RESEARCH REPORT RESEARCH TITLE ‘AN EVALUATION OF ANTIBIOTIC DOSING ACCORDING TO RENAL FUNCTION OF PATIENTS IN INTENSIVE CARE UNIT (ICU), HOSPITAL SULTANAH NUR ZAHIRAH, KUALA TERENGGANU’ Prepared by: Nurfatihah Nasiha Binti Bahagia Preesha A/P Nagalingam Preceptors: Erney Binti Mohd Shah

Provisional Registered Pharmacist research presentation 2013
Nov 30, 2014
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

RESEARCH REPORT
RESEARCH TITLE
‘AN EVALUATION OF ANTIBIOTIC DOSING ACCORDING TO RENAL FUNCTION OF
PATIENTS IN INTENSIVE CARE UNIT (ICU), HOSPITAL SULTANAH NUR ZAHIRAH,
KUALA TERENGGANU’
Prepared by:
Nurfatihah Nasiha Binti Bahagia
Preesha A/P Nagalingam
Preceptors:
Erney Binti Mohd Shah
Che Wan Mohd Hafidz
Pharmacy Department, Hospital SultanahNurZahirah, Kuala Terengganu, Terengganu

CONTENTS
1) Introduction…………………………………………………………………………….1
1.1 Definition……………………………………………………………………..........3
2) Problem Statement……………………………………………………………………..4
3) Literature Review…………………………………………………………………........5
4) Objectives…………………………………………………………………………........7
4.1 General………………………………………………………………………………
4.2 Specific………………………………………………………………………………
5) Methodology……………………………………………………………………….........9
6) Results and discussion………………………………………………………………...10
7) Conclusion……………………………………………………………………………..18
8) Limitation………………………………………………………………………………19
9) References……………………………………………………………………………..20

1) Introduction
Patients who are admitted in Intensive Care Unit (ICU) include representative of all
age groups with a range of organ dysfunction related to severe acute illness, which may
complicate long term illness[1]. Twenty-two to thirty-two percent of ICU patients die from
infections caused by gram-negative pathogens, despite appropriate antimicrobial therapy.
These patients are at very high risk of developing severe nocosomial infections, with
incidence rates five to ten fold higher than in general medical wards [2-5]. Serious infections
and sepsis whether community or hospital acquired are common in critically ill patients and
require rapid treatment to limit mortality and morbidity [1]. Antibiotics are among the most
important and commonly prescribed drugs in the management of critically ill patients[6].
ICU patients are frequently affected by acute kidney injury (AKI) accompanied by
dysfunction of other systems and organs while other cases are further complicated by a
secondary infection. Continuous renal replacement therapy (CRRT) is frequently used to treat
critically ill patients with acute or chronic renal failure. Since the prognosis in these patients
are very poor due to severe infection and the mortality rate reaching from 80% to 90%,
selecting appropriate antibiotic regimen is crucial for the clinical outcome. Choice of
antibiotic used for empirical treatment of bacterial infections in the intensive care unit (ICU)
is based predominantly on the identity and susceptibility pattern of bacteria isolated.
Administering sub-therapeutic doses of antibiotics may lead to a decreased efficiency of
therapy and development of resistant bacterial strains. On the other hand, high doses can be
harmful to vital organs such as the kidneys, bone marrow and liver, resulting in a significantly
worse prognosis [7].
Dosage adjustment of antibiotics to renal function is recommended for many
antibiotics especially those that are eliminated by the kidney.Changes in renal function,
whether associated with normal aging or disease, can have profound effects on the
pharmacology of antibiotics since kidney is the major organ for maintaining fluid and
electrolyte homeostasis. Renal function should always be taken into account because majority
of drugs are excreted by the kidney[8,9]. Therefore, an estimation of their kidney function is
crucial for appropriate drug dosing.

