The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire Martin Roland National Primary Care Research and Development Centre, University of Manchester, Williamson Building, Oxford Road, Manchester M13 6PL, United Kingdom. Tel +44 161 275 7659. Fax +44 161 275 7600. [email protected] Jeremy Fairbank Nuffield Orthopaedic Centre, Oxford OX3 7LD, United Kingdom Tel. +44 1865 741155. Fax +44 1865 744455. [email protected] Introduction Condition specific health status measures are commonly used as outcome measures in clinical trials, and to assess patient progress in routine clinical practice. The expert panel which met to discuss the special issue of Spine recommended that, where possible, a condition specific measure for back pain should be chosen from two widely used measures, the Roland-Morris Disability Questionnaire 106 (RDQ) or the Oswestry Disability Index (ODI) 30 . These two measures have been used in a wide - 1 -

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
The Roland-Morris Disability Questionnaire and the Oswestry Disability
Questionnaire
Martin RolandNational Primary Care Research and Development Centre, University of
Manchester, Williamson Building, Oxford Road, Manchester M13 6PL, United
Kingdom. Tel +44 161 275 7659. Fax +44 161 275 7600.
Jeremy FairbankNuffield Orthopaedic Centre, Oxford OX3 7LD, United Kingdom
Tel. +44 1865 741155. Fax +44 1865 744455.
Introduction
Condition specific health status measures are commonly used as outcome
measures in clinical trials, and to assess patient progress in routine clinical
practice. The expert panel which met to discuss the special issue of Spine
recommended that, where possible, a condition specific measure for back
pain should be chosen from two widely used measures, the Roland-Morris
Disability Questionnaire106 (RDQ) or the Oswestry Disability Index (ODI)30.
These two measures have been used in a wide variety of situations over
many years, and each is available in a number of languages.
This paper describes these two instruments along with evidence of their
validity and reliability, and some comparative results using the two
questionnaires. The instruments themselves are included in the appendices.
When used in the forms reproduced in the appendices, no permission is
required from the authors or from Spine. Other back pain specific health
status measures are described by Kopec elsewhere in this edition of Spine.
- 1 -
Oswestry and Roland-Morris
The Roland-Morris Disability Questionnaire (RDQ)
Development of the Roland Morris Disability Questionnaire
The Roland-Morris Disability Questionnaire (RDQ) 106 is a health status
measure designed to be completed by patients to assess physical disability
due to low back pain. It was designed for use in research, e.g. as an outcome
measure for clinical trials, but has also been found useful for monitoring
patients in clinical practice. It was originally designed for use in primary care
in the UK, but has been used in a variety of settings.
The RDQ was derived from the Sickness Impact Profile (SIP) 3, which is a
136 item health status measure covering all aspects of physical and mental
function. Twenty four items were selected from the SIP by the original authors
because they related specifically to physical functions likely to be affected by
low back pain. Each item was qualified with the phrase ‘because of my back
pain’ in order to distinguish back pain disability from disability due to other
causes – something which patients are in general able to do without difficulty
100
Patients completing the RDQ are asked to tick a statement if it applies to
them that day. This approach was chosen to make it suitable for following
short term changes in back pain, e.g. the relatively rapid resolution of
symptoms of most patients seen in primary care, or short terms changes in
response to treatment. The RDQ score is calculated by adding up the number
of items checked. Items are not weighted. The scores therefore ranges from
0 (no disability) to 24 (maximum disability). Although designed for paper
administration, the RDQ has also been satisfactorily used on computer and
by telephone.
The original RDQ also contains a six point pain rating scale in the form of a
pain thermometer. However, we now recommend that the pain scale of the
- 2 -
SF-36 should be used in preference, as described in the article on pain
measurement by von Korff elsewhere in this volume.
The RDQ is short, simple to complete, and readily understood by patients..
Stratford et al (1994)121 found fewer incomplete or ambiguous responses to
the RDQ than to the Oswestry questionnaire. These characteristics, along
with evidence of its scientific validity, have led to its widespread use: it is now
available in twelve languages (see below). The questionnaire is reproduced in
Appendix 1. There are no restrictions on its use: it may be used without
permission from either the authors or from Spine.
Modifications and translations of the RDQ
Translations of the RDQ are available in French, German, Dutch, Flemish,
Romanian, Spanish, Italian, Czech, Swedish, Portuguese and Polish.
Available translations may be downloaded from (enter Spine website). The
file on this website also contains available details of how the translations were
done so that users can judge the likely validity of the translation (reference
Beaton’s article on translating instruments in this volume of Spine). These
translations of the RDQ may also be used without permission from the journal
Spine, or permission from the authors. If other translations are made, they
may be sent to MR with details of how the translation was done, in order that
they can be included on the Spine website.
A number of researchers have proposed modifications to the RDQ. The
simplest modification to the wording of the questionnaire has been to change
the terminal phrase of each statement from ‘because of my back’ to ‘because
of my back or leg problem 98. This makes the questionnaire more suitable for
use in a population of patients with sciatica, and is an acceptable
modification.
Other authors have proposed modifications to individual items. Stratford and
Binkley (1997)118 suggested that a number of items were redundant, and
that the questionnaire could be improved by being reduced to 18 items.
- 3 -
Oswestry and Roland-Morris
Patrick et al (1995)98 removed five potentially redundant items, and
suggested that responsiveness could be increased by adding four additional
items relating to sexual function, daily work, expressions of concern to others,
and the need to rub or hold areas that hurt. On the whole these modifications
seem to provide only modest improvement on the original version, and an
international group of experts 23 suggested use of the original version since it
has been widely used in many countries.
Underwood et al (1999)144 suggested a modification which asked, for each
item of the RDQ, how many days of the previous month they had been
affected. Although this version has not been validated, it attempts to
incorporate elements of the amount of time that people are affected by their
back pain, which often fluctuates 146 However, it did not perform as well as a
modification of von Korff’s own questionnaire 144.
Properties of RDQ scores
In the original sample used for development and validation of the scale,
median scores of patients presenting with back pain in primary care were 11
on presentation, 8 one week later, and 4 one month later 105. RDQ scores
reported in a wide variety of settings are shown in Table 3. In general RDQ
scores have little or no relationship to the age or sex of the respondents.
Face and content validity of the RDQ
The RDQ focuses on a limited range of physical functions which include
walking, bending over, sitting, lying, dressing, sleeping, self care and daily
activities (see Appendix 1). These were chosen as functions which would be
relevant to all patients with back pain. The scoring system does not therefore
permit or require a ‘non-applicable’ response. The statements in the RDQ
focus almost exclusively on physical function, with only one question on
mood. Some aspects of physical function are not explicitly included, for
example lifting and twisting or turning.
- 4 -
The limited range of the RDQ is both a strength and weakness in terms of its
content validity. The questionnaire covers only a limited range of the
problems which a patient with back pain may face, and in particular does not
address psychological or social problems. These are undoubtedly of
importance, and in situations where their measurement is important, the RDQ
should be combined with specific measures of these functions. However, the
restricted nature of the domains covered by the RDQ is also a strength in that
this makes the scores easy to understand and interpret.
Construct validity of the RDQ
In assessing the construct validity of a health status measure, it is
conventional to compare scores of a questionnaire with those of other
established measures. As would be expected with a measure of self reported
physical disability, RDQ scores correlate well with other measures of physical
function, including the physical subscales of SF-36, the Sickness Impact
Profile 21,58,98, the Quebec Back Scale 66, and the Oswestry questionnaire
121,79. Relatively high correlations are also found between RDQ scores and
pain ratings 6
The RDQ does not attempt to measure psychological distress associated with
back pain, and thus correlates less well with measures of psychological
disability, for example the psychosocial scales of the Sickness Impact Profile
58. In common with other self reported disability measures, it shows only
modest correlation with direct measures of physical function 21,109.
