476.
olcombe, S.J., Erickson, K.I., Scalf, P.E., Kim, J.S., Prakash, R., McAuley, E., Elavsky,S., Marquez, D.X., Hu, L., Kramer, A.F., 2006. Aerobic exercise training increasesbrain volume in aging humans. J. Gerontol. A: Biol. Sci. Med. Sci. 61, 1166–1170.
onnor, C.M., Guo, Y., Akbarian, S., 2009. Cingulate white matter neurons inschizophrenia and bipolar disorder. Biol. Psychiatry 66, 486–493.
rump, C., Sundquist, K., Winkleby, M.A., Sundquist, J., 2013. Comorbidities andmortality in bipolar disorder: a Swedish National Cohort Study. JAMA Psychiatry.
zepielewski, L., Daruy Filho, L., Brietzke, E., Grassi-Oliveira, R., 2013. Bipolar dis-order and metabolic syndrome: a systematic review. Rev. Bras. Psiquiatr. 35,88–93.
a Silva, J., Goncalves-Pereira, M., Xavier, M., Mukaetova-Ladinska, E.B., 2013.Affective disorders and risk of developing dementia: systematic review. Br. J.Psychiatry 202, 177–186.
as, S., Basu, A., 2007. Inflammation: a new candidate in modulating adult neuro-genesis. J. Neurosci. Res.
avid Adams Jr., J.K., Lori, K., 2007. Sirtuins, nicotinamide and aging: a critical review.Lett. Drug Des. Discov. 4, 44–48.
e Jong, D., Jansen, R., Hoefnagels, W., Jellesma-Eggenkamp, M., Verbeek, M., Borm,G., Kremer, B., 2008. No effect of one-year treatment with indomethacin onAlzheimer’s disease progression: a randomized controlled trial. PLoS ONE 3,e1475.
e Sandre-Giovannoli, A., Bernard, R., Cau, P., Navarro, C., Amiel, J., Boccaccio, I.,Lyonnet, S., Stewart, C.L., Munnich, A., Le Merrer, M., Levy, N., 2003. Lamin atruncation in Hutchinson-Gilford progeria. Science 300, 2055.
eCarli, C., Massaro, J., Harvey, D., Hald, J., Tullberg, M., Au, R., Beiser, A., D’Agostino,R., Wolf, P.A., 2005. Measures of brain morphology and infarction in the fram-ingham heart study: establishing what is normal. Neurobiol. Aging 26, 491–510.
erhovanessian, E., Larbi, A., Pawelec, G., 2009. Biomarkers of human immunosenes-cence: impact of Cytomegalovirus infection. Curr. Opin. Immunol. 21, 440–445.
o Prado, C.H., Rizzo, L.B., Wieck, A., Lopes, R.P., Teixeira, A.L., Grassi-Oliveira, R.,Bauer, M.E., 2013. Reduced regulatory T cells are associated with higher levels ofTh1/TH17 cytokines and activated MAPK in type 1 bipolar disorder. Psychoneu-roendocrinology 38, 667–676.
ouillard-Guilloux, G., Guilloux, J.P., Lewis, D.A., Sibille, E., 2013. Anticipated brainmolecular aging in major depression. Am. J. Geriatr. Psychiatry 21, 450–460.
riscoll, I., Martin, B., An, Y., Maudsley, S., Ferrucci, L., Mattson, M.P., Resnick, S.M.,2012. Plasma BDNF is associated with age-related white matter atrophy but notwith cognitive function in older, non-demented adults. PLoS ONE 7, e35217.
lkind, M.S., Luna, J.M., Moon, Y.P., Boden-Albala, B., Liu, K.M., Spitalnik, S., Rundek,T., Sacco, R.L., Paik, M.C., 2010. Infectious burden and carotid plaque thickness:the northern Manhattan study. Stroke 41, e117–e122.
lvsashagen, T., Vera, E., Boen, E., Bratlie, J., Andreassen, O.A., Josefsen, D., Malt, U.F.,Blasco, M.A., Boye, B., 2011. The load of short telomeres is increased and associ-ated with lifetime number of depressive episodes in bipolar II disorder. J. Affect.Disord. 135, 43–50.
nzinger, C., Fazekas, F., Matthews, P.M., Ropele, S., Schmidt, H., Smith, S., Schmidt, R.,2005. Risk factors for progression of brain atrophy in aging: six-year follow-upof normal subjects. Neurology 64, 1704–1711.
rickson, K.I., Voss, M.W., Prakash, R.S., Basak, C., Szabo, A., Chaddock, L., Kim, J.S.,Heo, S., Alves, H., White, S.M., Wojcicki, T.R., Mailey, E., Vieira, V.J., Martin,S.A., Pence, B.D., Woods, J.A., McAuley, E., Kramer, A.F., 2011. Exercise train-ing increases size of hippocampus and improves memory. Proc. Natl. Acad. Sci.U.S.A. 108, 3017–3022.
riksson, M., Brown, W.T., Gordon, L.B., Glynn, M.W., Singer, J., Scott, L., Erdos, M.R.,Robbins, C.M., Moses, T.Y., Berglund, P., Dutra, A., Pak, E., Durkin, S., Csoka, A.B.,Boehnke, M., Glover, T.W., Collins, F.S., 2003. Recurrent de novo point mutationsin lamin A cause Hutchinson-Gilford progeria syndrome. Nature 423, 293–298.
agiolini, A., Chengappa, K.N., Soreca, I., Chang, J., 2008. Bipolar disorder and themetabolic syndrome: causal factors, psychiatric outcomes and economic bur-den. CNS Drugs 22, 655–669.
ernandes, B.S., Gama, C.S., Cereser, K.M., Yatham, L.N., Fries, G.R., Colpo, G., deLucena, D., Kunz, M., Gomes, F.A., Kapczinski, F., 2011. Brain-derived neu-rotrophic factor as a state-marker of mood episodes in bipolar disorders: asystematic review and meta-regression analysis. J. Psychiatr. Res. 45, 995–1004.
iedorowicz, J.G., Coryell, W.H., Rice, J.P., Warren, L.L., Haynes, W.G., 2012. Vas-culopathy related to manic/hypomanic symptom burden and first-generationantipsychotics in a sub-sample from the collaborative depression study. Psy-chother. Psychosom. 81, 235–243.
loratou, K., Giannopoulou, E., Antonacopoulou, A., Karakantza, M., Adonakis, G.,Kardamakis, D., Matsouka, P., 2012. Oxidative stress due to radiation in CD34(+)hematopoietic progenitor cells: protection by IGF-1. J. Radiat. Res. 53, 672–685.
otenos, A.F., Snyder, A.Z., Girton, L.E., Morris, J.C., Buckner, R.L., 2005. Normativeestimates of cross-sectional and longitudinal brain volume decline in aging andAD. Neurology 64, 1032–1039.
ranceschi, C., Capri, M., Monti, D., Giunta, S., Olivieri, F., Sevini, F., Panourgia, M.P.,Invidia, L., Celani, L., Scurti, M., Cevenini, E., Castellani, G.C., Salvioli, S., 2007.
