THE THE MEDIASTINUM MEDIASTINUM

The Mediastinum
Jan 04, 2016
The Mediastinum
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

THE THE MEDIASTINUMEDIASTINU
MM



The MediastinumThe Mediastinum


Subdivisions of the Mediastinum Subdivisions of the Mediastinum as seen in cross sectionas seen in cross section
• anterioranterior mediastinum (1) mediastinum (1)
• middlemiddle mediastinum (2) mediastinum (2)
• posteriorposterior mediastinum (3) mediastinum (3)

Anterior Superior Anterior Superior MediastinumMediastinum
• Thymus GlandThymus Gland• Aortic ArchAortic Arch• SVC ( Superior Vena Cava )SVC ( Superior Vena Cava )• Lymph NodesLymph Nodes• Parathyroid Gland Parathyroid Gland • Ectopic Thyroid TissueEctopic Thyroid Tissue

Middle MediastinumMiddle Mediastinum
• PericardiumPericardium• HeartHeart• Great VesselsGreat Vessels• Trachea and tracheal bifurcationTrachea and tracheal bifurcation• Main BronchiMain Bronchi• Phrenic NervesPhrenic Nerves• Hilar Lymph NodesHilar Lymph Nodes

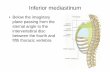
Posterior MediastinumPosterior Mediastinum
• EsophagusEsophagus• Vagus nervesVagus nerves• Sympathetic ChainSympathetic Chain• Thoracic ductThoracic duct• Descending thoracic aortaDescending thoracic aorta• Azygos veinAzygos vein• Hemiazygos veinHemiazygos vein• Paravertebral lymph nodesParavertebral lymph nodes


DiagnosticsDiagnostics
• Chest X-RaysChest X-Rays• CT ( Computed Tomography)CT ( Computed Tomography)• MRIMRI• CT guided needle biopsyCT guided needle biopsy FNAB vs CoreFNAB vs Core• Mediastinoscopy with biopsyMediastinoscopy with biopsy• VATSVATS• Radionuclide ScanningRadionuclide Scanning• AngiographyAngiography










MEDIASTINAL TUMORS MEDIASTINAL TUMORS AND CYSTSAND CYSTS
• Adults - 25-35% malignantAdults - 25-35% malignant
neurogenic tumors most neurogenic tumors most common common
( 20% )( 20% )
thymomas, congenital cysts, thymomas, congenital cysts,
lymphomaslymphomas• Children - 25-45% malignantChildren - 25-45% malignant
lymphomas, neurogenic lymphomas, neurogenic tumorstumors

SYMPTOMATOLOGYSYMPTOMATOLOGY
• 1/3 - ½ asymptomatic; in adults 1/3 - ½ asymptomatic; in adults correlatescorrelates
with malignancywith malignancy• Nonspecific Nonspecific chest pain, cough, dyspnea chest pain, cough, dyspnea ( COMPRESSION symptoms )( COMPRESSION symptoms )• Endocrine symptomsEndocrine symptoms Hypertension – pheochromocytomaHypertension – pheochromocytoma Hypercalcemia – parathyroid tumorHypercalcemia – parathyroid tumor Thyrotoxicosis – intrathoracic goiterThyrotoxicosis – intrathoracic goiter Gynecomastia - choriocarcinomaGynecomastia - choriocarcinoma

THYMOMATHYMOMA
• MOST COMMON anterior mediastinal MOST COMMON anterior mediastinal mass in adults; rare in childrenmass in adults; rare in children
• 1/3 asymptomatic at diagnosis1/3 asymptomatic at diagnosis• Symptoms: Symptoms:
Mass effectsMass effects
Systemic effects due to Systemic effects due to paraneoplasticparaneoplastic
syndromes ( Myasthenia gravis )syndromes ( Myasthenia gravis )




THYMOMATHYMOMA
• Myasthenia gravis – seen in 10-50% of Myasthenia gravis – seen in 10-50% of patients with thymomas; conversely, patients with thymomas; conversely, thymomas seen in only 8-15% of patients thymomas seen in only 8-15% of patients with Myasthenia graviswith Myasthenia gravis
• Histopathology – based on proportion of Histopathology – based on proportion of lymphocytes to epithelial elementslymphocytes to epithelial elements
• Malignancy is based on invasive character Malignancy is based on invasive character – presence of capsular or vascular invasion– presence of capsular or vascular invasion
• Treatment: surgeryTreatment: surgery radiation / chemotherapyradiation / chemotherapy

