DEPARTMENT OF MICROBIOLOGY AND INDUSTRIAL MICROBIOLOGY IMO STATE UNIVERSITY PMB 2000 OWERRI IMO STATE STUDENT SEMINAR RESEARCH IN PARTIAL FULFILMENT FOR THE AWARD OF BACHELOR OF SCIENCE DEGREE (B.Sc) IN MICROIOLOGY WITH FOCUS ON Mycobacterium tuberculosis AND ANTIBIOTICS RESISTANCE A REEMERGING DISEASE AND PUBLIC HEALTH PROBLEM BY AMETCHONOU SAMUEL VALENTINE IMSU/2008/5357 SUPERVISOR: MRS NWANCHUKWU

Mycobacterium tuberculosis and antibiotic resistant a rememerging disease and public health problem
Aug 03, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

DEPARTMENT OF MICROBIOLOGY AND INDUSTRIAL
MICROBIOLOGY
IMO STATE UNIVERSITY
PMB 2000 OWERRI IMO STATE
STUDENT SEMINAR RESEARCH IN PARTIAL FULFILMENT FOR THE AWARD OF BACHELOR OF SCIENCE DEGREE (B.Sc) IN MICROIOLOGY WITH FOCUS ON
Mycobacterium tuberculosis AND ANTIBIOTICS RESISTANCE A REEMERGING DISEASE AND PUBLIC HEALTH PROBLEM
BY
AMETCHONOU SAMUEL VALENTINE IMSU/2008/5357
SUPERVISOR: MRS NWANCHUKWU

DEDICATION
I dedicate this research work to my mum Mrs. Ayabavi Ametchonou for her unending care.

AKNOWLEGEMENT
I acknowledge the reservoirs of all knowledge and wisdom, the Most High God who has endowed me with wisdom, knowledge, understanding and good health of mind and body before and doing the period of my seminar research.
It is pertinent to express my sincere appreciation to the following people who have contributed immensely to my academic pursuit: My Mum Mrs. Ayabavi Ametchonou for providing me with the requisite need for my academic pursuit whenever the need arise, My Sisters: Mrs. Ajibode, Mrs. Odunkoya, Mrs. Akapo, Mrs. Moiett and my Brother Robert, who make up the ecological niche of my family for your cares and understanding. Thank you.
To all my Lecturers in the Department of Microbiology and Industrial Microbiology Imo State University Owerri., I really appreciate all your effort at impacting extensively in me the knowledge of Microbiology and its allies. To my zealous and active HOD Dr. M.I Nwanchukwu for the outstanding transformations you have brought to the department, May God continue to bestowed on you the grace to reap more success.
However, a research on this topic won’t have been achieved if not for the approval and guidelines I receive from my Supervisor Mrs. Nwanchukwu, may all your aspirations come to reality.
Am mostly indebted to all the researchers and writers to whom materials I have use in the writing of this seminar and Google for providing an easy platform for information acquisition.
Finally to all my Friends for their understanding and advice in the course of my writing and typesetting this research. Thank you all.

ABSTRACT
Anti-tuberculosis drugs are a two-edged sword. While they destroy pathogenic M. tuberculosis they also select for drug resistant bacteria against which those drugs are then ineffective. Global surveillance has shown that drug resistant Tuberculosis is widespread and is now a threat to tuberculosis control programs in many countries. Application of molecular methods during the last decade has greatly changed our understanding of drug resistance in tuberculosis. Application of molecular epidemiological methods was also central to the description of outbreaks of drug resistance in Tuberculosis.This paper will discuss the challenges and opportunities associated with controlling Mycobacterium tuberculosis drug resistance a communicable diseases in the coming decades, within the context of the New Public Health, as it refers to the ways in which health systems manage and monitor threats to public health.

TABLE OF CONTENT

CHAPTER ONE
1.0 GENERAL INTRODUCTION
Tuberculosis continues to be a major public health problem in many parts of the world. Significant obstacles in controlling the epidemic are the length of treatment and the large reservoir of latently infected people. However, Tuberculosis (TB) is a potentially fatal contagious disease that can affect almost any part of the body but is mainly an infection of the lungs. It is caused by a bacterial microorganism, the tubercle bacillus or Mycobacterium tuberculosis.
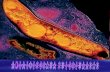
Fig 1.1
Colonies of Mycobacterium tuberculosis
1.1 HISTORICAL OVERVIEW OF M.tuberculosis
Tuberculosis was popularly known as consumption for a long time. Scientists know it as an infection caused by Mycobacterium tuberculosis. In 1882, the microbiologist Robert Koch discovered the tubercle bacillus, at a time when one of every seven deaths in Europe was caused by TB. Because antibiotics were unknown, the only means of controlling the spread of infection was to isolate patients in private hospitals limited to patients with TB—a practice that continues to this day in many countries. The net effect of this pattern of treatment was to separate the study of tuberculosis from mainstream medicine. Entire organizations were set up to study not only the disease as it affected individual patients, but its impact on the society as a whole. At the turn of the twentieth

century more than 80% of the population in the United States was infected before age 20, and tuberculosis was the single most common cause of death. By 1938 there were more than 700 TB hospitals in this country.
Tuberculosis spread much more widely in Europe when the industrial revolution began in the late nineteenth century. The disease became widespread somewhat later in the United States, because the movement of the population to large cities made overcrowded housing so common. When streptomycin, the first antibiotic effective against Mycobacterium tuberculosis, was discovered in the early 1940s, the infection began to come under control. Although other more effective anti-tuberculosis drugs were developed in the following decades, the number of cases of TB in the United States began to rise again in the mid-1980s. This upsurge was in part again a result of overcrowding and unsanitary conditions in the poor areas of large cities, prisons, and homeless shelters. An additional factor is the AIDS epidemic. AIDS patients are much more likely to develop tuberculosis because of their weakened immune systems. There is still an estimated of 8-10 million new cases of TB each year worldwide, causing roughly 3 million deaths.
In the 1960s, the idea that infectious disease would soon become a thing of the past became widespread in both professional and public circles. In 1963, a respected physician and anthropologist T. Aidan Cockburn, as quoted by Faucci, stated: “We can look forward with confidence to a considerable degree of freedom from infectious diseases at a time not too far in the future. Indeed… it seems reasonable to anticipate that within some measurable time… all the major infections will have disappeared.5
The hypotheses usually proposed to explain the emergence of these new agents of resistant refer to the complex interaction of numerous factors such as relative size of animal species populations, expanding human populations and settlements, change in technology, as well as the probable influence of global climatic changes.18
Progress in the field of public health has continue to tackle this re emergence specie of Mycobacterium tuberculosis through discoveries of active drugs, spontaneous research and constant education of the infected patient and isolation of such patient to avoid the communicable effect of such disease. These and other innovations raise the hope of new discoveries and vaccine development against other chronic diseases of infectious origin.