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
Inflammaging and anti-inflammaging: a systemic perspective on aging andlongevity emerged from studies in humans. Mech. Ageing Dev. 128, 92–105.
ries, G.R., Pfaffenseller, B., Stertz, L., Paz, A.V., Dargel, A.A., Kunz, M., Kapczinski, F.,2012. Staging and neuroprogression in bipolar disorder. Curr. Psychiatry Rep.14, 667–675.
PRESSvioral Reviews xxx (2014) xxx–xxx
Fuchs, T., Trollor, J.N., Crawford, J., Brown, D.A., Baune, B.T., Samaras, K., Campbell,L., Breit, S.N., Brodaty, H., Sachdev, P., Smith, E., 2013. Macrophage inhibitorycytokine-1 is associated with cognitive impairment and predicts cognitivedecline – the Sydney Memory and Ageing Study. Aging Cell.
Fuchsjager-Mayrl, G., Pleiner, J., Wiesinger, G.F., Sieder, A.E., Quittan, M., Nuhr, M.J.,Francesconi, C., Seit, H.P., Francesconi, M., Schmetterer, L., Wolzt, M., 2002. Exer-cise training improves vascular endothelial function in patients with type 1diabetes. Diabetes Care 25, 1795–1801.
Fukumoto, T., Morinobu, S., Okamoto, Y., Kagaya, A., Yamawaki, S., 2001. Chroniclithium treatment increases the expression of brain-derived neurotrophic factorin the rat brain. Psychopharmacology (Berl.) 158, 100–106.
Geerlings, M.I., den Heijer, T., Koudstaal, P.J., Hofman, A., Breteler, M.M., 2008. Historyof depression, depressive symptoms, and medial temporal lobe atrophy and therisk of Alzheimer disease. Neurology 70, 1258–1264.
Gergerlioglu, H.S., Savas, H.A., Bulbul, F., Selek, S., Uz, E., Yumru, M., 2007. Changes innitric oxide level and superoxide dismutase activity during antimanic treatment.Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 697–702.
Ghedim, F.V., Fraga Dde, B., Deroza, P.F., Oliveira, M.B., Valvassori, S.S., Steckert, A.V.,Budni, J., Dal-Pizzol, F., Quevedo, J., Zugno, A.I., 2012. Evaluation of behavioraland neurochemical changes induced by ketamine in rats: implications as ananimal model of mania. J. Psychiatr. Res. 46, 1569–1575.
Giunta, S., 2008. Exploring the complex relations between inflammation andaging (inflamm-aging): anti-inflamm-aging remodelling of inflamm-aging, fromrobustness to frailty. Inflamm. Res. 57, 558–563.
Glasper, E.R., Llorens-Martin, M.V., Leuner, B., Gould, E., Trejo, J.L., 2010. Blockade ofinsulin-like growth factor-I has complex effects on structural plasticity in thehippocampus. Hippocampus 20, 706–712.
Goldstein, B.I., Fagiolini, A., Houck, P., Kupfer, D.J., 2009a. Cardiovascular disease andhypertension among adults with bipolar I disorder in the United States. BipolarDisord. 11, 657–662.
Goldstein, B.I., Kemp, D.E., Soczynska, J.K., McIntyre, R.S., 2009b. Inflammation andthe phenomenology, pathophysiology, comorbidity, and treatment of bipo-lar disorder: a systematic review of the literature. J. Clin. Psychiatry 70,1078–1090.
Gomez-Isla, T., Blesa, R., Boada, M., Clarimon, J., Del Ser, T., Domenech, G., Ferro,J.M., Gomez-Anson, B., Manubens, J.M., Martinez-Lage, J.M., Munoz, D., Pena-Casanova, J., Torres, F., 2008. A randomized, double-blind, placebo controlled-trial of triflusal in mild cognitive impairment: the TRIMCI study. Alzheimer Dis.Assoc. Disord. 22, 21–29.
Goronzy, J.J., Fulbright, J.W., Crowson, C.S., Poland, G.A., O’Fallon, W.M., Weyand,C.M., 2001. Value of immunological markers in predicting responsiveness toinfluenza vaccination in elderly individuals. J. Virol. 75, 12182–12187.
Goshen, I., Kreisel, T., Ben-Menachem-Zidon, O., Licht, T., Weidenfeld, J., Ben-Hur, T., Yirmiya, R., 2007. Brain interleukin-1 mediates chronic stress-induceddepression in mice via adrenocortical activation and hippocampal neurogenesissuppression. Mol. Psychiatry.
Grabiec, A.M., Tak, P.P., Reedquist, K.A., 2011. Function of histone deacetylaseinhibitors in inflammation. Crit. Rev. Immunol. 31, 233–263.
Grande, I., Magalhaes, P.V., Kunz, M., Vieta, E., Kapczinski, F., 2012. Mediators ofallostasis and systemic toxicity in bipolar disorder. Physiol. Behav. 106, 46–50.
Gualtieri, C.T., Johnson, L.G., 2008. Age-related cognitive decline in patients withmood disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 32, 962–967.
Guo, S., Arai, K., Stins, M.F., Chuang, D.M., Lo, E.H., 2009. Lithium upregulates vascularendothelial growth factor in brain endothelial cells and astrocytes. Stroke 40,652–655.
Hallahan, B., Newell, J., Soares, J.C., Brambilla, P., Strakowski, S.M., Fleck, D.E.,Kieseppa, T., Altshuler, L.L., Fornito, A., Malhi, G.S., McIntosh, A.M., Yurgelun-Todd, D.A., Labar, K.S., Sharma, V., MacQueen, G.M., Murray, R.M., McDonald,C., 2011. Structural magnetic resonance imaging in bipolar disorder: an inter-national collaborative mega-analysis of individual adult patient data. Biol.Psychiatry 69, 326–335.
Harman, D., 2009. Origin and evolution of the free radical theory of aging: a briefpersonal history, 1954–2009. Biogerontology 10, 773–781.
Harrison, P.J., 2002. The neuropathology of primary mood disorder. Brain 125,1428–1449.
Hartmann, N., Boehner, M., Groenen, F., Kalb, R., 2010. Telomere length of patientswith major depression is shortened but independent from therapy and severityof the disease. Depress Anxiety 27, 1111–1116.
Hashimoto, R., Hough, C., Nakazawa, T., Yamamoto, T., Chuang, D.M., 2002. Lithiumprotection against glutamate excitotoxicity in rat cerebral cortical neurons:involvement of NMDA receptor inhibition possibly by decreasing NR2B tyrosinephosphorylation. J. Neurochem. 80, 589–597.
Hayflick, L., Moorhead, P.S., 1961. The serial cultivation of human diploid cell strains.Exp. Cell Res. 25, 585–621.
