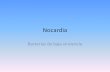
ORTHOPEDICS | ORTHOSuperSite.com ■ Case Report abstract Full article available online at ORTHOSuperSite.com. Search: 20111122-27 This article describes an immunocompetent patient with a spinal abscess that devel- oped from Nocardia asteroides. Nocardia is a rare etiology for spinal abscesses, es- pecially in immunocompetent patients. Nocardia usually affects the lungs and brain of immunocompromised individuals. Few reports of Nocardia involving bones or the spine have been published. The patient had a history of chronic back pain and had several procedures to allevi- ate the pain. In August 1997, the patient had an epidural block and a subsequent infection that was treated with antibiotics. In October 1997, she developed increas- ing back pain greater than her baseline chronic low back pain. Additional presenting symptoms were fever, chills, and nausea. On admission, magnetic resonance imaging (MRI) revealed an epidural abscess. The patient underwent irrigation and debridement. Postoperatively, the patient was initially placed on broad-spectrum antibiotics. After 38 days, the culture was identified as N asteroides, and the patient was placed on ap- propriate antibiotics. The patient has been followed with MRI prior to the discovery of the abscess and annually since the abscess due to her baseline chronic low back pain. No residual abscess was discovered. Drs West and Sun and Mr Mason are from the Department of Orthopedic Surgery, SUNY Upstate Medical University, Syracuse, New York. Dr Sun is a consultant for Seaspine and has grants pending with Amedica. Dr West and Mr Mason have no relevant financial relationships to disclose. Correspondence should be addressed to: Kristoffer R. West, MD, Department of Orthopedic Surgery, SUNY Upstate Medical University, 4400 University Hospital, 750 E Adams St, Syracuse, NY 13210 ([email protected]). doi: 10.3928/01477447-20111122-27 Nocardia Spinal Epidural Abscess: 14-year Follow-up KRISTOFFER R. WEST, MD; ROBERT C. MASON, MS; MIKE SUN, MD e128 Figure: Sagittal magnetic resonance image show- ing epidural abscess.

Nocardia Spinal Epidural Abscess: 14-year Follow-up
Aug 05, 2022
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
ORTHO0112West.inddabstract Full article available online at ORTHOSuperSite.com. Search: 20111122-27
This article describes an immunocompetent patient with a spinal abscess that devel- oped from Nocardia asteroides. Nocardia is a rare etiology for spinal abscesses, es- pecially in immunocompetent patients. Nocardia usually affects the lungs and brain of immunocompromised individuals. Few reports of Nocardia involving bones or the spine have been published.
The patient had a history of chronic back pain and had several procedures to allevi- ate the pain. In August 1997, the patient had an epidural block and a subsequent infection that was treated with antibiotics. In October 1997, she developed increas- ing back pain greater than her baseline chronic low back pain. Additional presenting symptoms were fever, chills, and nausea. On admission, magnetic resonance imaging (MRI) revealed an epidural abscess. The patient underwent irrigation and debridement. Postoperatively, the patient was initially placed on broad-spectrum antibiotics. After 38 days, the culture was identifi ed as N asteroides, and the patient was placed on ap- propriate antibiotics. The patient has been followed with MRI prior to the discovery of the abscess and annually since the abscess due to her baseline chronic low back pain. No residual abscess was discovered.
Drs West and Sun and Mr Mason are from the Department of Orthopedic Surgery, SUNY Upstate Medical University, Syracuse, New York.
Dr Sun is a consultant for Seaspine and has grants pending with Amedica. Dr West and Mr Mason have no relevant fi nancial relationships to disclose.
Correspondence should be addressed to: Kristoffer R. West, MD, Department of Orthopedic Surgery, SUNY Upstate Medical University, 4400 University Hospital, 750 E Adams St, Syracuse, NY 13210 ([email protected]).
doi: 10.3928/01477447-20111122-27
Nocardia Spinal Epidural Abscess: 14-year Follow-up KRISTOFFER R. WEST, MD; ROBERT C. MASON, MS; MIKE SUN, MD
e128
JANUARY 2012 | Volume 35 • Number 1
NOCARDIA SPINAL EPIDURAL ABSCESS | WEST ET AL
Spinal abscesses from Nocardia aster- oides are rare. Nocardia asteroides is a Gram-positive bacteria that usu-
ally affects the lungs and brain of immun- compromised hosts. Less often, it causes a cutaneous disease. The pathology shows branching and fi lamentous cells. It can be transmitted by direct inoculation or inha- lation of dust particles. The bacteria are ubiquitous and are found in soil. Nocardia asteroides is diagnosed on growth media, but it is slow growing and may need several weeks to show results. It is weakly acid-fast positive. A modifi ed Ziehl-Neelsen stain or Thayer-Martin agar can be used.
