The psyhician-patients relationship. Bartłomiej Drop, M.Sc.,PhD Chair and Department of Public Health Medical University of Lublin

The psyhician-patients relationship. Bartłomiej Drop, M.Sc.,PhD Chair and Department of Public Health Medical University of Lublin.
Dec 28, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

The psyhician-patients relationship.
Bartłomiej Drop, M.Sc.,PhDChair and Department of Public Health
Medical University of Lublin

What is Communication?
• The discipline of communication focuses on how people use messages to generate meanings within and across various contexts, cultures, channels, and media. The discipline promotes the effective and ethical practice of human communication.

Communication process

Communication process• Involves both a source (sender) and a receiver• Begins when sender has a thought or idea and wants to share it with one or more receivers.
Source: Person who encodes the message
Encoding: Words, Sounds, Colors, Space, Themes, Symbols, Pictures, Numbers, Gestures, Movement
Channel: Required for transmission , voice, gesture, newspaper, or other communication medium
Noise: Anything that interferes with, distorts, or slows the transmission of information. Message may not be received by the desired target audience
Receiver: Person who decodes the message.
Decoding: Interpretation of the language and symbols sent by the source through a channel.
Feedback: Interpersonal communicators get the receiver's response to a message directly.

Transactional Model of Communication
The transactional model of communication is a graphic representation of the collaborative and ongoing message exchange between individuals, or an individual and a group of individuals, with the goal of understanding each other. A communicator encodes (e.g., puts thoughts into words and gestures), then transmits the message via a channel (e.g., speaking, email, text message) to the other communicator(s) who then decode the message (e.g., take the words and apply meaning to them). The message may encounter noise (e.g., any physical, psychological, or physiological distraction or interference), which could prevent the message from being received or fully understood as the sender intended.

Verbal communicationHuman spoken and pictorial languages can be described as a
system of symbols and the grammars (rules) by which the symbols are manipulated. The word "language" also refers to common properties of languages. Language learning normally occurs most intensively during human childhood. Most of the thousands of human languages use patterns of sound or gesture for symbols which enable communication with others around them. Languages seem to share certain properties although many of these include exceptions. There is no defined line between a language and a dialect. Constructed languages such as Esperanto, programming languages, and various mathematical formalisms are not necessarily restricted to the properties shared by human languages. Communication is the flow or exchange of information within people or a group of people.

Nonverbal communicationNonverbal communication describes the process of conveying
meaning in the form of non-word messages. Some forms of non verbal communication include, haptics, gesture, body language or posture, facial expression and eye contact, object communication such as clothing, hairstyles, architecture, symbols, infographics, and tone of voice, as well as through an aggregate of the above. Speech also contains nonverbal elements known as paralanguage. These include voice lesson quality, emotion and speaking style as well as features such as rhythm, intonation and stress. Research has shown that up to 55% of human communication may occur through non verbal facial expressions, and a further 38% through paralanguage.[5] Likewise, written texts include nonverbal elements such as handwriting style, spatial arrangement of words and the use of emoticons to convey emotional expressions in pictorial form.

One-way and two-way communication
• Information flows only in one Information flows only in one
direction –from the sender to the direction –from the sender to the receiver with no feedbackreceiver with no feedback
• A much common way of A much common way of communication because it is faster communication because it is faster and easier for the sender and there and easier for the sender and there is no trouble from disagreement. is no trouble from disagreement.
• There may be mistakes in There may be mistakes in transmission of information.transmission of information.
One-way communication One-way communication

• A process in which A process in which information flows in two-information flows in two-directions –the receiver directions –the receiver provides feedback and the provides feedback and the sender receptive to the sender receptive to the feedback. feedback.
• It is more accurate and It is more accurate and fewer mistakes in fewer mistakes in transmission.transmission.
• But it is time-consuming and But it is time-consuming and more difficult for the more difficult for the sender. sender.
Two-way communicationTwo-way communication
One-way and two-way communication

Channels of communication
• Vertical communication channelsVertical communication channels::
• Lateral communication: Lateral communication:
© PhotoDisc

Channels of communication• Information passes downwards or Information passes downwards or
upwards in the organization.upwards in the organization.• Downward communication means that Downward communication means that
the manager tells employees about a the manager tells employees about a decision that has been already made. It decision that has been already made. It allows decisions to carried out quickly. allows decisions to carried out quickly.
• Upward communication refers to Upward communication refers to employees’ giving feedback to the employees’ giving feedback to the manager about the decision. It helps manager about the decision. It helps managers to understand employees’ managers to understand employees’ ideas on the decision.ideas on the decision.
Vertical communication Vertical communication