1.2 SCIENCTIFIC CLASSIFICATION
Kingdom : Bacteria
Phylum : Actinobacteteria
Order : Actinomycetales
Suborder : Corynebacteriacea
Family : Mycobacteriaceae
Genus : Mycobacterium
Species : tuberculosis
Binomial name: Mycobacterium tuberculosis
1.3 CAUSES AND SYMPTOMS
Transmission Tuberculosis spreads by droplet infection. This type of transmission means that when a TB patient exhales, coughs, or sneezes, tiny droplet of fluid containing tubercle bacilli are released into the air. This mist, or aerosol as it is often called, can be taken into the nasal passages and lungs of a susceptible person nearby. Tuberculosis is not, however, highly contagious compared to some other infectious diseases. Only about one in three close contacts of a TB patient, and fewer than 15% of more remote contacts, are likely to become infected. As a rule, close, frequent, or prolonged contact is needed to spread the disease. Of course, if a severely infected patient emits huge numbers of bacilli, the chance of transmitting infection is much greater. Unlike many other infections, TB is not passed on by contact with a patient's clothing, bed linens, or dishes and cooking utensils. The most important exception is pregnancy. The fetus of an infected mother may contract TB by inhaling or swallowing the bacilli in the amniotic fluid.
Progression Once inhaled, tubercle bacilli may reach the small breathing sacs in the lungs (the alveoli), where they are taken up by cells called macrophages. The bacilli multiply within these cells and then spread through the lymph vessels to nearby lymph

nodes. Sometimes the bacilli move through blood vessels to distant organs. At this point they may either remain alive but inactive (quiescent), or they may cause active disease. Actual tissue damage is not caused directly by the tubercle bacillus, but by the reaction of the person's tissues to its presence. In a matter of weeks the host develops an immune response to the bacillus. Cells attack the bacilli, permit the initial damage to heal, and prevent future disease permanently.
Infection does not always mean disease; in fact, it usually does not. At least nine of ten patients who harbor M. tuberculosis do not develop symptoms or physical evidence of active disease, and their x-rays remain negative. They are not contagious; however, they do form a pool of infected patients who may get sick at a later date and then pass on TB to others. It is thought that more than 90% of cases of active tuberculosis come from this pool. In the Africa, this group numbers 10-15 million persons. Whether or not a particular infected person will become ill is impossible to predict with certainty. An estimated 5% of infected persons get sick within 12-24 months of being infected. Another 5% heal initially but, after years or decades, develop active tuberculosis either in the lungs or elsewhere in the body. This form of the disease is called reactivation TB, or post-primary disease. On rare occasions a previously infected person gets sick again after a later exposure to the tubercle bacillus.
Public health has had enormous triumphs in the field of infectious disease control,
however, some disease still give certain problem in their complete eradication through their resistance to drugs which where initially active in their treatment. This resistivity may be as a result of many factors ranging from improper usage of drugs, new emerging strains of such pathogenic substances and partial treatment of such disease at the initial stage of the infection.
The reduced burden of many infectious diseases, such as TB, cholera, typhoid and other enteric infectious diseases which were rampant during the 19th century, can be attributed to sanitation, water and food safety regulations and improved nutrition and living standards. Vaccines developed during the late 19th and throughout the 20th century have successfully taken public health to new heights in terms of improving individual and societal well-being.4
In the 1960s, the idea that infectious disease would soon become a thing of the past became widespread in both professional and public circles. In 1963, a respected physician and anthropologist T. Aidan Cockburn, as quoted by Faucci,

stated: “ We can look forward with confidence to a considerable degree of freedom from infectious diseases at a time not too far in the future. Indeed… it seems reasonable to anticipate that within some measurable time… all the major infections will have disappeared.5
The hypotheses usually proposed to explain the emergence of these new agents of resistant refer to the complex interaction of numerous factors such as relative size of animal species populations, expanding human populations and settlements, change in technology, as well as the probable influence of global climatic changes.18
Progress in the field of public health has continue to tackle this re emergence specie of Mycobacterium tuberculosis through discoveries of active drugs, spontaneous research and constant education of the infected patient and isolation of such patient to avoid the communicable effect of such disease. These and other innovations raise the hope of new discoveries and vaccine development against other chronic diseases of infectious origin.
1.4 DISEASE SIMILAR TO TUBERCULOSIS There are many forms of mycobacteria other than M. tuberculosis, the tubercle bacillus. Some cause infections that may closely resemble tuberculosis, but they usually do so only when an infected person's immune system is defective. People who are HIV-positive are a prime example. The most common mycobacteria that infect AIDS patients are a group known as Mycobacterium avium complex (MAC). People infected by MAC are not contagious, but they may develop a serious lung infection that is highly resistant to antibiotics. MAC infections typically start with the patient coughing up mucus. The infection progresses slowly, but eventually blood is brought up and the patient has trouble breathing. In AIDS patients, MAC disease can spread throughout the body, with anemia, diarrhea, and stomach pain as common features. Often these patients die unless their immune system can be strengthened. Other mycobacteria grow in swimming pools and may cause skin infection. Some of them infect wound and artificial body parts such as a breast implant or mechanical heart valve.

CHAPTER TWO
2.0 HISTORY OF DRUG RESISTANCE AND GLOBAL SURVELANCE Mycobacterium tuberculosis
Shortly after the first anti-tuberculosis (TB) drugs were introduced, streptomycin (STR), para-aminosalicylic acid (PAS), isoniazid (INH) resistance to these drugs was observed in clinical isolates of Mycobacterium tuberculosis (Crofton and Mitchison, 1948). This led to the need to measure resistance accurately and easily.
The Pasteur Institute introduced the critical proportion method in 1961 for drug susceptibility testing in TB and this method became the standard method of use (Espinal, 2003). Studies on drug resistance in various countries in the 1960s showed that developing countries had a much higher incidence of drug resistance than developed countries (Espinal, 2003)
By the end of the 1960s rifampicin (RIF) was introduced and with the use of combination therapy, there was a decline in drug resistant and drug susceptible TB in developed countries. This led to a decline in funding and interest in TB control programs. As a result, no concrete monitoring of drug resistance was carried out for the following 20 years (Espinal, 2003). The arrival of HIV/AIDS in the 1980s resulted in an increase in transmission of TB associated with outbreaks of multi-drug-resistant TB (MDR-TB) (Edlin et al., 1992; Fischl et al., 1992) i.e. resistant to INH and RIF. In the early 1990s drug resistance surveillance was resumed in developed countries, but the true incidence remained unclear in the developing world (Cohn et al., 1997).
The WHO/IUATLD global project on drug-resistance surveillance In 1994 the Global Project on Drug-Resistance Surveillance was initiated to monitor the trends of resistance. The first report was published in 1997 and contained data from 35 geographical settings for the period 1994–1996 (World Health Organization, 1997; Pablos-Mendez et al., 1998). The report showed that drug resistance was present globally, and that MDR-TB ranged from 0% to 14% in new cases (median:1.4%) and 0% to 54% in previously treated cases (median:13%). A second report for the period 1996–1999, followed in 2000 and included surveillance data from 58 geographical sites (Espinal, 2003; World Health Organization, 2000). This report confirmed that drug resistant TB was a sufficient problem since MDRTB ranged from 0–16% (median: 1%) among new cases and from 0% to 48% (median: 9%) in

