65 Clinical Science (2000) 99, 65–75 (Printed in Great Britain) Relationship between the clinical features of neurological decompression illness and its causes Peter WILMSHURST* and Philip BRYSON *The Royal Shrewsbury Hospital, Shrewsbury SY3 8XQ, U.K., and The Hyperbaric Medical Centre, Tamar Science Park, Plymouth PL6 8BQ, U.K. A B S T R A C T There is dispute as to whether paradoxical gas embolism is an important aetiological factor in neurological decompression illness, particularly when the spinal cord is affected. We performed a blind case-controlled study to determine the relationship between manifestations of neurological decompression illness and causes in 100 consecutive divers with neurological decompression illness and 123 unaffected historical control divers. The clinical effects of neurological decompression illness (including the sites of lesions and latency of onset) were correlated with the presence of right-to-left shunts, lung disease and a provocative dive profile. The prevalence and size of shunts determined by contrast echocardiography were compared in affected divers and controls. Right-to-left shunts, particularly those which were large and present without a Valsalva manoeuvre, were significantly more common in divers who had neurological decompression illness than in controls (P ! 0.001). Shunts graded as large or medium in size were present in 52 % of affected divers and 12.2 % of controls (P ! 0.001). Spinal decompression illness occurred in 26 out of 52 divers with large or medium shunts and in 12 out of 48 without (P ! 0.02). The distribution of latencies of symptoms differed markedly in the 52 divers with a large or medium shunt and in the 30 divers who had lung disease or a provocative dive profile. In most cases of neurological decompression illness the cause can be determined by taking a history of the dive profile and latency of onset, and by performing investigations to detect a right-to-left shunt and lung disease. Using this information it is possible to advise divers on the risk of returning to diving and on ways of reducing the risk if diving is resumed. Most cases of spinal decompression illness are associated with a right-to-left shunt. INTRODUCTION Neurological symptoms may occur during or after ascent from a dive, on leaving a caisson or during sub- atmospheric decompression. There has been a call to Key words : airways obstruction, atrial septal defects, cerebral decompression illness, contrast echocardiography, decompression sickness, gas embolism, lung function tests, patent foramen ovale, pulmonary arteriovenous fistula, pulmonary barotrauma, smoking, spinal decompression illness. Abbreviations : CT, computed tomography. Correspondence : Dr Peter Wilmshurst. describe all cases using the encompassing term ‘ neuro- logical decompression illness ’ [1]. This allows the treating doctor to ascribe a diagnostic label without determining aetiology [1]. Assessment of the risk of recurrence on returning to diving requires knowledge of the cause of an # 2000 The Biochemical Society and the Medical Research Society

Relationship between the clinical features of neurological decompression illness and its causes
Oct 15, 2022
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
c:/ncl/cls51865Clinical Science (2000) 99, 65–75 (Printed in Great Britain)
Relationship between the clinical features of neurological decompression
illness and its causes
Peter WILMSHURST* and Philip BRYSON† *The Royal Shrewsbury Hospital, Shrewsbury SY3 8XQ, U.K., and †The Hyperbaric Medical Centre, Tamar Science Park, Plymouth PL6 8BQ, U.K.
A B S T R A C T
There is dispute as to whether paradoxical gas embolism is an important aetiological factor in
neurological decompression illness, particularly when the spinal cord is affected. We performed
a blind case-controlled study to determine the relationship between manifestations of
neurological decompression illness and causes in 100 consecutive divers with neurological
decompression illness and 123 unaffected historical control divers. The clinical effects of
neurological decompression illness (including the sites of lesions and latency of onset) were
correlated with the presence of right-to-left shunts, lung disease and a provocative dive profile.
The prevalence and size of shunts determined by contrast echocardiography were compared in
affected divers and controls. Right-to-left shunts, particularly those which were large and
present without a Valsalva manoeuvre, were significantly more common in divers who had
neurological decompression illness than in controls (P! 0.001). Shunts graded as large or
medium in size were present in 52% of affected divers and 12.2% of controls (P! 0.001). Spinal
decompression illness occurred in 26 out of 52 divers with large or medium shunts and in 12 out
of 48 without (P! 0.02). The distribution of latencies of symptoms differed markedly in the 52
divers with a large or medium shunt and in the 30 divers who had lung disease or a provocative
dive profile. In most cases of neurological decompression illness the cause can be determined by
taking a history of the dive profile and latency of onset, and by performing investigations to
detect a right-to-left shunt and lung disease. Using this information it is possible to advise divers
on the risk of returning to diving and on ways of reducing the risk if diving is resumed. Most cases
of spinal decompression illness are associated with a right-to-left shunt.
