7/28/08 dharl de la peña PAIN MANAGEMENT

Pain Managementdharl
Nov 19, 2014
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

7/28/08dharl de la peña
PAIN MANAGEMENT

dharl

dharl
PAIN• A high unpleasant and very personal
sensation that cannot be shared with others• More than a symptom of a problem• Presents both a physiologic and psychologic
dangers to health and recovery• Viewed as an emergency situation deserving
attention and prompt treatment

dharl
PAIN
P“ain is an unpleasant sensory and emotional experience in association
with actual or potential tissue damage, or described in terms of
such damage.”The International Association for the Study of Pain

dharl
Types of Pain
DURATION
LOCATION -
ETIOLOGY -
ACUTE PAIN
CHRONIC ( NON-MALIGNANT PAIN )
CANCER-RELATED PAIN
Example: CHEST PAIN HEADACHE PELVIC PAIN
Example: BURN PAINPOST-HERPETIC PAIN

dharl
Types of PainAccording to DURATION
• Acute– Lasts only through the expected recovery
period– Sudden or slow onset
• Chronic– Prolonged, recurring or persisting over 6
months or longer– Chronic malignant pain– Chronic nonmalignant pain

dharl
Mild to severeSympathetic NS response Related to tissue injuryRestless and anxious
Reports painBehavior indicative of pain
Mild to severeParasympathetic NS response
Continues beyond healingDepressed and withdrawn
Does not mention pain unless asked
Pain behavior often absent
Acute Pain vs. Chronic Pain

dharl
Types of PainAccording to ETIOLOGY
• Neuropathic pain– Current or past damage to the
peripheral or central nervous system and may not have a stimulus
• Intractable pain– Highly resistant to relief
• Phantom pain– Sensation perceived in a body part
that is missing

dharl
Concepts associated with Pain
• Pain threshold
• Pain reaction
• Pain tolerance
– Maximum amount and duration of pain that an individual willing to endure
– Amount of pain stimulation a person requires in order to feel pain
– ANS and behavioral responses to pain

dharl
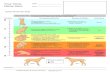
Physiology of Pain
• Nociception–Transduction
–Transmission
–Perception
–Modulation

dharl
Physiology of PainTransduction
• CHEMICAL MEDIATORS–chemicals that enhance pain perception
• Prostaglandin • Substance P• Bradykinin• Histamine

dharl
Physiology of PainTransduction
• ENDORPHINS–“endogenous morphines”–naturally occurring analgesic in
the body– is said to be released during
exercise

dharl
NOXIOUS STIMULI
1

dharl
IMPULSE TRANSMISSION
2

dharl
AFFERENT SENSORY FIBERS
3

dharl
SPINAL CORD JUNCTIONS
4

dharl
DORSAL HORN
5

dharl
SYNAPSE
6

dharl
CALCIUM AND GLUTAMATE
7

dharl
SYNAPTIC CLEFT
8

dharl
POST-SYNAPTIC TERMINAL
9

dharl
NOCICEPTIVE NEURON
10

dharl
PAIN PERCEPTION
11

dharl
Gate Control Theory• peripheral nerve fibers carrying
pain to the spinal cord can have their input at the spinal cord level before transmission to the brain
Physiology of PainModulation

dharl
Responses to Pain• Sympathetic NS and the Parasympathetic NS = Fight-or-flight response
• Proprioceptive reflex

dharl
Factors Affecting the Pain Experience
• Ethnic and Cultural Values• Developmental Stage• Environment and Support People• Past Pain Experiences• Meaning of Pain• Anxiety and Stress

dharl
Age Variations in the Pain experience
• Infant– Perceives pain; increased sensitivity
• Toddler and Preschooler– Develops ability to describe pain and its
intensity and location; crying and anger; a punishment
• School-age child– Tries to be brave; attempts to explain the
pain; may regress to an earlier stage

dharl
• Adolescent– Slow to acknowledge pain; may be
considered weakness; appear brave in front of peers
• Adult– Gender-based behaviors; may ignore pain
• Elderly– Perceives pain as part of the aging
process; decreased sensations and perceptions of the pain
Age Variations in the Pain experience

dharl
Nursing Assessment
• Pain History–Previous pain treatment and
effectiveness
–When and what analgesics were last taken
–Other medications being taken
–Allergies to medications

dharl
Mnemonics for Pain Assessment
PQRST
– P
– Q
– R
– S
– T
OLD CART
OLDCART

dharl
Why clients May be reluctant to Report Pain
• Unwillingness to trouble staff• Fear of the injectable route• Belief that pain is to be expected• Normal part of aging• Expressions of pain reveal weakness• Difficulty expressing personal discomfort• Concern about use of drugs and addiction• Will lead to further tests and expenses• Concern about unwanted side effects

dharl
Pain Intensity or Rating Scales
• VISUAL ANALOG SCALE–the person is asked to place a
mark indicating where the current pain lies on the line
–to score the results, a ruler is placed along the line and is measured and reported in mm or cm

dharl
Pain Intensity or Rating Scales VISUAL ANALOG SCALE

dharl
Pain Intensity or Rating Scales
• FACES PAIN SCALE –the instrument has six faces
depicting expressions that range from contented to obvious distress.
–the patient is asked to point to the face that most closely resembles the pain intensity felt

dharl
Pain Intensity or Rating Scales
FACES PAIN SCALE

dharl
Pain QualityCommonly Used Pain Descriptors
• Sensory– Searing– Scalding– Sharp– Piercing– Drilling– Wrenching– Shooting– Burning– Crushing – Penetrating
• Affective– Unbearable– Killing– Intense– Torturing– Agonizing– Terrifying– Exhausting– Suffocating– Frightful– Punishing– Miserable– Heavy

dharl

dharl
PrecipitatingPrecipitating FactorsFactors
• activities that precede pain
Alleviating FactorsAlleviating Factors anything that they have done to
alleviate pain

dharl
• Associated Symptoms• Effects on Activities of Daily
Living• Coping Resources• Affective Responses• Observation of Behavioral
and Physiologic Responses• Daily Pain Diary

dharl
PLACEBOPLACEBO• from the Latin for “I shall please”• is an inactive substance (pill,
liquid, etc.), which is administered as if it were a therapy, but which has no therapeutic value other than the placebo effect.