Hegele, R.A., 2003. Drawing the line in progeria syndromes. Lancet 362, 416–417.Heyn, H., Moran, S., Esteller, M., 2013. Aberrant DNA methylation profiles in the
premature aging disorders Hutchinson-Gilford Progeria and Werner syndrome.Epigenetics 8, 28–33.
Higashi, Y., Sukhanov, S., Anwar, A., Shai, S.Y., Delafontaine, P., 2012. Aging,atherosclerosis, and IGF-1. J. Gerontol. A: Biol. Sci. Med. Sci. 67, 626–639.
Holzenberger, M., Dupont, J., Ducos, B., Leneuve, P., Geloen, A., Even, P.C., Cervera, P.,
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Le Bouc, Y., 2003. IGF-1 receptor regulates lifespan and resistance to oxidativestress in mice. Nature 421, 182–187.
Ikram, M.A., Vrooman, H.A., Vernooij, M.W., van der Lijn, F., Hofman, A., van derLugt, A., Niessen, W.J., Breteler, M.M., 2008. Brain tissue volumes in the generalelderly population. The Rotterdam Scan Study. Neurobiol. Aging 29, 882–890.
1148
1149
1150
1151
1152
ING ModelN
iobeha
I
J
J
K
K
K
K
K
K
K
K
K
KK
K
K
K
K
K
K
L
L
L
L
L
L
M
M
1153
1154
1155
1156
1157
1158
1159
1160
1161
1162
1163
1164
1165
1166
1167
1168
1169
1170
1171
1172
1173
1174
1175
1176
1177
1178
1179
1180
1181
1182
1183
1184
1185
1186
1187
1188
1189
1190
1191
1192
1193
1194
1195
1196
1197
1198
1199
1200
1201
1202
1203
1204
1205
1206
1207
1208
1209
1210
1211
1212
1213
1214
1215
1216
1217
1218
1219
1220
1221
1222
1223
1224
1225
1226
1227
1228
1229
1230
1231
1232
1233
1234
1235
1236
1237
1238
1239
1240
1241
1242
1243
1244
1245
1246
1247
1248
1249
1250
1251
1252
1253
1254
1255
1256
1257
1258
1259
1260
1261
1262
1263
1264
1265
1266
1267
1268
1269
1270
1271
1272
1273
1274
1275
1276
1277
1278
1279
1280
1281
1282
1283
1284
1285
1286
1287
1288
1289
1290
1291
1292
1293
1294
1295
1296
1297
1298
1299
1300
1301
1302
1303
1304
1305
1306
1307
1308
1309
1310
1311
1312
1313
1314
1315
1316
1317
1318
1319
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
to, K., Colley, T., Mercado, N., 2012. Geroprotectors as a novel therapeutic strategyfor COPD, an accelerating aging disease. Int. J. Chron. Obstruct. Pulmon. Dis. 7,641–652.
ernigan, T.L., Archibald, S.L., Fennema-Notestine, C., Gamst, A.C., Stout, J.C., Bonner,J., Hesselink, J.R., 2001. Effects of age on tissues and regions of the cerebrum andcerebellum. Neurobiol. Aging 22, 581–594.
oca, S.R., Ferreira, F.R., Guimaraes, F.S., 2007. Modulation of stress consequencesby hippocampal monoaminergic, glutamatergic and nitrergic neurotransmittersystems. Stress 10, 227–249.
anfi, Y., Naiman, S., Amir, G., Peshti, V., Zinman, G., Nahum, L., Bar-Joseph, Z.,Cohen, H.Y., 2012. The sirtuin SIRT6 regulates lifespan in male mice. Nature483, 218–221.
ao, C.Y., Hsu, Y.C., Liu, J.W., Lee, D.C., Chung, Y.F., Chiu, I.M., 2013. The mood stabi-lizer valproate activates human FGF1 gene promoter through inhibiting HDACand GSK-3 activities. J. Neurochem. 126, 4–18.
apczinski, F., Dias, V.V., Kauer-Sant’Anna, M., Brietzke, E., Vazquez, G.H., Vieta, E.,Berk, M., 2009. The potential use of biomarkers as an adjunctive tool for stagingbipolar disorder. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 33, 1366–1371.
apczinski, F., Vieta, E., Andreazza, A.C., Frey, B.N., Gomes, F.A., Tramontina, J., Kauer-Sant’anna, M., Grassi-Oliveira, R., Post, R.M., 2008. Allostatic load in bipolardisorder: implications for pathophysiology and treatment. Neurosci. Biobehav.Rev. 32, 675–692.
arten, Y.J., Olariu, A., Cameron, H.A., 2005. Stress in early life inhibits neurogenesisin adulthood. Trends Neurosci. 28, 171–172.
atan, M., Moon, Y.P., Paik, M.C., Sacco, R.L., Wright, C.B., Elkind, M.S., 2013. Infectiousburden and cognitive function: The Northern Manhattan Study. Neurology 80,1209–1215.
auer-Sant’Anna, M., Kapczinski, F., Andreazza, A.C., Bond, D.J., Lam, R.W., Young,L.T., Yatham, L.N., 2009. Brain-derived neurotrophic factor and inflammatorymarkers in patients with early- vs. late-stage bipolar disorder. Int. J. Neuropsy-chopharmacol. 12, 447–458.
awahara, T.L., Michishita, E., Adler, A.S., Damian, M., Berber, E., Lin, M., McCord, R.A.,Ongaigui, K.C., Boxer, L.D., Chang, H.Y., Chua, K.F., 2009. SIRT6 links histone H3lysine 9 deacetylation to NF-kappaB-dependent gene expression and organismallife span. Cell 136, 62–74.
elley, K.W., O’Connor, J.C., Lawson, M.A., Dantzer, R., Rodriguez-Zas, S.L., McCusker,R.H., 2013. Aging leads to prolonged duration of inflammation-induceddepression-like behavior caused by Bacillus Calmette-Guerin. Brain Behav.Immun. 32, 63–69.
enyon, C.J., 2010. The genetics of ageing. Nature 464, 504–512.essing, L.V., Andersen, P.K., 2004. Does the risk of developing dementia increase
with the number of episodes in patients with depressive disorder and in patientswith bipolar disorder. J. Neurol. Neurosurg. Psychiatry 75, 1662–1666.
ita, Y., Baba, H., Maeshima, H., Nakano, Y., Suzuki, T., Arai, H., 2009. Serum amyloidbeta protein in young and elderly depression: a pilot study. Psychogeriatrics 9,180–185.
onarski, J.Z., McIntyre, R.S., Kennedy, S.H., Rafi-Tari, S., Soczynska, J.K., Ketter, T.A.,2008. Volumetric neuroimaging investigations in mood disorders: bipolar dis-order versus major depressive disorder. Bipolar Disord. 10, 1–37.