Internal consistency of the RDQ
The RDQ has good psychometric properties as evidenced by internal
consistency and responsiveness. Crohnbach’s alpha for the scale has been
estimated as 0.93 49 0.90 64, 0.84 57 The same statistic for modified
versions of the RDQ include 0.91 118 and 0.90 98. These are high but within
the range of 0.7 to 0.9 recommended by Nunnally (1978) 97.
- 5 -
Oswestry and Roland-Morris
Reproducibility of the RDQ
A number of attempts have been made to assess the reproducibility of the
RDQ by testing and re-testing some time after the initial assessment. While
generally regarded as an important element of the validity of a questionnaire,
the concept of test re-test reliability is somewhat doubtful for an instrument
which has been designed to pick up short term changes in a condition which
is itself notoriously changeable.
It is therefore not surprising that when the test re-test intervals are short
(e.g.), that correlations between two sets of scores are higher than when the
test retest interval is long. However, interpretation of these may be difficult if
the interval is so short that patients can remember their previous responses.
Quoted test-re-test correlations include 0.91 (same day106), 0.88 (1 week,
59), 0.83 (3 weeks21). In patients with chronic back pain, a correlation of 0.72
were reported for scores taken 39 days apart 58.
Responsiveness of the RDQ
A number of methods can be used to assess the responsiveness of health
status measures, in order to compare different measures in terms of their
ability to detect changes over time.
The RDQ compares well with other commonly used disability scales for back
pain 4. It is at least as responsive in patients with back pain as its parent the
Sickness Impact Profile or the SIP’s physical subscales 21,58. Data on
responsiveness of the RDQ have been published by a number of authors
21,64,98,124,6,120,104,122,119. In a later section, we comment on the
responsiveness of the RDQ compared to the Oswestry questionnaire.
Another important element of a questionnaire’s responsiveness is the
smallest effect that is clinically significant. 6 suggest that the smallest change
likely to be clinically significant lies between 2.5 and 5 points. However, this
may vary depending on the level of disability of the patients. Stratford et al
- 6 -
(1998)122 suggest that the minimum clinically important change in scores is
1-2 points for patients with little disability, 7-8 points for patients reporting high
levels of disability, and 5 points in unselected patients. Patrick et al (1995)98
suggests 2-3 points as the minimum clinically important difference (for a 23
item version of the RDQ). These are minimum changes in score which should
be regarded as clinically significant in relation to individual patients. Setting
the minimally clinically important difference as high as 5 in designing a clinical
trial would risk under-powering the trial, as fewer patients are needed if a trial
is designed on the basis of a large change in score. For sample size
calculations for clinical trials, we therefore recommend that changes in scores
of 2-3 points on the RDQ should be used.
Oswestry Disability Index
Development of the ODI
Development of the Oswestry Disability Index was initiated by John O'Brien in
1976 in a specialist referral clinic seeing large numbers of patients with
chronic low back pain. Back pain patients were interviewed by an
orthopaedic surgeon (Stephen Eisenstein), an occupational therapist (Judith
Couper) and a physiotherapist (Jean Davies) to identify the disturbance of
activities of daily living through chronic back pain. It was designed as a
measure of both assessment and outcome. Various drafts of the
questionnaire were tried. Version 1.0 of the questionnaire was published in
198030 and widely disseminated from the 1981 ISSLS meeting in Paris.
The questionnaire can be completed in less than five minutes and is scored in
less than a minute. Scores for the ODI in a wide variety of settings are shown
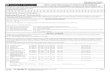
in table 1.
Category Total no.
No. of groups
Weighted mean ODI
S.D. / F Sources Sources not
- 7 -
Oswestry and Roland-Morris
score range used used
‘Normal’ populations 461 4 10.19 2.2 - 12 0.37 90,52,50,53,62
, 61
20
Pelvic fractures 31 1 13.26 15.4 - 44
Idiopathic scoliosis 1264 5 13.81 9.2-13 0.03 33,90
Neck pain 56 1 21 9.7 - 151
Spondylolisthesis 120 5 26.63 6.1-16 1.76 97,115-117,
128
Primary back pain 2166 21 27 5.8-
23.6
0.33 34,93,132,92,
52,63,50,53,62
,81,112,61,82,
110,111
86
Psychiatric patients 75 1 30.8 21.5 - 150
Neurogenic claudication 82 2 36.65 17-18 0.14 46-48 20
Chronic back pain 1530 25 43.3 10-21 0.02 113,24,40,42,
80,25-27,41
102,14,133,73,
116,69,74,117,
121,131,135,1
1,70,85,139,8,
9,128,129,130,
136,140,142,
71,72,138,137,
12,68,75,141
PID/Sciatica 663 9 44.65 10.5-
30.1
0.16 25,26,36,27,35
,13,38,131
73,69,
74,70-
72,114,
127,68,
75
Fibromyalgia 192 4 44.83 14.2-
18.9
0.07 133-
135,139,136,
140,142,138,
137,141
Metastases 100 2 48.04 18.1-23 0.04 99,140
- 8 -
Table 1. Normative data for ODI
ODI data have been pooled for various categories of patients. The weighted
mean of the groups is given. The ratio of the variances (F) is not significant in
any of the categories suggesting that the assumptions used to pool the data
to produce the these weighted mean values are reasonable ones. The
sources of data used are tabulated. Other sources of data are given in the
final column, but the information in these was not sufficient to use in
calculation of the weighted mean values.
Modifications and translations of the ODI
The ODI was validated and improved in a study by an MRC group. This
version (2.0) is recommended for general use 91,1,100,92. It has been widely
distributed by correspondence and is available as part of a computer
interview in the UK (slightly modified) 1,101 or in the US via MODEMS™. It
has been administered over the telephone90,53. A modified version of the
Oswestry Disability Questionnaire has been published by the North American
Spine Society (NASS) 19. This version, which is available from
www.modems.org also contains a pain diagram, questions from the SF36
health questionnaire, questions on neurological symptoms and on the
“bothersomeness” of back pain, and a modification of the ODI. The
modifications introduced were designed to clarify the wording of some
individual response items. This version also specifies that the respondent
should answer the questions in relation to ‘the past week’ (the original
instrument is not specific on this point, 2.0 uses “today”). The NASS version
is part of the battery of outcome measures recommended by Deyo et al
199823. Psychometric data are limited on the NASS instrument, though we
are aware that it is being used in a number of large studies, and that
psychometric data will become available in due course. This version has led
MODEMS™, PO Box 2354, Des Plaines, IL 60017-2354
- 9 -
Oswestry and Roland-Morris
to confusion over the scoring system in recent presentations from North
America. The reader is referred to Fairbank and Pynsent (2000) for further
details31
The wording and scoring system of ODI version 2.0 is reproduced in
Appendix 2. It has been translated into at least 9 languages. Non-English
language citations are shown in table 2. The authors of the original
publication hold the copyright of the ODI30. They support the widespread use
of version 2.0, and neither the authors nor Spine require permission for its
use. However, permission from the authors (JF) is required if modifications to
the instrument are being considered. Validated translation of ODI 2.0 into
other languages is strongly encouraged, though the authors ask to be
consulted when such translations are undertaken.