Sulfonamides are the preferred treat- ment, requiring an extended period of treatment (6 months to 1 year). Other com- binations involving sulfonamides are being evaluated to determine effi cacy due to the development of some resistant strains.
Few reports of N asteroides affecting the bones, specifi cally the spine, have been published. Graat et al1 reported a case of spinal osteomyelitis caused by Nocardia farcinica. They reported 11 cases of spinal osteomyelitis in the previ- ous 40 years.2-4
Few reports discussing N asteroides as a cause of epidural abscess exist in the lit- erature. We present a case of N asteroides as the cause of epidural abscess. Our pa- tient had a 20-year follow-up in the spine center with subsequent magnetic reso- nance imaging (MRI) due to her underly- ing chronic low back pain.
CASE REPORT A 70-year-old woman was diagnosed
with an epidural abscess in 1997. She was initially diagnosed with degenerative disk disease. Her initial MRI was performed in 1989. The patient was managed with nonsurgical treatment for her back com- plaints. Over the years, she was treated with physical therapy and nonsteroidal anti-infl ammatory drugs. In August 1996, her leg pain worsened. Electromyography was performed, which confi rmed an L5 radiculopathy. Magnetic resonance imag-
ing showed increasing spondylosis of the lumbar spine, with some stenosis. In the following months, the patient underwent thermal coagulation of posterior rami at L4-S1, neuroplasty at L5, and facet injec- tions.
In August 1997, MRI showed degen- erative disk disease and some apophyseal degenerative disease. Subsequently, she had another epidural block with a ques- tionable infection. A month later, she had a viral illness. These episodes were treated with antibiotics. She reported no subsequent increased back pain.
In October 1997, the patient devel- oped constant and surging back pain more severe than her baseline chronic back pain and reported fever, shaking chills, and nausea. On hospital admission, MRI showed an epidural abscess (Figures 1, 2). Her physical examination was unre- markable, except for positive tension sign with straight leg raise. She had no sensory or motor defi cits. Laboratory work indi- cated an erythrocyte sedimentation rate of 55 mm per hour (normal range, 0-30 mm per hour), and a white blood cell count of 10.4 K/uL (normal range, 4-10 K/uL). Two blood cultures were taken, and no growth was evident after 6 days. Reports were fi nalized at that time. She underwent formal irrigation and debride- ment, consisting of a left L5 laminotomy. Frank pus was found on exploration of the lumbar area. Further exploration re- vealed the presence of granulation tissue, likely representing a chronicity to the in- fection. The surgical incision was primar- ily closed in layers.
The patient improved dramatically af- ter the initial irrigation and debridement, eliminating the need for subsequent pro- cedures. She was started on cefazolin and gentamicin broad-spectrum intravenous antibiotics. Although cultures were still pending, Infectious Disease recommend- ed switching her to 2 g of ceftriaxone daily at discharge 3 days later.
After 22 days, the preliminary report identifi ed a Nocardia species. Nocardia
asteroides was confi rmed via the fi nal re- port at 38 days. The patient was continued on antibiotics while in the hospital and on discharge. After culture identifi cation, the patient’s antibiotics were tailored appro- priately based on the sensitivity. She had an unremarkable course on discharge but also had continued, baseline, chronic low back pain and routine annual postoperative MRIs due to the chronic low back pain. No residual epidural abscesses were noted
Figure 1: Sagittal magnetic resonance image showing epidural abscess.
Figure 2: Axial magnetic resonance image showing epidural abscess.