INTRODUCTION
Neurological symptoms may occur during or after ascent from a dive, on leaving a caisson or during sub- atmospheric decompression. There has been a call to
Key words : airways obstruction, atrial septal defects, cerebral decompression illness, contrast echocardiography, decompression sickness, gas embolism, lung function tests, patent foramen ovale, pulmonary arteriovenous fistula, pulmonary barotrauma, smoking, spinal decompression illness. Abbreviations : CT, computed tomography. Correspondence: Dr Peter Wilmshurst.
describe all cases using the encompassing term ‘neuro- logical decompression illness ’ [1]. This allows the treating doctor to ascribe a diagnostic label without determining aetiology [1]. Assessment of the risk of recurrence on returning to diving requires knowledge of the cause of an
# 2000 The Biochemical Society and the Medical Research Society
66 P. Wilmshurst and P. Bryson
earlier episode. In most, if not all, cases, decompression illness is caused by gas bubbles. If gas trapping as a result of lung disease or failure to exhale adequately during ascent causes pulmonary barotrauma, bubbles may in- vade the pulmonary veins to become arterial gas emboli. Decompression sickness occurs if ambient pressure is reduced sufficiently below the partial pressure of gas dissolved in tissues for bubbles to form in vivo. A contentious issue is whether such bubbles produce injury by an autochthonous mechanism (causing injury at the site where they are formed) or by embolism. Some cases might result from a combination of mechanisms.
Bubbles are common in the venous circulation after diving, but usually produce no symptoms because they are filtered by the pulmonary capillaries, where the gas diffuses along the concentration gradient into the alveoli. Exceptionally, when the dive profile is very provocative, massive venous gas embolism may overwhelm the filtering capacity of the pulmonary capillaries so that bubbles reach the systemic circulation. It is also possible that bubbles will pass through the pulmonary capillaries if there is transient recompression, as occurs during repetitive dives in a short time period. A case report and observational studies have suggested that paradoxical gas embolism across right-to-left shunts might have a role in the aetiology of some cases of neurological decom- pression sickness after conservative dives [2–4]. Such shunts usually occur across a foramen ovale, but occasionally shunting is through an atrial septal defect or a pulmonary arteriovenous fistula. A blinded case- controlled study showed that right-to-left shunts were particularly associated with neurological symptoms that occurred within 30 min of surfacing [5]. Neurological symptoms usually followed an unprovocative dive in divers who had a shunt, but were usually the result of a provocative dive if divers had no shunt [5]. Data extending these observations and a replication study performed under supervision of members of the Medical Research Council Decompression Sickness Panel have been reported [6,7]. There have been other human and animal studies which support the theory that neurological decompression sickness can be the result of paradoxical gas embolism [8–10]. However, the possibility that this mechanism may be associated with a significant number of cases of neurological decompression illness is contrary to established aetiology theories, and many experts in diving medicine remain unconvinced that paradoxical gas embolism is a numerically important cause of decom- pression illness [11–16]. A large controlled study proposed in 1990 by one of these groups [12] has not yet been published.
One objection is that between one-quarter and one- third of the population, and a similar proportion of divers, have a patent foramen ovale which might allow right-to-left shunting [5,17]. Considerably fewer than a quarter of divers develop decompression illness [18].
Many divers with a demonstrable shunt have no history of decompression illness [5,6,13,14]. Thus the relevance of a patent foramen ovale is disputed. This argument fails to take account of variations in risk based on shunt size, which is dependent on the anatomy and dimensions of the defect and the pressure gradient, and on venous bubble load, which is affected by individual susceptibility to bubble nucleation and the profiles of dives performed. Many dive profiles do not cause venous gas nucleation at a time when critical tissues have sufficient gas content to amplify gas emboli.
A second objection is that the greater blood flow to the brain generally ensures that embolic events in the spinal cord are much less frequent than in the brain, but involvement of the spinal cord is a common manifestation of decompression sickness. The pathological distribution of lesions and the time course of spinal cord decom- pression illness are considered by some to be incom- patible with an embolic mechanism [11,19,20]. This led to the assertion that autochthonous bubbles must be the cause of spinal decompression illness [11]. There is one clinical study in humans which suggests that a patent foramen ovale is not associated with spinal decom- pression illness [10], but it was our impression from our previous studies that spinal decompression illness may be more frequent when the diver has a right-to-left shunt and that, in affected cases, the shunt size is considerably larger than in the general population [5–8,21]. We therefore believed that the role of shunts in the causation of spinal decompression illness may be greater than generally appreciated. There have been cases of spinal cord dysfunction after air embolism following pulmon- ary barotrauma during submarine escape training [22]. Therefore, in the present study, we investigated how shunt size is related to susceptibility to neurological decompression illness, and in particular to spinal lesions. The primary (pre-analysis) aims of the study were : (a) to compare the prevalence and size distribution of right-to- left shunts in divers with a history of neurological decompression illness and in unaffected control divers ; (b) to determine the relationship between large and medium-sized right-to-left shunts and lesion site (spinal or cerebral) in divers with neurological decompression illness ; and (c) to determine what proportions of episodes of neurological decompression illness were related to the presence of cardiac shunts, lung disease or a provocative dive profile.
