1

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

1

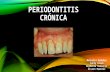
Definition
Chronic Periodontitis can be defined as “an infectious disease resulting in inflammation within the supporting tissues of the teeth, progressive attachment loss, and bone loss.”
- Previously known as adult periodontitis or slowly progressive periodontitis.
- Occur as a result of extension of inflammation from the gingiva into deeper periodontal tissue.
2

Common Characteristics
Onset - any age; most common in adults
Plaque initiates condition Subgingival calculus common finding Slow-mod progression; periods of
rapid progression possible Modified by local factors/systemic
factors/stress/smoking
3

Extent & Severity
Extent: Localized: <30% of sites affected Generalized: > 30% of sites affected
Severity: entire dentition or individual teeth/site Slight = 1-2 mm CAL Moderate = 3-4 mm CAL Severe = 5 mm CAL
4

Clinical Characteristics Gingiva
moderately swollen
Deep red to bluish-red tissues
Blunted and rolled gingival margin
Cratered papilla Bleeding and/or
suppuration
5

Clinical Characteristics Plaque/calculus
deposits Variable pocket
depths Loss of
periodontal attachment
Horizontal/vertical bone loss
Tooth mobility
6

CLASSIFICATION
7
A) Based on Disease Distribution:
Localized:Periodontitis is considered localized when <30% of the sites assessed in mouth demonstrate attachment loss and bone loss.
Generalized:Periodontitis is considered generalized when >30% of the sites assessed demonstrate attachment loss and bone loss.The pattern of bone loss in chronic periodontitis can be vertical or horizontal.

Sub classification of Chronic PeriodontitisSeverity Pocket
DepthsCAL Bone
Loss
Furcation
Early 4-5 mm 1-2 mm Slight
horizontal
Moderate 5-7 mm 3-4 mm Sl – mod
horizontal
Advanced > 7 mm 5 mm Mod-severe
horizontal
vertical
8

DISEASE DISTRIBUTION : It is a site-specific disease
CLINICAL SIGNS -
- Inflammation ,pocket formation ,attacment loss ,bone loss - All caused by site specific effects of a sub-gingival plaque accumulation
- That is why the effect are on one side only –other surface may maintain normal attachment level.
- Eg.-proximal surface with plaque may have C.A.L.
- And plaque free surface –FACIALsurface of same tooth may be without disease.

SYMPTOMS
Patient notices--
1. gum bleed
2. space appear between teeth due to tooth movement
3. May be painless (sleeping disease )goes unnoticed
4. Some time pain due to caries , root hypersensitivity
5. To cold /hot or both
6. PAIN-may be-- dull—deep radiating in the jaw
7. Area of food impaction can cause more discomfort
8. May be gingival tenderness or itchiness found

Periodontal Pathogens
• Gram negative organism dominate• P.g., P.i., A.a. may infiltrate:
• - Intercellular spaces of the epithelium• - Between deeper epithelial cells• - Basement lamina
11

Periodontal Pathogens Contn. Pathogens include:
Nonmotile rods: Facultative:
Actinobacillus a. E.c. Anaerobic:
P. g., P. i., B.f., F.n.
Motile rods: Facultative:
C.r.
Spirochetes: Anaerobic, motile:
Treponema denticola
12

Pathogenesis – Pocket Formation Bacterial
challenge initiates initial lesion of gingivitis
With disease progression & change in microorganisms development of periodontitis
13

Pocket Formation
Cellular & fluid inflammatory exudate degenerates CT
Gingival fibers destroyed Collagen fibers apical to JE destroyed
infiltration of inflammatory cells & edema
Apical migration of junctional epithelium along root
Coronal portion of JE detaches
14

Pocket Formation
Continued extension of JE requires healthy epithelial cells!
Necrotic JE slows down pocket formation
Pocket base degeneration less severe than lateral
15

Pocket Formation
Continue inflammation: Coronal extension of gingival margin JE migrates apically & separates from
root Lateral pocket wall proliferates &
extends into CT Leukocytes & edema
Infiltrate lining epithelium Varying degrees of degeneration &
necrosis
16

Development of Periodontal Pocket
17

Continuous Cycle!
Plaque gingival inflammation pocket formation more plaque
18

Classification of Pockets Gingival:
Coronal migration of gingival margin Periodontal:
Apical migration of epithelial attachment Suprabony:
Base of pocket coronal to height of alveolar crest
Infrabony: Base of pocket apical to height of alveolar
crest Characterized by angular bony defects
19

Histopathology
Connective Tissue: Edematous Dense infiltrate:
Plasma cells (80%) Lymphocytes, PMNs
Blood vessels proliferate, dilate & are engorged.
Varying degrees of degeneration in addition to newly formed capillaries, fibroblasts, collagen fibers in some areas.
20

Histopathology
Periodontal pocket: Lateral wall shows most severe
degeneration Epithelial proliferation & degeneration Rete pegs protrude deep within CT Dense infiltrate of leukocytes & fluid
found in rete pegs & epithelium Degeneration & necrosis of epithelium
leads to ulceration of lateral wall, exposure of CT, suppuration
21