When selecting potential candidate of renal dose regimens, the first consideration is
the creatinine clearance (CrCl).Patients with kidney disease, antibiotic dose adjustment are
commonly made to maintenance dose, or the dosing interval based on pharmacodynamics
effects of the drug. The most important information used for the prescribing of these
antibiotics includes dose recommendation based on Cockroch-Gault estimate creatinine
clearance (CrCl). Estimation of creatinine clearance is the most practical approach for
assessing kidney function while CockrochGault equation remains the most appropriate
method to determine drug dosage individualisation based on kidney function in clinical
setting[10]. Since most drugs require dosing adjustment at a creatinine clearance of
<50mL/min, therefore, the antibiotic dosing being prescribed for these patients need to be
monitored frequently[1, 11].Identification of optimal dosage adjustments among patients with
compromised renal function requires careful consideration of the relationships between
antibiotic exposure, efficacy, toxicity and the potential for antibiotic resistance [12].
However, several factors may contribute to the increasing difficulties in
establishing proper dosing regimen in critically ill patients [8]. Pathophysiological alterations
associated with critical illness can lead to both an increase in the apparent volume of
distribution (Vd) of an antibiotic as well as in clearance, thus, potentially leading to sub-
therapeutic plasma concentrations at the site of infection, treatment failure and the
development of antibiotic resistance. Volume of distribution (Vd) and drug clearance (Cl)
may be increased in ICU patients contributing to the altered concentration-time relationship of
many drugs. When drug concentration is reduced, it might proportionally increase the half-
life. The development of renal and/or hepatic impairment may be associated with the rapid
onset of toxic drug concentrations. Therefore, antibiotic dose should be reviewed daily in the
ICU and dosage adjustment is necessary to prevent accumulation and toxicity based on
patient’s condition[13].
In this small study, our primary aim is focused on assessing antibiotics dosing
being adjusted appropriately in patient with kidney disease according torecommended
guideline as well as to study the outcomes of dosage adjustment of antibiotics in critically ill
patients.

1.1 Definition
a) Renal impairment
1) Mild to severe
All categories of renal function other than the baseline category, which corresponded to creatinine >1.0 mg/dl, creatinine clearance (CrCl) or GFR <90 ml/min.[14]
2) Moderate to severe
Worst category of renal function which corresponded to creatinine ≥1.5 mg/dl, CrCl or GFR <53 ml/min[14]
Stages [15] CrCl (ml/min)
Stage 1 - Kidney damage with normal or GFR >90
Stage 2 - Kidney damage with mild or GFR 60-89
Stage 3 – Moderate GFR 30-59
Stage 4 – Severe GFR 15-29
Stage 5 – Kidney failure <15
b) Renal condition
1) Acute renal failure (ARF) :
Sudden loss of the ability of the kidneys to excrete wastes, concentrate urine, conserve electrolytes, and maintain fluid balance. [16]
2) Chronic kidney disease (CKD):
Kidney damage or GFR <60ml/minute for 3 months or more, irrespective of cause.[17]
3) Acute-on-chronic renal failure :
Acute renal failure (ARF) occurs in the background of pre-existing chronic kidney disease. [18]

2) Problem Statement
1) Patients with acute or chronic renal failure treated in ICU require adjustment of antibiotic
dose based on the patient’s renal function. If the dosage of antibiotic regimen given to
these patients is not well adjusted, it can lead to accumulation and toxicity of the drugs
with leads to increase in morbidity and mortality rates[19].
2) In some critically-ill patients who are suffering with renal impairment, they are given large
dose of antibiotics to fight the bacterial infections as their major priority, rather than
adjusting the dosage according to the patient’s renal function and creatinine clearance
(CrCl) [20].
3) Dose adjustment of antibiotics according to renal function is crucial as it largely
contributes to the clinical outcomes of patients[13].