Channels of communication• People in the same People in the same
level within an level within an organization pass organization pass information to each information to each other.other.
• It can strengthen the It can strengthen the understanding and understanding and coordination between coordination between people in different people in different departments. departments.
Lateral communicationLateral communication

Areas within Communication Areas of emphasis differ from one institution to another, but those listed
below are some of the most common areas of study:
• Applied Communication - The study of how communication theory, research, and/or best practices help inform knowledge and theory about communication for practical issues.
• Communication Education - The study of communication in the classroom and other pedagogical contexts.
• Communication Theory - The study of principles that account for the impact of communication in human social interaction.
• Electronic Media - The study of radio, television, media technology, and web design with streaming audio and video.
• Health Communication - The study of communication as it relates to health professionals and health education, including the study of provider-client interaction, as well as the diffusion of health information through public health campaign

Communication in medicine

Doctor and Patient RelationshipFundamental Elements of the Patient-Physician Relationship
From ancient times, physicians have recognized that the health and well-being of patients depends upon a collaborative effort between physician and patient. Patients share with physicians the responsibility for their own health care. The patient-physician relationship is of greatest benefit to patients when they bring medical problems to the attention of their physicians in atimely fashion, provide information about their medical condition to the best of their ability, and work with their physicians in a mutually respectful alliance. Physicians can best contribute to this alliance by serving as their patients' advocate and by fostering these rights

1. The patient has the right to receive information from physicians and to discuss the benefits, risks, and costs of appropriate treatment alternatives. Patients should receive guidance from their physicians as to the optimal course of action. Patients are also entitled to obtain copies or summaries of their medical records, to have their questions answered, to be advised of potential conflicts of interest that their physicians might have, and to receive independent professional opinions.
2. The patient has the right to make decisions regarding the health care that is recommended by his or her physician. Accordingly, patients may accept or refuse any recommended medical treatment.
3. The patient has the right to courtesy, respect, dignity, responsiveness, and timely attention to his or her needs.
Patient rights

4. The patient has the right to confidentiality. The physician should not reveal confidential communications or information without the consent of the patient, unless provided for by law or by the need to protect the welfare of the individual or the public interest.
5. The patient has the right to continuity of health care. The physician has an obligation to cooperate in the coordination of medically indicated care with other health care providers treating the patient. The physician may not discontinue treatment of a patient as long as further treatment is medically indicated, without giving the patient sufficient opportunity to make alternative arrangements for care.
6. The patient has a basic right to have available adequate health care. Physicians, along with the rest of society, should continue to work toward this goal. Fulfillment of this right is dependent on society providing resources so that no patient is deprived of necessary care because of an inability to pay for the care. Physicians should continue their traditional assumption of a part of the responsibility for the medical care of those who cannot afford essential health care.

There is considerable healing power in the physician-patient alliance. A patient who entrusts himself to a physician's care creates ethical obligations that are definite and weighty. Working together, the potential exists to pursue interventions that can significantly improve the patient's quality of life and health status.

1. What is a fiduciary relationship?2. How has the physician-patient relationship evolved?3. Will the patient trust me if I am a student?4. How much of herself should the physician bring to the
physician-patient relationship? 5. What role should the physician's personal feelings and beliefs
play in the physician-patient relationship?6. What can hinder physician-patient communication?7. What happens when physicians and patients disagree?8. What can a physician do with a particularly frustrating
patient?9. When is it appropriate for a physician to recommend a
specific course of action or override patient preferences?10. What is the role of confidentiality?11. Would a physician ever be justified in breaking a law requiring
mandatory reporting?12. What happens when the physician has a relationship with
multiple members of a family?

General Rules About Physician-Patient Relationships
1. Patient is number one; always place the interests of the patient first.a. Choose the patient's comfort and safety over anyone else's.b. The goal is to serve the patient, not to worry about legal protection for thephysician.2. Always respond to the patient.a. Answer any question that is asked.b. Respond to the emotional as well as the factual content of questions.3. Tell the patient everything. even if he or she does not ask.a. Do not force a patient to hear bad news if he does not want it at thatmoment, but do try to discuss it with him or her as soon as possible.b. Information should flow through the patient to the family, not the reverse.c. If you have only partial information, say that it is partial, and tell what youknow.4. Work on long-term relationships with patients, not just short-term problems.a. Make eye contact.b. Defined touch: tell him or her what you are doing.c. Talk to patient, not colleagues: patient is always the focus.d. Arrange seating for comfortable, close communication.e. Shy away from large desks and tables.f. Both patient and physician should both be sitting if at all possible.

