CONTENTS : 1) INTRODUCTION : 2) EPIDIMIOLOGY : 3) ETIOLOGY 4) CLASSIFICATION 5) DIAGOSIS AND DD : 6) TREATMENT :1)init 7) MONITORING 8) PROGNOSIS AND COMPLICATIONS .

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

CONTENTS :
1) INTRODUCTION :
2) EPIDIMIOLOGY :
3) ETIOLOGY
4) CLASSIFICATION
5) DIAGOSIS AND DD :
6) TREATMENT :1)init
7) MONITORING
8) PROGNOSIS AND COMPLICATIONS .
1) INTRODUCTION :

Acute gastroduodenal bleeding is a potentially life-threatening abdominal emergency
that remains a common cause of hospitalization. Upper gastrointestinal bleeding (UGIB)
is defined as bleeding derived from a source proximal to the ligament of Treitz.
The incidence of UGIB is approximately 100 cases per 100,000 population per year.[1] Bleeding from the upper GI tract is approximately 4 times as common as bleeding
from the lower GI tract and is a major cause of morbidity and mortality. Mortality rates
from UGIB are 6-10% overall.[1] (See Epidemiology, below.)
The diagnosis of and therapy for nonvariceal upper gastrointestinal bleeding (UGIB) has
evolved since the late 20th century from passive diagnostic
In patients with UGIB, comorbid illness, rather than actual bleeding, is the major cause
of death. Comorbid illness has been noted in 50.9% of patients, with similar
occurrences in males (48.7%) and females (55.4%).
One or more comorbid illnesses have been noted in 98.3% of mortalities in UGIB; in
72.3% of patients, comorbid illnesses have been noted as the primary cause of death.[3,
4] (See Epidemiology and Prognosis, below.)
Significant comorbidities have become more prevalent as the patient population with
UGIB has become progressively older. In a retrospective chart review by Yavorski et al,
73.2% of deaths occurred in patients older than 60 years.[4] (See Epidemiology and
Prognosis, below.)
Rebleeding or continued bleeding is associated with increased mortality; therefore,
differentiating the patient with a low probability of rebleeding and little comorbidity from
the patient at high risk for rebleeding with serious comorbidities is imperative. (See
Clinical Presentation and Workup, below.)
Annually, approximately 100,000 patients are admitted to US hospitals for therapy for
UGIB.
UGIB is a common occurrence throughout the world. In France, a report concludes that
the mortality from UGIB has decreased from about 11% to 7%; however, a similar report

from Greece finds no decrease in mortality. In a nationwide study from Spain, UGIB was
6 times more common than lower GI bleeding.[18]
The incidence of UGIB is 2-fold greater in males than in females, in all age groups;
however, the death rate is similar in both sexes.[4]
The population with UGIB has become progressively older, with a concurrent increase
in significant comorbidities that increase mortality. Mortality increases with older age
(>60 y) in males and females
Anatomy of the stomach

The stomach lies between the esophagus and the duodenum (the first part of the small
intestine). It is on the left upper part of the abdominal cavity. The top of the stomach lies
against the diaphragm. Lying behind the stomach is the pancreas. The greater
omentum hangs down from the greater curvature
The stomach is surrounded by parasympathetic (stimulant) and orthosympathetic
(inhibitor) plexuses (networks of blood vessels and nerves in
the anterior gastric, posterior, superior and inferior, celiac and myenteric), which
regulate both the secretions activity and the motor (motion) activity of its muscles.In
adult humans, the stomach has a relaxed, near empty volume of about 45 ml. Because
it is a distensible organ, it normally expands to hold about one litre of food,[4] but can
hold as much as two to three litres. The stomach of a newborn human baby will only be
able to retain about 30 ml.
Sections:The stomach is divided into four sections, each of which has different cells
and functions. The sections are:
Cardia Where the contents of the oesophagus empty into the stomach.
Fundus Formed by the upper curvature of the organ.
Body or
CorpusThe main, central region.
PylorusThe lower section of the organ that facilitates emptying the contents into
the small intestine.
Blood supply

Schematic image of the blood supply to the stomach: left and right gastric
artery, left and right gastro-omental artery and short gastric artery.[5]
Picture 1:
A more realistic image, showing the celiac artery and its branches; the liver has been
raised, and the lesser omentum and anterior layer of the greater omentum removed.
The lesser curvature of the stomach is supplied by the right gastric artery inferiorly, and
the left gastric artery superiorly, which also supplies the cardiac region. The greater
curvature is supplied by the right gastroepiploic artery inferiorly and the left
gastroepiploic artery superiorly. The fundus of the stomach, and also the upper portion
of the greater curvature, is supplied by the short gastric artery which arises from splenic
artery.
Like the other parts of the gastrointestinal tract, the stomach walls are made of the
following layers, from inside to outside:

mucosa
The first main layer. This consists of the epithelium and the lamina
propria (composed of loose connective tissue), with a thin layer ofsmooth
muscle called the muscularis mucosae separating it from the submucosa
beneath.
submucosa
This layer lies over the mucosa and consists of fibrous connective tissue,
separating the mucosa from the next layer. The Meissner's plexus is in
this layer (AKA submucosal plexus).
muscularis
externa
Over the submucosa, the muscularis externa in the stomach differs from
that of other GI organs in that it has three layers of smooth muscle instead
of two.
inner oblique layer: This layer is responsible for creating the motion
that churns and physically breaks down the food. It is the only layer of
the three which is not seen in other parts of the digestive system. The
antrum has thicker skin cells in its walls and performs more forceful
contractions than the fundus.
middle circular layer: At this layer, the pylorus is surrounded by a thick
circular muscular wall which is normally tonically constricted forming a
functional (if not anatomically discrete) pyloric sphincter, which
controls the movement of chyme into the duodenum. This layer is
concentric to the longitudinal axis of the stomach.
Auerbach's plexus (AKA myenteric plexus) is found between the outer
longitundinal and the middle circular layer and is responsible for the
innervation of both (causing peristalsis and mixing)
outer longitudinal layer
serosaThis layer is over the muscularis externa, consisting of layers of
connective tissue continuous with the peritoneum.

Ref :
* ^ Sherwood, Lauralee (1997). Human physiology: from cells to systems. Belmont,
CA: worth Pub. Co. ISBN 0-314-09245-5. OCLC 35270048.
* ^ Anne M. R. Agur; Moore, Keith L. (2007). Essential Clinical Anatomy (Point
(Lippincott Williams & Wilkins)). Hagerstown, MD: Lippincott Williams & Wilkins. ISBN 0-
7817-6274-X.OCLC 172964542.; p. 150
Anatomy of duodenum :

The duodenum is the first section of the small intestine. The duodenum precedes the
jejunum and ileum and is the shortest part of the small intestine, where most chemical
digestion takes place. the duodenum is a hollow jointed tube about 10–15 inches (25–
38 centimetres) long connecting the stomach to the jejunum. It begins with the duodenal
bulb and ends at the ligament of Treitz.
Sections
The duodenum is divided into four sections for the purposes of description. The first
three sections curve in a "C"-loop concavity in which the head of the pancreas lies. Only
the first 2 cm of the superior part is mobile (covered by peritoneum) – the distal 3 cm of
the first part along with the rest of the duodenum is retroperitoneal (immobile).
First part
The first (superior) part begins as a continuation of the duodenal end of the pylorus.
From here it passes laterally (right), superiorly and posteriorly, for approximately 5 cm,
before making a sharp curve inferiorly into the superior duodenal flexure (the end of the
superior part). It is the only intraperitoneal portion of the duodenum[8]. Relations:
Anterior
Gallbladder
Quadrate lobe of liver
Posterior
Bile duct
Gastroduodenal artery
Portal vein
Inferior vena cava
Superior

Neck of gallbladder
Hepatoduodenal ligament (lesser omentum)
Inferior
Neck of pancreas
Greater omentum
Second part
The second (descending) part of the duodenum begins at the superior duodenal flexure.
It passes inferiorly to the lower border of vertebral body L3, before making a sharp turn
medially into the inferior duodenal flexure (the end of the descending part).
The pancreatic duct and common bile duct enter the descending duodenum, commonly
known together as the hepatopancreatic duct (or pancreatic duct in the United States),
through themajor duodenal papilla (known as Ampulla of Vater). This part of the
duodenum also contains the minor duodenal papilla, the entrance for the accessory
pancreatic duct(of Santorini). The junction between the
embryological foregut and midgut lies just below the major duodenal papilla.
Third part
The third (inferior/horizontal) part of the duodenum begins at the inferior duodenal
flexure and passes transversely to the left, crossing the left ureter, left testicular/ovarian
vessels, inferior vena cava, abdominal aorta, superior mesenteric artery and
the vertebral column.
Fourth part
The fourth (ascending) part passes superiorly, either anterior to, or to the left of, the
aorta, until it reaches the inferior border of the body of the pancreas. Then, it curves
anteriorly and terminates at the duodenojejunal flexure where it joins the jejunum. The
duodenojejunal flexure is surrounded by a peritoneal fold containing muscle fibres:
the ligament of Treitz.
Blood supply
The duodenum receives arterial blood from two different sources. The transition
between these sources is important as it demarcates the foregut from the midgut.

Proximal to the 2nd part of the duodenum (approximately at the major duodenal papilla
– where the bile duct enters) the arterial supply is from the gastroduodenal artery and its
branch the superior pancreaticoduodenal artery. Distal to this point (the midgut) the
arterial supply is from the superior mesenteric artery (SMA), and its branch the inferior
pancreaticoduodenal artery supplies the 3rd and 4th sections. The superior and inferior
pancreaticoduodenal arteries (from the gastroduodenal artery and SMA respectively)
form an anastomotic loop between the celiac trunk and the SMA; so there is potential
for collateral circulation here.
The venous drainage of the duodenum follows the arteries. Ultimately these veins drain
into the portal system, either directly or indirectly through the splenic or superior
mesenteric vein.
Ref :
* http://bedahunmuh.wordpress.com/algoritma-bedah/
*van Gijn J, Gijselhart JP (2011). "Treitz and his ligament.". Ned Tijdschr
Geneeskd. 155 (8). PMID 21557825.

* http://books.google.com.pe/books?
id=ZR0RKtr7YBoC&pg=PA187&lpg=PA187&dq=duodenum+retroperitoneal+
portions+anatomy&source=bl&ots=VkFzZ4K6_G&sig=AlvypvJPNyT_DJHi6w
ccaYcro8c&hl=en&sa=X&ei=mWwDUIKKK-
qm6gHWpd3_Bg&ved=0CEsQ6AEwBA#v=onepage&q=duodenum
%20retroperitoneal%20portions%20anatomy&f=false
Etiology of gastroduodenal bleding :
1) Ulcer-related UGIB
Peptic ulcer is the most common cause of acute upper GI bleeding and accounts for
approximately 50% of all upper GI bleeding cases (69).
There are approximately 150,000 hospitalizations per year in the United States for evaluation
and treatment of bleeding ulcers. Although hospitalization and surgery for uncomplicated
ulcers have decreased in the United States and Europe over the past three decades, the
number of hospitalizations for hemorrhage associated with ulcers has remained unchanged

(70). Even though ulcer bleeding stops spontaneously in at least 80% of patients, the overall
mortality is also unchanged over the last 30 years, ranging from 6 to 7% in the United States
(70) and averaging
14% in the United Kingdom (71).
Without specific hemostatic intervention, peptic ulcer bleeding continues or recurs in
approximately
20% of patients (72).
Ulcer bleeding starts when the ulcer base erodes into a blood vessel. Spontaneous hemostasis
occurs when a sentinel clot (what is usually actually referred to as a “visible vessel”) plugs the
“side hole” in the vessel.
The clot may then enlarge, remain attached for some time as it organizes, and eventually slough
off, leaving the underlying vessel covered with a flat pigmented spot that fades to leave a clean
ulcer base (72). This process takes less than 72 hours, and rebleeding occurs if the clot
undergoes lysis or falls off prematurely (72).
The most common cause of peptic ulcer is H. pylori infection. Peptic ulcer can present
silently with complications such as hemorrhage, particularly in patients on NSAIDs. PPIs
are the mainstays of therapy and should be held prior to noninvasive diagnostic tests for
H. pylori. Effective eradication of H. pylori involves regimens utilizing multiple antibiotics.
COX-2 inhibitors have lower incidence of causing peptic ulcers. Upper endoscopy
effectively diagnoses peptic ulcers, reduces rebleeding, and allows for appropriate
triage of patients with upper GI bleeding complications.

2) Tumors :
A ) benign tumors:
Most patients with benign stomach and duodenal tumors remain asymptomatic for
long periods of time. When symptoms are present, these depend on the tumor size,
location and complications arising from the tumor (eg: bleeding and ulceration). The
most common presenting symptoms are bleeding (acute or chronic), abdominal pain
and discomfort, nausea, weight loss, intestinal obstruction and as for periampullary
tumors, such as adenomas in the papilla of Vater, recurrent pancreaticobiliary
complications including jaundice, cholangitis, and pancreatitis may occur. Patients
may be referred by another physician to the out-patient clinics with one of the above
symptoms, or be admitted as an emergency due to massive upper gastrointestinal
bleeding. Rarely, they may also present with intestinal obstruction
Types:
epithelial tumors of the stomach
According to results published by Orlowska in 1995, the potential of these
lesions becoming malignant poses a much more worrying problem than the
clinical symptoms themselves. Orlowska found that 1.3% of Hyperplastic
Polyps (HP) and 10% of Adenomas were malignant. Her results support the
belief that gastric HP, like adenomas, can become malignant, thus she
concluded that it is sensible to differentiate a subgroup of Foveolar
Hyperplasia (FH) from HP, since FH will not become malignant unless their
histology changes to that of HP. The view that FH and HP belong to the same
category accounts mainly for the widespread underestimation of the
malignant potential of HP. While it was believed that polyps that become
malignant exceed 2 cm in diameter, Orlowska found cancer cells in very
small polyps (diameter ≈ 5 mm).

