King Abdullah Medical City Department of Anesthesia

Perioperative management of sickle cell disease
Jul 16, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Perioperative Management of Sickle Cell Disease Patients
ByMohamed Ahmed
SayedalahlMD Anesthesia & Surgical Intensive
Care
Monday, February 23, 2015
-October 1902, Ohio state university.
-1905 North African Arab subjects.
-1910, James Herrick, detailed case report.
-1927, sickling by deoxygenation & reversed by reoxygenation.
-Clinical hypothesis:
-1955, 1st major review:
One of students noticed elliptical RBCs
Jaundice, dyspnea, LN, dark urine, leg ulcers,
epigastric pain & anemia
deoxygenation→sickling→vasoocclusion→moredeoxygenation→moresickling(vicious circle)
High incidence of perioperative serious and potentially fatal
complications
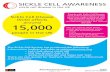
Epidemiology
- Mutant -globin gene → Hereditary hemoglobinopathy → production of variant Hb ( Hb SS) → Sickle cell anemia
- Variations in & Around sickle gene → different haplotypes ( 4 haplotypes in Africa & 1 Arabo-Indian or Asian haplotype in India & Persian gulf region)
- Heterozygous carrier state → SCT
Genotypes of Sickle cell disease
- Sickle cell anemia (Homozygous, HB SS)
Sickling occurs at PO2 ˂ 40 mmHg
- Sickle cell trait (Heterozygous, HB AS)
Sickling occurs at PO2 ˂ 20 mmHg
- Sickle-Hemoglobin C disease (HB SC)
- Sickle- β thalassemia disease (HB S β thal)
Gene penetration (heterogenicity)• Genotype differences (sickle cell anemia,
sickle cell trait, sickle cell HB C, sickle cellthalassemia)
• Haplotype differences (African, Arabo-Indian)
• HB synthesis, mutltistep, numerous genes(timing, extent and coordination)
• Extreme variability in HbF production• Polymorphism at cellular level (RBCs
membrane structure & function, hemecatabolic enzymes, nitric oxide generatingsystems & inflammatory mediators.
Molecular biology
1- Absence of the negative charge → instability of oxygenated hemoglobin → denaturation & break → RBCs hemolysis.
2- Hydrophobic amino acid → decrease in solubility of deoxygenated HB → polymerization & precipitation → sickling of RBCs.
Biochemistry
altered NO synthetase, increased leucocytic count,
activated coagulation pathway, increased circulatory cytokines
Historical hypothesis of RBCs sickling:
Role of endothelial and vascular dysfunction:- Survival of patients with SCD + cyanotic HD
- Studies:Effect of hypobaric hypoxia
Effect of inhalation of hypoxic gas mixture (FiO2 10-15%)
- Ascent to high altitudes or long aircraft flights
Clinical Picture
Progressive organ damage , intermittent periodsof severe pain & pulmonary complications
Severity and progression → markedly variable:Relatively benign course Early organ dysfunction and death
Pulmonary & Neurological complications
Chronic renal failure
Many deaths not attributed to chronic organ failure acute episode of pain, respiratory compromise, stroke
Clinical Picture…cont
Pain crises or VOC:
Most common sites: lumbar spine (49%), abdomen (32%),
femoral shaft (30%), and knee (21%)
Triggering events: without cause (˃50%), perceived skin
cooling (34%), emotional stress (10%), physical exertion (7%), and alcohol consumption (4%)
Arise from cortical infarction or from marrow infarction
Abdominal pain: bowel dysfunction, organ infarction, referred
from the ribs
Clinical Picture…cont
The acute chest syndrome (ACS):acute pneumonia like, new pulmonary infiltrate involving at leastone complete lung segment, but excluding atelectasis.
Additional diagnostic feature: chest pain, pyrexia greater than38.5°C, tachypnea, wheezing, & cough.
Precipitants: infectious pathogens, fat embolism after bone
marrow infarction, pulmonary infarction and surgical procedures.
Chronic progressive lung damage:persistent inflammatory process → lower airway obstruction &airway hyperreactivity → fibrosis and a progressive restrictivedisease → pulmonary hypertension, and right-sided cardiachypertrophy & and severe hypoxemia.