orte, M., Carroll, P., Wolf, E., Brem, G., Thoenen, H., Bonhoeffer, T., 1995. Hip-pocampal long-term potentiation is impaired in mice lacking brain-derivedneurotrophic factor. Proc. Natl. Acad. Sci. U.S.A. 92, 8856–8860.
ucyi, A., Alsuwaidan, M.T., Liauw, S.S., McIntyre, R.S., 2010. Aerobic physical exer-cise as a possible treatment for neurocognitive dysfunction in bipolar disorder.Postgrad. Med. 122, 107–116.
ugaya, A., Sanacora, G., 2005. Beyond monoamines: glutamatergic function in mooddisorders. CNS Spectr. 10, 808–819.
uhn, H.G., Dickinson-Anson, H., Gage, F.H., 1996. Neurogenesis in the dentate gyrusof the adult rat: age-related decrease of neuronal progenitor proliferation. J.Neurosci. 16, 2027–2033.
ai, J.S., Zhao, C., Warsh, J.J., Li, P.P., 2006. Cytoprotection by lithium and valproatevaries between cell types and cellular stresses. Eur. J. Pharmacol. 539, 18–26.
evine, E.S., Crozier, R.A., Black, I.B., Plummer, M.R., 1998. Brain-derived neu-rotrophic factor modulates hippocampal synaptic transmission by increasingN-methyl-d-aspartic acid receptor activity. Proc. Natl. Acad. Sci. U.S.A. 95,10235–10239.
isy, M.E., Jarvis, K.B., DelBello, M.P., Mills, N.P., Weber, W.A., Fleck, D., Strakowski,S.M., Adler, C.M., 2011. Progressive neurostructural changes in adolescent andadult patients with bipolar disorder. Bipolar Disord. 13, 396–405.
lorens-Martin, M., Torres-Aleman, I., Trejo, J.L., 2010. Exercise modulates insulin-like growth factor 1-dependent and -independent effects on adult hippocampalneurogenesis and behaviour. Mol. Cell. Neurosci. 44, 109–117.
udlow, A.T., Witkowski, S., Marshall, M.R., Wang, J., Lima, L.C., Guth, L.M., Span-genburg, E.E., Roth, S.M., 2012. Chronic exercise modifies age-related telomeredynamics in a tissue-specific fashion. J. Gerontol. A: Biol. Sci. Med. Sci. 67,911–926.
ue, L.F., Kuo, Y.M., Roher, A.E., Brachova, L., Shen, Y., Sue, L., Beach, T., Kurth, J.H.,Rydel, R.E., Rogers, J., 1999. Soluble amyloid beta peptide concentration as apredictor of synaptic change in Alzheimer’s disease. Am. J. Pathol. 155, 853–862.
acaulay, R., Akbar, A.N., Henson, S.M., 2013. The role of the T cell in age-relatedinflammation. Age (Dordr.) 35, 563–572.
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
achado-Vieira, R., Andreazza, A.C., Viale, C.I., Zanatto, V., Cereser Jr., V., da SilvaVargas, R., Kapczinski, F., Portela, L.V., Souza, D.O., Salvador, M., Gentil, V., 2007.Oxidative stress parameters in unmedicated and treated bipolar subjects duringinitial manic episode: a possible role for lithium antioxidant effects. Neurosci.Lett. 421, 33–36.
PRESSvioral Reviews xxx (2014) xxx–xxx 11
Machado-Vieira, R., Manji, H.K., Zarate, C.A., 2009. The role of the tripartite gluta-matergic synapse in the pathophysiology and therapeutics of mood disorders.Neuroscientist 15, 525–539.
Magalhaes, P.V., Jansen, K., Pinheiro, R.T., Colpo, G.D., da Motta, L.L., Klamt, F.,da Silva, R.A., Kapczinski, F., 2012. Peripheral oxidative damage in early-stagemood disorders: a nested population-based case-control study. Int. J. Neuropsy-chopharmacol. 15, 1043–1050.
Mahon, K., Burdick, K.E., Szeszko, P.R., 2010. A role for white matter abnormalities inthe pathophysiology of bipolar disorder. Neurosci. Biobehav. Rev. 34, 533–554.
Mahon, K., Wu, J., Malhotra, A.K., Burdick, K.E., DeRosse, P., Ardekani, B.A., Szeszko,P.R., 2009. A voxel-based diffusion tensor imaging study of white matter inbipolar disorder. Neuropsychopharmacology 34, 1590–1600.
Mansur, R.B., Cha, D.S., Asevedo, E., McIntyre, R.S., Brietzke, E., 2013. Selfish brainand neuroprogression in bipolar disorder. Prog. Neuropsychopharmacol. Biol.Psychiatry 43, 66–71.
Martinez-Aran, A., Vieta, E., Colom, F., Reinares, M., Benabarre, A., Torrent, C.,Goikolea, J.M., Corbella, B., Sanchez-Moreno, J., Salamero, M., 2002. Neu-ropsychological performance in depressed and euthymic bipolar patients.Neuropsychobiology 46 (Suppl. 1), 16–21.
Martinez-Aran, A., Vieta, E., Colom, F., Torrent, C., Reinares, M., Goikolea, J.M., Ben-abarre, A., Comes, M., Sanchez-Moreno, J., 2005. Do cognitive complaints ineuthymic bipolar patients reflect objective cognitive impairment? Psychother.Psychosom. 74, 295–302.
Martinez-Aran, A., Vieta, E., Reinares, M., Colom, F., Torrent, C., Sanchez-Moreno, J.,Benabarre, A., Goikolea, J.M., Comes, M., Salamero, M., 2004. Cognitive functionacross manic or hypomanic, depressed, and euthymic states in bipolar disorder.Am. J. Psychiatry 161, 262–270.
Martinez-Aran, A., Vieta, E., Torrent, C., Sanchez-Moreno, J., Goikolea, J.M., Salamero,M., Malhi, G.S., Gonzalez-Pinto, A., Daban, C., Alvarez-Grandi, S., Fountoulakis, K.,Kaprinis, G., Tabares-Seisdedos, R., Ayuso-Mateos, J.L., 2007. Functional outcomein bipolar disorder: the role of clinical and cognitive factors. Bipolar Disord. 9,103–113.
Martinsson, L., Wei, Y., Xu, D., Melas, P.A., Mathe, A.A., Schalling, M., Lavebratt, C.,Backlund, L., 2013. Long-term lithium treatment in bipolar disorder is associatedwith longer leukocyte telomeres. Translational psychiatry 3, e261.
McIntyre, R.S., Konarski, J.Z., Misener, V.L., Kennedy, S.H., 2005. Bipolar disorder anddiabetes mellitus: epidemiology, etiology, and treatment implications. Ann. Clin.Psychiatry 17, 83–93.