Leiomyoma/Leiomyoblastoma
These tumors constitute 2% of all resected neoplasms of the stomach, and
occur most frequently in males between fifty and seventy years old. 10–20%
of leiomyomas of the small intestine are located in the duodenum. They are
usually asymptomatic, but present with anemia in 50% of cases as a result of
mucosal ulceration. Leiomyomas are usually located in the corpus (40%) or
in the antrum (25%). Even when histopathologic tests are conducted, it is
difficult to distinguish benign lesions from malignant ones, partly because
leiomyomas are not encapsulated. The relationship between Leiomyoma
(LM), Leiomyoblastoma (LMB) and Leiomyosarcoma (LMS) is still unknown.
The “enigma” of LMB is its unusual histology, coupled with a somewhat
unpredictable clinical progression. Important in the assessment of the
malignant potential of LMB is the mitotic count, with counts over 5 for 50
high power fields, implying the possibility of malignancy and subsequent
metastasis. The accepted rate of malignant transformation is around 12%.
Duodenal adenomas in familial adenomatous polyposis (FAP)
This association is being increasingly recognized. Early diagnosis and
longterm surveillance of asymptomatic patients with this disease allows the
opportunity to diagnose and treat duodenal tumors at an early stage,
thereby avoiding the dismal prognosis once invasive cancer has developed in
patients who have survive for a mean period of 13 months.
Duodenal (periampullary) tumors
These tumors are rare. Villous and tubulovillous adenomas remain the most
common of such benign tumors and many have probably undergone
malignant change at the time of diagnosis. The presenting symptoms are
uncharacteristic, and endoscopy and ERCP are the most sensitive tools for
diagnosis. In the post-operative histology of one third of patients with
adenoma, we can observe severe third degree dysplasia (1).
Neurogenic gastric and duodenal tumors

These tumors constitute 4% of all benign neoplasms in stomach and 3% to
6% of all small bowel tumors. The most common tumors are neurilemomas
(schwanomas) and neurofibromas. About 40% of tumors present with
bleeding, and mechanical occlusion is not an unusual manifestation in the
duodenum.
Lipoma
Gastric lipoma is a benign tumor that occurs infrequently (1–3% of all benign
gastric tumors), and it is usually located in the antrum. Most lipomas are
found in the submucosa (95%), and they usually occur singly. The most
common clinical presentation (50– 60%) is gastrointestinal hemorrhage
caused by ulceration of the tumor. Currently, CT scanning is the study of
choice which identifies fatty tissue because of its low attenuation numbers,
but the definitive diagnosis is reached with the excision of the lesion and its
anatomopathologic study. In the duodenum we can observe approximately
35% of small intestine lipomas.
Brunner’s Gland Adenoma
This is the most common hamartoma, often found in the proximal
duodenum. It is believed to indicate hyperplasia of Brunner’s glands, perhaps
in response to excessive gastric acid secretion. Such hyperplasia has not
been associated with malignant degeneration. These tumors are usually
smaller than 1 cm, with multiple and polypoid incidence. As they are
asymptomatic, Brunner’s gland adenomas are often incidental findings
during endoscopy or radiographic examination.
1)Alstrup N, Burcharth F, Hauge C, Horn T. Transduodenal excision of tumors of the
ampulla of Vater. Eur J Surg. (1996);162:961–967. [PubMed]
2)Geis W, Baxt R, Kim H. Benign gastric tumors (Minimally invasive approach). Surg
Endosc. (1996);10:407–410. [PubMed]

b)malignant tumors :
The geographic incidence of gastric cancer has changed dramatically over the last few
decades. Prior to 1950, it was the most common cause of cancer death in men, and the
third leading cause of cancer death in women in the U.S. Mortalityfrom gastric cancer in
the United States has declined, perhaps due to dietary changes. This cancer is twice as
common in men than women, twice as common in blacks than whites, and more
common with advancing age. Gastric cancer is also seen in higher rates in Latin
America, Northern Europe and the Far East. It remains the second leading cause
of cancer death worldwide.
Gastric cancer peaks in the seventh decade of life. Often, a delay in diagnosis may
account for the poor prognosis. Fortunately, dedicated research into
itspathogenesis and identification of new risk factors, treatment, and advanced
endoscopic techniques have led to earlier detection of gastric cancer. Recognition
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=5FCA0CB9-5D29-45CF-800E-56E55FBD801C
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=7863A923-17D6-4F28-B5B2-13481ACC53A1
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=BEA63C15-50BB-4F91-A846-01F14F9E9BA5
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D

that Helicobacter pylori infection causes most gastric ulcers has revolutionized the
approach to gastric cancer today. Gastric tumors include adenocarcinoma, non-
Hodgkin’s lymphoma, and carcinoid tumors.
Adenocarcinoma
Adenocarcinomas arising from gastric epithelium are the most common malignancies of
the stomach (90% of cases).
Lymphoma
Primary gastrointestinal lymphoma may be of B- or T-cell type, with primary Hodgkin’s
disease being extremely uncommon.
Hemorrhaging occurs in approximately 6%–10% of patients with advanced
cancer [1]. When visible, it can be particularly distressing to patients and
their caregivers [2, 3]. In some patients, it may be the immediate cause of
death. This article focuses on hemorrhaging that is visible, as opposed to
occult bleeding. It reviews treatment options in the context of advanced
cancer
Bleeding may result from local vessel damage and invasion or from systemic
processes such as disseminated intravascular coagulopathy (DIC) or
abnormalities in platelet functioning and number. The underlying causes of
these abnormalities are varied and include liver failure, medications such as
anticoagulants, chemotherapy, radiotherapy, surgery, and the cancer itself
[4]. Occasionally, concurrent diseases, such as idiopathic thrombocytopenia,
may be responsible. Hemorrhaging may manifest in a variety of ways,
including hematemesis, hematochezia, melena, hemoptysis, hematuria,
epistaxis, vaginal bleeding, or ulcerated skin lesions [4]. It may also present
as echymoses, petechiae, or bruising. Hemorrhage may occur as an acute
catastrophic event, episodic major bleeds, or ongoing low-volume oozing.
These characteristics provide clues as to the underlying cause and guide
management.
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=3E4FD7B4-E7DE-4256-B06F-5D131CBB8059
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=3E4FD7B4-E7DE-4256-B06F-5D131CBB8059
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=B5E6103E-5F6F-4B04-9499-DD433056FC14
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=B5E6103E-5F6F-4B04-9499-DD433056FC14
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=F2DAAC09-AE43-4A42-B03D-49800D789453
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=F4C651E9-3D81-4F84-8C72-72E8A86C6D76
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=C8A68664-CE8A-431B-AB5A-2ECE7F01F9EE
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=B5E6103E-5F6F-4B04-9499-DD433056FC14
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=F4C651E9-3D81-4F84-8C72-72E8A86C6D76
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=34ADA0C9-6387-4FCF-BDAF-0301EE56945D
http://www.hopkins-gi.org/HTD/HTD_Term.aspx?CurrentUDV=31&TD_ID=DFC2B568-7D84-4D77-A0E2-43FEFEBAC7C8

↵1 Pereira J, Mancini I, Bruera E. The management of bleeding in patients
with advanced cancer. In: Portenoy RK, Bruera E, eds. Topics in Palliative
Care, Volume 4. New York: Oxford University Press, 2000:163–183.
↵ Gagnon B, Mancini I, Pereira J et al. Palliative management of bleeding
events in advanced cancer patients. J Palliat Care 1998;14:50–54.
↵ Hoskin P, Makin W. The role of surgical and radiological intervention in
palliation. In: Oncology for Palliative Medicine. Oxford, UK: Oxford University
Press, 1998:229–234.
3)Acute stress gastritis in UGIB
Acute stress gastritis results from predisposing clinical conditions that have the potential
to alter local mucosal protective barriers, such as mucus, bicarbonate, blood flow, and
prostaglandin synthesis. Any disease process that disrupts the balance of these factors
results in diffuse gastric mucosal erosions.
This is most commonly observed in patients who have undergone episodes of shock,
multiple trauma, acute respiratory distress syndrome, systemic respiratory distress
syndrome, acute renal failure, and sepsis.
The principal mechanisms involved are decreased splanchnic mucosal blood flow and
altered gastric luminal acidity.
4)Mallory-Weiss tears in UGIB
Mallory-Weiss tears account for 15% of acute upper GI hemorrhage.[5] Kenneth Mallory
and Soma Weiss first described the syndrome in 1929.[13] The massive UGIB results
from a tear in the mucosa of the gastric cardia.
This linear mucosal laceration is the result of forceful vomiting, retching, coughing, or
straining. These actions create a rapid increase in the gradient between intragastric and
intrathoracic pressures, leading to a gastric mucosal tear from the forceful distention of

the gastroesophageal junction.[14] In 80-90% of cases, this is a single, 1.75- to 2.5-cm
mucosal tear along the lesser curve of the stomach just distal to the gastroesophageal
junction.[13]
5) Dieulafoy lesions in UGIB
The Dieulafoy lesion, first described in 1896, is a vascular malformation of the proximal
stomach, usually within 6 cm of the gastroesophageal junction along the lesser
curvature of the stomach. However, it can occur anywhere along the GI tract. This
lesion accounts for 2-5% of acute UGIB episodes.[15]
Endoscopically, the lesion appears as a large submucosal vessel that has become
ulcerated. Because of the large size of the vessel, bleeding can be massive and brisk.
The vessel rupture usually occurs in the setting of chronic gastritis, which may induce
necrosis of the vessel wall. Alcohol consumption is reportedly associated with the
Dieulafoy lesion.
In a review of 149 cases, the Dieulafoy lesion mostly occurred in men and mostly in
those in their third to tenth decade.[16]
6) NSAIDs in UGIB
NSAIDs cause gastric and duodenal ulcers by inhibiting cyclooxygenase, which causes
decreased mucosal prostaglandin synthesis and results in impaired mucosal defenses.
Daily NSAID use causes an estimated 40-fold increase in gastric ulcer creation and an
8-fold increase in duodenal ulcer creation.[11]

Long-term NSAID use is associated with a 20% incidence in the development of
mucosal ulceration.[17] Medical therapy includes avoiding the ulcerogenic drug and
beginning a histamine-2 (H2)–receptor antagonist or a proton pump inhibitor that
provides mucosal protection.
7)Vomiting-related UGIB
During vomiting, the lower esophagus and upper stomach are forcibly inverted.
Vomiting attributable to any cause can lead to a mucosal tear of the lower esophagus or
upper stomach. The depth of the tear determines the severity of the bleeding. Rarely,
vomiting can result in esophageal rupture (Boerhaave syndrome), leading to bleeding,
mediastinal air entry, left pleural effusion (salivary amylase can be present) or left
pulmonary infiltrate, and subcutaneous emphysema.

CLASSIFICATION:
The gastrointestinal bleeding can be classified in acute or chronic;
A) ACUTE GI BLEEDING
The cardinal features are haematemesis and melaena. Following a bleed from the upper
GI tract, unaltered blood can appear per rectum, but the bleeding must be massive and
is almost always accompanied by shock.
Peptic ulceration is the commonest cause of serious and life-threatening G.I bleeding.
Drugs.
Aspirin and NSAIDs can produce ulcers and erosions. These agents are also responsible
for GI haemorrhage from both duodenal and gastric ulcers, particularly in the elderly.
Corticosteroids in the usual therapeutic doses probably have no influenceon GI
haemorrhage.
Anticoagulants do not cause acute GI haemorrhage per se but bleeding from any cause
is greater if the patient is anticoagulated.

All cases with a recent (i.e. within 48 hours) significant GI bleed should be seen in
hospital.
B) CHRONIC GI BLEEDING
Usually present with iron-deficiency anaemia (IDA).Chronic blood loss producing IDA in
all men and all women after the menopause is always due to bleeding from the GI tract.
The primary concern is to exclude cancer, articularly of the stomach or right colon,and
coeliac disease. Occult blood tests areunhelpful. Chronic blood loss can occur with any
lesion of the GI tract that produces acute bleeding.
FORMS OF PRESSENTING:1)HEMORAGic SHOKThe goal of the patient's physical examination is to evaluate for shock and blood loss.Assessing the patient for hemodynamic instability and clinical signs of poor perfusion is important early in the initial evaluation to properly triage patients with massive hemorrhage to ICU settings. Worrisome clinical signs and symptoms of hemodynamic compromise include tachycardia of more than 100 beats per minute (bpm),systolic blood pressure of less than 90 mm Hg, cool extremities,syncope, and other obvious signs of shock, such as ongoing brisk hematemesis or the occurrence of maroon or bright-red stools, which requires rapid blood transfusion.[24]Pulse and blood pressure should be checked with the patient in supine and upright positions to note the effect of blood loss. Significant changes in vital signs with postural changes indicate an acute blood loss of approximately 20% or more.Assessment of hemorrhagic shock
As previously mentioned, patients who present in hemorrhagic shock have a mortality rate of
up to 30%. Hemorrhage may be classified based on the amount of blood loss, as noted in the
following table.[25
Table Estimated Fluid and Blood Losses in Shock

