Development of Induced Pluripotent Stem Cell-based Therapies for Hematopoietic Stem Cell Disorders Joseph A. Panos, Luigi J. Alvarado, Ph.D., André Larochelle, M.D., Ph.D. National Heart, Lung, and Blood Institute; Hematology Branch; National Institutes of Health, 9000 Rockville Pike, Bethesda, MD 20892 INTRODUCTION Hematopoietic stem cells (HSCs) have the remarkable ability to reconstitute and maintain a functional hematopoietic system for the lifespan of an individual. In patients with inherited bone marrow (BM) failure disorders, HSCs are insufficient. Allogeneic HSC transplantation offers a potential cure, but there are well-described limitations. Also, sufficient autologous HSCs for gene therapy applications are unavailable in these patients, and methodologies for expansion of these rare HSCs are inexistent. Induced pluripotent stem cell (iPSC)-based therapies are a tractable alternative for these patients because of their potential to provide an unlimited source of autologous cells for gene therapy applications. Several protocols have been developed to generate hematopoietic stem and progenitor cells (HSPCs) from iPSCs but they are inefficient at producing the quantity and quality of HSCs required for clinical applications. Namely, phenotypically defined HSCs derived from iPSCs are incapable of reconstituting the hematopoietic system long-term in animal models; the cause of this functional defect remains unclear. We have recently shown that homing and engraftment of HSPCs to their BM microenvironment is mediated by polarized membrane domains enriched in adhesion molecules. The presence of polarized membrane domains on iPSC-derived HSCs has never been investigated as a possible cause for the homing/engraftment defect. A recent study has suggested that brief exposure of native HSPCs to hyperthermic conditions enhances domain polarization, homing, and engraftment.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Development of Induced Pluripotent Stem Cell-based Therapies for Hematopoietic Stem Cell
Disorders
Joseph A. Panos, Luigi J. Alvarado, Ph.D., André Larochelle, M.D., Ph.D.
National Heart, Lung, and Blood Institute; Hematology Branch; National Institutes of Health, 9000
Rockville Pike, Bethesda, MD 20892
INTRODUCTION
Hematopoietic stem cells (HSCs) have the remarkable ability to reconstitute and maintain a functional
hematopoietic system for the lifespan of an individual. In patients with inherited bone marrow (BM)
failure disorders, HSCs are insufficient. Allogeneic HSC transplantation offers a potential cure, but there
are well-described limitations. Also, sufficient autologous HSCs for gene therapy applications are
unavailable in these patients, and methodologies for expansion of these rare HSCs are inexistent.
Induced pluripotent stem cell (iPSC)-based therapies are a tractable alternative for these patients because
of their potential to provide an unlimited source of autologous cells for gene therapy applications. Several
protocols have been developed to generate hematopoietic stem and progenitor cells (HSPCs) from iPSCs
but they are inefficient at producing the quantity and quality of HSCs required for clinical applications.
Namely, phenotypically defined HSCs derived from iPSCs are incapable of reconstituting the
hematopoietic system long-term in animal models; the cause of this functional defect remains unclear.
We have recently shown that homing and engraftment of HSPCs to their BM microenvironment is
mediated by polarized membrane domains enriched in adhesion molecules. The presence of polarized
membrane domains on iPSC-derived HSCs has never been investigated as a possible cause for the
homing/engraftment defect. A recent study has suggested that brief exposure of native HSPCs to
hyperthermic conditions enhances domain polarization, homing, and engraftment.

Accordingly, this project endeavored to: 1. Develop a scalable protocol that supports hematopoietic
differentiation of human iPSCs to meet the threshold cell dose of HSPCs for clinical transplantation and
2. Investigate the presence of polarized membrane domains on native and iPSC-derived HSPCs, and the
potential role of hyperthermia to enhance domain polarization, HSPC homing, and engraftment.
METHODS
Hematopoietic Differentiation from Human iPSCs
Human iPSCs were reprogrammed using Sendai viral vectors from normal G-CSF-mobilized
CD34+/CD38- cells. iPSC colonies were cultured on Matrigel-coated plates in E8 medium. Cells were
exposed to a cocktail of mesodermal differentiation factors for 3 days in APEL medium, followed by
hematopoietic differentiation for 10 days. iPSC-differentiated cells were harvested from the culture
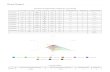
supernatant starting at Day 10 (Figure 1).
Figure 1. Experimental schematic for the generation of HSCs from iPSCs.
Hyperthermic Treatment and HSPC Homing

