-
7/28/2019 PVD K2
1/52
Peripheral Vascular
DiseaseGUNAWAN TOHIR
FK UMP PALEMBANG
2012
-
7/28/2019 PVD K2
2/52
Peripheral Vascular Disorders Ischemia-lack of blood
supply to meet the
needs of the tissue.
Causes of Ischemia
vasoconstriction
occlusion of lumen of
the artery due to:
Atherosclerosis (fatty
deposits)
Thrombosis/bloodclot/embolism
s/s = coldness, pallor,
or rubor (redness),
cyanosis (blueness) pain, changes in skin or
nails
-
7/28/2019 PVD K2
3/52
-
7/28/2019 PVD K2
4/52
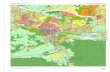
PRIMARY SITESOF
INVOLVEMENT
Femoral & Popliteal
arteries: 80-90%
Tibial & Peroneal
arteries: 40-50%
Aorta & Iliac arteries:
30%
Harrisons Principles of
Int Med
-
7/28/2019 PVD K2
5/52
-
7/28/2019 PVD K2
6/52
PVD
-
7/28/2019 PVD K2
7/52
DOPPLER
-
7/28/2019 PVD K2
8/52
Peripheral Arterial Occlusive
Disease (830) Pathophysiology: Narrowing and sclerosis of large
arteries (femoral, iliac, popliteal) especially atbifurcations due to plaque formation
Risk factors: smoking, obesity, sedentary lifestyle,HTN, DM, hyperlipidemia, Fa hx
S/S: see previous slide. May also have bruit overfemoral or popliteal : doppler area
Dx Tests: US, exercise testing (822), pulsevolumes, angiography (823), Trendelenberg test (seeAssessment text)
-
7/28/2019 PVD K2
9/52
Peripheral Vascular Diseases Arterial Manifestations:
Diminished or absent pulses
Smooth, shiny, dry skin, nohair
No edema
Round, regularly shapedpainful ulcers on distal foot,toes or webs of toes
Dependent rubor
Pallor and pain when legselevated
Intermittent claudication
Brittle, thick nails
Venous Manifestations:
Normal pulses
Brown patches ofdiscoloration on lower legs
Dependent edema
Irregularly shaped, usuallypainless ulcers on lower legsand ankles
Dependent cyanosis and
pain Pain relief when legs
elevated
No intermittent claudication
Normal nails
-
7/28/2019 PVD K2
10/52
Physical Assessment of PVD Arterial disease:
acutepain,intermittent
claudication (pain
increases with exercise,relieved with rest), hair
loss distant with
occulusion, thick brittle
nails
Parasthesia, pallor
when limb elevated,
rubor when limb
dependent(down), skintemp cold,
dimished/weak/or
absent pulses, no
edema, but ulcers in
distal areas, foot, toes,
ankles, calves
-
7/28/2019 PVD K2
11/52
Physical Assessment of PVD
Venous disease
little or no pain, some
tenderness along
inflamed vein,
no hair loss, skin color
brawny(reddish-
brown),cyanotic if
dependent position
Veins may be visible,
warm skin temperature,
edema typically
present, pulses normaland present/palpable,
no changes in hair or
nails, little skin
breakdown (ulcers)
-
7/28/2019 PVD K2
12/52
Risk Factors-PVD
Being a man over age
50 yr. of age
cigarette smoking hypertension, high
cholesterol
heart disease and
diabetes
inability of the kidneys
to filter out waste
products
And maintain fluid
balance
no/little exercise obesity
wearing tight
obstructive
garments/girdles,elastic top
socks/garters
-
7/28/2019 PVD K2
13/52
HOW DOES AN INTERMITTENT
-
7/28/2019 PVD K2
14/52
HOW DOES AN INTERMITTENT
CLAUDICATION PATIENT PRESENT
CLINICALLY?
