ORIGINAL ARTICLE: Clinical Endoscopy Narrow-band imaging without high magnification to differentiate polyps during real-time colonoscopy: improvement with experience Jason N. Rogart, MD, Dhanpat Jain, MD, Uzma D. Siddiqui, MD, Tal Oren, MD, Joseph Lim, MD, Priya Jamidar, MD, Harry Aslanian, MD New Haven, Connecticut, USA Background: There is no widely adopted, easily applied method for distinguishing between adenomatous and nonadenomatous polyps during real-time colonoscopy. Objective: To compare white light (WL) with narrow-band imaging (NBI) for the differentiation of colorectal polyps in vivo and to assess for a learning curve. Design: A prospective polyp series. Patients and Setting: A total of 302 patients referred for colonoscopy, between August 2006 and July 2007, to a single tertiary-referral center in the United States. Intervention: Standard WL colonoscopy was performed with Olympus 180-series colonoscopes. Each detected polyp was first characterized by WL and then by NBI. Modified Kudo pit pattern and vascular color intensity (VCI) were recorded, and the histology was predicted. Endoscopists were given feedback every 2 weeks. Main Outcome Measurements: Overall accuracy and sensitivity and specificity of endoscopic diagnosis by using WL alone and with NBI, as well as improvement in endoscopists’ performance. Results: A total of 265 polyps were found in 131 patients. Diagnostic accuracy was 80% with NBI and 77% with WL (P Z .35). NBI performed better than WL in diagnosing adenomas (sensitivity 80% vs 69%, P ! .05). Nonadenomatous polyps were more likely to have a ‘‘light’’ VCI compared with adenomas (71% vs 29%, P ! .001). During the second half of the study, NBI accuracy improved, from 74% to 87%, and outperformed an unchanged WL accuracy of 79% (P ! .05). Conclusions: Overall, NBI was not more accurate than WL in differentiating colorectal polyps in vivo; however, once a learning curve was achieved, NBI performed significantly better. Further refinements of an NBI pit- pattern classification and VCI scale are needed before broad application to clinical decisions regarding the necessity of polypectomy. (Gastrointest Endosc 2008;68:1136-45.) During colonoscopy, two main types of polyps are en- countered: adenomatous polyps, which carry a significant lifetime risk of malignancy if not removed, and nonade- nomatous polyps (variably termed as ‘‘hyperplastic polyps’’ or ‘‘serrated polyps’’). Traditionally, nonadenoma- tous polyps have been considered to have little if any ma- lignant potential and, per current guidelines, their presence does not generally warrant shortened colon-can- cer screening intervals in patients without polyposis syndromes. 1,2 Endoscopic methods to assist in distinguishing be- tween these two types of polyps have been difficult to ap- ply and interpret. High-magnification chromoendoscopy has not gained widespread acceptance in Western coun- tries, because dye application is labor intensive and most endoscopists are not familiar with their use and interpre- tation. 3,4 Confocal endomicroscopy is not widely available, and interpretation requires special training. Most endo- scopists currently remove all of the polyps they encounter Abbreviations: ACF, aberrant crypt foci; CCD, charge-coupled device; HD, high definition; NBI, narrow-band imaging; SSP, sessile serrated polyps; VCI, vascular color intensity; WL, white light. Copyright ª 2008 by the American Society for Gastrointestinal Endoscopy 0016-5107/$34.00 doi:10.1016/j.gie.2008.04.035 1136 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008 www.giejournal.org

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
ORIGINAL ARTICLE: Clinical Endoscopy
Narrow-band imaging without high magnification to differentiatepolyps during real-time colonoscopy: improvement withexperience
Jason N. Rogart, MD, Dhanpat Jain, MD, Uzma D. Siddiqui, MD, Tal Oren, MD, Joseph Lim, MD,Priya Jamidar, MD, Harry Aslanian, MD
New Haven, Connecticut, USA
Background: There is no widely adopted, easily applied method for distinguishing between adenomatous andnonadenomatous polyps during real-time colonoscopy.
Objective: To compare white light (WL) with narrow-band imaging (NBI) for the differentiation of colorectalpolyps in vivo and to assess for a learning curve.
Design: A prospective polyp series.
Patients and Setting: A total of 302 patients referred for colonoscopy, between August 2006 and July 2007, toa single tertiary-referral center in the United States.
Intervention: Standard WL colonoscopy was performed with Olympus 180-series colonoscopes. Each detectedpolyp was first characterized by WL and then by NBI. Modified Kudo pit pattern and vascular color intensity(VCI) were recorded, and the histology was predicted. Endoscopists were given feedback every 2 weeks.
Main Outcome Measurements: Overall accuracy and sensitivity and specificity of endoscopic diagnosis byusing WL alone and with NBI, as well as improvement in endoscopists’ performance.
Results: A total of 265 polyps were found in 131 patients. Diagnostic accuracy was 80% with NBI and 77% withWL (P Z .35). NBI performed better than WL in diagnosing adenomas (sensitivity 80% vs 69%, P ! .05).Nonadenomatous polyps were more likely to have a ‘‘light’’ VCI compared with adenomas (71% vs 29%,P ! .001). During the second half of the study, NBI accuracy improved, from 74% to 87%, and outperformedan unchanged WL accuracy of 79% (P ! .05).