Clinical & Histopathologic Features Clinical :1. Pocket wall bluish-
red2. Smooth, shiny
surface3. Pitting on
pressure
Histopathology:1. Vasodilation &
vasostagnation2. Epithelial
proliferation, edema
3. Edema & degeneration of epithelium
22

Clinical & Histopathologic FeaturesContn… Clinical:1. Pocket wall may
be pink & firm2. Bleeding with
probing3. Pain with
instrumentation
Histopathology:1. Fibrotic changes
dominate2. blood flow,
degenerated, thin epithelium
3. Ulceration of pocket epithelium
23

Clinical & Histopathologic FeaturesContn… Clinical :1. Exudate2. Flaccid tissues
Histopathology:1. Accumulation of
inflammatory products
2. Destruction of gingival fibers
24

Stages of Periodontal Disease
25

Root Surface Wall
Periodontal disease affects root surface: Perpetuates disease Decay, sensitivity Complicates treatment
Embedded collagen fibers degenerate cementum exposed to environment
Bacteria penetrate unprotected root
26

Root Surface Wall Contn…
Necrotic areas of cementum form; clinically soft
Act as reservoir for bacteria Root planing may remove necrotic
areas firmer surface
27

Inflammatory Pathway
Stages I-III – inflammation degrades gingival fibers
Spreads via blood vessels: Interproximal:
Loose CT transseptal fibers marrow spaces of cancellous bone periodontal ligament suprabony pockets & horizontal bone loss transseptal fibers transverse horizontally
28

Inflammatory Pathway
Interproximal: Loose CT periodontal ligament
bone infrabony pockets & vertical bone loss transseptal fibers transverse in oblique direction
29

Inflammatory Pathway
Facial & Lingual: Loose CT along periosteum marrow
spaces of cancellous bone supporting bone destroyed first alvoelar bone proper periodontal ligament suprabony pocket & horizontal bone loss
30

Inflammatory Pathway
Facial & Lingual: Loose CT periodontal ligament
destruction of periodontal ligament fibers infrabony pockets & vertical or angular bone loss
31

Periodontal Disease Activity Bursts of activity followed by periods of
quiescence characterized by: Reduced inflammatory response Little to no bone loss & CT loss
Accumulation of Gram negative organisms leads to: Bone & attachment loss Bleeding, exudates May last days, weeks, months
32

Periodontal Disease Activity Period of activity followed by period
of remission: Accumulation of Gram positive bacteria Condition somewhat stabilized
Periodontal destruction is site specific
PD affects few teeth at one time, or some surfaces of given teeth
33

Prevalence:
Chronic Periodontitis increases in prevalence & severity with age.
Affect both the sexes equally.
It is an age-associated, not age related disease.

RISK FACTORS FOR DISEASE:1) PRIOR HISTORY OF PERIODONTITIS—predictor-more risk for developing damage to periodontium.2) LOCAL FACTORS:
Plaque AccumulationOral HygieneTooth MalpositionRestoration
Preserve & Quantity of certain bacteriaHost defencesSubgingival RestorationEnvironmentCalculus, smoking
Connective Tissue destructionGenetic influenceInflammationPeriodontopathic bacteriaSmoking, Calculus
Loss of Attachment
MODIFYING
FACTORS

3) SYSTEMIC FACTORS: Type II or Non – Insulin dependent Diabetes Mellitus (NIIDDM)
4) ENVIRONMENTAL & BEHAVIORAL FACTORS: Smoking Emotional Stress5) GENETIC FACTORS: Frequent among family members and across different generations.
GENERAL CONCEPT FOR ETIOLOGY OF CHRONIC PERIODONTITISPlaque accumulation
Maturation of Plaque
Quality & Quantity of periodontopathic Plaque accumulation
Maturation of Plaque
Quality & Quantity of periodontopathic bacteria
InflammationPlaque accumulation
Maturation of Plaque
Quality & Quantity of periodontopathic bacteria
Inflammation
Connective tissue destruction.
Connective tissue destruction.bacteriaInflammation
Connective tissue destruction.
Host status and defences
Plaque accumulationPlaque accumulationMaturation of PlaqueMaturation of PlaqueQuality & Quantity of Quality & Quantity of periodontopathic bacteriaperiodontopathic bacteria
InflammationInflammation
connective tissue connective tissue destruction.destruction.

MANAGEMENT The treatment consists of –1. Non-surgical procedures
Scaling Root planing Curettage
2. Surgical procedure Pocket reduction surgery
Resective Regenerative
Correction of morphological / anatomic defects

Overall Prognosis
Dependent on: Client compliance Systemic involvement Severity of condition # of remaining teeth
38

Prognosis of Individual Teeth Dependent on:
Attachment levels, bone height Status of adjacent teeth Type of pockets: suprabony, infrabony Furcation involvement Root resorption
39
Related Documents