previously treated cases. The recently published third report has data on 77 geographical sites, collected between 1999 and 2002, representing 20% of the global total of new smear-positive TB cases (World Health Organization, 2003). Eight countries did not report any MDR-TB amongst new cases, while the highest incidence of MDR-TB amongst new cases occurred in Kazakhstan and Israel (14%). Significant increases in MDR-TB prevalence were seen in Estonia, Lithuania, Tomsk Oblast (Russian Federation) and Poland and significant decreasing trends in Hong Kong, Thailand and the USA. The highest prevalence of MDR-TB among previously treated cases was reported in Oman (58.3%, 7/12) and Kazakhstan (56.4%, 180/319). The annual incidence of MDR-TB in most Western and Central European Countries was estimated to be fewer than 10 cases each. Alarmingly, it is estimated that the annual incidence of MDR-TB for 2 provinces in China (Henan and Hubei) is 1000 and for Kazakhstan and South Africa it is more than 3000. According to the report, the most effective means to prevent the emergence of drug resistance is by implementing the direct observed therapy strategy (DOTS) (World Health Organization, 2003).
In 1994 the Global Project on Drug-Resistance Surveillance was initiated to monitor the trends of resistance. The first report was published in 1997 and contained data from 35 geographical settings for the period 1994–1996 (World Health Organization, 1997; Pablos-Mendez et al., 1998). The report showed that drug resistance was present globally, and that MDR-TB ranged from 0% to 14% in new cases (median:1.4%) and 0% to 54% in previously treated cases (median:13%). A second report for the period 1996–1999, followed in 2000 and included surveillance data from 58 geographical sites (Espinal, 2003; World Health Organization, 2000).
This report confirmed that drug resistant TB was a sufficient problem since MDRTB ranged from 0–16% (median: 1%) among new cases and from 0% to 48% (median: 9%) in previously treated cases. The recently published third report has data on 77 geographical sites, collected between 1999 and 2002, representing 20% of the global total of new smear-positive TB cases (World Health Organization, 2003). Eight countries did not report any MDR-TB amongst new cases, while the highest incidence of MDR-TB amongst new cases occurred in Kazakhstan and Israel (14%). Significant increases in MDR-TB prevalence were seen in Estonia, Lithuania, Tomsk Oblast (Russian Federation) and Poland and significant decreasing trends in Hong Kong, Thailand and the USA. The highest prevalence of MDR-TB among previously treated cases was reported in Oman (58.3%, 7/12) and Kazakhstan (56.4%, 180/319). The annual incidence of MDR-TB in most Western and Central European Countries was estimated to be fewer than

10 cases each. Alarmingly, it is estimated that the annual incidence of MDR-TB for 2 provinces in China (Henan and Hubei) is 1000 and for Kazakhstan and South Africa it is more than 3000. According to the report, the most effective means to prevent the emergence of drug resistance is by implementing the direct observed therapy strategy (DOTS) (World Health Organization, 2003).
2.1 CURRENT RECOMMENDATION FOR TB. TREATMENT BY W.H.O
TB persists as a global public health problem and the main focus for the twentieth century is firstly to cure the individual patient and secondly to minimize the transmission of M. tuberculosis to other persons (World Health Organization, 2003; Blumberg et al., 2003). The ongoing TB problem has been due to the neglect of TB control by governments, inadequate access and infrastructure, poor patient adherence to medication, poor management of TB control programs, poverty, population growth and migration, and a significant rise in the number of TB cases in HIV infected individuals. Treatment of patients with TB is most successful within a comprehensive framework based upon the following five key components:
• Government commitment
• Case detection by sputum smear microscopy
• Standardized treatment regimen of six to eight months
• A regular, uninterrupted supply of all essential anti-TB drugs
• A standard recording and reporting system.
These five key elements are the recommended approach by the World Health Organization (WHO) to TB control and are called the DOTS strategy (Walley, 1997).
DOTS is an inexpensive strategy for the detection and treatment of TB. DOTS was implemented as part of an adherence strategy in which patients are observed to swallow each dose of anti-TB medication, until completion of the therapy. Monthly sputum specimens are taken until 2 consecutive specimens are negative. Currently there are four recommended regimens for treating patients with TB

infection by drug-susceptible organisms. Each regiment has an initial phase of 2 months intensive phase followed by a choice of several options for the continuation phase of either 4 or 7 months. The recommended regimens together with the number of doses specified by the regimen are described in Table 1.
Since the introduction of the DOTS strategy in the early ‘90s by the WHO, considerable progress has been made in global TB control (Sterling et al., 2003). In 1997, the estimated average treatment success rate world wide was almost 80%. However, less than 25% of people who are sick with TB are treated through the DOTS strategy (Bastian et al., 2000). A total of 180 countries (including both developed and undeveloped countries) had adopted and implemented the DOTS strategy by the end of 2002 and 69% of the global population was living in areas covered by the DOTS strategy (Blumberg et al., 2003). However, even though DOTS programs are in place, treatment success rates are very low in developed countries due to poor management of TB control programs and patient non-compliance (Lienhardt and Ogden, 2004; Bastian et al., 2003). Furthermore, the effectiveness of DOTS is facing new challenges with respect to the spread and increase of MDR-TB and the co-epidemic of TB/HIV (World Health Organization, 2003). WHO and partners have addressed these new challenges and have developed a new strategy called DOTS-Plus for the treatment of MDRTB and its co-epidemic TB/HIV. The goal of DOTS-plus is to prevent further development and spread of MDR-TB and is a comprehensive management initiative built upon the DOTS strategy. It is important to note that DOTS-Plus should only be implemented in areas were the DOTS strategy is in place as there can be no DOTS-plus without an effective DOTS program.
2.2 MOLECULAR MECHANISM FOR DRUG RESISTANCE
In order to control the drug resistance epidemic it is necessary to gain insight into how M. tuberculosis develops drug resistance. This knowledge will help us to understand how to prevent the occurrence of drug resistance as well as identifying genes associated with drug resistance of new drugs. The development of clinical drug resistance in TB is summarized in Fig. 2.1 and is classified as acquired resistance when drug resistant mutants are selected as a result of ineffective treatment or as primary resistance when a patient is infected with a resistant strain.

Mutations in the genome of M. tuberculosis that can confer resistance to anti-TB drugs occur spontaneously with an estimated frequency of 3.5 × 10–6 for INH and 3.1 × 10–8 for RIF. Because the chromosomal loci responsible for resistance to various drugs are not linked, the risk of a double spontaneous mutation is extremely low: 9 × 10–14 for both INH and RIF (Dooley and Simone, 1994). MDR-TB defined as resistance to at least INH and RIF will thus occur mainly in circumstances where sequential drug resistance follows sustained treatment failure.
Few bacteria naturally resistant (mutations)
INH =3.5×10-6 RIF =3.1×10-8
Selection
Acquired Resistance Primary Resistance Overgrowth of resistant Transmission to different host (Mutant) bacteria in the same host Fig 2.1 Acquired resistance develops due to natural selection which is a function of ineffective treatment and non-compliance Treatment can be divided into first line and second line drugs according to the WHO TB treatment regimen and the mechanisms of these will be discussed separately.
2.3 FIRST LINE DRUGS FOR TB.
Any drug used in the anti-TB regiment is expected to have an effective sterilizing activity that is capable of shortening the duration of treatment. Currently, a four-drug regiment is used consisting of INH, RIF, pyrazinamide (PZA) and ethambutol

(EMB). Resistance to first line anti-TB drugs has been linked to mutations in at least 10 genes; katG, inhA, ahpC, kasA and ndh for INH resistance; rpoB for RIF resistance, embB for EMB resistance, pncA for PZA resistance and rpsL and rrs for STR resistance.
2.3:1 ISONIAZID
Isoniazid is a pro-drug that requires activation in isoniazid-susceptible mycobacterial species. Based on in vitro experiments, it has been proposed that the activation of isoniazid results in a number of highly reactive species that are capable of either oxidizing or acylating groups in proteins. However, the actual form of isoniazid that is active in vivo is still unknown. It was observed soon after isoniazid was introduced in the 1950s that isoniazid-resistant clinical isolates frequently lost catalase and peroxidase activity. However, the association of this enzyme with isoniazid activation was not proven until the early 1990s, when the primary mycobacterial catalase-peroxidase gene (katG) was cloned and sequenced . That study and others revealed that mutations in this gene are found in 42–58% of isoniazid-resistant clinical isolates. A large number of different mutations have been described thus far; however, the Ser315Thr mutation is found most often, occurring in approximately 40% of all isoniazid-resistant strains.The Ser315Thr mutation results in an enzyme without the ability to activate isoniazid, but retains approximately 50% of its catalase-peroxidase activity Thus, the altered catalase-peroxidase provides high-level resistance to isoniazid, while retaining a level of oxidative protection that is sufficient to enable the organism to maintain detoxifying activity against host antibacterial radicals. Isolates that carry other, less frequently occurring mutations in katG have been described as exhibiting varying levels of isoniazid resistance and catalase-peroxidase activity. Significant evidence supports the concept that isoniazid blocks the synthesis of cell-wall mycolic acids, the major components of the envelope of M tuberculosis .Two intracellular targets for the drug are currently being actively investigated: the fatty-acid enoyl-acyl carrier protein reductase (InhA), and a complex of an acyl carrier protein (AcpM) and a β-ketoacyl-ACP synthase (KasA).