Leg pain caused and reproduced by a certain degree
of exertion
Relieved by rest
Not affected by body position Atherosclerotic lesions usually found in arterial
segment one level above affected muscle group
Calf claudication more commonly due to disease in
femoral arteries and less commonly due to diseasein popliteal or proximal tibial or peroneal arteries;
Hip/Thigh/Buttock claudication due to aortoiliac
disease
Am J Cardiol 2001; 87 (suppl): 3D-13D
-
7/28/2019 PVD K2
15/52
DIFFERENTIAL DIAGNOSISCALF
Venous occlusion
Tight bursting pain /
dull ache that worsens
on standing and resolveswith leg elevation
Positional pain relief
Chronic compartment
syndromeTight bursting pain
Positional pain relief
Nerve root compression
Positional pain relief
HIP/THIGH/BUTTOCK Arthritis
Persistent pain, brought
on by variable amounts
of exercise
Associated symptoms inother joints
Spinal cord compression
History of back pain
Symptoms while
standing
Positional pain reliefFOOT
Arthritis
Buerger disease
(thromboangitis obliterans)
Am J Cardiol 2001; 87 (suppl): 3D-13D
-
7/28/2019 PVD K2
16/52
-
7/28/2019 PVD K2
17/52
-
7/28/2019 PVD K2
18/52
DIAGNOSIS History taking
Careful examination of leg
Pulse evaluation
Ankle-brachial index (ABI):
SBP in ankle (dorsalis pedis and posterior tibial
arteries)
___________________________________
SBP in upper arm (brachial artery)
Am J Cardiol 2001; 87 (suppl): 3D-13D
NEJM 2001; 344: 1608-1621
-
7/28/2019 PVD K2
19/52
-
7/28/2019 PVD K2
20/52
Ankle-Brachial Index Values and
Clinical Classification
Clinical Presentation Ankle-Brachial Index
Normal > 0.90
Claudication 0.50-0.90
Rest pain 0.21-0.49
Tissue loss < 0.20
Am J Cardiol 2001; 87 (suppl): 3D-13D
NEJM 2001; 344: 1608-1621
Values >1.25 falsely elevated; commonly seen in diabetics
-
7/28/2019 PVD K2
21/52
-
7/28/2019 PVD K2
22/52
-
7/28/2019 PVD K2
23/52
-
7/28/2019 PVD K2
24/52
The history and physical examination
(pulse evaluation and careful
examination of the leg) are usually
sufficient to establish the diagnosis
P i itif
-
7/28/2019 PVD K2
25/52
Diagnostik Buerger nilai positif
Kriteria +1 +2
Usia onset 30-40 tahun
Klaudikasio intermiten kaki Ada riwayat Ada saat pemeriksaan
Ekstremitas atas asimptomatik Simptomatik
Tromboflebitis superficial migrans Ada riwayat Ada saat pemeriksaan
Fenomena Raynaud Ada riwayat Ada saat pemeriksaan
Angiografi, biopsi Khas untuk salah satu Khas untuk keduanya
Poin positif
-
7/28/2019 PVD K2
26/52
Nilai negatif
Kriteria -1 -2
Usia onset 45-50 tahun >50 tahun
Jenis kelamin, kebiasaan merokok wanita Tidak merokok
lokasi 1 ekstremitas Tidak ada ekstremitas yang terlibat
Hilangnya pulsasi brakial Femoral
Artiosklerosis, DM, hipertensi,
hiperlipidemi
Terdiagnosis dalam 5-10 tahun kemudian Terdiagnosis dalam 2-5 tahun kemudian
-
7/28/2019 PVD K2
27/52
Interpretasi
Interpretasi dari total poin-poin tersebut antara
lain
0-1 diagnosisBuergers disease tersingkirkan 2-3 tersangka, probabilitas rendah
4-5 probabilitas sedang
6 probabilitas tinggi, diagnosis dapatdipastikan
-
7/28/2019 PVD K2
28/52
Raynauds & Buergers DZ
Raynauds-periodic
constriction ofarteries
that supply extremities,
mostly hands and feet
arteriospastic (pulses
never absent) spaz-out!
Freq. Young women s/s usually precipitated
by
Exposure to cold,
emotional upset,
tobacco usage.
