Journal of Pathology J Pathol 2009; 218: 66–75 Published online 23 December 2008 in Wiley InterScience (www.interscience.wiley.com) DOI: 10.1002/path.2510 Original Paper Gal-3 is stimulated by gain-of-function p53 mutations and modulates chemoresistance in anaplastic thyroid carcinomas Luca Lavra, 1,2 Alessandra Ulivieri, 1,2 Cinzia Rinaldo, 3 Roberto Dominici, 4 Marco Volante, 5 Emidio Luciani, 6 Armando Bartolazzi, 6,7 * Francesco Frasca, 8 Silvia Soddu 3 and Salvatore Sciacchitano 1,2 * 1 S. Pietro Fatebenefratelli Hospital, Rome, Italy 2 Department of Experimental Medicine and Pathology, II Faculty of Medicine, University ‘La Sapienza’, Rome, Italy 3 Department of Experimental Oncology, Regina Elena Cancer Institute, Rome, Italy 4 Institute of Neurobiology and Molecular Medicine, Consiglio Nazionale Ricerche (CNR), Rome, Italy 5 Department of Pathology, University of Turin at San Luigi Hospital, Orbassano, Turin, Italy 6 Department of Pathology, Sant’ Andrea Hospital, Rome, Italy 7 Cellular and Molecular Tumour Pathology Laboratory, Cancer Centre Karolinska, Karolinska Hospital, Stockholm, Sweden 8 Department of Internal Medicine and Specialistic Medicine, Endocrinology Unit, Garibaldi Hospital, University of Catania, Italy *Correspondence to: Salvatore Sciacchitano, S. Pietro Fatebenefratelli Hospital, Via Cassia 600, 00189 Rome, Italy. E-mail: salvatore.sciacchitano@ uniroma1.it Armando Bartolazzi, Sant’Andrea Hospital, Via di Grottarosa 1035, 00189 Rome, Italy. E-mail: [email protected] No conflicts of interest were declared. Received: 7 April 2008 Revised: 5 December 2008 Accepted: 12 December 2008 Abstract Galectin-3 (Gal-3) is an anti-apoptotic molecule of the β -galactoside-binding lectin family. Gal-3 is down-regulated by wt-p53 and this repression is required for p53-induced apoptosis. Since poorly differentiated thyroid carcinomas (PDTCs) and anaplastic thyroid carcinomas (ATCs) frequently harbour p53 mutations, we asked whether Gal-3 expression and activity could be influenced by such mutations in these tumours. We found a positive correlation between Gal-3 expression and p53 mutation in human thyroids and in thyroid carcinoma cell lines (TCCLs) harbouring different p53 mutations. Gal-3 was over-expressed in most ATCs and TCCLs, especially those with the most frequently detected p53 mutation (p 53 R273H ). Over-expression of p53 R273H in two p53-null cells (SAOS-2 and SW-1736) as well as in two wt- p53-carrying TCCLs (TPC-1 and K1), stimulated Gal-3 expression, while interference with p53 R273H endogenous expression in ARO cells down-regulated Gal-3 expression. Conversely, over-expression of wt-p53 in ARO cells restored the inhibitory effect on Gal-3 expression. ARO cells are highly resistant to apoptosis and express both p53 and Gal-3, which are increased upon cisplatin treatment. Interference with Gal-3 expression in these cells stimulated their chemosensitivity. In conclusion, gain-of-function p53 mutant acquires the de novo ability to stimulate Gal-3 expression and to increase chemoresistance in ATCs. Copyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd. Keywords: chemoresistance; apoptosis; thyroid carcinoma; Galectin-3; p53; anaplastic thyroid carcinoma (ATC); poorly differentiated thyroid carcinoma (PDTC); human thyroid carcinoma cell lines; clonogenic assay Introduction Mutations in the p53 gene are detectable in up to 50% of all neoplasms [1] and in 14% of malignant thyroid tumours [2]. p53 mutations, among thyroid tumours, are restricted to poorly differentiated thyroid carcinomas (PDTCs) and anaplastic thyroid carcino- mas (ATCs), where they are detected in 25% and in 60–85% of cases, respectively [3,4]. Conversely, in well-differentiated thyroid carcinomas (WDTCs) they are observed in <10% [3,5]. Hence, the occurrence of a mutation in the p53 gene is considered a key event in the malignant progression of WDTCs toward the development of the highly aggressive undifferentiated tumours. The biological relevance