Copyright © 2011 Cornetis; www.cornetis.com.pl PRACE ORYGINALNE / Original articles Dermatologia Kliniczna 2011, 13 (1): 5-8 ISSN 1730-7201 5 The many faces of fixed drug eruptions Wiele twarzy rumienia trwałego Olayinka Abimbola Olasode Department of Dermatology, Obafemi Awolowo University, Ile Ife, Osun state, Nigeria ABSTRACT Fixed drug eruption (FDE) is a form of presentation of recurrent cutaneous drug reaction characterized by appearance of single or multiple erythematous annular hyperpigmented macules/patch or bullae that appears each time at the same site whenever the offending drug is used. The lesion heals each time with typical post inflammatory hyperpigmentation. Diagnosis is based on drug history, drug associated excercebations and remissions, clinical presentations of typical polycyclic lesions with lack of systemic symptoms, drug challenge, skin tests and histology of skin biopsy. Diagnosis may not always easy. Unu- sual and atypical cases of FDE have been reported to raise awareness and raise index of suspicion in non classical or altered lesions. We report seven different presentations of Fixed Drug eruptions in a Nigerian population presenting in our skin clinic. The possibility of variant lesions occurring in Fixed Drug Erup- tions is hereby highlighted. Typical lesions of FDE can be altered secondarily by chronicity and applica- tion of some topical agents before the patient presents making correct diagnosis difficult. We suggest that attending dermatologist be aware and have these unusual presentations of FDE in mind while ma- king a diagnosis. The role of detailed accurate and precise history taking in these cases cannot be ove- remphasized. Key words: diagnosis, drug eruptions STRESZCZENIE Rumień trwały polekowy (fixed drug eruption, FDE) jest jedną ze skórnych reakcji niepożądanego działa- nia leków. Nierzadko ma charakter zmian nawracających. Może mieć postać pojedynczych lub wielo- ogniskowych rumieniowych plam o kształcie pierścieniowym, często z pęcherzem. Cechą charaktery- styczną jest występowanie zmian skórnych za każdym razem w tym samym miejscu po zastosowaniu prowokującego leku. Zmiany ustępują z pozostawieniem charakterystycznego pozapalnego przebar- wienia. Rozpoznanie oparte jest na wywiadzie, tj. ustaleniu, że do nasilenia lub wystąpienia zmian do- chodzi po przyjęciu prowokującego powstanie zmian leku. Charakterystyczny jest również obraz klinicz- ny, czyli obecność policyklicznych zmian rumieniowych, oraz brak objawów ogólnych; pomocne może być badanie histologiczne zmian skórnych. Rozpoznanie czasem może być utrudnione, z uwagi na nie- typowy obraz kliniczny. Nietypowe odmiany FDE są coraz częściej opisywane. Publikacje te podnoszą świadomość lekarzy i ułatwiają rozpoznawanie w wielu przypadkach FDE. W pracy przedstawiono sie- dem przypadków FDE obserwowanych w klinice dermatologii Obafemi Awolowo University (Nigeria). Zwrócono uwagę na różne odmiany FDE. Autorzy zauważyli, że na zmianę obrazu klinicznego może mieć wpływ zarówno przewlekłe stosowanie prowokujących leków, jak też leczenie miejscowe. Autorzy zasugerowali, aby brać pod uwagę nietypowe odmiany kliniczne FDE. Jednocześnie szczególnie przy podejrzeniu FDE bardzo duże znaczenie ma szczegółowy wywiad. Słowa kluczowe: diagnostyka, skórne reakcje polekowe Address for correspondence: Dr Olayinka Abimbola Olasode MBBCh, FWACP, FACP Consultant Physician/Dermatologist Department of Dermatology, Obafemi Awolowo University, Ile Ife Osun state, Nigeria e-mail: [email protected] Introduction There is a wide variety of morphological patterns of cutaneous drug reactions among which are Fixed Drug Eruptions (FDE).Typical lesions of FDE are annular recurrent hyperpigmented erythemato- us bordered sometimes bullous lesions (fig. 1, 2). Typical history of recurrence and association with offending drugs helps the clinician in diagnosis. Patients intrigued by these typical acute lesions seek medical consultation quickly. However, late presentations, misdia- gnosis of original lesions or application of irritant topical therapy for cure may alter the original lesions making subsequent diagnosis difficult. This is likely to occur in areas where access to medical or