GERM CELL TUMORSGERM CELL TUMORS
• Primary EXTRA-gonadal germ cell Primary EXTRA-gonadal germ cell tumors are RAREtumors are RARE
• 1% of all mediastinal tumors1% of all mediastinal tumors• Most common in the anterior Most common in the anterior
mediastinummediastinum• Usually in young adults; male to Usually in young adults; male to
female ration is 4:1female ration is 4:1

GERM CELL TUMORSGERM CELL TUMORS
• SeminomaSeminoma• Embryonal cell carcinomaEmbryonal cell carcinoma• ChoriocarcinomaChoriocarcinoma• Malignant teratomaMalignant teratoma• Endodermal yolk sac tumorEndodermal yolk sac tumor

GERM CELL TUMORSGERM CELL TUMORS• Role of tumor markersRole of tumor markers B-HCGB-HCG A-fetoproteinA-fetoprotein Carcinoembryonic antigen ( CEA )Carcinoembryonic antigen ( CEA )• Diagnosis: CT scanDiagnosis: CT scan• Treatment: attempt complete resectionTreatment: attempt complete resection adjuvant therapyadjuvant therapy Seminomas – radiosensitive; Seminomas – radiosensitive;
betterbetter prognosisprognosis Other tumors - ?chemotherapyOther tumors - ?chemotherapy





LYMPHOMASLYMPHOMAS
• Mediastinal involvement seen in 50% of Mediastinal involvement seen in 50% of both Hodgkin’s and non-Hodgkin’s both Hodgkin’s and non-Hodgkin’s lymphomalymphoma
• MOST COMMON mediastinal malignancyMOST COMMON mediastinal malignancy• Most commonly seen in the anterior Most commonly seen in the anterior
mediastinummediastinum• Symptoms – cough feverSymptoms – cough fever
chest pain weight chest pain weight lossloss

LYMPHOMASLYMPHOMAS
• Diagnosis - Chest x-ray and CT ScanDiagnosis - Chest x-ray and CT Scan
Mediastinotomy / Mediastinotomy / mediastinoscopy mediastinoscopy
with biopsywith biopsy• Treatment – radiotherapyTreatment – radiotherapy
chemotherapychemotherapy
surgery – mainly for surgery – mainly for diagnosisdiagnosis



TERATOMASTERATOMAS
• Mostly in adolescents; 80-85% are Mostly in adolescents; 80-85% are benignbenign
• Originate from branchial cleft pouchOriginate from branchial cleft pouch• Contain all 3 germ layers: endoderm, Contain all 3 germ layers: endoderm,
mesoderm and ectodermmesoderm and ectoderm• Many are asymptomatic; others have Many are asymptomatic; others have
symptoms related to compressionsymptoms related to compression• Smooth-walled cystic or solid lesions on Smooth-walled cystic or solid lesions on
x-ray pr CT Scanx-ray pr CT Scan• Treatment: total surgical excisionTreatment: total surgical excision

MIDDLE MEDIASTINAL MIDDLE MEDIASTINAL LESIONSLESIONS
• Usually cysticUsually cystic• 2 most common lesions – pericardial cyst2 most common lesions – pericardial cyst bronchogenic cystbronchogenic cyst• Pericardial cyst – usually asymptomatic; Pericardial cyst – usually asymptomatic;
found on chest x-ray, at cardiophrenic angle; found on chest x-ray, at cardiophrenic angle; surgery is both diagnostic and therapeuticsurgery is both diagnostic and therapeutic
• Bronchogenic cyst – usually arise posterior to Bronchogenic cyst – usually arise posterior to the carina; may be asymptomatic or may the carina; may be asymptomatic or may cause compression symptoms; treated by cause compression symptoms; treated by excisionexcision







