Dr/ ABD ALLAH NAZEER. MD. Radiological imaging of pulmonary embolism.

Presentation1.pptx, radiological imaging of pulmonary embolism.
Jul 15, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Pulmonary embolism (PE) is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream (embolism). PE most commonly results from deep vein thrombosis (a blood clot in the deep veins of the legs or pelvis) that breaks off and migrates to the lung, a process termed venous thromboembolism (VTE). A small proportion of cases are caused by the embolization of air, fat, or talc in drugs of intravenous drug abusers or amniotic fluid. The obstruction of the blood flow through the lungs and the resultant pressure on the right ventricle of the heart lead to the symptoms and signs of PE. The risk of PE is increased in various situations, such as cancer or prolonged bed rest.
Most Common Symptoms of PE (PIOPED Study) Dyspnea (73%)
Pleuritic chest pain (66%)Coughing (37%)Hemoptysis (13%) Atypical Presentations of PE Abdominal/pelvic pain
Decreasing level of consciousnessFeverProductive coughSeizuresSyncopeWheezing
Common Risk Factors for DVT and PEAIDSAntithrombin III deficiencyBechet diseaseBlood type ABurnsIndwelling venous catheters, PacemakerChemotherapyCHF, myocardial infarct History of prior DVTOral contraceptives, Estrogen replacementFractures, SurgeryMalignancyObesityProlong bed restPregnancyProtein C deficiency, resistance to active protein CSystemic lupus erythematosus (SLE)TraumaVaricose veins, venous stasis, venography
The Most Common Risk Factors for DVT and PE Venous stasis - a condition of stoppage or reduced blood flow through the veins. Prolonged immobilization - this situation occurs when one is put in a cast to heal a fracture, or suffers paralysis of a limb, or is bedridden due to illness or being elderly. Trauma and surgery - these conditions carry an increased risk of developing VTE and PE. When there are major multisystem injuries, such as a high impact motor vehicle accident, the incidence rate for DVT is approximately 58%. Oral Contraception - has been known for many years to be a contributor to PE. Oral contraceptive use combined with cigarette smoking is well documented as a cause of sudden death in healthy women. Pregnancy - In some women venous stasis can be a complication of pregnancy. The cause is contributed to a decrease in fibrinolytic function. Congenital - In a small fraction of the general population there are those who suffer chronic hypercoagulable blood condition. Often this is a congenitally caused hypercoagulation because of mutated Factor V. Mutated Factor V is the most common cause of congenital hypercoagulation and is seen in some form in about 5% of the population. Acquired deficiencies are seen in protein C, protein S and Antithrombin III. Acquired deficiencies occur in nearly 10% of young people who are diagnosed with PE.
Radiological Imaging:Chest X-rayThis noninvasive test shows images of your heart and lungs on film. Although X-rays can't diagnose pulmonary embolism and may even appear normal when pulmonary embolism exists, they can rule out conditions that mimic the disease.UltrasoundA noninvasive "sonar" test known as duplex ultrasonography (sometimes called duplex scan or compression ultrasonography) uses high-frequency sound waves to check for blood clots in your thigh veins. In this test, your doctor uses a wand-shaped device called a transducer to direct the sound waves to the veins being tested. These waves are then reflected back to the transducer and translated into a moving image by a computer. The absence of the presence of clots reduces the likelihood of DVT. If clots are present, treatment likely will be started immediately.CT scanRegular CT scans take X-rays from many different angles and then combine them to form images showing 2-D "slices" of your internal structures. In a spiral (helical) CT scan, the scanner rotates around your body in a spiral — like the stripe on a candy cane — to create 3-D images. This type of CT can detect abnormalities in the arteries in your lungs with much greater precision, and it's also much faster than are conventional CT scans. In some cases, contrast material is given intravenously during the CT scan to outline the pulmonary arteries.
V/Q lung scanThis test uses small amounts of radioactive material to study airflow (ventilation) and blood flow (perfusion) in your lungs. For the first part of the test, you inhale a small amount of radioactive material while a camera that's able to detect radioactive substances takes pictures of the movement of air in your lungs. Then a small amount of radioactive material is injected into a vein in your arm, and pictures are taken as the blood flows into the blood vessels of your lungs. Comparing the results of the two studies helps provide a diagnosis.