This
classification scheme aids in understanding the clinical manifestations of hemorrhagic shock. In
early class 1 shock, the patient may have normal vital signs, even with a 15% loss of total blood
volume. As the percentage of blood volume loss increases, pertinent clinical signs, symptoms,
and findings become more apparent.
Although early cardiovascular changes occur as blood loss continues, urine output, as a sign of
end organ renal perfusion, is only mildly affected until class 3 hemorrhage has occurred.
Bornman et al correlated the presence of shock (defined as a pulse rate >100 bpm or SBP < 100
mm Hg) with the incidence of rebleeding rates after initial nonsurgical intervention.[25] They
found that rebleeding (a marker for increased mortality and need for surgery) occurred in 2% of
patients without shock, in 18% with isolated tachycardia, and in 48% with shock.
Schiller et al determined that SBP is a sensitive clinical marker for helping to predict mortality.
They correlated mortality rates based on the patient's SBP at the time of bleeding and found
mortality rates of 8% for patients with SBP more than 100 mm Hg, rates of 17% for SBP of 80-90
mm Hg, and rates of more than 30% for SBP less than 80 mm Hg.
Unless the patient has evidence of shock, orthostatic testing should be performed to assess and
document a hypovolemic state. A positive tilt test finding is defined as an SBP decrease of 10
mm Hg and a pulse rate increase of 20 bpm with standing compared to the supine position. The
ASGE survey was able to correlate orthostatic changes with the incidence of mortality.[26] The
Class 1 Class 2 Class 3 Class 4
Blood Loss, mL Up to 750 750-1500 1500-2000 >2000
Blood Loss,% blood volume Up to 15% 15-30% 30-40% >40%
Pulse Rate, bpm < 100 >100 >120 >140
Blood Pressure Normal Normal Decreased Decreased
Respiratory Rate Normal or Increased Decreased Decreased Decreased
Urine Output, mL/h >35 30-40 20-30 14-20
CNS/Mental Status Slightly
anxious
Mildly
anxious
Anxious,
confused
Confused,
lethargic
Fluid Replacement, 3-for-1 rule Crystalloid Crystalloid Crystalloid and blood Crystalloid and blood

mortality rate when orthostatic changes are present is 13.6%, compared to 8.7% when they are
absent.
Knopp et al studied the use of the tilt test in phlebotomized healthy volunteers and found that
a positive tilt test result consistently correlated with a blood loss of 1000 mL. This becomes
extremely useful when evaluating patients with class 1 hemorrhagic shock.
2)iron deficiency anemia
Anemia is a condition in which the body does not have enough healthy red blood cells. Iron is
an important building block for red blood cells.
iron deficiency anemia related with chronic gastroduodenal bleeding is appearing when the
body is losing more blood cells and iron than the body can replace.
Most of the time, symptoms are mild at first and develop slowly. Symptoms may include:
Feeling grumpy
Feeling weak or tired more often than usual, or with exercise
Headaches
Problems concentrating or thinking
As the anemia gets worse, symptoms may include:
Blue color to the whites of the eyes
Brittle nails
Light-headedness when you stand up
Pale skin color
Shortness of breath
Sore tongue
Symptoms of the conditions that cause iron deficiency anemia include:
Pain in the upper belly (from ulcers)
Weight loss (in people with cancer)
Dark, tar-colored stools or blood

Ref: Mabry-Hernandez IR. Screening for iron deficiency anemia--including iron supplementation for
children and pregnant women. Am Fam Physician. 2009 May 15;79(10):897-8.
Alleyne M, Horne MK, Miller JL. Individualized treatment for iron-deficiency anemia in adults. Am J Med.
2008;121:943-948..
DIAGNOSIS:
A)CLINICAL DIAGNOSIS:
The history and physical examination of the patient provide crucial information for the
initial evaluation of persons presenting with a GI tract hemorrhage.[5]
History findings include weakness, dizziness, syncope associated with hematemesis
(coffee ground vomitus), and melena (black stools with a rotten odor).
Occasionally, a brisk UGIB manifests as hematochezia (red or maroon stools); the
redder the stool, the more rapid the transit, which suggests a large upper tract
hemorrhage. Laine and Shah found that 15% of patients presenting with hematochezia
had an upper gastrointestinal source of bleeding identified at urgent
esophagogastroduodenoscopy.[21]
Patients may have a history of dyspepsia (especially nocturnal symptoms), ulcer
disease, early satiety, and NSAID or aspirin use. A history of recent aspirin ingestion
suggests that the patient may have NSAID gastropathy with an enhanced bleeding
diathesis from poor platelet adhesiveness.[5]
Many patients with UGIB who are taking NSAIDs present without dyspepsia but with
hematemesis or melena as their first symptom, owing to the analgesic effect of the
NSAID. Low-dose aspirin (81 mg) has been associated with UGIB with or without the
addition of NSAID therapy. Using the lowest effective dose for both short-term and long-
term users is recommended.[22]
Patients with a history of ulcers are at an especially increased risk for UGIB when
placed on aspirin or NSAID therapy and should receive continuous acid suppression
with a proton pump inhibitor (PPI). The patient’s ulcer history is also important because

recurrence of ulcer disease is common, especially if he or she has not been treated
for H pylori gastritis or antibiotic therapy has failed.
Patients may present in a more subacute phase, with a history of dyspepsia and occult
intestinal bleeding manifesting as a positive fecal occult blood test result or as iron
deficiency anemia.
A history of chronic alcohol use of more than 50 g/d or chronic hepatitis (B or C)
increases the risk of variceal hemorrhage, gastric antral vascular ectasia (GAVE), or
portal gastropathy.
The finding of subcutaneous emphysema with a history of vomiting is suggestive of
Boerhaave syndrome (esophageal perforation) and requires prompt consideration of
surgical therapy.
The presence of postural hypotension indicates more rapid and severe blood loss.
A meta-analysis documented the incidence of acute UGIB symptoms as follows (see
also Physical Examination, below)[23] :
Hematemesis - 40-50%
Melena - 70-80%
Hematochezia - 15-20%
Either hematochezia or melena - 90-98%
Syncope - 14.4%
Presyncope - 43.2%
Symptoms 30 days prior to admission - No percentage available
Dyspepsia - 18%
Epigastric pain - 41%
Heartburn - 21%
Diffuse abdominal pain - 10%
Dysphagia - 5%
Weight loss - 12%
Jaundice - 5.2%

b)Lab tests :
CBC With Platelet Count
A complete blood count (CBC) is necessary to assess the level of blood loss in a patient
with upper gastrointestinal bleeding. Where possible, having the patient's previous
results is useful to gauge this loss. CBC should be checked frequently (q4-6h) during
the first day.
Hemoglobin Value and Type and Crossmatch Blood
Based on the patient's initial hemoglobin level and clinical assessment of shock, a type
and screen or type and crossmatch should be ordered. The patient should be
crossmatched for 2-6 units, based on the rate of active bleeding. The hemoglobin level
should be monitored serially in order to follow the trend. An unstable hemoglobin level
may signify ongoing hemorrhage requiring further intervention.
Patients generally require blood transfusions because of hypoperfusion and
hypovolemia. Patients with significant comorbid conditions (eg, advanced
cardiovascular disease) should receive blood transfusions to maintain myocardial
oxygen delivery to avoid myocardial ischemia.
BMP, BUN, and Coagulation
The basic metabolic profile (BMP) is useful in evaluating for renal comorbidity; however,
blood in the upper intestine can elevate the BUN (blood urea nitrogen) level as well.
Measurement of coagulation parameters is necessary to assess for continued bleeding.
Abnormalities should be corrected rapidly.
The BUN-to-creatinine ratio increases with upper gastrointestinal bleeding (UGIB). A
ratio of greater than 36 in a patient without renal insufficiency is suggestive of UGIB.
Coagulation Profile

The patient's prothrombin time (PT), activated partial thromboplastin time, and
International Normalized Ratio (INR) should be checked to document the presence of a
coagulopathy. The coagulopathy may be consumptive and associated with a
thrombocytopenia.
A platelet count of less than 50 with active acute hemorrhage requires a platelet
transfusion and fresh frozen plasma in an attempt to replete lost clotting factors.
The coagulopathy could be a marker for advanced liver disease.
The PT is used in calculating the Child-Pugh score.[11] Elevated aminotransferase levels
are a result of hepatocellular injury. Increased levels of alkaline phosphatase and
gamma–glutamyl transpeptidase are indicative of cholestatic liver disease.
Prolongation of the PT based on an INR of more than 1.5 may indicate moderate liver
impairment.
A fibrinogen level of less than 100 mg/dL also indicates advanced liver disease with
extremely poor synthetic function.
Calcium Level
Assessing patients’ calcium levels is useful in identifying individuals with
hyperparathyroidism as well as in monitoring calcium in patients receiving multiple
transfusions of citrated blood. Hypercalcemia increases acid secretion.
Gastrin level
A gastrin level can identify the rare patient with gastrinoma as the cause of upper
gastrointestinal bleeding and multiple ulcers.
c)imagestic studies :
Radiography

Plain radiographs of the abdomen are not usually helpful in the diagnosis of acute upper
gastrointestinal bleeding (UGIB). The pathophysiology of acute UGIB is often mucosal
erosion with subsequent hemorrhage, which is not detected with plain radiographs.
Occasionally, free air under the diaphragm is seen in cases of perforated viscous, and
this may be accompanied by UGIB. Other etiologies, such as upper GI masses (which
usually result in chronic, not acute, UGIB), aneurysms with calcifications, and ascites
suggestive of portal hypertension, may be seen on radiographs.[12]
The radiographic findings, as outlined above, are usually nonspecific. Calcifications
associated with aneurysms, in the aorta or branch vessels, are reliable but rare findings
regarding a source of upper gastrointestinal bleeding.
Chest radiographs should be ordered to exclude aspiration pneumonia, effusion, and
esophageal perforation.
Barium Contrast Studies
Barium contrast studies are not usually helpful and can make endoscopic procedures
more difficult (ie, white barium obscuring the view) and dangerous (ie, risk of aspiration)
CT Scanning
Computed tomography (CT) scanning and ultrasonography may be indicated for the
evaluation of liver disease with cirrhosis, cholecystitis with hemorrhage, pancreatitis with
pseudocyst and hemorrhage, aortoenteric fistula, and other unusual causes of upper GI
hemorrhage.[29] The 2010 ACR criteria state that CT is particularly useful for localizing
obscure UGIB and for evaluating a patient with UGIB and a history of aortic
reconstruction or pancreaticobiliary procedure.[28]
CT scanning is useful in the diagnosis of aortoenteric fistula because images may
reveal thickened bowel, perigraft fluid collection, extraluminal gas, or inflammatory
changes in the area of the duodenum and aortic graft.
Nuclear Medicine Scanning
Nuclear medicine scans may be useful in determining the area of active hemorrhage.
However, the 2010 ACR criteria state that Tc-99m-labeled erythrocyte scans are of

limited value in diagnosing UGIB, but continue to be useful in certain cases of obscure
UGIB.[28]
D)interventional procedures :
Nasogastric Lavage
This procedure may confirm recent bleeding (coffee ground appearance), possible
active bleeding (red blood in the aspirate that does not clear), or a lack of blood in the
stomach (active bleeding less likely but does not exclude an upper GI lesion).
A nasogastric tube is an important diagnostic tool, and tube placement can reduce the
patient's need to vomit. Placement for diagnostic purposes is not contraindicated in
patients with possible esophageal varices.
The characteristics of the nasogastric lavage fluid (eg, red, coffee grounds, clear) and
the stool (eg, red, black, brown) can indicate the severity of the hemorrhage. Red blood
with red stool is associated with an increased mortality rate from more active bleeding
compared with negative aspirate findings with brown stool.
Endoscopy
The development of endoscopy has provided clinicians with the ability for diagnostic
and therapeutic approaches to bleeding from the GI tract. Endoscopic examination of
the upper GI tract provides useful information regarding the source and site of bleeding.[26]
After a positive NG lavage, and even with a negative one if there is high enough
suspicion, the next step should be performance of an esophagogastroduodenoscopy
(EGD) for localization of the bleeding source. Upper endoscopy is the primary
method of evaluating a patient with UGI bleeding as it has a 90–95% success rate
[72]. There is debate as to the timing of early upper endoscopy [74]. Most agree

that an endoscopy should be performed within 24 hours [73] to evaluate UGIB
but several studies are evaluating whether some patients benefit from even earlier
endoscopy. Clearly, patients who have persistent or severe bleeding should undergo
very early endoscopy to avail themselves of the potential of endoscopic therapy
[74].During the procedure, the endoscopist is looking for any lesion that might have
caused the bleeding and for characteristics that suggest the likelihood of recurrence.
Forrest [16] classified peptic ulcers according to features that were associated with
risk of rebleeding (see Table 1).
Table 1 Forrest classification of peptic ulcers
Type Description
Ia Active spurting bleeding
Ib Active oozing bleeding
IIa Non-bleeding but visible vessel
IIb Non-bleeding with adherent clot
IIc Non-bleeding with pigmented ulcer base
III Clean base, no sign of bleeding
most ulcers
with a clean base, are associated with a 5%risk of rebleed and 2% mortality.
Patients
with ulcers that have a flat, pigmented spot on endoscopy have a 10% risk of
further
bleeding and 3% mortality. The presence of adherent clots on top of an ulcer
is associated with a 22% risk of further bleeding and 7% mortality. A visible,
nonbleeding
vessel is correlated with a 43% risk of rebleed and 11% mortality, while

actively bleeding vessels have the highest risk of recurrence at about 55%
and a
mortality of 11% [1]. Other lesions such as Mallory–Weiss tears are
associated with
a low risk (2%) of further bleeding [75]. These associations suggest that
proper evaluation
via endoscopy is crucial, as endoscopic findings are directly associated with
patients’ prognosis and therefore will aid in decisions concerning therapy.
Endoscopic findings and their incidence rate in patients with UGIB include the following:
Duodenal ulcer - 24.3%
Gastric erosion - 23.4%
Gastric ulcer - 21.3%
Esophageal varices - 10.3%
Mallory-Weiss tear - 7.2%
Esophagitis - 6.3%
Duodenitis - 5.8%
Neoplasm - 2.9%
Stomal (marginal) ulcer - 1.8%
Esophageal ulcer - 1.7%
Other/miscellaneous - 6.8%
Endoscopy should be performed immediately after endotracheal intubation (if indicated),
hemodynamic stabilization, and adequate monitoring in an ICU setting have been
achieved. The 2010 American College of Radiology (ACR) appropriateness criteria for
upper gastrointestinal bleeding recommend upper endoscopy as the initial diagnostic
examination for all patients presumed to have UGIB.[28]
In spite of the excellent results with EGD, the procedure is not without complications.
It can cause gastrointestinal perforations, precipitation of gastrointestinal
bleeding, aspiration pneumonia, respiratory arrest, and cardiovascular complications