3-color changes,
vasoconstrictive pallor-
cyanosis-ruboror
hyperemia cold, numbness,
pain,tingling,swelling
lasts minutes-hrs.
-
7/28/2019 PVD K2
29/52
Continued: Raynauds disease
Pallor-cyanosis
(especially fingers)-
painful-aching pain-
client learns warmth
relieves pain-go inside
warm, or placed in
warm water-which
relieves vasopsasms-
blood rushes to the
extremity
Ulcers/gangrene &
pain may appear at
fingertips with
chronicity
TX-prevent chilling,
avoid risk factors, no
ETOH,tobacco, weargloves, heat,
vasodilators, avoid
stress
-
7/28/2019 PVD K2
30/52
Buergers dz (arterial/venous)
thromboangitis obliterans
Inflamm. Of bld
vessels (arteries/veins)
and formations of clots
(thrombus)
usually lower
extremities
association: tobaccousage,men 25-40yrs
S/S- my foot fell
asleep,foot always
cold,
cyanosis,redness/
mottled-purplish-red of
the foot/leg, pain,
phlebitis may occur,
ulcers,gangrene,
changes skin/nails if
circl. is impaired
-
7/28/2019 PVD K2
31/52
Acute Arterial Occlusive Disease
(arterial embolism-840)
Pathophysiology: blood clots from arteries, left
ventricle, or trauma suddenly break loose and
become free flowing, lodge in bifurcations, causing
obstruction distally with acute and sudden symptoms
Assessment: +6 Ps (pain, pallor, pulselessness,
paresthesia, paralysis, poikilothermia), ABI
-
7/28/2019 PVD K2
32/52
Management of Arterial
Embolism
Medical:
Anticoagulants-heparin bolus then 1000U/hr
Thrombolytics
Surgical (depends on occlusion time): Embolectomy (840)
Bypass
Angioplasty with stent placement
Nursing:
Administer and monitor anticoag or thrombolytic tx
If surgery, then monitor for postop angioplasty and stentplacement, bypass, or embolectomy (similar to bypass
except no ICU and hospital time is less).
-
7/28/2019 PVD K2
33/52
Buergers Disease
(thromboangiitis obliterans-834)
Pathophysiology: obstructive and inflammatory
disease of small and medium sized arteries and
veins. Believed to be autoimmune. Has
exacerbations and remissions. Smoking is very high
risk factor.
Assessment: pain and instep claudication, intense
rubor, absence of distal pulses (pedal, radial, ulnar),paresthesias; segmental limb blood pressures, US,
angiography
-
7/28/2019 PVD K2
34/52
Management of Buergers
Disease
Medical/Surgical:
Pain meds
Stop smoking
Treatment of infection and gangrene Sympathectomy (removal of sympathetic ganglia or
branches-causes permanent vasodilation
Amputation
Nursing: Support stopping smoking
Administer pain meds
Education regarding protection extremities from cold and
trauma.
-
7/28/2019 PVD K2
35/52
Raynauds Disease (841)
Pathophysiology: arterial spasms of small
cutaneous vessels of fingers and toes. May
have too many alpha 2 receptors leading tovasoconstriction and not enough beta
receptors. Aggravated by cold and stress.
Assessment: classic tri-color symptoms-pallor, cyanosis, rubor, pain, and paresthesia.
Bilateral and symmetric.
-
7/28/2019 PVD K2
36/52
Management of Raynauds
Disease
Medical/Surgical:
Avoiding cold, stress, nicotine
Ca++ channel blockers (particularly nifedipine) especially
for acute vasospasm sympathectomy
Nursing:
Avoid stress, take stress mgmt classes
Avoid cold and trauma Teach about nifedipine (can cause orthostatic
hypotension)
-
7/28/2019 PVD K2
37/52
Hypertension (855)
Definitions and Etiology:
SBP > 140 and DBP > 90 at least 3 times.