METHODS
We performed a ‘blind’ retrospective analysis of 100 consecutive divers (34 female ; 91 amateur and nine
# 2000 The Biochemical Society and the Medical Research Society
67Causes of neurological decompression illness
professional) who were assessed following one or more episodes of neurological decompression illness. The first in this cohort was the next case seen after completion of our previous publication [8]. One episode occurred after a dry hyperbaric chamber dive in which air was breathed. The other episodes followed dives in water. One amateur diver had neurological decompression illness after a deep dive breathing trimix (helium, oxygen, nitrogen), with long nitrox (nitrogen and oxygen) decompression stops. All the other episodes of decompression illness followed dives in which air was breathed, but nitrox was used on one of the dives for decompression stops.
The referral and assessment of each amateur diver was in accordance with the Medical Standards of the United Kingdom Sport Diving Medical Committee. These re- quire enquiry into the circumstances of the incident, including the dive profile, and investigations to exclude the presence of physical predisposition (i.e. to exclude a right-to-left shunt and lung disease). The professional divers were referred for the same reason, although there is no formal requirement. The cases studied have not been reported previously, except for six cases reported in description of closure procedures ([23], but see [23a] ; [24]). Of the consecutive cases, 35 were treated for neurological decompression illness at a single centre (The Hyperbaric Medical Centre, Plymouth). The other referrals came from other recom- pression facilities, diving medical referees and general practitioners.
One of us (P.B.) retrospectively reviewed information about symptoms and signs at presentation with de- compression illness to determine the lesion site. This was done blind to knowledge of the results of cardio- respiratory investigations. It was also blind to dive profile, except for the 35 cases from his own centre. Another (P.W.) had previously reported the contrast echocardiography and lung function tests and analysed the dive profile to assign an aetiology label. This was performed blind to categorization of the lesion site. Possible causes of decompression illness were : (a) a clinically relevant (large or medium size) right-to-left shunt (atrial or pulmonary) determined from contrast echocardiography; (b) lung disease predisposing to pul- monary barotrauma determined from lung function tests and chest X-ray; (c) provocative dive (rapid ascent or inadequate decompression, including missed stops and computer malfunction) determined from the history; (d) any combination of these ; (e) unknown cause when there was no shunt or lung disease detected and the dive profile was considered unprovocative.
In all cases, transthoracic contrast echocardiography was performed to detect the presence of a right-to-left shunt and for semi-quantitative assessment of the size of any shunt detected [25]. We always perform contrast echocardiography before reading the referral letter and blind to history and physical findings, to avoid bias in
interpretation. We adhered to this practice for all cases and controls. The heart was imaged (apical four-chamber view) with a Hewlett Packard Sonos 500, 1000 or 2000 machine. Bubble contrast was produced by pushing approx. 5 ml of sterile saline (0.9% NaCl), 0.5 ml of the subject’s blood and 0.5 ml of air back and forth between two syringes connected by a three-way tap until there were no visible bubbles. This mixture was injected through a 21-gauge butterfly needle into a left antecubital vein. The first contrast injection was performed with the subject resting and breathing normally. If no shunt was seen with the first contrast injection, up to five sub- sequent injections were performed with Valsalva manoeuvres, with the operator causing sudden release of the manoeuvre, as described previously [8]. The size of the shunt was graded according to the maximum number of bubbles seen in the left heart on frame-by-frame analysis : small shunts, fewer than six bubbles ; medium shunts, six to 20 bubbles ; large shunts, more than 20 bubbles [25]. On the basis of our previous observations, we believe that small shunts represent a low risk of predisposing to decompression illness, and in the present study they were considered to be clinically irrelevant. Late appearance of bubbles in the left heart was taken to indicate a pulmonary shunt. Such shunts usually appear as a constant stream of bubbles in the left heart, and atrial shunts usually appear as groups of bubbles. When a pulmonary shunt was suspected, additional tests, in- cluding pulse oximetry assessment of orthodeoxia and, in some cases, pulmonary angiography, were performed. The sizes of shunts in the divers with decompression illness were compared with results obtained by the same method in 123 historical control divers who had not had decompression illness. (Some of the results from this population of normal divers have been presented pre- viously as an abstract [26].)