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Copyright © 2011 Cornetis; www.cornetis.com.pl
PRACE ORYGINALNE / Original articlesDermatologia Kliniczna 2011, 13 (1): 5-8
ISSN 1730-7201
5
The many faces of fixed drug eruptions Wiele twarzy rumienia trwałego
Olayinka Abimbola Olasode Department of Dermatology, Obafemi Awolowo University, Ile Ife, Osun state, Nigeria
ABSTRACT Fixed drug eruption (FDE) is a form of presentation of recurrent cutaneous drug reaction characterized by appearance of single or multiple erythematous annular hyperpigmented macules/patch or bullae that appears each time at the same site whenever the offending drug is used. The lesion heals each time with typical post inflammatory hyperpigmentation. Diagnosis is based on drug history, drug associated excercebations and remissions, clinical presentations of typical polycyclic lesions with lack of systemic symptoms, drug challenge, skin tests and histology of skin biopsy. Diagnosis may not always easy. Unu-sual and atypical cases of FDE have been reported to raise awareness and raise index of suspicion in non classical or altered lesions. We report seven different presentations of Fixed Drug eruptions in a Nigerian population presenting in our skin clinic. The possibility of variant lesions occurring in Fixed Drug Erup-tions is hereby highlighted. Typical lesions of FDE can be altered secondarily by chronicity and applica-tion of some topical agents before the patient presents making correct diagnosis difficult. We suggest that attending dermatologist be aware and have these unusual presentations of FDE in mind while ma-king a diagnosis. The role of detailed accurate and precise history taking in these cases cannot be ove-remphasized.
Key words: diagnosis, drug eruptions
STRESZCZENIE
Rumień trwały polekowy (fixed drug eruption, FDE) jest jedną ze skórnych reakcji niepożądanego działa-nia leków. Nierzadko ma charakter zmian nawracających. Może mieć postać pojedynczych lub wielo-ogniskowych rumieniowych plam o kształcie pierścieniowym, często z pęcherzem. Cechą charaktery-styczną jest występowanie zmian skórnych za każdym razem w tym samym miejscu po zastosowaniu prowokującego leku. Zmiany ustępują z pozostawieniem charakterystycznego pozapalnego przebar-wienia. Rozpoznanie oparte jest na wywiadzie, tj. ustaleniu, że do nasilenia lub wystąpienia zmian do-chodzi po przyjęciu prowokującego powstanie zmian leku. Charakterystyczny jest również obraz klinicz-ny, czyli obecność policyklicznych zmian rumieniowych, oraz brak objawów ogólnych; pomocne może być badanie histologiczne zmian skórnych. Rozpoznanie czasem może być utrudnione, z uwagi na nie-typowy obraz kliniczny. Nietypowe odmiany FDE są coraz częściej opisywane. Publikacje te podnoszą świadomość lekarzy i ułatwiają rozpoznawanie w wielu przypadkach FDE. W pracy przedstawiono sie-dem przypadków FDE obserwowanych w klinice dermatologii Obafemi Awolowo University (Nigeria). Zwrócono uwagę na różne odmiany FDE. Autorzy zauważyli, że na zmianę obrazu klinicznego może mieć wpływ zarówno przewlekłe stosowanie prowokujących leków, jak też leczenie miejscowe. Autorzy zasugerowali, aby brać pod uwagę nietypowe odmiany kliniczne FDE. Jednocześnie szczególnie przy podejrzeniu FDE bardzo duże znaczenie ma szczegółowy wywiad.