of such mutations is demonstrated by both in vitro and in vivo experiments. Over-expression of wt-p53 in cell lines with p53 muta- tions is accompanied by the restoration of apoptotic cell death and/or cell growth arrest [6,7], chemo- and radio-sensitization [8,9], induction of senescence [10], inhibition of angiogenesis [11], and secretion of growth inhibitors [12]. It is well known that p53 muta- tions not only abrogate apoptosis or cell cycle arrest, but also mediate new oncogenic properties. However, the mechanism by which such gain-of-function muta- tions affects chemoresistance in PDTCs and ATCs, as well as in other tumours, has not yet been fully eluci- dated [13–15]. Gal-3 is an antiapoptotic molecule, belonging to the β -galactoside-binding lectin family [16]. Gal-3 Copyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd. www.pathsoc.org.uk

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Journal of PathologyJ Pathol 2009; 218: 66–75Published online 23 December 2008 in Wiley InterScience(www.interscience.wiley.com) DOI: 10.1002/path.2510
Original Paper
Gal-3 is stimulated by gain-of-function p53 mutations andmodulates chemoresistance in anaplastic thyroidcarcinomasLuca Lavra,1,2 Alessandra Ulivieri,1,2 Cinzia Rinaldo,3 Roberto Dominici,4 Marco Volante,5 Emidio Luciani,6
Armando Bartolazzi,6,7* Francesco Frasca,8 Silvia Soddu3 and Salvatore Sciacchitano1,2*1S. Pietro Fatebenefratelli Hospital, Rome, Italy2Department of Experimental Medicine and Pathology, II Faculty of Medicine, University ‘La Sapienza’, Rome, Italy3Department of Experimental Oncology, Regina Elena Cancer Institute, Rome, Italy4Institute of Neurobiology and Molecular Medicine, Consiglio Nazionale Ricerche (CNR), Rome, Italy5Department of Pathology, University of Turin at San Luigi Hospital, Orbassano, Turin, Italy6Department of Pathology, Sant’ Andrea Hospital, Rome, Italy7Cellular and Molecular Tumour Pathology Laboratory, Cancer Centre Karolinska, Karolinska Hospital, Stockholm, Sweden8Department of Internal Medicine and Specialistic Medicine, Endocrinology Unit, Garibaldi Hospital, University of Catania, Italy
*Correspondence to:Salvatore Sciacchitano, S. PietroFatebenefratelli Hospital, ViaCassia 600, 00189 Rome, Italy.E-mail: [email protected]
Armando Bartolazzi, Sant’AndreaHospital, Via di Grottarosa 1035,00189 Rome, Italy.E-mail:[email protected]
No conflicts of interest weredeclared.
Received: 7 April 2008Revised: 5 December 2008Accepted: 12 December 2008
AbstractGalectin-3 (Gal-3) is an anti-apoptotic molecule of the β-galactoside-binding lectin family.Gal-3 is down-regulated by wt-p53 and this repression is required for p53-induced apoptosis.Since poorly differentiated thyroid carcinomas (PDTCs) and anaplastic thyroid carcinomas(ATCs) frequently harbour p53 mutations, we asked whether Gal-3 expression and activitycould be influenced by such mutations in these tumours. We found a positive correlationbetween Gal-3 expression and p53 mutation in human thyroids and in thyroid carcinoma celllines (TCCLs) harbouring different p53 mutations. Gal-3 was over-expressed in most ATCsand TCCLs, especially those with the most frequently detected p53 mutation (p53R273H ).Over-expression of p53R273H in two p53-null cells (SAOS-2 and SW-1736) as well as in two wt-p53-carrying TCCLs (TPC-1 and K1), stimulated Gal-3 expression, while interference withp53R273H endogenous expression in ARO cells down-regulated Gal-3 expression. Conversely,over-expression of wt-p53 in ARO cells restored the inhibitory effect on Gal-3 expression.ARO cells are highly resistant to apoptosis and express both p53 and Gal-3, whichare increased upon cisplatin treatment. Interference with Gal-3 expression in these cellsstimulated their chemosensitivity. In conclusion, gain-of-function p53 mutant acquires thede novo ability to stimulate Gal-3 expression and to increase chemoresistance in ATCs.Copyright 2008 Pathological Society of Great Britain and Ireland. Published by JohnWiley & Sons, Ltd.
