PULMONARY EMBOLISM DR. ASWINI KUMAR MOHAPATRA PROFESSOR AND HEAD PULMONARY MEDICINE

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
PULMONARY EMBOLISM-
Otherwise called Pulmonary Vascular Diseases / Venous Thromboembolism (VTE)
Venous thromboembolism encompasses deep venous thrombosis (DVT) and Pulmonary embolism (PE)
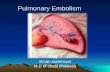
Pathophysiology
Venous thrombi dislodge from site of formation embolize to pulmonary arterial circulation and sometimes to arterial circulation through a patent foramen ovale or atrial septal defect
Physiology-
Most common gas exchange abnormalities are hypoxaemia (decreased arterial PO2) and an increased alveolar arterial O2 tension gradient
Other pathological abnormalities1. Increased pulmonary vascular resistance
2. Impaired gas exchange due to increased alveolar dead space from vascular obstruction
3. Alveolar hypoventilation due to reflex stimulation of irritant receptors
4. Increased airway resistance due to constriction of airways distal to bronchi
5. Decreased pulmonary compliance due to lung edema, lung hemorrhage or loss of surfactant
Clinical features –
VTE is difficult to diagnose It is fore most to find out the risk factors for VTE
Risk factors for VTE-
1. Surgery- Major abdominal surgery Post operative intensive care Hip/knee surgery
2. Obstretics- Pregnancy Puerperium
3. Lower limb problems- Fracture Varicose veins Stroke /spinal cord injury
4. Cardio-respiratory diseases- . COPD
. Congestive cardiac failure
5. Malignant diseases- Abdominal/pelvic Concurrent chemotherapy
6. Miscellaneous- Increasing age Previous proven VTE Immobility Trauma
Features of pulmonary thromboembolism : A. Acute massive PE :
I .Pathophysiology: Cardiac output acute right heart failure
II. Symptoms: faintness or collapse crushing central chest pain
Apprehension Severe dyspnoea
III. Signs: Tachycardia Hypotension JVP Rt. Ventricular gallop rhythm loud P2
Severe cyanosis Urinary output
IV. Chest X-ray:Usually normalmay be subtle oligaemic
V. ECG:S1 Q3 T3 anterior T-wave inversion
Rt. Bundle branch block (RBBB)VI. ABG:
PaO2 and PaCo2Metabolic acidosis
VII. D/D: Myocardial infarction
Pericardial tamponade Aortic dissection
B. Chronic PE:I. Pathophysiology:
Chronic occlusion of pulmonary microvasculature, Rt. Heart failure
II. Symptoms:
Exertional dyspnoea
III. Signs:
May be minimal early in disease
Later RV heave, loud P2
Termnal: signs of right heart failure
IV. Chest X-ray:
Enlarged pulmonary artery trunk
Enlarged heart
Prominent RV
V. ECG:
RV hypertrophy and strain
VI. ABG:
Exertional PaO2 or desaturation on formal exercise testing
2. ECG:
3. Arterial blood gases: Reduced PaO2
Normal or low PaCo2 and an increased alveolar-arterial oxygen gradient
4. D-dimer studies: D-dimer is a specific degradation product released into
the circulation when cross linked fibrin undergoes endogenous fibrinolysis
An elevated D-dimer is of limited value
D-dimer :
Myocardial infraction
Pneumonia
Sepsis along with pulmonary embolism
5. Imaging : CT pulmonary angiography (CTPA) is most commonly
used to diagnose PE
Ventilation Perfusion Scanning is less commonly used as its utility is limited in patients with pre-existing chronic cardiopulmonary pathology and the scan is most frequently regarded as indeterminate. Color Doppler ultrasound of the leg veins remains the investigation of choice in patients with suspected DVT
6. Echocardiography:
Extremely useful in differential diagnosis and assessment of acute circulatory collapse
RA, RV dilatation in massive PE and thrombus (embolism in transit) may be vissible.
MANAGEMENT
General measures:
Prompt recognition and treatment is life saving especially in cases of massive PE
Oxygen –all hypoxaemic patients to maintain Sao2 >90 %
Circulatory shock treated with IVF, plasma expanders.
Ionotropic agents are of limited value as the hypoxic dilated Rt. Ventricle is maximally stimulated by endogenous catecholamines
Diuretics and vasodilators should be avoided as they cause cardiac output
Opiates may be necessary to relieve pain and distress, but should be used with caution in hypotensive patients
Resuscitation by external cardiac massage may be successful in the moribund patients by dislodging and breaking up a large central embolus.
B. Anticoagulation: Commenced immediately if established
Heparin-
-reduces further propagation of clot - the risk of further emboli, - lowers the mortality
Low molecular weight heparin (LMWH) –
The duration of LMWH treatment should be at least 5 days, during which time oral warfarin is commenced. LMWH should not be discontinued until the INR is greater than 2
Patients with persistent prothrombotic risk factors require 3 months of therapy
C. Thrombolytic Therapy: Indicated in any patient presented with massive PE
accompanied by cardiogenic shock
Helpful in patients with Rt. Ventricular dilatation, hypokinesia or sever hypoxaemia
Selected patients –surgical pulmonary embolectomy
D. Caval filters : Inferior vena caval filters
Indications:
i. massive haemorrhage on anticoagulation therapy
ii. Recurrent VTE despite anticoagulation
Related Documents