Sickle cell disease Khoo Ser Chin Jasmine Tijana Jovanovic Mary Kathleen Lilleness

Sickle Cell
Sep 13, 2015
Presentation Sickle Cell
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Sickle cell disease
Khoo Ser Chin Jasmine Tijana Jovanovic Mary Kathleen Lilleness OutlineIntroductionEpidemiologyGeneticsSymptoms Diagnosis Treatment ConclusionIntroduction Autosomal recessive genetic disorderSingle base mutation in gene chromosome 11Inherited blood disorder that leads to mutant form of beta globin chain of hemoglobin (Hb) Abnormal hemoglobin (Hb) chains cause RBC to be rigid and have concave shapes
http://learn.genetics.utah.edu/content/disorders/whataregd/sicklecell/What is sickle cell disease?
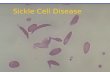
Normal Hb contains glutamate but sickle cell Hb contains valine Single change in amino acid cause abnormal hemoglobin (HbS) to be less soluble HbS stacks up into long rigid rods and distort RBC into sickle shape Sickle cells have short life span
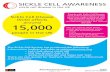
http://learn.genetics.utah.edu/content/disorders/whataregd/sicklecell/Sickle cell disease is typically caused by a single missense mutation that effects a substitution of valine for glutamic acid at position 6 of the beta globin polypeptide chain. In homozygotes, this A.A substitution alters the structure of hemoglobin molecules such that they aggregates, causing RBC to assume a characteristic sickle shape under conditions of low oxygen tension.Epidemiology Common among people whose ancestors come from sub-Saharan Africa and Mediterranean countries Affects about 72,000 people in USDisease occurs in 1 in every 500 African-American births About 1 in 12 African Americans carry the sickle cell trait
In the United States, the disease most commonly affects African-Americans. Sickle cell disease is most common among people from Africa, India, the Caribbean, the Middle East, and the Mediterranean. The high prevalence of the defective gene in these regions may be due to the fact that carriers of a mutation in the beta-subunit of hemoglobin are more resistant to malaria.
Genetics
Parents with sickle cell trait can produce children with 3 phenotypesHeterozygous individuals have survival advantage against malaria Sickle cell anemia is an autosomal recessive genetic disorder caused by a defect in the HBB gene, which codes for hemoglobin. The presence of two defective genes (SS) is needed for sickle cell anemia.2 individuals with sickle cell trait can produce children with 3 phenotypes. The chances of producing a individual with normal genotype (HbAHbA) are 25% , sickle cell trait (HbAHbS) 50% and sickle cell disease (HbSHbS). Although sickle cell disease is a devasting disease, it provides heterozygous individuals with a survival advantage. People who have sickle cell are resistant to the protozoan parasite that cause malaria. The parasite spends part of its life cycle in rbc, feeding hemoglobin but it cannot complete its life cycle when sickle shaped cells form and break down earlier.
Clinical manifestationhomozygosity for HbShemoglobin SC diseas sickle cell trait (heterozygosity for HbS)HbSC -combined heterozygosity for hemoglobins S and CClinical manifestationmicroinfarcts (heart, skeleton, spleen, central nervous system)
Hemolytic anemiaCardinal signsPainful vaso-occlusive crisisMultiple organ damage Anemia - shortness of the breath, dizziness, headaches, coldness in hands and feet, paler skin of mucous membranes, jaundicePain - bone crisis,abdominal crisis, joint crisis, acute chest syndrome, Complications Hand-Foot Syndrome Splenic Crisis Infections Acute Chest Syndrome Pulmonary Hypertension Delayed Growth and Puberty Stroke Eye Problems Gallstones Ulcers on the Legs Multiple Organ Failure
Diagnosisprenatal diagnosis - fetal DNA samples are obtained by chorionic villus neonatal screeninginfants - do not usually manifest any signs and symptoms until 6 months oldchildren - dactylitis, pain and infection
DiagnosisDiagnostic testshemoglobin electrophoresis thin-layer isoelectric focusing high performance liquid chromatography (HPLC)solubility test for Hb S (e.g. Sickledex)
TreatmentNo way to prevent or reverse sicklingNo established cureCase by case disease managementdifferent severity and symptomsRegular check-ups and testing RBC countorgan x-raysblood transfusionsDrug treatmentantibioticspain reliefhydroxyurea
HydroxyureaMost prescribed treatment for SCDTaken daily, breaks down sickle cellsIncreases fetal hemoglobin concentrationImproves RBC survival and reduces need for blood transfusions
Positive and negative effectsReduces vascular inflammationLeads to fewer and less severe acute pain episodesHowever, increases risk for infection
Potential CuresBone marrow transplantHas been effective but is not in wide useAttempted on patients with severe symptoms and who are non-responsive to hydroxyureaMany difficulties donor, health complications
Gene therapy-globulin gene transfer to produce normal HbUnsuccessful, so far
ConclusionsSCD has a severe effect on health, leading to reduced life expectancy and possibly death
Proper disease management can help patients lead a relatively normal lifeLife expectancy: 40s and 50s
Single gene disease does not mean easy to cure or live with
Related Documents