Pediatric Critical Care Telemedicine in a Rural Underserved Area Barry Heath, MD; 1 Richard Salerno, MD, MS; 1 Jeremy Hertzig, MD; 2 Michael Caputo, MS 3 . 1 Division of Pediatric Critical Care Medicine, Department of Pediatrics, University of Vermont College of Medicine, 2 Department of Pediatrics, University of Vermont College of Medicine, 3 Central Information Technology Services, Washington University at St. Louis School of Medicine. The authors have no financial disclosures.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Pediatric Critical Care Telemedicine in a Rural Underserved Area
Barry Heath, MD;1 Richard Salerno, MD, MS;1 Jeremy Hertzig, MD;2 Michael Caputo, MS3.
1Division of Pediatric Critical Care Medicine, Department of Pediatrics, University of Vermont College of Medicine, 2Department of Pediatrics, University of Vermont College of Medicine, 3Central Information Technology Services, Washington University at St. Louis School of Medicine.
The authors have no financial disclosures.

Introduction
• A disparity in access to health care exists between rural and urban areas.
• 21% of children in the United States live in rural areas.
• 3% of board certified pediatric intensivists practice in rural areas.
• Outcomes for critically ill pediatric patients are better when they are cared for by pediatric intensivists, in tertiary care pediatric intensive care units, and Level 1 trauma centers.

Introduction
• Vermont Children’s Hospital is the tertiary referral center for Vermont and northern up-state New York.
• The referral area includes 19 rural counties with a population of 750,000.
• Pediatric Intensivists n= 2.• Pediatric Emergency Medicine specialists n = 0.

Introduction
• In an attempt to address the issue of local rural access to sub-specialty pediatric critical care, we implemented a pilot program to examine the feasibility and effectiveness of pediatric critical care telemedicine consultations in rural emergency departments.

Methods• Approval was obtained from the University of
Vermont Institutional Review Board for a prospective study of pediatric critical care consultations in rural emergency departments March through October 2006.
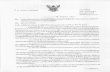
• 10 rural emergency departments in a referral area with a population of 750,000 in 19 rural counties in VT and upstate NY.
• Ground distance to the PICU averaged 75 miles (median 61, range 26-143 miles).
• Clear-weather round-trip ground transport times ranged from 70 to 360 minutes (mean 204, median 215 minutes).

■ Massena (1)■ Malone (2)
■ Saranac Lake (3)
Ticonderoga (2) ■
■ St. Albans (0)
■ Morrisville (3)
■ Middlebury (4)
■ Rutland (1)
■ Burlington
Plattsburgh (9) ■
■ Canton (1)
50 miles

Methods
• ISDN telephone lines and hardware-based dedicated videoconferencing systems were installed in the emergency departments, the PICU office, and the homes of the two pediatric intensivists.
• Telemedicine contact was initiated by the attending pediatric intensivist following a request for transport or consultation, on a 24 hour-a-day, 7-day-a-week basis.
• Post-consultation questionnaires using a 5 point Likert scale were given to consulting intensivists and referring providers.

Results
• Total of 26 consultations were performed from 9 of 10 sites.
• Average of 2.6 consultations per referring emergency department (median 2, range 0 to 9 consultations).
• Patients ranged in age from 2 days to 16 years (mean 61, median 34.5 months).
• All patients were transported to the tertiary care hospital.
• 20 by the tertiary care hospital’s transport team. • 5 by local emergency medical services.• 1 by air.

Primary Diagnosis Number
Status epilepticus 6
Drug overdose 3
Respiratory distress 3
Diabetic ketoacidosis 2
Septic shock 2
Status asthmaticus 2
Angioedema 1
Blunt abdominal trauma 1
GI bleed 1
Neck abscess 1
Oomphalitis 1
Pulmonary hemorrhage 1
Respiratory failure 1
Subarachnoid hemorrhage 1

Results
• Consulting intensivists made a total of 100 specific recommendations (mean 2.6, range 1 to 10 recommendations per consultation).
• 6 children underwent tracheal intubation and mechanical ventilation initiated at the referring hospital.
• 1 for bronchiolitis, 1 for pneumonia and septic shock, 2 for respiratory failure due to drug overdose, and 2 for respiratory failure due to status epilepticus.
• 2 of the intubations were supervised in real time on telemedicine.
• Transport team was supervised by telemedicine in 9 cases.