5. Listening is better than talking.a. Getting the patient to talk is generally better than having the physiciantalk.b. Take time to listen to the patient before you, even if other patients or colleaguesare waiting.6. Negotiate rather than order.a. Treatment choices are the result of agreement, not commands by thephysician.b. Remember, the patient makes medical decisions from the choices providedby the physician.7.Trust must be built. not assumed.a. Don't assume that the patient likes or trusts you.b. Treat difficult or suspicious patients in a friendly, open manner.8. Admit to the patient when you make a mistake.a. Take responsibility. Don't blame it on the nursing staff or on a medicalstudent.b. Admit the mistake even if it was corrected and the patient is fine.
General Rules About Physician-Patient Relationships

General Rules About Physician-Patient Relationships
9. Never "pass off" your patient to someone else.a. Refer to psychiatrist or other specialist when beyond your expertise (butusually not the case).b. Refer only for ophthalmology or related subspecialties.c. Provide instruction in aspects of care, e.g., nutrition, use of medications.10.Express empathy, then give control: "I'm sorry, what would you like to do?"a. Important when faced with a patient who is grieving or is angry.b. Important when faced with angry or upset family members.11. Agree on problem before moving to solution.a. Tell the patient your perceptions and conclusions about the conditionbefore moving to treatment recommendations.b. Informed consent requires the patient to fully understand what is wrong.c. Offering a correct treatment before the patient understands his or hercondition is wrong.12. Be sure you understand what the patient is talking about before intervening.a. Seek information before acting.b. When presented with a problem, get some details before offering a solution.c. Begin with open-ended questions, then move to closed-ended questions.

General Rules About Physician-Patient Relationships
13. Patients do not get to select inappropriate treatments.a. Patients select treatments, but only from presented, appropriate choices.b. If a patient asks for an inappropriate medication that he heard advertised,explain why it is not indicated and suggest an alternative.14. Be sure who your patient is.a. Is it the injured child, or the mother who brings him in? (the child)b. Is it your long-term patient who is now in a coma, or her husband? (thepatient)15. Never lie.a. Not to patients, their families, or insurance companies.b. Do not deceive to protect a colleague.16. Accept the health beliefs of patients.a. Be accepting of benign folk medicine practices. Expect them. Diagnosesneed to be explained in the way patients can understand, even if not technicallyprecise.c. Be careful about having young family members translate for elderlypatients.17. Accept patients' religious beliefs and participate if possible.a. Your goal is to make the patient comfortable. Religion is a source of comfortto many.b. Agrowing body of research suggests that patients who pray and are prayedfor have better outcomes.

General Rules About Physician-Patient Relationships
c. Ask about a patient's religions beliefs if you are not sure (but not as a preludeto passing off to the chaplain!).d. Of course, you are not expected to do anything against your own religiousor moral beliefs.18. Anything that increases communication is good.a. Take the time to talk with patients, even if others are waiting.b. Ask "why?"c. Seek information about the patient beyond the disease.19. Be an advocate for the patient.a. Work to get the patient what he or she needs.b. Never refuse to treat a patient because he or she cannot pay.20. The key is not so much what you do. but how you do it.a. The right choices are those that are humane and sensitive, and put theinterests of the patient first.b. Treat family members with courtesy and tact, but the wishes and interestsof the patient come first.
The key is not what physicians actually do, but what the most ideal physician should do.

Types of doctor-patient relationship

Paternalism
• Is widely regarded as the traditional form of doctor-patient relationship
• A passive patient and a dominant doctor

Parsons’ model
• Parson saw the doctor and patient as fulfilling necessary functions in a well balanced and maintained social structure
• Sickness is considered to be a necessary, occasional respite, providing a brief exemption for patient from social responsibilities

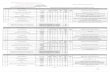
SOCIAL ROLES OF DOCTORS AND PATIENTSParsons’ model of the sick role and doctor’s role
Parsons (1951) was one of the earliest sociologists to examine the relationship between doctors and patients.
Parsons believed that the amount of illness is controlled through the socially roles for doctors and patients, which facilitate interaction, and ensure both parties work together to return people to a state of health and normal role performance as quickly as possible.
Parsons’ description of the roles of doctor and patient is presented as an ‘ideal type’ model. Parsons depicted the role of sick people as involving four general expectations.
First, sick people are allowed, and might even be required, to give up some of their normal activities and responsibilities, such as going to work or playing football.
Second, they are regarded as being in need of care. These two expectations and privileges are, however, contingent on the sick person fulfilling the third obligation of wanting to get well as quickly as possible, and the fourth of seeking professional medical advice and, most importantly for the doctor–patient relationship, cooperating with the doctor (Table ).