These enzymes are involved in synthesis of mycolic acids, and mutations have been found in the promoter regions, or less commonly in the genes that encode these proteins (inhA, acpM, and kasA), in clinical isolates that exhibit low-level resistance to isoniazid. It is proposed that over-expression of one or more of these target proteins may be the reason for isoniazid resistance in these strains. However, the role of kasA mutations in isoniazid resistance is presently unclear, because similar mutations were also found in isoniazid-susceptible isolates, and, in cases of isoniazid resistance, mutations were also found in katG or inhA . Mutations in the promoter region of a gene that encodes an alkyl hydroperoxidase reductase (ahpC) have been found in approximately 10% of isoniazid-resistant isolates, but mutations inkatG were also found in these isolates . The resulting over-expression of alkyl hydroperoxidase reductase may compensate for the loss of catalase-peroxidase activity in these mycobacteria.
2.3:2 RIFAMPIN
One of the main reasons for treatment failure and fatal clinical outcome in tuberculosis patients is resistance to rifampin .In addition to a significant early bactericidal effect on metabolically active M tuberculosis, rifampin also exhibits excellent late sterilizing action on semi-dormant organisms undergoing short bursts of metabolic activity. The recognition of this late effect of rifampin, and the additional effectiveness of pyrazinamide, has allowed for the reduction of routine tuberculosis treatment from 1 year to 6 months . Whereas monoresistance to isoniazid is quite common, monoresistance to rifampin is rare. Instead, rifampin resistance occurs most often in strains that are also resistant to isoniazid; thus, rifampin resistance can be used as a surrogate marker for MDR. The mechanism of action of rifampin is to inhibit mycobacterial transcription by targeting DNA-dependent RNA polymerase. The development of resistance to rifampin is due to mutations in a well-defined, 81 base pair (bp) (27 codons) central region of the gene that encodes the β-subunit of RNA polymerase (rpoB) More than 96% of the rifampin-resistant strains contain a mutation in this 81 bp region of rpoB, thus facilitating a straightforward approach to detecting rifampin resistance and/or MDR rapidly .

The most common mutations (65–86%) alter either codon 526 or codon 531, and result in high-level resistance to rifampin (minimal inhibitory concentration [MIC] >32 μg/ml). However, not all mutations within the 81 bp region exhibit the same level of resistance. For example, alterations in codons 511, 516, 518, and 522 result in organisms that have low-level resistance to rifampin and another rifamycin derivative (rifapentin), but remain susceptible to two other rifamycins (rifabutin and rifalazyn) (Parsons LM, unpublished data). Rare mutations associated with rifampin resistance have also been found in the amino-terminal region of rpoB .Most reference laboratories that use molecular methods examine only the 81 bp region. However, it is advisable to screen for amino-terminal mutations in cases in which rifampin resistance is suspected, but no mutation is found in the 81 bp region.
2.3:3 PYRAZINAMIDE
PZA, a nicotinamide analog, was first discovered to have anti-TB activity in 1952. PZA targets an enzyme involved in fatty-acid synthesis and is responsible for killing persistent tubercle bacilli in the initial intensive phase of chemotherapy (Somoskovi et al., 2001). However, during the first two days of treatment, PZA has no bactericidal activity against rapidly growing bacilli (Zhang and Mitchison, 2003). PZA on the other hand has effective sterilizing activity and shortens the chemotherapeutic regiment from 12 to 6 months. PZA is a prodrug which is converted to its active form, pyrazinoic acid (POA) by the pyrazinamidase (PZase) encoded by pncA. The activity of PZAis highly specific for M. tuberculosis, as it has no effect on other mycobacteria.
Mycobacterium bovis is naturally resistant to PZA due to a unique C-G point mutation in codon 169 of the pncA gene. PZA is only active against M. tuberculosis at acidic pH where POA accumulates in the cytoplasm due to an ineffective efflux pump. Accumulation of POA results in the lowering of intracellular pH to a level that inactivates a vital fatty acid synthase (Zimhony et al., 2004). Cloning and characterization of the M. tuberculosis pncA gene by Scorpio et al. (Scorpio and Zhang, 1996) showed that pncA mutations conferred PZA resistance. Various pncA mutations have been identified in more than 70% of PZA resistant clinical isolates scattered throughout the pncA gene but thus far no mutational hot spot has been identified (Scorpio and Zhang, 1996; Sreevatsan et

al., 1997b; Scorpio et al., 1997). In a study from Peru it was found that 59% of MDR patients also had M. tuberculosis resistant to PZA(Saravia et al., 2005).
PZA susceptibility testing is not done routinely in many countries due to technical difficulties. Thus the extent of PZA resistance globally is largely unknown. A study done by Louw et al. (Louw et al., 2006). showed that PZA resistance is common amongst drug-resistant clinical M. tuberculosis isolates from South Africa. PZA resistance was shown to be strongly associated with MDR-TB and therefore it was concluded that PZA should not be relied upon in managing patients with MDR-TB in this setting. PZA resistant isolates had diverse nucleotide changes scattered throughout the pncA gene. Mutations in the pncA gene correlate well with phenotypic resistance to PZA.
However, PZA resistant isolates without pncA mutations were also observed suggesting that another mechanism may be involved in conferring PZA resistance in these isolates. In addition, not all mutations (e.g. Thr114Met) were associated with PZA resistance. In summary, the complexity of PZA resistance makes the development of molecular methods for rapid diagnosis difficult.
2.3:4 ETHAMBUTOL
EMB, a first line drug, is used in combination with other drugs and is specific to the mycobacteria. EMB inhibits an arabinosyl transferase (embB) involved in cell wall biosynthesis (Takayama and Kilburn, 1989). Telenti et al. (Telenti et al., 1997) identified 3 genes, designated embCAB, that encode homologous arabinosyl transferase enzymes involved in EMB resistance. Various studies have identified five mutations in codon 306 [(ATG-GTG), (ATG-CTG), (ATG-ATA), (ATG-ATC) and (ATG-ATT)] which result in three different amino acid substitutions (Val, Leu and Ile) in EMB-resistant isolates (Lee et al., 2002; Sreevatsan et al., 1997c; Mokrousov et al., 2002b; Ramaswamy et al., 2000). These five mutations are associated with 70–90% of all EMB resistant isolates (Ramaswamy and Musser, 1998). Missense mutations were identified in three additional codons: Phe285leu, Phe330Val and Thr630Ile in EMB resistant isolates. MIC’s were generally higher for strains with Met306Leu, Met306Val, Phe330Val and Thr630Ile substitutions than those organisms with Met306Ile substitutions. Mutations outside of codon 306 are present but quite rare. In a study recently done by Johnson et al. (Johnson

