Recovery of neurocognitive functions following sustained abstinence after substance dependence and implications for treatment Mieke H.J. Schulte a,b, ⁎, Janna Cousijn a,e , Tess E. den Uyl a , Anna E. Goudriaan b,c , Wim van den Brink b , Dick J. Veltman d , Thelma Schilt a , Reinout W. Wiers a a Addiction, Development, and Psychopathology (ADAPT) lab, Department of Psychology, University of Amsterdam, Weesperplein 4, 1018 XA Amsterdam, The Netherlands b Amsterdam Institute for Addiction Research (AIAR), Department of Psychiatry, Academic Medical Center, University of Amsterdam, Meibergdreef 5, 1105 AZ Amsterdam, The Netherlands c Arkin Mental Health Care, Amsterdam, The Netherlands d VU University Medical Center, Amsterdam, The Netherlands e Department of Developmental Psychology and Psychonomics, Utrecht University, Utrecht, The Netherlands HIGHLIGHTS • Review of prospective studies on neurocognitive recovery after sustained abstinence. • Literature on neurocognitive recovery after sustained abstinence is scarce. • Few conclusions regarding recovery of neurocognitive functioning can be drawn. • Some cognitive functions (partially) recover after long-term abstinence. • Treatment possibilities range from cognitive training to stimulating the brain. abstract article info Article history: Received 24 February 2014 Revised 19 June 2014 Accepted 14 August 2014 Available online 20 August 2014 Keywords: Addiction Clinical implications Neuropsychology Recovery Substance dependence Background: Substance Use Disorders (SUDs) have been associated with impaired neurocognitive functioning, which may (partly) improve with sustained abstinence. New treatments are emerging, aimed at improving cognitive functions, and being tested. However, no integrated review is available regarding neurocognitive recovery following sustained abstinence. Objectives: In this review, results from prospective studies on neurocognitive recovery using neuropsychological assessments before and after sustained abstinence from SUDs are summarized and discussed. Results: Thirty-five prospective studies were selected for this review, including twenty-two alcohol, three cannabis, four cocaine, three (meth)amphetamine, and three opioid studies. Results suggest that some cognitive functions (partially) recover after sustained abstinence, and that there are predictors of an unfavorable course such as poly-substance use and number of previous detoxifications. Conclusions: Prospective studies indicate that sustained abstinence after SUDs generally results in (partial) neurocognitive recovery. However, a final answer regarding full recovery awaits prospective studies with neurocognitive assessments before, during, and after sustained abstinence from SUDs. New interventions that might enhance neurocognitive recovery after abstinence are discussed, including neurocognitive training, medication and neuromodulation. © 2014 Published by Elsevier Ltd. Contents 1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 532 2. Methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533 3. Prospective studies on recovery of neurocognitive functioning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533 3.1. Alcohol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533 3.2. Group comparison studies on recovery after alcohol dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 534 3.3. Group by time comparison studies on recovery after alcohol dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 535 Clinical Psychology Review 34 (2014) 531–550 ⁎ Corresponding author at: Weesperplein 4, 1018 XA Amsterdam, The Netherlands. Tel.: +31 20 8913704. E-mail address: [email protected] (M.H.J. Schulte). http://dx.doi.org/10.1016/j.cpr.2014.08.002 0272-7358/© 2014 Published by Elsevier Ltd. Contents lists available at ScienceDirect Clinical Psychology Review

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Clinical Psychology Review 34 (2014) 531–550
Contents lists available at ScienceDirect
Clinical Psychology Review
Recovery of neurocognitive functions following sustained abstinenceafter substance dependence and implications for treatment
Mieke H.J. Schulte a,b,⁎, Janna Cousijn a,e, Tess E. den Uyl a, Anna E. Goudriaan b,c, Wim van den Brink b,Dick J. Veltman d, Thelma Schilt a, Reinout W. Wiers a
a Addiction, Development, and Psychopathology (ADAPT) lab, Department of Psychology, University of Amsterdam, Weesperplein 4, 1018 XA Amsterdam, The Netherlandsb Amsterdam Institute for Addiction Research (AIAR), Department of Psychiatry, Academic Medical Center, University of Amsterdam, Meibergdreef 5, 1105 AZ Amsterdam, The Netherlandsc Arkin Mental Health Care, Amsterdam, The Netherlandsd VU University Medical Center, Amsterdam, The Netherlandse Department of Developmental Psychology and Psychonomics, Utrecht University, Utrecht, The Netherlands
H I G H L I G H T S
• Review of prospective studies on neurocognitive recovery after sustained abstinence.• Literature on neurocognitive recovery after sustained abstinence is scarce.• Few conclusions regarding recovery of neurocognitive functioning can be drawn.• Some cognitive functions (partially) recover after long-term abstinence.• Treatment possibilities range from cognitive training to stimulating the brain.
⁎ Corresponding author at: Weesperplein 4, 1018 XA AE-mail address: [email protected] (M.H.J. Schulte).
http://dx.doi.org/10.1016/j.cpr.2014.08.0020272-7358/© 2014 Published by Elsevier Ltd.
a b s t r a c t
a r t i c l e i n f oArticle history:
Received 24 February 2014Revised 19 June 2014Accepted 14 August 2014Available online 20 August 2014Keywords:AddictionClinical implicationsNeuropsychologyRecoverySubstance dependence
Background: Substance Use Disorders (SUDs) have been associated with impaired neurocognitive functioning,which may (partly) improve with sustained abstinence. New treatments are emerging, aimed at improvingcognitive functions, and being tested. However, no integrated review is available regarding neurocognitiverecovery following sustained abstinence.Objectives: In this review, results from prospective studies on neurocognitive recovery using neuropsychologicalassessments before and after sustained abstinence from SUDs are summarized and discussed.Results: Thirty-five prospective studies were selected for this review, including twenty-two alcohol, threecannabis, four cocaine, three (meth)amphetamine, and three opioid studies. Results suggest that some cognitivefunctions (partially) recover after sustained abstinence, and that there are predictors of an unfavorable coursesuch as poly-substance use and number of previous detoxifications.Conclusions: Prospective studies indicate that sustained abstinence after SUDs generally results in (partial)
neurocognitive recovery. However, a final answer regarding full recovery awaits prospective studies withneurocognitive assessments before, during, and after sustained abstinence from SUDs. New interventions thatmight enhance neurocognitive recovery after abstinence are discussed, including neurocognitive training,medication and neuromodulation.© 2014 Published by Elsevier Ltd.
Contents
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5322. Methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5333. Prospective studies on recovery of neurocognitive functioning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533
3.1. Alcohol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5333.2. Group comparison studies on recovery after alcohol dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5343.3. Group by time comparison studies on recovery after alcohol dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 535
msterdam, The Netherlands. Tel.: +31 20 8913704.
532 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
3.4. Studies using multiple dependent groups with different lengths of abstinence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5353.5. Moderating factors in alcohol dependence studies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5353.6. Conclusion on recovery after alcohol dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 535
4. Substances other than alcohol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.1. Cannabis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.2. Group by time comparison studies on recovery after heavy cannabis use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.3. Cocaine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.4. Group comparison studies on recovery after cocaine dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.5. Group by time comparison studies on recovery after cocaine dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5414.6. Studies using multiple dependent groups with different lengths of abstinence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5424.7. Methamphetamine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5434.8. Group comparison studies on recovery after methamphetamine dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5434.9. Group by time comparison studies on recovery after methamphetamine dependence . . . . . . . . . . . . . . . . . . . . . . . . . 5434.10. Opiates . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5444.11. Group comparison studies on recovery after opiate dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5444.12. Studies using multiple dependent groups with different lengths of abstinence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5444.13. Moderating factors for studies on drugs other than alcohol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5444.14. Conclusions on recovery after drug dependence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 544
5. Discussion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5455.1. Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 545
6. Discussion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5456.1. Future research . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5466.2. Enhancing recovery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5466.3. Training neurocognitive functions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 546. Pharmacological treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5476.4. Neuromodulation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 547
7. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 547Acknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 547References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 547
1. Introduction
In recent years, Substance Use Disorders (SUDs), or addictionsto psychoactive substances, have often been characterized aschronic brain diseases that result from long-term exposure to psy-choactive drugs to the brain (Leshner, 1997; Volkow & Li, 2005).Although this perspective dominates the biomedical literature (aswitnessed by a recent editorial in Nature (Nature, 506:6)), it shouldbe noted that there are alternative theories of SUDs from a varietyof social sciences (sociology, history, psychology, behavioral eco-nomics) in which persistent changes of the brain are not the defin-ing feature (e.g., Heyman, 2009; Orford, 2001). In these alternativeconceptualizations, the continuity between addiction and otherexcessive behaviors is stressed and spontaneous recovery is em-phasized. This does not exclude the possibility that for somesubstances and/or some individuals prolonged heavy use of psy-choactive substances is indeed accompanied by persistent cogni-tive and brain changes (for a recent discussion on this topic seeCunningham & McCambridge, 2012). The main goal of this paperis to systematically review the extent to which cognitive functionsrecover after prolonged abstinence from drugs in formerly addictedpeople. A brief note on terminology: in the DSM-5 (American Psy-chiatric Association, 2013), the category of disorders centralin this paper is labeled substance-related and addictive disorders,including pathological gambling (not included in the present re-view, which focused on recovery from substance dependence).SUDs are now scored on a continuous scale with a severity score in-dicating the number of criteria met out of 11. These criteria are thecombined criteria of the previously separate criteria for substanceabuse (4) and substance dependence (7), with one replacement(craving instead of recurring problems with the law). However,all papers reviewed here used previous versions of the DSM to char-acterize participants, therefore we will adapt the same terminologyas in almost all of the reviewed papers: substance dependence (ex-cept for cannabis, see below).
Themain reason for this review is that an abundance of studies haveshown associations between substance dependence and a variety ofneurocognitive impairments. The term neurocognitive here refers toboth behavioral (as measured with questionnaires and behavioraltasks) and neural measures (as measured with for instance fMRI) ofcognitive functions. Some neurocognitive impairments appear to begeneral to all SUDswhereas other dysfunctionsmay bemore specificallylinked to a certain substance of abuse (Fernández-Serrano, Pérez-García, & Verdejo-García, 2011). Although neurocognitive impairmentshave been well profiled in various substance use disorders, much less isknown about the persistence of such deficits. Importantly, from a clini-cal perspective, successful recovery of cognitive impairments has beenfound to predict treatment response and stable abstinence (review:Bates, Buckman, & Nguyen, 2013). Hence, a better understanding ofwhich neurocognitive deficits are found in different SUDs, and whichones may recover, is of direct clinical relevance. In addition, these func-tions may further be targeted by recently developed training modules(e.g. Eberl et al., 2013; Houben, Wiers, & Jansen, 2011; Schoenmakerset al., 2010).
The current review aims to investigate recovery of neurocognitivefunctions following a period of sustained abstinence from substanceuse in substance dependent individuals and to discuss implicationsfor treatment directed at enhancing neurocognitive recovery.Within the context of this review, the term recovery refers to sig-nificant improvement as well as to return to normal functioningof cognitive functions and their neural correlates. To investigateneurocognitive recovery following abstinence, studies should ide-ally take into account two important issues. First of all, any residualneurotoxic damage caused by excessive drug use needs to be dis-tinguished from the sub-acute (pharmacological) effects of drugs(see Fernández-Serrano et al., 2011). In order to make this distinction,a minimum of two weeks of abstinence at one of the assessments is re-quired concerning dependence to alcohol, cocaine, (meth)amphet-amines and opiates. However, for cannabis a longer minimum periodof four weeks is required given its longer lasting sub-acute cognitive
533M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
and neural effects (Pope, Gruber, Hudson, Huestis, & Yurgelun-Todd,2001; Schweinsburg et al., 2010). Second, it is important to study cogni-tive functions of substance dependent groups at different lengths of ab-stinence and to compare the findings with cognitive functioning ofhealthy controls, to see how recovery progresses during course ofabstinence.
A number of review papers have focused on cognitive functioningafter substance dependence, but these reviews are limited in someway. They either did not specifically exclude possible sub-acute effects(Fernández-Serrano et al., 2011), only focused on particular substances(e.g., Badiani, Belin, Epstein, Calu, & Shaham, 2011; Stavro, Pelletier,& Potvin, 2013), focused on cross-sectional studies (e.g., Van Holst &Schilt, 2011), or focused on the effects of cognitive recovery ontreatment outcome (Bates et al., 2013). The present review paperdistinguishes itself from previous review papers by systematicallyreviewing 1) prospective neurocognitive studies that includedmore than one neurocognitive assessment in substance dependentpatients (i.e. before and after a period of abstinence) compared tohealthy controls and 2) studies testing multiple groups of patientswith a substance use disorder at different lengths of abstinencecompared to healthy controls. It is important to note that this reviewdoes not include prospective studies measuring cognitive function-ing prior to substance use in people who later became dependent,but focuses on recovery after abstinence. Another important noteis the possible effect of poly-substance use. The studies included inthis review have dealt with this possible confounding factor in dif-ferent ways, for instance by excluding participants that reported ortested positive for the use of multiple substances, or by reportingthe extent by which other substances are used. This information isincluded in the tables. Moreover, to account for sub-acute effectsof substance use, only studies in which subjects were abstinent fora minimum period of two weeks at least at one of the assessmentswere included. Some studies contained more than two assessments.In order to investigate recovery, studies were included in which atleast one of the assessments took place at two-week abstinence ormore. For cannabis slightly broader inclusion criteria were used(heavy use irrespective of dependence) than for other substances.The reason is that in many Western countries the general opinionhas long been that cannabis is not addictive, and therefore no treat-ment was offered for people with cannabis use related problems.Even though the demand for and the supply of treatment has mark-edly increased the past decades (UNODC, world drug report, 2012),this shift is not yet discernible in the literature, and most studies onthe neurocognitive consequences of cannabis have been performedin heavy cannabis users not seeking treatment, instead of peoplewith an established diagnosis of cannabis dependence.
After systematically reviewing the studies included, which focus onrecovery of functions after prolonged abstinence, we discuss recentdevelopments to enhance neurocognitive recovery through variousforms of neurocognitive training, medication or neuromodulationtechniques. It is important to first establish natural recovery of func-tions after abstinence, before discussing novel techniques which mayenhance neurocognitive recovery.
2. Methods
A literature search in Pubmed was performed for the followingsubstances: alcohol, cannabis, (meth-)amphetamine, cocaine, GHB,ketamine, ecstasy/MDMA, opiates, and LSD. The following searchterms were used in combination with every substance: (dependenceOR addiction) AND (neuropsychol* OR cognition OR craving ORrecovery OR abstinence OR intelligence OR IQ OR attention OR mem-ory OR executive funct* OR (f)MRI OR DTI OR VBM ORMRS OR CT ORPET OR SPECT OR EEG OR ERP OR spectroscopy OR neuroimaging ORneurophysiology). When different terms are used for a substance(e.g., alcohol, ethanol), all were entered in the search strategy.