3) Literature Review
From the previous study of Fahimi et al, findings show that two hundreds and ninety-
one instructions (79.9%) of 364 antibiotic prescriptions required dosage adjustment based on
the patient’s renal condition. These adjustments were rationally performed in 43.7% and
61.4% of prescriptions, according to the two guidelines used. Ciprofloxacin (29.1% of
cases) and Vancomycin (33.6% of cases), were the most inappropriate prescribed antibiotics
in terms of dose administration. The results demonstrate a significant need to develop a
unanimous drug dosing system for patients with renal dysfunction. As conclusion from the
study, finding a reliable and easily applied dosing guideline is highly recommended since
lack of uniformity exists among dosing recommendations of commonly used drug
information handbooks. The results of their study may not be extrapolated to other clinical
settings, since they represent a unique situation. Therefore, further research is still required
to reveal the clinical importance of drug dosage adjustment in renal failure patients. [21]
Review by Eyler R. F and Mueller B. A, found that appropriate dosing of antibiotics in
these patients is essential since the common cause of acute kidney injury (AKI) is sepsis.
Drug dosing in critically ill patients with AKI, however, can be complicated. Critical illness
and AKI can both substantially alter pharmacokinetic parameters as compared with healthy
individuals or patients with end-stage renal disease. Furthermore, drug pharmacokinetic
parameters are highly variable within the critically ill population. In addition, volume of
distribution (Vd) of hydrophilic agents can increase as a result of fluid overload and
decreased binding of the drug to serum proteins, and antibiotic loading doses must be
adjusted upwards to account for these changes. Although renal elimination of drugs is
decreased in patients with AKI, residual renal function in conjunction with renal
replacement therapies (RRTs) result in enhanced drug clearance, and maintenance doses
must reflect this situation. Antibiotic dosing decisions should be individualized to take into
account patient-related, RRT-related, and drug-related factors. Efforts must also be made to
optimize the attainment of antibiotic pharmacodynamic goals in this population. [22]
According to the study done by Cathrine McKenzie on 2011, her finding shows that
antibiotics factor and patient factors affect antibiotic dosing. Early and effective antibiotic
therapy is essential in the management of infection in critical illness. The loading dose is
probably the most important dose and is a function of the volume of distribution of the drug

and the desired plasma concentration but independent of renal function. Doses of
hydrophilic agents such as b-lactams should be increased in the early stages of sepsis as the
extravascular space increases while lipophilic agents such as macrolides, the inflammatory
process is less important, although factors such as obesity will affect dosing. Concentration-
dependent antibiotics such as aminoglycosides should be administered by extended interval
regimens, which maximize bactericidal effect, minimize nephrotoxicity and allow time
between doses for the post-antibiotic effect. The critical factor for time-dependent agents,
such as b-lactams, is time above the MIC. Ideally administration of these agents should be
continuous, although vascular access availability can restrict infusion time to between 4 and
6 h, which is probably adequate. Besides, patient factors such as hepatic and renal failure
also will affect dosing. Hepatic failure will affect antibiotic metabolism, although it is most
important in end-stage failure. Renal failure and support will affect drug elimination.
According to the authors, knowledge of these factors is essential. Patient safety and
prevention of unnecessary harm is a weighty consideration in critical illness. Therapy should
be reviewed daily and adjusted in the light of changes in patient organ function and
underlying pathology to ensure effective treatment and minimize adverse effects. [23]

4) Objectives
General
To evaluatethe antibiotic doseadjustment according to renal function of patient of intensive
care unit (ICU), Hospital SultanahNurZahirah(HSNZ), Kuala Terengganu.
Specific
1. To determine the percentage of prescribed antibiotics being appropriately adjusted
according to recommended guideline.
2. To compare the clinical outcomes of critically ill patient receiving antibiotic
requiring dose adjustment in ICU based on its adherence.

5) Methodology
Study design and location
- A cross-sectional study, conducted retrospectively.
Sample population
- All patients aged 12 years and above in intensive care unit, ICU, Hospital
SultanahNurZahirah, Kuala Terengganu.
- Patients were recruited by using inclusion and exclusion criteria.
Inclusion criteria Exclusion criteria
All renal impaired patients. 1) Patient on continuous renal replacement therapy (CRRT).
2) Patient admitted during weekend and was transferred out/passed away during the same weekend.
3) Patient that has incomplete data
-
Data collection
1. Clerked CP2 sheet of each patient in ICU starting from July to December 2012
(6months) were used to review patient information.
2. HIS system to collect extra information such as progress note of the patient and
laboratory parameters during their admission in ICU.
3. All the data that were collected using Microsoft Excel 2007.
Data analysis
- The data collected wereanalyzed using the SPSS® (Statistical Package for the Social
Sciences) software program for Windows® Version (20.0).
- For all tests, a p value of < 0.05 will be defined as statistically significant.