dharl
PLACEBO EFFECTPLACEBO EFFECT• occurs when a person responds to
the medication or other treatment because of the expectation that the treatment will work

dharl
ETHICAL ADMINISTRATION OF PLACEBOS
• A placebo effect is not an indication that the person does not have pain; rather, it is a true physiologic response
• Placebos should never be used to test the person’s truthfulness about pain or as the first-line of treatment
• A positive response to a placebo (ex. A reduction in pain) should never be interpreted as an indication that the person’s pain is not real
• A patient should never be given a placebo as a substitute for pain medication

dharl
NURSE’S ROLE IN PAIN NURSE’S ROLE IN PAIN MANAGEMENTMANAGEMENT
• Administers pain-relieving medication
• Assesses the effectiveness of the medications
• Serves as an advocate for the patient when the prescribed medication is ineffective
• Educator to the patient and family on how to manage pain effectively.

dharl
PAIN MANAGEMENT PAIN MANAGEMENT STRATEGIESSTRATEGIES
• PHARMACOLOGIC– Makes use of pain
medications as ordered by the physician

dharl
• NON-PHARMACOLOGIC– Other measures to
relieve pain other than administering pain medications

dharl
PHARMACOLOGIC INTERVENTIONS
• Before administering pain medications, the nurse should:1.) Ask for previous history of drug allergy
2.) Ask patient’s current medications
3.) Ask the patient’s current pain status
4.) Check vital signs

dharl
APPROACHES FOR USING
ANALGESIC AGENTS• Balanced Anesthesia Approach
• PRN Approach
• Preventive Analgesia or Pre-Emptive Analgesia
• Patient-Controlled Analgesia

dharl
APPROACHES FOR USING APPROACHES FOR USING ANALGESIC AGENTSANALGESIC AGENTS Balanced Analgesia Approach
– Refers to use of MORE THAN ONE form of analgesia concurrently to obtain more relief with fewer side effects
– Example:• Morphine 30mg• 8 mg morphine + 30 mg ketorolac
** Both approaches offers the same pain relief but the second
approach has lesser side effects

dharl
APPROACHES FOR USING APPROACHES FOR USING ANALGESIC AGENTSANALGESIC AGENTS
PRN Approach• “PRO RE NATA” – “as needed approach”• The medication is administered when the
patient complains of pain• Some patients remained in pain because
they are not aware that they have to ask for pain medications
• This is the standard method used in the past.

dharl
APPROACHES FOR USING APPROACHES FOR USING ANALGESIC AGENTSANALGESIC AGENTS
Preventive Analgesia or Pre-Emptive Analgesia
• “An ounce of preventions is better than a pound of cure”
• Administration of pain medications 1-2 hours before the scheduled procedure
• It is also the administration of pain medications ROUND THE CLOCK (RTC)

dharl
APPROACHES FOR USING APPROACHES FOR USING ANALGESIC AGENTSANALGESIC AGENTS Patient-Controlled Analgesia
• Used to manage post-operative pain or chronic pain
• Allows the patient to personally control the administration of pain medication

dharl
• PCA PUMP• permits the patient to self-administer extra
medication with increasing pain• is electronically controlled by a timing device• patients can administer small amounts of
medication at a time• the timer can be programmed so even if the
patient pushes the button a couple of times, no additional doses are released
APPROACHES FOR USING APPROACHES FOR USING ANALGESIC AGENTSANALGESIC AGENTS Patient-Controlled Analgesia

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
CUTANEOUS STIMULATION• MASSAGE– generalized
cutaneous stimulation of the body
– causes the release of endorphins, decreasing pain.

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
ICE AND HEAT THERAPY• May be effective pain-relief strategies but
their mechanisms of action are not well understood.
• ICE THERAPY
– should be placed on the injury site immediately after injury
– application should not be longer than 30mins (long applications may cause frostbite or nerve injury)

dharl
• Application of heat increases blood flow to an area.
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
HEAT THERAPY

dharl
• ICE AND HEAT THERAPIES

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
TRANSCUTANEOUS ELECTRICALNERVE STIMULATION (TENS)
• Makes use of a battery-operated unit with electrodes applied to the skin to produce a tingling, vibrating or buzzing sensation in the area of pain
• Stimulates non-pain receptors, thus blocking pain sensation
• Another possible explanation is the placebo effect

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
DISTRACTION• Involves focusing the patient’s attention on something rather than the pain
• Doesn’t relieve severe pain
• DISTRACTION TECHNIQUES
- Watching TV- Listening to music

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS
RELAXATION TECHNIQUES• Effective in controlling
low back pain• Skeletal muscle
relaxation is believed to reduce pain by relaxing muscles that contribute to pain.
• Example:– Benson’s Relaxation
Technique

dharl
NON-PHARMACOLOGIC NON-PHARMACOLOGIC INTERVENTIONSINTERVENTIONS GUIDED IMAGERY
• Using one’s imagination in a special way to distract one’s self from an uncomfortable sensation
• Advice Guided Imagery for 5 minutes 3x a day
• ** This may not work in severe pain

Sacrifices are sometimes useless especially if that someone doesn’t know how to appreciate…
They’ll come to realize important things when it’s already late…
TOO LATE!!!
Related Documents