McIntyre, R.S., Konarski, J.Z., Soczynska, J.K., Wilkins, K., Panjwani, G., Bouffard, B.,Bottas, A., Kennedy, S.H., 2006. Medical comorbidity in bipolar disorder: impli-cations for functional outcomes and health service utilization. Psychiatr. Serv.57, 1140–1144.
Miller, C.L., Llenos, I.C., Cwik, M., Walkup, J., Weis, S., 2008. Alterations in kynurenineprecursor and product levels in schizophrenia and bipolar disorder. Neurochem.Int. 52, 1297–1303.
Miller, C.L., Llenos, I.C., Dulay, J.R., Weis, S., 2006. Upregulation of the initiating stepof the kynurenine pathway in postmortem anterior cingulate cortex from indi-viduals with schizophrenia and bipolar disorder. Brain Res. 1073–1074, 25–37.
Milne, J.C., Lambert, P.D., Schenk, S., Carney, D.P., Smith, J.J., Gagne, D.J., Jin, L., Boss,O., Perni, R.B., Vu, C.B., Bemis, J.E., Xie, R., Disch, J.S., Ng, P.Y., Nunes, J.J., Lynch,A.V., Yang, H., Galonek, H., Israelian, K., Choy, W., Iffland, A., Lavu, S., Medvedik,O., Sinclair, D.A., Olefsky, J.M., Jirousek, M.R., Elliott, P.J., Westphal, C.H., 2007.Small molecule activators of SIRT1 as therapeutics for the treatment of type 2diabetes. Nature 450, 712–716.
Mitschelen, M., Yan, H., Farley, J.A., Warrington, J.P., Han, S., Herenu, C.B., Csiszar,A., Ungvari, Z., Bailey-Downs, L.C., Bass, C.E., Sonntag, W.E., 2011. Long-termdeficiency of circulating and hippocampal insulin-like growth factor I inducesdepressive behavior in adult mice: a potential model of geriatric depression.Neuroscience 185, 50–60.
Modabbernia, A., Taslimi, S., Brietzke, E., Ashrafi, M., 2013. Cytokine alterations inbipolar disorder: a meta-analysis of 30 studies. Biol. Psychiatry 74, 15–25.
Moore, G.J., Bebchuk, J.M., Hasanat, K., Chen, G., Seraji-Bozorgzad, N., Wilds, I.B.,Faulk, M.W., Koch, S., Glitz, D.A., Jolkovsky, L., Manji, H.K., 2000. Lithiumincreases N-acetyl-aspartate in the human brain: in vivo evidence in supportof bcl-2’s neurotrophic effects? Biol. Psychiatry 48, 1–8.
Naydenov, A.V., MacDonald, M.L., Ongur, D., Konradi, C., 2007. Differences in lym-phocyte electron transport gene expression levels between subjects with bipolardisorder and normal controls in response to glucose deprivation stress. Arch.Gen. Psychiatry 64, 555–564.
Ng, F., Dodd, S., Berk, M., 2007. The effects of physical activity in the acute treatmentof bipolar disorder: a pilot study. J. Affect. Disord. 101, 259–262.
O’Neill, P., 1997. Aging homeostasis. Rev. Clin. Gerontol. 7, 199–211.Olsson, J., Wikby, A., Johansson, B., Lofgren, S., Nilsson, B.O., Ferguson, F.G., 2000.
Age-related change in peripheral blood T-lymphocyte subpopulations andcytomegalovirus infection in the very old: the Swedish longitudinal OCTOimmune study. Mech. Ageing Dev. 121, 187–201.
Osby, U., Brandt, L., Correia, N., Ekbom, A., Sparen, P., 2001. Excess mortality in bipolarand unipolar disorder in Sweden. Archiv. Gen. Psychiatry 58, 844–850.
Osorio, R.S., Gumb, T., Pomara, N., 2013. Soluble amyloid-beta levels and late-lifedepression. Curr Pharm Des.
Ouyang, Q., Wagner, W.M., Wikby, A., Walter, S., Aubert, G., Dodi, A.I., Travers, P.,
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Pawelec, G., 2003. Large numbers of dysfunctional CD8+ T lymphocytes bearingreceptors for a single dominant CMV epitope in the very old. J. Clin. Immunol.23, 247–257.
Padmos, R.C., Bekris, L., Knijff, E.M., Tiemeier, H., Kupka, R.W., Cohen, D.,Nolen, W.A., Lernmark, A., Drexhage, H.A., 2004. A high prevalence of
1320
1321
1322
1323
1324
ING ModelN
1 iobeha
P
P
P
P
P
P
P
P
Q
RR
R
R
R
R
R
R
RR
R
S
S
S
S
S
S
S
S
1325
1326
1327
1328
1329
1330
1331
1332
1333
1334
1335
1336
1337
1338
1339
1340
1341
1342
1343
1344
1345
1346
1347
1348
1349
1350
1351
1352
1353
1354
1355
1356
1357
1358
1359
1360
1361
1362
1363
1364
1365
1366
1367
1368
1369
1370
1371
1372
1373
1374
1375
1376
1377
1378
1379
1380
1381
1382
1383
1384
1385
1386
1387
1388
1389
1390
1391
1392
1393
1394
1395
1396
1397
1398
1399
1400
1401
1402
1403
1404
1405
1406
1407
1408
1409
1410
1411
1412
1413
1414
1415
1416
1417
1418
1419
1420
1421
1422
1423
1424
1425
1426
1427
1428
1429
1430
1431
1432
1433
1434
1435
1436
1437
1438
1439
1440
1441
1442
1443
1444
1445
1446
1447
1448
1449
1450
1451
1452
1453
1454
1455
1456
1457
1458
1459
1460
1461
1462
1463
1464
1465
1466
1467
1468
1469
1470
1471
1472
1473
1474
1475
1476
1477
1478
1479
1480
1481
1482
1483
1484
1485
1486
1487
1488
1489
1490
1491
ARTICLEBR 1894 1–13
2 L.B. Rizzo et al. / Neuroscience and B
organ-specific autoimmunity in patients with bipolar disorder. Biol. Psychiatry56, 476–482.
apanastasiou, E., Gaughran, F., Smith, S., 2011. Schizophrenia as segmental progeria.J. R. Soc. Med. 104, 475–484.
ark, S.E., Lawson, M., Dantzer, R., Kelley, K.W., McCusker, R.H., 2011. Insulin-likegrowth factor-I peptides act centrally to decrease depression-like behavior ofmice treated intraperitoneally with lipopolysaccharide. J. Neuroinflamm. 8, 179.
awelec, G., Derhovanessian, E., 2011. Role of CMV in immune senescence. VirusRes. 157, 175–179.
enna, C., Perrelli, M.G., Pagliaro, P., 2013. Mitochondrial pathways, permeabilitytransition pore, and redox signaling in cardioprotection: therapeutic implica-tions. Antioxid. Redox Signal. 18, 556–599.