[11]. The incidence of complications is low, but it is important to be certain
that in each patient the benefit of the procedure outweighs the risk
Angiography
Angiography may be useful if bleeding persists and endoscopy fails to identify a
bleeding site. According to the 2010 ACR guidelines, angiography along with
transcatheter arterial embolization (TAE) should be considered for all patients with a
known source of arterial UGIB that does not respond to endoscopic management, with
active bleeding and a negative endoscopy.[28]
In cases of aortoenteric fistula, angiography requires active bleeding (1 mL/min) to be
diagnostic.
Differential Diagnoses
Abdominal Aortic Aneurysm Barrett Esophagus and Barrett Ulcer
Esophageal Cancer Esophageal Varices Esophagitis
Pancreatic pseudoaneurysm
Cardiac cirrhosis Celiac sprue Cholecystitis Cirrhosis Disseminated intravascular coagulation Strongyloidiasis Syncope von Willebrand disease Zollinger-Ellison syndrome Dengue fever

Emergency treatment in GD bleeding :
The goal of medical therapy in upper gastrointestinal bleeding (UGIB) is to correct
shock and coagulation abnormalities and to stabilize the patient so that further
evaluation and treatment can proceed
Resuscitation of a hemodynamically unstable patient begins with assessing and
addressing the ABCs (ie, airway, breathing, circulation) of initial management.
(Baradarian et al demonstrated that early, aggressive resuscitation can reduce mortality
in acute UGIB.[30] )
Patients presenting with severe blood loss and hemorrhagic shock present with mental
status changes and confusion. In such circumstances, patients cannot protect their
airway, especially when hematemesis is present. In these cases, patients are at
increased risk for aspiration, which is a potentially avoidable complication that can

significantly affect morbidity and mortality. This situation must be recognized early, and
patients should be electively intubated in a controlled setting.
Intravenous access must be obtained. Bilateral, 16-gauge (minimum), upper extremity,
peripheral intravenous lines are adequate for volume resuscitative efforts. Poiseuille’s
law states that the rate of flow through a tube is proportional to the fourth power of the
radius of the cannula and is inversely related to its length.[17] Thus, short, large-bore,
peripheral intravenous lines are adequate for rapid fluid infusion.
According to the 2008 SIGN guideline, either colloid or crystalloid solutions may be
used to attain volume restoration prior to administering blood products.[27] A rough
guideline for the total amount of crystalloid fluid volume needed to correct the
hypovolemia is the 3-for-1 rule. Replace each milliliter of blood loss with 3 mL of
crystalloid fluid. This restores the lost plasma volume. Patients with severe coexisting
medical illnesses, such as cardiovascular and pulmonary diseases, may require
pulmonary artery catheter insertion to closely monitor hemodynamic cardiac
performance profiles during the early resuscitative phase.
Once the ABCs have been addressed, assess the patient's response to resuscitation,
based on evidence of end organ perfusion and oxygen delivery.
Pulmonary artery catheters may be helpful to guide therapy.
Foley catheter placement is mandatory to allow a continuous evaluation of the urinary
output as a guide to renal perfusion. This labor-intensive management should be
performed only in an ICU setting.
Once the maneuvers to resuscitate are underway, insert a nasogastric tube and perform
an aspirate and lavage procedure. This should be the first procedure performed to
determine whether the GI bleeding is emanating from above or below the ligament of
Treitz. If the stomach contains bile but no blood, UGIB is less likely. If the aspirate
reveals clear gastric fluid, a duodenal site of bleeding may still be possible.
In a retrospective review of 1190 patients, Luk et al found that positive nasogastric-tube
aspirate findings were 93% predictive of an upper GI source of bleeding.[32]

According to a study performed by the ASGE, however, a nasogastric-tube aspirate
finding can be negative even in the setting of a large duodenal bleeding ulcer. The study
compared nasogastric-tube aspirate findings with endoscopic findings of the bleeding
source.[20] The investigation revealed that 15.9% of patients with a clear nasogastric-
tube aspirate, 29.9% of patients with coffee-ground aspirate, and 48.2% of patients with
red blood aspirate had an active upper GI source of bleeding at the time of endoscopy.
A study correlated mortality with the color of the fluid from the nasogastric-tube aspirate
and the color of the stool.[29] As shown in the following table, the color of the nasogastric-
tube aspirate can be a prognostic indicator.
Table 4. Effect of the Color of the Nasogastric Aspirate and of the Stool on UGIB
Mortality Rate)
Nasogastric Aspirate Color Stool Color Mortality Rate, %
Clear Brown or red 6
Coffee-ground Brown or black 8.2
Red 19.1
Red blood Black 12.3
Brown 19.4
Red 28.7
Surgery
Primary surgical intervention should be considered in patients with a perforated viscus
(eg, from perforated duodenal ulcer, perforated gastric ulcer, or Boerhaave syndrome).
In patients who are poor operative candidates, conservative treatment with nasogastric
suction and broad-spectrum antibiotics can be instituted. Endoscopic clipping or sewing
techniques have also been used in such patients.

Emergency surgery in UBIG typically entails oversewing the bleeding vessel in the
stomach or duodenum (usually preoperatively identified by endoscopy), vagotomy with
pyloroplasty, or partial gastrectomy. Angiographic obliteration of the bleeding vessel is
considered in patients with poor prognoses.
Treatment-related contraindications :
Contraindications to upper endoscopy include an uncooperative or obtunded patient,
severe cardiac decompensation, acute myocardial infarction (unless active, life-
threatening hemorrhage is present), and perforated viscus (eg, esophagus, stomach,
intestine).
Contraindications to emergency surgery include impaired cardiopulmonary status and
bleeding diathesis.
Esophagogastroduodenoscopy may be more difficult or impossible if the patient has
had previous oropharyngeal surgery or radiation therapy to the oropharynx.
The presence of a Zenker diverticulum can make intubation of the esophagus more
difficult.
Patients with Down syndrome are more sensitive to conscious sedation and should
receive much less sedation, or they should be monitored by an anesthesiologist and/or
intubated prophylactically prior to the procedure.
Hypotension may be exacerbated by sedation; therefore, patients who are unstable
should be given less sedation.
Patients with massive bleeding should be considered for intubation to reduce the
increased risk of aspiration. Such patients should be treated in an intensive care setting.
Ideally, the patient should be stabilized prior to endoscopy and abnormalities in
coagulation should be corrected. When this is not possible, the judgment of an
experienced endoscopist is vital.

Endoscopy
Since the late 1980s, endoscopic techniques to achieve hemostasis for bleeding ulcers
and varices have continued to evolve. Endoscopy is now the method of choice for
controlling active ulcer hemorrhage.
Several randomized clinical trials and meta-analyses have demonstrated and supported
the idea that early endoscopic hemostatic therapy significantly reduces rates of
recurrent bleeding, the need for emergent surgery, and mortality in patients with acute
nonvariceal upper gastrointestinal bleeding (UGIB).
In the early history of endoscopy for UGIB, multiple published studies questioned the
cost-effectiveness of endoscopy in this setting, because it was unclear whether the
outcome was changed. In a setting in which 80% of patients respond to conservative
medical management, studies were hampered by type 2 errors because of the large
number of patients needed to demonstrate statistical significance.
In 1989, a National Institutes of Health (NIH) consensus conference on UGIB concluded
that effective therapy was needed in the presence of active bleeding or a visible vessel.
The conference affirmed that the treatment, when performed by an experienced
endoscopist using 1 of 4 techniques (ie, injection of epinephrine or sclerosants, heater-
probe coagulation, bipolar electrode coagulation, laser coagulation), was proven
effective by the published evidence.
Three other techniques have since been developed: (1) endoscopic application of clips,
(2) use of banding devices, and (3) argon plasma coagulation. Aside from ulcer
hemorrhaging, other causes of gastrointestinal bleeding, including mucosal tears in the
esophagus or upper stomach due to vomiting (Mallory-Weiss tears), venous blebs, and
vascular ectasias, can also be treated with endoscopic coagulation.
Patients should be considered for upper endoscopy if blood loss from the upper
gastrointestinal tract is suspected.

The patient should undergo upper endoscopy prior to any operative intervention in order
to diagnose and localize the bleeding site. Most patients (85-90%) respond to
endoscopic therapy.
The bleeding from gastric cancers and ulcers in leiomyomas does not usually respond
to endoscopic therapy; surgical or radiologic intervention is needed.
Much debate has focused on the significance of the nonbleeding visible vessel (ie,
color, size, diagnostic characteristics, risk of rebleeding) in ulcer hemorrhage. These
matters became clarified after the characteristics and significance of the visible vessel in
the ulcer crater were defined and the evidence for endoscopic therapy was established,
demonstrating that patients requiring therapy to control bleeding or rebleeding could be
diagnosed and treated at the time of the upper endoscopy.
During the endoscopy, the patient is monitored according to analgesia and sedation
guidelines formulated by the American Society of Anesthesiology. The characteristics of
the bleeding lesion are noted, and appropriate therapy is applied when necessary for
high-risk lesions or active bleeding.

Urgent endoscopy
Urgent endoscopy is indicated when patients present with hematemesis, melena, or
postural changes in blood pressure. Cooper et al have demonstrated a lower rate of
rebleeding and shorter length of stay when endoscopy is performed within 24 hours of
admission.[39, 32]
Early endoscopy
Cooper et al studied the effectiveness of performing an early endoscopy within the first
24 hours of an acute UGIB episode and found it to be associated with reductions in the
length of hospital stay, rate of recurrent bleeding, and need for emergent surgical
intervention.[39]
According to the 2010 international consensus on nonvariceal upper gastrointestinal
bleeding, early endoscopy (within 24 hours of presentation) is appropriate for most
patients with UGIB.[40] In a retrospective review involving more than 30,000 cases,
Yavorski et al showed that the mortality rates were more than twice as high for patients
who did not undergo an early endoscopic procedure than for those who did undergo the
procedure early on (11.1% vs 5.2%, respectively).
Endoscopic techniques
The following endoscopic techniques have been developed for achieving hemostasis[5] :
Injection of epinephrine or sclerosants
Bipolar electrocoagulation
Band ligation[41]
Heater probe coagulation
Constant probe pressure tamponade
Argon plasma coagulator
Laser photocoagulation
Rubber band ligation
Application of hemostatic materials, including biologic glue
Application of hemoclips or endoclips

Application of nanopowder (experimental)[42]
Treatment using a combination of endoscopic therapies has become more common.
For example, injection therapy can be applied first to better clarify the bleeding site,
especially in the actively bleeding patient, followed by the application of heater probe or
bipolar (gold) probe coagulation. Injection therapy can also be performed prior to
endoscopic placement of hemoclips.
According to the 2008 SIGN guideline, combinations of endoscopy with an injection of
at least 13 mL of 1:10,000 adrenaline, coupled with either a thermal or mechanical
treatment, are more effective than single modalities.[27]
The 2010 international consensus guidelines on UGIB recommend the use of
endoscopic clips or thermal therapy for high-risk lesions.[40] As another example,
injection therapy is useful prior to laser therapy to reduce the heat sink effect of rapidly
flowing blood prior to laser coagulation.
Heater probe coagulation
The heater probe consists of a resistor electrode enveloped by a titanium capsule and
covered by Teflon (to reduce sticking to the mucosa by the probe). The probe
temperature rises to 250°C (482°F).
Bipolar electrocoagulation
The bipolar probe consists of alternating bands of electrodes producing an electrical
field that heats the mucosa and the vessel. The electrodes are coated with gold to
reduce adhesiveness. The probes are stiff in order to allow adequate pressure to the
vessel to appose the walls and thus produce coaptive coagulation when the electrical-
field energy is transmitted. Careful technique is required to heat-seal the perforated
vessel.
Injection therapy
Injection therapy involves the use of several different solutions injected into and around
the bleeding lesion. The different solutions available for injection are epinephrine,
sclerosants, and clot-producing materials, such as fibrin glue.

Laser therapy
Laser phototherapy uses an Nd:YAG laser to create hemostasis by generating heat and
direct vessel coagulation. This is a noncontact thermal method. It is not as effective as
coaptive coagulation, because it lacks the use of compression to create a tamponade
effect.[1] An additional deterrent to its use is expense.
To perform laser coagulation, the area near the vessel is first injected with epinephrine
to reduce blood flow (reducing the heat-sink effect); then, the laser is applied around the
vessel, producing a wall of edema. Caution must be observed to avoid drilling into the
vessel with the laser, causing increased bleeding.
Hemostatic clips and endoclips
Modification of the delivery system has made clip placement much easier than it was in
the original model. With careful placement of the clip, closing the defect in the vessel is
possible. Usually, multiple clips are applied. They vary in the size and the strength of
the clip. Four models of hemoclips are available: QuickClip2, which is rotatable;
Resolution Clip, which can be reopened after closure; TriClip, which has 3 prongs; and
In Scope, which is a multiclip applier with 4 endoclips. The Resolution Clip seems to be
the current clip of choice by experienced endoscopists.
There are some clinical settings in which endoclips may be preferred over other
hemostatic methods. These include the treatment of ulcers in patients who are
coagulopathic or who require ongoing anticoagulation; in such patients,
electrocoagulation will increase the size, depth, and healing time of treated lesions.
Endoclips may also be preferable in the retreatment of lesions that rebleed after initial
thermal hemostasis.
Ulcers on the lesser curvature, the posterior duodenum, or the cardia increase the
difficulty of clip deployment and clip failure rates.
Larger endoclips have advantages over smaller hemoclips for the hemostasis of chronic
ulcers and the closure of larger lesions.
Argon plasma coagulation

Argon plasma coagulation is a technique in which a stream of electrons flows along a
stream of argon gas. The coagulation is similar to monopolar cautery, with the current
flow going from a point of high current density (the point of contact of the gas with the
mucosa) to an area of low current density (the conductive pad on the patient's body).
The current flows through the body in an erratic path to the pad.
Nanopowder
Nanopowder has been found to be effective in a small study using a porcine model of
arterial bleeding.[42] Further trails are awaited.
Endoscopic treatment decisions
The choice of treatment modality is influenced by the size of the vessel. Animal studies
have demonstrated that the heater probe and bipolar probe are effective for vessels as
large as 2 mm in diameter.
Other techniques (eg, clips, band ligation) or a combination of techniques are needed
for larger vessels or vessels that are not approachable by the heater probe or bipolar
probe. (Surgical intervention should be considered when dealing with vessels larger

than 2 mm in diameter, discounting an enlargement due to the development of
pseudoaneurysm.)
Ulcers with an overlying clot
In the patient who has an ulcer with an overlying clot, attempting to remove the clot by
target washing is critical. Endoscopic removal of the clot by washing or cold snare has
been demonstrated to be effective in reducing the recurrence of bleeding.[47] (Cutting
away the adherent clot is somewhat controversial but is recommended based on study
results from experienced centers.)
The findings under the clot (eg, bleeding vessel, visible vessel, flat spot, clean base,
examples of which are seen in the images below) help to determine the therapy needed
and improve efficacy by allowing treatment to be applied directly to the vessel. (See the
table below.)

