Overview of childhood cancer research at musc 2010
Oct 21, 2014
Chase After a Cure proudly supports Dr. Kraveka's lab at Musc. The money we raise is doing great research, the proof is in the slideshow.
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript


MUSC
Founded in 1824 as the first school of medicine in the southeastern U.S., the Medical University of south Carolina is now the core of the state’s largest medical complex.
A freestanding academic health center, MUSC is the only tertiary/ quaternary care referral center in South Carolina for a statewide population of about 4.3 million people.
MUSC is the lead biomedical research institution in Health Sciences South Carolina, a statewide consortium to facilitate efficiency and speed in developing, testing and bringing health interventions and therapies to widespread use.

MUSC Children’s HospitalThe MUSC Children’s Hospital is dedicated to enhancing the
health of children throughout South Carolina and to providing an environment that supports excellence in pediatric patient care, teaching, and research.
MUSC Children's Hospital is the largest and most comprehensive pediatric medical center in South Carolina.
Our health system covers the state with an extensive network of physicians, health care professionals and services – all dedicated to children. MUSC Children’s Hospital has earned top rankings from Child magazine and American Health Magazine.

Darby Children’s Research InstituteThe Darby Children's Research Institute (DCRI) opened in
February 2005 as the largest and most comprehensive pediatric research facility in the Carolinas.
Its mission is to improve the lives of children, their families and communities by conducting high quality children’s research, training superior physicians and scientists, and fostering innovation through the sciences of discovery and application.
The overall goals of the DCRI are to empower talented scientists, promote inclusiveness and collaboration, enable established and new investigators, and increase and diversify funding for pediatric research.

Hollings Cancer Center In spring 2009, Hollings Cancer Center was named a
designated cancer center by the National Cancer Institute (NCI). Hollings is South Carolina's only NCI-designated cancer center -- and one of only 65 in the country.
This distinction identifies cancer centers offering the most advanced research and clinical trails for cancer. NCI-designated cancer centers are a major source in developing new cancer treatments and more effective approaches to cancer prevention and diagnosis. These cancer research centers deliver medical advances to patients and their families, educate health care professionals and the public, and reach out to underserved populations.

Facts on Childhood Cancer - IChildhood cancer is the #1 cause of death from disease in children in
the US, more than from asthma, diabetes, cystic fibrosis, congenital anomalies, and pediatric AIDS combined. It is the 2nd leading cause of death in children overall, after automobile accidents.
~ 12,500 children are diagnosed with cancer per year.
More than 40,000 children and adolescents are currently in treatment.
Each and every school day, 46 children, or more than two full classrooms of kids, are diagnosed with cancer in the United States alone.
1 in every 4 elementary schools has a child with cancer.
The average age of cancer diagnosis is 6 years old.

Facts on Childhood Cancer - II 1 in 300 children will be diagnosed with cancer before age 20.
Each year over 2,000 children die, and over 40,000 are in treatment.
The average high school has 2 students who are survivors.
3 out of 5 survivors experience a late effects treatment.
The causes of childhood cancer are unknown.
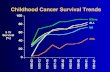
Today, up to 78% of the children with cancer can be cured, yet some forms of childhood cancer have proven so resistant to treatment that, in spite of research, a cure is illusive.
Cancer in childhood occurs regularly, randomly and spares no ethnic group, socioeconomic class, or geographic region.

Facts on Childhood Cancer Funding In 2008, The National Cancer Institute’s (NCI) federal
budget was $4.9 billion. Of that, breast cancer received 12% ($572.6 million) prostate cancer received 7% ($285.4 million) and all 12 major groups of pediatric cancers combined received less than 4%. ($189.8 million). Funding for Neuroblastoma research was $18.6 million.
In comparison, the cost of one C-17 Globemaster airplane is $202.3 million. Alex Rodriguez salary was $28 million and Shaquille O’Neal’s salary was $20 million. The payroll of the New York Yankees ($238.7 million) was more than the amount of money allotted to pediatric cancer research.
The American Cancer Society spends less than 70 cents of each 100 dollars raised on childhood cancer.
Only Research Cures Childhood Cancer.

Solid tumor cancer that originates in the nerve tissue of the neck, chest, abdomen, or pelvis, but most commonly in the adrenal gland.
Neuroblastoma is a common and often difficult to treat cancer.
Neuroblastomas are the most common cancer of infancy, with an incidence rate almost double that of leukemia, during the first year of life.
Accounts for ~15% of all childhood cancer deaths
3rd most common pediatric cancer: Most commonly diagnosed cancer of infancy Majority diagnosed under age 5.
Neuroblastoma has one of the lowest survival rates of all pediatric cancers.
Neuroblastoma Facts - I

Over 80% of children diagnosed with neuroblastoma during infancy are alive 5 years following diagnosis.
In contrast, for children diagnosed with neuroblastoma at age 1 year or older, the 5-year relative survival was about 45%.
In the United States, about 700 children are diagnosed with neuroblastoma each year. Of these ~45% with have advanced “high risk” disease.
The survival rate of high risk children is less than 40%.
There are few effective treatments for relapsed neuroblastoma.
Neuroblastoma Facts - II