ereira, A.C., McQuillin, A., Puri, V., Anjorin, A., Bass, N., Kandaswamy, R., Lawrence,J., Curtis, D., Sklar, P., Purcell, S.M., Gurling, H.M., 2011. Genetic association andsequencing of the insulin-like growth factor 1 gene in bipolar affective disorder.Am. J. Med. Genet. B: Neuropsychiatr. Genet. 156, 177–187.
erovic, M., Tesic, V., Mladenovic Djordjevic, A., Smiljanic, K., Loncarevic-Vasiljkovic,N., Ruzdijic, S., Kanazir, S., 2012. BDNF transcripts, proBDNF and proNGF, in thecortex and hippocampus throughout the life span of the rat. Age (Dordr).
iccinni, A., Origlia, N., Veltri, A., Vizzaccaro, C., Marazziti, D., Catena-Dell’osso, M.,Conversano, C., Moroni, I., Domenici, L., Dell’osso, L., 2012. Plasma beta-amyloidpeptides levels: a pilot study in bipolar depressed patients. J. Affect. Disord. 138,160–164.
orton, B., Delisi, L.E., Bertisch, H.C., Ji, F., Gordon, D., Li, P., Benedict, M.M., Greenberg,W.M., Kao, H.T., 2008. Telomerase levels in schizophrenia: a preliminary study.Schizophr. Res. 106, 242–247.
iu, W.Q., Sun, X., Selkoe, D.J., Mwamburi, D.M., Huang, T., Bhadela, R., Bergethon, P.,Scott, T.M., Summergrad, P., Wang, L., Rosenberg, I., Folstein, M., 2007. Depres-sion is associated with low plasma Abeta42 independently of cardiovasculardisease in the homebound elderly. Int. J. Geriatr. Psychiatry 22, 536–542.
ajkowska, G., 2002. Cell pathology in bipolar disorder. Bipolar Disord. 4, 105–116.az, N., Rodrigue, K.M., 2006. Differential aging of the brain: patterns, cognitive
correlates and modifiers. Neurosci. Biobehav. Rev. 30, 730–748.ege, S., Hodgkinson, S.J., 2013. Immune dysregulation and autoimmunity in bipo-
lar disorder: synthesis of the evidence and its clinical application. Aust. N. Z. J.Psychiatry.
izzo, L.B., Do Prado, C.H., Grassi-Oliveira, R., Wieck, A., Correa, B.L., Teix-eira, A.L., Bauer, M.E., 2013. Immunosenescence is associated with humancytomegalovirus and shortened telomeres in type I bipolar disorder. BipolarDisord..
obinson, L.J., Thompson, J.M., Gallagher, P., Goswami, U., Young, A.H., Ferrier, I.N.,Moore, P.B., 2006. A meta-analysis of cognitive deficits in euthymic patients withbipolar disorder. J. Affect. Disord. 93, 105–115.
osa, A.R., Franco, C., Martinez-Aran, A., Sanchez-Moreno, J., Reinares, M., Salamero,M., Arango, C., Ayuso-Mateos, J.L., Kapczinski, F., Vieta, E., 2008. Functionalimpairment in patients with remitted bipolar disorder. Psychother. Psychosom.77, 390–392.
osa, A.R., Gonzalez-Ortega, I., Gonzalez-Pinto, A., Echeburua, E., Comes, M.,Martinez-Aran, A., Ugarte, A., Fernandez, M., Vieta, E., 2012. One-year psychoso-cial functioning in patients in the early vs. late stage of bipolar disorder. ActaPsychiatr. Scand. 125, 335–341.
osa, A.R., Reinares, M., Amann, B., Popovic, D., Franco, C., Comes, M., Torrent, C.,Bonnin, C.M., Sole, B., Valenti, M., Salamero, M., Kapczinski, F., Vieta, E., 2011.Six-month functional outcome of a bipolar disorder cohort in the context of aspecialized-care program. Bipolar Disord. 13, 679–686.
ose, M.R., 1991. Evolutionary Biology of Aging. Oxford University Press, New York.osenberg, G., 2007. The mechanisms of action of valproate in neuropsychiatric
disorders: can we see the forest for the trees? Cell Mol Life Sci 64, 2090–2103.ybakowski, J.K., Wykretowicz, A., Heymann-Szlachcinska, A., Wysocki, H., 2006.
Impairment of endothelial function in unipolar and bipolar depression. Biol.Psychiatry 60, 889–891.
amame, C., Martino, D.J., Strejilevich, S.A., 2013. A quantitative review of neurocog-nition in euthymic late-life bipolar disorder. Bipolar Disord. 15, 633–644.
avas, H.A., Herken, H., Yurekli, M., Uz, E., Tutkun, H., Zoroglu, S.S., Ozen, M.E., Cengiz,B., Akyol, O., 2002. Possible role of nitric oxide and adrenomedullin in bipolaraffective disorder. Neuropsychobiology 45, 57–61.
cott, J., Leboyer, M., Hickie, I., Berk, M., Kapczinski, F., Frank, E., Kupfer, D., McGorry,P., 2013. Clinical staging in psychiatry: a cross-cutting model of diagnosis withheuristic and practical value. Br. J. Psychiatry 202, 243–245.
elek, S., Savas, H.A., Gergerlioglu, H.S., Bulbul, F., Uz, E., Yumru, M., 2008. The courseof nitric oxide and superoxide dismutase during treatment of bipolar depressiveepisode. J. Affect. Disord. 107, 89–94.
esti, G., Sciacqua, A., Cardellini, M., Marini, M.A., Maio, R., Vatrano, M., Succurro, E.,Lauro, R., Federici, M., Perticone, F., 2005. Plasma concentration of IGF-I is inde-pendently associated with insulin sensitivity in subjects with different degreesof glucose tolerance. Diabetes Care 28, 120–125.
imon, N.M., Smoller, J.W., McNamara, K.L., Maser, R.S., Zalta, A.K., Pollack, M.H.,Nierenberg, A.A., Fava, M., Wong, K.K., 2006. Telomere shortening and mooddisorders: preliminary support for a chronic stress model of accelerated aging.Biol. Psychiatry 60, 432–435.
nyder, E.M., Nong, Y., Almeida, C.G., Paul, S., Moran, T., Choi, E.Y., Nairn, A.C., Salter,
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
M.W., Lombroso, P.J., Gouras, G.K., Greengard, P., 2005. Regulation of NMDAreceptor trafficking by amyloid-beta. Nat. Neurosci. 8, 1051–1058.
odhi, S.K., Linder, J., Chenard, C.A., Miller del, D., Haynes, W.G., Fiedorowicz, J.G.,2012. Evidence for accelerated vascular aging in bipolar disorder. J. Psychosom.Res. 73, 175–179.
PRESSvioral Reviews xxx (2014) xxx–xxx
Soreca, I., Fagiolini, A., Frank, E., Houck, P.R., Thompson, W.K., Kupfer, D.J., 2008.Relationship of general medical burden, duration of illness and age in patientswith bipolar I disorder. J. Psychiatr. Res. 42, 956–961.
