-
7/31/2019 Review of Myelopathy
1/27
5/7/
Learning Objectives:
Describe the 5 main signs & symptoms of myelopathy: Para-/quadriparesis, sensory level, urinary incontinence, constipation,
sexual dysfunction Identify & distinguish the different causes of myelopathy by their clinical
presentations
Describe the evaluation & management of spinal cord compression
-
7/31/2019 Review of Myelopathy
2/27
When approaching a patient with a neurologic complaint, it is important tothink like a neurologist. The initial most important aspect of the neurologicevaluation is to anatomically localize the site of the lesion.
Example: Is the lesion in the central or peripheral nervous system?
If central, is it in the brain or spinal cord? Within the brain, is the lesioncortical or subcortical?
If peripheral, is it in the nerve root, peripheral nerve, neuromuscularjunction, or muscle?
The process of "localizing the lesion" from the onset of the evaluation will
serve as a guide to focus the neurologic assessment.
Localizing the lesion ultimately lays the foundation for forming a differential
diagnosis and developing a plan for evaluation, management, andcounseling of the patient.
5/7/
-
7/31/2019 Review of Myelopathy
3/27
Numbness requires clarification to determine whether the patient isdescribing a loss of sensation, or a positive phenomena, such asparesthesias (abnormal spontaneous sensation) or dysesthesias (abnormal
sensation to stimulus). Destructive or compressive lesions of the CNS moreoften cause sensory loss whereas inflammatory or irritative lesions often
result in positive phenomena.
Cold feeling in the legs can be neurologic in nature but can also be due toperipheral vascular disease.
Hemibody symptoms can result from a contralateral cerebral hemisphere or
brainstem lesion, or from a spinal cord lesion. However, bilateral symptomsare more likely due to spinal cord or peripheral nerve disorders.
A complaint of tightness in a band around the chest or abdomen is
characteristic of a spinal cord lesion. This usually correlates with findings of
a sensory level on neurologic examination.
5/7/
-
7/31/2019 Review of Myelopathy
4/27
Progressive symptoms suggest an expanding lesion.
Gait difficulty can be due to weakness, sensory ataxia (proprioceptive loss),or cerebellar ataxia.
Urinary incontinence can result from upper-motor neuron dysfunction (brain,spinal cord) or lower-motor neuron dysfunction (peripheral nerves).
Diminished perianal and genital sensation indicates either spinal cord orsacral nerve root lesion.
The most likely lesion localization in a patient with gait difficulty, bilateral legsymptoms, urinary incontinence, decreased perianal and genital sensation is
either the spinal cord or bilateral lumbosacral nerves. However, whenassociated with band-like tightness around the chest, the most likelylocalization is the spinal cord.
If the upper extremities are not involved, the lesion is more likely below thelevel of the brachial plexus (C5-T1).
5/7/
-
7/31/2019 Review of Myelopathy
5/27
Our patient has no family history of neurologic disease, no risk factors forinfection or tumor, and no history of trauma.
5/7/
-
7/31/2019 Review of Myelopathy
6/27
Our patients vital signs and general exam are normal. There are no signs ofinfection. In addition, there is no spinal tenderness to suggest a bone lesion(e.g., vertebral compression fracture either pathologic or osteoporotic,
bone metastases, osteomyelitis) or paraspinal tenderness to suggest anepidural abscess, hematoma, or other mass lesion
5/7/
-
7/31/2019 Review of Myelopathy
7/27
The initial portion of the neurologic examination shows bilateral lowerextremity weakness and supports our suspicions of either a spinal cordlesion below the level of the cervical spinal cord, or lesions involving bilateral
lumbosacral nerves (e.g., bilateral lumbosacral plexus, cauda equina).Further testing for the presence of a sensory level and reflex testing will help
to confirm the lesion localization.
lesions in the bilateral medial cerebral hemispheres or brainstem can cause
weakness of both legs, normal mental status and normal cranial nerve exammakes a lesion in either of these locations less likely.
5/7/
-
7/31/2019 Review of Myelopathy
8/27
The presence of a sensory level strongly suggests a spinal cord lesion.Depending on the extent of nerve-fiber damage, a sensory level can berelative, meaning that the sensation is partially diminished, orabsolute,
meaning that the sensation is completely absent below the level of thelesion.
Our patients sensory level suggests a spinal cord lesion at the level of T3.
However, a sensory level may be hung a few to several levels below theactual site of the lesion. For example, a cervical lesion may result in a hungsensory levelin the upper-thoracic cord.
5/7/
-
7/31/2019 Review of Myelopathy
9/27
Hyperreflexia, 3+ or 4+ reflexes, and Babinski sign indicates upper-motorneuron dysfunction.