1
2
e129
DISCUSSION Nocardia is a rare cause of infection,
usually only affecting immunocompro- mised patients. It is most commonly found in soil, decaying vegetable matter, and aquatic environments. Nocardia is typically transmitted via inhalation of dust particles or direct contact penetrating past the natural human protective barriers.5 The most com- mon Nocardia infection is usually caused by one of the variants of the N asteroides com- plex, which consists of N asteroides sensu strico, N farcinica, and Nocardia nova.6 The 3 main types of disease caused by Nocardia (nocardiosis) are cutaneous disease, pul- monary disease, and disseminated disease. Nocardia farcinica is the most virulent form and is more frequently found to cause dis- seminated disease.
Disseminated disease is also more prevalent in immunocomprimised patients. Nocardia brasiliensis is the most common to cause cutaneous disease, often leading to the development of a mycetoma over months to years.7 The presentation in our patient is un- known. The patient’s only recollection of a
potential source was an epidural pain block that she received approximately 2 months prior to identifi cation of the abscess.
When a patient presents with back pain, a spinal epidural abscess is a rare cause and not likely to be in the initial dif- ferential diagnosis. An indicator that an abscess could be present is when a patient presents with the classic triad of fever, spi- nal pain, and neurologic defi cit.8-10 Fever often leads clinicians to include a spinal epidural abscess in the differential diag- nosis because it is typically absent in the more common presentations of back pain.
Once a spinal epidural abscess is determined as the cause, the contami- nants in order of likelihood range from Staphylococcus aureus (approximately two-thirds of the total cases), Gram- negative bacilli, streptococci, coagulase- negative staphylococci (mostly in patients with previous spinal instrumentation), and anaerobes.11-13 Nocardia is another poten- tial cause of epidural abcesses.
The likelihood of infection with this type of bacteria is minimal but should be considered. Increased concerns for no- cardiosis typically involves patients with
depressed cellular immunity or humor- ally immunocompromised patients, such as those with acquired immune defi ciency syndrome, hematologic and solid organ malignancies, prolonged systemic ste- roid therapy, and transplant recipients.14 However, immunocompetent individuals are still capable of developing an infection. The overall incidence of nocardiosis is of- ten not reported in literature, with the most frequently cited study in the United States reporting 500 to 1000 new cases per year between 1972 and 1974.15 These numbers have likely increased since then due to the increase in immunocomprimised individu- als and likely lack reporting in the initial count because it is not a reportable disease. Although the incidence is limited, it should remain in the differential diagnosis, espe- cially when cultures are still negative after a few days and the clinical suspicion of in- fection is high.
It is diffi cult to diagnose Nocardia because of its long incubation period. The typical time frame for growth can be as early as 4 days, but it can take sev- eral weeks for the colonies to develop. In our case, it took 22 days for the colonies to grow, with a fi nal report at 38 days. Correspondence with the laboratory is vi- tal when Nocardia is being considered to ensure that cultures are kept long enough to allow for ample growth periods.
Figure 3: Sagittal magnetic resonance image showing no residual abscess.
Figure 4: Anteroposterior lumbar spine radiograph.
Figure 5: Lateral spine/lumbar radiograph.
3
4
5
e130
NOCARDIA SPINAL EPIDURAL ABSCESS | WEST ET AL
Nocardia is grown in the laboratory using common fungal (ie, Sabouraud dex- trose agar) or mycobacterial isolation me- dia (ie, Middlebrook synthetic agar and Lowenstein-Jensen medium).16 Selective media, such as Thayer-Martin agar, can be used to increase the yield.14 The stains that are used to differentiate Nocardia from Actinomyces are the Kinyoun acid- fast stain or a Ziehl-Neelsen acid-fast stain. The Lysozyme test can also be used to identify Nocardia species that is ben- efi cial for those species which are not acid fast. Nocardia is identifi ed as weak- ly acid-fast positive vs its counterpart, Actinomyces, which is an acid-fast nega- tive. The property that causes the differen- tiation of Nocardia is the varying amounts of mycolic acid within its cell wall caus- ing the acid-fast staining.16
Antibiotics are the treatment of choice, except when surgery is initially indicated, with antibiotics still given postoperatively. Sulfonamides have been the preferred antibiotic used for treat- ment for many years. Due to resistance developing to sulfonamides in many variants of Nocardia, a combination therapy is often given, especially in se- vere or disseminated disease. To ensure coverage of all isolates of Nocardia in severe cases, a 3-drug regimen of tri- methoprim-sulfamethoxazole, amika- cin, and either ceftriaxone or imipenem should be started because no resistance has been reported to this combina- tion.17,18 In milder cases, treatment with trimethoprim-sulfamethoxazole, mino- cycline, or ceftriaxone have shown to be effective. Treatment with trimethoprim- sulfamethoxazole in combination with a fl ouroquinolone has also been effective, but only in mild cases.