Keywords: chemoresistance; apoptosis; thyroid carcinoma; Galectin-3; p53; anaplasticthyroid carcinoma (ATC); poorly differentiated thyroid carcinoma (PDTC); human thyroidcarcinoma cell lines; clonogenic assay
Introduction
Mutations in the p53 gene are detectable in up to50% of all neoplasms [1] and in 14% of malignantthyroid tumours [2]. p53 mutations, among thyroidtumours, are restricted to poorly differentiated thyroidcarcinomas (PDTCs) and anaplastic thyroid carcino-mas (ATCs), where they are detected in 25% and in60–85% of cases, respectively [3,4]. Conversely, inwell-differentiated thyroid carcinomas (WDTCs) theyare observed in <10% [3,5]. Hence, the occurrence ofa mutation in the p53 gene is considered a key eventin the malignant progression of WDTCs toward thedevelopment of the highly aggressive undifferentiatedtumours. The biological relevance of such mutations is
demonstrated by both in vitro and in vivo experiments.Over-expression of wt-p53 in cell lines with p53 muta-tions is accompanied by the restoration of apoptoticcell death and/or cell growth arrest [6,7], chemo-and radio-sensitization [8,9], induction of senescence[10], inhibition of angiogenesis [11], and secretion ofgrowth inhibitors [12]. It is well known that p53 muta-tions not only abrogate apoptosis or cell cycle arrest,but also mediate new oncogenic properties. However,the mechanism by which such gain-of-function muta-tions affects chemoresistance in PDTCs and ATCs, aswell as in other tumours, has not yet been fully eluci-dated [13–15].
Gal-3 is an antiapoptotic molecule, belonging tothe β-galactoside-binding lectin family [16]. Gal-3
Copyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.www.pathsoc.org.uk
Gal-3 and p53 mutations in ATC 67
aberrant expression has been proposed as a diagnos-tic marker of thyroid malignancy in WDTCs [17,18].However, Gal-3 is also over-expressed in several ATCs[17]. Gal-3 belongs to a newly identified apoptoticpathway, involving wt-p53 and HIPK2 [19]. Althoughmany other different apoptotic pathways play a rele-vant role in thyroid tumorigenesis, in this study wefocus our attention on the p53/Gal-3 pathway andspecifically to the effects of mutant p53. We foundthat in human PDTCs and ATCs the occurrence ofp53 mutation is associated with Gal-3 over-expression.We demonstrated that RNA interference with Gal-3expression sensitizes the ATC-derived ARO cell lineto chemotherapic treatment. These results indicate that,in ARO cells, Gal-3 over-expression represents a criti-cal step in the acquisition of chemoresistance and thismechanism is likely relevant in PDTCs and ATC invivo.
Materials and methods
Thyroid tissue specimens collection
Since ATCs are rare, we collected tissue samples fromtwo different Italian hospitals, Ospedale Le Molinette,University of Turin, and Ospedale St. Andrea, Uni-versity ‘La Sapienza’ of Rome. Tissue samples wereobtained at surgery according to local ethical com-mittee recommendations. Histological diagnoses were
rendered in agreement with WHO indications [20] andaccording to the recently published new criteria [21].Thyroid tumours were classified as 21 PDTCs [11 withrecognizable papillary thyroid carcinoma (PTC) ori-gin and seven with follicular thyroid carcinoma (FTC)origin] and seven ATCs (Table 1).