Pulmonary angiogramThis test provides a clear picture of the blood flow in the arteries of your lungs. It's the most accurate way to diagnose pulmonary embolism, but because it requires a high degree of skill to administer and carries potentially serious risks, it's usually performed when other tests fail to provide a definitive diagnosis.In a pulmonary angiogram, a flexible tube (catheter) is inserted into a large vein — usually in your groin — and threaded through your heart into the pulmonary arteries. A special dye is then injected into the catheter, and X-rays are taken as the dye travels along the arteries in your lungs.A risk of this procedure is a temporary change in your heart rhythm. In addition, the dye may cause kidney damage in people with decreased kidney function.
MRIMRI scans use radio waves and a powerful magnetic field to produce detailed images of internal structures. Because MRI is expensive, it's usually reserved for pregnant women and people whose kidneys may be harmed by dyes used in other tests
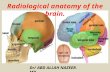
Types of pulmonary embolism.
Thrombotic pulmonary embolism.
Acute pulmonary embolism.
Chronic pulmonary embolism.
Non-thrombotic pulmonary embolism.
Pathology.
Hi Sensitivity D-Dimer.• High negative predictive value for PE (based
on pulmonary angiography) • For D-dimer <500ng/mL, negative predictive
value (NPV) 91-99%• For D-dimer >500ng/mL, sens=93%,
spec=25%, and positive predictive value (PPV) = 30%
• PPV and NPV are affected by prevalence.• Test is also useful for DVT rule out
(<500ng/mL): NPV 92% • If pretest probability is intermediate (27.8)
you are supposed to image, but if you order a D-Dimer what do the results mean?
D-Dimer• False Positive D-Dimer
–Pregnancy
– Trauma
–Postoperative Recovery
– Inflammation
–Cancer
–Rheumatoid Factor
–Older Age
• False Negative D-Dimer
–Heparin
Massive filling defects over bilateral pulmonary arteries and almost total obliteration of right pulmonary arterial flow (arrows).
Bilateral severe emboli can be shown in coronal MIP as well.
These two CT images show a large pulmonary embolus in the left main branch of the pulmonary artery. On the left is a lateral view of the artery and on the right is the anterior view of the same artery.
Coronal CT images show large occluding pulmonary emboli in branches of the left pulmonary artery and distal peripheral branches (orange arrows).
Two coronal CT images are of the same patient who presented with dyspnea, chest pain, and mild core pulmonale. The chest CT angiogram reveals multiple PE (arrows) as was suspected by clinical observations. Pulmonary emboli were found in several secondary, tertiary, and distal branches of the pulmonary arteries.
The axial CT image (left) shows large pulmonary emboli bilaterally. The pulmonary arteries from this image are magnified on the right to show these emboli better (yellow arrows)
These two axial CT images show profound pulmonary emboli. On the left the embolus almost completely blocks the right pulmonary artery (yellow arrow). Right image show an extensive saddle embolus forming in both pulmonary arteries and becoming extensive. Both of these types of pulmonary emboli are life threatening and require immediate medical attention.
This coronal image shows a large pulmonary embolus in a branch of the left pulmonary artery and scattered emboli in both lung fields. A magnified view of the chest is seen on the right with arrows pointing to several pulmonary emboli.
Sagittal images are not routinely made for the chest CTA; however, it is shown here (right) to show the extensive distribution of the pulmonary embolus seen on the coronal image (left).
Sagittal CT image shows small subsegmental branches of the pulmonary artery. Radiocontrast outlines pulmonary emboli in some of these small branches (yellow arrows).
Multiple filling defects both at the bifurcation ("saddle" pulmonary embolism) and in the pulmonary arteries.
(a) CT angiography shows thromboembolic material in both lower lobe pulmonary arteries (arrows). (b) High spatial resolution MR angiography demonstrates the same findings (arrows).
Chronic Pulmonary embolism and Pulmonary Hypertension. Eccentric wall-adherent thrombus in principal pulmonary arteries, and bending of the interventricular septum
• High probability scans identify only ~50% of patients with PE overall • Abnormal (high + intermediate + low prob) scans detect 98% of PE's, but
low specificity • About 60% of V/Q scans will be in determinant (intermediate + low
probability) • Of intermediate probability scans, ~33% occur with angiographically
proven PE • Test results not affected by presence of pre-existing cardiac or pulmonary
disease • Conclude: normal test rules out PE in ~98% of cases • Note that low probability test still has ~15-25% chance of PE • However, there were no deaths due to PE within 6 months in a study of
536 patients with low probability scans • Further evaluation is clearly required for intermediate probability scans • For low probability scan with normal D-dimer level, no additional workup
needed • Consider helical CT in patients with non-diagnostic V/Q scan. • NPV of helical CT with non-diagnostic V/Q is 96%.