The following selection criteria were used: (1) longitudinal stud-ies with at least two neurocognitive measurements, of which at leastone was assessed during abstinence, or inclusion of at least two sub-stance dependent groups with differing lengths of abstinence,(2) published between the year 2000 and June 2013 (including papersahead of print), following the suggestion by Fernández-Serrano et al.(2011) to include studies that were published after the surge of con-temporary neuroscientific models of addiction, (3) reporting on re-covery of neuropsychological functions or craving, or on the use ofneurobiological measures relating to neuropsychological functions,craving or clinical outcome, (4) at least 24 participants of which atleast 12 dependent participants at baseline (when applicable),based on DSM or ICD criteria. For cannabis, participants had to usecannabis at least 5 times a week for the last two years, since moststudies investigating neurocognitive deficits in cannabis users onlyobserve deficits in the heaviest users (e.g. Cousijn et al., 2013),(5) a minimum abstinence duration of two weeks (at least 4 weeksfor cannabis), and (6) a measure of comparison using a control groupor a regression analysis using abstinence duration.
The search resulted in 4555 hits, of which 108 articles were se-lected based on information provided in the abstract. These articleswere then critically studied to determine whether they indeed metthe selection criteria for this review, ultimately resulting in 35 eligi-ble articles about alcohol, cannabis, (meth)amphetamine, cocaine,and opiates. There were no eligible studies on GHB, ecstasy/MDMA,or LSD. The resulting number of studies is displayed in Table 1 anda detailed overview of the studies is presented in Tables 3–7, with in-formation on participants, study design, and recovery of cognitivefunctioning. Studies that did not meet the selection criteria (e.g., nocontrol group, small sample, double countings, no experimentaltasks) are not discussed.
A pragmatic classification of cognitive domains and sub-domainswas used (Table 2), that was similar to the classification used in a previ-ous review by (Fernández-Serrano et al., 2011). An important drawbackof any classification is that there is overlap between the various domainsand sub-domains. Moreover, not all neurocognitive tasks are specificindicators of particular neuropsychological functions. For example,working memory, which is currently regarded to be a central executivefunction (Friedman et al., 2008; Kane, Bleckley, Conway, & Engle, 2001;Miyake et al., 2000), is treated as a memory factor in older studies.Moreover, for the assessment of working memory, often a combinedscore of “digit-span forward” and “digit-span backward” is used.However, the former is not an indicator of working memory (but ofshort termmemory),whereas the latter is (i.e.manipulation of informa-tion in the short termmemory). Finally, it should be noted thatworkingmemory is strongly related to performance IQ (Kane & Engle, 2002),which complicates “controlling for IQ” when comparing groups with adifferent IQ.
In the following paragraphs, longitudinal studies on neurocognitiverecovery following sustained abstinence will be discussed persubstance. It is important to note that not all studies used a longitudinaldesign for the control group, and thus practice effects in the SUD groupcannot be excluded as a possible explanation for “recovery” effects insuch studies. We therefore distinguish between “group comparisonstudies” without a longitudinal design for the control group, “group bytime comparison studies” with a longitudinal design for the controlgroup, and studies with multiple substance dependent groups withdiffering lengths of abstinence.
3. Prospective studies on recovery of neurocognitive functioning
3.1. Alcohol
Twenty-two studies investigating recovery after alcohol depen-dence were included. In five studies the control group was testedonly once. Therefore, it cannot be excluded that improvements in
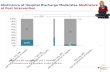
Table 1Number of studies resulting from the literature search.
Alcohol Cannabis Cocaine (Meth-) amphetamine Opiates GHB Ketamine XTC/MDMA Total
Hits 2321 191 658 464 857 7 34 23 4555Inspected 56 9 23 14 6 0 0 0 108Included 22 3 4 3 3 0 0 0 35
534 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
neurocognitive functions of dependent participants represent prac-tice effects. The remaining studies took practice effects and/or natu-ral course effects into account by either testing the control group atleast twice (16 studies), or by using multiple dependent groupswith differing lengths of abstinence (1 study). The details of thesestudies are displayed in Table 3.
3.2. Group comparison studies on recovery after alcohol dependence
These studies show improvement or even complete recovery tonormal performance (compared to the performance of healthy con-trols) in several cognitive domains, including visual short-term
Table 2Subdivision of cognitive functions: main domains and sub-domains.
Main domain Sub-domain Abbreviation Tasks
Learning & memory Episodic Memory EM FCSRTSemantic Memory SMNon-Declarative Memory ndMAssociative Memory AM PALVerbal short term memory Verbal STM BPDP,Verbal long term memory Verbal LTM BSRT,Visual short term memory Visual STM BPDP,Visual long term memory Visual LTM BVMT
Attention Selective Attention SA CPT, DSustained Attention SUAT CPT, DDivided Attention DA DAT, PPrimed selective attention Primed SA CCPT
Executive functions Working Memory WM BDS, Bseque
Abstraction Abilities AA CFT, CUpdating U HCT, LFlexibility F ARAAInhibition I CPT, HImpulsive Action IA IGTDecision Making DM IGTPlanning P SOCVerbal Fluency VF COWA
Fine motor functioning FMF FFMT,Processing speed PS D2 tesSpatial processing Visuospatial skills VS DL, HFIntelligence Performance IQ pIQ WASI
General IQ gIQ WARDVerbal IQ vIQ WAIS-
Emotion and affect Emotional Facial Expression Recognition EFER EFETEmotion Regulation ER DERSPositive Affect PA PANANegative Affect NA PANACraving Cr DDQ,
Tasks: ARAAT, Alternative Response subtest of Attentional Assessment Test; BDS, Backward DigTest; BVMT, Brief Visual Memory Test; BVRT, Benton Visual Retention Test; CCPT, ComputarizeAssociation Test; CPT, Cognitive Performance Test; CT, Categories Test; CVLT, California Verbafor Drugs Questionnaire; DERS, Difficulties in Emotion Regulation Scale; DL, Discrimination Leanition; EFET, Emotional Facial Expression Test; FAS, Verbal Fluency Test; FCSRT, Free and Cued SFigure Position Test; GPB, Grooved Peg Board; HCT, Halstead Category Test; HCST, Hayling SentIntra/ExtraDimensional Set Shift; IGT, IowaGambling Task; LFT, Letter Fluency Task; LPT, LogicaScreening Test; MT immediate, Memory Test immediate recall; NWM, NumericWorking MemScale; PAL, Paired Associates Learning; PASAT, Paced Auditory Serial Addition Test; PRM, PatterComplex Figure; RTT, Reaction Time Test; SAT, Sustained Attention Task; SCT, Short Categoriestest; SWM, Spatial Working Memory test; TMT-A/B, Trail Making Test part A/B; VAS, Visual AWechsler Adult Intelligence Scale; WASI, Wechsler Abbreviated Scale of Intelligence; WCST, WWechsler Memory Scale 3rd edition Verbal Paired Associates test.
memory, visual long-term memory, verbal IQ, verbal fluency, and epi-sodic memory (Fujiwara, Brand, Borsutzky, Steingass, & Markowitsch,2008; Gazdzinski et al., 2008; Moriyama, Muramatsu, Kato, Mimura, &Kashima, 2006; Pitel et al., 2009).
Furthermore, using structuralMagnetic Resonance Imaging (MRI), itwas found that an increase in hippocampal volumepositively correlatedwith visual short term memory and visual long term memory(Gazdzinski et al., 2008). Since the hippocampus is critically involvedin several memory functions, this may indicate a biomarker forimproved memory functions.
Several cognitive functions are reported to show no improve-ments, including visuospatial skills, divided attention, sustained
, HVLT, WMS-III VPA
BSRT, CVLT, MC, MT immediate, R-AVLT, WISC-R digit span, WMS digit span forwardCVLT, MC, WMS-III VPABVMT, BVRT, FPT, PRM, WAIS-III symbol search, BVRT, R-OCF delayed2 test, Stroop, MC, WAIS-III symbol searchVT, FDS, MC, PASAT, SATASAT, RTT, SDM
PDP, FPT, MC, NWM, SST, SWM, VST, WAIS-III arithmetic, WAIS-III letter numberncing, WISC-R arithmetic/digit span, WMS digit span backwardT, MC, SCT, WAIS-III similarities, WISC-R similaritiesPT, SCT, WAIS-III similarities, WCST, WISC-R similaritiesT, HCT, IED, SCT, TMT-B, WAIS-III symbol search, WCSTCST, MC, Stroop
T, FAS, LFT, VFTGPB, MSTt, MC, MST, PASAT, SDM, Stroop, TMT-A, WAIS-III symbol searchT, MC, R-OCF copy, SDM, WAIS block design, WISC-R block designmatrix reasoning7-IQ, WASI vocabularyIII information, WISC-R vocabulary
SSOCDS, VAS
it Span; BPDP, Brown-Peterson Distractor Paradigm; BSRT, Buschke's Selective Remindingd Contextual Priming Task; CFT, Categorical Fluency Task; COWAT, Controlled Oral Wordl Learning Test; D2 test, D2 cancellation test; DAT, Divided Attention Task; DDQ, Desiresrning; DRS, Dementia Rating Scale; DVT, Digit Vigilance Test; DWR, Delayed Word Recog-elective Reminding Test; FDS, Forward Digit Span; FFMT, Fine Finger Movement Test; FPT,ence Completion Test; HFT, Hidden Figures Test; HVLT, Hopkins Verbal Learning Test; IED,l Problems Test;MC,MicroCog;MT immediate,Memory Test immediate recall;MST,Motorory test; OCDS, Obsessive Compulsive Drinking Scale; PANAS, Positive And Negative Affectn Recognition Memory; R-AVLT, Rey Auditory Verbal Learning Test; R-OCF, Rey-OsterriethTest; SDM, Symbol Digit Modalities; SST, Spatial Span Task; SOC, Stockings of Cambridgenalog Scale; VFT, Verbal Fluency Test; VST, Verbal Span Task; VT, Vocabulary Test; WAIS,isconsin Card Sorting Task; WISC, Wechsler Intelligence Scale for Children; WMS-III VPA,
535M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
attention, verbal short term memory, and craving (Gazdzinskiet al., 2008; Heinz et al., 2005; Moriyama et al., 2006; Pitel et al.,2009). Also, mu-opioid receptor availability did not normalizeafter five weeks of abstinence, with alcohol dependent subjectsshowing a persistently greater availability compared to controls(Heinz et al., 2005). This is of relevance, because mu-opioidreceptor availability showed a positive correlation with craving(Heinz et al., 2005), possibly indicating that an increase in theavailability of this receptor could be a biomarker for the urge toconsume alcohol.
Inconsistent findings were found for several cognitive functions,including processing speed, working memory, selective attention,inhibition, and flexibility (Gazdzinski et al., 2008; Moriyama et al.,2006; Pitel et al., 2009). These inconsistencies could be the result ofmethodological issues, such as the use of different tests across studiesto investigate a particular neurocognitive function.
3.3. Group by time comparison studies on recovery after alcoholdependence
After controlling for practice effects by testing the control groupmore than once, sustained abstinence in alcohol-dependentpatients was found to improve an array of cognitive functions, in-cluding inhibition, craving, associative memory, general IQ, perfor-mance IQ, verbal memory, and negative and positive affect (Bartschet al., 2007; Bendszus et al., 2001; Cordovil De Sousa Uva et al.,2010; Durazzo, Rothlind, Gazdzinski, Banys, & Meyerhoff, 2007;Manning et al., 2008; Rosenbloom et al., 2007). In the study byRosenbloom et al. (2007), memory was also found to improve inhealthy controls, indicating the presence of practice effects. How-ever, the study also showed a negative association between mem-ory improvement and lateral ventricular volume in abstinentalcoholics, but not in the controls, suggesting a positive effect ofabstinence on memory through neural recovery. A similar associa-tion between abstinence related improvement in short term mem-ory and shrinkage of the third ventricle was found by Sullivan,Rosenbloom, Lim, and Pfefferbaum (2000). In structural MRI stud-ies, an increase in insular and cingulate cortex volume was ob-served in abstinent alcohol dependent patients, as well as adecrease in cerebrospinal fluid (CSF; Bendszus et al., 2001;Demirakca et al., 2011). Tissue volume gain has also been reportedby Cardenas, Studholme, Gazdzinski, Durazzo, and Meyerhoff(2007). Furthermore, a 1H-MRS study showed an increase in cho-line and NAA that positively correlated with neurocognitive per-formance (Bendszus et al., 2001). Together, these results indicatethat alterations in brain structures may index cognitive recovery.
There was no abstinence related improvement reported for decisionmaking, semantic memory, sustained attention, impulsive action,emotional facial expression recognition, planning, and verbal IQ(Cordovil De Sousa Uva et al., 2010; Foisy et al., 2007; Loeber et al.,2010; Manning et al., 2008; Rosenbloom et al., 2007; Sullivan et al.,2000). For decision making it has to be noted that there were nodifferences with the control group at either time point (Loeber et al.,2010), indicating that there was no deterioration in this particularcognitive function.
Inconsistent findings have been reported for processing speed,fluency, verbal short term memory, verbal long term memory, visualshort term memory, visual long term memory, verbal fluency, abstrac-tion abilities, updating, visuospatial skills, working memory, episodicmemory, language, and fine motor functioning (Bartsch et al., 2007;Bendszus et al., 2001; Block, Erwin, & Ghoneim, 2002; Cordovil DeSousa Uva et al., 2010; Durazzo et al., 2007; Hanson, Medina, Padula,Tapert, & Brown, 2011; Loeber et al., 2010; Manning et al., 2008; Monet al., 2013; Rosenbloom, Pfefferbaum, & Sullivan, 2004; Sullivan et al.,2000).
3.4. Studies using multiple dependent groups with different lengths ofabstinence
One study controlled for possible practice effects by comparinggroups with different lengths of abstinence. Only the group with thelongest period of abstinence (more than 6 months) experienced noprimed selective attention in a computerized contextual priming taskwith alcohol cues (Feldtkeller, Weinstein, Cox, & Nutt, 2001). Thisindicates that with prolonged abstinence, alcohol dependent subjectsmay become less vulnerable to alcohol cues in their environment.
3.5. Moderating factors in alcohol dependence studies
Several factors complicate the interpretation of studies on recov-ery. Poorer baseline performance on neurobiological measures werefound to be related to greater recovery, possibly because there ismore room for recovery with greater impairment (Cardenas et al.,2007; Gazdzinski, Durazzo, & Meyerhoff, 2005). Poor performanceon visuospatial construction was associated with cumulative alco-hol use and drug withdrawal in polysubstance users (Hansonet al., 2011), whereas tissue volume alterations and alterations inneurometabolites over time were modulated by duration of absti-nence as well as recency and severity of drinking (Bartsch et al.,2007; Bendszus et al., 2001; Cardenas et al., 2007; Gazdzinskiet al., 2005; Rosenbloom et al., 2007). Furthermore, the number ofdetoxifications had a negative impact on recovery (Fujiwara et al.,2008; Pitel et al., 2009). Participants with less than two detoxifica-tions showed greater recovery of decision making and impulsive ac-tion compared to those with two or more detoxifications (Loeberet al., 2010). Another factor is a family history of alcohol depen-dence. Cognitive recovery was less evident in the alcohol dependentgroup with a positive family history of alcohol use disorders(Moriyama et al., 2006). One reason could be that family history ofalcohol use disorder has also been associated with suboptimal de-velopment of cognitive functions (especially executive functions,Peterson, Finn, & Pihl, 1992), hence lack of recovery may indicateweaker development before the onset of a SUD.