Nocardia farcinica is the 1 type of Nocardia that should be of concern when treating empirically with a fl ouroquino- lone because most patients are resistant to it. Nocardia farcinica has also shown resistance to third-generation cephalospo- rins.18 Linezolid has demonstrated effec-
tive in vitro activity against most species and strains, but clinical data are limited. It has promising results as a potential option in the replacement of the current treatment regimens when resistance is a concern.19,20 Once sensitivities are ob- tained, the focus of the treatment should be narrowed appropriately. Intravenous therapy treatment must be continued for several weeks with an eventual transition to oral therapy. Duration of treatment is dependent on type of disease and organ involvement.14
Few reports of patients with Nocardia infections have been published. This article presents a long-term follow-up of a patient who was diagnosed with a N asteroides spinal epidural abscess treated successfully with irrigation and debridement and intra- venous antibiotics. She had MRIs on a con- sistent basis both pre- and postoperatively for 20 years. When treating patients with a possible spine infection, one should in- clude Nocardia in the differential diagno- sis. This patient had her fi rst MRI in 1989, but she was not diagnosed with the infec- tion until 1997. Since the infection and subsequent irrigation and debridement, the patient has had several MRIs. Early post- operative MRIs show no accumulation of abscess. This trend continued with the re- mainder of the MRIs.
REFERENCES: 1. Graat HC, Van Ooij A, Day GA, McPhee
IB. Nocardia farcinica spinal osteomyeli- tis. Spine (Phila Pa 1976). 2002; 27(10): E253-E257.
2. Awad I, Bay JW, Petersen JM. Nocardial osteomyelitis of the spine with epidural spinal cord compression–a case report. Neurosurgery. 1984; 15(2):254-256.
3. Epstein S, Holden M, Feldshuh J, Singer JM. Unusual cause of spinal cord compression: nocardiosis. N Y State J Med. 1963; 63:3422- 3427.
4. Vander Heiden T, Stahel PF, Clutter S, et al. Nocardia osteomyelitis: a rare complica- tion after intramedullary nailing of a closed tibial shaft fracture. J Orthop Trauma. 2009; 23(3):232-236.
5. Goodfellow M, Williams ST. Ecology of ac- tinomycetes. Annu Rev Microbiol. 1983; 37: 189-216.
6. Saubolle MA, Sussland D. Nocardiosis: a re- view of clinical and laboratory experience. J Clin Microbiol. 2003; 41(10):4497-4501.
7. Satterwhite TK, Wallace RJ Jr. Primary cuta- neous nocardiosis. JAMA. 1979; 242(4):333- 336.
8. Chen WC, Wang JL, Wang JT, Chen YC, Chang SC. Spinal epidural abscess due to Staphylococcus aureus: clinical manifesta- tions and outcomes. J Microbiol Immunol Infect. 2008; 41(3):215-221.
9. Davis DP, Wold RM, Patel RJ, et al. The clinical presentation and impact of diagnos- tic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004; 26(3):285-291.
10. Curry WT Jr, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: clini- cal presentation, management, and outcome. Surg Neurol. 2005; 63(4):364-371.
11. Danner RL, Hartman BJ. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987; 9(2):265-274.
12. Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL. Spinal epidural abscess: a report of 40 cases and re- view. Surg Neurol. 1992; 38(3):225-231.
13. Gellin BG, Weingarten K, Gamache FW Jr, et al. Epidural abscess. In: Scheld WM, Whitley RJ, Durack DT, eds. Infections of the Central Nervous System. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1997:507.
14. Ambrosioni J, Lew D, Garbino J. Nocardiosis: updated clinical review and ex- perience at a tertiary center [published online ahead of print March 20, 2010]. Infection. 2010; 38(2):89-97.
15. Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the Unitied States, 1972-1974. J Infect Dis. 1976; 134(4):286-289.