Conclusions: Overall, NBI was not more accurate than WL in differentiating colorectal polyps in vivo; however,once a learning curve was achieved, NBI performed significantly better. Further refinements of an NBI pit-pattern classification and VCI scale are needed before broad application to clinical decisions regarding thenecessity of polypectomy. (Gastrointest Endosc 2008;68:1136-45.)
During colonoscopy, two main types of polyps are en-countered: adenomatous polyps, which carry a significantlifetime risk of malignancy if not removed, and nonade-nomatous polyps (variably termed as ‘‘hyperplasticpolyps’’ or ‘‘serrated polyps’’). Traditionally, nonadenoma-tous polyps have been considered to have little if any ma-
Abbreviations: ACF, aberrant crypt foci; CCD, charge-coupled device;
HD, high definition; NBI, narrow-band imaging; SSP, sessile serrated
polyps; VCI, vascular color intensity; WL, white light.
Copyright ª 2008 by the American Society for Gastrointestinal Endoscopy
0016-5107/$34.00
doi:10.1016/j.gie.2008.04.035
1136 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008
lignant potential and, per current guidelines, theirpresence does not generally warrant shortened colon-can-cer screening intervals in patients without polyposissyndromes.1,2
Endoscopic methods to assist in distinguishing be-tween these two types of polyps have been difficult to ap-ply and interpret. High-magnification chromoendoscopyhas not gained widespread acceptance in Western coun-tries, because dye application is labor intensive and mostendoscopists are not familiar with their use and interpre-tation.3,4 Confocal endomicroscopy is not widely available,and interpretation requires special training. Most endo-scopists currently remove all of the polyps they encounter
www.giejournal.org
Rogart et al Narrow-band imaging to differentiate colorectal polyps
and submit them for histologic analysis. The unnecessaryremoval of nonadenomatous polyps results in a prolongedprocedure time, increased risk, and increased costs re-lated to the instruments used for polypectomy, the physi-cian fee, specimen processing, and histopathologicinterpretation.
Narrow-band imaging (NBI) is a new optical technologythat uses optical interference filters that spectrally narrowthe bandwidths used in conventional white light (WL)(red-green-blue) medical videoendoscopy. NBI preferen-tially uses and narrows the shorter blue-light and green-light spectrums, which has 2 effects: (a) light does notpenetrate the mucosa as deeply and, therefore, providesmore visual detail to the superficial mucosal structures,and (b) absorption of blue light by hemoglobin withinsuperficial capillaries makes their observation possible asbrownish markings, usually in neoplastic tissue.5,6
Initial pilot studies identified a relatively high diagnos-tic accuracy for NBI in predicting colon polyp histology7
when using Kudo’s ‘‘pit-pattern’’ classification, whichwas developed with the use of chromoendoscopy.8-10 Inthis prospective trial, we aimed to compare standardbroadband WL with NBI for the differentiation of colorec-tal polyps during real-time colonoscopy by using a combi-nation of a modified Kudo pit-pattern classification andvascular color intensity (VCI) grading. We also sought toassess the learning curve for NBI when used to character-ize colorectal polyps.
PATIENTS AND METHODS
NBI and pit-pattern educationFour experienced endoscopists, with a minimum num-
ber of 1000 colonoscopies previously performed (range1000-10,000), participated in this study. Before enrollingpatients, they attended a 1-hour interactive lecture onNBI and were provided with an atlas of endoscopic imagesof polyps examined with both chromoendoscopy and NBI.Instruction on the study design was also given, includinga simplified Kudo pit-pattern classification and VCI grad-ing (see below). Laminated reference sheets for these clas-sifications, with pictures and sketches, were posted ineach endoscopy room.
On a separate day, each endoscopist completed a pre-test that consisted of 20 unknown polyps photographedwith the NBI system described below. Throughout thestudy period, endoscopists received feedback every 2weeks about the accuracy of their endoscopic predictionscompared with the histopathologic diagnosis. After enroll-ment was completed, the same endoscopists completeda posttest that involved the same 20 unknown polyps,which were randomly reordered. Before initiating thestudy, we planned to assess endoscopists’ individual andgroup accuracy in the first and second halves of the study.The halfway point in the study was determined after com-
www.giejournal.org
Capsule Summary
What is already known on this topic
d Endoscopic methods to distinguish adenomatous fromnonadenomatous polyps have been difficult to apply andinterpret.
What this study adds to our knowledge
d In a prospective series of 265 polyps in 131 patients,narrow-band imaging (NBI) was not more accurate thanbroadband white-light colonoscopy in differentiatingcolorectal polyps in vivo, but once a learning curve wasachieved, NBI performed significantly better.
pletion of study enrollment by dividing in half the totalnumber of polyps removed by each endoscopist.
PatientsFrom August 2006 to July 2007, consecutive individuals
referred for routine colonoscopy to one of the study phy-sicians at Yale University were invited to participate in thestudy. Exclusion criteria included patients with known orsuspected familial polyposis syndromes, those seen withacute GI bleeding, and those with an internationalnormalized ratio greater than 2.0 or platelets less than50,000/mm3. Informed consent was obtained from eachpatient before colonoscopy. The study was approved bythe human investigation committee of Yale UniversitySchool of Medicine.