Immunohistochemical (IHC) analysis
Serial tissue sections for conventional histologicaland immunophenotypical analysis were obtained fromformalin-fixed, paraffin-embedded tissue specimens.HRP-conjugated rat mAb to Gal-3 (Space Import–Export s.r.l., Milan, Italy), mouse mAb to p53 (Dako)and mouse mAb to MDM-2 (AbD Serotec, Oxford,UK) were used in immunohistochemistry accordingto the manufacturer’s instructions and as previouslydescribed [14]. Antigen-retrieval microwave treatmentof tissues slides in 0.01 M citrate buffer, pH 6.0, wasapplied as required. HRP-conjugated rabbit anti-mouseimmunoglobulins were used as secondary antibodiesfor p53 and MDM-2 immunostaining, in an indirectimmunoperoxidase assay (Dako). Immunohistochemi-cal evaluations were carried out independently by twoexperienced pathologists. A positive immunostainingfor p53 is usually considered as a surrogate of p53mutation. However, to better correlate p53 functionalactivity and Gal-3 over-expression, we also analysed
Table 1. Pathological features of our group of patients with PDTCs and ATCs
Case no. Sex/age Size (cm) Original histological pattern
Poorly differentiated thyroid carcinomas (PTC and FTC origin) with solid areas1 F/58 na PTC, insular >75%2 M/65 4 PTC, insular 90%3 F/53 na FTC, solid/trabecular 60%, follicular 40%4 F/54 na FTC, solid/trabecular 60%, follicular 40%5 M/65 5.5 PDTC, solid/trabecular 60%, follicular 40%6 F/54 3 PDTC, insular/solid >90%7 M/70 5 PTC, insular 20%, follicular 80%8 M/52 3 PTC, solid/trabecular 60%, follicular 40%9 F/56 1.5 PTC, solid 50%, follicular 50%
10 F/36 2 PTC, solid 15%, follicular 85%11 F/62 8 PTC, solid/trabecular 50%, follicular 50%12 F/57 3 PTC, papillary 60%, solid/trabecular 40%13 M/61 na PTC14 F/75 7 FTC, solid/trabecular >75%15 M/73 4.5 FTC, solid/trabecular >80%16 F/40 3.5 FTC, solid/trabecular >90%17 F/74 4.5 FTC, insular/solid 20%, follicular 80%18 F/70 4 PTC, insular/trabecular 50%, papillary (fv) 50%19 F/27 2.5 PTC, solid/trabecular >90%20 M/70 5 FTC, solid/trabecular >90%21 F/74 5 PDTC, solid/trabecular >90%
Anaplastic thyroid carcinomas22 F/74 1.5 ATC, giant cell/sarcomatoid23 F/69 4 ATC, giant cell variety24 F/72 7 ATC, sarcomatoid/giant cell variety25 F/65 8 ATC, giant cell variety26 F/63 6 ATC, insular 30%, anaplastic 40%, follicular 30%27 M/82 6 ATC, squamous, residual trabecular ca. (80%)28 M/56 10 ATC, sarcomatoid
na = not applicable
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
68 L Lavra et al
the expression of MDM2, a well-known physiologicaltarget of wt-p53 [22].
Cell culture
A total of 12 human thyroid carcinoma cell lines(TCCLs) were used. Four PTC-derived cell lines(TPC-1, 8305-C, Bc-Pap, and NPA), as well as oneFTC-derived (FTC-133) cell line and six ATC-derivedcell lines (C-643, SW-1736, KAT-4, ARO, FF-1and Hth-74) were cultured as previously described[23]. The human PTC-derived K1 cells were pur-chased from ECACC (Salisbury, UK) and grownin DMEM : Ham’s F12 (Lonza Walkersville, Walk-ersville, MD, USA):MCDB-105 (Sigma, St. Louis,MO, USA) (2 : 1:1) medium with 10% FBS (Lonza)added. SAOS-2 cells were cultured in DMEM (Lonza)supplemented with 10% FBS (Lonza). The HepG2cell line was maintained in MEM (Lonza). All culturemedia were supplemented with 2 mM glutamine and100 µg/ml penicillin and streptomycin mix (Lonza).Transient transfections were performed using Lipofec-tamine (Invitrogen) according to the manufacturer’sinstructions. Transfection experiments were performedin duplicate. Transfection efficiency was 10–30% andwas related to the cell type.