Słowa kluczowe: diagnostyka, skórne reakcje polekowe
Address for correspondence:Dr Olayinka Abimbola Olasode
MBBCh, FWACP, FACP
Consultant Physician/Dermatologist
Department of Dermatology,
Obafemi Awolowo University, Ile Ife
Osun state, Nigeria
e-mail: [email protected]
Introduction
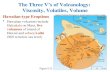
There is a wide variety of morphological patterns of cutaneous drug reactions among which are Fixed Drug Eruptions (FDE).Typical lesions of FDE are annular recurrent hyperpigmented erythemato-us bordered sometimes bullous lesions (fig. 1, 2). Typical history of
recurrence and association with offending drugs helps the clinician in diagnosis. Patients intrigued by these typical acute lesions seek medical consultation quickly. However, late presentations, misdia-gnosis of original lesions or application of irritant topical therapy for cure may alter the original lesions making subsequent diagnosis difficult. This is likely to occur in areas where access to medical or
Dermatologia Kliniczna 2011, 13 (1)Olayinka Abimbola Olasode The many faces of fixed drug eruptions
6
expert dermatology care is limited or where the initial lesions have been altered by over the counter medications.
Clinical Presentations
Cases presented at a dermatology clinic of a teaching hospital and were seen by an attending dermatologist. Demographic data, drug history, family history and past medical history were documented. The initial presenting lesions and their progress were described by the patients. Previous topical therapy applied was recorded. Diagnosis was based on history, clinical findings and recurrence of lesions associated with offending drug at same site. Skin biopsy was used to confirm doubtful cases. Pictures of lesions were taken.
Results
See table I and figures 1-7.
Table I: Clinical presentations in patients with diagnosis of FDE presenting in a dermatology clinic, Obafemi Awolowo University, Ile Ife, Osun State, Nigeria
Tabela I: Objawy kliniczne u pacjentów z FDE leczonych w klinice dermatologicznej, Obafemi Awolowo University, Ile Ife, Osun State, Nigeria
Figures Rycina
Age[in years]
Wiek pacjenta [w latach]
SexPłeć
Offending drugLek powodujący zmiany
Initial lesionRodzaj pierwot-
nych zmian
DurationCzas trwania
Clinic presentationObraz kliniczny
1 20 F SulphonamideSulfonamidy
MaculePlama
6 months6 miesięcy
Hyperpigmented maculesHiperpigmentowane plamy
2 4 F SulphonamideSulfonamidy
BullaePęcherze
4 weeks4 tygodnie
BullaePęcherze
3 55 F ParacetamolParacetamol
MaculePlama
9 months9 miesięcy
Hyperpigmented patchHiperpigmentowane blaszki
4 32 M SulphonamideSulfonamidy
MaculePlama
8 months8 miesięcy
Facial hyperpigmentationHiperpigmentacja twarzy
5 40 M SulphonamideSulfonamidy
BullaePęcherze
10 months10 miesięcy
Hyperkeratotic lesionsHiperkeratotyczne zmiany
6 42 M TetracyclineTetracyklina
BullaePęcherze
2 years2 lata
Lichenified depigmentationOdbarwienia i lichenifikacja
7 36 F SulphonamideSulfonamidy
MaculePlama
2 years2 lata
Vitiligo like lesionsZmiany typu bielactwa nabytego
F – female / kobieta, M – men / mężczyzna
Fig. 1. Typical polycyclic hyperpigmented macule of FDERyc. 1. Typowe policykliczne przebarwienia w przebiegu FDE
Fig. 2. Typical bullous lesion of FDE on the abdomen in a 4-year-oldRyc. 2. Typowe pęcherze w przebiegu FDE na skórze brzucha
u 4-letniego chłopca
Fig. 3. Flexural hyperpigmented lesion of FDE with erythematous borders limited to neck area
Ryc. 3. Przebarwienia w okolicach zgięciowych z rumieniową granicą ograniczone do okolicy szyi
7
Olayinka Abimbola Olasode Wiele twarzy rumienia trwałego
Discussion
An adverse drug reaction is any unintended or undesirable re-sponse to a medication given at an appropriate dose [1]. Any organ may exhibit an allergic reaction, but the skin is commonly affected because it has both metabolic and immunologic functions. Clinical and morphological approaches as well as cutaneous biopsy and histology may be necessary to make a diagnosis of cutaneous drug reactions. Histology can distinguish between a drug-induced dise-ase and other diseases but it does not allow for identification of the causative drug. Often the causative agent is made out from the pa-tient’s history; in some cases, oral challenge or topical testing may be required.