Squassina, A., Costa, M., Congiu, D., Manchia, M., Angius, A., Deiana, V., Ardau, R.,Chillotti, C., Severino, G., Calza, S., Del Zompo, M., 2013. Insulin-like growth fac-tor 1 (IGF-1) expression is up-regulated in lymphoblastoid cell lines of lithiumresponsive bipolar disorder patients. Pharmacol. Res. 73, 1–7.
Stadler, K., 2012. Oxidative stress in diabetes. Adv. Exp. Med. Biol. 771, 272–287.Stambolic, V., Ruel, L., Woodgett, J.R., 1996. Lithium inhibits glycogen synthase
kinase-3 activity and mimics wingless signalling in intact cells. Curr. Biol. 6,1664–1668.
Steckert, A.V., Valvassori, S.S., Moretti, M., Dal-Pizzol, F., Quevedo, J., 2010. Role ofoxidative stress in the pathophysiology of bipolar disorder. Neurochem. Res. 35,1295–1301.
Strakowski, S.M., DelBello, M.P., Zimmerman, M.E., Getz, G.E., Mills, N.P., Ret, J., Shear,P., Adler, C.M., 2002. Ventricular and periventricular structural volumes in first-versus multiple-episode bipolar disorder. Am. J. Psychiatry 159, 1841–1847.
Sullivan, P.F., Daly, M.J., O’Donovan, M., 2012. Genetic architectures of psychi-atric disorders: the emerging picture and its implications. Nat. Rev. Genet. 13,537–551.
Sun, X., Mwamburi, D.M., Bungay, K., Prasad, J., Yee, J., Lin, Y.M., Liu, T.C., Summer-grad, P., Folstein, M., Qiu, W.Q., 2007. Depression, antidepressants, and plasmaamyloid beta (Beta) peptides in those elderly who do not have cardiovasculardisease. Biol. Psychiatry 62, 1413–1417.
Swann, A.C., Bowden, C.L., Calabrese, J.R., Dilsaver, S.C., Morris, D.D., 1999. Differen-tial effect of number of previous episodes of affective disorder on response tolithium or divalproex in acute mania. Am. J. Psychiatry 156, 1264–1266.
Swardfager, W., Black, S.E., 2013. Dementia: a link between microbial infection andcognition? Nature reviews. Neurology 9, 301–302.
Swardfager, W., Herrmann, N., Marzolini, S., Saleem, M., Kiss, A., Shammi, P., Oh,P.I., Lanctot, K.L., 2010a. Cardiopulmonary fitness is associated with cognitiveperformance in patients with coronary artery disease. J. Am. Geriatr. Soc. 58,1519–1525.
Swardfager, W., Herrmann, N., Marzolini, S., Saleem, M., Shammi, P., Oh, P.I., Albert,P.R., Daigle, M., Kiss, A., Lanctot, K.L., 2011. Brain derived neurotrophic factor,cardiopulmonary fitness and cognition in patients with coronary artery disease.Brain Behav. Immun. 25, 1264–1271.
Swardfager, W., Lanctot, K., Rothenburg, L., Wong, A., Cappell, J., Herrmann, N.,2010b. A meta-analysis of cytokines in Alzheimer’s disease. Biol. Psychiatry 68,930–941.
Tabata, T., Kawakatsu, H., Maidji, E., Sakai, T., Sakai, K., Fang-Hoover, J., Aiba, M.,Sheppard, D., Pereira, L., 2008. Induction of an epithelial integrin alphavbeta6 inhuman cytomegalovirus-infected endothelial cells leads to activation of trans-forming growth factor-beta1 and increased collagen production. Am. J. Pathol.172, 1127–1140.
Teixeira, M.T., Arneric, M., Sperisen, P., Lingner, J., 2004. Telomere length homeosta-sis is achieved via a switch between telomerase-extendible and -nonextendiblestates. Cell 117, 323–335.
Thal, D.R., Del Tredici, K., Braak, H., 2004. Neurodegeneration in normal brain agingand disease. Sci. Aging Knowledge Environ. 2004, pe26.
Tong, L., Thornton, P.L., Balazs, R., Cotman, C.W., 2001. Beta-amyloid-(1–42) impairsactivity-dependent cAMP-response element-binding protein signaling in neu-rons at concentrations in which cell survival is not compromised. J. Biol. Chem.276, 17301–17306.
Torrao, A.S., Cafe-Mendes, C.C., Real, C.C., Hernandes, M.S., Ferreira, A.F., Santos, T.O.,Chaves-Kirsten, G.P., Mazucanti, C.H., Ferro, E.S., Scavone, C., Britto, L.R., 2012.Different approaches, one target: understanding cellular mechanisms of Parkin-son’s and Alzheimer’s diseases. Rev. Bras. Psiquiatr. 34 (Suppl. 2), S194–S205.
Torrent, C., Martinez-Aran, A., Daban, C., Sanchez-Moreno, J., Comes, M., Goikolea,J.M., Salamero, M., Vieta, E., 2006. Cognitive impairment in bipolar II disorder.Br. J. Psychiatry 189, 254–259.
Torres, I.J., Boudreau, V.G., Yatham, L.N., 2007. Neuropsychological functioning ineuthymic bipolar disorder: a meta-analysis. Acta Psychiatr. Scand. Suppl., 17–26.
Ustun, T.B., 1999. The global burden of mental disorders. Am. J. Public Health 89,1315–1318.
van der Lijn, F., den Heijer, T., Breteler, M.M., Niessen, W.J., 2008. Hippocampussegmentation in MR images using atlas registration, voxel classification, andgraph cuts. Neuroimage 43, 708–720.
van Praag, H., Christie, B.R., Sejnowski, T.J., Gage, F.H., 1999. Running enhances neu-rogenesis, learning, and long-term potentiation in mice. Proc. Natl. Acad. Sci.U.S.A. 96, 13427–13431.
Vaziri, H., Dragowska, W., Allsopp, R.C., Thomas, T.E., Harley, C.B., Lansdorp, P.M.,1994. Evidence for a mitotic clock in human hematopoietic stem cells: loss oftelomeric DNA with age. Proc. Natl. Acad. Sci. U.S.A. 91, 9857–9860.
Vernooij, M.W., Smits, M., 2012. Structural neuroimaging in aging and Alzheimer’sdisease. Neuroimaging Clin. N. Am. 22, 33–55, vii–viii.
von Zglinicki, T., 2000. Role of oxidative stress in telomere length regulation andreplicative senescence. Ann. N. Y. Acad. Sci. 908, 99–110.
Vostrikov, V.M., Uranova, N.A., Orlovskaya, D.D., 2007. Deficit of perineuronal oligo-dendrocytes in the prefrontal cortex in schizophrenia and mood disorders.Schizophr. Res. 94, 273–280.