Affects 20-25% of population. 90-95% have primary or
essential HTN (unknown etiology). Other 5-10% havesecondary, meaning there is a disease process causing it(i.e., thyrotoxicosis, renal artery stenosis,
pheochromocytoma). Hypertensive crisis-DBP > 120.Malignant HTN-rises rapidly. White coat HTN-
increased BP when patient goes to MD. Risk factors are similar to CAD
Classifications p. 855, Table 32-1
-
7/28/2019 PVD K2
38/52
Assessment of HTN
S/S:
Usually absent unless
severe or advanced
If symptoms theyinclude HA, blurred
vision, dizziness,
nosebleeds
BP > 140/90
S4 gallop rhythm
Dx Tests:
BP readings
CBC, UA, lytes, lipids,
glucose, renal and liverfunctions
ECG
CXR
Echo
-
7/28/2019 PVD K2
39/52
TX-management of Buergers Disease
No tobacco , avoid
factors cause
vasoconstriction
Avoid becoming chilled,wear warm socks, boots,
gloves, warm water
baths
Avoid prolongedstanding- job changes?
Nursing?
Avoid injury/infection
exercising to stimulatecirculation, however, aslong as it doesnt cause
pain
Buerger-Allen exercises-
Do not keep legselevated-ischemia
vasodilators/anti-
coagulants may help
-
7/28/2019 PVD K2
40/52
Buerger-Allen exercises Elevate feet/legs till feet
blanch(whitish), thenlowering them till turnred, then resting legs/feet
in a horizontal position.
Client performs exerciseslying in bed or on sofa.
Dr. tells client how often
to perform them
The client is instructed to
watch the changes in
color blanching indicates
inadequate blood.Supply-maintaining this
position could harm
tissues (death)
May instead walk, foot
exercises help too
-
7/28/2019 PVD K2
41/52
Varicose Veins-dilated tortuous
veins, with incompetent valves
Competent Valves
allow bld. To return to
the heart and prevent
back-flow
Risk factors: obesity,
standing in 1 place too
long, pregnancy constriction and or
pressure on the legs
Generally, bld collects
Saphenous Vein,
Superficial Veins
dilated and distended,dark blue
purplish swellings
c/o legs tired/heavyfeeling, cramping pain
-
7/28/2019 PVD K2
42/52
TX & Management of Varicosities
TX: ligation/stripping-
may use surgical or
more likely lasar tx.
Zap- them
DX- Doppler studies
Injection
sclerotherapy- old tx Prevention-Best Tx
Avoid sitting/standing
for long periods of time
maintain ideal body
weight
avoid injury to legs
no crossing legs
no constrictiveclothing/hosiery
-
7/28/2019 PVD K2
43/52
Continued Tx: Varicosities
Elastic stockings long-
(TED) hose- removed
once q 8hr. X 30min.
Check skin
Promote circulation
Taught to apply hose
while lying in bed w/legs elevated
Change position
frequently
Keep legs elevated at
rest, to promote venous
return back to the heart
Avoid infections, wear
comfortable but
supportive shoes
Maintain weight
-
7/28/2019 PVD K2
44/52
Disorders of veins-most common is thrombophlebitis-
formation of a thrombus (clot)in association with
inflammation of vein
Classified as either
superficial or deep
65% IV therapy-
superficial; 5% of
surgical patients-deep,
especially bedrest, long
abdominal surgery, hip,
anything causes venousstasis
Worry clot-travels or
emboli to lung, heart,
brain
Etiology- 3 things
In 1846, VirchowsTriad: formation of clot
1.venous stasis/pooling2.damage of endothelium
or inner lining of vein 3. hypercoagulabilty of
blood-
are your clients high risk
to any of these? Prolonged bedrest,
obesity,varicose veins,hip/knee replacements,Oral contraceptives.
-
7/28/2019 PVD K2
45/52
Thrombophlebitis- superficial or
deep (DVT)?