Language Citation(s)
Danish 15,88,87,143
Dutch 143
Finnish 54,56,40,39,73,42,69,74,70,46-
48,52,74,83,84,128-
130,41,50,51,53,71,72,55,68,75
115-117,151,86,62,61,145
French 28,143
78,89
German 2,95,149
9,16,148
Greek 7
Norwegian 29,36,35,114,131
Spanish 76
Swedish 112,110,111
- 10 -
Table 2. Non English language citations of the ODI
Face and Content Validity of the ODI
These address the extent to which the scale appears to be assessing the
intended attributes. 25 patients in their first attack of low back pain who might
reasonably be expected to improve over a period were shown to do so30.
Beuerskins and others carried out a more sophisticated analysis of 81
patients over a 5 weeks period confirming an expected improvement in ODI
scores6. Their study allows calculation of an effect size of 0.818. However
Kopec66 reported an effect size of only 0.07. Fisher and Johnson performed
one of the most detailed validations of the questionnaire (version 2.0). They
related patient behaviour whilst they were completing this and other
questionnaires to their responses within the questionnaires32. Two sections
of the questionnaires (sitting and walking) did correlate with patient response
but was less satisfactory for a third (lifting).
Construct validity of the ODI
The wording of the ODI was designed on the basis of patients complaints and
symptoms with chronic low back pain. The ODI shows moderate correlation
with pain measures such as a visual analogue scale (n=94, r=0.62)39 and the
McGill pain questionnaire94,43.
The ODI has been used to validate the Pain Disability Index108 123 39,42;
the Low Back Outcome Score37; The Manniche Scale88,87; the Aberdeen
score107; a new German language scale2; the Curtin Scale45; and a
functional capacity evaluation63.
- 11 -
Oswestry and Roland-Morris
The ODI correlates with SF3638. ODI is a better predictor of return to work
than two different mechanical methods of lumbar spine assessment96,82. It
predicts isokinetic performance60; isometric endurance77; and with sitting
and standing (but not lifting) in a secret observation study32. In the
Mackenzie system of evaluation, “centralisers” show improving ODI
scores125. Physical tests correlate with the ODI42 but range of movement
does not41.
Internal Consistency of the ODI
Strong et al (using version 1.0) found Cronbach's to be 0.71123, Fisher and
Johnson (using version 2.0) 0.7632 and Kopec 0.8766. All these
investigations show an “acceptable” degree of internal consistency.
Reproducibility of the ODI
In the original study chronic low back pain patients were tested twice at a 24
hours interval (n=22, r= 0.99)30. This may include a memory effect. If the
test/retest interval is extended to 4 days the correlation of scores drops to
n=22, r=0.9166 and, if retested after a week, n= 22, r=0.8339. The
disadvantage of increasing the time interval is that natural symptom
fluctuation may also be an influence. Grevitt (personal communication) found
a poorer test/retest correlation in a study where he mailed versions of the
questionnaire to patients to fill in and then asked them to fill in the
questionnaire again in a different format when they attended as out-patients.
Responsiveness of the ODI
Receiver Operating Characteristic (ROC) is a concept used to explore “the
diagnostic test performance of an instrument” or the ability of the instrument
to detect change21, where its sensitivity is plotted against (1 minus
specificity). This allows the ability of the instrument to detect change to be
investigated. The ROC index (D) for the ODI was found to be 0.76, a score
which is acceptable but not as good as the RDQ scale. This is perhaps not
- 12 -
surprising in a population of not too severely affected patients (mean
ODI=26.2, sd=13.5)6, 82. The ROC index has not been calculated for the
ODI in a group of more severely affected patients. As the ROC curve
depends on sensitivity and specificity, there is an inherent assumption that a
“true disability” is known. This may be difficult to justify21.
Meade110 chose 4 points as the minimum difference in mean scores
between groups carrying clinical significance. The FDA has chosen a
minimum 15 point change in spinal fusion patients before surgery and at
follow-up (Lipscombe, Personal Communication). Table 2 shows change in
weighted means calculated from publications reporting ODI before and after
treatment in various subgroups of patients. Large changes in score are seen
in primary back pain patients and the least in those with spinal metastases.
More work is needed in this area.
Comparison between the Roland Disability Questionnaire and the Oswestry
Disability Index.
It is important to emphasise that differences between these instruments are
not great. Both are widely used, have been extensively tested, and are
applicable to a wide variety of settings. The situation where a choice between
the two instruments would be most clear cut would be where a validated
translation exists for one, but not the other.
Both were originally designed for paper administration. The RDQ has been
widely administered over the telephone. While the ODI can be administered
by phone, the multiple nature of the response items makes this more difficult.
Floor and ceiling effects may influence the choice of instruments. A greater
proportion of patients score in the top half of the distribution of RDQ scores
than that of ODI scores 65. At high levels of disability, the ODI may still show
change where RDQ scores are maximal. At the other end of the scale,
Roland scores may still discriminate when ODI scores are at a minimum1 . We
- 13 -
Oswestry and Roland-Morris
therefore recommend the ODI where patients are likely to have persistent
severe disability, and the RDQ for populations are likely to have relatively little
disability. However, for most populations, both instruments will function
satisfactorily in this respect.
RDQ and ODI scores are highly correlated, with similar test re-test reliability
and internal consistency 1,17, 64 In terms of discriminating power, including
ability to detect change over time, Stratford et al (1994)121 found that the
properties of the two instruments were very similar. Other authors have
reported that the ODI performs better 79 or the reverse 5, or that the result
depends on the exact comparison being made 64. It is difficult to compare
these studies in detail, since they relate to different patient populations.
Normative data for RDQ and ODI
In table 3, we have included normative data to give clinicians an idea of the
sort of scores that that they can expect in a variety of clinical situations The
table includes studies in which RDQ and ODI scores were both measured on
the same group of patients to allow comparison between scores on the two
instruments.
RDQ ODI
Patients recruited to
trial, less than 3/12 pain,
no radiculopathy 79
(Canada), mean values,
range, standard
deviation
10.9, 0-22, 4.7 33.0, 4-70, 14.7
Patients with EMG
evidence of
radiculopathy in hospital
clinic 79 (Canada),
mean values, range,
14.2, 0-24, 5.2 49.1, 6-86, 17.1
- 14 -
standard deviation
Patients referred to
physiotherapy, Canada
121 Mean values and
standard deviations at
enrolment (mean
duration symptoms 48
days) and 4 week follow
up
Enrolment:11.8, 6.2
4 weeks later: 7.1, 5.7
Enrolment: 40.5, 17.8
4 weeks later: 24.4,
15.5
Patients with non-
specific low back pain
for >6 weeks. Mean
score at baseline and 5
weeks. 6
12.1, 7.5
Improved patients 12.1,
4.3
Non-improved 11.8,
10.6
27.6, 21.9
Improved patients 26.2,
14.3
Non-improved 29.1,
29.5
Table 3. RDQ and ODI scores measured simultaneously in a range of patient populations
Summary
The Roland-Morris Disability Scale is a short and simple method of assessing
self rated physical function in patients with back pain. Its ease of use makes it
suitable for following progress of individual patients in clinical settings, and for
combining with other measures of function (e.g. psychological or work
disability) in research settings. The ODI is likewise an effective method of
measuring disability in back pain patients with a wide degree of severity and
aetiology. Both instruments have stood the test of time and been used in a
wide variety of clinical situations, in the UK, USA and many other countries.