Finally, smokingmay hinder recovery, as heavy smoking is associat-ed with less recovery over time (Durazzo et al., 2007). However, somestudies also report no additional effect of smoking on cognitive or neu-robiological recovery (Gazdzinski et al., 2008). Thus, these factors areimportant to take into account when interpreting the literature andwhen treating alcohol dependence.
3.6. Conclusion on recovery after alcohol dependence
From the included literature it appears that the only consistentfinding across the three types of studies concerns sustained atten-tion, which appears to improve with prolonged abstinence. Howev-er, when looking within these types of studies, the findings appearto be ambiguous. Findings in the domains of memory, attention, cog-nitive processing speed, working memory and other executive func-tions are inconsistent, i.e. both recovery and persistent dysfunctiondespite sustained abstinence has been reported. Neural correlatesof cognitive recovery were also reported (Bartsch et al., 2007), in-cluding increases in neurometabolites, decreases in ventricular vol-ume and increases in regional brain volumes (Gazdzinski et al.,2008; Sullivan et al., 2000). These inconsistencies exist betweenstudies that do and do not control for practice effects, but also withinthese study designs, and could be due to numerous reasons, such assubject characteristics, assessment tools, etc. Selective recoverycould result from pre-existing factors, increasing the vulnerabilityof developing an addiction. For example, functions such as impulsecontrol, working memory and IQ have been found to predict the de-velopment of addiction (Penick et al., 2010).
Table 3Longitudinal neurocognitive studies on alcohol dependence. Cognitive functions in bold emphasize improvements with a significance level of at least p b0.05.
Article Design Subjects, N(male) Abstinence,Mean (SD)
Duration ofabuse, mean(SD)
Quantity of use,mean (SD)
Technique Tasks Cognitivefunctions/NIfactor
No improvement/improvement
Bartsch et al.(2007)
T1 & T2 Alcohol Dependent: 15(10) T1: ≤1 wT2: 6/7 w
12(7)y 10 g/d NP D2-test SA SAPS PS
1H-MRS – Cho ↑ FrontomesialCho x ↑SA or ↑PS
T1 & T1 + 34–60 d
Healthy controls: 10(6) – – ?
↑ CerebellarCho x ↑SA or ↑PS
– NAA ↑ FrontomesialNAA x ↑SA and ↑PS↑CerebellarNAA x ↑SA or ↑ PS
MRI – PBVC ↑PBVC x ↑SA or ↑PSBendszus et al.(2001)
T1 & T2 Alcohol dependent: 17(11) T1: 1–3 d 9.9(6.2) y 26.9(12.7) d/3 m NP D2-test SA SAPS PST1 & T2 Healthy controls: 12(7) T2: 36–39 d – –
R-AVLT Verbal STM Verbal STM1H-MRS – NAA ↑ cerebellar NAA x ↑SA and ↑PS
↑NAA x ↑LTMMRI – CSF CSF x NP
Block et al. (2002) T1 & T2 Substance users: 56(33) T1:17.1(0.3) dT2:99.4(1.7) d
? 21.1(1) d/m last2 y
NP BSRT Verbal STM Verbal STMCFT AA AA
T1 & T2 Alcohol users: 91(77) T1:17.1(0.3) dT2:99.4(1.7) d
? 21.1(1) d/m last2 y
T1 & T2 Poly drug users: 33(24) T1:17.1(0.3) dT2:99.4(1.7) d
? 21.1(1)d/m last2y
T1 & T2 Healthy controls: 137(69) – – b3 d last 2 yCardenas et al.(2007)
T1 & T2 Abstinent alcohol dependent:17(?)
T1:5.8(2.9) dT2:188(66) d
? 396(199) d/m lastyear
MRI: WM andGM volumes
– Temporallobes
Tissue gain in all areas, but greater forabstinent compared to relapsed participants
– Thalamus
T1 & T2 Relapsed alcohol dependent:8(?)
T1:5.8(2.9) dT2: 8(6) d
? 359(121) d/m lastyear
– Brainstem– Cerebellum
T1 &T1 + 12 m
Light drinkers: 8(?) – – 8(13) d/m lastyear
– Corpuscallosum
– ACC– Insula– Subcortical
white matterCordovil De SousaUva et al.(2010)
T1 & T2 Alcohol Dependent: 35(17) T1: ≤2 dT2: 14–18 d
? ? NP OCDS Cr ↓CrD2-test SA SA
PS PST1 & T2 Healthy controls: 22(14) – – ? TMT-A/B PS PS
F FStroop I I
SA SAIGT DM DM
IA IAPANAS PA, NA PA, NA
Demirakca et al. T1 & T2 Abstinent alcohol dependent: T1: 17.19(7.82) y 13.3(15.0) g/kg MRI GM – Abstinent Alcohol Dependents: insula,
536M.H.J.Schulte
etal./ClinicalPsychologyReview
34(2014)
531–550
(2011) 14(8) 16.5(7.3) dT2: 3 m
thalamus and ACCGM/TIV ratio
WM – WM/TIV ratioT1 & T2 Relapsed alcohol dependent:
16(9)T1:16.5(7.3) dT2: 3 m
10.54(6.46) y 13.3(15.0) g/kg CSF – Abstinent alcohol dependent: ↓CSFCSF/TIV ratio
T1 & T2 Healthy controls: 66(34) – – ?Durazzo et al.(2007)
T1 & T2 Smoking alcohol dependent:13(12)
T1: 33(9) dT2:194(38) d
30(11) y 302(112) d/m NP SCT AA AA in non-smoking Alcohol DependentF F in non-smoking Alcohol DependentU U in non-smoking Alcohol Dependent
TMT-A PS PS in both Alcohol Dependent groupsTMT-B F F in non-smoking Alcohol Dependent
T1 & T2 Non-smoking alcohol depen-dent: 12(11)
T1: 33(9) dT2:178(57) d
36(12) y 124(56) d/m WAIS-III similarities AA AA in non-smoking Alcohol DependentU U in non-smoking Alcohol Dependent
WAIS-III arithmetic & digitspan
WM WM in non-smoking Alcohol Dependent
WCST F F in non-smoking Alcohol DependentU U in non-smoking Alcohol Dependent
T1 + 334(129) d
Non-smoking light drinkers:22(20)
– – 17(11) d/m CVLT-II Verbal STM Verbal STM in both AlcoholDependent groups
Verbal LTM Verbal STM in both AlcoholDependent groups
BVMT-R Visual STM Visual STMVisual LTM Visual LTM
GPB FMF FMFWARD7-IQ gIQ gIQ in non-smoking Alcohol DependentStroop I I in non-smoking Alcohol Dependent
SA SA in non-smoking Alcohol DependentPS PS in both Alcohol Dependent groups
WAIS-III block design VS VS in non-smoking Alcohol DependentWAIS-III digit symbol &symbol search
PS PS in both Alcohol Dependent groups
Feldtkeller et al.(2001)
T1 Short term abstinent alcoholdependent: 15(11)
9(4.5) d 13.2 y 50.68 units/w NP CCPT Primed SA Primed SA in Long Term AbstinentAlcohol Dependent
T1 Medium term abstinentalcohol dependent: 16(11)
50(3.5) d 11.7 y 49.61 units/w
T1 Long term abstinent alcoholdependent: 15(11)
12(8) m 16.7 y 47.35 units/w
T1 Healthy controls: 20(13) – – 2.5 units/wFoisy et al. (2007) T1 & T2 Alcohol dependent: 22(13) T1:
29.5(7.9) dT2: N2 m
161(114) m 14.77(7.9) drinks/d
NP EFET EFER EFER
T1 & T2 Healthy controls: 22(12) – – 0.4(0.4) drinks/dFujiwara et al.(2008)
T1 & T2 Korsakov patients: 20(14) T1:10.3(5.2) yT2: +N2 y
25.8(10.1) y ? NP WAIS-R information vIQ vIQR-OFC copy VS VS
T1 Healthy controls: 20(11) ornormative scores
– – ? WMS digit span forward Verbal STM Verbal STMWMS BDS WM WMStroop PS PS
SA SAI I
MT immediate Verbal STM Verbal STMR-OFC delayed Visual LTM Visual LTMFAS VF VF
Gazdzinski et al.(2005)
T1, T2, T3 Abstinent alcohol dependent:7(?)
T1: 6(3) dT2: 33(9) dT3: 6–12 m
20.2(7.4) y 357(247) d/m MRI – Whole brainvolume
Whole brain volume
– CSF ↓CSF in lateral, 3rd, 4th ventricals, lobeboundaries, cerebellum, pons andhippocampi
T1T1 + 33(9) d
Relapsed alcoholdependent:10(?)
T1: 6(3) dT2:?
19.2(8.7) y 522(215) d/m
(continued on next page)
537M.H.J.Schulte
etal./ClinicalPsychologyReview
34(2014)
531–550
Table 3 (continued)
Article Design Subjects, N(male) Abstinence,Mean (SD)
Duration ofabuse, mean(SD)
Quantity of use,mean (SD)
Technique Tasks Cognitivefunctions/NIfactor
No improvement/improvement
T1 + 6–12 m T3:?T1 & T1+762(70) d
Healthy controls:17(15) – – 6(7) d/m
Gazdzinski et al.(2008)
T1 & T2 Smoking alcohol dependent:13(13)
T1:6(3)T2: 32(9) d
308(106) m 425(187) d/m NP BVMT-R Visual STM Visual STMVisual LTM Visual LTM
T1 & T2 Non-smoking alcoholdependent: 11(11)
T1:6(3)T2: 32(9) d
225(106) m 387(178) d/m MRI – hc ↑hc x visual STM and visual LTM in Non-Smoking Alcohol Dependent
Hanson et al.(2011)
T1 & T2 Alcohol/substance usedisorder: 18(14)
50.8(109) d ? 53.2(84.5) d/mlast 3 m
NP WISC-R/WAIS-R vocabulary Language LanguageWISC-R/WAIS-R similarities AA AA
U UWISC-R/WAIS-R blockdesign
VS VS
WISC-R/WAIS-R arithmetic WM WMWISC-R/WAIS-R digit span Verbal STM Verbal STM
WM WMCOWAT VF VF
T1 & T2 Abstinent alcohol dependent:19(9)
371.5(468) d ? 9.0(17.2) d/m last3 m
CVLT/CVLT-II Verbal STM Verbal STMVerbal LTM Verbal LTM
TMT-A PS PST1 & T2 Healthy controls: 14(6) – – 5.1(5.5) d/m last
3 mTMT-B F FWMS visual reproduction/R-OCF copy and 30 m delay
Visual LTM Visual LTMVS VS
Heinz et al.(2005)
T1 & T2 Alcohol dependent: 12(12) T1: 6–22 dT2: 5 w
? 17.3(5.5) kg last3 m
NP OCDS Cr CrPET – Central μ-
opiatereceptor
↑μ-opiate receptor x ↑CrT1 Healthy controls: 10(10) – – 0.3(0.3) kg last
3 mLoeber et al.(2010)
T1, T2, T3 High detox group: 25(19) T1:treatmentT2: 3 mT3: 6 m
? 51.7(20.2)drinking days last3 m
NP TMT-B F FWCST F F
U UIGT DM DM
IA IAR-AVLT Verbal STM Verbal STMT1, T2, T3 Low detox group: 10(5) T1:
treatmentT2: 3 mT3: 6 m
? 50.7(26.5)drinking days last3 m
BVRT Visual STM Visual STMVisual LTM Visual LTM
T1, T2 Healthy controls: 16(9) – – ?Manning et al.(2008)
T1 & T2 Alcohol Dependent: 30(10) T1: 4 dT2: 26 d
11.7(?) y 37.6(18.3) units/d NP WASI vocabulary Language LanguagegIQ gIQ
WASI matrix reasoning pIQ pIQ– Healthy Controls: norm
scores– – – WMS letter number
sequencingWM WM
WMS—III VPA EM EMVerbal LTM Verbal LTM
PAL AM AMPRM Visual STM Visual STMMST PS PS
MF MFFAS VF VFHSCT I IIED F FSOC P P
Mon et al. (2013) T1 & T2 VAL homozygous alcoholdependent: 26(23)
T1:6.5(2.5) dT2: 34(9.4) d
240(97) m 204(111) d/mlifetime
NP WAIS-III digit span WM WMWAIS-III digit symbol PS PS
T1 & T2 VAL/MET heterozygous T1: 239(114) m 183(81) d/m BVMT-R Visual STM Visual STM
538M.H.J.Schulte
etal./ClinicalPsychologyReview
34(2014)
531–550
alcohol dependent: 15(13) 6.5(2.5) dT2: 34(9.4) d
lifetime Visual LTM Visual LTMMRI – GM tissuevolume
↑ GM tissue volume x WM, PS,visual STM/LTM
T1 & T1+ 7 m Non-smoking light drinkers:17(?)