Plasmid vectors and RNA interference (RNAi)
Over-expression of wt and mutant p53 R273H wasperformed using the following expression vectors:pLXSP, pLwtp53SP, pLp53H273SP [19]. p53 and Gal-3 RNAi was obtained by using the following con-structs: pSUPERretro, pSUPER-p53 for p53 and pSU-PER, pSUPER–Gal3–845 and pSUPER–Gal3–551for Gal-3 interference [19].
RNAi with mutated p53 was obtained in AROcells by transient transfection of pSUPERretro andpSUPER-p53 constructs.
Two clones of ARO cells, stably transfected withpSUPER–Gal3–845 (ARO-Gal-3i/845) andpSUPER–Gal3–551 (ARO–Gal-3i/551) vectors, anda control cell line (ARO–ctr) transfected with emptypSUPER vector, were generated and grown in theappropriate medium. Selection of stably transfectedcells was performed by treatment with puromicin atthe concentration of 2 µg/ml (Sigma). Stable interfer-ence with Gal-3 expression was confirmed by westernblot (WB) analysis.
Western blot analysis
Total cell extracts (TCEs) were obtained as previ-ously described [24]. An aliquot of TCE (30–70 µg)was separated via 10% SDS–PAGE and blotted ontonitrocellulose membrane (BIO-RAD). The followingantibodies were used in immunoblotting: mouse mAbanti-p53, rabbit polyclonal anti-poly (ADP-ribose)polymerase-1 (PARP-1), mouse mAb anti-α-tubulin,mouse mAb anti-vinculin and anti-caspase-3 (Santa
Cruz Biotechnology, Santa Cruz, CA, USA), purifiedrat mAb anti-Gal-3 antibody (Mabtech AB, NackaStrand, Sweden), mouse mAb anti-β-actin (Sigma),and HRP-conjugated anti-mouse, anti-rat or anti-rabbitantibodies (Sigma). Immunoreactivity was detectedusing ECL kits (Amersham, UK). Densitometric anal-ysis of the intensity of the bands was performed usingthe software NIH ImageJ (version 1.32j).
Treatment with cisplatin
The same number (2–3 × 105) of parental ARO andK1 cells, as well as ARO–Gal–3i/845, ARO–Gal–3i/551 and ARO–ctr cells, were seeded on six-wellplates in the appropriate culture medium. After 24 h,we added cisplatin (Sigma Aldrich) at different doses(0.1–10 µg/ml) to the culture medium. Cells werecollected after 24 and 48 h and TCEs were obtainedto perform WB analysis.
Clonogenic assay
Both Gal-3-interfered ARO cells (ARO–Gal–3i/845,ARO–Gal–3i/551) and ARO–ctr cells were treatedwith cisplatin and then analysed by clonogenic assayas previously described [25]. Cisplatin was removedfrom the medium 24 h after treatment. The cellswere counted and seeded on six-well plates at theconcentration of 1 × 103 cells/well. Duplicate plateswere incubated for 10 days and newly formed cellclones were fixed in cold methanol and stained with0.1% w/v crystal violet (Sigma). Clone counts wereperformed using NIH ImageJ software, version 1.32j.A threshold level of 30 rdu was arbitrarily set todiscriminate intensity of clones composed of morethan 50 cells. A series of two independent experimentswas performed.