Fixed drug eruption (FDE) is characterized by the development of recurrent site-specific lesions on the skin and/or mucosa during treatment with the drug responsible. Fixed drug eruptions repre-sent an immunologic cutaneous reaction to a systemic medication. Cell-mediated, rather than humoral immunity is thought to be in-volved in the pathophysiology of FDE [2]. Drugs that have been as-sociated with FDE include phenolphthalein, sulfonamides, phenyl-butazone, barbiturates, dapsone, chlordiazepoxide, indomethacin, quinine, salicylates and tetracyclines [3]. Typical Fixed drug erup-tions have been documented in Nigeria. Olumide [4] observed FDE among patients being treated with pyrazolone analgesic and ben-zodiazepine in Lagos, Nigeria.
FDE manifest as well circumscribed eczematous or bullous le-sions on the skin and heals with residual hyperpigmentation (fig. 1, 2). Various and atypical morphological patterns of fixed drug eruption have been described in various studies [5, 6]. Fixed drug eruption has been documented to mimick lichen planus, erythema multiforme, Steven Johnson syndrome, paronychia, cheilitis, pso-riasis, housewife dermatitis, melasma, lichen planus actinicus, disco-id lupus erythematosus, erythema annulare centrifugum, pemphi-gus vulgaris, chilblains, pityriasis rosea and vulval and perianal hy-permelanosis [5, 6]. Similar diagnostic challenges are yet to be docu-mented in literature in Nigeria. This paper describes some atypical presentations of FDE presenting at a skin clinic in Western Nigeria.
FDE with Pigmentary loss
Figures 6 and 7 both show pigmentary loss in their secondary le-sions after 2 years of recurrence. There is primary loss of pigmenta-tion with attempt at follicular repigmentation case presented in fi-
Fig. 4. Multiple thick facial hyperpigmented lesions of FDERyc. 4. Wieloogniskowe obrzękowe przebarwienia na twarzy
w przebiegu FDE
Fig. 7. Solitary vitiligo like lesion with perifollicular repigmentation following FDE on the thigh
Ryc. 7. Pojedyncze ognisko przypominające bielactwo nabyte z repig -mentacją przymieszkową powstałe na udzie w przebiegu FDE
Fig. 6. Lesion with post inflammatory depigmentation following itchy bullous lesions of FDE
Ryc. 6. Zmiana z pozapalnym odbarwieniem w miejscu swędzących pęcherzy w przebiegu FDE
Fig. 5. Multiple hyperkeratotic lesions following initial bullous lesions of FDE on the back
Ryc. 5. Wieloogniskowe hiperkeratotyczne zmiany w przebiegu FDE powstałe w miejscu pęcherzy na plecach
Dermatologia Kliniczna 2011, 13 (1)Olayinka Abimbola Olasode The many faces of fixed drug eruptions
8
perivascular infiltrate. There are also neutrophils and melanopha-ges, indicative of repeat injury at the dermoepidermal junction. How ever, occasionally, early lesions may show epidermal spongio-sis, dermal edema, neutrophilic microabscesses, and dermal eosi-nophils.
Conclusion
Atypical and secondary lesions can be a diagnostic challenge to an otherwise simple straightforward diagnosis. The patient must be able to adequately describe the original primary lesion, the pro-gression, aggravating and relieving factors. Yet an accurate diagno-sis is essential for appropriate therapy. In chronic and altered lesions histology may not be totally exclusive. An experienced dermatolo-gist knows the value of detailed history of a skin lesion for diagno-sis. Late presentations of skin lesions can occur where there are too few/no dermatologists or long appointments before a patient is seen. Application of topical agents which are easily available over the counter may alter the presenting lesion. All these conditions are present in the developing world. There is a need to increase our awareness that fixed drug eruptions come in different clinical forms. It is well known that drug eruptions can mimic a wide range of skin conditions. Attention is being drawn to drug induced der-matosis mimicry.
References
1. Anderson J.A., Adkinson N.F.Jr.: Allergic reactions to drugs and biologic agents. JAMA, 1987, 258, 2891-2899.
2. Smoller B.R., Luster A.D., Krane J.F., et al.: Fixed drug eruptions: evidence for a cytokine mediated process. J. Cutan. Pathol., 1991, 18, 13-19.