Ulcer with active bleeding. Ulcer
with a clean base. Diagram of an ulcer with a clean base.
Ulcer with a flat spot. Ulcer with

an overlying clot. Ulcer with a visible vessel.
Diagram of an ulcer with a visible vessel.
Table 5. Ulcer Characteristics and Correlations (Open Table in a new window)
If the clot cannot be removed by washing, then cutting away the clot using a cold snare
can be considered by experienced endoscopists.
Vigorous washing of the clot formed after therapy is useful in determining the adequacy
of coagulation. A combination of injection with heater probe or bipolar coaptive
coagulation is often used and has been shown to be more effective in patients with
active bleeding.
Active bleeding and rebleeding
The endoscopy should not be started unless the endoscopist is equipped for any
potential lesions (eg, ulcer, varix, angioectasia, tear, tumor). The patient should be
monitored for recurrent bleeding and treated a second time if appropriate. A surgical
consultation should be considered for all patients with gastrointestinal hemorrhage.

Rebleeding occurs in 10-30% of endoscopically treated patients. A second attempt at
endoscopic control is warranted. Some authorities have concerns about the perils of a
second esophagogastroduodenoscopy, which may result in delayed surgery,
perforation, and increased morbidity and mortality rates. However, this approach has
been validated in a large, randomized, controlled trial that showed decreased morbidity
and mortality rates.[48]
Specific characteristics at endoscopy can predict rebleeding. Rebleeding occurs in 55%
of patients who have active bleeding (pulsatile, oozing), in 43% who have a nonbleeding
visible vessel, in 22% who have an ulcer with an adherent clot, and in 0-5% who have
an ulcer with a clean base.
At endoscopy, the prevalence rate for a clean base is 42%, for a flat spot is 20%, for an
adherent clot is 17%, for a visible vessel is 17%, and for active bleeding is 18%. (See
the images below.)
Freeman et al have described a pale, visible vessel that appears to have a very high
risk for rebleeding.[49] This must be differentiated from the presence of a clean ulcer
base.
Good visualization is important. The uncleared fundal pool may obscure an ulcer,
mucosal tear, gastric varices, portal gastropathy, or tumor (eg, leiomyoma,
adenocarcinoma, lymphoma). Endoscopic therapy is recommended for ulcers at
increased risk for rebleeding.
According to the 2008 SIGN guidelines, TIPS should be considered to prevent gastric
variceal rebleeding.[27]
Using a combination of techniques is prudent when re-treating the ulcer site because
the first therapy produced necrosis and weakening of the intestinal wall. Ulcers on the
anterior surface of the stomach and duodenum are at increased risk for perforation.
Using injection as the first step increases the thickness of the submucosal layer, thus
providing an extra margin of safety.

Even operative techniques can have a significant rebleeding rate with significant
mortality, as noted in the study of Poxon et al. In this investigation, the rebleeding rate
was 10% (80% mortality for rebleeders) in patients who underwent a conservative
surgical technique in which the ulcer base was undersewn.[50] This more conservative
approach was compared with the standard surgical technique (ie, vagotomy and
pyloroplasty or partial gastrectomy). The comparison of the conservative approach with
a standard gastrectomy resulted in similar mortality rates, ie, 26% versus 19%,
respectively, with no rebleeding after partial gastrectomy.
Postendoscopic monitoring
Postoperatively, the patient is monitored for recovery from conscious sedation after
endoscopy and from general anesthesia after abdominal surgery. Monitor the patient's
mental status, vital signs, chest, cardiac, and abdominal findings to ascertain that the
patient's clinical status has stabilized and that no complications (eg, aspiration,
perforation, recurrent bleeding, myocardial infarction due to hypotension) have
occurred. Monitor the hemoglobin level.
TREATMENT OF MAJOR CAUSES OF GASTRODUODENAL DISEASES :
1)Bleeding Peptic Ulcer Treatment
Upper GI endoscopy is the most effective diagnostic tool for PUD and has become the
method of choice for controlling active ulcer hemorrhage. Failure of endoscopy to
maintain hemostasis is one of the indications to initiate surgical intervention, especially
in high-risk patients.
Regardless of the endoscopic therapy, however, 10-12% of patients with acute ulcerous
hemorrhage require an operation as the definitive procedure to control the bleeding
ulcer. In most circumstances, the operation is performed emergently, and the
associated mortality rate is as high as 15-25%.
Medical therapy used in conjunction with endoscopy involves PPI administration. PPIs
decrease rebleeding rates in patients with bleeding ulcers associated with an overlying
clot or visible, nonbleeding vessel in the base of the ulcer.[52, 53] Consider transcatheter

angiographic embolization in patients who are poor surgical candidates. Because of the
extensive collateral circulation of the upper GI tract, ischemic complications are rare.
Surgical treatment
If 2 attempts at endoscopic control of the bleeding vessel are unsuccessful, avoid
further attempts (ie, because of increased rebleeding and mortality rates) and pursue
surgical intervention. The indications for surgery in patients with bleeding peptic ulcers
are as follows:
Severe, life-threatening hemorrhage not responsive to resuscitative efforts
Failure of medical therapy and endoscopic hemostasis with persistent recurrent
bleeding
A coexisting reason for surgery, such as perforation, obstruction, or malignancy
Prolonged bleeding, with loss of 50% or more of the patient's blood volume
A second hospitalization for peptic ulcer hemorrhage
The operative treatment options for a bleeding duodenal ulcer historically include
vagotomy, gastric resection, and drainage procedures. Each specific operative option is
associated with its own incidence of ulcer recurrence, postgastrectomy syndrome, and
mortality (as seen in the table below). When making an intraoperative judgment on how
to best manage the bleeding ulcer, it is extremely important for the surgeon to be aware
of these differences.[11]
Table 6. Recurrent Ulcer and Postgastrectomy Syndromes After Operations for
Duodenal Ulcer
Original OperationRecurrence Rate,
%
Postgastrectomy Syndrome
Rate, %
Mortality Rate,
%
Proximal gastric
vagotomy
10 5 0.1
Truncal vagotomy and
drainage
7 20-30 < 1

Truncal vagotomy and
antrectomy
Billroth I or Billroth II
1 30-50 0-5
Truncal vagotomy and
antrectomy
Roux-en-Y
5-10 50-60 0-5
The 3 most common operations performed for a bleeding duodenal ulcer are as
follows[5] :
Truncal vagotomy and pyloroplasty with suture ligation of the bleeding ulcer
Truncal vagotomy and antrectomy with resection or suture ligation of the bleeding
ulcer
Proximal (highly selective) gastric vagotomy with duodenostomy and suture ligation of
the bleeding ulcer
The purpose of the vagotomy is to divide the nerves to the acid-producing body and
fundus of the stomach. This inhibits the acid production that occurs during the cephalic
phase of gastric secretion. Although acid secretion is controlled, gastric motility and
gastric emptying is affected, as indicated in the following table.[11]
Proximal vagotomy abolishes gastric receptive relaxation and impairs storage in the
proximal stomach. As a result, a more rapid gastric emptying of liquids occurs. A
drainage procedure is not required, because the innervation of the antrum and pylorus

is still intact. Because of this, the gastric emptying of solid food is not altered. The
antropyloric mechanism still functions normally and continues to prevent duodenogastric
reflux.
In addition to having the same effects as a highly selective vagotomy in the proximal
stomach, a truncal vagotomy also has marked effects on distal gastric motor function. It
weakens distal gastric peristalsis, thus requiring the creation of a pyloroplasty to
decrease the resistance to outflow from the stomach.
Truncal vagotomy and suture ligation of a bleeding ulcer is a frequently used operation
for treating upper gastrointestinal bleeding (UGIB) in elderly patients with life-
threatening hemorrhage and shock. The procedure can be performed rapidly,
minimizing the time spent in the operating room under general anesthesia.
The principles of suture ligation of a duodenal bleeding ulcer that involves the
gastroduodenal artery require use of the 3-point ligation technique.
The gastroduodenal artery is ligated proximally and distally to the arterial bleeding site.
The third suture is a horizontal mattress placed to control hemorrhage from the
transverse pancreatic branch of the gastroduodenal artery. Failure to place this third
stitch may result in recurrent bleeding that requires another emergent laparotomy of the
abdomen. Vagotomy with antrectomy is reserved for patients whose conditions have
failed to respond to more conservative attempts at surgical intervention and for those
with aggressive and recurrent duodenal ulcer diathesis, such as gastric outlet
obstruction.
When performing a highly selective vagotomy, the duodenostomy or the
pyloroduodenostomy is closed anatomically, preserving the normal pyloric sphincter
muscle. Most commonly, this operation is reserved for young, stable, low-risk patients.
Although long-term follow-up care is still necessary, the recurrent ulcer rate is less than
10% at a mean follow-up of 3.5 years.[5]
Much of what is now known about the operations performed for bleeding duodenal
ulcers came from the era before the etiologic role for H pylori and NSAIDs in the
development of peptic ulcers was understood. Reducing gastric acidity has been proven

to be beneficial, with lower rebleeding rates when using high-dose omeprazole.[1] Although PPIs seem to have an advantage, they have no affect on mortality.
The diagnosis of H pylori infection is important in the management of patients with a
complicated bleeding peptic ulcer. If a patient with a bleeding ulcer requires surgery,
then knowledge of the patient's H pylori status becomes pertinent, because it may help
to guide the decision to choose a particular surgical procedure, eg, simply oversewing
the ulcer as opposed to performing an antiulcer operation. Many studies support the
decision to manage the bleeding ulcer in conjunction with eradication of H pylori.
Bleeding Gastric Ulcer Treatment
The surgical management of bleeding gastric ulcers is slightly different from that of duodenal
ulcers, but the concepts are identical. The 3 most common complications of a gastric ulcer that
mandate emergent surgical intervention are hemorrhage, perforation, and obstruction. The goals
of surgery are to correct the underlying emergent problem, prevent recurrent bleeding or
ulceration, and exclude malignancy.
A bleeding gastric ulcer is most commonly managed by a distal gastrectomy that includes the
ulcer, with a gastroduodenostomy or a gastrojejunostomy reconstruction.
The common operations for the management of a bleeding gastric ulcer include (1) truncal
vagotomy and pyloroplasty with a wedge resection of the ulcer, (2) antrectomy with wedge
excision of the proximal ulcer, (3) distal gastrectomy to include the ulcer, with or without truncal
vagotomy, and (4) wedge resection of the ulcer only.
Types of gastric ulcers
The choice of operation for a bleeding gastric ulcer depends on the location of the ulcer and the
hemodynamic stability of the patient to withstand an operation. Five types of gastric ulcers
occur, based on their location and acid-secretory status.
Type 1 gastric ulcers are located on the lesser curvature of the stomach, at or near the incisura
angularis. These ulcers are not associated with a hypersecretory acid state.

Type 2 ulcers represent a combination of 2 ulcers that are associated with a hypersecretory acid
state. The ulcer locations occur in the body of the stomach in the region of the incisura. The
second ulcer occurs in the duodenum.
Type 3 ulcers are prepyloric ulcers. They are associated with high acid output and are usually
within 3 cm of the pylorus.
Type 4 ulcers are located high on the lesser curvature of the stomach and (as with type 1 ulcers)
are not associated with high acid output.
Type 5 ulcers are related to the ingestion of NSAIDs or aspirin. These ulcers can occur anywhere
in the stomach.
Surgical management according to ulcer type
A vagotomy is added to manage type 2 or type 3 gastric ulcers.
Patients who are hemodynamically stable but have intermittent bleeding requiring blood
transfusions should undergo a truncal vagotomy and distal gastric resection to include the ulcer
for type 1, 2, and 3 ulcers.
In patients who present with life-threatening hemorrhage and a type 1, 2, or 3 ulcer, biopsy and
oversew or excision of the ulcer in combination with a truncal vagotomy and a drainage
procedure should be considered.
Patients with type 4 ulcers usually present with hemorrhage. The left gastric artery should be
ligated, and a biopsy should be performed on the ulcer. Then, the ulcer should be oversewn
through a high gastrotomy.
Rebleeding rates for the procedures that keep the ulcer in situ range from 20-40%.[11]
Gastric bleeding in the immediate postoperative period from recurrent PUD is initially best
managed by endoscopic or angiographic means. If reoperation is required, gastric resection is
usually indicated, because a repeat vagotomy is not reliable. A more definitive solution is
warranted.