et al., 2006) it was shown that genotypic analysis identified mutations at codon 306 of the embB gene rendering resistance to EMB.
However, routine phenotypic analysis failed to identify EMB resistance in 91.4% of resistant isolates in this setting and confirm the difficulty of EMB phenotypic testing. The inability to accurately detect true EMB resistance by the culture based method have a negative impact on the TB control program. Molecular-based methods offers a rapid diagnosis of EMB resistance and could thereby benefit the management of TB patents within days. However a number of EMB phenotypic resistant isolates (about 30%) still lack an identified mutation in embB. There is therefore a need to fully understand the mechanism of EMB resistance in clinical isolates.
2.3:5 STREPTOMYCIN
Streptomycin an aminocyclitol glycoside, is an alternative first line anti-TB drug recommended by the WHO (Cooksey et al., 1996). STR is therefore used in the retreatment of TB cases together with the four drug regimen that includes INH, RIF, PZA and EMB (Brzostek et al., 2004). The effect of STR has been demonstrated to take place at the ribosomal level (Telenti et al., 1993). STR interacts with the 16S rRNA and S12 ribosomal protein (rrs and rpsL) (Escalante et al., 1998; Finken et al., 1993; Sreevatsan et al., 1996; Abbadi et al., 2001), inducing ribosomal changes, which cause misreading of the mRNA and inhibition of protein synthesis. Although STR is a recommended anti-TB drug, is it less effective against M. tuberculosis than INH and RIF. Point mutations in STR resistant isolates have been reported in rrs and rpsL genes in 65–67% of STR resistant isolates (Ramaswamy and Musser, 1998). In the rrs gene a C-T transition at positions 491, 512 and 516, and a A-C/T transversion at position 513 were observed in the highly conserved 530 loop. The 530 loop region is part of the aminoacyl–tRNA binding site and is involved in the decoding process (Carter et al., 2000). The C-T transition at codon 491 is not responsible for resistance to STR as it occurs in both STR resistant and susceptible isolates but is strongly associated with the global spread of M. tuberculosis with a Western Cape F11 genotype (van Rie et al., 2001; Victor et al., 2001). Other mutations in the 915 loop [903 (C-A/G) and 904 (A-G)] have also been reported to have an association with STR resistance

(Carter et al., 2000). Mutations in the rpsL gene at codon 43 (AAG-AGG/ACG) (Lys-Arg/Thr) and codon 88 (AAGAGG/CAG) (Lys-Arg/Gln) are associated with STR resistance. MIC analysis of STR resistant isolates indicate that amino acid replacements in the rpsL genes correlate with a high level of resistance, whereas mutations in the rrs gene correlate with an intermediate level of resistance (Cooksey et al., 1996; Meier et al., 1996). In addition, it has been suggested that low levels of STR resistance are also associated with altered cell permeability or rare mutations which lie outside of the rrs and rpsL genes.
2.4 SECOND LINE OF DRUG FOR TB.
According to the WHO the following drugs can be classified as second line drugs: aminoglycosides (kanamycin and amikacin) polypeptides (capreomycin, viomycin and enviomycin), fluoroquinolones (ofloxacin, ciprofloxacin, and gatifloxacin), D-cycloserine and thionamides (ethionamide and prothionamide) (World Health Organization, 2001). Unfortunately, second-line drugs are inherently more toxic and less effective than first-line drugs (World Health Organization, 2001). Second line drugs are mostly used in the treatment of MDR-TB and as a result prolong the total treatment time from 6 to 9 months (Cheng et al., 2004). The current understanding of molecular mechanisms associated with resistance to second line drugs are summarized in Table 3. The phenotypic methods to detect resistance to second line drugs are less well established and the molecular mechanisms of resistance are also less defined.
2.4:1 FLUOROQUINOLNES
Ciproflaxin (CIP) and ofloxacin (OFL) are the two fluoroquinolones (FQs) used as second-line drugs in MDR-TB treatment (World Health Organization, 2001). The quinolones target and inactivate DNA gyrase, a type II DNA topoisomerase (Cynamon and Sklaney, 2003; Ginsburg et al., 2003; Rattan et al., 1998). DNA gyrase is encoded by gyrA and gyrB (Rattan et al., 1998; Takiff et al., 1994) and introduces negative supercoils in closed circular DNA molecules (Rattan et al., 1998; Ramaswamy and Musser, 1998). The quinolone resistance-determining region (QRDR) is a conserved region in the gyrA (320bp) and gyrB (375bp) genes

(Ginsburg et al., 2003) which is the point of interaction of FQ and gyrase (Ginsburg et al., 2003). Missense mutations in codon 90, 91, and 94 of gyrA are associated with resistance to FQs (Takiff et al., 1994; Xu et al., 1996). A 16-fold increase in resistance was observed for isolates with a Ala90Val substitution, a 30-fold increase for Asp94Asn or His94Tyr and a 60-fold increase for Asp94Gly (Xu et al., 1996). A polymorphism at gyrA codon 95 is not associated with FQ resistance, and is used, with the katG463 polymorphism, to classify M. tuberculosis into 3 phylogenetic groups (Sreevatsan et al., 1997a).
2.4:2 AMINOGLYCOSIDES
Kanamycin (KAN) and Aminokacin (AMI) are aminoglycosides which inhibit protein synthesis and thus cannot be used against dormant M. tuberculosis. Aminoglycosides bind to bacterial ribosomes and disturb the elongation of the peptide chain in the bacteria. Mutations in the rrs gene encoding for 16s rRNA are associated with resistance to KAN and AMI. Nucleotide changes at positions 1400, 1401 and 1483 of the rrs gene have been found to be specifically associated with KAN resistance (Suzuki et al., 1998). An A.G change at codon 1400 in the rrs gene showed resistance to KAN of MICs more that 200 µg/ml (Taniguchi et al., 1997; Suzuki et al., 1998).
2.4:3 ETHIONAMIDE
Ethionamide (ETH) is an important drug in the treatment of MDR-TB, and is mechanistically and structurally analogous to INH. Like INH, ETH is also thought to be a prodrug that is activated by bacterial metabolism. The activated drug then disrupts cell wall biosynthesis by inhibiting mycolic acid synthesis.
Mutations in the promoter of the inhA gene are associated with resistance to INH and ETH (Morlock et al., 2003). EthA catalyses a two step activation of ETH and gene alterations leading to reduced EthA activity lead to ETH resistance

(Engohang-Ndong et al., 2004; Morlock et al., 2003; Vannelli et al., 2002). The expression of ethA is under the control of the neighbouring ethR gene encoding a repressor. EthR negatively regulates the expression of ethA, by binding upstream of ethA to suppress ethA expression (Engohang-Ndong et al., 2004).
2.4:4 D-CYCLOSERINE
D-cycloserine (DCS) is a cyclic analog of D-alanine which is one of the central molecules of the cross linking step of peptidoglycan assembly (Ramaswamy and Musser, 1998; Feng and Barletta, 2003; David, 2001; Caceres et al., 1997). DCS inhibits cell wall synthesis by competing with D-Alanine for the enzymes D-alanyl-D-alanine synthetase (Ddl) and D-alanine racemase (Alr) and also inhibiting the synthesis of these proteins. Over expression of alr cause DCS resistance. A G.T transversion in the alr promoter may lead to the overexpression of alr (Feng and Barletta, 2003; Ramaswamy and Musser, 1998).
2.4:5 PEPTIDES
Viomycin (VIO) and capreomycin (CAP) are basic peptide antibiotics that inhibit prokaryotic protein synthesis and are used as second-line anti-TB drugs. Earlier studies have shown that resistance to VIO in M. smegmatis is caused by alterations in the 30S or 50S ribosomal subunits (Taniguchi et al., 1997). Mutations in the rrs gene that encodes the 16S rRNA is associated with resistance to VIO and CAP, specifically a G.Aor G.T nucleotide change at codon 1473 (Taniguchi et al., 1997).
CHAPTER THREE
3.0 CLINICAL DIAGNOSIS OF TUBERCULOSIS DRUG RESISTANCE