NBI systemOlympus CF-H180AL colonoscopes (Olympus Corp,
Center Valley, Pa) were used with Evis Exera II CV-180 pro-cessors (Olympus). This system uses a xenon lamp as alight source and a color charge-coupled device (CCD),and provides a high-definition (HD) picture (1080 hori-zontal lines of resolution) when used with an HD monitor.The double-band NBI filter (415 nm and 540 nm � 30 nm)is activated by pushing a button on the handle of thecolonoscope and is deactivated by pushing the same but-ton. It takes approximately 1 to 2 seconds for the image tochange on the monitor. The processor is also equippedwith a �1.5 electronic magnification feature that can beactivated with a separate button on the colonoscopeand provides up to �70 total magnification.
Colonoscopy and polyp-assessment protocolAll patients underwent a standard bowel preparation
with either a polyethylene glycol–electrolyte lavage solu-tion or oral sodium phosphate. A routine colonoscopywas performed to the cecum by using standard, broad-band WL. When a polyp was encountered, the location,size, and shape were recorded. The image was electroni-cally magnified to �1.5 the standard magnification, and
Volume 68, No. 6 : 2008 GASTROINTESTINAL ENDOSCOPY 1137
Narrow-band imaging to differentiate colorectal polyps Rogart et al
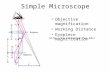
the endoscopist predicted the polyp type (adenoma, can-cer, or nonadenomatous) and the endoscopist’s level ofconfidence (low or high). Under the same magnification,NBI was activated, and the polyp was reevaluated. Endo-scopists were asked to classify the polyp as modifiedKudo A (Kudo pit-pattern I or II) or Kudo B (Kudo pit-pat-terns III-V) (Fig. 1) and then to specify a specific pit-pat-tern (I-V). Kudo A suggests nonadenomatous, whereasKudo B suggests adenomatous polyp or cancer.
The VCI was graded by examining the mucosal hue ofthe polyp under NBI: light (same color as surroundingmucosa), medium (mildly darker than surrounding mu-cosa, overall light-brown appearance), and dark (muchdarker than surrounding mucosa, dark brown or blackin appearance). Image quality (good, fair, or poor) wasalso recorded. A final prediction of polyp histology andconfidence level was then made based on a summationof all of the information gathered. The polyp was photo-graphed under WL and NBI, and removed with a snareor a biopsy forceps. This process was repeated for eachpolyp identified during colonoscopy.
Histologic analysisSpecimens collected in 10% buffered formalin were
routinely processed, paraffin embedded, and sectionedat 4 mm. They were stained with hematoxylin and eosinand examined by 2 pathologists, with either expertise orspecial interest in GI pathology, who were blinded to theendoscopic images and predictions. The cases were classi-fied as adenomatous polyps (tubular adenomas, villousadenomas, and tubulovillous adenomas), serrated polyps,lymphoglandular complexes, aberrant crypt foci,11 ormiscellaneous. Polyps initially placed in the serrated cate-gory were further subclassifed and defined as serratedadenoma, sessile serrated polyp (SSP), or hyperplasticpolyp.12,13 Serrated adenomas show dysplasia similar to ad-enomatous polyps and were grouped with adenomatouspolyps for the analysis. Aberrant crypt foci (ACF) were de-fined as nondysplastic lesions that were characterized byslightly elongated crypts, with larger and/or irregularlumina, but histologically lacking diagnostic features of ad-enomatous polyps or hyperplastic polyps. If the initial diag-nosis of the 2 pathologists was discordant, then the case inquestion was simultaneously reexamined at a 2-headedmicroscope by both pathologists, and a consensus wasreached. In the event that the initial sections appeared nor-mal or did not reveal a specific diagnosis, multiple deepersections (18-30 sections) were obtained from the storedparaffin block until the entire tissue was exhausted.
StatisticsThe Student t test was used to analyze continuous vari-
ables and outcomes. The c2 test or the Fisher exact testwas used for categorical variables and outcomes. The Ftest was used to determine differences in variances. Gen-eralized kappa statistics were calculated to assess interob-
1138 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008
server agreement for the pretests and posttests.14 A Pvalue less than .05 was considered statistically significant.
RESULTS
Polyps detectedA total of 302 patients were enrolled. A total of 265
polyps were found in 131 patients. Ninety-one patientshad at least one adenoma or carcinoma, which representsan adenoma detection rate of 30%. The cecal intubationrate was 96%. The demographics of patients with polypsare shown in Table 1. A breakdown of the histologic diag-noses, as well as polyp sizes and locations as detected andviewed with WL, are shown in Table 2. Examples of adeno-matous and nonadenomatous polyps viewed with NBI areshown in Figure 2. Of the polyps, 49% were adenomas orcarcinomas, whereas 51% were nonadenomatous; 74% ofadenomas were 5 mm or smaller, and 42% were 3 mm orsmaller.
Overall, nonadenomatous polyps were more likely tohave a light VCI compared with adenomas (71% vs 29%,P ! .001) (Fig. 3). Both carcinomas, but no nonadenoma-tous polyps, had a dark VCI. The image quality of thepolyps viewed with NBI was judged to be good for 191(72%), fair for 72 (27%), and poor for 2 (1%). There wasno statistical difference between image quality of nonade-nomatous and adenomatous polyps. The confidence levelfor endoscopic predictions of histology was high in 126polyps (48%) viewed with WL compared with 201 polyps(76%) after assessment with NBI (P ! .01).