16. Winn W Jr, Allen S, Janda W. Aerobic ac- tinomycetes. In: Winn W Jr, Allen S, Janda W, et al, eds. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:858-874.
17. Lerner Pl: Nocardiosis. Clin Infect Dis. 1996; 22(6):891-903.
18. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory fea- tures for the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006; 19(2):259-282.
19. Brown-Elliot BA, Ward SC, Crist CJ, Mann LB, Wilson RW, Wallace RJ Jr. In vitro ac- tivities of linezolid against multiple Nocardia species. Antimicrob Agents Chemother. 2001; 45(4):1295-1297.
20. Moylett EH, Pacheco SE, Brown-Elliot BA, et al. Clinical experience with linezolid for treatment of nocardia infection [published online ahead of print January 13, 2003]. Clin Infect Dis. 2003; 36(3):313-318.
e131
This article describes an immunocompetent patient with a spinal abscess that devel- oped from Nocardia asteroides. Nocardia is a rare etiology for spinal abscesses, es- pecially in immunocompetent patients. Nocardia usually affects the lungs and brain of immunocompromised individuals. Few reports of Nocardia involving bones or the spine have been published.
The patient had a history of chronic back pain and had several procedures to allevi- ate the pain. In August 1997, the patient had an epidural block and a subsequent infection that was treated with antibiotics. In October 1997, she developed increas- ing back pain greater than her baseline chronic low back pain. Additional presenting symptoms were fever, chills, and nausea. On admission, magnetic resonance imaging (MRI) revealed an epidural abscess. The patient underwent irrigation and debridement. Postoperatively, the patient was initially placed on broad-spectrum antibiotics. After 38 days, the culture was identifi ed as N asteroides, and the patient was placed on ap- propriate antibiotics. The patient has been followed with MRI prior to the discovery of the abscess and annually since the abscess due to her baseline chronic low back pain. No residual abscess was discovered.
Drs West and Sun and Mr Mason are from the Department of Orthopedic Surgery, SUNY Upstate Medical University, Syracuse, New York.
Dr Sun is a consultant for Seaspine and has grants pending with Amedica. Dr West and Mr Mason have no relevant fi nancial relationships to disclose.
Correspondence should be addressed to: Kristoffer R. West, MD, Department of Orthopedic Surgery, SUNY Upstate Medical University, 4400 University Hospital, 750 E Adams St, Syracuse, NY 13210 ([email protected]).
doi: 10.3928/01477447-20111122-27
Nocardia Spinal Epidural Abscess: 14-year Follow-up KRISTOFFER R. WEST, MD; ROBERT C. MASON, MS; MIKE SUN, MD
e128
JANUARY 2012 | Volume 35 • Number 1
NOCARDIA SPINAL EPIDURAL ABSCESS | WEST ET AL
Spinal abscesses from Nocardia aster- oides are rare. Nocardia asteroides is a Gram-positive bacteria that usu-
ally affects the lungs and brain of immun- compromised hosts. Less often, it causes a cutaneous disease. The pathology shows branching and fi lamentous cells. It can be transmitted by direct inoculation or inha- lation of dust particles. The bacteria are ubiquitous and are found in soil. Nocardia asteroides is diagnosed on growth media, but it is slow growing and may need several weeks to show results. It is weakly acid-fast positive. A modifi ed Ziehl-Neelsen stain or Thayer-Martin agar can be used.
Sulfonamides are the preferred treat- ment, requiring an extended period of treatment (6 months to 1 year). Other com- binations involving sulfonamides are being evaluated to determine effi cacy due to the development of some resistant strains.
Few reports of N asteroides affecting the bones, specifi cally the spine, have been published. Graat et al1 reported a case of spinal osteomyelitis caused by Nocardia farcinica. They reported 11 cases of spinal osteomyelitis in the previ- ous 40 years.2-4
Few reports discussing N asteroides as a cause of epidural abscess exist in the lit- erature. We present a case of N asteroides as the cause of epidural abscess. Our pa- tient had a 20-year follow-up in the spine center with subsequent magnetic reso- nance imaging (MRI) due to her underly- ing chronic low back pain.