Both instruments perform as well most other currently available instruments,
and better than some. The RDQ may be better suited to settings where
patients have mild to moderate disability, and the ODI to situations where
patients may have persistent severe disability. The availability of the two
- 15 -
Oswestry and Roland-Morris
instruments in a wide range of languages permits comparison between
studies carried out in a wide range of countries.
Note that some of the text of this paper has been derived from Fairbank and Pynsent 2000 31
- 16 -
References
Baker D, Pynsent P, Fairbank J. The Oswestry Disability Index revisited. In:
Roland M, Jenner J, eds. Back pain: New Approaches to Rehabilitation
and Education. Manchester: Manchester University Press, 1989: 174-86.
1. Basler HD, Jakle C, KronerHerwig B. Incorporation of cognitive-behavioral
treatment into the medical care of chronic low back patients: A controlled
randomized study in German pain treatment centers. Patient Education
and Counseling 1997;31:113-24.
2. Beaton D, Bombardier C, Guillemin F, Bosi-Ferraz M. Guidelines for the
process of cross-cultural adaptation of self-report measures. Paper on in
this edition of Spine
3. Bergner M, Bobbitt R, Carter W, Gilson B. The Sickness Impact Profile:
development and final revision of a health status measure. Medical Care
1981;19:787-805.
4. Beurskens A, de Vet H, Koke A, van der Heijden G, Knipschild P.
Measuring functional status of patients with low back pain: assessment of
the quality of four disease specific questionniares. Spine 1995;20:1017-
28.
5. Beurskens A, deVet HCW, Koke AJA. Responsiveness of functional status
in low back pain: A comparison of different instruments. Pain 1996;65:71-
6.
6. Boscainos P, Sapkas G, Stilianesi E, Prouskas C, Stathakopoulos D.
Clinical relevance of specific parameters isolated within the Oswestry and
Roland-Morris functional disability scales. J Bone Jt Surg 1999;81-B:239.
- 17 -
Oswestry and Roland-Morris
7. Bossons CR, Levy J, Sutterlin CE. Reconstructive spinal surgery:
Assessment of outcome. Southern Medical Journal 1996;89:1045-52.
8. Breitenseher MJ, Eyb RP, Matzner MP, et al. MRI of unfused lumbar
segments after spondylodesis. Journal of Computer Assisted Tomography
1996;20:583-7.
9. Burchiel KJ, Anderson VC, Brown FD, et al. Prospective, multicenter study
of spinal cord stimulation for relief of chronic back and extremity pain.
Spine 1996;21:2786-94.
10.Burchiel KJ, Anderson VC, Wilson BJ, et al. Prognostic Factors of Spinal-
Cord Stimulation For Chronic Back and Leg Pain. Neurosurgery
1995;36:1101-10.
11.Campello M, Weiser S, van Doorn JW, Nordin M. Approaches to improve
the outcome of patients with delayed recovery. Baillieres Clinical
Rheumatology 1998;12:93-113.
12.Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injections
for sciatica due to herniated nucleus pulposus. New England Journal of
Medicine 1997;336:1634-40.
13.Cassisi J, Sypert G, Salamon A, Kapel L. Independent evaluation of a
multidisciplinary rehabilitation program for chronic low back pain.
Neurosurgery 1989;25:877-83.
14.Christensen TH, Bliddal H, Hansen SE, et al. Severe Low-Back-Pain .1.
Clinical-Assessment of 2 Weeks Conservative Therapy. Scandinavian
Journal of Rheumatology 1993;22:25-9.
- 18 -
15.Chrubasik S, Zimpfer C, Schutt U, Ziegler R. Effectiveness of
Harpagophytum procumbens in treatment of acute low back pain.
Phytomedicine 1996;3:1-10.
16.Co Y, Eaton S, Maxwell M. The relationship between the St Thomas and
Oswestry disability scores and the severity of low back pain. J
Manipulative Physiol Ther 1993;16:14-8.
17.Cohen J. Statistical power analysis for the behavioural sciences. New
York: Academic Press, 1977: 1-27.
18.Daltroy L, Cats-Braril W, Katz J, Fossel A, Liang M. The North American
Spine Socity lumbar spine outcome assessment instrument. Reliability
and validity tests. Spine 1996;21:74-749.
19. Deo S, Wanders L, Makan P, et al. Outcome measures for neurogenic
claudication. North American Spine Society 1998, San Francisco.
20.Deyo R, Centor R. Assessing the responsiveness of functional scales to
clinical change: an analagy to diagnostic test performance. J Chronic Dis
1986;39:897-906.
21.Deyo RA. Measuring the Functional Status of Patients With Low-Back
Pain. Archives of Physical Medicine and Rehabilitation 1988;69:1044-53.
22.Deyo RA, Battie M, Beurskens A, et al. Outcome measures for low back
pain research - A proposal for standardized use. Spine 1998;23: 2003-13.
23.Difabio RP. Efficacy of Manual Therapy. Physical Therapy 1992;72:853-
64.
- 19 -
Oswestry and Roland-Morris
24.Difabio RP. Efficacy of Comprehensive Rehabilitation Programs and Back
School For Patients With Low-Back-Pain - a Metaanalysis. Physical
Therapy 1995;75:865-78.
25.Difabio RP, Mackey G, Holte JB. Disability and Functional Status in
Patients With Low-Back-Pain Receiving Workers Compensation - a
Descriptive Study With Implications For the Efficacy of Physical Therapy.
Physical Therapy 1995;75:180-93.
26.DiFabio RP, Mackey G, Holte JB. Physical therapy outcomes for patients
receiving workers' compensation following treatment for herniated lumbar
disc and mechanical low back pain syndrome. Journal of Orthopaedic &
Sports Physical Therapy 1996;23:180-7.
27.Dropsy R, Marty M. Quality-of-Life Indexes For Assessment of Low-Back-
Pain. Revue Du Rhumatisme 1994;61:S44-S8.
28.Dullerud R, Amundsen T, Lie H, et al. Clinical-Results After Percutaneous
Automated Lumbar Nucleotomy - a Follow-Up-Study. Acta Radiologica
1995;36:418-24.
29. Fairbank J, Couper J, Davies J, O'Brien J. The Oswestry low back pain
questionnaire. Physiotherapy 1980;66:271-3.
30.Fairbank J, Pynsent P. The Oswestry Disability Index. Spine 2000
(accepted for publication).
31.Fisher K, Johnson M. Validation of the Oswestry low back pain disability
questionaire, its sensitivity as a measure of change following treatment
and its relationship with other aspects of the chronic pain experience.
Physiotherapy Theory and Practice 1997;13:67-80.
- 20 -
32.Goldberg M, Mayo N, Poitras B, Scott S, Hanley J. The Ste-Justine
adolescent idiopathic scoliosis cohort study: Part III: Back pain. Spine
1994;14:1173-581.
33.Gorman D, Patumianos G, Williams K, et al. Relationship between alcohol
abuse and low back pain. Alcohol and Alcoholism 1987;22:61-3.
34.Graver V, Ljunggren AE, Magnaes B, Loeb M, Lie H. Is the outcome of
traditional lumbar disc surgery related to the size of the exposure? Acta
Neurochirurgica 1996;138:824-8.
35.Graver V, Ljunggren AE, Malt UF, et al. Can Psychological Traits Predict
the Outcome of Lumbar Disc Surgery When Anamnestic and Physiological
Risk-Factors Are Controlled For - Results of a Prospective Cohort Study.
Journal of Psychosomatic Research 1995;39:465-76.
36.Greenough CG. Recovery From Low-Back-Pain - 1-5-Year Follow-Up of
287 Injury- Related Cases. Acta Orthopaedica Scandinavica 1993;64:1-
34.