Identification of new targets and novel therapeutic approaches are needed for
“high risk” patients
Risk Group Prognosis

Childhood Cancer at MUSC - I The division of pediatric hematology-oncology at MUSC offers
comprehensive care for children with cancer and blood disorders. The members of the division include: Dr. Michelle Hudspeth, Dr. Jacqueline Kraveka, Dr. Shayla Bergman, and Dr. Sherron Jacskon.
There are over 60 new childhood cancer diagnoses seen annually at MUSC. 28 children have been diagnosed with neuroblastoma at MUSC since 2001.
MUSC Children’s Hospital is the only pediatric bone marrow transplant center in South Carolina.
Dr. Michelle Hudspeth was recruited to MUSC from John Hopkins University in 2007 to lead and expand the stem cell transplant program. In 2008 the number of pediatric transplants increased 125%.
As the only pediatric stem cell transplant center in the state, the majority of patients in South Carolina with high-risk neuroblastoma are seen here for autologous transplant. Over 60% of these patients will relapse. New therapies are needed for these patients. In the past 4 years the division has performed 13 autologous transplants for neuroblastoma.

Childhood Cancer at MUSC - II MUSC Children’s Hospital is a member of the Children’s Oncology Group
(COG). The Children’s Oncology Group (COG) is the world’s premier pediatric cancer
research collaborative. This network of more than 200 Hospitals and 5,000 healthcare professionals dedicates their lives to finding answers and sharing results. 90% of children in North America are treated at COG institutions and enrolled on COG clinical trials. COG members have been the primary innovators in new treatments for children with cancer.
Dr. Kraveka is very involved on the national level in the COG she is member of the Neuroblastoma Disease Committee and the Non-Hodgkin’s Lymphoma Committee. As a Neuroblastoma Disease Committee member, she has been involved in the design of the recently opened Phase III clinical trial for high-risk neuroblastoma: ANBL0532: A Phase III Randomized Trial of Single versus Tandem Myeloablative Consolidation Therapy for High-Risk Neuroblastoma. She is also a member of the Neuroblastoma Clinical and Biological Risk Factors Task Force. This task force’s mission is to find new clinical and biologic markers for neuroblastoma treatment and risk assignment.

Laboratory Neuroblastoma Research at MUSC - I In addition to seeing patients, Dr. Kraveka is a researcher in the Darby
Children’s Research Institute and a member of the “Lipid Signaling in Cancer Research Group” at the MUSC Hollings Cancer Center. Her research focuses on developing novel therapeutic strategies for the treatment of neuroblastoma.
Current laboratory research projects focus on: 1) Studying the therapeutic potential of regulating the protein enzyme
dihydroceramide desaturase (DEGS-1) 2) Examining whether specific sphingolipids (fats) (ceramides) and/or
expression of sphingolipid enzymes (proteins) control the growth and spread of neuroblastoma tumors.
The laboratory has been awarded research grants from the National Cancer Institute, the St. Baldrick’s Foundation, the Rally Foundation for Childhood Cancer Research, and the National Childhood Cancer Foundation. Laboratory research costs are between $150,000- 200,000/ year.
This is the only research laboratory in South Carolina dedicated to Pediatric Cancer Research.

Laboratory Neuroblastoma Research at MUSC - IIResearch on the Dihydroceramide Desaturase (DEGS-1) Enzyme
DEGS-1 is the enzyme (protein) is responsible for the conversion of the sphingolipid (fat) dihydroceramide (dhCer) to ceramide (Cer). Ceramide is a bioactive sphingolipid that mediates important cellular activities
such as induction of cell differentiation, growth arrest, senescence, and apoptosis. We have found that the drug, fenretinide (a synthetic retinoid in phase II clinical trials) inhibits the DEGS-1 enzyme. This research has found novel biologic functions for dhcers and identified DEGS-1 as a target for neuroblastoma and other pediatric and adult cancers. The laboratory is currently studying the localization and regulation of this enzyme. Understanding how DEGS-1 and dhCers works is crucial the development of novel treatments for cancer.

Laboratory Neuroblastoma Research at MUSC- III Metabolomic Profiling of Bioactive Sphingolipids in Neuroblastoma
The laboratory is examining the differences in sphingolipid levels and the expression of sphingolipid enzymes in low grade versus high-grade neuroblastoma tumor tissue samples.
Analysis of endogenous ceramides and expression of related enzymes has not previously been correlated with disease or treatment prognosis in neuroblastoma.
If our hypothesis is true and specific ceramide/dihydroceramide species or sphingolipid metabolizing enzyme levels associated with high-risk neuroblastoma can be identified, then this study would be of considerable clinical relevance.
It is proposed that these experiments will identify new targets for treatment in patients with high risk/ poor prognosis neuroblastoma.
The data obtained from this project has great potential to be incorporated into future clinical trials for neuroblastoma.