– – 19(15) d/mlifetime
WM tissuevolume
STM/LTM↑ WM tissue volume x WM, PS,visual STM/LTM
Moriyama et al.(2006)
T1 & T2 Alcohol dependents withpositive family history:19(19)
T1: 2 wT2: 7 w
14.4(8.6) y ? NP TMT-A PS PS for FHNTMT-B F FFPT Spatial WM Spatial WM both groups
Spatial STM Spatial STM both groupsT1 & T2 Alcohol dependents with
negative family history:20(20)
T1: 2 wT2: 7 w
12.5(8.1) y ? SDM VS VSDA DAPS PS
WAIS block design VS VST1 Healthy controls: 15(15) – – ? Reaction time test i RT RT for FHP
Reaction time test ii SA SA for FHNI I for FHN
Reaction time test iii SA SAI IPS PS
Pitel et al. (2009) T1 & T2 Abstinent alcohol dependent:14(13)
T1: duringtreatmentT2: 6 m
9.75(8.62) y 15.11(8.96) d/day NP FCSRT EM EMLFT, CFT VF VFStroop I I
T1& T2 Relapsed alcohol dependent:20(15)
T1: duringtreatmentT2: 6 m
9.61(48.26) y 16.28(8.78) d/day ARAAT F FVST, SST WM WMRTT, DAT DA DA
T1 Healthy controls: 54(?) – – 0.25(0.25) d/day SAT SUAT SUATRosenbloom et al.(2004)
T1, T2 & T3 Abstinent alcohol dependent:14(0)
T1: 15 wT2:18.1(4.8) mT3:44.6(18.0) m
? 411.4(353.4) kglifetime
NP BPDP Verbal STM T1–T2: verbal STMT2–T3: Verbal STM
Visual STM T1–T2: Nonverbal STMT2–T3: visual STM
WM T1–T2: WMT2–T3: WM
DRS memory subscale Dementia T1–T2: DementiaT2–T3: Dementia
WAIS—Digit symbol VS T1–T2: VST2–T3: VS
T1 & T2 Relapsed alcohol dependent:9(0)
T1: 15 wT2:3.5(3.3) m
? 638.3(350.0) kglifetime
T1& T1 + 3 y Healthy controls: 14(0) – – ?Rosenbloom et al.(2007)
T1 & T2 Abstinent alcohol dependent:10(6)
T1: 6 wT2: 2 y
13.5(8.3)? 732.8(562.8) kglifetime
NP WMS visual memory Visual M Visual M in abstainersVerbal M Verbal M in abstainers
T1 & T2 Relapsed alcohol dependent:5(2)
T1: 6 wT2: 80 d
20.5(13.0)? 816.4(224.7) kglifetime
General M General M in abstainersSUAT SUAT in abstainersDelayed M Delayed M in abstainers
WASI vIQ vIQ in abstainerspIQ pIQ in abstainersfull IQ Full IQ in abstainersT1 &
T1 + 94(24) dHealthy controls: 26(12) – – 56.6(64.4) kg
lifetime MRI – VV (4th,lateral)
↑ lateral volume x ↑ general Mwhole AD group4th ventricle x general M
Sullivan et al.(2000)
T1& T2 Abstinent alcohol dependent:20(20)
T1: 1 mT2: 2–12 m
18.9(9.4) y 1406.2(939) kglifetime
NP WCST F FU U
BPDT Verbal STM Verbal STMVisual STM Visual STMWM WM
WMS WM WMEM EM
T1 & T2 Relapsed alcohol dependent:22(22)
T1: 1 mT2:
18.1(11.1) y 1338(882) kglifetime
SM SMFDS, FBS SUAT SUAT
– Healthy controls: – – – – HFT VS VS
(continued on next page)
539M.H.J.Schulte
etal./ClinicalPsychologyReview
34(2014)
531–550
Table 3 (continued)
Article Design Subjects, N(male) Abstinence,Mean (SD)
Duration ofabuse, mean(SD)
Quantity of use,mean (SD)
Technique Tasks Cognitivefunctions/NIfactor
No improvement/improvement
FFMT FMF FMFMRI – GM
WMVV (4th,lateral)
↑ cortical WM x ↑ immediate/delayed recall↑basal ganglia x ↑ STM↑ anterior cortical GM x ↑WM↓ lateral ventricle x ↑ STM and ↑FMF↓ 3rd ventricle x ↑ STM
Tasks: ARAAT, Alternative Response subtest of Attentional Assessment Test; BDS, Backward Digit Span; BPDP, Brown-Peterson Distractor Paradigm; BSRT, Buschke's Selective Reminding Test; BVMT, Brief Visual Memory Test; CCPT, ComputerizedContextual Priming Test; CFT, Categorical Fluency Test; COWAT, ControledOralWordAssociation Test; CVLT, California Verbal Learning Test; D2 test, D2 cancellation test; DAT, DividedAttention Task; EFET, Emotional Facial Encoding Test; FAS, VerbalFluency Test; FCSRT, Free andCued Selective Reminding Test; FDS, ForwardDigit Span; FFMT, Fine FingerMovement Test; FPT, Figure Position Test; GPB, Grooved Peg Board; HFT, Hidden Figures Test; IGT, IowaGambling Task; LFT, Letter Fluency Task;MT immediate,Memory Test immediate recall; OCDS, Obsessive Compulsive Drinking Scale; PANAS, Positive AndNegative Affect Scale; R-AVLT, Rey Auditory Verbal Learning Test; RTT, Reaction Time Test; R-OCF, Rey-Osterrieth Complex Figure Test;SAT, Sustained Attention Task; SCT, Short Categories Test; SDM, Symbol Digit Modalities test; SST, Spatial Span Task; TMT-A/B, Trail Making Test part A/B; VST, Verbal Span Task;WAIS, Wechsler Adult Intelligence Scale;WASI,Wechsler AbbreviatedScale of Intelligence; WCST, Wisconsin Card Sorting Task; WISC, Wechsler Intelligence Scale for Children; WMS, Wechsler Memory Scale;Cognitive functions: AA, Abstraction Abilities; AM, Associative Memory; Cr, Craving; DA, Divided Attention; DM, Decision making; EFER, Emotional Facial Expression Recognition; EM, Episodic Memory; F, Flexibility; FMF, Fine Motor Functioning;gIQ, general IQ, I, Inhibition; IA, Impulsive Action; LTM, Long Term Memory; MF, Motor Functioning; NA, Negative Affect; P, Planning; PA, Positive Affect; pIQ, Performance IQ; PS, Processing Speed; RT, Reaction Time; SA, Selective Attention; SM,Semantic Memory; STM, Short Term Memory; SUAT, Sustained Attention; U, Updating; vIQ, verbal IQ; VF, Verbal Fluency; VS, Visuospatial Skills; WM, Working Memory;Neuroimaging: Cho, Choline; CSF, CerebroSpinal Fluid; GM, Grey Matter; H-MRS, proton Magnetic Resonance Spectroscopy; hc, hippocampus; NAA, N-acetylaspartate; PBVC, Percentage Brain Volume Change; TIV, Total Intracranial Volume; VV,Ventricular Volume; WM, White Matter.Other: ↓, decrease; ↑, increase; NP, NeuroPsychological Testing;?, not specified in article; −, n.a.
540M.H.J.Schulte
etal./ClinicalPsychologyReview
34(2014)
531–550
541M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
4. Substances other than alcohol
4.1. Cannabis
Three studies on recovery after cannabis dependence were in-cluded, all of which controlled for practice effects by testing the con-trol group more than once. The details of these studies are displayedin Table 4. Of note, none of the included studies on cannabis explic-itly studied a dependent group, but participants met the inclusioncriterion of more than 5 joints weekly for more than 2 years and atleast 4 weeks abstinence.
4.2. Group by time comparison studies on recovery after heavy cannabisuse
Improvements associated with sustained abstinence were foundfor verbal short-term memory and verbal long term memory (Pope,Gruber, Hudson, Huestis, & Yurgelun-Todd, 2002; Pope et al.,2001). After adjustment for potentially confounding factors, includ-ing pre-drug performance in the relevant cognitive domain, currentregular heavy users did significantly worse than never-users in over-all IQ, processing speed, as well as verbal short term memory andverbal long term memory, whereas former cannabis smokers whowere abstinent for at least 3 months did not show any cognitive im-pairments compared to never-users (Fried, Watkinson, & Gray,2005). It was concluded that residual cannabis effects are no longerapparent 3 months after cessation of regular use, even among formerheavy using young adults. These data therefore suggest that chroniccannabis use during adolescence does not result in persistent cogni-tive damage and that after more than three months of abstinence fullrecovery may occur.
Table 4Longitudinal neurocognitive studies on cannabis dependence. Cognitive functions in bold emp
Article Design Subjects N(male)
Abstinence,Mean (SD)
Duration of abuse,mean (SD)
Fried et al.(2005)
T1 & T2 Light Users:19(12)
T1:T2:
1.8(2.0) y
T1 & T2 Heavy Users:19(13)
T1:T2:
2.6(1.3) y
T1 & T2 Former Users:16(9)
T1:T2:
2.2(1.4) y
T1 & T2 HealthyControls: 59(24)
– –
Pope et al.(2001, 2002)
T1, T2,T3, T4
Heavy Users:77(55)
T1: 0(?)dT2: 1(?) dT3: 7(?) dT4: 28(?) d
19(?)y
T1, T2,T3, T4
Former Users:45(30)
T1: 0(?) dT2: 1(?) dT3: 7(?) dT4: 28(?) d
15(?) y
T1, T2,T3, T4
HealthyControls: 87(61)
– –
Tasks: BSRT, Buschke's Selective Reminding Test; BVRT, Benton Visual Retention Test; CPT, CoWMS, Wechsler Memory Scale.Cognitive functions: AA, Abstraction Abilities; I, Inhibition; LTM, Long TermMemory; pIQ, perfoSustained Attention.Other: NP, NeuroPsychological Testing;?, not specified in article; −, n.a.
4.3. Cocaine
Four studies on recovery after cocaine dependence were included.Two studies tested the control group only once, one study took practiceeffects and natural course effects into account by either testing thecontrol group at least twice or using normative scores, and one studyused multiple dependent groups with differing lengths of abstinence.The details are displayed in Table 5.
4.4. Group comparison studies on recovery after cocaine dependence
Recovery was reported for selective attention, emotion regulation,inhibition, verbal and visual long term memory, working memory,(primed) verbal memory, abstraction abilities, spatial processing,positive affect, visuospatial skills, processing speed, flexibility, verbalfluency, fine motor functioning, divided attention, sustained attention,and updating (Di Sclafani, Tolou-Shams, Price, & Fein, 2002; Fox,Axelrod, Paliwal, Sleeper, & Sinha, 2007). However, verbal and visualshort term memory were not improved (Di Sclafani et al., 2002).
4.5. Group by time comparison studies on recovery after cocaine dependence
In a three-week longitudinal inpatient study of cognitive changesduring drug use and abstinence, cocaine dependent patients showednormal working memory compared to healthy controls. Sustainedattention and divided attention was significantly worse during thefirst and secondweek of abstinence compared to days onwhich cocainewas used, suggesting that certain pre-existing or cocaine-inducedimpairments may be acutely normalized by cocaine use, but resurfaceduring abstinence (Pace-Schott et al., 2008). This also implies thatrecent use of cocaine may mask deterioration of cognition.
hasize improvements with a significance level of at least p b0.05.
Quantity of use,mean (SD)
Technique Tasks Cognitive domains/NI factor
No improvement/improvement
1.4(1.2) joints/w NP WAIS IQ IQ for Heavy UsersIQ for Former Users
pIQ pIQ for Heavy UserspIQ for Former Users
WAIS PS PS for Heavy UsersPS for Former Users
12.4(9.8) joints/w WMS Verbal STM Verbal STM for HeavyUsersVerbal STM for For-mer Users
Verbal LTM Verbal LTM for HeavyUsersVerbal LTM for For-mer Users
≤2 joints/w CT AA AA for Heavy UsersAA for Former Users
0(0) joints/w
18720(?) jointslifetime
NP BSRT Verbal STM Verbal STMVerbal LTM Verbal LTM
BVRT Visual STM Visual STM
11000(?) jointslifetime
Visual LTM Visual LTMCPT SA SA
SUAT SUATI I
10(?) jointslifetime
ntinuous Performance Test; CT, Categories Test; WAIS, Wechsler Adult Intelligence Scale;
rmance IQ, PS, Processing Speed; SA, Selective Attention; STM, Short TermMemory; SUAT,
542 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
4.6. Studies using multiple dependent groups with different lengths ofabstinence
One study controlled for natural course effects by comparing thewhite matter integrity of several brain areas between three groups with
Table 5Longitudinal neurocognitive studies on cocaine dependence. Cognitive functions in bold emph
Article Design Subjects N(male) Abstinence,Mean (SD)
Duration ofabuse, mean(SD)
Bell et al.(2011)
T1 Short Term Abstinent CocaineDependent: 13(13)
0.7–5.1 w 11.9(6.0) y
T1 Medium Term AbstinentCocaine Dependent: 14(14)
10–40.3 w 8.8(5.5) y
T1 Long Term Abstinent CocaineDependent: 16(14)
44–102 w 7.1(7.1) y
T1 Healthy Controls: 43(36) – –
Di Sclafaniet al. (2002)
T1 &T2
Cocaine Dependent: 20(19) T1:N35dT2: 6 m
T1: 169(72) mT2: 153(77) m
T1 &T2
Cccaine and AlcoholDependent: 37(31)
T1:N35dT2: 6 m
T1: 167(67) mT2: 151(75) m
T1 Healthy Controls: 29(11) – –
Fox et al.,2007
T1 &T2
Cocaine Dependent: 60(32) T1: 1 wT2: 3–4 w
?
T1 Healthy Controls: 50(26) – –
Pace-Schottet al. (2008)
T1, T2,T3
Cocaine Dependent: 17(14) t2: 1 wt3: 2 w
?
– HC: normative scores – –
Tasks: COWAT, ControlledOralWordAssociation Test; DERS, Difficulties in Emotion Regulation SMC, MicroCog; NWM, Numeric Working Memory test; R-OCF, Rey-Osterrieth Complex FiguresSWM, Spatial Working Memory test; TMT-A/B, Trail Making Test part A/B.Cognitive functions: AA, Abstraction Abilities; DA, Divided Attention; I, Inhibition; E, Emotion; EPS, Processing Speed;M,Memory; SA, Selective Attention; SP, Spatial Processing; STM, Short TerMemory.Neuroimaging: DTI, Diffusion Tensor Imaging; FA, Fractional Anisotropy.Other: ↓, decrease; ↑, increase; NP, NeuroPsychological Testing;?, not specified in article; −, n.
different lengths of abstinence (Bell, Foxe, Nierenberg, Hoptman, &Garavan, 2011). It appeared that some specific differences in white mat-ter are persistent throughout abstinence, while others appear to changeas a function of abstinence duration. These changes inwhitematter integ-rity could facilitate recovery of cognitive function during abstinence.
asize improvements with a significance level of at least p b0.05.
Quantity of use,mean (SD)
Technique Tasks Cognitivedomains/NIfactor
No improvement/improvement
? DTI – FA Short Term—
Medium Term:↑R anterior thalamicradiation↑R cingulum↑ L superior coronaradiate↓L superiorlongitudinalfasciculus
?
?
Medium Term—
Long Term:↑R precentral gyrusWM↑VPL of R thalamus↓ R superior longitu-dinal fasciculus↓ L inferior longitu-dinal fasciculus↓ R inferior longitu-dinal fasciculus↓ L superior coronaradiate↓VPL of R thalamus
?
T1:957(1056) $/mT2:977(933) $/m
NP MC SA SASUAT SUATI IVerbal STM Verbal STMVerbal LTM Verbal LTMWM WMPriming M Priming MAA AA
T1: 740(707) $/mT2: 882(812) $/m
VS VSPS PS
R-OCF VS VSVisual STM Visual STMVisual LTM Visual LTM
TMT-A PS PSTMT-B F F
0 $/m SDM VS VSDA DAPS PS
COWAT VF VFStroop I I
SA SAPS PS
GPB FMF FMFSCT AA AA
F FU U
? NP DERS E E
–
9(3–5.5) g/w NP RTT DA DADVT SUAT SUAT
– DWR EM EMSWM WM WMNWM WM WM
cale; DVT, Digit Vigilance Test; DWR, DelayedWordRecognition;GPB, Grooved Peg Board;; RTT, Reaction Time Test; SCT, Short Categories Test; SDM, Symbol Digit Modalities test;
M, Episodic Memory; F, Fluency; FMF, FineMotor Functioning; LTM, Long TermMemory;mMemory; SUAT, Sustained Attention; U, Updating; VS, Visuospatial Skills;WM,Working
a.
543M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
4.7. Methamphetamine
Three studies on recovery after methamphetamine dependence areincluded, of which one study controlled for practice effects and twodid not. Details of these studies are displayed in Table 6.
4.8. Group comparison studies on recovery after methamphetaminedependence
In a recent study, abstinent methamphetamine dependent subjectsperformed not significantly different from healthy controls on flexibili-ty, updating, inhibition, selective attention, processing speed, episodicmemory, visual short term and long termmemory, finemotor function-ing, verbal fluency, working memory, divided attention, and sustainedattention (Iudicello et al., 2010). In a 1H-MRS study, methamphetaminedependent patients showed lower glutamate and glutamine (GLX)
Table 6Longitudinal neurocognitive studies on (meth)amphetamine dependence. Cognitive functions
Article Design Subjects N(male) Abstinence,Mean (SD)
Duration ofabuse, mean(SD)
Quus(S
Ernst andChang(2008)
T1 &T2
MethamphetamineDependent: 12(?)