SOCIAL ROLES OF DOCTORS AND PATIENTSParsons’ model of the sick role and doctor’s role

SOCIAL ROLES OF DOCTORS AND PATIENTSParsons’ model of the sick role and doctor’s role
Summing up:
Doctor and patient position are coupled to each other, but it is strongly asymmetric system. The doctor has a dominant position.
Doctor has to follow three principles:- Universalism,- Emotional neutrality,- The specificity of function.
The object of therapy is a disease and not a person.
Your doctor authoritatively establish and maintain therapy. The doctor knowsbest what is best for the patient.
Patient has to submit to treatment requirements

Patient’s role
• When sick, a patient is allowed the privileges of convalescence-he or she is not held responsible for poor health and is excused from everyday responsibilities
• In order to enjoy these privileges, the patient must seek technically competent help and comply with medical advice
→passive and dependent

Doctor’s role
• The doctor legitimates the patient’s illness and determines the course of treatment.
• In doing so, the physician is compelled by professional ethics to act only in his or her sphere of expertise, to maintain an emotional detachment and distance from the patient, and to act in the patient’s best interest
→professionally dominant and autonomous

Advantages
• The supportive nature of paternalism appears to be all the more important when patient are very sick at their most vulnerable
• Relief from the burden of worry is curative in itself, and the trust and confident implied by this model allow doctor to perform “medical magic” →placebo

Disadvantages
• It is the potential for legitimate medical authority to be used for manipulation and exploitation of the vulnerable and ill that has fueled the ascendance of the autonomy doctrine to the preeminent bioethical value in patient-physician relationships.

Consumerism
• The patients’ challenge to unilateral decision making by physicians in reaching closure on diagnoses and working out treatment plans
• Reversing the very basic nature of the power relationship

Patient’s role
• Health shoppers
Indications of consumer behavior
• Cost-consciousness
• Information seeking
• Exercising independent judgment
• Consumer knowledge

Doctor’s role
• Health care providers
• Technical consultant
• To convince the necessity of medical services
• A tendency for the “consumer to be right”

Advantages
• Patients can have their own choices
• Medicine is not an accomplished science. There are tremendous gaps in knowledge. Indeed, it has been estimated that the effectiveness of treatment is unknown for about 90% of the medical condition seen in routine practice

Disadvantages
• Patients are being more selective in the acceptance of provider advice, based on its cost
• When things seem to go wrong, when satisfaction is low, or when a patient suspect less than optimal care or outcome, patients are more likely to question physician authority

Mutuality
• The optimal doctor-patient relationship model
• This model views neither the patient nor the physician as standing aside
• Each of participants brings strengths and resources to the relationship
• Based on the communication between doctors and patients

Patient’s role
• Patients need to define their problems in an open and full manner
• The patient’s right to seek care elsewhere when demands are not satisfactorily met

Doctor’s role
• Physicians need to work with the patient to articulate the problem and refine the request
• The physician’s right to withdraw services formally from a patient if he or she feels it is impossible to satisfy the patient’s demand

Advantages
• Patients can fully understand what problem they are coping with through physicians’ help
• Physicians can entirely know patient’s value
• Decisions can easily be made from a mutual and collaborative relationship

Disadvantages
• Physicians do not know what certain degree should they reach in communication
• If the communication is fake, both physicians and patients do not have mutual understanding, making decision is overwhelming to a patient

Default
• When patient and physician expectation are at odds, or when the need for change in the relationship cannot be negotiated, the relationship may come to a dysfunction standstill

Doctor-patient relationship in the past
• Paternalism
• Because physicians in the past are people who have higher social status
• “doctor” is seen as a sacred occupation which saves people’s lives
• The advices given by doctors are seen as paramount mandate

Doctor-patient relationship at present
• Consumerism and mutuality
• Patients nowadays have higher education and better economic status
• The concept of patient’s autonomy
• The ability to question doctors

Reasons for the change
• Doctors’ condition
• Patients’ condition
• Environmental factors

Conclusion
• Relationship between patients and doctors are often unstated, and thy are dynamic
• As conditions change, the kind of relationship that works best for a patient may change
• Doctors and patients should choose a “relationship fit”

The research tool was a survey carried out the patients of healthcare institutions in Lublin
The survey was conducted on a random sample of 100 individuals of both sexes and all ages.
SurveyMatherial and methods

Results
Respondents’ age was form 18 to 64 years old.
There were more young people (between 18-40 years old) in the group of respondents.