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Wang, L., Yang, H.J., Xia, Y.Y., Feng, Z.W., 2010. Insulin-like growth factor 1 pro-tects human neuroblastoma cells SH-EP1 against MPP+-induced apoptosis byAKT/GSK-3beta/JNK signaling. Apoptosis 15, 1470–1479.
Weng, N.P., Akbar, A.N., Goronzy, J., 2009. CD28(−) T cells: their role in the age-associated decline of immune function. Trends Immunol. 30, 306–312.
1492
1493
1494
1495
1496
ING ModelN
iobeha
W
W
W
W
W
W
W
W
1497
1498
1499
1500
1501
1502
1503
1504
1505
1506
1507
1508
1509
1510
1511
1512
1513
1514
1515
1516
1517
1518
1519
1520
1521
1522
1523
1524
1525
1526
1527
1528
1529
1530
1531
1532
1533
1534
1535
1536
1537
1538
1539
1540
1541
1542
1543
1544
1545
1546
1547
1548
1549
1550
1551
1552
ARTICLEBR 1894 1–13
L.B. Rizzo et al. / Neuroscience and B
erner, C., Hanhoun, M., Widmann, T., Kazakov, A., Semenov, A., Poss, J., Bauersachs,J., Thum, T., Pfreundschuh, M., Muller, P., Haendeler, J., Bohm, M., Laufs, U., 2008.Effects of physical exercise on myocardial telomere-regulating proteins, survivalpathways, and apoptosis. J. Am. Coll. Cardiol. 52, 470–482.
ieck, A., Grassi-Oliveira, R., do Prado, C.H., Rizzo, L.B., de Oliveira, A.S.,Kommers-Molina, J., Viola, T.W., Teixeira, A.L., Bauer, M.E., 2013. Differentialneuroendocrine and immune responses to acute psychosocial stress in womenwith type 1 bipolar disorder. Brain Behav. Immun.
ikby, A., Johansson, B., Olsson, J., Lofgren, S., Nilsson, B.O., Ferguson, F., 2002. Expan-sions of peripheral blood CD8 T-lymphocyte subpopulations and an associationwith cytomegalovirus seropositivity in the elderly: the Swedish NONA immunestudy. Exp. Gerontol. 37, 445–453.
ikgren, M., Maripuu, M., Karlsson, T., Nordfjall, K., Bergdahl, J., Hultdin, J., Del-Favero, J., Roos, G., Nilsson, L.G., Adolfsson, R., Norrback, K.F., 2012. Shorttelomeres in depression and the general population are associated with ahypocortisolemic state. Biol. Psychiatry 71, 294–300.
olf, S.A., Melnik, A., Kempermann, G., 2011. Physical exercise increases adult neu-rogenesis and telomerase activity, and improves behavioral deficits in a mousemodel of schizophrenia. Brain Behav. Immun. 25, 971–980.
olkowitz, O.M., Epel, E.S., Reus, V.I., Mellon, S.H., 2010. Depression gets oldfast: do stress and depression accelerate cell aging? Depress. Anxiety 27,327–338.
olkowitz, O.M., Mellon, S.H., Epel, E.S., Lin, J., Dhabhar, F.S., Su, Y., Reus, V.I.,Rosser, R., Burke, H.M., Kupferman, E., Compagnone, M., Nelson, J.C., Blackburn,E.H., 2011. Leukocyte telomere length in major depression: correlations withchronicity, inflammation and oxidative stress—preliminary findings. PLoS ONE
Please cite this article in press as: Rizzo, L.B., et al., The theory of bipclinical care and research. Neurosci. Biobehav. Rev. (2014), http://dx.d
6, e17837.olkowitz, O.M., Mellon, S.H., Epel, E.S., Lin, J., Reus, V.I., Rosser, R., Burke, H.,
Compagnone, M., Nelson, J.C., Dhabhar, F.S., Blackburn, E.H., 2012. Resting leuko-cyte telomerase activity is elevated in major depression and predicts treatmentresponse. Mol. Psychiatry 17, 164–172.
PRESSvioral Reviews xxx (2014) xxx–xxx 13
Wonodi, I., Schwarcz, R., 2010. Cortical kynurenine pathway metabolism: a noveltarget for cognitive enhancement in Schizophrenia. Schizophr. Bull. 36, 211–218.
Worman, H.J., Bonne, G., 2007. Laminopathies: a wide spectrum of human diseases.Exp. Cell Res. 313, 2121–2133.
Xiang, G.D., Pu, J., Sun, H., Zhao, L., Yue, L., Hou, J., 2009. Regular aerobic exer-cise training improves endothelium-dependent arterial dilation in patients withsubclinical hypothyroidism. Eur. J. Endocrinol. 161, 755–761.
Yasuda, S., Liang, M.H., Marinova, Z., Yahyavi, A., Chuang, D.M., 2009. The moodstabilizers lithium and valproate selectively activate the promoter IV of brain-derived neurotrophic factor in neurons. Mol. Psychiatry 14, 51–59.
Yildiz-Yesiloglu, A., Ankerst, D.P., 2006. Neurochemical alterations of the brain inbipolar disorder and their implications for pathophysiology: a systematic reviewof the in vivo proton magnetic resonance spectroscopy findings. Prog. Neuropsy-chopharmacol. Biol. Psychiatry 30, 969–995.
Yildiz, O., 2007. Vascular smooth muscle and endothelial functions in aging. Ann. N.Y. Acad. Sci. 1100, 353–360.
Yu, C.E., Oshima, J., Fu, Y.H., Wijsman, E.M., Hisama, F., Alisch, R., Matthews, S.,Nakura, J., Miki, T., Ouais, S., Martin, G.M., Mulligan, J., Schellenberg, G.D., 1996.Positional cloning of the Werner’s syndrome gene. Science 272, 258–262.
Zhang, D., Cheng, L., Craig, D.W., Redman, M., Liu, C., 2010. Cerebellar telomere lengthand psychiatric disorders. Behav. Genet. 40, 250–254.
Zhang, Y.W., Thompson, R., Zhang, H., Xu, H., 2011. APP processing in Alzheimer’sdisease. Mol. Brain 4, 3.
Zhang, Z., Zhang, Z.Y., Fauser, U., Schluesener, H.J., 2008. Valproic acid attenu-ates inflammation in experimental autoimmune neuritis. Cell Mol. Life Sci. 65,4055–4065.
olar disorder as an illness of accelerated aging: Implications foroi.org/10.1016/j.neubiorev.2014.02.004
Zhang, Z., Zhang, Z.Y., Wu, Y., Schluesener, H.J., 2012. Valproic acid amelioratesinflammation in experimental autoimmune encephalomyelitis rats. Neuro-science 221, 140–150.
Zipursky, R.B., Reilly, T.J., Murray, R.M., 2012. The myth of schizophrenia as a pro-gressive brain disease. Schizophr. Bull..
1553
1554
1555
1556
1557
Related Documents