Ventilation-Perfusion (V/Q) Scans.
Lower Extremity Doppler US.
• To evaluate for DVT as possible cause of PE or to help rule in PE
• Up to 40% of patients with DVT without PE symptoms will HAVE a PE by angiography
• Serial US should be probably be performed in patients with abnormal (or non-diagnostic) V/Q scans and positive D-Dimers.
• These US should be carried out on days 1, 3, 7, and 14.
• A positive US on any of these days with abnormal V/Q rules IN a PE.
• Negative serial US scans reduce likelihood of PE to <2%.
A subtotal occlusive thrombus in the right popliteal vein is shown in this colour Doppler image.
Right lower extremity (A) transverse and (B) sagittal images from color Doppler ultrasound demonstrates blood flow in the femoral artery but not in the common femoral vein (arrows). This is an indirect finding that suggests common femoral DVT.
Echocardiography.• Transthoracic echocardiography is not sensitive as screening test to rule
out PE. • However, echocardiography is a very sensitive indicator of massive or
unstable PE • Echocardiography should be done on any patient with suspected massive
or unstable PE • Also critical for selecting patients for thrombolysis or other aggressive
therapy. • Right ventricular (RV) function is most predictive of outcomes • About 40% of patients with PE and normal blood pressure (BP) have
abnormalities of the RV • Unstable patients include those with RV hypokinesis, dilation, abnormal
septal motion, patent foramen ovale, free floating right-heart thrombus • Large PEs predicted by >30% loss of blood flow to either lung (on V/Q
Scanning) • Pulmonary artery pressures can be estimated (physical exam has poor
sensitivity). • May be used for chronic monitoring of P-HTN as well.
Contrast Pulmonary Angiography. • This has been the gold standard for diagnosis but it is highly
invasive • The pulmonary catheter may also be used therapeutically
(angioplasty) • Angiography can be avoided in most patients by using other
tests above • Positive result is a filling defect or sharp cutoff in a pulmonary
artery branch • A negative angiogram with magnification excludes clinically
significant PE • Increased sensitivity is obtained with sub-selective dye
injection • May be morbid with worsening shortness of breath, artery
perforation, others • Spiral CT scanning can be used to detect proximal PEs instead
of angiography. • CT pulmonary angiography is safer than standard invasive
angiography and can be used to effectively rule out PE.
Magnetic Resonance Angiography (MRA).
• Techniques for use of MRA for diagnosing PE are evolving rapidly
• Estimated sensitivity ~80% (~100% for larger emboli), specificity 95%
• Non-invasive with little morbidity • Dynamic gadolinium enhancement is
used, allowing high quality images • Strongly consider prior to standard
invasive pulmonary angiography
Large pulmonary embolus (arrows) at the bifurcation of the right pulmonary artery in a 67 year old female. (A) CTPA, (B) bolus-triggered 3D MRPA, axial reformations, (C) recirculation phase 3D GRE and (D) free-induction steady state precession with ECG gating and respiratory triggering (TFISP-T).
Pulmonary embolism. transverse real-time MR image show large embolus in left pulmonary artery. Arrowheads
indicate embolic material. SPECT show the same finding and MRV show lower and upper leg DVT.
CT angiography clearly shows the central embolic material (arrow). (b) Coronal real-time MR, performed the same day, with similar information (arrow). (c) Transversal real-time image showing the saddle thrombus (arrows).
Axial and coronal SSFP localizer raised the suspicion of a saddle embolus (white arrow) at the RPA/LPA bifurcation
ConclusionsPulmonary embolus is a major health problem that is highly treatable when diagnosed, but carries high risk for morbidity and mortality is undiagnosed. Radiography is a major diagnostic tool in finding pulmonary embolus. There are several diagnostic studies like CT, nuclear V/Q scan and angiographic procedures that diagnose pulmonary embolus. The main cause of PE is venous thromboembolus that is diagnosed with ultrasound. Treatment for both PE and VTE can reduce the risk of recurring disease to below 2%, which is medically acceptable.
Related Documents