CASE REPORT A 70-year-old woman was diagnosed
with an epidural abscess in 1997. She was initially diagnosed with degenerative disk disease. Her initial MRI was performed in 1989. The patient was managed with nonsurgical treatment for her back com- plaints. Over the years, she was treated with physical therapy and nonsteroidal anti-infl ammatory drugs. In August 1996, her leg pain worsened. Electromyography was performed, which confi rmed an L5 radiculopathy. Magnetic resonance imag-
ing showed increasing spondylosis of the lumbar spine, with some stenosis. In the following months, the patient underwent thermal coagulation of posterior rami at L4-S1, neuroplasty at L5, and facet injec- tions.
In August 1997, MRI showed degen- erative disk disease and some apophyseal degenerative disease. Subsequently, she had another epidural block with a ques- tionable infection. A month later, she had a viral illness. These episodes were treated with antibiotics. She reported no subsequent increased back pain.
In October 1997, the patient devel- oped constant and surging back pain more severe than her baseline chronic back pain and reported fever, shaking chills, and nausea. On hospital admission, MRI showed an epidural abscess (Figures 1, 2). Her physical examination was unre- markable, except for positive tension sign with straight leg raise. She had no sensory or motor defi cits. Laboratory work indi- cated an erythrocyte sedimentation rate of 55 mm per hour (normal range, 0-30 mm per hour), and a white blood cell count of 10.4 K/uL (normal range, 4-10 K/uL). Two blood cultures were taken, and no growth was evident after 6 days. Reports were fi nalized at that time. She underwent formal irrigation and debride- ment, consisting of a left L5 laminotomy. Frank pus was found on exploration of the lumbar area. Further exploration re- vealed the presence of granulation tissue, likely representing a chronicity to the in- fection. The surgical incision was primar- ily closed in layers.
The patient improved dramatically af- ter the initial irrigation and debridement, eliminating the need for subsequent pro- cedures. She was started on cefazolin and gentamicin broad-spectrum intravenous antibiotics. Although cultures were still pending, Infectious Disease recommend- ed switching her to 2 g of ceftriaxone daily at discharge 3 days later.
After 22 days, the preliminary report identifi ed a Nocardia species. Nocardia
asteroides was confi rmed via the fi nal re- port at 38 days. The patient was continued on antibiotics while in the hospital and on discharge. After culture identifi cation, the patient’s antibiotics were tailored appro- priately based on the sensitivity. She had an unremarkable course on discharge but also had continued, baseline, chronic low back pain and routine annual postoperative MRIs due to the chronic low back pain. No residual epidural abscesses were noted
Figure 1: Sagittal magnetic resonance image showing epidural abscess.
Figure 2: Axial magnetic resonance image showing epidural abscess.
1
2
e129
DISCUSSION Nocardia is a rare cause of infection,
usually only affecting immunocompro- mised patients. It is most commonly found in soil, decaying vegetable matter, and aquatic environments. Nocardia is typically transmitted via inhalation of dust particles or direct contact penetrating past the natural human protective barriers.5 The most com- mon Nocardia infection is usually caused by one of the variants of the N asteroides com- plex, which consists of N asteroides sensu strico, N farcinica, and Nocardia nova.6 The 3 main types of disease caused by Nocardia (nocardiosis) are cutaneous disease, pul- monary disease, and disseminated disease. Nocardia farcinica is the most virulent form and is more frequently found to cause dis- seminated disease.
Disseminated disease is also more prevalent in immunocomprimised patients. Nocardia brasiliensis is the most common to cause cutaneous disease, often leading to the development of a mycetoma over months to years.7 The presentation in our patient is un- known. The patient’s only recollection of a
potential source was an epidural pain block that she received approximately 2 months prior to identifi cation of the abscess.
When a patient presents with back pain, a spinal epidural abscess is a rare cause and not likely to be in the initial dif- ferential diagnosis. An indicator that an abscess could be present is when a patient presents with the classic triad of fever, spi- nal pain, and neurologic defi cit.8-10 Fever often leads clinicians to include a spinal epidural abscess in the differential diag- nosis because it is typically absent in the more common presentations of back pain.
Once a spinal epidural abscess is determined as the cause, the contami- nants in order of likelihood range from Staphylococcus aureus (approximately two-thirds of the total cases), Gram- negative bacilli, streptococci, coagulase- negative staphylococci (mostly in patients with previous spinal instrumentation), and anaerobes.11-13 Nocardia is another poten- tial cause of epidural abcesses.