Lung function tests were performed after contrast echocardiography and after determining the latency of symptoms (the interval between surfacing and the first neurological symptom). In 17 cases the late onset of symptoms was considered to exclude pulmonary baro- trauma, and lung function tests were not performed. (Our current practice is to carry out lung function tests in all cases of neurological decompression ill- ness.) The presence of lung disease predisposing to pulmonary barotrauma was assessed by spirometry, flow volume loops and chest X-ray in 83 cases. Evidence of small-airways disease was sought by examination of the flow volume loops, as described previously [8]. The reading of these tests was also performed blind to the history of decompression illness (i.e. before reading the referral letter, taking a history or examining the patient).
The series of dives leading up to the episode of decompression illness was then analysed for provocative events. The series of dives was considered to have started
# 2000 The Biochemical Society and the Medical Research Society
68 P. Wilmshurst and P. Bryson
after the last 48 h dive-free interval prior to the episode of decompression illness. A dive series was considered provocative if the diver had made a rapid ascent or had performed inadequate decompression stops (as required by the decompression table or computer he}she used for the dive series, or if computer malfunction led to missed stops) or there had been both rapid ascent and inadequate decompression stops. Divers were also asked about unusual events during the dives. A history of tobacco smoking was taken.
One of us (P.B.), who regularly treats divers with decompression illness, was responsible for determining whether the neuological injury was spinal, cerebral, both spinal and cerebral, or indeterminate. This categorization was based on pre-treatment symptoms and signs, and was performed blind to knowledge of the presence of right- to-left shunts or lung disease. It was also blind to dive profiles, except in the cases he had treated. In the majority of cases referred from his own centre, P.B. had examined the patients during their acute illness and he based his diagnosis on his own clinical records. In the other cases, information about presenting features was obtained from the notes made by the treating centre or the referral letter. Neurological injury was considered to be spinal if there was a sensory level, Brown–Sequard syndrome, unimodal (sensory or motor) involvement of both legs in com- bination with girdle discomfort or bimodal involvement of both legs with or without girdle discomfort. There was considered to be cerebral involvement if there was disturbance of higher functions (including a fit or syncope), vision or speech, cerebellar signs, or unimodal involvement of an arm and the ipsilateral leg. In some cases there were criteria for both spinal and cerebral involvement on either a single or different episodes. Other cases with mild signs or subjective symptoms, particularly where there was unimodal involvement of one limb without a clear demarcation, were considered to be indeterminate.
Results are expressed as medians and range or mean³S.D. as appropriate. Statistical comparisons were with the Chi-squared test and Student’s t-test. Results were considered significant when P ! 0.05.
The investigations performed on cases (contrast echo- cardiography and lung function tests) were part of normal investigations performed to enable divers to receive advice about future diving. All patients were specifically referred to one of us (P. W.) for these investigations by doctors outside his hospital, and they were performed in accordance with national recommendations as part of a clinical service. The hospital ethics committee approved the review and analysis of data for research purposes. Patients gave written consent to the review and analysis. The historical control subjects used for comparison of shunt size were part of a study published in abstract form which had ethics committee approval, and all gave written consent.
RESULTS
The 100 divers studied had 115 episodes of neurological decompression illness : two divers each had three episodes, eleven divers each had two episodes and 87 divers had a single episode. With regard to lesions, 24 divers had spinal lesions in 26 episodes, 54 divers had cerebral lesions in 66 episodes, 14 divers had spinal and cerebral lesions in 15 episodes, and eight divers had lesions at indeterminate sites in eight episodes.
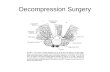
Comparison of the prevalence and size distribution of shunts in divers with a history of neurological decompression illness and in controls Figure 1 shows the prevalence and size of right-to-left shunts detected by the series of six contrast injections in divers with a history of neurological decompression illness and in unaffected control divers. A single injection detected large shunts in 41% of cases and in 4.9% of controls. The detection rates for large shunts were increased to 51% and 7.3% respectively by use of up to six injections. Whether one considered large shunts, large and medium shunts or all shunts, there were significantly more shunts present in the divers who had decompression illness than in the controls, and this difference existed irrespective of the number of contrast injections given (for each comparison, P ! 0.001).
The size criteria used in the present study is an established grading method [25]. Unfortunately it failed to reflect the massive degree of right-to-left shunting seen in many of the individuals with neurological decom- pression illness. In many cases the number of bubbles shunting was impossible to count, but there were clearly many hundreds, if not thousands, of bubbles in the left heart on image frames.