Babinski sign, or extensor plantar response, is tested by stroking thelateral aspect of the sole from the heel across the ball to the big toe. Toeflexion is the normal response.
Clonus is a series of involuntary muscle contractions stimulated by suddenstretching of the muscle. It is most common at the ankle. It can be sustained(indefinite) or nonsustained (described by the number of beats).
Bilateral hyperreflexia and Babinski signs in lower extremities with normal
reflexes in the upper extremities suggests a spinal cord lesion below thelevel of the nerves roots supplying the brachial plexus.
5/7/
-
7/31/2019 Review of Myelopathy
10/27
Localization in clinical neurology refers to the process of determining an anatomical/structural location of the patientsneurological problem. For example, is the problem in the brain, brainstem, cerebellum, spinal cord, roots, peripheral nerves,
neuromuscular or muscle.
5/7/
-
7/31/2019 Review of Myelopathy
11/27
Based&upon&the&examina0on&findings&outlined&on&this&slide&the&most&likely&
localiza0on&is&the&low9cervical&or&high9thoracic&spinal&cord.&
5/7/
-
7/31/2019 Review of Myelopathy
12/27
The differential diagnosis is the cornerstone of clinical medicine: determining
diagnostic possibilities based upon history and examination.
5/7/
-
7/31/2019 Review of Myelopathy
13/27
5/7/5/7/
The spinal cord is normally protected by the spine. Spinal cord compressionresults when the cord is externally compressed by bone (e.g., compressionfracture, bony metastasis, Potts disease), tumor, infection or hemorrhage.
Cord compression syndromes are typically associated with pain.
Myelitis, or transverse myelitis (TM), is an inflammatory myelopathy. It
typically develops over hours to days. The most common etiologies arelisted on this slide. Post-infectious TM is thought to be immune-mediatedafter exposure to a foreign antigen.
Spinal cord tumors can be intramedullary (within the cord), intradural-extramedullary (e.g., meningioma, neuro-fibroma), or extradural (usually
bony metastasis). Intradural tumors are usually low-grade astrocytoma,ependymoma, or hemangioblastoma
Arteriovenous malformations (AVM) are congenital abnormal tangles of
arteries and veins. In the cord, AVMs can cause symptoms by threemechanisms bleeding, compression, or shunting of blood. Spinal cord
AVMs are rare but must be considered in the differential diagnosis.
-
7/31/2019 Review of Myelopathy
14/27
5/7/5/7/
Syringomyelia, or syrinx, is a cystic cavitation of the spinal cord, most common in the
cervical cord. It is typically associated with congenital brainstem anomalies (Chiari
malformation), remote spinal cord trauma, or tumors within the spinal cord. Compression of
central cord structures by the enlarging syrinx can cause loss of pain & temperature
sensation in cape-distribution (anterior white commissure - crossing spinothalamic tract
fibers), atrophy and weakness (anterior horn cells), and spastic para- or quadriparesis
(corticospinal tracts). Typically vibration and proprioception are intact due to sparing of thedorsal columns
-
7/31/2019 Review of Myelopathy
15/27
5/7/5/7/
Neurosyphilis can result in tabes dorsalis many years after the initial syphilisinfection if it is left untreated. Typically, the posterior spinal nerve roots in thelumbosacral region are involved causing lancinating pain radiating into the
legs. Eventually, there is progressive degeneration of the posterior columnsof the spinal cord.
-
7/31/2019 Review of Myelopathy
16/27
5/7/5/7/
Vitamin B12 deficiency can cause a myelopathy that presents subacutely over weeks tomonths. Degeneration of both the lateral corticospinal tracts and the posterior columnsoccur so the myelopathy is referred to as subacute combined degeneration of the spinalcord. Loss of vibration and proprioception results in severe sensory ataxia evidenced by thepresence of Romberg sign on exam. HIV vacuolar myelopathy also affects the posterior andlateral columns and presents similarly to Vitamin B12 deficiency.
-
7/31/2019 Review of Myelopathy
17/27
5/7/5/7/
Spinal cord infarction is rare and generally occurs in the anterior spinal artery territory. The
paired posterior spinal arteries are well-supplied by feeders so infarction is rare in the
posterior cord. Acute paraparesis and loss of pain & temperature sensation below the
lesion with intact vibration and proprioception is characteristic. Reflexes and tone may be
decreased acutely (spinal shock). Causes include trauma, dissecting aortic aneurysm,
hypotensive crisis (e.g., intraoperative blood loss, aortic cross-clamping).
-
7/31/2019 Review of Myelopathy
18/27
5/7/
HTLV-1 (Human T-lymphotrophic virus 1) is a retrovirus that causes T-cellleukemia and T-cell lymphoma in adults. It is endemic in the Carribbean,Japan, and Africa. Infection of the spinal cord by HTLV-1 results in HTLV-1
associated myelopathy, a chronic progressive demyelinating inflammatorymyelopathy primarily affecting the cortico-spinal tracts of the thoracic cord.