Of the nonadenomatous polyps, the most common his-tology was hyperplastic or aberrant crypt foci (35% and24%, respectively); 11% were SSPs. Compared with allother nonadenomatous polyps, SSPs (Fig. 2F) were larger(4.1 mm vs 3.1 mm, P!.01), more right sided (53% vs 9%,P ! .001), less likely to be classified as Kudo A pit pattern(47% vs 81%, P! .01), or have a type I pit pattern (27% vs66%, P ! .01), and showed a trend toward darker VCI(47% medium VCI vs 28%, P Z .08).
NBI accuracy versus broad-band WLOverall, NBI accuracy was 80% compared with 77% for
WL alone (P Z .35)(Table 3). NBI performed significantlybetter than WL in diagnosing adenomas (sensitivity 80%vs 69%, P ! .05), but there was no difference for nonade-nomatous polyps. This difference was most pronouncedfor adenomas %5 mm (75% vs 60%, P ! .05).
Diagnostic accuracies were better for larger polyps(mean size of correct prediction 4.7 mm vs 3.9 mm, P !.05) and nonsignificant for polypoid shape (87% vs 79%for polyps with sessile shape, P Z .08). Compared withWL, however, NBI did not significantly improve accuracyin any size or shape category, nor for any segment ofthe colon. There were also no significant differences indiagnostic accuracies, regardless of bowel preparation
www.giejournal.org
Rogart et al Narrow-band imaging to differentiate colorectal polyps
Figure 1. Modified Kudo’s pit-pattern classification and VCI grading scale. Kudo A suggests nonadenomatous, whereas Kudo B suggests adenomatous
polyp. *Adapted from Ref. 9.
quality or image quality. NBI predictions were more accu-rate when the confidence level was high rather than low(83% vs 75%, P Z .05). There was a trend toward im-proved NBI accuracy compared with WL when confidencewas low (75% vs 67%, P Z .09) but no difference whenconfidence was high (83% vs 81%). The use of NBI didnot significantly improve the diagnostic accuracy for anysubtype of nonadenomatous polyp.
Of the 52 polyps misdiagnosed by NBI, 22 of 26 adeno-mas incorrectly classified were graded as having a lightVCI, and 20 of 26 nonadenomatous polyps were gradedas having a medium VCI (Fig. 2C). Approximately a thirdof the 52 incorrectly predicted polyps were not of typicalhistologic patterns; 8 were SSP, and 8 others had atypicalfeatures (1 condyloma, 3 with significant lamina propria
www.giejournal.org
fibrosis, 2 with vascular congestion, and 2 with significantinflammation). SSPs were incorrectly diagnosed more of-ten than all other nonadenomatous polyps (53% vs 15%,P ! .05). If SSPs instead are included in the ‘‘adenoma’’category because of emerging evidence that suggests pos-sible malignant potential (see Discussion), then diagnosticaccuracy, sensitivity, and specificity for NBI and WL werelargely unchanged (81%, 77%, 85% and 78%, 67%, 91%,respectively).
NBI learning curveAn equal number of polyps were analyzed in each of
the 2 study periods (133 and 132, respectively). NBI accu-racies improved from 74% to 87% (P ! .05), from the firstto second half of the study, whereas, WL accuracies
Volume 68, No. 6 : 2008 GASTROINTESTINAL ENDOSCOPY 1139
Narrow-band imaging to differentiate colorectal polyps Rogart et al
improved only from 78% to 79% (Fig. 4). In the secondhalf of the study, therefore, NBI was significantly more ac-curate than WL (P!.05). If SSPs were included in the ‘‘ad-enoma’’ category, then the magnitude of improvementwith NBI was even greater, increasing from 72% to 90%.NBI sensitivity for adenomas also improved, from 73% to88% (P ! .05), and was also significantly higher than theWL sensitivity of 72% for adenomas in the second half (P! .05). Three of the endoscopists showed significant im-provements in diagnostic accuracies during the study,whereas one showed no change. There was little correla-tion, however, between the degree of improvement andpolyp volume for each endoscopist (Pearson correlationcoefficient 0.35). During the study, endoscopists changedtheir prediction of 32 polyps (12%) after examination withNBI (Fig. 2D); although this led to a correct diagnosis only56% of the time during the first half of the study, this in-creased to 80% in the second half (100% for two of the en-doscopists). Furthermore, the variation between theindividual endoscopist’s diagnostic accuracies decreasedfrom the first to second half of the study (SD 12.6% vsSD 4.1%, P ! .05), so that, by the end of the study, allthe endoscopists had approximately equal accuracy withNBI.
Endoscopists scored high on both the pretests andposttests, with only a minimal increase in correct diagno-ses (mean score 90% vs 95%, P Z.55). However, there wasa categorical improvement in interobserver agreement
TABLE 1. Demographics of patients with polyps
With
polyp
(n Z 131)
Without
polyp
(n Z 171)
Total
(n Z 302)
Mean (SD) age
(minimum, maximum)
(y)
59 � 10.0
(27, 79)
54 � 10.8
(18, 75)
56 � 10.7
(18, 79)
Sex (no. [%])
Men 85 (65) 95 (55) 180 (60)
Women 46 (35) 76 (44) 122 (40)
Indication for
colonoscopy (no. [%])
Screening 72 (55) 98 (58) 170 (56)
History of polyps 24 (18) 20 (12) 44 (15)
History of CRC 8 (6) 6 (4) 14 (5)
IBD surveillance 0 (0) 4 (2) 4 (1)
Hemeþ or rectal
blood
14 (11) 14 (8) 28 (9)
Anemia 5 (4) 9 (5) 14 (5)
Other 8 (6) 20 (12) 28 (9)
CRC, Colorectal cancer; IBD, inflammatory bowel disease.