T1: b1 mT2: 2.1(3.0) m
109(69) m 1.35.9
T1 Healthy Controls: 28(14) – – –
Iudicelloet al.(2010)
T1 &T2
AbstinentMethamphetamineDependent: 25(22)
T1:54.8(28.5) dT2:378(107.6) d
3167(1975) d 31to
T1 &T2
MethamphetamineDependent: 59(53)
T1:40.2(20.1) dT2:68.8(102.3) d
2787(2070) d 21to
T1 Healthy Controls: 38(31) – – –
Simon et al.(2010)
T1 &T2
MethamphetamineDependent: 18(12)
t1: 6.2(1.5) dt2: +1 m
7.6(6.9) 5.4we
T1 &T2
Healthy Controls: 21(13) – – –
Tasks: BDS, Backward Digit Span; BVMT, Brief Visuospatial Memory Test; COWAT, ControlledReminding Test; GPB, Grooved Peg Board; HCT, Halstead Category Test; HVLT: Hopkins VerbSDM, Symbol Digit Modalities; TMT-A/B, Trail Making Test Part A/B; VAS, Visual Analog ScalWCST, Wisconsin Card Sorting Task.Cognitive functions: Cr, Craving; DA, Divided Attention; EM, Episodic Memory; F, Flexibility; FMProcessing Speed; SA, Selective Attention; STM, Short Term Memory; SUAT, Sustained AttentioNeuroimaging: GLX, Glutamata + Glutamine; GM, Grey Matter; MRS, Magnetic Resonance SpOther: NP, NeuroPsychological Testing;?, not specified in article; −, n.a.
brain concentrations than normal controls during early abstinence,followed by GLX concentrations within normal limits after 1–2 monthsof abstinence, with some evidence for overcompensation in the longerterm, especially in the frontal gray matter (Ernst & Chang, 2008).Moreover, GLX normalization was associated with a reduction ofcraving, thereby probably facilitating abstinence.
4.9. Group by time comparison studies on recovery aftermethamphetaminedependence
In the only group by time comparison study in methamphetamineaddicts, abstinence was not associated with improvements in perfor-mance IQ, selective attention, inhibition, processing speed, workingmemory, flexibility, verbal fluency, updating, and visuospatial skills,but patients showed slightly more improvement on the compositescore of the entire neurocognitive test battery compared with controls
in bold emphasize improvements with a significance level of at least p b0.05.
antity ofe, meanD)
Technique Tasks Cognitivedomains/NI factor
Noimprovement/improvement
(1.2) g/d(1.7) x/w
NPMRS
VAS Cr ?Glx in basalganglia, frontalGM/WM
↑Cr x ↓ frontalGM GLX
53(3009) gtal
NP HCT F FU U
WCST F FU U
TMT-B F F36(2628) gtal
Stroop I ISA SAPS PS
HVLT EM EMBVMT Visual STM Visual STM
Visual LTM Visual LTMGPB FMF FMFTMT-A PS PSCOWAT VF VFWAIS-III digitsymbol
PS PSVisual LTM Visual LTMSA SA
WAIS-III symbolsearch
PS PSF FSA SAVisual STM Visual STM
WAIS-III letternumbersequencing
WM WM
PASAT PS PSDA DASUAT SUAT
(5.8) g/ek
NP SHTV pIQ pIQTMT-A PS PSStroop SA SA
I IPS PS
BDS WM WMVST WM WMTMT-B F FCOWAT VF VFWCST F F
U UDL VS VSLPT U U
Oral Word Association Test; DL, Discrimination Learning; FCSRT, Free and Cued Selectiveal Learning Test; LPT, Logical Problems Test; PASAT, Paced Auditory Serial Addition Test;e; VST, Verbal Span Task; VT, Vocabulary Test; WAIS, Wechsler Adult Intelligence Scale;
F, FineMotor Functioning; I, Inhibition; LTM, Long TermMemory; pIQ, performance IQ; PS,n; U, Updating; VF, Verbal Fluency; VS, Visuospatial Skills; WM, Working Memory.ectroscopy, WM, White Matter.
544 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
(Simon, Dean, Cordova, Monterosso, & London, 2010). However, thecontrol group was better educated, and when education was used as acovariate these effects were no longer significant.
4.10. Opiates
Three studies on recovery after opiate dependence were included.One study did not control for practice effects, the other two used multi-ple groupswith differing lengths of abstinence. The details are displayedin Table 7.
4.11. Group comparison studies on recovery after opiate dependence
Irrespective of whether cue exposure therapy (CET) or placebotherapy was given, all opioid dependent patients showed a decreasein selective attention to opiate related stimuli (Marissen et al., 2006).
4.12. Studies using multiple dependent groups with different lengths ofabstinence
Zhang et al. (Zhang et al., 2011) tested decision making in groupsof opiate dependent patients with different lengths of abstinence,varying from 3 days to 24 months, and found that longer abstinencewas correlated with better performance: most participants per-formed worse than healthy controls, except for those who were ab-stinent for 24 months. However, psychological stress unmasked alatent impairment in decision making still present in the 24-monthabstinence group, who performed similarly to healthy comparisonsubjects in the absence of stress. Interestingly, propranolol blockedthis stress-induced impairment of decision making in formerly
Table 7Longitudinal neurocognitive studies on opiate dependence. Cognitive functions in bold empha
Article Design Subjects N(male) Abstinence,mean (SD)
Duration of abumean (SD)
Marissenet al.(2006)
T1&T2
Abstinent Opiate Dependent:84(?)
T1: N2 wT2: T1 + 3 wT3: T2 + 3 m
9.3 y
T1&T2
Relapsed Opiate Dependent:26(?)
T1: N2 wT2: T1 + 3 wT3: T2 + 3 m
9.3 y
Zhang et al.(2011)
T1 Alcohol Dependent Group1:18(?)
3 d 7.0(4.7) y
T1 Alcohol Dependent Group2:19(?)
7 d 7.6(3.8) y
T1 Alcohol Dependent Group3:18(?)
15 d 6.8(4.6) y
T1 Alcohol Dependent Group4:20(?)
30 d 7.9(3.5) y
T1 Alcohol Dependent Group5:19(?)
3 m 7.9(4.0) y
T1 Alcohol Dependent Group6:19(?)
6 m 8.0(3.4) y
T1 Alcohol Dependent Group7:21(?)
12 m 7.3(3.8) y
T1 Alcohol Dependent Group8:20(?)
24 m 8.1(3.6) y
T1 Healthy Controls: 20(?) – –
Zhao et al.(2012)
T1 Short Term Abstinent OpiateDependent: 26(8)
b1 m 5.7(3.7) y
T1 Long Term Abstinent OpiateDependent: 29(11)
N1 y 7.6(3.6) y
T1 Healthy Controls: 26(11) – –
Tasks: DDQ, Desires for Drugs Questionnaire; IGT, Iowa Gambling Task.Cognitive functions: Cr, Craving; DM, Decision Making; I, Inhibition; PS, Processing Speed; SA,Other: NP, NeuroPsychological Testing;?, not specified in article; −, n.a.
heroin dependent patients. Another study tested physiological andcraving responses in participants who had been abstinent for overa year and compared them to recently abstinent dependent individ-uals (Zhao et al., 2012). Long-term abstainers still showed physiolog-ical responses and subjective craving towards heroin cues, except forheart rate, which was only elevated in recently abstinent users.
4.13. Moderating factors for studies on drugs other than alcohol
Extent and duration of dependence were negatively correlated withneurocognitive recovery in studies with cocaine dependent patients (DiSclafani et al., 2002; Fox et al., 2007; Pace-Schott et al., 2008). Further-more, in studies with opioid dependent patients, methadone mainte-nance treatment may have a negative effect on neurocognitiverecovery from (chronic) heroin use. For instance, a recent paper report-ed that opiate dependent subjects using methadone were impaired onemotion perception compared to abstinent opiate dependent subjects(McDonald, Darke, Kaye, & Torok, 2013). However, these potentiallynegative effects must be weighed against the well-known advantagesof methadone maintenance treatment in terms of illicit opiate use,crime, risk behavior, quality of life, morbidity and mortality (Mattick &Breen, 2009).
4.14. Conclusions on recovery after drug dependence
Several functions appear to improve with sustained abstinence,including verbal short term memory (Pope et al., 2001, 2002),inhibition, visuospatial skills, and flexibility after cocaine depen-dence (Di Sclafani et al., 2002), working memory, sustained atten-tion, and episodic memory after methamphetamine dependence
size improvements with a significance level of at least p b0.05.
se, Quantity ofuse
Technique Task Cognitivedomains/NIfactor
No improvement/improvement
? NP Stroop I IPre-treatment Ipredicted relapse
? SA SAPre-treatment SApredicted relapse
PS PSPre-treatment PSpredicted relapse
DDQ Cr Cr x stroop0.9(0.6) g/x NP IGT DM DM
Alcohol DependentGroup8 = HC0.9(0.7) g/x
1.0(0.6) g/x
0.9(0.8) g/x
0.8(0.6) g/x
0.8(0.8) g/x
0.8(0.4) g/x
0.9(0.5) g/x
?20.1(14.0) dlast 30 d
NP Cr Cr
23.3(10.6) dlast 30 d?
Selective Attention;
1 Not included in this review because it could not be ascertained that the studymet theinclusion criteria for this study.
2 Not included in this review because it could not be ascertained that the studymet theinclusion criteria for this study.
545M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
(Iudicello et al., 2010), and selective attention to opiate related stim-uli may decrease in patients with heroin dependence (Marissenet al., 2006). Neural correlates of recovery have also been reported,such as an alteration in frontal GLX concentrations, which was asso-ciated with craving and length of abstinence (Ernst & Chang, 2008).
Only after abstinence following heavy cannabis use, full recovery ofaffected function was reported in adolescent cannabis users (Friedet al., 2005). Of course this does not imply that smoking marijuanaduring adolescence is without harm. It has been related to a variety ofnegative outcomes in the medical domain (e.g., increased chances oflung cancer, Callaghan, Allebeck, & Sidorchuk, 2013), psychiatricdomain (e.g., increased risk for psychosis, Davis, Compton, Wang,Levin, & Blanco, 2013) and psychological domain (e.g., increased riskof school dropout, Horwood et al., 2010). There is some evidence thatdivided attention and verbal short term memory do not recover aftersustained abstinence from cocaine use (Pace-Schott et al., 2008; Popeet al., 2001, 2002), that workingmemory and other executive functionsdo not improve after sustained abstinence frommethamphetamine use(Iudicello et al., 2010; Simon et al., 2010), and that decision making andcraving do not improve after opiate dependence (Zhang et al., 2011;Zhao et al., 2012). However, due to the scarcity of longitudinal studies,any conclusions drawn with regard to neurocognitive recovery fromcannabis, cocaine, methamphetamine or opioid dependence should beregarded as tentative.
5. Discussion
5.1. Summary
This review examined recovery of neurocognitive functioning aftersustained abstinence in patients with a DSM diagnosis of substance de-pendence (with the exception of cannabis). Only studies investigatingprolonged abstinence with a longitudinal design or multiple groupswith different lengths of abstinence were included in this review.Many cognitive functions appear to (partially) recover when long-term alcohol or drug use is discontinued (Bartsch et al., 2007; Loeberet al., 2010; Manning et al., 2008; Pace-Schott et al., 2008; Pope et al.,2001, 2002). Partial recovery could be related to premorbid impairedfunctioning, which has been found for verbal skills, impulsivity, IQ,and working memory (Fried et al., 2005; Penick et al., 2010).
Some studies attempted to find structural brain correlates ofneurocognitive recovery. For instance, in recovering alcoholics, positivecorrelations have been reported between increases in hippocampalvolume and visual short-term memory and visual long-term memoryfunctions (Gazdzinski et al., 2008). Moreover, a negative associationbetween memory improvement and lateral ventricular volume inabstinent alcoholics has been reported (Rosenbloom et al., 2007). Inrecovering cocaine dependent subjects, white matter changes werefoundwith prolonged abstinence (Bell et al., 2011), and a normalizationof GLX concentrationswas associationwith reductions in craving. Thesestudies indicate that alterations in brain structure may index cognitiverecovery. However, it must be noted that studies relating changes inbrain structure to neurocognitive recovery are virtually absent forsubstances other than alcohol.
In patients with alcohol dependence, recovery of a number ofneurocognitive functions in several cognitive domains, includingmemory and executive functions, was absent in those who were alsosmoking. If confirmed, this finding may encourage clinical researchinto the combined treatment of alcohol and smoking either simulta-neously or sequentially (Kalman, Kim, DiGirolamo, Smelson, &Ziedonis, 2010). For excessive cannabis use and cannabis dependence,the results on recovery of neurocognitive functions after sustainedabstinence are still minimal and inconsistent. One of the includedstudies showed full recovery in early onset heavy cannabis users afterat least three months abstinence (Fried et al., 2005). For the remainingsubstances (hard drugs) there are very few studies on neurocognitive
recovery and their results are not always straightforward. In patientswith cocaine dependence, executive functions improvedwith sustainedabstinence, whereas attentional processes remained impaired. Forpatients with (meth)amphetamine dependence, a variety of cognitivefunctions recovered after sustained abstinence. Finally, attentional biasfor opioid cues decreased with sustained abstinence in patients withheroin dependence, while decision making and craving did not improve.
6. Discussion
The term recovery suggests that the observed neurocognitiveimpairments in substance dependent patients are the consequence ofchronic and/or excessive substance use. However, some of theneurocognitive functions in dependent patients that failed to improveduring sustained abstinence may represent pre-existing vulnerabilityfactors for the development and onset of substance dependence. Forexample, suboptimal working memory and other executive functionshave been related to a family history of alcohol dependence and to theenhanced risk to develop dependence in this group (Nigg et al., 2004;Penick et al., 2010; Peterson et al., 1992; Sher, Walitzer, Wood, &Brent, 1991). While the present review focused on recovery ofneurocognitive functions after prolonged abstinence from SUDs,regarding the question whether observed differences in neurocognitivefunctioning between patients with SUDs are a cause or consequence ofthe SUD, large-scale prospective studies (in which subjects are testedbefore, during and after substance dependence) are necessary to inves-tigate cause and effect. For instance, Penick et al. (2010)1 found that afamily history of alcohol dependence predicted the development of al-coholism, but not the course of the dependence. Furthermore, impulsiv-ity, IQ and working memory predicted both the development and thecourse of alcohol dependence. In another study, persistent cannabisuse was associated with neuropsychological decline in participantswho initiated cannabis use before the age of 18 years but not in thosewho started using cannabis after the age of 18 years (Meier et al.,20122). Based on these findings, the authors proposed that cannabishas persistent neurotoxic effects on early onset users whereas cognitiveimpairments in late onset cannabis users are reversible after sustainedperiods of abstinence. However, others have claimed that the findingsof Meier et al. (2012)were confounded by differences in socioeconomicstatus (Rogeberg, 2013) and/or personality (Daly, 2013). In response,Moffitt, Meier, Caspi, and Poulton (2013) tested these alternative expla-nations and concluded that socioeconomic status and personality didnot confound the results. One of themost promising prospective studiesto address questions regarding causality is the IMAGEN study(Schumann et al., 2010), which started in 2007 and investigates the ef-fect of biological and environmental factors on mental health and risktaking behavior. The study's objective is to identify the neural basis ofpsychiatric disorders (including addiction) in relation to neurocognitivefunctions like reinforcement sensitivity and executive control.