Relationship between large and medium- sized right-to-left shunts and lesion site (spinal or cerebral) in divers with neurological decompression illness In the analyses described below it was only in the 51 divers with large shunts and the one diver with a medium shunt that it was considered that paradoxical gas em- bolism might be the mechanism for decompression illness. The six divers with small shunts (a priori defined as clinically irrelevant shunts) were considered to have suffered decompression illness by other mechanisms. In five of the six cases other mechanisms were found (one each of lung disease, rapid ascent, lung disease with rapid ascent, missed stops, and rapid ascent with missed stops).
# 2000 The Biochemical Society and the Medical Research Society
69Causes of neurological decompression illness
Figure 1 Comparison of prevalence and size of right-to-left shunts measured by contrast echocardiography in patients with neourological decompression illness and in controls Up to six injections of contrast medium were performed.
Table 1 Relationship between causes of neurological decompression illness and lesion site
Cause Spinal Spinal and cerebral Cerebral Indeterminate Total
No large or medium shunt Lung disease only 1 (9%) 2 (18%) 8 (73%) 0 11 Lung disease and rapid ascent 0 0 3 (100%) 0 3 Rapid ascent alone 0 1 (14%) 5 (71%) 1 (14%) 7 Rapid ascent and missed decompression stops 0 0 3 (75%) 1 (25%) 4 Inadequate decompression stops 2 (40%) 0 2 (40%) 1 (20%) 5 Unknown cause : short latencies 3 (25%) 3…
Relationship between the clinical features of neurological decompression
illness and its causes
Peter WILMSHURST* and Philip BRYSON† *The Royal Shrewsbury Hospital, Shrewsbury SY3 8XQ, U.K., and †The Hyperbaric Medical Centre, Tamar Science Park, Plymouth PL6 8BQ, U.K.
A B S T R A C T
There is dispute as to whether paradoxical gas embolism is an important aetiological factor in
neurological decompression illness, particularly when the spinal cord is affected. We performed
a blind case-controlled study to determine the relationship between manifestations of
neurological decompression illness and causes in 100 consecutive divers with neurological
decompression illness and 123 unaffected historical control divers. The clinical effects of
neurological decompression illness (including the sites of lesions and latency of onset) were
correlated with the presence of right-to-left shunts, lung disease and a provocative dive profile.
The prevalence and size of shunts determined by contrast echocardiography were compared in
affected divers and controls. Right-to-left shunts, particularly those which were large and
present without a Valsalva manoeuvre, were significantly more common in divers who had
neurological decompression illness than in controls (P! 0.001). Shunts graded as large or
medium in size were present in 52% of affected divers and 12.2% of controls (P! 0.001). Spinal
decompression illness occurred in 26 out of 52 divers with large or medium shunts and in 12 out
of 48 without (P! 0.02). The distribution of latencies of symptoms differed markedly in the 52
divers with a large or medium shunt and in the 30 divers who had lung disease or a provocative
dive profile. In most cases of neurological decompression illness the cause can be determined by
taking a history of the dive profile and latency of onset, and by performing investigations to
detect a right-to-left shunt and lung disease. Using this information it is possible to advise divers
on the risk of returning to diving and on ways of reducing the risk if diving is resumed. Most cases
of spinal decompression illness are associated with a right-to-left shunt.
INTRODUCTION
Neurological symptoms may occur during or after ascent from a dive, on leaving a caisson or during sub- atmospheric decompression. There has been a call to
Key words : airways obstruction, atrial septal defects, cerebral decompression illness, contrast echocardiography, decompression sickness, gas embolism, lung function tests, patent foramen ovale, pulmonary arteriovenous fistula, pulmonary barotrauma, smoking, spinal decompression illness. Abbreviations : CT, computed tomography. Correspondence: Dr Peter Wilmshurst.
describe all cases using the encompassing term ‘neuro- logical decompression illness ’ [1]. This allows the treating doctor to ascribe a diagnostic label without determining aetiology [1]. Assessment of the risk of recurrence on returning to diving requires knowledge of the cause of an
# 2000 The Biochemical Society and the Medical Research Society
66 P. Wilmshurst and P. Bryson
earlier episode. In most, if not all, cases, decompression illness is caused by gas bubbles. If gas trapping as a result of lung disease or failure to exhale adequately during ascent causes pulmonary barotrauma, bubbles may in- vade the pulmonary veins to become arterial gas emboli. Decompression sickness occurs if ambient pressure is reduced sufficiently below the partial pressure of gas dissolved in tissues for bubbles to form in vivo. A contentious issue is whether such bubbles produce injury by an autochthonous mechanism (causing injury at the site where they are formed) or by embolism. Some cases might result from a combination of mechanisms.