1140 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008
between the pretest and the posttest with respect toVCI (k Z 0.523 vs k Z 0.645), modified Kudo pit-patterngroup (k Z 0.716 vs k Z 0.900), and endoscopic diagno-sis (k Z 0.666 vs k Z 0.900), with ‘‘substantial’’ or ‘‘almostperfect’’ agreement achieved on the posttest.15 Interob-server agreement for a polyp’s specific pit pattern (typeI-V) was only fair for both the pretest and posttest (k Z0.377 and k Z 0.291, respectively).
DISCUSSION
As HD colonoscopy becomes the standard, colorectalpolyps are being detected at increasing rates, and a sub-stantial number of these will be nonadenomatouspolyps.16 Our prospective study of 265 colorectal polyps,designed to reflect real-world use of NBI, is, to our knowl-edge, the largest study to date that addressed the questionof whether NBI outperforms ordinary WL in determiningthe histopathologic diagnosis of polyps during real-timecolonoscopy. Our overall accuracy of 80% for NBI is con-sistent with the accuracies achieved in the small NBI polypstudies previously published,7,17,18 and we demonstratedthat improved performance can be achieved over time.We found NBI to be most useful in correctly identifying ad-enomas, especially those that are small. This is clinicallyimportant, because the consequence of incorrectly diag-nosing an adenoma (ie, leaving an adenoma in place)likely outweighs the risks of incorrectly diagnosing a non-adenomatous polyp (ie, the polyp gets removed).
Factors that limit the generalizability of prior NBI-polypreports include the smaller number of polyps and varyingpercentages of adenomas examined, the lack of imageprocessors equipped with HD color CCDs, the assessmentof archived still images rather than real-time video, andthe use of high-magnification zoom NBI colonoscopesthat are not commercially available in the UnitedStates.17-21 Several investigators suggested that chromoen-doscopy and NBI are more accurate and reproduciblewhen used with high magnification (�80-�150).7,17,22
Our use of widely available NBI colonoscopes withouthigh magnification, however, is more likely to be mostrepresentative of the real-life impact of NBI on colonpolyp differentiation. Our WL accuracy of 77% was higherthan previously reported17 and may be explained by theuse of HD (1080 lines of vertical resolution) imaging,which may mitigate some of the advantages that NBI hasover a non-HD picture.16 In our experience, we were oftenable to identify the pit patterns of larger polyps withoutNBI, and it was mainly for the smaller adenomas thatNBI was superior to WL in predicting histology. NBI alsoappeared to be more helpful when there was a low levelof confidence in the WL interpretation.
Unlike chromoendoscopy, NBI makes the superficialvasculature of GI mucosa visible, because the centralwavelength of 415 � 30 nm is preferentially absorbed by
www.giejournal.org
Rogart et al Narrow-band imaging to differentiate colorectal polyps
TABLE 2. Histology and characteristics of detected polyps
Size, mm Location
Total no. Mean 1-5 6-9 O10 Left Right
Carcinoma 2 14.00 0 1 1 1 1
Adenoma 129 4.98 95 22 12 62 67
Tubular adenoma 125 4.76 93 22 10 59 66
Tubulovillous adenoma 2 8.5 1 0 1 2 0
Serrated adenoma 2 11.5 1 0 1 1 1
Nonadenomatous 134 3.22 126 7 1 115 19
Serrated polyps
Hyperplastic 47 3.06 44 3 0 44 3
Sessile serrated polyp 15 4.13 13 2 0 7 8
Serrated polyp NOS 9 3.33 8 1 0 9 0
Other polyps
Aberrant crypt foci 32 2.91 32 0 0 30 2
Lymphoglandular complex 16 2.75 16 0 0 13 3
WSA 9 3.00 8 1 0 7 2
Miscellaneous* 6 5.33 5 0 1 5 1
NOS, Not otherwise specified; WSA, without significant abnormality.
*Inflammatory polyp (3), condyloma (2), leiomyoma (1).
hemoglobin.5 This feature is potentially advantageous, be-cause angiogenesis and neovascularization are importantevents in tumorogenesis.23 Without high magnification,however, it is difficult to characterize the polyp microvas-cular architecture.6,24 The VCI grading scale is intended toidentify polyps with a greater density and caliber of ves-sels, resulting in a darker and browner appearance withNBI.6,18 Our simplified grading scale, however, lackeda high degree of accuracy. We found 19% of all adenomasto have a light VCI, similar to reported results with high-magnification NBI.24 Conversely, we observed that somenonadenomatous polyps with inflammation on histologyhad a darker appearance with NBI. Further investigationinto other benign processes that mimic neovascularizationunder NBI is warranted.