Another important issue is the fact that the literature is notconsistent with regard to the meaning of the term ‘neurocognitiverecovery’. As stated before, for many authors recovery implies restora-tion from the negative neurocognitive consequences of chronic andexcessive substance use. However, several other explanations can beput forward. First, changes in the use of medication (e.g., methadone),the use of other substances than the one under study (e.g., nicotine inalcohol dependent patients) or the presence of comorbid mental disor-ders may have contributed to the observed problems and subsequentimprovements in neurocognitive functions. Another factor possiblyinfluencing the extent of neurocognitive impairment reported by thedifferent studies discussed in our review is the age at which substance
546 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
use is initiated. That is, an early age of onset has been found to beassociated with more severe cognitive deficits (Dom, D'haene,Hulstijn, & Sabbe, 2006; Ehrenreich et al., 1999). These differentialeffects between early and late-onset could also moderate the extent ofneurocognitive recovery. Indeed, this was reported by Meier et al.(2012), showing persistent impairments in early onset cannabis usersbut recovery in late onset cannabis users.
Second, not all studies verified abstinence by means of urinalysis,blood samples or breathalyzer and thus the possibility of false reportsof abstinence cannot be ruled out, which would likely result in anobserved lack of recovery. Third, characteristics of the control groupsoften differ between studies, such as demographic information andsubstance use characteristics. Therefore, to identify the impact ofsubstance dependence unconfounded by excessive use and abuse,studies should ideally compare groups with the same history of use, inwhich one group is dependent and the other group is not. However, itis impossible to recruit a perfectly matched control group, which is afundamental shortcoming of observational and quasi-experimentalresearch, a shortcoming that, in contrast to what many researchersassume, cannot be solved by merely adding covariates to the analyses(Meehl, 1970). Fourth, varying periods of abstinence are reportedbetween studies, suggesting that participants were in different phasesof abstinence and thus in different stages of cognitive recovery. Fifth,various neuropsychological tests are used to assess functions withinthe same domain, or a particular test is used by several studies tomeasure different domains while the overlap between these domainsis not taken into account.
A final issue refers to the fact that we did not include otherwiseinteresting studies inwhich no neuropsychological taskswere assessed,but indicators of related personality traits such as coping motives andneed for incentives (“sensation seeking”) related to neuropsychologicalfunctioning (cf., Wiers, Rinck, Kordts, Houben, & Strack, 2010) were in-vestigated. For example, a recent prospective study inwhichpersonalitytraits were measured, but no neuropsychological tests were adminis-tered, showed that excessive alcohol consumption during adolescenceaggravated impulsivity, but that impulse control normalized when ex-cessive consumption was discontinued (White et al., 2011).
6.1. Future research
Many opportunities remain for future research. Most importantly,studies into neurocognitive recovery should becomemore standardizedand samples should be enlarged, with research institutes and treatmentcenters collaborating. Both parties can benefit from such initiatives,because standardized assessment of neurocognitive functions relatedto the progress of recovery may foster development of treatment strat-egies in clinical practice. Also, such standardized neuropsychologicaltests will enhance comparability of results of similar studies in otherdisorders, such as schizophrenia, affective disorders and possiblypathological gambling and eating disorders. Further use of functionalimaging techniques may reveal subtle abnormalities that have not yetbeen identified by behavioral measures. Many studies have beenpublished that reported subtle abnormalities identified with behavioralas well as imaging techniques, but most of these studies lack a longitu-dinal design or repeated measures in the control group and only veryfew have data prior to the onset of substance use (e.g., Fried et al.,2005; Meier et al., 2012). Of course, the characteristics of the controlgroup should be carefully considered and the same tasks should be re-peatedly applied in both the SUD and in the control group in order tocontrol for practice effects.
6.2. Enhancing recovery
This review focused on currently available reports about spontane-ous recovery of neurocognitive functions after sustained abstinence insubstance dependent patients. One important finding of this review is
that several neurocognitive functions do not recover with abstinence.On the other hand, we know that diminished neurocognitive functions(e.g. Stevens et al., 2014) are a vulnerability factor for relapse. Therefore,neurocognitive training may prove to be beneficial not only forimproving neurocognitive functions, but also for reducing relapse.One exciting new avenue of clinical research focuses on methods toenhance neurocognitive recovery, through training, medication orneuromodulation. This line of research is important both for theoreticaland clinical reasons. First, it is theoretically important to establish ifcertain neurocognitive functions can be enhanced,whichdonot sponta-neously recover after abstinence: this can complement informationfrom prospective longitudinal studies which assess neurocognitivefunctioning before and after substance dependence (for example, it isconceivable that premorbid deficits are not open to enhanced “recov-ery”). Second, given the motivating effects of neurocognitive recoveryfor clinical success (Bates et al., 2013), ways to enhance neurocognitiverecovery can be considered as clinically promising. However, beforesuch treatment is initiated, several factors should be taken into account.First, abstinence duration should be established, because (sub)acutepharmacological effects of a substance andwithdrawal effects can affectneurocognitive functioning substantially. Furthermore, patients intreatment for dependence on a particular substance are not alwaysfully abstinent, due to poly-substance use or the use of medications totreat withdrawal symptoms. In order to investigate neurocognitivefunctioning of individual patients and to establish an indication for acognitive enhancing interventions, clinicians should assess thisabstinence and cognitive functions repeatedly at fixed intervals. Thisway, the progress of a patient can be closely monitored. A thoroughcase history and chart review, in which a variety of dependence-related information is collected, can also be helpful in treating patients.
6.3. Training neurocognitive functions
An imbalance between dysfunctional regulatory processes andhyperactive motivational processes has been proposed to underlie thedevelopment and persistence of addiction (Bechara, 2005; Strack &Deutsch, 2004; Volkow, Fowler, & Wang, 2004; Wiers et al., 2007).Varieties of these dual process models provide a range of opportunitiesto treat these patients taking into account their individual, basic‘neurocognitive profile’. Neurocognitive rehabilitation is importantwhen treating dependent patients, regardless of the speed and extentof recovery.
Cognitive training is a novel development in the treatment of addic-tion and other mental disorders in which regulatory or motivationalneurocognitive functions are targeted. Cognitive training has alreadyshown good results in schizophrenia (meta-analysis: Wykes, Huddy,Cellard, McGurk, & Czobor, 2011) and in children with ADHD andother cognitive problems (Klingberg, 2010, but see Sonuga-Barkeet al., 2013). Recently, Bickel, Yi, Landes, Hill, and Baxter (2011)employed working memory training in stimulant dependent patientsand found decreased delayed discounting compared to control training,but no clinical effects were reported. Training cognitive functions mayalso improve clinical outcome. For example, Houben et al. (2011)found that online working memory training in problem drinkers led toa significant reduction in alcohol consumption. Another approach isattentional bias re-training directed at a reductionof automatic appetitiveresponses. Positive effects have been reported for alcohol dependent pa-tients in terms of an attentional bias for alcohol (Schoenmakers et al.,2010), as well as for automatic approach tendencies to alcohol relatedstimuli in alcohol dependent patients (Eberl et al., 2013; Wiers, Eberl,Rinck, Becker, & Lindenmeyer, 2011). Cognitive bias modification hasalso been applied in treatment of other psychiatric disorders, includinganxiety and other addictions (reviews: MacLeod & Mathews, 2012;Wiers, Gladwin, Hofmann, Salemink, & Ridderinkhof, 2013). An advan-tage is that this approach is easy to add to currently available treatmentsand has clinically relevant effects as an adjunct to standard therapy
547M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
(e.g., Eberl et al., 2013; Schoenmakers et al., 2010;Wiers et al., 2011). It isan interesting open question to what extent neurocognitive recovery isstimulated more by this type of training than by abstinence andtreatment as usual alone.
Pharmacological treatment
Over the past few years, evidence has emerged that medications,which improve neurocognitive functions in patientswith ADHD, schizo-phrenia and healthy groups, can also have an effect on impulsivity inaddictive behavior. An example of such a pharmacological treatmentof cognitive impairment in substance dependent patients isgalantamine, a reversible and competitive cholinesterase inhibitor. Incigarette smokers, 4-day treatment with galantamine led to reducedself-reported craving and improved performance on a Go/No-Go task(Sofuoglu, Herman, Li, & Waters, 2012).
Another example is modafinil, a wakefulness promoting compoundwith a complex receptor binding profile. In a first small study, modafinilled to improved performance on an impulse control task in high-impulsive pathological gamblers, whereas in low-impulsive pathologi-cal gamblers modafinil resulted in worse performance (Zack & Poulos,2009). In addition, modafinil reduced craving in high-impulsivepathological gamblers. A similar observation was recently reported ina randomized clinical trial of modafinil in alcohol dependent patients:modafinil improved treatment outcome in high-impulsive alcoholdependent patients, whereas it decreased treatment efficacy in thosepatients characterized by low impulsivity (Joos et al., 2013). In otherstudies, modafinil was found to reduce impulsivity in amphetaminedependent patients (Dean et al., 2011) and to reduce cue reactivity andcraving in cocaine dependent patients (Goudriaan, Veltman, van denBrink, Dom, & Schmaal, 2013). From these initial studies it appears thatmodafinil may be clinically effective, especially in high-impulsive alco-holics and pathological gamblers, and in cocaine and stimulant depen-dent patients (Joos et al., 2013).
These examples of cognitive enhancers such as galantamine andmodafinil show promising results in the treatment of substance depen-dence. However, the use of cognitive enhancers in the treatment of sub-stance dependence should be examined more extensively, in particulargiven the evidence that the effects of this type of medication depend on(improvement of) baseline neurocognitive functions. For a recent re-view on cognitive enhancers in the treatment of substance dependencethe reader is referred to Sofuoglu, DeVito, Waters, and Carroll (2013).
6.4. Neuromodulation
In addition to medications, other methods may directly influenceregional brain function of substance dependent patients, includingneurofeedback and neurostimulation.
With regard to neurofeedback, a distinction can be made betweenEEG neurofeedback (for an overview of methods and first results inaddiction, Sokhadze, Cannon, & Trudeau, 2008), real-time fMRIneurofeedback (for a review of methods and first results, Weiskopf,2012). Real-time fMRI neurofeedback has shown to be beneficial in im-proving clinical symptoms in depression (Linden et al., 2012) and to re-duce cue-induced craving in smokers (Li et al., 2012). A problem withthe literature on neurofeedback is that there are virtually no controlledstudies, and thus, randomized controlled trials with adequate shamconditions are clearly needed (as have been done in ADHD, e.-g., Gevensleben et al., 2009).
With regard to neurostimulation, various techniques can be distin-guished (for a review, see Feil & Zangen, 2010), including the applicationof a low-voltage direct current at the surface of the skull (tDCS: transcra-nial Direct Current Stimulation; Boggio et al., 2008),magnetic stimulationat the surface of the skull (TMS: Transcranial Magnetic Stimulation;Amiaz, Levy, Vainiger, Grunhaus, & Zangen, 2009) or with themore inva-sive technique of deep brain stimulation (DBS: for a review of DBS in
chronic, treatment-resistant substance dependent patients, see Luigjeset al., 2011). First promising results have been obtained in the domainof addiction with these techniques (e.g., reductions in cocaine cravingusing rTMS, Politi, Fauci, Santoro, & Smeraldi, 2008, reductions in alcoholcraving using tDCS, Boggio et al., 2008, and alcohol intake using DBS,Kuhn et al., 2007). These new developing treatments could be imple-mented taking a stepped care approach, starting with the less invasive,cost-effective interventions before proceeding to the more invasive,more expensive interventions.
7. Conclusion
In summary, few definite conclusions regarding spontaneousrecovery of neurocognitive functioning after prolonged abstinence andconventional treatment can be drawn. The reviewed literature indicatesthat even after sustained abstinence, substance dependent subjectsdiffer from healthy controls with regard to various aspects ofneurocognitive functioning, whereas other functions may improve oreven completely recover. However, the number of high-quality studiesis limited for most substances and there is a need for well-designedstudies, preferably in combinationwith newly developed neurocognitiveenhancement interventions, including cognitive training, medication andneuromodulation. With regard to the application of such new technolo-gies, a “stepped care” approach appears most appropriate, starting withpsychosocial and/or pharmacological interventions that are evidence-based, moving to (add-on) training, medication or non-invasiveneuromodulation when standard treatments are not successful, andending with experimental medications or deep brain stimulation inchronic, treatment refractory patients. Furthermore, such researchcould help to adjust future treatment after abstinence to the‘neurocognitive profile’ of the patient (cf., Van den Brink & Schippers,2012). Finally, further research into spontaneous and aidedneurocognitive recovery is of great clinical relevance, since it appears tohelp many clients in their motivation to remain abstinent.
Acknowledgments
This review has been supported by ZonMW (Dutch Medical ScienceFoundation, 60-60600-97-275).
Mieke H. J. ter Mors-Schulte is supported by grant 022.003.038 fromNWO (Dutch National Science Foundation), awarded to the Dutch-Flemish Research School Experimental Psychopathology.
Janna Cousijn and Reinout W. Wiers are supported by VICI award453.008.001.
Tess E. den Uyl is supported by NWO Talent grant, 406-11-203 andERAB grant EA 12 39. Anna E. Goudriaan is supported by a VIDI innova-tive research grant (grant no. 91713354) funded by the Dutch ScientificResearch Association (NWO-ZonMW).
References
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disor-ders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Amiaz, R., Levy, D., Vainiger, D., Grunhaus, L., & Zangen, A. (2009). Repeated high-frequen-cy transcranial magnetic stimulation over the dorsolateral prefrontal cortex reducescigarette craving and consumption. Addiction, 104(4), 653–660.
Badiani, A., Belin, D., Epstein, D., Calu, D., & Shaham, Y. (2011). Opiate versuspsychostimulant addiction: The differences do matter. Nature Reviews Neuroscience,12, 685–700. http://dx.doi.org/10.1038/nrn3104.
Bartsch, A. J., Homola, G., Biller, A., Smith, S. M., Weijers, H., Wiesbeck, G. A., et al. (2007).Manifestations of early brain recovery associated with abstinence from alcoholism.Brain, 130, 36–47. http://dx.doi.org/10.1093/brain/awl303.
Bates, M. E., Buckman, J. F., & Nguyen, T. T. (2013). A role for cognitive rehabilitation inincreasing the effectiveness of treatment for alcohol use disorders. NeuropsychologyReview, 23(1), 27–47. http://dx.doi.org/10.1007/s11065-013-9228-3.
Bechara, A. (2005). Decision making, impulse control and loss of willpower to resistdrugs: A neurocognitive perspective. Nature Neuroscience, 8(11), 1458–1463. http://dx.doi.org/10.1038/nn1584.
Bell, R. P., Foxe, J., Nierenberg, J., Hoptman, M. J., & Garavan, H. (2011). Assessing whitematter integrity as a function of abstinence duration in former cocaine-dependent
548 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
individuals. Drug and Alcohol Dependence, 114, 159–168. http://dx.doi.org/10.1016/j.drugalcdep.2010.10.001.Assessing.