5) Methodology
Guideline
1. The Malaysian Society of Anaesthesiology (MSA) Guide to Antimicrobial Therapy in
Adult ICU, September 2006.
2. Antibiotic product pamphlet was used for evaluation of Piperacillin + Tazobactam
(Tazosin) and Amoxycillin + Clavulanic Acid (Augmentin) doses.
The MSA Guide to Antimicrobial Therapy in Adult ICU, September 2006were used for all
antibiotic that need dose adjustment except Tazosin and Augmentin. Product pamphlets were
used forTazosinsince we use the product from the company itself and there is no dose
adjustment in recommended guideline for IV Augmentin.
Adherence to guideline
Dose of antibiotic prescribed in accordance to recommended dose based on CrCl of
patients as stated in the guideline.
Outcome [24]
Systemic Inflammatory Response System (SIRS) were used to evaluate the samples after
receiving antibiotic regimen.
SIRS : Two or more of the following indicates no improvement :
1) Temperature >38°C or <36° C2) Heart rate > 90 b/min, 3) Respiratory rate > 20 b/min, or PaCO2 <32mmHg4) White blood count >12000/mm3 or <4000/mm3 or >10% band
form

6) Result and Discussion
Demographic data
Frequency, n Percent
Male 72 63.7
Female 41 36.3
Total 113 100.0
Table 1: Gender
From our study, 63.7% from total sample consists of male, n = 72 and 36.3%
constitute female patient, n = 41.
Type of antibiotic treatment
Table 2: Type of antibiotic treatment
About 68.1 % of total samples, n= 77 treated with antibiotic as empirical and the rest
of them treated as definitive.
Frequency, n Percent
Empirical 77 68.1
Definitive 36 31.9
Total 113 100.0

Samples according to different stages of Creatinine Clearance (CrCl) and renal condition.
Stage 2 (60-89)
Stage 3 (30-59)
Stage 4 (15-29)
Stage 5 (0-14)
010203040
2
24 28
100
87
16
0
7 38
Stages of Creatinine Clearance According to KDOQi Clin-ical Practice Guidelines, 2013 [15]
Acute on Chronic
Chronic
Acute
Stages of Creatinine Clearance (CrCl)
Num
ber
of S
ampl
es
Chart 6.1 : Samples according to different stages of Creatinine Clearance (CrCl) and renal
condition.
Chart 6.1 shows the number of samples according to different stages of creatinine
clearance and renal condition. The stages of creatinine clearance is according to KDOQi
clinical practice guideline,2013[15].
From the chart, 2 out of 2 samples in stage 2 creatinine clearance contributed to acute
kidney disease, whereas, in stage 3, 24 samples are acute, 8 and 7 samples are chronic and
acute on chronic respectively. For stage 4, 28 samples are acute, 7 chronic and 3 acute on
chronic. Lastly, stage 5, 16 samples are chronic, followed by 10 samples acute and 8 samples
acute on chronic. The chart showed that majority of samples contributed to acute kidney
disease and having stage 4 creatinine clearance which consisted of 28 samples.

Percentage of Antibiotics Adherence to Guideline
89.4% n=101
10.6% n=12
High doses
Adherence of Antibiotics to Guideline
Yes No
Total sam-ple,
n = 113
Chart 6.2 : Percentage of Antibiotics Adherence to Guideline
Chart 6.2 shows the percentage of antibiotics adherence to recommended guideline.
From the pie chart, 89.4 % constituting of 101 out of 113 samples adhere to recommended
guideline whereas 10.6% constituting 12 out of 113 samples did not adhere to recommended
guideline whereby they were prescribed with high doses of antibiotics despite renal function
and creatinine clearance stages.

Frequency of antibiotics prescribed and its adherence to recommended guideline
Ampicillin
+ Su
lbactam
Amoxycill
in + Clav
ulanic A
cid
Cefepim
e
Cefotax
ime
Ceftazi
dime
Cefuro
xime
Ciprofloxa
cin
Imipen
em +
Cilasta
tin
Meropen
em
Metronidazo
le
Piperacili
n + Ta
zobact
am
Trimeto
prim +
Sulphometh
oxa...
Vanco
mycin
Polymyx
in E0
5
10
15
20
25
30
58
2 2
105 5 3
1713
24
3 2 2
14
3
3
1
NoYes
Types of antibiotics
Num
ber o
f sam
ples
Chart 6.3: Frequency of antibiotics prescribed and its adherence to recommended guideline
Chart 6.3 shows the frequency of different types of antibiotics prescribed. Based on our
result, 12 samples did not adhere to guideline consisting of 5 types of antibiotics that include
Ampicillin + Sulbactam (Unasyn), Ciprofloxacin, Imipenem + Cilastation (Tienem),
Meropenem and Metronidazole. Many previous studies suggested that dose of those
antibiotics should be higher than recommended guideline. From our result, it was found that
dose of Ciprofloxacin were prescribed with a high dose of 400mg BD comparing to the
recommended 200mg BD as stated in recommended guideline based on creatinine clearance.
From the study of Zanteen et al (2008), IV Ciprofloxacin 400 mg BD leads to adequate
AUC/MIC and Cmax/MIC ratios in many cases. Effective killing concentrations were only
achieved in pathogens with MIC less than 0.25. As bacteria in intensive care unit patients
often exceed this threshold, it is recommended to use higher doses of ciprofloxacin (1200 mg
daily) to ensure optimal bacterial killing and avoid antibiotic resistance[25].
Besides that, meropenem is another antibiotic that did not adhere to recommended
guideline consisting of 3 samples that did not adhere. Study by Eggiman, P and Pittet, D