Bubbles are common in the venous circulation after diving, but usually produce no symptoms because they are filtered by the pulmonary capillaries, where the gas diffuses along the concentration gradient into the alveoli. Exceptionally, when the dive profile is very provocative, massive venous gas embolism may overwhelm the filtering capacity of the pulmonary capillaries so that bubbles reach the systemic circulation. It is also possible that bubbles will pass through the pulmonary capillaries if there is transient recompression, as occurs during repetitive dives in a short time period. A case report and observational studies have suggested that paradoxical gas embolism across right-to-left shunts might have a role in the aetiology of some cases of neurological decom- pression sickness after conservative dives [2–4]. Such shunts usually occur across a foramen ovale, but occasionally shunting is through an atrial septal defect or a pulmonary arteriovenous fistula. A blinded case- controlled study showed that right-to-left shunts were particularly associated with neurological symptoms that occurred within 30 min of surfacing [5]. Neurological symptoms usually followed an unprovocative dive in divers who had a shunt, but were usually the result of a provocative dive if divers had no shunt [5]. Data extending these observations and a replication study performed under supervision of members of the Medical Research Council Decompression Sickness Panel have been reported [6,7]. There have been other human and animal studies which support the theory that neurological decompression sickness can be the result of paradoxical gas embolism [8–10]. However, the possibility that this mechanism may be associated with a significant number of cases of neurological decompression illness is contrary to established aetiology theories, and many experts in diving medicine remain unconvinced that paradoxical gas embolism is a numerically important cause of decom- pression illness [11–16]. A large controlled study proposed in 1990 by one of these groups [12] has not yet been published.
One objection is that between one-quarter and one- third of the population, and a similar proportion of divers, have a patent foramen ovale which might allow right-to-left shunting [5,17]. Considerably fewer than a quarter of divers develop decompression illness [18].
Many divers with a demonstrable shunt have no history of decompression illness [5,6,13,14]. Thus the relevance of a patent foramen ovale is disputed. This argument fails to take account of variations in risk based on shunt size, which is dependent on the anatomy and dimensions of the defect and the pressure gradient, and on venous bubble load, which is affected by individual susceptibility to bubble nucleation and the profiles of dives performed. Many dive profiles do not cause venous gas nucleation at a time when critical tissues have sufficient gas content to amplify gas emboli.
A second objection is that the greater blood flow to the brain generally ensures that embolic events in the spinal cord are much less frequent than in the brain, but involvement of the spinal cord is a common manifestation of decompression sickness. The pathological distribution of lesions and the time course of spinal cord decom- pression illness are considered by some to be incom- patible with an embolic mechanism [11,19,20]. This led to the assertion that autochthonous bubbles must be the cause of spinal decompression illness [11]. There is one clinical study in humans which suggests that a patent foramen ovale is not associated with spinal decom- pression illness [10], but it was our impression from our previous studies that spinal decompression illness may be more frequent when the diver has a right-to-left shunt and that, in affected cases, the shunt size is considerably larger than in the general population [5–8,21]. We therefore believed that the role of shunts in the causation of spinal decompression illness may be greater than generally appreciated. There have been cases of spinal cord dysfunction after air embolism following pulmon- ary barotrauma during submarine escape training [22]. Therefore, in the present study, we investigated how shunt size is related to susceptibility to neurological decompression illness, and in particular to spinal lesions. The primary (pre-analysis) aims of the study were : (a) to compare the prevalence and size distribution of right-to- left shunts in divers with a history of neurological decompression illness and in unaffected control divers ; (b) to determine the relationship between large and medium-sized right-to-left shunts and lesion site (spinal or cerebral) in divers with neurological decompression illness ; and (c) to determine what proportions of episodes of neurological decompression illness were related to the presence of cardiac shunts, lung disease or a provocative dive profile.
METHODS
We performed a ‘blind’ retrospective analysis of 100 consecutive divers (34 female ; 91 amateur and nine
# 2000 The Biochemical Society and the Medical Research Society
67Causes of neurological decompression illness
professional) who were assessed following one or more episodes of neurological decompression illness. The first in this cohort was the next case seen after completion of our previous publication [8]. One episode occurred after a dry hyperbaric chamber dive in which air was breathed. The other episodes followed dives in water. One amateur diver had neurological decompression illness after a deep dive breathing trimix (helium, oxygen, nitrogen), with long nitrox (nitrogen and oxygen) decompression stops. All the other episodes of decompression illness followed dives in which air was breathed, but nitrox was used on one of the dives for decompression stops.