Bendszus, M., Weijers, H. G., Wiesbeck, G., Warmuth-Metz, M., Bartsch, A. J., Engels, S.,et al. (2001). Sequential MR imaging and proton MR spectroscopy in patients whounderwent recent detoxification for chronic alcoholism: Correlation with clinicaland neuropsychological data. American Journal of Neuroradiology, 22(10),1926–1932 (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11733327).
Bickel, W. K., Yi, R., Landes, R. D., Hill, P. F., & Baxter, C. (2011). Remember the future:Work-ing memory training decreases delay discounting among stimulant addicts. BiologicalPsychiatry, 69(3), 260–265. http://dx.doi.org/10.1016/j.biopsych.2010.08.017.
Block, R. I., Erwin, W. J., & Ghoneim, M. M. (2002). Chronic drug use and cognitive impair-ments. Pharmacology Biochemistry and Behavior, 73, 491–504 (Retrieved from http://www.sciencedirect.com/science/article/pii/S009130570200816X).
Boggio, P. S., Sultani, N., Fecteau, S., Merabet, L., Mecca, T., Pascual-Leone, A., et al. (2008).Prefrontal cortex modulation using transcranial DC stimulation reduces alcohol crav-ing: A double-blind, sham-controlled study. Drug and Alcohol Dependence, 92, 55–60.http://dx.doi.org/10.1016/j.drugalcdep.2007.06.011.
Callaghan, R. C., Allebeck, P., & Sidorchuk, A. (2013). Marijuana use and risk of lung can-cer: A 40-year cohort study. Cancer Causes & Control, 24(10), 1811–1820. http://dx.doi.org/10.1007/s10552-013-0259-0.
Cardenas, V. A., Studholme, C., Gazdzinski, S., Durazzo, T. C., & Meyerhoff, D. J. (2007).Deformation-based morphometry of brain changes in alcohol dependence and absti-nence. NeuroImage, 34(3), 879–887 (Retrieved from http://www.sciencedirect.com/science/article/pii/S1053811906010263).
Cordovil De Sousa Uva, M., Luminet, O., Cortesi, M., Constant, E., Derely, M., & De Timary,P. (2010). Distinct effects of protracted withdrawal on affect, craving, selective atten-tion and executive functions among alcohol-dependent patients. Alcohol andAlcoholism, 45(3), 241–246. http://dx.doi.org/10.1093/alcalc/agq012.
Cousijn, J., Goudriaan, A. E., Ridderinkhof, K. R., van den Brink, W., Veltman, D. J., & Wiers,R. W. (2013). Neural responses associated with cue-reactivity in frequent cannabisusers. Addiction Biology, 18(3), 570–580. http://dx.doi.org/10.1111/j.1369-1600.2011.00417.x.
Cunningham, J. A., & McCambridge, J. (2012). Is alcohol dependence best viewed as achronic relapsing disorder? Addiction, 107(1), 6–12. http://dx.doi.org/10.1111/j.1360-0443.2011.03583.x.
Daly, M. (2013). Personality may explain the association between cannabis use and neu-ropsychological impairment. Proceedings of the National Academy of Sciences of theUnited States of America, 110(11), E979. http://dx.doi.org/10.1073/pnas.1218571110.
Davis, G. P., Compton,M. T.,Wang, S., Levin, F. R., & Blanco, C. (2013). Association betweencannabis use, psychosis, and schizotypal personality disorder: Findings from the Na-tional Epidemiologic Survey on Alcohol and Related Conditions. SchizophreniaResearch, 151(1–3), 197–202. http://dx.doi.org/10.1016/j.schres.2013.10.018.
Dean, A. C., Sevak, R. J., Monterosso, J. R., Hellemann, G., Sugar, C. A., & London, E. D.(2011). Acute modafinil effects on attention and inhibitory control inmethamphetamine-dependent humans. Journal of Studies on Alcohol and Drugs, 72,943–953 (Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3211965&tool=pmcentrez&rendertype=abstract).
Demirakca, T., Ende, G., Kämmerer, N., Welzel-Marquez, H., Hermann, D., Heinz, A., et al.(2011). Effects of alcoholism and continued abstinence on brain volumes in bothgenders. Alcoholism, Clinical and Experimental Research, 35(9), 1678–1685. http://dx.doi.org/10.1111/j.1530-0277.2011.01514.x.
Di Sclafani, V., Tolou-Shams, M., Price, L., & Fein, G. (2002). Neuropsychological perfor-mance of individuals dependent on crack–cocaine, or crack–cocaine and alcohol, at6 weeks and 6 months of abstinence. Drug and Alcohol Dependence, 66(2), 161–171.http://dx.doi.org/10.1016/j.bbi.2008.05.010.
Dom, G., D'haene, P., Hulstijn, W., & Sabbe, B. (2006). Impulsivity in abstinent early- andlate-onset alcoholics: Differences in self-report measures and a discounting task.Addiction, 101, 50–59. http://dx.doi.org/10.1111/j.1360-0443.2005.01270.x.
Durazzo, T. C., Rothlind, J. C., Gazdzinski, S., Banys, P., & Meyerhoff, D. J. (2007). Chronicsmoking is associated with differential neurocognitive recovery in abstinent alcoholicpatients: A preliminary investigation. Alcoholism: Clinical and Experimental Research,31(7), 1114–1127. http://dx.doi.org/10.1111/j.1530-0277.2007.00398.x.
Eberl, C., Wiers, R. W., Pawelczack, S., Rinck, M., Becker, E. S., & Lindenmeyer, J. (2013).Approach bias modification in alcohol dependence: Do clinical effects replicate andfor whom does it work best? Developmental Cognitive Neuroscience, 4, 38–51.http://dx.doi.org/10.1016/j.dcn.2012.11.002.
Editorial: “Animal Farm”? [Editorial] (2014). Nature, 506(7486), 5. http://dx.doi.org/10.1038/506005a.
Ehrenreich, H., Rinn, T., Kunert, H. J., Moeller, M. R., Poser, W., Schilling, et al. (1999).Specific attentional dysfunction in adults following early start of cannabis use.Psychopharmacology, 142, 295–301.
Ernst, T., & Chang, L. (2008). Adaptation of brain glutamate plus glutamine during absti-nence from chronic methamphetamine use. Journal of Neuroimmune Pharmacology,3(3), 165–172. http://dx.doi.org/10.1007/s11481-008-9108-4.Adaptation.
Feil, J., & Zangen, A. (2010). Brain stimulation in the study and treatment of addiction.Neuroscience and Biobehavioral Reviews, 34, 559–574.
Feldtkeller, B., Weinstein, A., Cox, W. M., & Nutt, D. (2001). Effects of contextual primingon reactions to craving and withdrawal stimuli in alcohol-dependent participants.Experimental and Clinical Psychopharmacology, 9(3), 343–351 (Retrieved fromhttp://psycnet.apa.org/journals/pha/9/3/343/).
Fernández-Serrano, M. J., Pérez-García, M., & Verdejo-García, A. J. (2011). What are thespecific vs. generalized effects of drugs of abuse on neuropsychological performance?Neuroscience and Biobehavioral Reviews, 35(3), 377–406. http://dx.doi.org/10.1016/j.neubiorev.2010.04.008.
Foisy, M., Kornreich, C., Fobe, A., D'Hondt, L., Pelc, I., Hanak, C., et al. (2007). Impairedemotional facial expression recognition in alcohol dependence: Do these deficits
persist with midterm abstinence? Alcoholism: Clinical and Experimental Research,31(3), 404–410. http://dx.doi.org/10.1111/j.1530-0277.2006.00321.x.
Fox, H. C., Axelrod, S. R., Paliwal, P., Sleeper, J., & Sinha, R. (2007). Difficulties inemotion regulation and impulse control during cocaine abstinence. Drug and AlcoholDependence, 89(2–3), 298–301. http://dx.doi.org/10.1016/j.drugalcdep.2006.12.026.
Fried, P. A., Watkinson, B., & Gray, R. (2005). Neurocognitive consequences of marihuana—A comparison with pre-drug performance. Neurotoxicology and Teratology, 27,231–239. http://dx.doi.org/10.1016/j.ntt.2004.11.003.
Friedman, N. P., Miyake, A., Young, S. E., Defries, J. C., Corley, R. P., & Hewitt, J. K. (2008).Individual differences in executive functions are almost entirely genetic in origin.General Journal of Experimental Psychology, 137(2), 201–225. http://dx.doi.org/10.1037/0096-3445.137.2.201.
Fujiwara, E., Brand, M., Borsutzky, S., Steingass, H. -P., & Markowitsch, H. J. (2008).Cognitive performance of detoxified alcoholic Korsakoff syndrome patients remainsstable over two years. Journal of Clinical and Experimental Neuropsychology, 30(5),576–587. http://dx.doi.org/10.1080/13803390701557271.
Gazdzinski, S., Durazzo, T. C., & Meyerhoff, D. J. (2005). Temporal dynamics anddeterminants of whole brain tissue volume changes during recovery from alcoholdependence. Drug and Alcohol Dependence, 78(3), 263–273. http://dx.doi.org/10.1016/j.drugalcdep.2004.11.004.
Gazdzinski, S., Durazzo, T. C., Yeh, P. H., Hardin, D., Banys, P., & Meyerhoff, D. J. (2008).Chronic cigarette smoking modulates injury and short-term recovery of the medialtemporal lobe in alcoholics. Psychiatry Research, 162(2), 133–145. http://dx.doi.org/10.1016/j.pscychresns.2007.04.003.Chronic.
Gevensleben, H., Holl, B., Albrecht, B., Schlamp, D., Kratz, O., Studer, P., et al. (2009). Dis-tinct EEG effects related to neurofeedback training in children with ADHD: A ran-domized controlled trial. International Journal of Psychophysiology, 74, 149–157.
Goudriaan, A. E., Veltman, D. J., van den Brink, W., Dom, G., & Schmaal, L. (2013). Neuro-physiological effects of modafinil on cue-exposure in cocaine dependence: A ran-domized placebo‐controlled cross-over study using pharmacological fMRI. AddictiveBehaviors, 28(2), 1509–1517.
Hanson, K. L., Medina, K. L., Padula, C. B., Tapert, S. F., & Brown, S. A. (2011). Impact ofadolescent alcohol and drug use on neuropsychological functioning in youngadulthood: 10-year outcomes. Journal of Child & Adolescent Substance Abuse, 20(2),135–154. http://dx.doi.org/10.1080/1067828X.2011.555272.
Heinz, A., Reimold, M., Wrase, J., Hermann, D., Croissant, B., Mundle, G., et al. (2005).Correlation of stable elevations in striatal mu-opioid receptor availability indetoxified alcoholic patients with alcohol craving: A positron emission tomographystudy using carbon 11-labeled carfentanil. Archives of General Psychiatry, 62, 57–64.http://dx.doi.org/10.1001/archpsyc.62.1.57.
Heyman, G. M. (2009). Addiction: A disorder of choice. Harvard University Press.Horwood, L. J., Fergusson, D. M., Hayatbakhsh, M. R., Najman, J. M., Coffey, C., Patton, G. C.,
et al. (2010). Cannabis use and educational achievement: Findings from three Aus-tralasian cohort studies. Drug and Alcohol Dependence, 110(3), 247–253. http://dx.doi.org/10.1016/j.drugalcdep.2010.03.008.
Houben, K., Wiers, R. W., & Jansen, A. (2011). Getting a grip on drinking behavior: Train-ing working memory to reduce alcohol abuse. Psychological Science, 22(7), 968–975.http://dx.doi.org/10.1177/0956797611412392.
Iudicello, J. E., Woods, S. P., Vigil, O., Scott, J. C., Cherner, M., Heaton, R. K., et al. (2010).Longer term improvement in neurocognitive functioning and affective distressamong methamphetamine users who achieve stable abstinence. Journal of Clinicaland Experimental Neuropsychology, 32(7), 704–718. http://dx.doi.org/10.1080/13803390903512637.
Joos, L., Goudriaan, A. E., Schmaal, L., Fransen, E., van den Brink, W., Sabbe, B. G. C., et al.(2013). Effect of modafinil on impulsivity and relapse in alcohol dependent patients:A randomized, placebo-controlled trial. European Neuropsychopharmacology, 23,948–955. http://dx.doi.org/10.1016/j.euroneuro.2012.10.004.
Kalman, D., Kim, S., DiGirolamo, G., Smelson, D., & Ziedonis, D. (2010). Addressing tobaccouse disorder in smokers in early remission from alcohol dependence: The case forintegrating smoking cessation services in substance use disorder treatmentprograms. Clinical Psychology Review, 30(1), 12–24. http://dx.doi.org/10.1016/j.cpr.2009.08.009.
Kane, M. J., Bleckley, M. K., Conway, A. R. A., & Engle, R. W. (2001). A controlled-attentionview of working-memory capacity. General Journal of Experimental Psychology,130(2), 169–183 (Retrieved from http://psycnet.apa.org/psycinfo/2001-17501-002).
Kane, M. J., & Engle, R. W. (2002). The role of prefrontal cortex in working-memorycapacity, executive attention, and general fluid intelligence: an individual-differences perspective. Psychonomic Bulletin & Review, 9(4), 637–671 (Retrievedfrom http://www.ncbi.nlm.nih.gov/pubmed/12613671).
Klingberg, T. (2010). Training and plasticity of working memory. Trends in CognitiveSciences, 14, 317–324. http://dx.doi.org/10.1016/j.tics.2010.05.002.
Kuhn, J., Lenartz, D., Huff, W., Lee, S., Koulousakis, A., Klosterkoetter, J., et al. (2007).Remission of alcohol dependency following deep brain stimulation of the nucleusaccumbens: Valuable therapeutic implications? Journal of Neurology, Neurosurgery,and Psychiatry, 78(10), 1152–1153. http://dx.doi.org/10.1136/jnnp.2006.113092.
Leshner, A. I. (1997). Addiction is a brain disease, and it matters. Science, 278(5335),45–47. http://dx.doi.org/10.1126/science.278.5335.45.
Li, X., Hartwell, K. J., Borckardt, J., Prisciandaro, J. J., Saladin, M. E., Morgan, P. S., et al.(2012). Volitional reduction of anterior cingulate cortex activity produces decreasedcue craving in smoking cessation: A preliminary real-time fMRI study. AddictionBiology, 18, 739–748. http://dx.doi.org/10.1111/j.1369-1600.2012.00449.x.
Linden, D. E. J., Habes, I., Johnston, S. J., Linden, S., Tatineni, R., Subramanian, L., et al.(2012). Real-time self-regulation of emotion networks in patients with depression.PLoS ONE, 7(6) e38115.
Loeber, S., Duka, T., Welzel Márquez, H., Nakovics, H., Heinz, A., Mann, K., et al. (2010). Ef-fects of repeatedwithdrawal from alcohol on recovery of cognitive impairment under
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3211965&tool=pmcentrez&rendertype=abstract
549M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
abstinence and rate of relapse. Alcohol and Alcoholism, 45(6), 541–547. http://dx.doi.org/10.1093/alcalc/agq065.
Luigjes, J., van den Brink, W., Feenstra, M., van den Munckhof, P., Schuurman, P. R.,Schippers, R., et al. (2011). Deep brain stimulation in addiction: A review of potentialbrain targets. Molecular Psychiatry, 17, 572–583.