found that there is potential inadequacies noted for standard doses of
meropenemwhich may be further compounded in the intensive care unit
(ICU) as they typically harbor the most resistantpathogens within a given
population[26].
Furthermore, another study found that the pharmacokinetics of the
critically ill may differ from non-critically ill patients, often resulting in a
reduction in exposure of meropenem [27].
For these reasons, higher empiric doses may be required to adequately
achieve pharmacodynamic targets against pathogens encountered within
the ICU[28].
This study also found that there is only 1 from 6 samples of Ampicillin + Sulbactam
(Unasyn) that did not adhere to guideline, which administered 1.5 g TDS instead of 3g OD as
stated in recommended guideline. Study from Adnan, S et al. suggested that for optimization
of therapy higher dose for treatment of infection is recommended since alteration of
pharmacokinetics are common inβ-lactam agents in critical illness[29].
The need of higher dosage of antibiotics in critically ill patients was
supported by few studies. According to Nathwani D and Davey P, they
suggest that the highest dose in the range should be given in severe
sepsis since low doses may not only be ineffective but have been shown to
contribute to resistance [30]. Another study by Federico P and Pierluigi conclude that
selecting higher dosage and alternative dosing regimens focused at maximizing the
pharmacodynamics of antimicrobials might be worthwhile, in order to increase clinical cure
rates among critically ill patients.[31]

Outcomes of samples
SIRS parameters were used to evaluate the outcome of this study whereby the mean of each
parameter were calculated before and after the initiation of antibiotics and the respective
means were compared to evaluate the outcome.
(a) Improvement of outcomes based on SIRS parameters
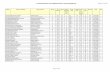
(T = temperature, WBC = White Blood Cells, RR= Respiratory rate, HR= Heart Rate)
Type of antibiotics
Sample, n
Mean T
Mean T
Mean WBC
Mean WBC
Mean RR
Mean RR
MeanHR
Mean HR
Before After Before
After Before After Before After
Cefepime 2 38.1 37.5 7.6 8.7 16.5 18.2 81.2 83.4
Cefotaxime 2 39.6 36.7 8.9 6.9 21.4 17.0 85.6 76.5
Vancomycin 2 36.7 36.4 13.3 8.5 20.3 18.4 78.4 68.7
Polymyxin E 2 37.9 36.9 8.3 9.6 18.1 17.6 84.5 79.6
Amoxycillin + Clavulanic Acid (Augmentin)
5 (8) 38.6 37.8 11.0 14.6 18.9 17.6 80.5 77.0
Ceftazidime 7 (10) 37.8 36.8 8.4 7.5 18.3 16.7 89.3 87.5
Piperacillin + Tazobactam (Tazosin)
18 (24) 37.3 37.8 9.5 8.3 18.5 16.0 90.4 88.3
Table 6.1 :Antibiotics that 100 % adhere to guideline
Table 6.3 shows the antibiotics which 100% adhere to guideline and showed improvement
based on SIRS parameters which includes Cefepime, Cefotaxime, Vancomycin, Polymyxin E,
Amoxycillin + Clavulanic Acid, Ceftazidime and Piperacillin + Tazobactam. As for
Cefepime, Cefotaxime, Vancomycin and Polymyxin E, 2 out of 2 samples adhere to guideline
and showed improvement contributing to 100% adherence and 100% positive outcome. The