Minor sensory loss may also be present.
-
7/31/2019 Review of Myelopathy
19/27
5/7/5/7/
Lateral hemisection of the spinal cord due to trauma or compression leads toa characteristic presentation of Brown-Squard Syndrome:
Ipsilaterally below the level of the lesion there is weakness (corticospinaltract dysfunction), hyperreflexia, and a sensory level to vibration &proprioception (posterior column dysfunction).
Contralaterally below the level of the lesion there is a sensory level topinprick (spinothalamic tract dysfunction). Remember that the spinothalamictract fibers enter the spinal cord and cross over to the opposite side of thecord, then ascend to the brain, unlike both the corticospinal tract and
posterior column fibers which decussate in the lower brainstem
-
7/31/2019 Review of Myelopathy
20/27
Evaluation is partially synonymous with plan. This refers to the clinicians plan for
testing to definitively diagnose the etiology of the patient's complaint based upon the
differential diagnosis.
5/7/
-
7/31/2019 Review of Myelopathy
21/27
Spinal X-rays may be helpful in detecting causes of back pain involving bonesuch as vertebral compression fractures, bone metastasis, and degenerative
joint disease. However, it does not allow visualization of disks, nerves, or
soft tissue. Spinal MRI is needed if spinal cord compression is suspected.
MRI is the preferred study for obtaining detailed images of the bony
structures and soft tissues of the spine, the spinal cord, and the spinal nerveroots. If MRI can be obtained quickly, spinal X-rays are not usuallynecessary in evaluating suspected spinal cord compression.
5/7/
-
7/31/2019 Review of Myelopathy
22/27
5/7/5/7/
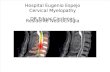
The sagittal view of our patients thoracic-spine MRI, showing the midlineof the spinal cord, is shown here. On T1-weighted images CSF appearsdark, while on T2-weighted images it appears white. Notice the posterior
mass at the T3-T4 level evident on both images, resulting in severecompression of the spinal cord posteriorly. This mass is extramedullary
(outside the spinal cord)and intradural, and enhances homogeneouslywith contrast. Its appearance ismost consistent with a calcifiedmeningioma (calcium is black on T2-weighted images).
-
7/31/2019 Review of Myelopathy
23/27
Review the final diagnosis with the learners.
5/7/
-
7/31/2019 Review of Myelopathy
24/27
Management refers to therapeutic interventions (including medications, procedures,
therapies, etc) to provide acute and/or long term treatment for the patients disease
and risk factors. Management also includes rehabilitation and lifestyle modification.
5/7/
-
7/31/2019 Review of Myelopathy
25/27
5/7/5/7/
Mild cord compression may be asymptomatic or cause only minimaldisruption of signal conduction. More significant compression may causesevere disruption or blockage of nerve signal transmission, resulting in
severe muscle weakness, sensory loss, and bowel and bladder dysfunction.If the compression is not relieved, irreversible spinal cord damage can occur
within 24 hours. Acute cord compression from any cause (e.g., trauma,acute disk herniation, tumor, abscess, hematoma) is an emergency andwarrants immediate referral to neurosurgery for decompression.
-
7/31/2019 Review of Myelopathy
26/27
Counseling refers to physician discussion and education sessions with the patient,
family and caregivers regarding the patients illness, diagnostic evaluation, treatment
plan and long term prognosis. These counseling sessions should also include
education regarding how the patients disease will affect their daily life and ability to
perform activities of daily living and employment capability. When appropriate,
counseling regarding advanced directives and goals of care should also beperformed. The physician can also refer the patient and family to other resources and
allied health disciplines as appropriate: social work, case management, chaplains,
vocational rehabilitation, etc.
5/7/
-
7/31/2019 Review of Myelopathy
27/27
5/7/5/7/
Prognosis depends on the severity and duration of the neurologic deficitprior to decompression. Improvement can occur post-operatively withremyelination and resolution of edema and inflammation. Some neurologic
deficits may be irreversible
Autonomic hyperreflexia can occur with cervical and thoracic cord lesions.Stimuli below the lesion level that are easily tolerated in healthy people (e.g.,overfull bladder) trigger excess sympathetic nerve activation resulting in blood pressure, heart rate, excessive sweating and flushing.
Neurogenic bladder occurs due to dysynergy between the bladderdetrusor and sphincter muscles, often resulting in a flaccid bladder requiring
intermittent self-catheterization.
Neuropathic pain, often described as burning, lancinating, stabbing, orelectric shock-like, can be severe & difficult to treat.