According to the 2008 SIGN guidelines, patients with confirmed gastric variceal hemorrhage
require endoscopic therapy, preferably with cyanoacrylate injection.[27]
Stress Gastritis Treatment
Knowledge of the predisposing conditions for stress ulceration allows the clinician to
identify patients at risk for developing gastritis and GI bleeding. Treatment in this group
of high-risk patients should focus on prevention. This is best accomplished by treating
the underlying causes of ulceration.
Aggressive support of hemodynamic parameters ensures adequate mucosal blood flow.
In addition, several strategies have evolved to treat gastric luminal acidity. Histamine
receptor antagonists (HRAs) have proven to be the most effective at controlling
stomach pH. Proton pump inhibitors (PPIs) are superior to the HRAs at suppressing
acid; however, their role in stress ulceration prophylaxis is still being studied.[12]
Stress-related bleeding usually occurs 7-10 days after the initial insult but may manifest
sooner. Initially, endoscopy is the most important diagnostic tool. The acute superficial
erosions are multiple, begin in the fundus, and progress toward the antrum. Ninety
percent of patients stop bleeding with conservative medical therapy that includes NGT
lavage and gastric acid–controlling medications to maintain the gastric luminal pH
above 5.0.[13]
Endoscopic hemostasis is attempted using electrocoagulation, laser, or injection
therapy. Selective angiographic catheterization of the left gastric artery may be
attempted with selective infusion of vasopressin (48-72 h) or embolization using
Gelfoam, coils, or autologous clot to embolize the left gastric artery. Regardless of the
angiographic technique used, it is often unsuccessful because of the rich and extensive
submucosal plexus and collateral circulation within the stomach.
Surgical treatment
Surgical intervention becomes necessary if nonoperative therapy fails and blood loss
continues. The goals of operative treatment are to control bleeding and to reduce

recurrent bleeding and mortality. These patients are at extremely high risk, and the most
expeditious procedure is the best option.
Simply oversewing an actively bleeding erosion is sometimes effective enough to
control the bleeding. In the setting of life-threatening hemorrhage not amenable to
endoscopic control, gastric resection with or without vagotomy with reconstruction may
be necessary.
The type of gastric resection depends on the location of the gastric erosions, ie, whether
they are proximal or distal. The options are antrectomy and subtotal, near total, or total
gastrectomy. Operative mortality rates range from 4-17%.[54] The choice of the initial
operation must be made with an understanding of the patient's condition, the amount
and location of gastric disease, and an accurate assessment of one's technical ability to
rapidly and safely perform a gastric resection. The trend has been to perform less
surgery in general and to minialize the type of surgical procedure performed.[55]
Managing the underlying insult causing the gastric stress ulcerations is also important.
This involves supportive measures to maintain acceptable hemodynamic parameters, to
provide adequate nutritional support in the critically ill patient, and to treat sepsis (if
present).
Mallory-Weiss Syndrome Treatment
Distinguishing Mallory-Weiss syndrome from Boerhaave syndrome is critical. Although
both entities share a common pathogenesis, their management is completely different.
Boerhaave syndrome represents a full-thickness transmural laceration with perforation
of the esophagus. A Gastrografin swallow helps to confirm the presence of the
perforation in most cases, and prompt surgical intervention is necessary to prevent
mediastinitis and sepsis.
On the other hand, surgical intervention in Mallory-Weiss syndrome is required to
achieve hemostasis in only 10% of cases.[13] The bleeding from a Mallory-Weiss tear
spontaneously ceases in 50-80% of patients by the time endoscopy is performed.[13]

For patients in whom bleeding is visualized at endoscopy, the endoscopic treatment
options are electrocoagulation, heater-probe application, hemoclips, epinephrine
injection, or sclerotherapy.
In a series published by Bataller et al, hemostasis was achieved in 100% of patients
with Mallory-Weiss tears by using endoscopic sclerotherapy with epinephrine (1:10,000)
and 1% polidocanol. Other nonoperative therapies are reserved for cases in which
endoscopic attempts at creating hemostasis have failed.
Other available options are angiographic intra-arterial infusion of vasopressin and
transcatheter embolization of branches of the left gastric artery using Gelfoam. Avoid
the balloon tamponade technique using the Sengstaken-Blakemore tube in this
particular circumstance, because this apparatus may extend the mucosal laceration into
a transmural laceration with perforation.[13]
Surgical intervention is indicated in patients with continued bleeding after failed attempts
at nonoperative therapies.
Bleeding from the gastroesophageal junction is visualized through an anterior
gastrotomy. Once the tear is localized, the bleeding is controlled by oversewing the
lesion.
The overall mortality rates for patients who require emergent surgery is 15-25%, in
contrast to a mortality rate of 3% or less for patients whose bleeding stops by the time
of the initial endoscopy.[13]
Dieulafoy Lesion Treatment
The initial endoscopic management of this lesion can be highly successful. In a report
by Norton et al describing their experience with 90 Dieulafoy lesions, endoscopic
management achieved primary hemostasis in 96% of cases.
Contact thermal ablation with a heater probe is the most effective technique, with or
without the combined use of epinephrine to slow or stop the bleeding prior to applying
the heater probe. No studies have been performed that compare surgical and
endoscopic therapy for Dieulafoy lesions.

Although surgical intervention may be required after failed endoscopic therapy,
endoscopy is still an important adjunct for management, because a nonbleeding
Dieulafoy lesion may be undetectable through a gastrotomy.
Because of this potential problem, a combined endoscopic and surgical approach has
been adopted. The vascular malformation can be marked with India ink through the
endoscope.
Rebleeding after endoscopic therapy occurs in 11-15% of cases, with most cases of
rebleeding controlled at repeat endoscopy.[16] (Repeat endoscopy for patients who have
rebleeding has been validated in controlled studies of endoscopy and surgery.)
The 30-day mortality rate from the study by Norton et al was 42%, which is a reflection
of the severe comorbid conditions associated with patients who have bleeding from a
Dieulafoy lesion.
Angiodysplasia Treatment
Bleeding from angiodysplasias can range from occult blood loss to life-threatening
hemorrhage. Because the lesions are small and superficial, endoscopic therapy is
highly successful. Endoscopic treatments and devices used for hemostasis include
lasers, contact heat probes, electrocoagulation, and injection therapy.
The contact probe coagulators have been the most common form of endoscopic
treatment because of their proven success and ability to target a bleeding lesion
tangentially.
Recurrent bleeding can occur from the mucosal injury caused by the coagulation. To
overcome the possibility of a delayed hemorrhage, endoscopic band ligation has been
applied for hemostasis in nonvariceal GI bleeding, including angiodysplasias.[56]
When endoscopic techniques fail, surgical resection becomes necessary. When
pangastric involvement is the source of bleeding, a total gastrectomy may be required;
however, this is extremely rare. Available nonsurgical options include angiography with
catheter-directed vasopressin. Combined hormonal therapy with estrogen and

progesterone for patients in whom the diagnosis is unknown and vascular lesions are
suggested has not been demonstrated to be effective.
Aortoenteric Fistula
Patients with an aortoenteric fistula most often present with a self-limiting sentinel
hemorrhage that is then followed by an exsanguinating, massive GI bleed. For the
warning lesser sentinel bleed in a patient with a history of an abdominal aortic aneurysm
repair or a known aortic aneurysm, the diagnosis of a graft-enteric fistula should be
considered.
An upper endoscopy is the procedure of choice to help diagnose the fistula. It should be
performed to the ligament of Treitz. Upper endoscopy findings also help to exclude
other sources of UGIB.
Once the diagnosis of aortoenteric fistula is confirmed or seriously considered,
emergency surgical intervention is required. In most instances, the aortic graft is
removed after debridement and closure of the duodenum, followed by an extra-
anatomic vascular bypass in order to bypass the ligated aorta and revascularize the
lower extremities.
The perioperative mortality rate is 22-75%,[57] and major complications are common.
Published opinions state that graft excision is not necessary as long as no gross
contamination and purulence are present at the time of laparotomy.[58]Under these
circumstances, antibiotics are administered long-term.
Another option emerging in the surgical literature is the use of endovascular stents to
repair the fistula.[59, 60] Endovascular stent management is technically feasible and may
be used as a bridge to more definitive treatment after hemodynamic stabilization in
high-risk surgical patients.
Stent grafting immediately controls hemorrhage; however, the device is placed in an
infected field. As a result, adjunctive measures, such as long-term antibiotic use,
percutaneous drainage, and bowel diversion, may be required.[61]

According to the 2010 ACR UGIB guidelines, variceal UGIB that does not respond to
endoscopic management should be treated with a transjugular intrahepatic
portosystemic stent shunt (TIPS).[28] The 2008 SIGN guidelines consider TIPS to be the
treatment of choice for uncontrolled variceal bleeding.[27] Primary and secondary TIPS
patency rates have greatly improved with the use of stent grafts in lieu of bare metal
stents. Doppler ultrasonography of the liver is useful for TIPS monitoring, and both
Doppler ultrasonography and CT may be useful for planning TIPS insertion.[28] Although
endovascular stents have been shown to be effective in treating aortoenteric fistulas,
case reports are emerging describing aortoenteric fistulas in patients with abdominal
aortic aneurysm treated initially with stent grafts as well.[62]
Treatment Complications
Complications of endoscopic therapy include aspiration pneumonia and perforation (1%
for the first endoscopic therapy, 3% for the second). Bleeding can be caused by drilling
into the vessel with the laser, by perforating the vessel with an injection, or by removing
the clot with failure to coagulate the vessel.
Tseng et al investigated the cardiovascular effects of emergency endoscopy for UGIB in
patients with stable coronary artery disease (CAD)[63] and found that the patients
commonly experienced, primarily on a subclinical level, ventricular arrhythmias and
myocardial ischemia. The authors' results were as follows:
Incidence of ventricular arrhythmias during endoscopy - 42% (patients with CAD)
versus 16% (controls)
Frequency of ventricular arrhythmias during endoscopy - 1.19 events per minute
(patients with CAD) versus 0.12 events per minute (controls)
Number of patients with ischemic ST changes - 9 patients with CAD versus 1 control
Complications from emergency abdominal surgery include ileus, sepsis, poor wound
healing, and myocardial infarction.
Salvage surgery is associated with a high mortality rate, reflecting the comorbidities of
patients who rebleed or continue to bleed.

Post-treatment Monitoring and Care
The 2010 international consensus guidelines on UGIB state that selected low-risk
patients may be discharged immediately following endoscopy, but high-risk patients
should remain hospitalized for at least 72 hours.[40]
According to the 2008 SIGN guideline, patients with a post-endoscopic Rockall score of
less than 3 have a low risk of rebleeding or death and are candidates for early
discharge and outpatient follow up.[27]
The goal is to maintain the intragastric pH above 6 to maintain the clot. This is most
easily achieved by intravenous proton pump inhibitor (PPI) therapy. After the acute
phase, 72 hours, the coagulated vessel should be stable and the patient can be
switched to oral therapy. If the patient rebleeds or has ongoing bleeding, then repeat of
endoscopic therapy would be considered. If this is not successful, then interventional
radiology is performed to clot the bleeding vessel. If this fails, then surgery would be
considered.
In the subsequent 48-72 hours after endoscopic therapy, the patient should receive
acid-suppressive therapy to maintain a high gastric pH (above 6). A high gastric pH can
be achieved by a continuous infusion of high-dose intravenous PPI therapy.
Patients who do not require endoscopic therapy and do not have other comorbidities
should be considered for discharge.

Patients who did not require endoscopic treatment should receive routine, oral dosing of
a PPI, ie, daily dosing prior to breakfast. Whether high-dose intravenous PPI therapy is
advantageous in this setting remains controversial.
Oral PPI therapy can be achieved with any of the oral PPI preparations.
Patients should be tested for H pylori either by histology of gastric biopsy specimens
taken on initial upper endoscopy or by serologic tests. If positive, H pylori therapy
should be instituted after the patient has been discharged and is in stable condition.
Moreover, H pylori eradication should be confirmed 4-6 weeks later in patients with
UGIB. This can be done by checking the stool for the H pyloriantigen.
Tachyphylaxis may develop within 24 hours if H2-receptor antagonists are
administered.
Data on acid suppression via oral PPI therapy in order to produce a reduction in
rebleeding are limited. High-dose intravenous PPI therapy appears to reduce
rebleeding, but PPIs are not currently approved by the US Food and Drug
Administration (FDA) for such treatment. The patient may be fed after recovery from
local and intravenous anesthesia.
Some patients may require further endoscopic therapy. If repeat endoscopic therapy is
needed, the stomach will empty liquids without residue within 3 hours. The 2008 SIGN
guideline recommends repeat endoscopy and endotherapy within 24 hours when initial
endoscopic treatment is deemed suboptimal or in patients in whom rebleeding will likely
be life threatening.[27]
If the patient remains stable, the patient can then be started on therapy for ulcer
healing.
The patient should continue oral therapy for ulcer disease noted on endoscopy or for
ulcers caused by cautery techniques during endoscopic therapy. The greatest risk for
perforation is usually within the first 48 hours after endoscopic therapy. Long-term acid
suppression therapy should be offered with either full-dose H2-receptor antagonists or
low-dose PPIs to prevent ulcer recurrence or its complications.[64]

Aspirin and NSAID therapies should be avoided in view of their adverse effect on
platelet aggregation and ulcer healing. However, according to the 2010 international
consensus guidelines, resumption of aspirin therapy in patients who require anticlotting
prophylaxis should not be delayed as cardiovascular risks outweigh the risk of
rebleeding.[40]
The 2008 SIGN guidelines state that patients with healed bleeding ulcers who are
negative for H pylori require concomitant PPI therapy at the usual daily dose if NSAIDs,
aspirin, or COX-2 inhibitors are indicated.[27]
If patients must remain on NSAIDs or low-dose aspirin, secondary prophylaxis against
NSAID-induced ulcers should be given. According to the 2010 international consensus
guidelines on UGIB, postdischarge use of aspirin or NSAIDs requires cotherapy with
PPI.[40]
Only lansoprazole (15 mg or 30 mg daily),[65] esomeprazole (20-40 mg daily), and
misoprostol (200 µg 4 times daily)[66] are approved by the FDA for prophylaxis against
NSAID-induced ulcers.
The patient's hemoglobin value should be monitored to assess the efficacy of iron
therapy as an outpatient; further improvement should be noted. Erythropoietin
analogues have been shown to be effective in increasing the rate of hemoglobin
production after ulcer hemorrhage.
Repeat endoscopy should be done in a few weeks in patients with gastric ulcers to
document ulcer healing and to exclude cancer.[67]
Deterrence and Prevention of UGIB

Antibiotic therapy should be given if H pylori is present in the setting of any history of
ulcer disease. Eradication of H pylori has been demonstrated to reduce the risk of
recurrent ulcers and, therefore, recurrent ulcer hemorrhages.
NSAIDs should be avoided. If not possible, they should be used at the lowest dose and
duration.
PPI or misoprostol cotherapy should be used along with NSAIDs.
The use of cyclooxygenase-2 inhibitors has been shown to reduce the risk of ulcer
hemorrhage, although only when not combined with aspirin therapy. Concerns have
been raised about an increase in myocardial infarction and stroke in patients taking
selective cyclooxygenase-2 inhibitors.
As demonstrated in the study by al-Assi et al, the combination of H pylori infection and
NSAID use may increase the risk of ulcer hemorrhage; however, the treatment of H
pylori in patients who are taking NSAIDs remains controversial.[23]
Medication Summary
Rebleeding is associated with increased morbidity and mortality; therefore, this is the
major goal of therapy.
As advised in the 2008 SIGN guidelines, patients with chronic liver disease who present
with acute UGIB should be started on antibiotic therapy.[27]
The use of H2-receptor antagonists has not been shown to be effective in altering the
course of UGIB. A meta-analysis concluded that there was a possible minor benefit with
intravenous H2 antagonists in bleeding gastric ulcers but no benefit in duodenal ulcers.[68]
The use of cyclooxygenase-2 inhibitors has been shown to reduce the risk of ulcer
hemorrhage, although only when not combined with aspirin therapy. Concerns have
been raised about an increase in myocardial infarction and stroke in patients taking
selective cyclooxygenase-2 inhibitors.