37.Grevitt M, Khazim R, Webb J, Mulholland R, Shepperd J. The short form-
36 health survey questionnaire in spine surgery. Journal of Bone and Joint
Surgery-British Volume 1997;79B:48-52.
38.Gronblad M, Hupli M, Wennerstrand P, et al. Intercorrelation and test-
retest reliability of the Pain Disability Index (PDI) and the Oswestry
Disability Questionnaire (ODQ) and their correlation with pain intensity in
low back pain patients. Clin J Pain 1993;9:189-95.
39.Gronblad M, Hupli M, Wennerstrand P, et al. Intercorrelation and Test-
Retest Reliability of the Pain Disability Index (Pdi) and the Oswestry
Disability Questionnaire (Odq) and Their Correlation With Pain Intensity in
Low-Back-Pain Patients. Clinical Journal of Pain 1993;9:189-95.
- 21 -
Oswestry and Roland-Morris
40.Gronblad M, Hurri H, Kouri JP. Relationships between spinal mobility,
physical performance tests, pain intensity and disability assessments in
chronic low back pain patients. Scandinavian Journal of Rehabilitation
Medicine 1997;29:17-24.
41.Gronblad M, Jarvinen E, Hurri H, Hupli M, Karaharju EO. Relationship of
the Pain Disability Index (Pdi) and the Oswestry Disability Questionnaire
(Odq) With 3 Dynamic Physical Tests in a Group of Patients With Chronic
Low-Back and Leg Pain. Clinical Journal of Pain 1994;10:197-203.
42.Haas M, Nyiendo J. Diagnostic utility of the McGill Pain Questionaire and
the Oswestry Disability Questionaire for classification of low back
syndromes. J Manipulative Physiol Ther 1992;15:90-8.
43.Hakim RNM, Gruen GS, Delitto A. Outcomes of patients with pelvic-ring
fractures managed by open reduction internal fixation. Physical Therapy
1996;76:286-95.
44.Harper AC, Harper DA, Lambert LJ, et al. Development and Validation of
the Curtin Back Screening Questionnaire (Cbsq) - a Discriminative
Disability Measure. Pain 1995;60:73-81.
45.Herno A, Airaksinen O, Saari T, Luukkonen M. Lumbar spinal stenosis: A
matched-pair study of operated and non-operated patients. British Journal
of Neurosurgery 1996;10:461-5.
46.Herno A, Airaksinen O, Saari T, Sihvonen T, Luukkonen M. The effect of
prior back surgery on surgical outcome in patients operated on for lumbar
spinal stenosis - A matched- pair study. Acta Neurochirurgica
1996;138:357-63.
- 22 -
47.Herno A, Airaksinen O, Saari T, Svomalainen O. Pre- and postoperative
factors associated with return to work following surgery for lumbar spinal
stenosis. American Journal of Industrial Medicine 1996;30:473-8.
48.Hsieh C, Phillips R, Adams A, Pope M. Functional outcomes of low back
pain: comparison of four treatment groups in a randomised controlled trial.
J Manip Physiol Ther 1992;15:4-9.
49.Hupli M, Heinonen R, Vanharanta H. Height changes among chronic low
back pain patients during intense physical exercise. Scandinavian Journal
of Medicine & Science in Sports 1997;7:32-7.
50.Hupli M, Hurri H, Luoto S, et al. Low synthesis rate of type I procollagen is
normalized during active back rehabilitation. Spine 1997;22:850-4.
51.Hupli M, Hurri H, Luoto S, Sainio P, Alaranta H. Isokinetic performance
capacity of trunk muscles .1. The effect of repetition on measurement of
isokinetic performance capacity of trunk-muscles among healthy controls
and two different groups of low-back pain patients. Scandinavian Journal
of Rehabilitation Medicine 1996;28:201-6.
52.Hupli M, Sainio P, Hurri H, Alaranta H. Comparison of trunk strength
measurements between two different isokinetic devices used at clinical
settings. Journal of Spinal Disorders 1997;10:391-7.
53.Hurri H. The Swedish back school in chronic low back pain. Part II.
Factors predicting the outcome. Scand J Rehabil Med 1989;21:41-4.
54.Hurri H, Slatis P, Soini J, et al. Lumbar spinal stenosis: Assessment of
long-term outcome 12 years after operative and conservative treatment.
Journal of Spinal Disorders 1998;11:110-5.
- 23 -
Oswestry and Roland-Morris
55.Hurri HO, Petaja JM, Alaranta HT, et al. Fibrinolytic Defect in Chronic
Back Pain - a Controlled-Study of Plasminogen-Activator Activity in 20
Patients. Acta Orthopaedica Scandinavica 1991;62:407-9.
56.Jarvikoski A, Mellin G, Estlander A. Outcome of two multimodal back
treatment programmes with and without intensive physical training.
Journal of Spinal Disorders 1995;6:93-8.
57.Jensen MP, Strom SE, Turner JA, Romano JM. Validity of the Sickness
Impact Profile Roland Scale As a Measure of Dysfunction in Chronic Pain
Patients. Pain 1992;50:157-62.
58.Johansson E, Lindberg P. Subacute and chronic low back pain. Reliability
and validity of a Swedish version of the Roland and Morris Disability
Questionnaire. Scandinavian Journal of Rehabilitation Medicine
1998;30:139-43.
59.Kaivanto KK, Estlander AM, Moneta GB, Vanharanta H. Isokinetic
Performance in Low-Back-Pain Patients - the Predictive Power of the Self-
Efficacy Scale. Journal of Occupational Rehabilitation 1995;5:87-99.
60.Kankaanpaa M, Taimela S, Laaksonen D, Hanninen O, Airaksinen O.
Back and hip extensor fatigability in chronic low back pain patients and
controls. Archives of Physical Medicine and Rehabilitation 1998;79:412-7.
61.Kankaanpaa M, Taimela S, Webber CL, Airaksinen O, Hanninen O.
Lumbar paraspinal muscle fatigability in repetitive isoinertial loading: EMG
spectral indices, Borg scale and endurance time. European Journal of
Applied Physiology and Occupational Physiology 1997;76:236-42.
62.Kaplan GM, Wurtele SK, Gillis D. Maximal effort during functional capacity
evaluations: An examination of psychological factors. Archives of Physical
Medicine and Rehabilitation 1996;77:161-4.
- 24 -
63.Kopec J, Esdaile J. Spine Update: Functional Disability Scales for Back
Pain. Spine 1995;20:1943-9
64. Kopec JA, Esdaile JM, Abrahamowicz et al. The Quebec Back Pain Disability
Scale: Measurement Properties. Spine 1995; 20: 341-352
65.Kopec JA, Esdaile JM, Abrahamowicz M, et al. The Quebec Back Pain
Disability Scale: Conceptualization and development. Journal of Clinical
Epidemiology 1996;49:151-61.
66.Kopec JA. Paper on back specific health status measures in this edition of
Spine
67.Kotilainen E. Long-term outcome of patients suffering from clinical
instability after microsurgical treatment of lumbar disc herniation. Acta
Neurochirurgica 1998;140:120-5.
68.Kotilainen E, Alanen A, Erikintalo M, Valtonen S, Kormano M. Magnetic-
Resonance Image Changes and Clinical Outcome After Microdiscectomy
or Nucleotomy For Ruptured Disc. Surgical Neurology 1994;41:432-40.