The traditional concept of classifying polyps into eitheradenomatous or nonadenomatous categories for stratify-ing cancer risk is gradually evolving,25 with evidence thatsuggests that a subgroup of serrated polyps may have pre-neoplastic potential and could progress to colon cancer viathe microsatellite instability pathway.12,26-28 As the nomen-clature, diagnostic criteria, and understanding of the natu-ral history of these polyps evolve, endoscopic methods todifferentiate the various subtypes more reliably will like-wise need to become more refined. In our study, we ob-served that SSPs were the most challenging to evaluate
www.giejournal.org
with NBI. SSPs are not histologically adenomas, are notdefinitively addressed in the multisociety colonoscopysurveillance guidelines,2 and are often difficult to distin-guish from other serrated polyps.29 In fact, in our study12 of 15 SSPs had initially been reported as hyperplasticpolyps. We, therefore, grouped SSPs in the ‘‘nonadenoma-tous’’ category, because this better reflected our use of NBIto correlate macroscopic features to histology. Becausethere is emerging evidence that SSPs may have malignantpotential,30 however, we reanalyzed our results with SSPsin the ‘‘adenoma’’ category and found that accuraciesand sensitivities were not appreciably different. A retro-spective review of the images of all 15 SSPs detected inour study identified NBI features that were ascribed onlyto adenomas. Conversely, East et al18 recently observeda small number of adenomas with nonadenomatous NBIfeatures (type II pit patterns) and a significant discordancebetween the appearance of pit patterns on NBI and chro-moendoscopy. Our findings support the suggestion thatKudo’s pit-pattern classification, developed and validatedfor chromoendoscopy, may require further modificationfor application with NBI and that there is a subset of non-adenomatous polyps that may not adhere to Kudo’s classi-fication. Use of other NBI features or complementarytechnologies31-33 that do not rely on pit patterns couldalso be explored to improve the accuracy of NBI.
Volume 68, No. 6 : 2008 GASTROINTESTINAL ENDOSCOPY 1141
Narrow-band imaging to differentiate colorectal polyps Rogart et al
Figure 2. Examples of nonadenomatous and adenomatous polyps viewed under NBI. A, Hyperplastic polyp with Kudo A pit pattern (type I) and light
VCI. B, Hyperplastic polyp with Kudo A pit pattern (type II) and light VCI. C, Hyperplastic polyp, with significant vascular congestion on histology
showed a Kudo A pit pattern but a medium VCI and was incorrectly predicted to be an adenoma. D, A 3-mm polyp seen under WL was diagnosed
by endoscopy as nonadenomatous (left) but was rediagnosed as an adenoma after being viewed with NBI (right) because of a Kudo B pit pattern
and medium VCI. E, Tubular adenoma with Kudo B pit pattern and dark VCI. F, SSP with Kudo B pit pattern.
The clinical significance of ACF, which may be precur-sors to adenomas,34 is another issue that deserves furtherattention, because these small lesions are likely to be en-countered and removed more frequently with improve-
1142 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008
ments in the resolution of colonoscopic imagingtechniques. Although there are many studies that de-scribed the histologic appearance of ACF, well-establishedcriteria are lacking. Lesions in our study that clearly
www.giejournal.org
Rogart et al Narrow-band imaging to differentiate colorectal polyps
showed dysplasia were included in the adenomatous cat-egory, irrespective of their size or appearance, whereasthose showing well-defined serrations were included inthe serrated category. We believe this is a practical ap-proach that emphasizes clinical relevance. However, werecognize that further studies are needed to better charac-terize ACF in clinically useful terms to strengthen futurepolyp surveillance guidelines.
The most effective methods to teach and learn ad-vanced endoscopic imaging techniques remain to be de-termined. Wide acceptance of a new technology requiresthat it be inexpensive, readily available, accurate, repro-ducible, and easy to use. We believe that the prestudy ed-ucation sessions in combination with continual feedbackevery 2 weeks throughout the study were important fac-tors in achieving the learning curve we observed.35 A sim-ilar, though steeper, learning curve with magnifyingchromoendoscopy was previously reported.36 Overall, inour study, there was an absolute increase in the diagnosticaccuracy of NBI by 13% from the first half to the secondhalf of the study compared with only a 1% increase forWL. We, therefore, did not find that NBI induced a ‘‘train-ing effect’’ on WL examination.37 In addition, all endo-scopists completed the study with a similar level ofaccuracy, and this decrease in variance was paralleled byan increase in the posttest interobserver agreement forour proposed polyp characterization scheme, as well asfor predicting polyp histology. The lack of improvementin agreement for specific pit-pattern type (I-V) further sug-gests that a simplified, dichotomous Kudo categorization,along with a VCI scale, may be important to learning andapplying NBI to colorectal polyps, particularly when highmagnification is not available. Based on our findings, wewould expect even greater improvements in diagnostic ac-curacies with continued experience. Accuracies of 100%,however, may be difficult to achieve with current limita-tions, such as the absence of high magnification and theuncertainty of both the natural history and superficialmucosal characteristics of certain subtypes of nonadenom-atous polyps. As advanced endoscopic imaging technolo-
Figure 3. VCI of detected polyps.
www.giejournal.org
gies continue to develop and become more widelyapplied, issues of training and learning will likely have con-tinued importance.