Conclusions
The study indicates that the majority of patients are not satisfied enough with their family doctors. They point to the lack of interest in their disease and not suitable communication. The most important things for the patients are: physician education, atmosphere in their office, and the way they cooperate each other. According to the respondents, these relationship sholuld be better.
In most cases respondents indicate a lack of agreement with the doctors. They are not happy with their health service. Respondents expect from their doctors mainly respect, commitment to work and their listening skills. Also suggest that they should be more interested in their disease. Most of the interviewed people think that there is a possibility to improve physician-patient relationships. The survey shows that relationships between patient - physician often are different from the models presented at books.

Doctor/Patient Relationship-Are the Surveys Accurate?
We have all seen them. You know…those charts showing us how satisfied patients are with the way their doctors communicate. Did your doctor listen to you? Did you doctor explain things in a way you could understand?
Funny thing about these charts, whether for they be for hospitals or doctor’s offices, is that 1)they never seem to change from year to year – 8O-90% of doctors communicate well with patients and 2)doctors’ communication are highly rated in patient satisfaction surveys at most if not all provider organizations.

The problem with satisfaction data related to doctor-patient communication is that, at face value, it simply doesn’t correlate with other published data on the subject. There is a “disconnect” between what patients say in satisfaction surveys and what happens in actual practice.

Here’s what I mean.Recent studies of hospitalized patients have shown that:
•68% to 85.3% of patients could not name the physician in charge of their care.
•43% to 58% of patients did not know the reason for their hospital admission.
•67% of patients received a new medication while hospitalized… yet 25% of these patients were unaware that they were given a new medication.
•90% of patients given a new medication reported never being told of adverse effects of the new medication.
•38% of patients were not aware of planned tests for the day.
The amazing thing was that majority of these patients (up to 58% in one study) said that their doctors always explained things in ways they could understand!

The same types of “disconnects” show up in satisfaction surveys done in doctor’s offices.
Studies of primary care physicians show that:
•Patients are interrupted by their physicians within the first 18 seconds of their opening statement during office visits
•Physicians and patients agree on the reason for the office visit only 50% to 70% of the time
•Physician underestimate the patient’s desire for health information in 65% of the time
•50% of patients walk out of their doctor’s office not understanding what their doctor told them to do
•Patient are not asked if they have any questions in up to 50% of office visits
Again, these same patients praised their physicians’ communication skills on one or another satisfaction survey instrument.

So What Explains The “Disconnect” Between How Physicians Actually Talk To Patients…And Patient Satisfaction?
Today’s high patient satisfaction scores are an artifact of the way we (when we become patients) have been “socialized” when it comes to a trip to the doctor’s office.
1) Beginning with childhood, we have all been socialized to assume the “sick role” when seeing the doctor. From our initial visits to the pediatrician with our Mom we quickly learned that the doctor is in charge and that our Mom’s role (and ours) is to sit passive by while the doctor does most of the talking. Notwithstanding all the “talk” about how empowered patients are today, most of us still assume the “sick role” when seeing our doctor.

2) Accustomed as most of us today are to the sick role, and accepting the fact that physicians are very busy, we are not surprised when doctors don’t seem to listen to us or interrupt us. We are not surprised that they don’t have time for all our questions or frown on us bringing in lists of things we have researched on the internet. This for most patients is what we are used to…it is what we are satisfied with given that most of us have don’t another or better point of comparison, i.e., a highly patient-centered physician.
3) Consistent with the sick role, we as patients “tend to be overly patient.” We “grant our doctors the benefit of every doubt.” Most of us begrudgingly put up with poor service, inconvenience, and unnecessary discomforts, until we can’t overlook it anymore. Even then we are reluctant to take our busy, overburdened doctor to task for these shortcomings by giving them a low score on a satisfaction survey.

The physician-family relationship also holds considerable healing power. The potential exists to pursue options that can improve the quality of life and health for the entire family.

Thank You
Related Documents