Clinical / Translational Neuroblastoma Research - I NMTRC Consortium
The Neuroblastoma and Medulloblastoma Translational Research Consortium (NMTRC) was formed in 2008 by Dr. Giselle Sholler at the University of Vermont to conduct clinical trials that test new drugs and new combinations of drugs against relapsed neuroblastoma and medulloblastoma. NMTRC consists of a group of closely collaborating investigators who are linked with laboratory programs to develop novel therapies. Those treatments with promising results will then be considered for more extensive national testing. MUSC is a member of this new consortium. Other member institutions include:
University of Vermont The University of Texas, MD Anderson Cancer Center MD Anderson Cancer Center, Orlando FL Rady Children’s Hospital San Diego, CA Cardinal Glennon Children’s Medical Center , St Louis. MO Levine Children’s Hospital, Charlotte, NC Helen DeVos Children’s Hospital, Grand Rapids, MI Hospital for Sick Children, Toronto, Canada Children’s Hospital Orange County, Orange, CA U of Hawaii, Kapiolani Medical Center for Women & Children. Honolulu, HI

Clinical / Translational Neuroblastoma Research - II NMTRC Consortium
The goals of this consortium are to: allow patients across a broad geographic range to participate in cutting-edge
clinical trials, accelerate the development of neuroblastoma and medulloblastoma
treatment by evaluating prospective new therapies faster; provide an efficient single clinical trial resource for research sponsors; expedite implementation of clinical trials by using standard documents; improve communication and resource sharing between Members and
standardize data collection; and, by all of the foregoing, advance the science of treating neuroblastoma and medulloblastoma and
communicate advancements to the medical community in a timely and efficient manner.
Currently there are 4 innovative clinical trails open in the consortium for children with relapsed neuroblastoma and medulloblastoma, with more trials planned to open in 2010.
These trails offer children new hope for a cure.

Clinical Neuroblastoma Research – IIIMIBG Radiotherapy
I-131 MIBG is one of the most effective therapies for children with relapsed neuroblastoma, with a response rate of almost 40%.
While it doesn't cure, I-131 MIBG can allow patients to gain control of their disease and, in combination with other treatments, bring them closer to being cured.
MIBG therapy is currently available in < 10 hospitals in the country.
Dr. Kraveka and Dr. Leonie Gordon in the Department of Radiology at MUSC are participating in a Phase II trial with Molecular Insight Pharmaceuticals, Inc to bring I131 MIBG therapy to MUSC.
Ultratrace™ Iobenguane I131 is a targeted radiopharmaceutical that is designed to maximize delivery of radiolabeled MIBG molecules to diagnose and treat neuroendocrine cancers such as neuroblastoma.
The proprietary Ultratrace technology minimizes the proportion of non-radioactive MIBG molecules that are delivered, resulting in a radiation therapy with very high specific activity.

Accomplishments Publications
Dihydroceramide Desaturase Activity is Modulated by Oxidative Stress” Idkowiak-Baldys J, Apraiz A, Li L, Rahmaniyan M, Clarke CJ, Kraveka JM, Asumendi A, Hannun YA. in press 2010 Biochemical Journal.
Identification of Dihydroceramide Desaturase as a Direct In-Vitro Target for Fenretinide Rahmaniyan M, Curley RW, Li L, Hannun YA, Obeid LM, Kraveka JM. Submitted for publication
Oral Presentations “Characterization of the Dihydroceramide Desaturase Enzyme and the Effects of Fenretinde
on Enzyme Activity In-Vitro” - 5th International Charleston Ceramide Conference, 2009 March 11-14, Charleston, SC.
“Association of High Ceramide Levels with Unfavorable Neuroblastoma Risk Factors: A Report from the Children’s Oncology Group”- 5th International Charleston Ceramide Conference, 2009 March 11-14, Charleston, SC.
Poster Presentations Characterization of the Dihydroceramide Desaturase Enzyme and the Effects of
Fenretinde on Enzyme Activity In-Vitro” - 100th American Association for Cancer Research Meeting (AACR), 2009 April 17- 22 Denver, CO.
“Association of High Ceramide Levels with Unfavorable Neuroblastoma Risk Factors: A Report from the Children’s Oncology Group” - 100th American Association for Cancer Research Meeting (AACR), 2009 April 17- 22 Denver, CO.
“Mechanisms of Fenretinide Sensitivity” - 11th Gordon Research Conference on Glycolipid and Sphingolipid Biology, 2010 February 7-12 Ventura, CA.
“A Phase I Trial Of TPI-287 as a Single Agent and in Combination with Temozolomide in Relapsed Neuroblastoma or Medulloblastoma” - 46th American Society for Clinical Oncology Meeting, 2010 June 4-8 Chicga0, IL

Allocation of Funds Research Technician and Post-
Doctoral Fellow’s Salaries Defray Costs of Laboratory Supplies
such as reagents, flasks, pipettes, tissue culture media, plates, enzymes
Equipment such as centrifuges and computers
Maintenance of laboratory equipment
Pay for LC/MS analysis of neuroblastoma tumors
Defray costs of microStar™ portable dosimetry readers for monitoring radiation exposures to families & staff during I-131 MIBG therapy
Education of nursing staff on I-131 MIBG therapy

THANKS FOR YOUR SUPPORT !!!
Related Documents