69.Kotilainen E, Alanen A, Parkkola R, et al. Cross-Sectional Areas of
Lumbar Muscles After Surgical- Treatment of Lumbar Disc Herniation - a
Study With Magnetic- Resonance-Imaging After Microdiscectomy or
Percutaneous Nucleotomy. Acta Neurochirurgica 1995;133:7-12.
70.Kotilainen E, Heinanen J, Gullichsen E, Koivunen T, Aro HT.
Spondylodesis in the treatment of segmental instability of the lumbar spine
with special reference to clinically verified instability. Acta Neurochirurgica
1997;139:629-35.
- 25 -
Oswestry and Roland-Morris
71.Kotilainen E, Muittari P, Kirvela O. Intradiscal glycerol or bupivacaine in
the treatment of low back pain. Acta Neurochirurgica 1997;139:541-5.
72.Kotilainen E, Valtonen S. Clinical Instability of the Lumbar Spine After
Microdiscectomy. Acta Neurochirurgica 1993;125:120-6.
73.Kotilainen E, Valtonen S. Percutaneous Nucleotomy in the Treatment of
Lumbar Disc Herniation Results After a Mean Follow-Up of 2 Years. Acta
Neurochirurgica 1994;128:47-52.
74.Kotilainen E, Valtonen S. Long-term outcome of patients who underwent
percutaneous nucleotomy for lumbar disc herniation: Results after a mean
follow-up of 5 years. Acta Neurochirurgica 1998;140:108-13.
75.Kovacs FM, Abraira V, Lopezabente G, Pozo F. Neuroreflexotherapic
Intervention in the Treatment of Nonspecific Low-Back-Pain - a
Randomized, Double-Blind, Controlled Clinical-Trial. Medicina Clinica
1993;101:570-5.
76.Kuukkanen T, Malkia E. Muscular performance after a 3 month
progressive physical exercise program and 9 month follow-up in subjects
with low back pain. A controlled study. Scandinavian Journal of Medicine
& Science in Sports 1996;6:112-21.
77.Le Huec J, Hussen J, Lesprit E, Liquois F, Chauveau D. Anterior
endoscopic lumbar arthrodesis (L2 to L5). (RPS: tetroperitoneoscopy); 28
cases, one to 2 years follow-up. North American Spine Society 1998, San
Francisco.
78.Leclaire R, Blier F, Fortin L, Proulx R. A cross-sectional study comparing
the Oswestry and Roland- Morris functional disability scales in two
populations of patients with low back pain of different levels of severity.
Spine 1997;22:68-71.
- 26 -
79.Lefort SM, Hannah TE. Return to Work Following an Aquafitness and
Muscle Strengthening Program For the Low-Back Injured. Archives of
Physical Medicine and Rehabilitation 1994;75:1247-55.
80.Loisel P, Abenhaim L, Durand P, et al. A population-based, randomized
clinical trial on back pain management. Spine 1997;22:2911-8.
81.Loisel P, Poitras S, Lemaire J, et al. Is work status of low back pain
patients best described by an automated device or by a questionnaire?
Spine 1998;23:1588-94.
82.Luoto S, Hupli M, Alaranta H, Hurri H. Isokinetic performance capacity
trunk muscles .2. Coefficient of variation in isokinetic measurement in
maximal effort and in submaximal effort. Scandinavian Journal of
Rehabilitation Medicine 1996;28:207-10.
83.Luoto S, Taimela S, Hurri H, et al. Psychomotor speed and postural
control in chronic low back pain patients - A controlled follow-up study.
Spine 1996;21:2621-7.
84.Luscombe FE, Wallace L, Williams J, Griffiths DPG. A district-general-
hospital - pain management program - first year experiences and
outcomes. Anaesthesia 1995;50:114-7.
85.Malmivaara A, Hakkinen U, Aro T, et al. The Treatment of Acute Low-
Back-Pain - Bed Rest, Exercises, or Ordinary Activity. New England
Journal of Medicine 1995;332:351-5.
86.Manniche C. Assessment and Exercise in Low-Back-Pain - With Special
Reference to the Management of Pain and Disability Following First-Time
Lumbar Disc Surgery. Danish Medical Bulletin 1995;42:301-13.
- 27 -
Oswestry and Roland-Morris
87.Manniche C, Asmussen K, Lauritsen B, et al. Low-Back-Pain Rating-Scale
- Validation of a Tool For Assessment of Low-Back-Pain. Pain
1994;57:317-26.
88.Marty M, Blotman F, Avouac B, Rozenberg S, Valat JP. Validation of the
French version of the Dallas Pain Questionnaire in chronic low back pain
patients. Revue Du Rhumatisme 1998;65:126-34.
89.Mayo NE. Letter. Spine 1995;20:1535-6.
90.Meade T, Browne W, Mellows S, al. e. Comparison of chiropractic and
outpatient management of low back pain: a feasibility study. J Epidem
Comm Health 1986;40:12-7.
91.Meade TW, Dyer S, Browne W, Frank AO. Randomized Comparison of
Chiropractic and Hospital Outpatient Management For Low-Back-Pain -
Results From Extended Follow-Up. British Medical Journal 1995;311:349-
51.
92.Meade TW, Dyer S, Browne W, Townsend J, Frank AO. Low-Back-Pain of
Mechanical Origin - Randomized Comparison of Chiropractic and Hospital
Outpatient Treatment. British Medical Journal 1990;300:1431-7.
93.Melzack R. The McGill pain questionaire: Major properties and scoring
methods. Pain 1975;1:277-99.
94.MullerBusch HC, Hoffmann P. Active music therapy for chronic pain: A
prospective study. Schmerz 1997;11:91-100.
95.Nordin M, Skovron ML, Hiebert R, et al. Early predictors of delayed return
to work in patients with low back pain. Journal of Musculoskeletal Pain
1997;5:5-27.
- 28 -
96.O'Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing
exercise in the treatment of chronic low back pain with radiologic
diagnosis of spondylolysis or spondylolisthesis. Spine 1997;22:2959-67.
97.Patrick D, Deyo R, Atlas S, et al. Assessing Health-Related Quality of Life
in Patients With Sciatica. Spine 1995;20:1899-909.
98.Purohit OP, Anthony C, Radstone CR, Owen J, Coleman RE. High-Dose
Intravenous Pamidronate For Metastatic Bone Pain. British Journal of
Cancer 1994;70:554-8.
99.Pynsent P, Fairbank J, Carr A. Outcome measures in orthopaedics.
Oxford: Butterworth-Heinemann, 1993.
100. Pynsent PB, Fairbank JCT. Computer Interview System For Patients
With Back Pain. Journal of Biomedical Engineering 1989;11:25-9.
101. Reesor KA, Craig KD. Medically Incongruent Chronic Back Pain -
Physical Limitations, Suffering, and Ineffective Coping. Pain 1988;32:35-
45.
102. Ren XS. Are patients capable of attributing functional impairments to
specific diseases? American Journal of Public Health 1998;88:837-8.
103. Riddle DL, Stratford PW, Binkley JM. Sensitivity to change of the
Roland-Morris back pain questionnaire: Part 2. Physical Therapy
1998;78:1197-207.
104. Roland M, Morris R. A study of the natural history of back pain. Part 2:
Development of guidelines for trials of treatment in primary care. Spine
1983;8:145-50.
- 29 -
Oswestry and Roland-Morris
105. Roland M, Morris R. A study of the natural history of low back pain.
Part 1: Development of a reliable and sensitive measure of disability in
low-back pain. Spine 1983;8:141-4.
106. Ruta D, Garratt A, Wardlaw D, Russell I. Developing a Valid and
Reliable Measure of Health Outcome for Patients With Low Back Pain.