The likelihood of infection with this type of bacteria is minimal but should be considered. Increased concerns for no- cardiosis typically involves patients with
depressed cellular immunity or humor- ally immunocompromised patients, such as those with acquired immune defi ciency syndrome, hematologic and solid organ malignancies, prolonged systemic ste- roid therapy, and transplant recipients.14 However, immunocompetent individuals are still capable of developing an infection. The overall incidence of nocardiosis is of- ten not reported in literature, with the most frequently cited study in the United States reporting 500 to 1000 new cases per year between 1972 and 1974.15 These numbers have likely increased since then due to the increase in immunocomprimised individu- als and likely lack reporting in the initial count because it is not a reportable disease. Although the incidence is limited, it should remain in the differential diagnosis, espe- cially when cultures are still negative after a few days and the clinical suspicion of in- fection is high.
It is diffi cult to diagnose Nocardia because of its long incubation period. The typical time frame for growth can be as early as 4 days, but it can take sev- eral weeks for the colonies to develop. In our case, it took 22 days for the colonies to grow, with a fi nal report at 38 days. Correspondence with the laboratory is vi- tal when Nocardia is being considered to ensure that cultures are kept long enough to allow for ample growth periods.
Figure 3: Sagittal magnetic resonance image showing no residual abscess.
Figure 4: Anteroposterior lumbar spine radiograph.
Figure 5: Lateral spine/lumbar radiograph.
3
4
5
e130
NOCARDIA SPINAL EPIDURAL ABSCESS | WEST ET AL
Nocardia is grown in the laboratory using common fungal (ie, Sabouraud dex- trose agar) or mycobacterial isolation me- dia (ie, Middlebrook synthetic agar and Lowenstein-Jensen medium).16 Selective media, such as Thayer-Martin agar, can be used to increase the yield.14 The stains that are used to differentiate Nocardia from Actinomyces are the Kinyoun acid- fast stain or a Ziehl-Neelsen acid-fast stain. The Lysozyme test can also be used to identify Nocardia species that is ben- efi cial for those species which are not acid fast. Nocardia is identifi ed as weak- ly acid-fast positive vs its counterpart, Actinomyces, which is an acid-fast nega- tive. The property that causes the differen- tiation of Nocardia is the varying amounts of mycolic acid within its cell wall caus- ing the acid-fast staining.16
Antibiotics are the treatment of choice, except when surgery is initially indicated, with antibiotics still given postoperatively. Sulfonamides have been the preferred antibiotic used for treat- ment for many years. Due to resistance developing to sulfonamides in many variants of Nocardia, a combination therapy is often given, especially in se- vere or disseminated disease. To ensure coverage of all isolates of Nocardia in severe cases, a 3-drug regimen of tri- methoprim-sulfamethoxazole, amika- cin, and either ceftriaxone or imipenem should be started because no resistance has been reported to this combina- tion.17,18 In milder cases, treatment with trimethoprim-sulfamethoxazole, mino- cycline, or ceftriaxone have shown to be effective. Treatment with trimethoprim- sulfamethoxazole in combination with a fl ouroquinolone has also been effective, but only in mild cases.
Nocardia farcinica is the 1 type of Nocardia that should be of concern when treating empirically with a fl ouroquino- lone because most patients are resistant to it. Nocardia farcinica has also shown resistance to third-generation cephalospo- rins.18 Linezolid has demonstrated effec-
tive in vitro activity against most species and strains, but clinical data are limited. It has promising results as a potential option in the replacement of the current treatment regimens when resistance is a concern.19,20 Once sensitivities are ob- tained, the focus of the treatment should be narrowed appropriately. Intravenous therapy treatment must be continued for several weeks with an eventual transition to oral therapy. Duration of treatment is dependent on type of disease and organ involvement.14
Few reports of patients with Nocardia infections have been published. This article presents a long-term follow-up of a patient who was diagnosed with a N asteroides spinal epidural abscess treated successfully with irrigation and debridement and intra- venous antibiotics. She had MRIs on a con- sistent basis both pre- and postoperatively for 20 years. When treating patients with a possible spine infection, one should in- clude Nocardia in the differential diagno- sis. This patient had her fi rst MRI in 1989, but she was not diagnosed with the infec- tion until 1997. Since the infection and subsequent irrigation and debridement, the patient has had several MRIs. Early post- operative MRIs show no accumulation of abscess. This trend continued with the re- mainder of the MRIs.