POSTERIOR MEDIASTINAL POSTERIOR MEDIASTINAL LESIONS LESIONS
• Mostly neurogenic lesions, along the Mostly neurogenic lesions, along the paravertebral gutterparavertebral gutter
• Up to 25% are malignantUp to 25% are malignant• 75% occur in children less than age 4; higher 75% occur in children less than age 4; higher
probability of malignancyprobability of malignancy• Common histologic typesCommon histologic types Neurilemomas – from Schwann cellsNeurilemomas – from Schwann cells Neurofibromas – can become malignantNeurofibromas – can become malignant NeurosarcomasNeurosarcomas Ganglioneuromas – from sympathetic gangliaGanglioneuromas – from sympathetic ganglia Neuroblastomas – also from sympathetic chainNeuroblastomas – also from sympathetic chain

POSTERIOR MEDIASTINAL POSTERIOR MEDIASTINAL LESIONS LESIONS
• Pheochromocytomas may occur rarely; Pheochromocytomas may occur rarely; behave similarly to adrenal lesionsbehave similarly to adrenal lesions
• Symptoms – chest painSymptoms – chest pain spinal cord compressionspinal cord compression endocrine symptomsendocrine symptoms neuroblastoma – fever, neuroblastoma – fever,
vomiting,vomiting, diarrhea, coughdiarrhea, cough• Treatment: surgicalTreatment: surgical radiotherapy for malignant radiotherapy for malignant
lesionslesions

SUPERIOR VENA CAVA SUPERIOR VENA CAVA SYNDROMESYNDROME
• 85% of cases are due to Bronchogenic CA85% of cases are due to Bronchogenic CA
( most commonly small cell type – 40% )( most commonly small cell type – 40% )• Other causes – mediastinal tumorsOther causes – mediastinal tumors
fibrosing mediastinitisfibrosing mediastinitis
thoracic aortic aneurysmthoracic aortic aneurysm
SVC thrombosis due to SVC thrombosis due to
catheterization / instrumentationcatheterization / instrumentation

SUPERIOR VENA CAVE SUPERIOR VENA CAVE SYNDROMESYNDROME
• Presents as venous distension, facial edema, Presents as venous distension, facial edema, plethora, headache, respiratory symptomsplethora, headache, respiratory symptoms
• Diagnosis – confirmed by CT ScanDiagnosis – confirmed by CT Scan• Treatment – usually palliative radiation or Treatment – usually palliative radiation or chemotherapychemotherapy ?steroids ?diuretics?steroids ?diuretics role of surgery – for benign lesionsrole of surgery – for benign lesions ( bypass or vein reconstruction )( bypass or vein reconstruction ) endovascular procedures - stentingendovascular procedures - stenting






MEDIASTINITISMEDIASTINITIS• Acute vs Chronic infectionAcute vs Chronic infection• Acute infectionAcute infection Fulminant infection with high morbidity andFulminant infection with high morbidity and mortalitymortality RAPID spread through areolar planes, withinRAPID spread through areolar planes, within 24 hours, to involve neck and lungs24 hours, to involve neck and lungs Both Gram (+) and (-) bacteriaBoth Gram (+) and (-) bacteria Esophageal or tracheal perforation; open Esophageal or tracheal perforation; open
heart heart surgery – more indolent course; usually surgery – more indolent course; usually
due to due to Staphylococcus ( MRSA )Staphylococcus ( MRSA )

ACUTE MEDIASTINITISACUTE MEDIASTINITIS
• Symptoms – chest pain, dysphagia, Symptoms – chest pain, dysphagia, respiratory distress, subcutaneous respiratory distress, subcutaneous crepitationcrepitation
• Diagnosis – chest x-rayDiagnosis – chest x-ray
water soluble contrast studywater soluble contrast study• Treatment – must be early and aggressiveTreatment – must be early and aggressive
hydration, drainage, control ofhydration, drainage, control of
primary problemprimary problem

CHRONIC CHRONIC MEDIASTINITISMEDIASTINITIS
• Chronic fibrosing mediastinitisChronic fibrosing mediastinitis
Chronic fibrosis and Chronic fibrosis and inflammationinflammation
Usually due to granulomatous Usually due to granulomatous infectioninfection
( TB, Histoplasmosis )( TB, Histoplasmosis )



Related Documents