As demonstrated in the study by al-Assi et al, the combination of H pylori infection and
NSAID use may increase the risk of ulcer hemorrhage; however, the treatment of H
pylori in patients who are taking NSAIDs remains controversial.[23]
The 2008 SIGN guidelines clearly advocate the discontinuation of aspirin and NSAIDs
in patients who present with peptic ulcer bleeding. When ulcer healing and eradication
of H pylori are confirmed, aspirin and NSAIDs should only be resumed if there is a clear
indication for their use.[27]
Eradication of H pylori can reduce the risk of rebleeding. Current anti-H pyloriregimens
include a variety of drug combinations. Typically, an antimicrobial agent is combined
with an H2-receptor antagonist or a PPI.
The treatment regimens approved by FDA have eradication rates for H pylori of 70-
90%.[11]
Drugs used to treat H pylori infection include the following:
Omeprazole
Ranitidine bismuth citrate
Bismuth subsalicylate
Lansoprazole
Consider for admission and early endoscopy (and calculation of full Rockall
score) if:
aged ≥60 years (all patients who are aged >70 years should be admitted); or witnessed haematemesis or haematochezia (suspected continued bleeding); or haemodynamic disturbance (systolic blood pressure <100 mm Hg, pulse ≥100
beats per minute); or liver disease or known varices.
Other significant comorbidity (especially cardiac disease, malignancy) should also lower the
threshold for admission.
RISK ASSESSMENT AND PROGNOSIS IN GASTRODUODENAL BLEEDING:

Recommendations emphasise early risk stratification, using validated prognostic scales, and early
endoscopy (within 24 hours).6 The following formal risk assessment scores are recommended by
the National Institute for Health and Clinical Excellence (NICE) for all patients with acute UGIB:2
the Blatchford score at first assessment, and the full Rockall score after endoscopy.
The Blatchford risk assessment is designed to be used pre-endoscopy. Scores are added using the
level of urea, haemoglobin, systolic blood pressure, pulse rate, presentation with melaena,
presentation with syncope, hepatic disease and cardiac failure. A score of 0 is the cut-off with any
patient scoring >0 being at risk of requiring an intervention.
The Scottish Intercollegiate Guidelines Network (SIGN) guideline on the management of acute upper
and lower gastrointestinal bleeding recommends that an initial (pre-endoscopic) Rockall score be
calculated for all patients presenting with acute UGIB. In patients with an initial Rockall score >0,
endoscopy is recommended for a full assessment of bleeding risk.3
Rockall Numerical Risk Scoring System4
Initial Score Criteria (prior to gastroscopy)
1) Age:AGE <60->O POINT
60-79->1 POINT
>80->2 POINTS
Shock
Co-morbidity
Additional Criteria for Full Score (after gastroscopy)
"No shock" = (SBP =100 mm Hg, pulse <100/min) - 0 points"Tachycardia" = (SBP =100 mm Hg, pulse =100/min) - 1 point"Hypotension" = (SBP <100 mm Hg) - 2 points
No major comorbidity - 0 pointsCardiac failure, IHD or any major comorbidity - 2 pointsRenal or liver failure, disseminated malignancy - 3 points
Reset

Diagnosis
Major stigmata of recent haemorrhage (SRH)?
PrognosisElderly patients and people with chronic medical conditions withstand acute UGIB less well and have
a higher risk of death.2 Mortality is about 7% in patients admitted with an UGIB. It is as high as 26%
in patients who develop bleeding whilst in hospital having been admitted for another cause.3 A score
of less than 3 using the Rockall system above is associated with an excellent prognosis, whereas a
score of 8 or above is associated with high mortality.4
Factors which affect the risk of death include:
Age: deaths under age 40 years are rare. 30% of patients over 90 years old with UGIB die as a result of the bleed.
Comorbidity: complications are more likely with comorbid disease. Shock: the presence of signs of shock at presentation confers a worse prognosis. Prognosis is also worse with: liver disease, inpatient, continued bleeding after
presentation, haematemesis, haematochezia and elevated blood urea.3
Endoscopic findings: much work has been done on classifying and identifying endoscopic findings which correlate with high risk - for example:
o Mallory-Weiss tears or clean ulcers have a low risk of re-bleeding and death.o Active bleeding in a shocked patient carries an 80% risk of re-bleeding or death.o Non-bleeding but visible vessel has a 50% risk of re-bleeding.
Mortality is reported to be lower in specialist units, possibly because of adherence to protocols rather
than because of technical advances. The prognosis in liver disease relates significantly to the
severity of the liver disease rather than to the magnitude of the haemorrhage.
REF: Document references
Mallory-Weiss tear, no lesion seen nor SRH - 0 pointsAll other diagnoses - 1 pointMalignancy of upper GI tract - 2 points
None or dark spot only - 0 pointsBlood in the upper GI tract, adherent clot, visible or spurting vessel - 2 points
Reset

1. Holster IL, Kuipers EJ; Management of acute nonvariceal upper gastrointestinal bleeding: current policies World J Gastroenterol. 2012 Mar 21;18(11):1202-7. [abstract]
2. Acute upper GI bleeding, NICE Clinical Guideline (June 2012)3. Management of acute upper and lower gastrointestinal bleeding, Scottish
Intercollegiate Guidelines Network - SIGN (September 2008)4. Rockall TA, Logan RF, Devlin HB, et al; Risk assessment after acute upper
gastrointestinal haemorrhage. Gut. 1996 Mar;38(3):316-21. [abstract]5. Baradarian R, Ramdhaney S, Chapalamadugu R, et al; Early intensive resuscitation
of patients with upper gastrointestinal bleeding decreases mortality. Am J Gastroenterol. 2004 Apr;99(4):619-22. [abstract]
6. Barkun AN, Bardou M, Kuipers EJ, et al; International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010 Jan 19;152(2):101-13. [abstract]
7. Cerulli MA et al, Upper Gastrointestinal Bleeding, Medscape, Nov 20118. Stent insertion for bleeding oesophageal varices, NICE Interventional Procedure
Guideline (April 2011)
References:
1. Fallah MA,
Prakash C,
Edmundowicz S.
Acute
gastrointestinal
bleeding. Med
Clin North Am.
Sep
2000;84(5):1183-
208.
2. Pongprasobchai
S, Nimitvilai S,
Chasawat J,
Manatsathit S.
Upper
gastrointestinal

bleeding etiology
score for
predicting
variceal and non-
variceal
bleeding. World J
Gastroenterol.
Mar 7
2009;15(9):1099-
104.
3. Straube S,
Tramèr MR,
Moore RA, Derry
S, McQuay HJ.
Mortality with
upper
gastrointestinal
bleeding and
perforation:
effects of time
and NSAID
use. BMC
Gastroenterol.
Jun 5 2009;9:41.
4. Yavorski RT,
Wong RK,
Maydonovitch C,
Battin LS, Furnia
A, Amundson DE.
Analysis of 3,294
cases of upper
gastrointestinal
bleeding in
military medical
facilities. Am J
Gastroenterol.
Apr
1995;90(4):568-
73.
5. Stabile BE,
Stamos MJ.
Surgical
management of
gastrointestinal
bleeding. Gastroe
nterol Clin North
Am. Mar
2000;29(1):189-
222.
6. Cheung FK, Lau
JY. Management
of massive peptic
ulcer
bleeding. Gastroe
nterol Clin North
Am. Jun
2009;38(2):231-
43.
7. Tiriveedhi K,
Simon J, Cerulli
MA. Does Gastric
Lavage Reduce
the Detection of
Helicobacter
Pylori in the
Biopsy
Specimens?. Gas
trointest Endosc.
2007;67:Abstract
239.
8. Boonpongmanee
S, Fleischer DE,
Pezzullo JC,
Collier K, Mayoral
W, Al-Kawas F,
et al. The
frequency of
peptic ulcer as a
cause of upper-
GI bleeding is
exaggerated. Gas
trointest Endosc.
Jun
2004;59(7):788-
94.
9. Elmunzer BJ,
Young SD,
Inadomi JM,
Schoenfeld P,
Laine L.

Systematic
review of the
predictors of
recurrent
hemorrhage after
endoscopic
hemostatic
therapy for
bleeding peptic
ulcers. Am J
Gastroenterol.
Oct
2008;103(10):262
5-32; quiz 2633.
10.Sung JJ, Tsoi KK,
Ma TK, Yung MY,
Lau JY, Chiu PW.
Causes of
mortality in
patients with
peptic ulcer
bleeding: a
prospective
cohort study of
10,428
cases. Am J
Gastroenterol.
Jan
2010;105(1):84-9.
11.Corson JD,
Williamson RCN,
eds. Surgery.
London, UK:
Mosby-Year
Book; 2001.
12.Stollman N, Metz
DC.
Pathophysiology
and prophylaxis
of stress ulcer in
intensive care
unit patients. J
Crit Care. Mar
2005;20(1):35-45.
13.Cameron JL,
ed. Current
Surgical Therapy.
5th ed. St. Louis,
Mo: Mosby-Year
Book; 1995.
14.Jensen DM,
Machicado GA,
Hirabayashi K.
Randomized
controlled study
of 3 different
types of
hemoclips for
hemostasis of
bleeding canine
acute gastric
ulcers. Gastrointe
st Endosc. Nov
2006;64(5):768-
73.
15.Larson G,
Schmidt T, Gott
J, Bond S,
O'Connor CA,
Richardson JD.
Upper
gastrointestinal
bleeding:
predictors of
outcome. Surger
y. Oct
1986;100(4):765-
73.
16.Reilly HF 3rd, al-
Kawas FH.
Dieulafoy's
lesion. Diagnosis
and
management. Dig
Dis Sci. Dec
1991;36(12):1702
-7.
17.Pilotto A, Maggi
S, Noale M,

Franceschi M,
Parisi G, Crepaldi
G. Development
and validation of
a new
questionnaire for
the evaluation of
upper
gastrointestinal
symptoms in the
elderly
population: a
multicenter
study. J Gerontol
A Biol Sci Med
Sci. Feb
2010;65(2):174-8.
18.Lanas A, Perez-
Aisa MA, Feu F,
Ponce J, Saperas
E, Santolaria S,
et al. A
nationwide study
of mortality
associated with
hospital
admission due to
severe
gastrointestinal
events and those
associated with
nonsteroidal
antiinflammatory
drug use. Am J
Gastroenterol.
Aug
2005;100(8):1685
-93.
19.Peter DJ,
Dougherty JM.
Evaluation of the
patient with
gastrointestinal
bleeding: an
evidence based
approach. Emerg
Med Clin North
Am. Feb
1999;17(1):239-
61, x.
20.Adler DG,
Leighton JA,
Davila RE, Hirota
WK, Jacobson
BC, Qureshi WA,
et al. ASGE
guideline: The
role of endoscopy
in acute non-
variceal upper-GI
hemorrhage. Gas
trointest Endosc.
Oct
2004;60(4):497-
504.
21.Laine L, Shah A.
Randomized trial
of urgent vs.
elective
colonoscopy in
patients
hospitalized with
lower GI
bleeding. Am J
Gastroenterol.
Dec
2010;105(12):263
6-41; quiz 2642.
22.Huang ES, Strate
LL, Ho WW, Lee
SS, Chan AT.
Long-term use of
aspirin and the
risk of
gastrointestinal
bleeding. Am J
Med. May
2011;124(5):426-
33.
23.al-Assi MT,
Genta RM,

Karttunen TJ,
Graham DY.
Ulcer site and
complications:
relation to
Helicobacter
pylori infection
and NSAID
use. Endoscopy.
Feb
1996;28(2):229-
33.
24.American College
of Surgeons
Committee on
Trauma. Advance
d Trauma Life
Support Course
Manual. Chicago,
Ill: American
College of
Surgeons; 1997.
25.Bornman PC,
Theodorou NA,
Shuttleworth RD,
Essel HP, Marks
IN. Importance of
hypovolaemic
shock and
endoscopic signs
in predicting
recurrent
haemorrhage
from peptic
ulceration: a
prospective
evaluation.Br
Med J (Clin Res
Ed). Jul 27
1985;291(6490):2
45-7..
26.Silverstein FE,
Gilbert DA,
Tedesco FJ,
Buenger NK,
Persing J. The
national ASGE
survey on upper
gastrointestinal
bleeding. II.
Clinical
prognostic
factors. Gastroint
est Endosc. May
1981;27(2):80-93.
27.Scottish
Intercollegiate
Guidelines
Network
(SIGN). Manage
ment of acute
upper and lower
gastrointestinal
bleeding. A
national clinical
guideline. (SIGN
publication; no.
105). Edinburgh
(Scotland):
Scottish
Intercollegiate
Guidelines
Network (SIGN);
Sep 2008:
28.Schenker MP,
Majdalany BS,
Funaki BS, et al;
and Expert Panel
on Vascular
Imaging and
Interventional
Radiology. ACR
Appropriateness
Criteria® upper
gastrointestinal
bleeding. [online
publication].
Reston (VA):
American College
of Radiology
(ACR); 2010