One limitation to our study is that it was conducted ata single academic institution. We included 4 endoscopists,however, with differing levels of experience to improvethe generalizability of our findings. Endoscopists did nothave extensive experience with NBI or chromoendoscopybefore the study and, although this makes our study morerelevant to the average colonoscopist, it may have limitedthe accuracy rates achieved. Including greater numbers ofpolyps may have resulted in accuracies that approachedthose of Eastern colonoscopists, who are more familiarwith chromoendoscopic techniques. In addition, as dis-cussed above, polyp assessment was largely dependenton Kudo’s pit-pattern classification, which even though
TABLE 3. Performance characteristics of NBI and WL for
predicting adenoma
NBI, no. (%)
(N Z 265)
WL, no. (%)
(N Z 265)
P
value
Accuracy 213/265 (80) 205/265 (77) NS
Sensitivity* 105/131 (80) 90/131 (69) !.05
Specificityy 108/134 (81) 115/134 (86) NS
PPV 105/131 (80) 90/109 (83) NS
NPV 108/134 (81) 115/156 (74) NS
NS, Not significant; PPV, positive predictive value; NPV, negative
predictive value.
*Diagnostic accuracy for adenomas.
yDiagnostic accuracy for nonadenomatous polyps.
Figure 4. NBI learning curve. Diagnostic accuracies for NBI improved by
an absolute 13% from the first half to the second half of the study, com-
pared with only 1% for WL. NBI improvement was most pronounced for
adenomas. In addition, when endoscopists changed their diagnosis based
on NBI evaluation, there was a 24% absolute improvement in accuracy by
the end of the study.
Volume 68, No. 6 : 2008 GASTROINTESTINAL ENDOSCOPY 1143
Narrow-band imaging to differentiate colorectal polyps Rogart et al
simplified in our study, cannot yet be validated for NBI asit has been for chromoendoscopy. Although the lack ofhigh magnification may also have been a limitation inour study, only commercially available NBI colonoscopeswere used to better assess the real-world impact of NBIon polyp interpretation.
In summary, our study is the largest to date that com-pared NBI to WL in the real-time diagnosis of colorectalpolyps in a Western population. We demonstrated thatthere is a learning curve with regard to NBI assessmentof colorectal polyps, and that NBI outperforms ordinarybroadband WL once this ‘‘learning’’ is achieved. Our find-ings also highlight the variable NBI appearance amongsome subtypes of nonadenomatous polyps. Further inves-tigation into superficial mucosal patterns of polyps andthe optimal method of viewing them with NBI is needed.At the present time, current NBI accuracy rates of 80% arelikely inadequate to defer polypectomy and, therefore,may limit the utility of NBI in evaluating colorectal polypsduring routine clinical practice. Accuracy rates that ap-proach 100% would be required for endoscopists to usethis assessment to determine the need for polyp removalwith confidence.
ACKNOWLEDGMENTS
We thank Rafaela Dancygier and Katherine Kacena forstatistical consultation; Grace Gathangu, Hemchand Ram-beran, and Anish Sheth, for assistance in patient enroll-ment; and Denise Conte, and the Yale GI ProcedureCenter nurses.
DISCLOSURE
The authors report that there are no disclosures rele-vant to this publication.
REFERENCES
1. Vogelstein B, Fearon ER, Hamilton SR, et al. Genetic alterations during
colorectal-tumor development. N Engl J Med 1988;319:525-32.
2. Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy
surveillance after polypectomy: a consensus update by the US Multi-
Society Task Force on colorectal cancer and the American Cancer So-
ciety. Gastroenterology 2006;130:1872-85.
3. Eisen GM, Kim CY, Fleisher DE, et al. High-resolution chromoendo-
scopy for classifying colonic polyps: a multicenter study. Gastrointest
Endosc 2002;55:687-94.
4. Hurlstone DP, Fujii T. Practical uses of chromoendoscopy and magni-
fication at colonoscopy. Gastrointest Endosc Clin N Am 2005;15:
687-702.
5. Gono K, Obi T, Yamaguchi M, et al. Appearance of enhanced tissue
feature in narrow-band endoscopic imaging. J Biomed Opt 2004;9:
568-77.
6. Sano Y, Kobayahi M, Hamamoto Y, et al. New diagnostic method
based on color imaging using narrow band imaging (NBI) system
1144 GASTROINTESTINAL ENDOSCOPY Volume 68, No. 6 : 2008
for gastrointestinal tract [abstract]. Gastrointest Endosc 2001;53:
AB125.
7. Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the
diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy
2004;36:1094-8.
8. Kudo S, Hirota S, Nakajima T, et al. Colorectal tumours and pit pattern.
J Clin Pathol 1994;47:880-5.
9. Kudo S, Tamura S, Nakajima T, et al. Diagnosis of colorectal tumorous
lesions by magnifying endoscopy. Gastrointest Endosc 1996;44:8-14.
10. Kudo S, Rubio CA, Teixeira CR, et al. Pit pattern in colorectal neoplasia:
endoscopic magnifying view. Endoscopy 2001;33:367-73.
11. Takayama T, Katsuki S, Takahashi Y, et al. Aberrant crypt foci of the co-
lon as precursors of adenoma and cancer. N Engl J Med 1998;330:
1277-84.
12. Torlakovic E, Skovlund E, Snover DC, et al. Morphologic reappraisal of
serrated colorectal polyps. Am J Surg Pathol 2003;27:65-81.
13. Snover DC, Jass JR, Fenoglio-Preiser C, et al. Serrated polyps of the
large intestine: a morphologic and molecular review of an evolving
concept. Am J Clin Pathol 2005;124:380-91.