Identification and treatment of infected patients is the primary strategy for the control of TB. The nonspecificity of clinical features of TB and the technical demands in identifying and determining drug susceptibility of M. tuberculosis in clinical specimens make the diagnosis of resistant TB difficult and extremely challenging. It is estimated that only 50%–60% of all patients with TB worldwide are actually diagnosed, and only a small proportion of those with drug-resistant disease are recognized. The identification of acid-fast bacilli via Ziehl-Neelsen staining and direct microscopy is the primary modality for diagnosing TB throughout the world. Smear-based diagnosis, however provides no information on drug susceptibility and has only moderate sensitivity. Fig3.1
The identification of M. tuberculosis by culture is required for confirmation of TB. Mycobacterial culture on solid media takes 3–8 weeks and is not available in many areas. Radiometric culture systems, combined with DNA probe analysis, can reduce the time required to cultivate M. tuberculosis to 1–3 weeks, but the use of these methods throughout much of the developing world is both prohibitively expensive and technically unfeasible. Standard laboratory methods for drug susceptibility testing in mycobacteria are tedious and slow, the reference standard is the proportions method, in which critical concentrations of drugs are placed in solid media, and the number of M. tuberculosis colonies that grow is compared with those growing in drug-free media; if the proportion is ∼1%, the isolate is considered resistant. Results are generally not available for several months after the patient first seeks care. The use of radiometric or fluorescence-based systems speeds the detection of resistance considerably, although results still require a number of weeks from

presentation. As noted, however, the expense of this approach limits its applicability in many parts of the world. A number of methods for more rapidly identifying drug-resistant M. tuberculosis isolates have been proposed. Direct microscopic observation of characteristic colonial morphology in both cultures was shown to have high sensitivity (>90%) and fast turnaround (>10 days) for both initial diagnosis and drug susceptibility testing. Use of redox agents such as Alamar blue or tetrazolium also can identify resistant organisms rapidly and at lower cost than more conventional approaches . Molecular techniques for identifying resistant isolates have largely focused on rifampin resistance because the genetic target is circumscribed and the presence of rifampin resistance is almost always synonymous with MDR-TB. Recent reports of rapid detection of rifampin resistance mutations in clinical specimens by use of molecular beacons, line-probe assays, and PCR techniques are encouraging, but implementation of molecular diagnostics in settings where MDR-TB is common remains an enormous challenge
3.1 TREATMENT OF DRUG RESISTANT TB
The clinical implications of drug-resistant TB depend on the agents to which an infecting strain is resistant. Isoniazid resistance, for example, can be effectively treated with a standard 4-drug regimen for 2 months, followed by 4 months of rifampin and isoniazid; this regimen has very high rates of treatment success despite essential monotherapy in the continuation phase. However, an analysis of patients treated in British MRC trials who had initial resistance to isoniazid found that relapses after cure occurred significantly more often than in patients whose initial isolate was not resistant. Current practice for treating isolates with lone isoniazid resistance is to use rifampin, pyrazinamide, and ethambutol for 6–9 months. Rifampin resistance is associated with poorer clinical outcomes and requires an increase in the duration of therapy from 6 months to at least 9 months (and many experts prefer 12 months). Isolated rifampin resistance can be treated with a regimen of isoniazid, pyrazinamide, streptomycin, and ethambutol for 9 months. Unfortunately, the presence of rifampin resistance is often a marker for MDR-TB, with the majority of such isolates also having resistance to isoniazid—and often to other agents as well. Moreover, isolates that are resistant to rifampin are usually

resistant to other rifamycins, such as rifabutin and rifapentine. The treatment of patients with MDR-TB is much more difficult and relies extensively on second-line drugs, which include fluoroquinolones (moxifloxacin, gatifloxacin, levofloxacin, and ofloxacin), ethionamide, the aminoglycosides kanamycin and amikacin, capreomycin, cycloserine, para-aminosalicylic acid, and clofazimine. Use of these agents, with the possible exception of the fluoroquinolones, is made more difficult by their poorer activity than the first-line drugs and their greater propensity to cause adverse reactions. Fluoroquinolones such as moxifloxacin and levofloxacin have considerable activity against M. tuberculosis and are preferred in the treatment of all MDR-TB cases, unless resistance to this class is also demonstrated. 3.2 POTENTIAL REGIMENS FOR PATIENTS WITH TUBERCULOSIS WITH VARIOUS PATERNS OF DRUG RESISTANCE Surgical treatment of MDR-TB has sometimes proved useful for patients with adequate pulmonary reserve and disease localized to a segment or lobe. Recently, Pomerantz et al. reported the results of 180 resections in 172 patients with MDR-TB, 50% of whom were sputum culture positive at the time of surgery. They noted an operative mortality of 3% and late mortality of 7%. Only 2% of patients remained culture positive during follow-up. Although these results were achieved at a specialty center in highly selected patients, they indicate the potential role that surgery can play in the management of MDR-TB. Treatment of MDR-TB in developing countries is a particular dilemma because the susceptibility testing and second-line agents are usually insufficient. Most national TB-control programs endorse algorithms for treating patients whose infections fail to respond to treatment that rely on the addition of 1–2 second-line agents to the standard first-line regimen. In settings with limited amounts of MDR-TB, these algorithms may be appropriate. However, in settings where MDR-TB is prevalent, such an approach may actually increase levels of resistance by selecting for additional mutants during therapy. A new strategy that uses a standardized regimen of second-line drugs (kanamycin, a fluoroquinolone, pyrazinamide, ethambutol, and ethionamide) after the infection fails to respond to the standard retreatment regimen has been recommended recently by the WHO.

Conversely, Farmer et al. and Kim et al. have advocated tailoring individual treatment regimens through drug susceptibility tests to first- and second-line TB drugs (DOTS-Plus). Using this approach, they have demonstrated treatment response rates of ∼70% in Peruvian patients with MDR-TB and are expanding the program to other regions, including Russia. There is now considerable discussion and research underway regarding the most effective methods for managing MDR-TB in developing countries. Whatever the approach, data concerning efficacy, feasibility, and long-term cost-effectiveness are badly needed.

CHAPTER FOUR
4.0 CHALENGES TO PUBLIC HEALTH AND HEALTH ADMINISTRATORS
Mortality due to infectious disease has fallen dramatically in the past centuries as a result of sanitary and food safety development along with vaccines, antibiotics and other advances in societal conditions and medical sciences. However, the challenges of population growth, urbanization, deforestation, pollution, global climate change and global movement of populations have been associated with a shift in geographical distribution and accelerated diffusion of old and new pathogens resulting in an increased number of outbreaks of Mycobacterium tuberculosis cases.
The health, social, economic, and political consequences associated with these emerging diseases are still significant to public health. In the context of the New Public Health, they are still central issues because of the enormous unfulfilled potential to reduce morbidity and mortality globally. The public health community has learned much about facing new challenges of newly emerging or as yet widespread infectious diseases, as well as about infections as causes of chronic diseases.
Infectious diseases are a significant cause of hospitalization, especially among vulnerable population groups, such as those with chronic disease as AIDS, and the elderly, placing a severe economic burden on health insurance and national health services. This means that greater attention must be paid to immunizing these subgroups especially Tuberculosis.
Global anticipation of the most recent TB epidemic has required international, national and local health authorities to undertake extensive preparation. Despite the preparation, public awareness and acceptance of immunization were insufficient and the pandemic eventually faded from public view by itself. Hence, much effort is still needed to better understand the biological mechanisms of viral transmission and diffusion as well as people’s behaviors/attitudes in the face of risk before we can hope to better combat tomorrow’s outbreaks of Tuberculosis resistance to antibiotics.