Spine 1994;19:1887-96.
107. Salen BA, Spangfort EV, Nygren AL, Nordemar R. The Disability
Rating Index - an Instrument For the Assessment of Disability in Clinical
Settings. Journal of Clinical Epidemiology 1994;47:1423-34.
108. Simmonds M, Olson S, Jones S, et al. Psychometric Characteristics
and Clinical Usefulness of Physical Performance Tests in Patients With
Low Back Pain. Spine 1998;23:2412-21.
109. Skargren EI, Carlsson PG, Oberg BE. One-year follow-up comparison
of the cost and effectiveness of chiropractic and physiotherapy as primary
management for back pain - Subgroup analysis, recurrence, and
additional health care utilization. Spine 1998;23:1875-83.
110. Skargren EI, Oberg BE. Predictive factors for 1-year outcome of low-
back and neck pain in patients treated in primary care: comparison
between the treatment strategies chiropractic and physiotherapy. Pain
1998;77:201-7.
111. Skargren EI, Oberg BE, Carlsson PG, Gade M. Cost and effectiveness
analysis of chiropractic and physiotherapy treatment for low back and
neck pain - Six-month follow-up. Spine 1997;22:2167-77.
112. Skinner JB, Erskine A, Pearce S, et al. The Evaluation of a Cognitive
Behavioral Treatment Program in Outpatients With Chronic Pain. Journal
of Psychosomatic Research 1990;34:13-9.
- 30 -
113. Skouen JS, Larsen JL, Gjerde IO, Hegrestad SE, Vollset SE.
Cerebrospinal fluid protein concentrations in patients with sciatica caused
by lumbar disc herniation: An investigation of biochemical, neurologic, and
radiologic predictors of long-term outcome. Journal of Spinal Disorders
1997;10:505-11.
114. Soini J, Laine T, Pohjolainen T, Hurri H, Alaranta H. Spondylodesis
Augmented By Transpedicular Fixation in the Treatment of Olisthetic and
Degenerative Conditions of the Lumbar Spine. Clinical Orthopaedics and
Related Research 1993:111-6.
115. Soini J, Slatis P, Kannisto M, Sandelin J. External Transpedicular
Fixation-Test of the Lumbar Spine Correlates With the Outcome of
Subsequent Lumbar Fusion. Clinical Orthopaedics and Related Research
1993:89-96.
116. Soini JR, Harkonen HI, Alaranta HT, Seitsalo SK. External Fixation-
Test in Low-Back-Pain - Function Analyzed in 25 Patients. Acta
Orthopaedica Scandinavica 1994;65:87-90.
117. Stratford P, Binkley J. Measurement properties of the RM-18: a
modified version of the Roland-Morris diability scale. Spine 1997;22:2416-
21.
118. Stratford P, Binkley J. Applying the Results of Self-Report Measures to
Individual Patients: An Example Using the Roland-Morris Questionnaire.
Journal of Orthopaedic & Sports Physical Therapy 1999;29:232-9.
119. Stratford PW, Binkley J, Solomon P, et al. Defining the minimum level
of detectable change for the Roland- Morris questionnaire. Physical
Therapy 1996;76:359-65.
- 31 -
Oswestry and Roland-Morris
120. Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assessing
Change Over Time in Patients With Low-Back-Pain. Physical Therapy
1994;74:528-33.
121. Stratford PW, Binkley JM, Riddle DL, Guyatt GH. Sensitivity to change
of the Roland-Morris back pain questionnaire: Part 1. Physical Therapy
1998;78:1186-96.
122. Strong J, Ashton R, Large RG. Function and the Patient With Chronic
Low-Back-Pain. Clinical Journal of Pain 1994;10:191-6.
123. Stucki G, Lian M, Fossel A, Katz J. Relative Responsiveness of
Condition-Specific and Generic Health Status Measures in Degenerative
Lumbar Spine Stenosis. J Clin Epidemiol 1995;48:1369-78.
124. Sufka A, Hauger B, Trenary M, et al. Centralization of low back pain
and perceived functional outcome. Journal of Orthopaedic & Sports
Physical Therapy 1998;27:205-12.
125. Taylor S, Taylor A, Foy M, Fogg A. Responsiveness of common
outcome measures for patients with low back pain. Spine 1999;24:1805-
12.
126. Tesio L, Granger CV, Fiedler RC. A unidimensional pain/disability
measure for low-back pain syndromes. Pain 1997;69:269-78.
127. Tiusanen H, Schlenzka D, Seitsalo S, Poussa M, Osterman K. Results
of a trial of anterior or circumferential lumbar fusion in the treatment of
severe isthmic spondylolisthesis in young patients. Journal of Pediatric
Orthopaedics-Part B 1996;5:190-4.
- 32 -
128. Tiusanen H, Seitsalo S, Osterman K, Soini J. Anterior interbody lumbar
fusion in severe low back pain. Clinical Orthopaedics and Related
Research 1996:153-63.
129. Tiusanen H, Seitsalo S, Osterman K, Soini J. The role of external
transpedicular fixation in anterior interbody lumbar fusion. Journal of
Spinal Disorders 1996;9:433-8.
130. Torstensen T, Lunggren A, Meen H, et al. Efficiency and costs of
medical excercise therapy, conventional physiotherapy, and self-excercise
in patients ith chronic low back pain: A pragmatic, randomized, single-
blinded, controlled trial with 1-year follow-up. Spine 1998;23:2616-24.
131. Triano J, Hondras M, McGregor M. A comparison of outcome
measures for use with back pain patients: Results of a feasibility study. J
Manipulative Physiol Ther 1993;16:67-73.
132. Turk DC, Kerns RD, Rosenberg R. Effects of Marital Interaction On
Chronic Pain and Disability - Examining the Down Side of Social Support.
Rehabilitation Psychology 1992;37:259-74.
133. Turk DC, Marcus DA. Assessment of Chronic Pain Patients. Seminars
in Neurology 1994;14:206-12.
134. Turk DC, Okifuji A. Detecting Depression in Chronic Pain Patients -
Adequacy of Self-Reports. Behaviour Research and Therapy 1994;32:9-
16.
135. Turk DC, Okifuji A. Perception of traumatic onset, compensation
status, and physical findings: Impact on pain severity, emotional distress,
and disability in chronic pain patients. Journal of Behavioral Medicine
1996;19:435-53.
- 33 -
Oswestry and Roland-Morris
136. Turk DC, Okifuji A. Evaluating the role of physical, operant, cognitive,
and affective factors in the pain behaviors of chronic pain patients.
Behavior Modification 1997;21:259-80.
137. Turk DC, Okifuji A. What factors affect physicians' decisions to
prescribe opioids for chronic noncancer pain patients? Clinical Journal of
Pain 1997;13:330-6.
138. Turk DC, Okifuji A, Scharff L. Chronic Pain and Depression - Role of
Perceived Impact and Perceived Control in Different Age Cohorts. Pain
1995;61:93-101.
139. Turk DC, Okifuji A, Sinclair JD, Starz TW. Pain, disability, and physical
functioning in subgroups of patients with fibromyalgia. Journal of
Rheumatology 1996;23:1255-62.
140. Turk DC, Okifuji A, Sinclair JD, Starz TW. Interdisciplinary treatment
for fibromyalgia syndrome: Clinical and statistical significance. Arthritis
Care and Research 1998;11:186-95.
141. Turk DC, Okifuji A, Starz TW, Sinclair JD. Effects of type of symptom
onset on psychological distress and disability in fibromyalgia syndrome
patients. Pain 1996;68:423-30.