Recommendations (n=100) Number
Transport patient 26
Give crystalloid 12
Care reviewed with transport team 9
Obtain further laboratory data 7
Medical management of seizures 6
Initiation and stabilization on mechanical ventilation 6
Sedation for mechanical ventilation 6
Medical management of wheezing 5
Changes in intravenous fluid therapy 4
Obtain vascular access 4
Antibiotic therapy 3
Insulin therapy 2
Intubate 2
Intubation drugs and equipment 2
Do not intubate 1
Inotrope/vasopressor therapy 1
Local EMS cleared for transport 1
Move endotracheal tube (right main intubation) 1
Pain control 1
Vent gastrostomy tube 1

Results
• Technical problems were encountered in 2 consultations.
• In both circumstances, the television units at the referral emergency departments had been inadvertently turned off.
• The consultant could see and hear while the referring providers had audio capability only.

Results
• Questionnaires were returned for 26/26 (100%) consultations by intensivists and 19/26 (73%) consultations by referring providers.

Results
Referring MD
Consultant
Improved the quality of patient's care (agree/strongly agree) 78% 85%
Ease of equipment use (good/very good) 89% 92%
Quality of video (good/very good) 90% 85%
Quality of audio (good/very good) 100% 96%
Provider-to-Provider communications (good/very good) 100% 92%

Results
“This consult could have been performed as well by telephone”Intensivists
• Disagree, Strongly Disagree 96%Referring providers
• Disagree, Strongly Disagree 42%• Agree, Strongly Agree 37%
Despite this difference, provider-to-provider communications were rated superior by referring providers.

Discussion
• The vast amount of audiovisual information (vs telephone consultation) concerning the patient made available to the consultant by telemedicine may not be clearly appreciated by referring providers.
• The value of early examination and management of a patient long before arrival at the tertiary center may also be underappreciated from the perspective of the referring provider.
• The perceived difference may lie in the benefit of triage and planning accrued to the receiving intensivist.

Discussion
• Telemedicine was also used to communicate with the transport team at referring hospitals during stabilization prior to ground transports of patients.
• This application of telemedicine has been described only in a feasibility study.

Conclusions
• It is feasible to provide urgent subspecialty critical care for children in underserved rural emergency departments with a high degree of provider satisfaction.
• The application of pediatric critical care telemedicine technology may help to address the disparities in the access to medical care between rural and urban areas.

Funding
• Funded by a grant by the U.S. Department of Transportation
• US DOT FAST STAR: Linking Telemedicine to the Moving Ambulance CONTINUATION/Project #2 of Telemedicine and Rural Specialty Care: A Pilot Study.

References1. US Census Bureau. Available at www.factfinder.census.gov. Accessed September 20, 2006.2. Althouse L, Stockman J, The Future of Pediatric Education II organizing pediatric education to meet the needs of infants,
children, adolescents, and young adults in the 21st century. Pediatrics 2000;105 :163-212.3. Stoddard J, Cull W, Jewett E, et al. Providing pediatric subspecialty care a workforce analysis. Pediatrics 2000;106: 1325-
1333.4. Institute of Medicine: Emergency Medical Services for Children. Washington DC: National Academy Press, 1993.5. American Academy of Pediatrics, Committee on Pediatric Emergency Medicine American College of Critical Care Medicine
and Society of Critical Care Medicine, Pediatric Section, Task Force on Regionalization of Pediatric Critical Care. Consensus Report for Regionalization of Services for Critically Ill or Injured Children. Pediatrics 2000;105:152-155.
6. McGillivray D, Nijssen-Jordan C, Kramer M, et al. Critical pediatric equipment availability in Canadian hospital emergency departments. Ann Emerg Med 2001;37:371-376.
7. Athey J, Dean J, Ball J, et al. Ability of hospitals to care for pediatric emergency patients. Ped Emerg Care 2001;17:170-174.8. Pollack M, Katz R, Ruttimann U, Getson P. Improving the outcome and efficiency of intensive care: the impact of an
intensivist. Crit Care Med 1988;16:11-7. 9. Pollack M, Alexander S, Clarke N, et al. Improved outcomes from tertiary center pediatric intensive care: a statewide
comparison of tertiary and nontertiary care facilities. Crit Care Med 1991;19:150-9. 10. Yeh TS. Regionalization of pediatric critical care. Crit Care Clin 1992;8:23-35. 11. Pearson G, Shann F, Barry P, et al. Should paediatric intensive care be centralised? Lancet 1997;349:1213-7. 12. Tilford JM, Simpson PM, Green JW, Lensing S, Fiser DH. Volume-outcome relationships in pediatric intensive care units.
Pediatrics 2000;102:289-94. 13. Brilli RJ, Spevetz A, Branson RD, et al. Critical care delivery in the intensive care unit ; defining clinical roles and the best
practice model. Crit Care Med 2001; 29:2007-2001. 14. Nakayama DK, Copes WS, Saco WJ. Differences in pediatric trauma cxare among pediatric and nonpediatric centers. J
Pediatr Surg 1992;27:427-431.15. Hall JR, Reyes HM, Meller JT, et al. Outcome for blunt trauma is best at pediatric trauma centers J Pediatr Surg 1996;31:72-
77.16. Potoka DA, Schall LC, Gardner MJ, et al. Impact of pediatric trauma centers on mortality in a statewide system. J Traum
2000;49:237-245.17. Potoka DA, Schall LC, Ford HR. Improived functional outcome for severely injuredchildren treated at pediatric trauma
centers. J Traum 2001;51:824-834.18. Osler TM, Vane DW, Tepas JJ, et al. Do pediatric trauma centers have better survival rates than adult traumas centers? An
examination of the Natoinal Pediatric Trauma Registry. J Trauma 2001;50:96-101. 19. Farrell LS, Hannah EL, Cooper A. Severity of injury and mortality associated with pediatric blunt injuries: hospitals with
pediatric intensive care units vs. other hospitals. Pediatr Crit Care Med 205;5:5-9.