The referral and assessment of each amateur diver was in accordance with the Medical Standards of the United Kingdom Sport Diving Medical Committee. These re- quire enquiry into the circumstances of the incident, including the dive profile, and investigations to exclude the presence of physical predisposition (i.e. to exclude a right-to-left shunt and lung disease). The professional divers were referred for the same reason, although there is no formal requirement. The cases studied have not been reported previously, except for six cases reported in description of closure procedures ([23], but see [23a] ; [24]). Of the consecutive cases, 35 were treated for neurological decompression illness at a single centre (The Hyperbaric Medical Centre, Plymouth). The other referrals came from other recom- pression facilities, diving medical referees and general practitioners.
One of us (P.B.) retrospectively reviewed information about symptoms and signs at presentation with de- compression illness to determine the lesion site. This was done blind to knowledge of the results of cardio- respiratory investigations. It was also blind to dive profile, except for the 35 cases from his own centre. Another (P.W.) had previously reported the contrast echocardiography and lung function tests and analysed the dive profile to assign an aetiology label. This was performed blind to categorization of the lesion site. Possible causes of decompression illness were : (a) a clinically relevant (large or medium size) right-to-left shunt (atrial or pulmonary) determined from contrast echocardiography; (b) lung disease predisposing to pul- monary barotrauma determined from lung function tests and chest X-ray; (c) provocative dive (rapid ascent or inadequate decompression, including missed stops and computer malfunction) determined from the history; (d) any combination of these ; (e) unknown cause when there was no shunt or lung disease detected and the dive profile was considered unprovocative.
In all cases, transthoracic contrast echocardiography was performed to detect the presence of a right-to-left shunt and for semi-quantitative assessment of the size of any shunt detected [25]. We always perform contrast echocardiography before reading the referral letter and blind to history and physical findings, to avoid bias in
interpretation. We adhered to this practice for all cases and controls. The heart was imaged (apical four-chamber view) with a Hewlett Packard Sonos 500, 1000 or 2000 machine. Bubble contrast was produced by pushing approx. 5 ml of sterile saline (0.9% NaCl), 0.5 ml of the subject’s blood and 0.5 ml of air back and forth between two syringes connected by a three-way tap until there were no visible bubbles. This mixture was injected through a 21-gauge butterfly needle into a left antecubital vein. The first contrast injection was performed with the subject resting and breathing normally. If no shunt was seen with the first contrast injection, up to five sub- sequent injections were performed with Valsalva manoeuvres, with the operator causing sudden release of the manoeuvre, as described previously [8]. The size of the shunt was graded according to the maximum number of bubbles seen in the left heart on frame-by-frame analysis : small shunts, fewer than six bubbles ; medium shunts, six to 20 bubbles ; large shunts, more than 20 bubbles [25]. On the basis of our previous observations, we believe that small shunts represent a low risk of predisposing to decompression illness, and in the present study they were considered to be clinically irrelevant. Late appearance of bubbles in the left heart was taken to indicate a pulmonary shunt. Such shunts usually appear as a constant stream of bubbles in the left heart, and atrial shunts usually appear as groups of bubbles. When a pulmonary shunt was suspected, additional tests, in- cluding pulse oximetry assessment of orthodeoxia and, in some cases, pulmonary angiography, were performed. The sizes of shunts in the divers with decompression illness were compared with results obtained by the same method in 123 historical control divers who had not had decompression illness. (Some of the results from this population of normal divers have been presented pre- viously as an abstract [26].)
Lung function tests were performed after contrast echocardiography and after determining the latency of symptoms (the interval between surfacing and the first neurological symptom). In 17 cases the late onset of symptoms was considered to exclude pulmonary baro- trauma, and lung function tests were not performed. (Our current practice is to carry out lung function tests in all cases of neurological decompression ill- ness.) The presence of lung disease predisposing to pulmonary barotrauma was assessed by spirometry, flow volume loops and chest X-ray in 83 cases. Evidence of small-airways disease was sought by examination of the flow volume loops, as described previously [8]. The reading of these tests was also performed blind to the history of decompression illness (i.e. before reading the referral letter, taking a history or examining the patient).
The series of dives leading up to the episode of decompression illness was then analysed for provocative events. The series of dives was considered to have started
# 2000 The Biochemical Society and the Medical Research Society
68 P. Wilmshurst and P. Bryson
after the last 48 h dive-free interval prior to the episode of decompression illness. A dive series was considered provocative if the diver had made a rapid ascent or had performed inadequate decompression stops (as required by the decompression table or computer he}she used for the dive series, or if computer malfunction led to missed stops) or there had been both rapid ascent and inadequate decompression stops. Divers were also asked about unusual events during the dives. A history of tobacco smoking was taken.