MacLeod, C., & Mathews, A. (2012). Cognitive bias modification approaches to anxiety.Annual Review of Clinical Psychology, 8, 189–217. http://dx.doi.org/10.1146/annurev-clinpsy-032511-143052.
Manning, V., Wanigaratne, S., Best, D., Hill, R. G., Reed, L. J., Ball, D., et al. (2008). Changesin neuropsychological functioning during alcohol detoxification. European AddictionResearch, 14, 226–233. http://dx.doi.org/10.1159/000156479.
Marissen, M. A. E., Franken, I. H. A., Waters, A. J., Blanken, P., van den Brink, W., &Hendriks, V. M. (2006). Attentional bias predicts heroin relapse following treatment.Addiction, 101, 1306–1312. http://dx.doi.org/10.1111/j.1360-0443.2006.01498.x.
Mattick, R., & Breen, C. (2009). Methadone maintenance therapy versus no opioid re-placement therapy for opioid dependence. Cochrane Database of SystematicReviews(3) (Retrieved from http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002209.pub2/pdf/standard).
McDonald, S., Darke, S., Kaye, S., & Torok, M. (2013). Deficits in social perception in opioidmaintenance patients, abstinent opioid users and non-opioid users. Addiction(Abingdon, England), 108(3), 566–574. http://dx.doi.org/10.1111/add.12040.
Meehl, P. (1970). Nuisance variables and the ex post facto design. Analyses of theories andmethods of physics and psychology (pp. 373–402). Minneapolis: University of Minnesota.
Meier, M. H., Caspi, A., Ambler, A., Harrington, H., Houts, R., Keefe, R. S. E., et al. (2012).Persistent cannabis users show neuropsychological decline from childhood to mid-life. Proceedings of the National Academy of Sciences of the United States of America,109(40), E2657–E2664. http://dx.doi.org/10.1073/pnas.1206820109.
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D.(2000). The unity and diversity of executive functions and their contributions tocomplex “Frontal Lobe” tasks: A latent variable analysis. Cognitive Psychology, 41(1),49–100. http://dx.doi.org/10.1006/cogp.1999.0734.
Moffitt, T. E., Meier, M. H., Caspi, A., & Poulton, R. (2013). Reply to Rogeberg and Daly: Noevidence that socioeconomic status or personality differences confound the associa-tion between cannabis use and IQ decline. Proceedings of the National Academy ofSciences, 110(11), E980–E982. http://dx.doi.org/10.1073/pnas.1300618110.
Mon, A., Durazzo, T. C., Gazdzinski, S., Hutchison, K. E., Pennington, D., & Meyerhoff, D. J.(2013). Brain-derived neurotrophic factor genotype is associated with brain grayand white matter tissue volumes recovery in abstinent alcohol-dependent individ-uals. Genes, Brain, and Behavior, 12(1), 98–107. http://dx.doi.org/10.1111/j.1601-183X.2012.00854.x.
Moriyama, Y., Muramatsu, T., Kato, M., Mimura, M., & Kashima, H. (2006). Family historyof alcoholism and cognitive recovery in subacute withdrawal. Psychiatry and ClinicalNeurosciences, 60, 85–89. http://dx.doi.org/10.1111/j.1440-1819.2006.01464.x.
Nigg, J., Glass, J. M., Wong, M. M., Poon, E., Jester, J. M., Fitzgerald, H. E., et al. (2004). Neu-ropsychological executive functioning in children at elevated risk for alcoholism:Findings in early adolescence. Journal of Abnormal Psychology, 113(2), 302–314.http://dx.doi.org/10.1037/0021-843X.113.2.302.
Orford, J. (2001). Addiction as excessive appetite. Addiction (Abingdon, England), 96(1),15–31. http://dx.doi.org/10.1080/09652140020016932.
Pace-Schott, E. F., Morgan, P. T., Malison, R. T., Hart, C. L., Edgar, C., Walker, M., et al.(2008). Cocaine users differ from normals on cognitive tasks which show poorer per-formance during drug abstinence. The American Journal of Drug and Alcohol Abuse,34(1), 109–121. http://dx.doi.org/10.1080/00952990701764821.
Penick, E. C., Knop, J., Nickel, E. J., Jensen, P., Manzardo, A. M., Lykke-Mortensen, E., et al.(2010). Do premorbid predictors of alcohol dependence also predict the failure to re-cover from alcoholism? Journal of Studies on Alcohol and Drugs, 71, 685–694(Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2930498&tool=pmcentrez&rendertype=abstract).
Peterson, J. B., Finn, P. R., & Pihl, R. O. (1992). Cognitive dysfunction and the inheritedpredisposition to alcoholism. Journal of Studies on Alcohol and Drugs, 53(2),154–160 (Retrieved from http://www.jsad.com/jsad/article/Cognitive_Dysfunction_and_the_Inherited_Predisposition_to_Alcoholism_/1789.html).
Pitel, A. L., Rivier, J., Beaunieux, H., Vabret, F., Desgranges, B., & Eustache, F. (2009).Changes in the episodic memory and executive functions of abstinent and relapsedalcoholics over a 6-month period. Alcoholism: Clinical and Experimental Research,33(3), 490–498. http://dx.doi.org/10.1111/j.1530-0277.2008.00859.x.
Politi, E., Fauci, E., Santoro, A., & Smeraldi, E. (2008). Daily sessions of transcranial magneticstimulation to the left prefrontal cortex gradually reduce cocaine craving. The AmericanJournal on Addictions, 17, 345–346. http://dx.doi.org/10.1080/10550490802139283.
Pope, H. G., Gruber, A., Hudson, J. I., Huestis, M. A., & Yurgelun-Todd, D. (2001). Neuropsy-chological performance in long-term cannabis users. Archives of General Psychiatry,58(10), 909–915 (Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11576028).
Pope, H. G., Gruber, A. J., Hudson, J. I., Huestis, M. A., & Yurgelun-Todd, D. (2002). Cognitivemeasures in long-term cannabis users. The Journal of Clinical Pharmacology, 42(11suppl), 41S–47S. http://dx.doi.org/10.1177/0091270002238793.
Rogeberg, O. (2013). Reply to Moffitt et al.: Causal inference from observational data re-mains difficult. Proceedings of the National Academy of Sciences, 110(11), E983-E983.http://dx.doi.org/10.1073/pnas.1301881110.
Rosenbloom, M. J., Pfefferbaum, A., & Sullivan, E. V. (2004). Recovery of short-termmem-ory and psychomotor speed but not postural stability with long-term sobriety in al-coholic women. Neuropsychology, 18(3), 589–597. http://dx.doi.org/10.1037/0894-4105.18.3.589.
Rosenbloom, M. J., Rohlfing, T., O'Reilly, A. W., Sassoon, S. A., Pfefferbaum, A., & Sullivan, E.V. (2007). Improvement in memory and static balance with abstinence in alcoholicmen and women: Selective relations with change in brain structure. PsychiatryResearch, 155(2), 91–102. http://dx.doi.org/10.1016/j.bbi.2008.05.010.
Schoenmakers, T. M., de Bruin, M., Lux, I. F. M., Goertz, A. G., Van Kerkhof, D. H. A. T., &Wiers, R. W. (2010). Clinical effectiveness of attentional bias modification trainingin abstinent alcoholic patients. Drug and Alcohol Dependence, 109, 30–36. http://dx.doi.org/10.1016/j.drugalcdep.2009.11.022.
Schumann, G., Loth, E., Banaschewski, T., Barbot, A., Barker, G., Büchel, C., et al. (2010). TheIMAGEN study: Reinforcement-related behaviour in normal brain function and psy-chopathology. Molecular Psychiatry, 15, 1128–1139. http://dx.doi.org/10.1038/mp.2010.4.
Schweinsburg, A. D., Schweinsburg, B. C., Medina, K. L., McQeeny, T., Brown, S. A., & Tapert,S. F. (2010). The influence of recency of use on fMRI response during spatial workingmemory in adolescent marijuana users. Journal of Pscyhoactive Drugs, 42(3), 401–412.http://dx.doi.org/10.1016/j.bbi.2008.05.010.
Sher, K. J., Walitzer, K. S., Wood, P. K., & Brent, E. E. (1991). Characteristics of children ofalcoholics: Putative risk factors, substance use and abuse, and psychopathology.Journal of Abnormal Psychology, 100(4), 427–448.
Simon, S. L., Dean, A. C., Cordova, X., Monterosso, J. R., & London, E. D. (2010). Metham-phetamine dependence and neuropsychological functioning: Evaluating change dur-ing early abstinence. Journal of Studies on Alcohol and Drugs, 71(3), 335–344.
Sofuoglu, M., DeVito, E. E., Waters, A. J., & Carroll, K. M. (2013). Cognitive enhancement asa treatment for drug addictions. Neuropharmacology, 64, 452–463. http://dx.doi.org/10.1016/j.neuropharm.2012.06.021.
Sofuoglu, M., Herman, A. I., Li, Y., & Waters, A. J. (2012). Galantamine attenuates some ofthe subjective effects of intravenous nicotine and improves performance on a Go No-Go task in abstinent cigarette smokers: A preliminary report. Psychopharmacology,224, 413–420. http://dx.doi.org/10.1007/s00213-012-2763-4.
Sokhadze, T. M., Cannon, R. L., & Trudeau, D. L. (2008). EEG biofeedback as a treatment forsubstance use disorders: Review, rating of efficacy, and recommendations for furtherresearch. Applied Psychophysiology and Biofeedback, 33(1), 1–28.
Sonuga-Barke, E. J. S., Brandeis, D., Cortese, S., Daley, D., Ferrin, M., Holtmann, M., et al.(2013). Nonpharmacological interventions for ADHD: Systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments.The American Journal of Psychiatry, 170(3), 275–289. http://dx.doi.org/10.1176/appi.ajp.2012.12070991.
Stavro, K., Pelletier, J., & Potvin, S. (2013). Widespread and sustained cognitive deficits inalcoholism: A meta-analysis. Addiction Biology, 18(2), 203–213. http://dx.doi.org/10.1111/j.1369-1600.2011.00418.x.
Stevens, L., Verdejo-García, A., Goudriaan, A. E., Roeyers, H., Dom, G., & Vanderplasschen,W. (2014). Impulsivity as a vulnerability factor for poor addiction treatment out-comes: A review of neurocognitive findings among individuals with substance usedisorders. Journal of Substance Abuse Treatment, 47(1), 58–72. http://dx.doi.org/10.1016/j.jsat.2014.01.00.
Strack, F., & Deutsch, R. (2004). Reflective and impulsive determinants of social behavior.Personality and Social Psychology Review, 8(3), 220–247. http://dx.doi.org/10.1207/s15327957pspr0803_1.
Sullivan, E. V., Rosenbloom, M. J., Lim, K. O., & Pfefferbaum, A. (2000). Longitudinal chang-es in cognition, gait, and balance in abstinent and relapsed alcoholic men: Relation-ships to changes in brain structure. Neuropsychology, 14(2), 178–188. http://dx.doi.org/10.1037//0894-4105.14.2.178.
UNODC (2012). World Drug Report. United Nations publication (Sales No. E.12.XI.1).Van den Brink,W., & Schippers, G. M. (2012). Staging and profiling in addiction. Tijdschrift
voor Psychiatrie, 54(11), 941–948.Van Holst, R. J., & Schilt, T. (2011). Drug-related decrease in neuropsychological functions
of abstinent drug users. Current Drug Abuse Reviews, 4(1), 42–56 (Retrieved fromhttp://www.ncbi.nlm.nih.gov/pubmed/21466500).
Volkow, N. D., Fowler, J. S., & Wang, G. (2004). The addicted human brain viewed in thelight of imaging studies: Brain circuits and treatment strategies. Neuropharmacology,47, 3–13. http://dx.doi.org/10.1016/j.neuropharm.2004.07.019.
Volkow, N. D., & Li, T. -K. (2005). Drugs and alcohol: Treating and preventing abuse, ad-diction and their medical consequences. Pharmacology & Therapeutics, 108(1), 3–17.http://dx.doi.org/10.1016/j.pharmthera.2005.06.021.
Weiskopf, N. (2012). Real-time fMRI and its application to neurofeedback. NeuroImage,62, 682–692. http://dx.doi.org/10.1016/j.neuroimage.2011.10.009.
White, H. R., Marmorstein, N. R., Crews, F. T., Bates, M. E., Mun, E. Y., & Loeber, R. (2011).Associations between heavy drinking and changes in impulsive behavior among ad-olescent boys. Alcoholism, Clinical and Experimental Research, 35, 295–303.
Wiers, R. W., Bartholow, B. D., van denWildenberg, E., Thush, C., Engels, R. C. M. E., Sher, K.J., et al. (2007). Automatic and controlled processes and the development of addictivebehaviors in adolescents: A review and a model. Pharmacology, Biochemistry, andBehavior, 86, 263–283. http://dx.doi.org/10.1016/j.pbb.2006.09.021.
Wiers, R. W., Eberl, C., Rinck, M., Becker, E. S., & Lindenmeyer, J. (2011). Retraining auto-matic action tendencies changes alcoholic patients' approach bias for alcohol and im-proves treatment outcome. Psychological Science, 22(4), 490–497. http://dx.doi.org/10.1177/0956797611400615.
Wiers, R. W., Gladwin, T. E., Hofmann, W., Salemink, E., & Ridderinkhof, K. R. (2013).Cognitive bias modification and cognitive control training in addiction and relatedpsychopathology: Mechanisms, clinical perspectives, and ways forward. ClinicalPsychological Science, 1(2), 192–212. http://dx.doi.org/10.1177/2167702612466547.
Wiers, R.W., Rinck, M., Kordts, R., Houben, K., & Strack, F. (2010). Re-training utomatic ac-tion-tendencies to approach alcohol in hazardous drinkers. Addiction, 105, 279–287.
Wykes, T., Huddy, V., Cellard, C., McGurk, S. R., & Czobor, P. (2011). A meta-analysis ofcognitive remediation for schizophrenia: Methodology and effect sizes. TheAmerican Journal of Psychiatry, 168, 472–485. http://dx.doi.org/10.1176/appi.ajp.2010.10060855.
Zack, M., & Poulos, C. X. (2009). Effects of the atypical stimulant modafinil on a briefgambling episode in pathological gamblers with high vs. low impulsivity. Journal ofPsychopharmacology, 23(6), 660–671. http://dx.doi.org/10.1177/0269881108091072.
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2930498&tool=pmcentrez&rendertype=abstract
550 M.H.J. Schulte et al. / Clinical Psychology Review 34 (2014) 531–550
Zhang, X., Shi, J., Zhao, L., Sun, L., Wang, J., Wang, G., et al. (2011). Effects of stress ondecision-making deficits in formerly heroin-dependent patients after different dura-tions of abstinence. American Journal of Psychiatry, 168(6), 610–616 (Retrieved fromhttp://ajp.psychiatryonline.org/cgi/content/abstract/168/6/610).
Zhao, M., Fan, C., Du, J., Jiang, H., Chen, H., & Sun, H. (2012). Cue-induced cravingand physiological reactions in recently and long-abstinent heroin-dependentpatients. Addictive Behaviors, 37(4), 393–398. http://dx.doi.org/10.1016/j.addbeh.2011.11.030.
Related Documents