REFERENCES: 1. Graat HC, Van Ooij A, Day GA, McPhee
IB. Nocardia farcinica spinal osteomyeli- tis. Spine (Phila Pa 1976). 2002; 27(10): E253-E257.
2. Awad I, Bay JW, Petersen JM. Nocardial osteomyelitis of the spine with epidural spinal cord compression–a case report. Neurosurgery. 1984; 15(2):254-256.
3. Epstein S, Holden M, Feldshuh J, Singer JM. Unusual cause of spinal cord compression: nocardiosis. N Y State J Med. 1963; 63:3422- 3427.
4. Vander Heiden T, Stahel PF, Clutter S, et al. Nocardia osteomyelitis: a rare complica- tion after intramedullary nailing of a closed tibial shaft fracture. J Orthop Trauma. 2009; 23(3):232-236.
5. Goodfellow M, Williams ST. Ecology of ac- tinomycetes. Annu Rev Microbiol. 1983; 37: 189-216.
6. Saubolle MA, Sussland D. Nocardiosis: a re- view of clinical and laboratory experience. J Clin Microbiol. 2003; 41(10):4497-4501.
7. Satterwhite TK, Wallace RJ Jr. Primary cuta- neous nocardiosis. JAMA. 1979; 242(4):333- 336.
8. Chen WC, Wang JL, Wang JT, Chen YC, Chang SC. Spinal epidural abscess due to Staphylococcus aureus: clinical manifesta- tions and outcomes. J Microbiol Immunol Infect. 2008; 41(3):215-221.
9. Davis DP, Wold RM, Patel RJ, et al. The clinical presentation and impact of diagnos- tic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004; 26(3):285-291.
10. Curry WT Jr, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: clini- cal presentation, management, and outcome. Surg Neurol. 2005; 63(4):364-371.
11. Danner RL, Hartman BJ. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987; 9(2):265-274.
12. Nussbaum ES, Rigamonti D, Standiford H, Numaguchi Y, Wolf AL, Robinson WL. Spinal epidural abscess: a report of 40 cases and re- view. Surg Neurol. 1992; 38(3):225-231.
13. Gellin BG, Weingarten K, Gamache FW Jr, et al. Epidural abscess. In: Scheld WM, Whitley RJ, Durack DT, eds. Infections of the Central Nervous System. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1997:507.
14. Ambrosioni J, Lew D, Garbino J. Nocardiosis: updated clinical review and ex- perience at a tertiary center [published online ahead of print March 20, 2010]. Infection. 2010; 38(2):89-97.
15. Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the Unitied States, 1972-1974. J Infect Dis. 1976; 134(4):286-289.
16. Winn W Jr, Allen S, Janda W. Aerobic ac- tinomycetes. In: Winn W Jr, Allen S, Janda W, et al, eds. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:858-874.
17. Lerner Pl: Nocardiosis. Clin Infect Dis. 1996; 22(6):891-903.
18. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory fea- tures for the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006; 19(2):259-282.
19. Brown-Elliot BA, Ward SC, Crist CJ, Mann LB, Wilson RW, Wallace RJ Jr. In vitro ac- tivities of linezolid against multiple Nocardia species. Antimicrob Agents Chemother. 2001; 45(4):1295-1297.
20. Moylett EH, Pacheco SE, Brown-Elliot BA, et al. Clinical experience with linezolid for treatment of nocardia infection [published online ahead of print January 13, 2003]. Clin Infect Dis. 2003; 36(3):313-318.
e131
Related Documents







![Epidural steroid injections: our experience and a review of the ......Infectious Epidural abscess, Discitis, Osteomyelitis [38-45] Intravascular injection Intravenous or Intraarterial](https://static.cupdf.com/doc/110x72/60df39605510cf3a1862f983/epidural-steroid-injections-our-experience-and-a-review-of-the-infectious.jpg)