One of us (P.B.), who regularly treats divers with decompression illness, was responsible for determining whether the neuological injury was spinal, cerebral, both spinal and cerebral, or indeterminate. This categorization was based on pre-treatment symptoms and signs, and was performed blind to knowledge of the presence of right- to-left shunts or lung disease. It was also blind to dive profiles, except in the cases he had treated. In the majority of cases referred from his own centre, P.B. had examined the patients during their acute illness and he based his diagnosis on his own clinical records. In the other cases, information about presenting features was obtained from the notes made by the treating centre or the referral letter. Neurological injury was considered to be spinal if there was a sensory level, Brown–Sequard syndrome, unimodal (sensory or motor) involvement of both legs in com- bination with girdle discomfort or bimodal involvement of both legs with or without girdle discomfort. There was considered to be cerebral involvement if there was disturbance of higher functions (including a fit or syncope), vision or speech, cerebellar signs, or unimodal involvement of an arm and the ipsilateral leg. In some cases there were criteria for both spinal and cerebral involvement on either a single or different episodes. Other cases with mild signs or subjective symptoms, particularly where there was unimodal involvement of one limb without a clear demarcation, were considered to be indeterminate.
Results are expressed as medians and range or mean³S.D. as appropriate. Statistical comparisons were with the Chi-squared test and Student’s t-test. Results were considered significant when P ! 0.05.
The investigations performed on cases (contrast echo- cardiography and lung function tests) were part of normal investigations performed to enable divers to receive advice about future diving. All patients were specifically referred to one of us (P. W.) for these investigations by doctors outside his hospital, and they were performed in accordance with national recommendations as part of a clinical service. The hospital ethics committee approved the review and analysis of data for research purposes. Patients gave written consent to the review and analysis. The historical control subjects used for comparison of shunt size were part of a study published in abstract form which had ethics committee approval, and all gave written consent.
RESULTS
The 100 divers studied had 115 episodes of neurological decompression illness : two divers each had three episodes, eleven divers each had two episodes and 87 divers had a single episode. With regard to lesions, 24 divers had spinal lesions in 26 episodes, 54 divers had cerebral lesions in 66 episodes, 14 divers had spinal and cerebral lesions in 15 episodes, and eight divers had lesions at indeterminate sites in eight episodes.
Comparison of the prevalence and size distribution of shunts in divers with a history of neurological decompression illness and in controls Figure 1 shows the prevalence and size of right-to-left shunts detected by the series of six contrast injections in divers with a history of neurological decompression illness and in unaffected control divers. A single injection detected large shunts in 41% of cases and in 4.9% of controls. The detection rates for large shunts were increased to 51% and 7.3% respectively by use of up to six injections. Whether one considered large shunts, large and medium shunts or all shunts, there were significantly more shunts present in the divers who had decompression illness than in the controls, and this difference existed irrespective of the number of contrast injections given (for each comparison, P ! 0.001).
The size criteria used in the present study is an established grading method [25]. Unfortunately it failed to reflect the massive degree of right-to-left shunting seen in many of the individuals with neurological decom- pression illness. In many cases the number of bubbles shunting was impossible to count, but there were clearly many hundreds, if not thousands, of bubbles in the left heart on image frames.
Relationship between large and medium- sized right-to-left shunts and lesion site (spinal or cerebral) in divers with neurological decompression illness In the analyses described below it was only in the 51 divers with large shunts and the one diver with a medium shunt that it was considered that paradoxical gas em- bolism might be the mechanism for decompression illness. The six divers with small shunts (a priori defined as clinically irrelevant shunts) were considered to have suffered decompression illness by other mechanisms. In five of the six cases other mechanisms were found (one each of lung disease, rapid ascent, lung disease with rapid ascent, missed stops, and rapid ascent with missed stops).
# 2000 The Biochemical Society and the Medical Research Society
69Causes of neurological decompression illness
Figure 1 Comparison of prevalence and size of right-to-left shunts measured by contrast echocardiography in patients with neourological decompression illness and in controls Up to six injections of contrast medium were performed.
Table 1 Relationship between causes of neurological decompression illness and lesion site
Cause Spinal Spinal and cerebral Cerebral Indeterminate Total
No large or medium shunt Lung disease only 1 (9%) 2 (18%) 8 (73%) 0 11 Lung disease and rapid ascent 0 0 3 (100%) 0 3 Rapid ascent alone 0 1 (14%) 5 (71%) 1 (14%) 7 Rapid ascent and missed decompression stops 0 0 3 (75%) 1 (25%) 4 Inadequate decompression stops 2 (40%) 0 2 (40%) 1 (20%) 5 Unknown cause : short latencies 3 (25%) 3…
Related Documents