The future will undoubtedly bring scientific advances to mankind as discoveries of new microbiological agents of important infectious diseases and those causing chronic diseases arise. Some new discoveries will render diseases preventable and treatable
New knowledge concerning micronutrients, oral diseases and infectious diseases will become part of public health methodology. New methods of producing vaccines against infectious agents like Tuberculosis will bring huge public health gains in the coming decades, but the urgency is great for new vaccines, such as that for Tuberculosis. Infections are unequally spread and unpredictably transferred around the world. Rapid mass transportation and human mobility helps introduce and spread organisms to previously unexposed populations, which can then become resistant to treatments available, thus, rendering the disease Tuberculosis even more dangerous.
There is good reason for cautious optimism given all the progress which has been made in recent years on account of the tremendous efforts in public health. Since 2005, coverage of antiviral treatment in poorer countries has increased tenfold, “resulting in the first decline in the number of AIDS deaths since the epidemic was recognized in the 1980s
OUR HOPE
Optimism but not complacency is justified. Political and financial support is needed to maintain and develop the gains achieved in the past century and to transmit the latest knowledge and technology to many parts of the world where preventable deaths measure in the hundreds of thousands. The potential for saving human life is high with current technology. The New Public Health calls for fair distribution of resources and the timely application of existing knowledge and tools; this mainly rests on political will, funding, initiative and training, all with the aim or eradicating the resistance of Mycobacterium tuberculosis to antibiotics.

CONCLUSION
Drug resistance is a worldwide problem that threatens to undermine effective control of TB. As shown by the recent report of WHO/IUATLD, hot spots of MDR-TB have appeared in regions with weak TB-control programs and misuse of anti-TB drugs. Prevention of drug resistance depends on appropriate treatment of all patients with TB with combination drug regimens and early detection of resistance followed by tailored treatment with second-line agents. In countries with low levels of MDR-TB, efforts should be concentrated on preventing acquired MDR-TB by endorsing and widely implementing the WHO DOT strategy. In regions with high levels of MDR-TB, although concentration on detecting and treating new susceptible TB cases remains critically important, MDR-TB management efforts should tailor treatment by performing drug susceptibility testing. In countries with limited resources, more operational research is needed to define the best cost-effective strategies for individual versus standardized patient management of MDR-TB under national program conditions. The development of better and more rapid diagnostic assays and new classes of anti-TB drugs are urgent priorities for the containment of MDR-TB. However, surgical treatment of TB may be used if medications are ineffective. There are three surgical treatments for pulmonary TB: pneumothorax, in which air is introduced into the chest to collapse the lung; thoracoplasty, in which one or more ribs are removed; and removal of a diseased lung, in whole or in part. It is possible for patients to survive with one healthy lung. Spinal TB may result in a severe deformity that can be corrected surgically.
General measures General measures such as avoidance of overcrowded and unsanitary conditions are also necessary aspects of prevention. Hospital emergency rooms and similar locations can be treated with ultraviolet light, which has an antibacterial effect.

Vaccination Vaccination is one major preventive measure against TB. A vaccine called BCG (Bacillus Calmette-Guérin, named after its French developers) is made from a weakened mycobacterium that infects cattle. Vaccination with BCG does not prevent infection by M. tuberculosis but it does strengthen the immune system of first-time TB patients. As a result, serious complications are less likely to develop. BCG is used more widely in developing countries. The effectiveness of vaccination is still being studied; it is not clear whether the vaccine's effectiveness depends on the population in which it is used or on variations in its formulation.
Prophylactic use of isoniazid INH can be given for the prevention as well as the treatment of TB. INH is effective when given daily over a period of six to 12 months to people in high-risk categories. INH appears to be most beneficial to persons under the age of 25. Because INH carries the risk of side-effects (liver inflammation, nerve damage, changes in mood and behavior), it is important to give it only to persons at special risk.
In summary, the ultimate goals are provision of timely, appropriate, and adequate services. These must be provided, and continually evaluated and updated. A highly infectious tuberculosis patient must have access to state-of-the-art laboratory services, even if the patient resides in an area where a local laboratory is not capable of providing those services. Innovative ideas, such as centralized testing by a large public health laboratory, may be required to achieve this goal. District, state, or national boundaries should not limit access to these laboratory services. The benefits of providing new and more clinically relevant assays to a larger population, especially in high-incidence regions of the world such as Africa and some part of Asia, would be of great public health significance to all populations. Coordinated efforts to monitor and prevent misuse of antibiotics are crucial to reducing the spread of microbial resistance, which can arise due to factors such as self-medication, prescription of antibiotics for viral infection and general overuse of antibiotics.

MAJOR TERMS USE
AFB : - Acid Fast Bacilli
AMI : - Aminokacin
CIP : - Ciproflaxin
DCS : - D-cycloserine
DOT : - Directly Observe Therapy
ETH : - Ethionamide
EMB : - Ethambutol
FQs : - Fluoroquinolones
INH : - Isoniazid
KAN : - Kanamycin
MDR-TB: - Multi Drug Resistance Tuberculosis
MAC : - Mycobacterium avium complex
OFL : - Ofloxacin
POA : - Pyrazinoic Acid
PZase : - Pyrazinamidase
RIP : - Rifampin
STR : - Streptomycin
IUATLD :- The International Union Against Tuberculosis and Lung Disease
VIO : - Vicomycin

REFERENCE Abbadi, S., Rashed, H.G., Morlock, G.P., Woodley, C.L., El Shanawy, O., and Cooksey, R.C. (2001). Characterization of IS6110 restriction fragment length polymorphism patterns and mechanisms of antimicrobial resistance for multidrug-resistant isolates of Mycobacterium tuberculosis from a major reference hospital in Assiut, Egypt. J. Clin. Microbiol. 39, 2330– 2334. Banerjee, A., Dubnau, E., Quemard, A., Balasubramanian,V., Um, K.S., Wilson, T., Collins, D., de Lisle, G., andJacobs, W.R., Jr. (1994). inhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science 263, 227–230. Bastian, I., Rigouts, L., Van Deun, A., and Portaels, F. (2000). Directly observed treatment, short-course strategy and multidrug- resistant tuberculosis: are any modifications required? Bull. World Health Organ 78, 238–251. Bastian, I., Stapledon, R., and Colebunders, R. (2003). Current thinking on the management of tuberculosis. Curr. Opin. Pulm. Med. 9, 186– 192. Baulard, A.R., Betts, J.C., Engohang-Ndong, J., Quan, S., McAdam, R.A., Brennan, P.J., Locht, C., and Besra, G.S. (2000). Activation of the pro-drug ethionamide is regulated in mycobacteria. J. Biol. Chem. 275, 28326 -28331. Beck-Sague, C., Dooley, S.W., Hutton, M.D., Otten, J.,Breeden, A., Crawford, J.T., Pitchenik, A.E., Woodley,C., Cauthen, G., and Jarvis, W.R. (1992). Hospital outbreak of multidrug-resistant Mycobacterium tuberculosis infections. Factors in transmission to staff and HIV-infected patients. JAMA 268, 1280–1286. Bifani, P.J., Plikaytis, B.B., Kapur, V., Stockbauer, K., Pan, X., Lutfey, M.L., Moghazeh, S.L., Eisner, W., Daniel, T.M., Kaplan, M.H., Crawford, J.T., Musser, J.M., and Kreiswirth, B.N. (1996). Origin and interstate spread of a New York City multidrug- resistant Mycobacterium tuberculosis clone family. JAMA 275,