rest of the antibiotics, Amoxycillin + Clavulanic Acid, Ceftazidime and Piperacillin +
Tazobactam 100 % adhere to guideline but did not 100% show positive outcome whereby
only 5 out of 8 for Amoxycillin + Clavulanic Acid, 7 out of 10 for Ceftazidime and 18 out of
24 for Piperacillin + Tazobactam showed improvement based on SIRS parameters.
Table 6.2 :Antibiotics that did not 100% adhere to guideline
Table 6.2 focused on the antibiotics that did not 100% adhere to guideline but however
showed improvement based on SIRS parameters. From the table, 5 out of 9 samples of
Ciprofloxacin showed improvement, 4 out of 5 samples adhere to guideline whereas 1 sample
did not adhere to guideline and yet showed improvement. As for Imipenem + Cilastatin, 2 out
of 6 samples showed improvement, 2 out 6 samples showed improvement whereby both the
samples adhere to guideline. Next, Meropenem, 17 out of 20 samples showed improvement
whereby 14 samples adhere to guideline and 3 samples did not adhere to guideline. As for
Ampicillin + Sulbactam, 4 out of 6 samples showed improvement, 3 samples adhere to
guideline and 1 sample did not adhere to guideline. Lastly, Metronidazole consist of 5 out 14
samples that showed improvement based on SIRS parameters and all 5 adhere to
recommended guideline.
Type of antibiotics
Sample, n Mean T
Mean T
Mean WBC
Mean
WBC
MeanRR
Mean RR
Mean HR
Mean HR
Before After Before After Before After Before After
Ciprofloxacin 5 (9)
4 37.9 37.3 13.5 10.3 18.8 19.1 92.9 86.0
1 38.1 36.7 14.6 12.5 23.6 18.9 87.3 86.5
Imipenem + Cilastatin (Tienem)
2(6)
2 37.7 37.8 11.4 9.0 19.5 17.6 88.4 77.0
Meropenem 17(20)
14 37.4 38.1 8.9 11.7 18.4 18.9 98.7 89.9
3 38.7 36.4 11.3 13.9 20.2 18.7 89.7 85.3
Ampicillin + Sulbactam (Unasyn)
4 (6)
3 38.1 37.3 9.0 10.3 23.4 19.1 94.4 91.3
1 37.5 37.1 13.7 10.4 19.3 22.4 94.5 89.1
Metronidazole
5 (14)
5 38.4 37.4 8.2 7.9 25.4 17.2 82.7 86.7

b) Adherence of antibiotics towards guidelines and patient outcomes
Table 6.3: Adherence of antibiotics towards guidelines and patient outcomes
Table 6.4: Pearson Chi-Square test: Association of antibiotics adherence towards guidelines and
patient outcomes
Data was analysed using SPSS version 20 and p value less than 0.05 indicate
significant. From table 6.3 and 6.4, statistical analysis using Chi-Square test found that there
was no significant between adherence of antibiotics towards guidelines and patient outcomes
(p = 0.53) in this study.

7) Conclusion
- Almost 90 % samples adhere to guideline MSA Guide to Antimicrobial Therapy in
Adult ICU, September 2006 and product pamphlet.
- Although high percentage of improvement seen in adhere group compare to non-
adhere group, there was no significant between adherence of antibiotics towards
guidelines.
- Therefore, we recommend to adjust dose in order to save renal function whereby
dosing of antibiotic in critically ill patients should be individualized and not solely
based on creatinine clearance or renal function.

8) Limitation
- Clinical improvement of patient cannot be evaluated solely based on septic parameters
instead prospective study should be proposed to evaluate the outcomes of this study.