References20. Karp W, Grigsby R, McSwiggan-Hardin M, et al. Use of Telemedicine for Children With Special Health Care Needs.
Pediatrics 2000;105:843-847.21. Gray J, Safran C, Davis R, et al. Baby CareLink: Using the Internet and Telemedicine to Improve Care for High-Risk
Infants. Pediatrics 2000;106:1318-1324.22. Pammer W, Haney N, Wood B, et al. Use of Telehealth Technology to Extend Child Protection Team Services. Pediatrics
2001;108:584-590.23. Sable C, Cummings S, Pearson G, et al. Impact of Telemedicine on the Practice of Pediatric Cardiology in Community
Hospitals. Pediatrics, 2002;109:e3.24. Young T, Ireson C. Effectiveness of School-Based Telehealth Care in Urban and Rural Elementary Schools. Pediatrics
2003;112:1088-1094.25. Marcin J, Jeff Ellis J, Roland Mawis R, et al. Using Telemedicine to Provide Pediatric Subspecialty Care to Children With
Special Health Care Needs in an Underserved Rural Community. Pediatrics 2004;113:1-6.26. Lobe T. Telemedicine and the Future of Healthcare for Our Children
Pediatrics 2004;113:e130.27. Spooner A, Edward M. Gotlieb E, the Steering Committee on Clinical Information Technology and Committee on Medical
Liability. Telemedicine: Pediatric Applications. Pediatrics 2004;113:e639. 28. McConnochie P, Wood N, Kitzman H, et al. Telemedicine Reduces Absence Resulting From Illness in Urban Child Care:
Evaluation of an InnovationPediatrics 2005;115:1273-1282.
29. Committee on Pediatric Emergency Medicine. Access to Optimal Emergency Care for Children. Pediatrics 2007;119:161-4.
30. Marcin JP, Nesbitt TS, Kallas HJ, et al. Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr 2004;144:375-80.
31. Marcin JP, Schepps DE, Page KA, et al. Struve The use of telemedicine to provide pediatric critical care consultations to pediatric trauma patients admitted to a remote trauma intensive care unit: A preliminary report. Ped Crit Care Med 2004;5:251-256.
32. Marcin JP, Cole S. Pediatric Critical Care Telemedicine Consultations to Rural Emergency Departments. The 16th Pediatric Critical Care Colloquium, February 21-24, 2006. Snowbird, UT.
33. Marcin JP, Reznik M, Ozuah PO. Telemedicine for children presenting to rural emergency departments or intensive care units. Telepediatrics: Telemedicine and Child Health. Wootton R and Batch J eds. Royal Society of Medicine Press, London, 2005; p183-192.
34. Mayer, ML. Are We There Yet? Distance to Care and Relative Supply Among Pediatric Medical Subspecialties. Pediatrics 2006;118:2313-21.
35. Kofos D, Pitetti R, Orr R, Thompson A. Telemedicine in Pediatric Transport; A Feasibility Study. Pediatrics 1998;e58.
Related Documents