14. Fleiss JL. Measuring nominal scale agreement among many raters.
Psychol Bull 1971;76:378-82.
15. Landis JR, Koch GG. The measurement of observer agreement for
categorical data. Biometrics 1977;33:159-74.
16. Rex DK, Helbig CC. High yields of small and flat adenomas with high-
definition colonoscopes using either white light or narrow band imag-
ing. Gastroenterology 2007;133:42-7.
17. Chiu HM, Chang CY, Chen CC, et al. A prospective comparative study
of narrow-band imaging, chromoendoscopy, and conventional colo-
noscopy in the diagnosis of colorectal neoplasia. Gut 2007;56:373-9.
18. East JE, Suzuki N, Saunders BP. Comparison of magnified pit pattern
interpretation with narrow band imaging versus chromoendoscopy
for diminutive colonic polyps: a pilot study. Gastrointest Endosc
2007;66:310-6.
19. Su MY, Hsu CM, Ho YP, et al. Comparative study of conventional colo-
noscopy, chromoendoscopy, and narrow-band imaging systems in
differential diagnosis of neoplastic and nonneoplastic colonic polyps.
Am J Gastroenterol 2006;101:2711-6.
20. Tanaka S, Oka S, Hirata M, et al. Pit pattern diagnosis for colorectal
neoplasia using narrow band imaging magnification. Dig Endosc
2006;18:S52-6.
21. Hirata M, Tanaka S, Oka S, et al. Magnifying endoscopy with narrow
band imaging for diagnosis of colorectal tumors. Gastrointest Endosc
2007;65:988-95.
22. Fu KI, Sano Y, Fujii T, et al. Magnification or nonmagnification: that is
the question. Am J Gastroenterol 2007;102:1326-7.
23. Risau W. Mechanisms of angiogenesis. Nature 1997;386:671-4.
24. Hirata M, Tanaka S, Oka S, et al. Evaluation of microvessels in colorec-
tal tumors by narrow band imaging magnification. Gastrointest
Endosc 2007;66:945-52.
25. Cunningham KS, Ridell RH. Serrated mucosal lesions of the colorec-
tum. Curr Opin Gastroenterol 2006;22:48-53.
26. Montgomery E. Serrated colorectal polyps: emerging evidence
suggests the need for a reappraisal. Adv Anat Pathol 2004;11:
143-9.
27. Torlakovic E, Snover DC. Sessile serrated adenoma: a brief history and
current status. Crit Rev Oncog 2006;12:27-39.
28. Harvey NT, Ruszkiewicz A. Serrated neoplasia of the colorectum. World
J Gastroenterol 2007;13:3792-8.
29. Lauwers GY, Chung DC. The serrated polyp comes of age. Gastroenter-
ology 2006;131:1631-4.
30. O’Brien MJ. Hyperplastic and serrated polyps of the colorectum.
Gastroenterol Clin North Am 2007;36:947-68.
31. Curvers WL, Singh R, Song LM, et al. Endoscopic tri-modal imaging for
detection of early neoplasia in Barrett’s oesophagus: a multi-centre
feasibility study using high-resolution endoscopy, autofluorescence
imaging and narrow band imaging incorporated in one endoscopy
system. Gut 2008;57:167-72.
www.giejournal.org
Rogart et al Narrow-band imaging to differentiate colorectal polyps
32. Dhar A, Johnson KS, Novelli MR, et al. Elastic scattering spectroscopy
for the diagnosis of colonic lesions: initial results of a novel optical bi-
opsy technique. Gastrointest Endosc 2006;63:257-61.
33. Van Den Broek FJ, Hardwick JC, Reitsma JB, et al. Endoscopic trimodal-
ity imaging (ETMI) for the detection and classification of colonic
polyps [abstract]. Gastrointest Endosc 2007;65:AB93.
34. Gupta AK, Pretlow TP, Schoen RE. Aberrant crypt foci: what we know
and what we need to know. Clin Gastroenterol Hepatol 2007;5:526-33.
35. Sowden P, Pauli R, Roling P, et al. Improvement in screening perfor-
mance: the importance of appropriate feedback in screening mam-
mography. Proc Med Imaging 1996;2712:180-8.
36. Togashi K, Konishi F, Ishizuka T, et al. Efficacy of magnifying endos-
copy in the differential diagnosis of neoplastic and non-neoplastic
polyps of the large bowel. Dis Col Rectum 1999;42:1602-8.
www.giejournal.org
37. Adler A, Pohl H, Papanikolaou IS, et al. A prospective randomized
study on narrow-band imaging versus conventional colonoscopy for
adenoma detection: does NBI induce a learning effect? Gut 2008;57:
59-64.
Received December 15, 2007. Accepted April 18, 2008.
Current affiliations: Section of Digestive Diseases (J.N.R., U.D.S., J.L., P.J.,
H.A.), Department of Medicine, Department of Pathology (D.J., T.O.), Yale
University School of Medicine, New Haven, Connecticut, USA.
Reprint requests: Jason Rogart, MD, Department of Internal Medicine, Yale
University School of Medicine, 333 Cedar St - 1080 LMP, New Haven, CT
06520-8019.
Volume 68, No. 6 : 2008 GASTROINTESTINAL ENDOSCOPY 1145
Related Documents