3. Lee A., Thomas S.H.L.: Adverse drug reactions. Churchill Livingstone. 4. Olumide Y.: Fixed drug eruption: a lesson in drug usage. Int. J. Dermatol.,
1979, 18, 818-821. 5. Thankappan T.P., Zachariah J.: Drug specific clinical pattern in fixed drug
eruption. Int. J. Dermatol., 1991, 30, 867-870. 6. Sehgal V.N., Gangwani O.P.: Fixed drug eruption: Current concepts. Int.
J. Dermatol., 1987, 26, 67-74. 7. Dereure O., Guilhou J.J.: Non Pigmenting fixed drug eruption: a new case
due to betahistine. Dermatology, 1996, 193, 248-250. 8. Shelley W.B., Shelley E.D.: Non pigmenting fixed drug eruption as a distinc-
tive pattern: examples caused by sensitivity to pseudoephedrine hydrochlo-ride and tetrahydrozoline. J. Am. Acad. Dermatol., 1987, 17, 403-407.
9. Guin J.D., Baker G.F.: Chronic fixed drug eruption caused by acetamino-phen. Cutis, 1988, 41,106-108.
10. Mukhyaprana Prabhu, Smitha Prabhu, Pranay Mishra, et al.: Cellulitis-like fixed drug eruption attributed to paracetamol (acetaminophen). Dermatol. Online J., 2005, 11, 24.
11. Dar N.R., Masood S., Mustafvi S.A.: Reticulated multifocal fixed drug erup-tion due to mefenamic acid: a new morphologic pattern. J. Coll. Physician Surg. Pak., 2005, 15, 562-563.
12. Wolf R., Brenner S., Krakowski A.: Intertriginous drug eruption. Acta Derm. Venereol., 1992, 72, 441-442.
Received: 2010.12.02. Approved: 2011.02.23.
gure 7. In figure 6, the initial lesion is typical FDE healing with hyper-pigmentation with secondary depigmentation in the middle of the lesion. Pigmentary loss can be post inflammatory or local loss of melanocytes. In literature non pigmenting subset of FDE is a di-stinctive, clinically recognizable entity. Characteristically, the le-sions are large, symmetrical, well-circumscribed tender erythema-tous plaques that suddenly appear and reappear in exactly the same sites. They fade without pigmentation or any other trace over a 2- to 3-week period [7]. Shelley and Shelley [8] described three examples of this overlooked non pigmenting fixed drug reaction pattern. These presentations can be overlooked but management requires recognition and avoidance of implicated drugs. The le-sions described in figures 6 and 7 do not fit into the picture of non pigmentary FDE but are a different variant actually with loss of pig-ment and attempt at repigmentation.
Chronic lesions of FDE
Chronic forms of FDE presentations have also been described. A case of chronic fixed drug eruption resembling parapsoriasis was reported, which presented with persistent, stable lesions that were present for seven months before the diagnosis was established [9]. Chronic alteration of lesions can result from scratching lesions, ulce-ration, superadded bacterial infections, application of irritants, and healing with lichenification. Lichenification is thickened and rough skin characterized by rough skin due to repeated rubbing. Repe-ated injury to the skin can result in this picture (fig. 5). This is indeed a challenge to diagnosis of the primary lesion. Chronicity may alter typical lesions of FDE.
Other variants of FDE
A case of biopsy-confirmed fixed drug eruption (FDE) associated with paracetamol and presenting like cellulites was reported by Prabhu, et al. [10]. Another unique morphology of widespread mul-tifocal fixed drug eruption showing a reticulated and bullous pat-tern caused by mefenamic acid was reported by another group [11]. Attention has been drawn drug eruptions confined to the intertri-genous areas [12]. Other presentations include a wandering fixed drug eruption in which the lesion keeps on changing its position and giant fixed drug eruption [11].
Confirming diagnosis of FDE
Drug rechallenge in FDE is a reliable method of identifying cau-sative drugs, but increasingly the use of skin tests has gained the at-tention of investigators.
Histopathology in FDE
The histopathology in typical FDE is lichenoid dermatitis. The ac-companying inflammatory cell infiltrate is a superficial and deep
Related Documents