Immune-deficient (NSG) mice were injected i.v. with ~1x106 human CD34+ cells or iPSC-derived
HSPCs immediately after a 4.5 hour-pre-culture at 39.5°C or 37°C. Twenty-four hours post-injection,
mice were euthanized, their BM harvested from 6 bones, stained with anti-human CD45-FITC antibodies,
and analyzed by flow cytometry. For visualization of membrane domains, cells were stained with
AlexaFluor 555-‐conjugated Cholera toxin subunit B and visualized with a Zeiss LSM 780 confocal
microscope.
RESULTS
Hematopoietic Differentiation from Human iPSCs
Exposure to mesodermal and hematopoietic differentiation factors promoted the formation of a
hemogenic endothelial monolayer. As early as Day 7, spherical hematopoietic-like cells formed
superficial clusters over the endothelial monolayer. These cells spontaneously sprouted in the culture
supernatant between Days 10 and 14, allowing easy harvest (Figure 2).

Figure 2. Time course depiction of HSPC generation from iPSCs.

The initial iPSC plating density was identified to be critical for optimal hematopoietic differentiation
from human iPSCs (Figure 3).
Figure 3. Plating densities exceeding 70,000 cells/plate allowed for multiple HSPC harvests on both
Days 12 and 14.
CD34hi/CD45lo (primitive HSPCs) and CD34lo/CD45hi (more mature HSPCs) populations, were observed
in supernatant collected from all cultures with initial iPSC plating densities >70,000 cells per plate
(Figure 4).
70,000 iPSCs 90,000 iPSCs iPSCs
100,000 iPSCs

Figure 4. Generation of human iPSCs (CD45+CD34+) from iPSCs at various iPSC plating densities.
Estimation of various HSPC counts shows that the density condition of 70,000 cells per plate most
efficiently generated the desired CD34hi/CD45lo progenitor population for harvests conducted at Day 12.
Density
(cells/plate)
CD34+/CD45+
count
CD34lo/CD45hi
count
CD34hi/CD45lo
count
CD34hi
/CD45lo -
CD34lo
/CD45hi
Ratio
Efficiency
of HSPC
generation
70,000 151,438 15,003 30,439 2.03 6.49
90,000 17,523 819 5,291 6.56 1.71
100,000 50,607 1,701 15,485 9.10 1.51
Hyperthermic Treatment and HSPC Homing
Homing of human CD34+ cells was measured as the percentage of human CD45+ cells in the mouse BM
24 hours after transplantation. The proportion of CD45+ cells was significantly greater in the heat-treated
group compared to the heat-untreated group (Figure 5).
Figure 5. Heat treatment confers a greater homing capacity among human CD34+ cells.

Hyperthermic Treatment and Domain Polarization
Lipid rafts on heat-treated and heat-untreated cells were detected directly using AlexaFluor 555-
conjugated Cholera toxin subunit B, which binds specifically to ganglioside GM1. The polarization of
lipid rafts, as a result of heat treatment, may explain enhanced CD34+ homing to the bone marrow niche
(Figure 6).
Figure 6. Heat-treatment promotes the polarization of lipid rafts.
CONCLUSIONS
Hematopoietic Differentiation of Human iPSCs
The protocol optimized in this study provides an efficient approach for the generation of human HSPCs
with a primitive CD45lo/CD34hi phenotype from iPSCs generated from mobilized CD34+CD38- cells.
Initial plating density of iPSCs was identified as a critical factor for efficient hematopoietic
differentiation, with 70,000 iPSCs as the most efficient cell density for generation of CD34hi/CD45lo
progenitors with the iPSC line utilized. Days 10-14 of the differentiation protocol were identified as
optimal collection times for HSPCs.
Hyperthermic Treatment and HSPC Homing

Brief hyperthermic treatment of 39.5°C of native human CD34+ cells is effective in increasing their
homing within the BM of NSG mice. Enhanced homing may be related to increased polarization of
membrane-domain, enriched in adhesion molecules. These findings provide proof-of-principle that this
approach may enhance homing and engraftment of iPSC-derived HSPCs.
REFERENCES
1. Focosi, D., Amabile, G., Di Ruscio, A., Quaranta, P., Tenen, D.G., Pistello, M. (2014).
Induced pluripotent stem cells in hematology: current and future applications. Blood
Cancer Journal, 2(114), 1-8.
2. Kaufman, D.S. (2009). Toward clinical therapies using hematopoietic cells derived from
human pluripotent stem cells. Blood, 114(7), 3513-3523.
3. Capitano, M.L., Hangoc, G., Cooper, S., Broxmeyer H.E. (2015). Mild Heat Treatment
Primes Human CD34+ Cord Blood Cells for Migration Toward SDF-1 and Enhances
Engraftment in an NSG Mouse Model. Stem Cells Express, 33, 1975-1984.
Related Documents