452–457. Bifani, P.J., Mathema, B., Kurepina, N.E., and Kreiswirth, B.N. (2002). Global dissemination of the Mycobacterium tuberculosis W-Beijing family strains. Trends Microbiol.10, 45–52. Bloom BR, Murray CJL (1992)Tuberculosis: commentary on a reemergent killer Science 257:1055-6 Blower, S.M. and Chou, T. (2004). Modeling the emergence of the ‘hot zones’: tuberculosis and the amplification dynamics of drug resistance. Nat. Med 10, 1111–1116. Blumberg, H.M., Burman, W.J., Chaisson, R.E., Daley, C.L., Etkind, S.C., Friedman, L.N., Fujiwara, P., Grzemska, M., Hopewell, P.C. Iseman, M.D., Jasmer, R.M., Koppaka, V., Menzies, R.I., O’Brien, R.J., Reves, R.R., Reichman, L.B., Simone, P.M., Starke, J.R., and Vernon, A.A. (2003). American Thoracic Society/ Centers for Disease Control and Prevention/ Infectious Diseases Society of America: treatment of tuberculosis. Am. J. Respir. Crit Care Med. 167, 603–662. Centers for Disease Control. {CDC} (1999) Achievements in public health, 1900-1999: control of infectious diseases. MMWR Morb Mortal Wkly;48:621-9. Cardoso, R.F., Cooksey, R.C., Morlock, G.P., Barco, P., Cecon, L., Forestiero, F., Leite, C.Q., Sato, D.N., Shikama Md, M.L., Mamizuka , E.M., Hirata, R.D., and Hirata, M.H. (2004). Screening and Characterization of Mutations in Isoniazid- Resistant Mycobacterium tuberculosis Isolates Obtained in Brazil. Antimicrob.Agents Chemother. 48, 3373–3381. Cohen, T. and Murray, M. (2004). Modeling epidemics of multidrug- resistant M. tuberculosis of heterogeneous fitness. Nat. Med. 10, 1117–1121. Cohn, D.L., Bustreo, F., and Raviglione, M.C. (1997). Drug-resistant

tuberculosis: review of the worldwide situation and the WHO/IUATLD Global Surveillance Project. International Union Against Tuberculosis and Lung Disease. Clin. Infect. Dis. 24 Suppl 1, S121- S130. Cooksey, R.C., Morlock, G.P., McQueen, A., Glickman, S.E., and Crawford, J.T. (1996). Characterization of streptomycin Resistance mechanisms among Mycobacterium tuberculosis Isolates from patients in New York City. Antimicrob. Agents Chemother. 40,1186–1188. Crofton, J. and Mitchison, D. (1948). Streptomycin resistance in pulmonary tuberculosis. Br. Med. J. 2, 1009–1015. Dolin PJ, Raviglione MC, Kochi A. (1994) Global tuberculosis incidence and mortality during 1990-2000. Bull World Health Organ; 72 213-2 Dooley, S.W. and Simone, P.M. (1994). The extent and management of drug- resistant tuberculosis: the American experience. Clinical tuberculosis. London:Chapman & Hall 171–189. Edlin, B.R., Tokars, J.I., Grieco, M.H., Crawford, J.T., Williams, J., Sordillo, E.M., Ong, K.R., Kilburn, J.O., Dooley, S.W., Castro, K.G., (1992). An outbreak of multidrug-resistant tuberculosis among hospitalized patients with the acquired immunodeficiency syndrome. 112-132 Eltringham, I.J., Wilson, S.M., and Drobniewski, F.A. (1999). Evaluation of a bacteriophage-based assay (phage amplified biologically assay) as a rapid screen for resistance to isoniazid, ethambutol, streptomycin,pyrazinamide, and ciprofloxacin among clinical isolates of Mycobacterium tuberculosis. J. Clin. Microbiol. 37,3528–3532. Fischl, M.A., Uttamchandani, R.B., Daikos, G.L., Poblete, R.B., Moreno, J.N., Reyes, R.R., Boota, A.M., Thompson, L.M., Cleary, T.J., and Lai, S. (1992). An outbreak of tuberculosis caused by multiple-drug-resistant tubercle bacilli among patients with HIV infection. Ann. Intern. Med. 117, 177–183.

Frieden, T.R., Sherman, L.F., Maw, K.L., Fujiwara, P.I., Crawford, J.T., Nivin, B., Sharp, V., Hewlett, D., Jr., Brudney, K., Alland, D., and Kreisworth, B.N. (1996). A multi-institutional outbreak of highly drug-resistant tuberculosis: epidemiology and clinical outcomes. JAMA 276, 1229–1235. Ginsburg, A.S., Grosset, J.H., and Bishai, W.R. (2003). Fluoroquinolones, tuberculosis, and resistance. Lancet Infect. Dis. 3, 432–442. Heym, B., Saint-Joanis, B., and Cole, S.T. (1999). The molecular basis of isoniazid resistance in Mycobacterium tuberculosis. Tuber. Lung Dis. 79, 267–271. Jereb, J.A., Klevens, R.M., Privett, T.D., Smith, P.J., Crawford, J.T., Sharp, V.L., Davis, B.J., Jarvis, W.R., and Dooley, S.W. (1995). Tuberculosis in health care workers at a hospital with an outbreak of multidrugresistant Mycobacterium tuberculosis. Arch. Intern. Med. 155, 854–859. Johnson, R., Jordaan, A.M., Pretorius, L., Engelke, E., van der, S.G., Kewley, C., Bosman, M., van Helden, P.D., Warren, R., and Victor, T.C. (2006). Ethambutol resistance testing by mutation detection. Int. J. Tuberc. Lung Dis. 10, 68–73. Lienhardt, C. and Ogden, J.A. (2004). Tuberculosis control in resource-poor countries: have we reached the limits of the universal paradigm? Trop. Med. Int. Health 9, 833–841. Rattan, A., Kalia, A., and Ahmad, N. (1998). Multidrugresistant Mycobacterium tuberculosis: molecular perspectives. Emerg. Infect. Dis. 4, 195–209. Raviglione, M.C., Snider, D.E., Jr., and Kochi, A. (1995). Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA 273, 220– 226. Slayden, R.A. and Barry, C.E., III (2000). The genetics and biochemistry of isoniazid resistance in Mycobacterium tuberculosis. Microbes. Infect. 2, 659–669.

Sterling, T.R., Lehmann, H.P., and Frieden, T.R. (2003). Impact of DOTS compared with DOTS-plus on multidrug resistant tuberculosis and tuberculosis deaths: decision analysis. Br. Med. J. 326, 574. Taniguchi, H., Chang, B., Abe, C., Nikaido, Y., Mizuguchi, Y., and Yoshida, S.I. (1997). Molecular analysis of kanamycin and viomycin resistance in Mycobacterium smegmatis by use of the conjugation system. J. Bacteriol. 179, 4795–4801. Victor, T.C., van Helden, P.D., and Warren, R. (2002). Prediction of drug resistance in M. tuberculosis: molecular mechanisms, tools, and applications. IUBMB. Life 53, 231–237. Victor, T.C., Jordaan, A.M., van Rie, A., van der Spuy, G.D., Richardson, M., van Helden, P.D., and Warren, R. (1999). Detection of mutations in drug resistance genes of Mycobacterium tuberculosis by a dot-blot hybridization strategy. Tuber. Lung Dis. 79, 343–348. Walley, J. (1997). DOTS for TB: it’s not easy. Afr. Health 20, 21–22. World Health Organization.( 1997) Anti-tuberculosis drug resistance surveillance 1994 – 1997 (WHO/TB/97.229). World Health Organization (2000) Anti-tuberculosis drug resistance in the world. report no. 2. Prevalence and trends. World Health Organization (2003) Guidelines for drug susceptibility testing for second-line anti-tuberculosis drugs for DOTS-plus. World Health Organization. (2003) WHO report 2003: Global Tuberculosis Control. Zhang, Y., Heym, B., Allen, B., Young, D., and Cole, S. (1992). The catalase- peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature 358, 591–593.
Related Documents