Clinical Picture…cont
-Neurological: (stroke)
Infarctive : in adolescence, intimal hyperplasia.
Hemorrhagic : third decade of life, rupture of chronically damaged arteries.
Renal: (Nephropathy)
Papillary necrosis → painful gross hematuria
Glomerular lesions → proteinuria
Hyposthenuria → specific gravity ˂1010
Chronic renal failure → third or fourth decade
Perioperative Epidemiology
Perioperative complications:
SCD-specific complications: Pain crisis and ACS
SCD-related complications:
Erythrocyte alloimmunization and transfusion reactions
Nonspecific complications:, bleeding, infection , fever, thrombosis, embolism, and death from causes other than SCD.
Preoperative Assessment
- Determine the risk of perioperative SCDcomplications
- Most frequent procedures: cholecystectomy,splenectomy, dilation and curettage, caesareansection, hysterectomy, adenotosillectomy,myringotomy and orthopedic prosthetic surgery.
- Incidence of complications: 3% for orthopedicsurgery, 8% for non-obstetrical intraabdominalsurgery, 17% for caesarean section andhysterectomy.
Perioperative Management
Erythrocyte Transfusion
Indications: prevention or treatment.
Rationale: dilution of sickle cells.
Studies:
Transfusion Vs Nontransfusion
Aggressive Vs Conservative
CPB and craniotomies
Alloimmunization: Non-ABO AB against Rh, Kell, & Lewis, 8-50% in SCD, causes.
Perioperative ManagementProphylactic erythrocyte transfusion remains a treatment with many complications.
Lack of clinical guidelines.
The National Heart, Lung, and Blood Institute (NHLBI)
SCD perioperative management Guideline.doc
Intraoperative Management
Improvement of Oxygen Delivery
Oxygen delivery impaired: obstructive or restrictive lung disease, vascular damage, abnormal rheology, peripheral A-V shunting ↑NO scavenging.
Compensatory mechanisms: ↑MV, ↑cardiac SV, ↓ PVR, ↑2,3- DG, and ↓Hct, and ↑ NO production.
Induced hypotension & autologous transfusion
Intraoperative ManagementOxygenation-Hypoxia as a precipitant of perioperative SCD-specific complications.
Prolonged O2 supplementation:-Suppression of erythrogenesis.-Withdrawal → VOC.
Little rationale:-Avoidance of preoperative anxiolytic medication.-Intraoperative hyperoxygenation.-Prolonged postoperative O2 supplementation.
Maintenance of adequate oxygenation
Intraoperative Management
Hydration
- Dehydration as a cause of perioperative complications.
- Adequate hydration.
- Modification of fluid management .
Intraoperative Management
Thermoregulation-Hypothermia as a precipitant of SCD complications
-Hyperthermia (SCT)
-Maintenance of normothermia.
Acid-base Regulation-Acidosis accelerates erythrocyte deformation.
-Alkalinization is not effective .
-Maintenance of normal acid-base balance.
Intraoperative Management
-Anesthetic technique
-GA Vs. RA
-Epidural anesthesia or Analgesia:
Pain control
VD
Oxygenation
-Avoid or minimize tourniquet
Postoperative Management- Oxygen supplementation.
- Adequate hydration.
- Aggressive pain management.
- Incentive spirometry.
- Early ambulation.
- Consider daily CBC, platelet and reticulocyte.
Postoperative ManagementPain Crisis
- Analgesia: Opioids: morphine, PCA, Fentanylpatch, Pethidine, (tolerance), NSAID, Corticosteroids,Epidural analgesia
- Incentive spirometry
- Supplemental oxygen
- Adequate hydration
- Erythrocyte & plasma transfusion.
- ACS, precipitated by pain crisis.
- psychological distress.
Postoperative Management
Acute Chest Syndrome
- 3 days after surgery and lasted 8 days
- Early incentive spirometry, bronchodilator therapy, supplemental oxygen, adequate analgesia, and broad-spectrum antibiotics.
- Blood transfusion.
- Nitric oxide and corticosteroids.
- Mechanical ventilation.
Related Documents