Superficial
palpable, firm, cordlike
vein, surrounding vein,
warm, reddened,
tender, edema maybe
IV therapy-arms
varicose veins-legs
Deep- DVT
no s/s in 50% of casesor unilateral leg
edema/swelling, pain,warm skin, mildtemp, cyanosis
possibly, Positive
Homans sign: painupon dorsiflexion offoot - but not always
present in all cases
-
7/28/2019 PVD K2
46/52
Dx- thrombophlebitis-Various ( venogram, non-invasive doppler
studies, coagulation studies PT,PTT,platelet ct., bleeding time,
INR, arteriogram, Lung scan if emboli?
Conservative tx:
bedrest with leg
elevated until
tenderness is reduced
about 5-7 days. Warm
moist heat (K-pad)
may be used to relievepain and inflammation
Dont massage legs
Pain control/anti-
inflammatory drugs
If edema- TED hose or
ace (elastic) wraps
Anti-coagulants like
Heparin Drip- IV-
(DVTs only) bleedingand safety precautions
-
7/28/2019 PVD K2
47/52
Cont. TX/Management
thrombophlebitis
Pharmacological Tx-
aimed to prevent clots,
dont dissolve them
(Heparin/Lovenox-SQ/Coumadin-po.)
Heparin/Lovenox-SQ-
lw. Abdomen 2 inchesaway umbilicus
Dont rub with alcohol
pad after shot, use 5/8
inch needle
SQ- no more than 1cc
ever injected into tissue
or one site, if more
needed use divideddoses.
-
7/28/2019 PVD K2
48/52
Cont. general guidelines
thrombophlebitis/DVTs
Measurement- of bothlegs/calves
Heparin/Coumadin
Coumadin is startedwhile on Heparin-IV;Monitor PT, (A)PTT,INR-
antidote coumadin is
Vit.K Heparin-Protamine
sulfate antidote
Avoid aspirin while on
anti-coagulants like
Heparin/Coumadin
Nurse recognize high riskpatients for
thrombophlebitis,
bedrest, age, dehydration,
oral contraceptives,steroids, IV drug use
-
7/28/2019 PVD K2
49/52
Continued:
thrombophlebitis/DVTs
If on
Heparin/Coumadin- s/s
bleeding gums, urine,
stool, any orifice,bruising, epistaxsis,
petehiae, no foley, no
rectal temp, no IM
injections
Always check lab
values PT- & INR for
Coumadin
(A)PTT & INR-
Heparin (IV)
5000 u Heparin SQ
considered low doseprophylaxsis/mainten
ance dosage
-
7/28/2019 PVD K2
50/52
Cont. DVT-thrombophlebitis
Elastic stocking (TED)
hose-properly
measured, fitted, and
evenly applied -stockings compress
superficial veins &
prevent venous stasis-
or pnuematic
alternating
compression boots
Prevent pressure under
the knee avoid
pillows/knee gatches
on bed)
No pressure on
popliteal space
Avoid OC withrecurrent
thrombophlebitis
rest/exercise/fluids
-
7/28/2019 PVD K2
51/52
More general guidelines
Avoid prolongsitting-pressure underknee
Elderly, heart dz,infection, dehydrationmost proned tothrombophlebitis
Avoid prolong sittingcar/airplane/bus ride
Or sitting in front of TV
long period of time
(Sedentary lifestyle)
Change positionsfrequently and exercise
legs at intervals is
necessary
Avoid standing longperiod of time too!
-
7/28/2019 PVD K2
52/52
Lab values for Coumadin/Heparin Coumadin/warfarin :
Check the PT (pro-thrombin time)
Want the PT about 1.5-
2.0 times control value(normal for adults=10-13sec)
INR you want a targetlevel for coumadin or
warfarin therapy between(2.0-3.0) for mostconditions like DVT, hipsurgery etc.
INR is more reliable test
PTT or APTT (partialthromboplastin time oractivated partialthromboplastin time)
Used in Heparin therapy& also INR too!
PTT control=60-70 sec;and APTT=20-35 sec.
Want 1.5-2.5 times
control value in secondsfor optimal anticoagulanttherapy
Most cases: INR level tobe within (2-3)