29.Frattaroli FM,
Casciani E,
Spoletini D,
Polettini E,
Nunziale A,
Bertini L, et al.
Prospective study
comparing multi-
detector row CT
and endoscopy in
acute
gastrointestinal
bleeding. World J
Surg. Oct
2009;33(10):2209
-17.
30.Baradarian R,
Ramdhaney S,
Chapalamadugu
R, Skoczylas L,
Wang K, Rivilis S,
et al. Early
intensive
resuscitation of
patients with
upper
gastrointestinal
bleeding
decreases
mortality. Am J
Gastroenterol.
Apr
2004;99(4):619-
22.
31.Kaplan LJ,
McPartland K,
Santora TA,
Trooskin SZ.
Start with a
subjective
assessment of
skin temperature
to identify
hypoperfusion in
intensive care
unit patients. J
Trauma. Apr
2001;50(4):620-7;
discussion 627-8.
32.Sarin N, Monga
N, Adams PC.
Time to
endoscopy and
outcomes in
upper
gastrointestinal
bleeding. Can J
Gastroenterol. Jul
2009;23(7):489-
93.
33.Green FW Jr,
Kaplan MM,
Curtis LE, Levine
PH. Effect of acid
and pepsin on
blood coagulation
and platelet
aggregation. A
possible
contributor
prolonged
gastroduodenal
mucosal
hemorrhage
.Gastroenterology
. Jan
1978;74(1):38-43.
34.Lau JY, Leung
WK, Wu JC, et al.
Omeprazole
before endoscopy
in patients with
gastrointestinal
bleeding.N Engl J
Med. Apr 19
2007;356(16):163
1-40.
35.Barkun AN,
Herba K, Adam
V, Kennedy W,

Fallone CA,
Bardou M. High-
dose intravenous
proton pump
inhibition
following
endoscopic
therapy in the
acute
management of
patients with
bleeding peptic
ulcers in the USA
and Canada: a
cost-
effectiveness
analysis. Aliment
Pharmacol Ther.
Mar 1
2004;19(5):591-
600.
36.Laine L, Shah A,
Bemanian S.
Intragastric pH
with oral vs
intravenous bolus
plus infusion
proton-pump
inhibitor therapy
in patients with
bleeding
ulcers. Gastroent
erology. Jun
2008;134(7):1836
-41.
37. [Best Evidence]
Leontiadis GI,
Sharma VK,
Howden CW.
Proton pump
inhibitor therapy
for peptic ulcer
bleeding:
Cochrane
collaboration
meta-analysis of
randomized
controlled
trials. Mayo Clin
Proc. Mar
2007;82(3):286-
96.
38. [Best Evidence]
Leontiadis GI,
Sharma VK,
Howden CW.
Systematic
review and meta-
analysis of proton
pump inhibitor
therapy in peptic
ulcer
bleeding. BMJ.
Mar 12
2005;330(7491):5
68.
39.Cooper GS, Chak
A, Way LE,
Hammar PJ,
Harper DL,
Rosenthal GE.
Early endoscopy
in upper
gastrointestinal
hemorrhage:
associations with
recurrent
bleeding, surgery,
and length of
hospital
stay.Gastrointest
Endosc. Feb
1999;49(2):145-
52.
40. [Guideline]
Barkun AN,
Bardou M,
Kuipers EJ, et al.
International
consensus
recommendations

on the
management of
patients with
nonvariceal upper
gastrointestinal
bleeding. Ann
Intern Med. Jan
19
2010;152(2):101-
13.
41.Matsui S,
Kamisako T,
Kudo M, Inoue R.
Endoscopic band
ligation for control
of nonvariceal
upper GI
hemorrhage:
comparison with
bipolar
electrocoagulatio
n. Gastrointest
Endosc. Feb
2002;55(2):214-8.
42.Giday SA, Kim Y,
Krishnamurty
DM, et al. Long-
term randomized
controlled trial of
a novel
nanopowder
hemostatic agent
(TC-325) for
control of severe
arterial upper
gastrointestinal
bleeding in a
porcine
model
.Endoscopy. Apr
2011;43(4):296-9.
43.Vargas HE,
Gerber D, Abu-
Elmagd K.
Management of
portal
hypertension-
related
bleeding. Surg
Clin North Am.
Feb
1999;79(1):1-22.
44.Cipolletta L,
Bianco MA,
Marmo R,
Rotondano G,
Piscopo R,
Vingiani AM, et
al. Endoclips
versus heater
probe in
preventing early
recurrent
bleeding from
peptic ulcer: a
prospective and
randomized
trial.Gastrointest
Endosc. Feb
2001;53(2):147-
51.
45.Lin HJ, Hsieh YH,
Tseng GY, Perng
CL, Chang FY,
Lee SD. A
prospective,
randomized trial
of endoscopic
hemoclip versus
heater probe
thermocoagulatio
n for peptic ulcer
bleeding. Am J
Gastroenterol.
Sep
2002;97(9):2250-
4.
46. [Best Evidence]
Saltzman JR,
Strate LL, Di

Sena V, Huang
C, Merrifield B,
Ookubo R, et al.
Prospective trial
of endoscopic
clips versus
combination
therapy in upper
GI bleeding
(PROTECCT--
UGI
bleeding). Am J
Gastroenterol. Jul
2005;100(7):1503
-8.
47.Bini EJ, Cohen J.
Endoscopic
treatment
compared with
medical therapy
for the prevention
of recurrent ulcer
hemorrhage in
patients with
adherent
clots. Gastrointes
t Endosc. Nov
2003;58(5):707-
14.
48.Lau JY, Sung JJ,
Lam YH, et al.
Endoscopic
retreatment
compared with
surgery in
patients with
recurrent
bleeding after
initial endoscopic
control of
bleeding
ulcers. N Engl J
Med. Mar 11
1999;340(10):751
-6.
49.Freeman ML,
Cass OW, Peine
CJ, Onstad GR.
The non-bleeding
visible vessel
versus the
sentinel clot:
natural history
and risk of
rebleeding. Gastr
ointest Endosc.
May-Jun
1993;39(3):359-
66.
50.Poxon VA,
Keighley MR,
Dykes PW,
Heppinstall K,
Jaderberg M.
Comparison of
minimal and
conventional
surgery in
patients with
bleeding peptic
ulcer: a
multicentre
trial. Br J Surg.
Nov
1991;78(11):1344
-5.
51.Lau JY, Sung JJ,
Lam YH, Chan
AC, Ng EK, Lee
DW, et al.
Endoscopic
retreatment
compared with
surgery in
patients with
recurrent
bleeding after
initial endoscopic
control of
bleeding

ulcers. N Engl J
Med. Mar 11
1999;340(10):751
-6.
52.Leontiadis GI,
Howden CW. The
role of proton
pump inhibitors in
the management
of upper
gastrointestinal
bleeding. Gastroe
nterol Clin North
Am. Jun
2009;38(2):199-
213.
53.Targownik LE,
Bolton JM, Metge
CJ, Leung S,
Sareen J.
Selective
serotonin
reuptake
inhibitors are
associated with a
modest increase
in the risk of
upper
gastrointestinal
bleeding. Am J
Gastroenterol.
Jun
2009;104(6):1475
-82.
54.So JB, Yam A,
Cheah WK, Kum
CK, Goh PM.
Risk factors
related to
operative
mortality and
morbidity in
patients
undergoing
emergency
gastrectomy. Br J
Surg. Dec
2000;87(12):1702
-7.
55.Sadic J,
Borgström A,
Manjer J, Toth E,
Lindell G.
Bleeding peptic
ulcer - time
trends in
incidence,
treatment and
mortality in
Sweden. Aliment
Pharmacol Ther.
Aug 15
2009;30(4):392-8.
56.Jo Y, Matsumoto
T, Aoyagi K,
Yano Y,
Kawasaki A,
Fujishima M.
Endoscopic band
ligation device for
bleeding gastric
angiodysplasia. G
astrointest
Endosc. Oct
1999;50(4):599.
57.Socrate AM,
Rosati L, Locati
P. Surgical
treatment of
aorto-enteric
fistulas. Minerva
Cardioangiol. Feb
2001;49(1):37-45
58.Young RM,
Cherry KJ Jr,
Davis PM,
Gloviczki P,
Bower TC,
Panneton JM, et
al. The results of

in situ prosthetic
replacement for
infected aortic
grafts. Am J
Surg. Aug
1999;178(2):136-
40.
59.Deshpande A,
Lovelock M,
Mossop P,
Denton M,
Vidovich J, Gurry
J. Endovascular
repair of an
aortoenteric
fistula in a high-
risk patient. J
Endovasc Surg.
Nov
1999;6(4):379-
84Lonn L, Dias
N, Veith
Schroeder T,
Resch T. Is
EVAR the
treatment of
choice for
aortoenteric
fistula?. J
Cardiovasc Surg
(Torino). Jun
2010;51(3):319-
27.
60.Burks JA Jr,
Faries PL,
Gravereaux EC,
Hollier LH, Marin
ML.
Endovascular
repair of bleeding
aortoenteric
fistulas: a 5-year
experience. J
Vasc Surg. Dec
2001;34(6):1055-
9. .
61.Abou-Zamzam
AM Jr, Bianchi C,
Mazraany W,
Teruya TH,
Hopewell J,
Vannix RS, et al.
Aortoenteric
fistula
development
following
endovascular
abdominal aortic
aneurysm repair:
a case
report. Ann Vasc
Surg. Mar
2003;17(2):119-
22.
62.Tseng PH, Liou
JM, Lee YC, Lin
LY, Yan-Zhen Liu
A, Chang DC, et
al. Emergency
endoscopy for
upper
gastrointestinal
bleeding in
patients with
coronary artery
disease. Am J
Emerg Med. Sep
2009;27(7):802-9.
63.Penston JG,
Wormsley KG.
Review article:
maintenance
treatment with
H2-receptor
antagonists for
peptic ulcer
disease. Aliment
Pharmacol Ther.
Feb 1992;6(1):3-
29.

64.Lai KC, Lam SK,
Chu KM, Wong
BC, Hui WM, Hu
WH, et al.
Lansoprazole for
the prevention of
recurrences of
ulcer
complications
from long-term
low-dose aspirin
use. N Engl J
Med. Jun 27
2002;346(26):203
3-8.
65.Raskin JB, White
RH, Jackson JE,
Weaver AL,
Tindall EA, Lies
RB, et al.
Misoprostol
dosage in the
prevention of
nonsteroidal anti-
inflammatory
drug-induced
gastric and
duodenal ulcers:
a comparison of
three
regimens. Ann
Intern Med. Sep 1
1995;123(5):344-
50.
66.Podolsky I,
Storms PR,
Richardson CT,
Peterson WL,
Fordtran JS.
Gastric
adenocarcinoma
masquerading
endoscopically as
benign gastric
ulcer. A five-year
experience. Dig
Dis Sci. Sep
1988;33(9):1057-
63.
67.Levine JE,
Leontiadis GI,
Sharma VK,
Howden CW.
Meta-analysis:
the efficacy of
intravenous H2-
receptor
antagonists in
bleeding peptic
ulcer. Aliment
Pharmacol Ther.
Jun
2002;16(6):1137-
42.
68. .
Silverstein FE,
Gilbert DA,
Tedesco FJ, et
al. The national
ASGE survey on
uppergastroint
estinal
bleeding. II.
Clinical
prognostic
factors.
Gastrointest
Endosc
1981;27: 80–
93.
69. . Laine L,
Peterson WL.
Bleeding peptic
ulcer. N Engl J
Med 1994; 331:
717–727.
70. Rockall
TA, Logan RFA,
Deylin GB, et

al. Risk
assessment
after upper
gastrointestinal
hemorrhage.
Gut 1996; 38:
316–321.
71.Freeman ML.
Stigmata of
hemorrhage in
bleeding ulcers.
Gastrointest
Endosc
72. Cappell
MS and Friedel
D. Acute
nonvariceal
upper
gastrointestinal
bleeding:
endoscopic
diagnosis and
therapy. Med
Clin NA
2008;92:511–
550.
73. Eisen GM,
Dominitz JA,
Faigel DO, et
al. An
annotated
algorithmic
approach to
uppergastroint
estinal
bleeding.
Gastrointest
Endosc
2001;53(7):853
–858.
74. Tammaro
L, Palol M, Zullo
A, et al.
Endoscopic
findings in
patients with
upper
gastrointestinal
bleeding
clinically
classified into
three risk
groups prior to
endoscopy.
World J
Gastroenterol
2008;14:5046–
5050.
75. Bjorkman
D, Zaman A,
Fennerty B, et
al. Urgent vs.
elective
endoscopy for
acute non-
variceal upper-
GI bleeding: an
effectiveness
study.
Gastrointest
Endosc
2004;60(1):1–7.
76. Tai C,
Huang S, Wang
H, et al. High-
risk ED patients
with
nonvariceal
upper
gastrointestinal
hemorrhage
undergoing
emergency or
urgent
endoscopy: a
retrospective
analysis. Am J
Emerg Med
2007;25:273–
278.
77.Forrest JA,
Finalyson N

and Shearman
DJ. Endoscopy
in
gastrointestinal
bleeding.
Lancet
1974;ii:394–
397.
Related Documents



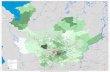





![2017 H H H H H H H H H H H H H H H H H H H …...2017 V 25 9 The LEGION LINK C C _ t Á Á X G } ] o P ] } v X } P P 1 H H H H H H H H H H H H H H H H H H H A In This Edition.... 22](https://static.cupdf.com/doc/110x72/5e9641686b534117c07b3323/2017-h-h-h-h-h-h-h-h-h-h-h-h-h-h-h-h-h-h-h-2017-v-25-9-the-legion-link-c-c-.jpg)