142. Tyrrell CT, Bruning PF, MayLevin F, et al. Pamidronate infusions as
single-agent therapy for bone metastases: A phase II trial in patients with
breast cancer. European Journal of Cancer 1995;31A:1976-80.
143. Underwood M, Barnett A, Vicker M. Evaluation of Two Time-Specific
Back Pain Outcome Measures. Spine 1999;24:1104-12.
- 34 -
144. Viikari-Juntura E, Takala EP. Standardized physical examination
protocol for low back disorders: Feasibility of use and validity of symptoms
and signs. Journal of Clinical Epidemiology 1998;51:245-55.
145. Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the Severity of
Chronic Pain. Pain 1992;50:133-49.
146. Von Korff M, Jensen P. Assessing global pain by self-report in clinical
and health services research. article in this edition of Spine
147. Werners R, Pynsent P, Bulstrode C. Randomised trial comparing
interferential therapy with motorised lumbar traction and massage in the
treatment of low back pain in a primary care setting. Spine 1999;24:1579-
84.
148. Wiesinger G, Nuhr M, Quittan M, et al. Cross-cultural adaption of the
Roland-Morris questionnaire for german-speaking patients with low back
pain. Spine 1999;24:1099-103.
149. Wise TN, Mann LS. Utilization of pain medications in hospitalized
psychiatric patients. General Hospital Psychiatry 1996;18:422-5.
150. Ylinen J, Ruuska J. Clinical Use of Neck Isometric Strength
Measurement in Rehabilitation. Archives of Physical Medicine and
Rehabilitation 1994;75:465-9
- 35 -
Oswestry and Roland-Morris
Appendix 1. The Roland-Morris Disability Questionnaire
When you back hurts, you may find it difficult to do some things you normally
do.
This list contains sentences that people have used to describe themselves
when they have back pain. When you read them, you may find that some
stand out because the describe you today. As you read the list, think of
yourself today. When you read a sentence that describes you today, put a
tick against it. If the sentence does not describe you, then leave the space
blank and go on to the next on. Remember, only tick the sentence if you are
sure it describes you today.
Scoring the RDQ. The score is the total number of items checked – i.e. from a minimum of 0 to a maximum of 24.
1. I stay at home most of the time because of my back.
2. I change position frequently to try and get my back comfortable.
3. I walk more slowly than usual because of my back.
4. Because of my back I am not doing any of the jobs that I usually do
around the house.
5. Because of my back, I use a handrail to get upstairs.
6. Because of my back, I lie down to rest more often.
7. Because of my back, I have to hold on to something to get out of an
easy chair.
- 36 -
8. Because of my back, I try to get other people to do things for me.
9. I get dressed more slowly then usual because of my back.
10. I only stand for short periods of time because of my back.
11. Because of my back, I try not to bend or kneel down.
12. I find it difficult to get out of a chair because of my back.
13. My back is painful almost all the time.
14. I find it difficult to turn over in bed because of my back.
15. My appetite is not very good because of my back pain.
16. I have trouble putting on my socks (or stockings) because of the pain
in my back.
17. I only walk short distances because of my back.
18. I sleep less well because of my back.
19. Because of my back pain, I get dressed with help from someone else.
20. I sit down for most of the day because of my back.
21. I avoid heavy jobs around the house because of my back.
22. Because of my back pain, I am more irritable and bad tempered with
people than usual.
23. Because of my back, I go upstairs more slowly than usual.
- 37 -
Appendix 2. Oswestry Disability Index (2.0)
Could you please complete this questionnaire It is designed to give us information as
to how your back (or leg) trouble has affected your ability to manage in everyday life.
Please answer every section. Mark one box only in each section that most closely
describes you today.
Section 1 - Pain intensity
I have no pain at the moment.
The pain is very mild at the moment.
The pain is moderate at the moment.
The pain is fairly severe at the moment.
The pain is very severe at the moment.
The pain is the worst imaginable at the moment.
Section 2 - Personal care (washing, dressing, etc.)
I can look after myself normally without causing extra pain.
I can look after myself normally but it is very painful.
It is painful to look after myself and I am slow and careful.
I need some help but manage most of my personal care.
I need help every day in most aspects of self care.
I do not get dressed, wash with difficulty and stay in bed.
Section 3 - Lifting
I can lift heavy weights without extra pain.
I can lift heavy weights but it gives extra pain.
Pain prevents me from lifting heavy weights off the floor but I can manage if they
are conveniently positioned, e.g. on a table.
- 39 -
Oswestry and Roland-Morris
Pain prevents me from lifting heavy weights but I can manage light to medium
weights if they are conveniently positioned.
I can lift only very light weights.
I cannot lift or carry anything at all.
Section 4 - Walking
Pain does not prevent me walking any distance.
Pain prevents me walking more than 1 mile.
Pain prevents me walking more than than of a mile.
Pain prevents me walking more than 100 yards.
I can only walk using a stick or crutches.
I am in bed most of the time and have to crawl to the toilet.
Section 5 - Sitting
I can sit in any chair as long as I like.
I can sit in my favourite chair as long as I like.
Pain prevents me from sitting for more than 1 hour.
Pain prevents me from sitting for more than an hour.
Pain prevents me from sitting for more than 10 minutes.
Pain prevents me from sitting at all.
Section 6 - Standing
I can stand as long as I want without extra pain.
I can stand as long as I want but it gives me extra pain.
Pain prevents me from standing for more than 1 hour.
Pain prevents me from standing for more than an hour.
Pain prevents me from standing for more than 10 minutes.
Pain prevents me from standing at all.
Section 7 - Sleeping
My sleep is never disturbed by pain.
My sleep is occasionally disturbed by pain.
Because of pain I have less than 6 hours sleep.
- 40 -
Because of pain I have less than 4 hours sleep.
Because of pain I have less than 2 hours sleep.
Pain prevents me from sleeping at all.
Section 8 - Sex life (if applicable)
My sex life is normal and causes no extra pain.
My sex life is normal but causes some extra pain.
My sex life is nearly normal but is very painful.
My sex life is severely restricted by pain.
My sex life is nearly absent because of pain.
Pain prevents any sex life at all.
Section 9 - Social life
My social life is normal and causes me no extra pain.
My social life is normal but increases the degree of pain.
Pain has no significant effect on my social life apart from limiting my more
energetic interests, e.g. sport, etc.
Pain has restricted my social life and I do not go out as often.
Pain has restricted social life to my home.
I have no social life because of pain.
Section 10 - Travelling
I can travel anywhere without pain.
I can travel anywhere but it gives extra pain.
Pain is bad but I manage journeys over two hours.
Pain restricts me to journeys of less than one hour.
Pain restricts me to short necessary journeys under 30 minutes.
Pain prevents me from travelling except to receive treatment
Scoring the ODI
For each section of 6 statements the total score is 5; if the first statement is
marked the score = 0; if the last statement is marked it = 5. Intervening
statements are scored according to rank. If more than one box is marked in
- 41 -
Oswestry and Roland-Morris
each section, take the highest score. If all 10 sections are completed the
score is calculated as follows:
Example: if 16 (total scored) out of 50 (total possible score) 100 = 32%
If one section is missed (or not applicable) the score is calculated:
Example:16 (total scored) / 45 (total possible score) 100 = 35.5%
So the final score may be summarised as:
(total score / (5 number of questions answered)) 100 %
We suggest rounding the percentage to a whole number for convenience.
- 42 -
Related Documents