9) References
1. Scaglione, F. and Luca, P. (2008). Pharmacodynamics/Pharmacokinetics of Antibacterials
in ICU, 294-301.
2. Vincent, J. L., Bihari, D. J., Suter, P.M., Bruning, H. A., White, J., Nicolas- Chanoin, M.
H., et al. (1995). The prevalence of nosocomial infection in intensive care units in Europe.
Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC
International Advisory Committee. JAMA, 274:639–44.
3. Weber, D.J., Raasch, R., Rutala, W.A. (1999). Nosocomial infections in the ICU: the
growing importance of antibiotic-resistant pathogens, 115,34S–41S
4. Vincent, J. L. (2003). Nosocomial infections in adult intensive-care units. Lancet, 361,
2068–77.
5. Paterson, D. L. (2003). Restrictive antibiotic policies are appropriate in intensive care
units. Critical Care Medicine, 31, S25–8.
6. Joao, G.P. and Pedro, P. (2011). Antibiotics in critically ill patients : A systematic view of
pharmacokinetics of β-Lactams.
7. Joanna, M., Rowińska, Jolanta, M., Ewa, W., Paweł, K. (2011). Dosing of antibiotics in
critically ill patients: are we left to wander in the dark? Journal Antimicrobial
Chemotherapy.
8. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney
disease: evaluation, classification, and stratification. (2002). American Journal Kidney of
Disease,39, S1–266.
9. Bonapace, C.R., White, R. L., Frich, L. V. et al. (2002). Differences in antimicrobial drug
exposure in patients with various degrees of renal function based on recommendations
from dosing references. Pharmacotherapy, 22, 1097–104.
10. Cockcroft, D. W., Gault, M. H.(1976). Prediction of creatinine clearance from serum
creatinine. Nephrology, 16, 31–41.

11. Van, D. E. et al. (2006) Drug dosage adjustments according to renal function at hospital
discharge. Annals Pharmacotherapy, 40, 7-8, 1254-60.
12. Nimish, P. et al. Determination of antibiotic dosage adjustments in patients with renal
impairment: elements for success.
13. Jason, A. R., Jeffrey, L. (2009). Critical Care Medicine,.Pharmacokinetic issues for
antibiotics in the critically ill patient.
14. Grace L. Smith et al. Renal Impairment and Outcomes in Heart Failure Systematic Review
and Meta-Analysis.
15. KDOQi Clinical Practice Guidelines(2013)
16. Robert W. Et al. Acute renal failure: definitions, diagnosis, pathogenesis, and therapy,
2004
17. S.W Andrew et al. Definition and classification of chronic kidney disease: A position
statement from Kidney Disease: Improving Global Outcomes (KDIGO)
18. Andrew S.L et al. Definition and classification of chronic kidney disease; A position
statement from KDIGO,Kidney International, 2005.
19. Swan, S. K. and Bennett, W. M. (1992). Drug dosing in patients with renal failure.
Western Journal Medicine, 156, 633-8.
20. Moore, R., Lietman, P., Smith, C. (1987). Clinical response to Aminoglycoside therapy:
importance of the ratio of peak concentration to minimal inhibitory concentration. Journal
Infectious Disease, 155, 93–9.
21. Fahimi et al. The Rate of Antibiotic Dosage Adjustment in Renal Dysfunction, Iranian
Journal of Pharmaceutical Research (2012)
22. Eyler, R. F., and Mueller, B. A. Nature Review of Nephrology, April 2011
23. Cathrine McKenzie. Antibiotic dosing in critical illnes, Journal of Antimicrobial
Chemotherapy, 2011.
24. N.D Madala, Acute renal failure in patients with chronic kidney disease, American College
of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM)
25. Zanteen et al. (2008). Ciprofloxacin pharmacokinetics in critically ill patients: A
Prospective cohort study, Journal of Critical Care, 23, 422-430
26. Eggimann,P. andPittet, D. (2001).Journal of Infection control in ICU.
Chest Journal, 120, 2059–2093
27. Roberts J.A. and Lipman, J. (2009) Pharmacokinetic issues for antibiotics
in the critically ill patient. Critical Care Medicine, 37, 840–851.

28. Jared L et al. (2010). Optimization of meropenem dosage in the critically
ill population based on renal function, Intensive Care Medicine.
29. Adnan S et al. (2013) Ampicillin/sulbactam: Its potential use in treating infections in
critically ill patients. Journal International Antimicrobial Agents.
30. Nathwani D, Davey P. Antibiotic prescribing—are therelessons for
physicians? QJM 1999;92(5):287–92.
31. Federico, P and Pierluigi, V. Review Bench-to-bedside review: Appropriate antibiotic
therapy insevere sepsis and septic shock - does the dose matter?
Related Documents











![Document1 - Emergency Medicine PNG · C] New Registration for License to Practice Provisional License to practice Temporary License Fees Waiver Pharmaceutical Board Pharmacist Pharmacy](https://static.cupdf.com/doc/110x72/5f08fd527e708231d424b2ea/document1-emergency-medicine-c-new-registration-for-license-to-practice-provisional.jpg)