Results
p53 and Gal-3 protein expression analysis
A total of 28 histological samples, including 21PDTCs and seven ATCs, were analysed for both p53and Gal-3 protein expression (Tables 1, 2). Gal-3 wasexpressed in 8/21 PDTCs (38.1%) and in 6/7 ATCs(85.7%) analysed. p53 was detected by immunohisto-chemistry in 18 cases, including 12/21 (57.1%) PDTCsand 6/7 (85.7%) ATCs. Among this group of p53-positive thyroid tumours, Gal-3 was detected in 10cases, equal to 55.5% (Table 2B). Comparative anal-ysis of immunohistochemical expression results forboth p53 and Gal-3 proteins indicates that they wereboth expressed in five PDTCs and five ATCs, whilethey were both negative in six PDTCs. Therefore,p53 and Gal-3 are expressed in a concordant man-ner in a total of 16/28 cases (57.1%). In particu-lar, 11/21 cases among PDTCs (52.4%) and in 5/7cases among ATCs (71.4%) were characterized byeither concordant-positive or -negative p53 and Gal-3
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Gal-3 and p53 mutations in ATC 69
expression. The remaining cases showed the absenceof p53 expression in the presence of Gal-3 (threePDTCs and one ATC) or viceversa (seven PDTCsand one ATC) (Table 2A, B). To further analyse thepossible correlation between p53 mutation and Gal-3expression, we decided to test the functional activity ofwt-p53 by evaluating the expression of a well-knownp53 physiological transcriptional target, viz. MDM2[22].
We performed immunohistochemical analysis forMDM2 to check for the absence of MDM-2 expres-sion, indicative of loss of p53 wild-type activity. In10/18 p53-positive cases MDM2 expression was low,suggesting loss of p53 physiological transcriptionalactivity (Table 3). The percentage of Gal-3-positivesamples among this group of 10 lesions express-ing a non-functional p53 protein increased to 70%,compared to 55.5% when only p53 immunodetec-tion was considered. Interestingly, MDM2 analysisdid not change the results in ATCs, indicating that in
Table 2. P53 and Gal-3 expression in thyroid tumours byimmunohistochemistry. Comparative expression analysis of p53and Gal-3 in PDTCs, with the indicated origin, and in ATCs, usingbiotin-free immunohistochemistry. (A) Cases with absence ofp53 expression. (B) Cases with positive p53 staining, suggestinga possible mutation
Caseno. Origin p53 Gal-3
(A) p53-negative cases1 PTC Neg Neg2 PTC Neg Neg3 FTC Neg Neg4 FTC Neg Neg5 PDTC Neg Neg6 PDTC Neg Neg
18 PTC Neg +19 PTC Neg +20 FTC Neg +28 ATC Neg +
(B) p53-positive cases (possible mutation)21 PDTC + Neg8 PTC + ±9 PTC ++ ±
10 PTC + ±14 FTC + ±15 FTC + ±16 FTC + ±23 ATC ++ ±7 PTC + +
11 PTC + +12 PTC + +13 PTC + ++17 FTC + +22 ATC + +24 ATC + +25 ATC + +26 ATC + +27 ATC + +
Neg, negative, i.e. no immunostaining was observed; ±, immunostainingrestricted to <10% of malignant cells; +, positivity seen in 10–70% ofcells; ++, >70% of malignant cells positive to immunostaining. Gal-3expression was classified as positive when >10% of cells were positivein the cytoplasm
Table 3. Correlation between p53 functional status, assessedby MDM2 immunohistochemistry, and Gal-3 expressionanalysed in p53 thyroid tumours, classified as positive at p53immunohistochemistry
Case no. Origin p53 MDM-2 Gal-3
(A) p53-positive and MDM2-positive thyroid tumours with loss of wt-p53activity21 PDTC + ± Neg.8 PTC + ± ±15 FTC + ± ±12 PTC + ± +17 FTC + ± +22 ATC + ± +24 ATC + ± +25 ATC + ± +26 ATC + ± +27 ATC + ± +
(B) p53-positive and MDM2-negative tumours with retained wt-p53 activity9 PTC ++ + ±10 PTC + ++ ±14 FTC + + ±16 FTC + ++ ±23 ATC ++ + ±11 PTC + ++ +7 PTC + + +13 PTC + + ++
±, immunostaining restricted to <10% of malignant cells; +, positivity10–70%; ++, >70% of malignant cells positive to immunostaining.MDM2 expression, indicative of a wt-p53-mediated stimulation, wasclassified as positive when >10% of tumour cells showed nuclearstaining.
these tumours p53 immunodetection is always asso-ciated with alteration in p53 transcriptional activ-ity. There was no correlation between p53, Gal-3expression and the specific histological background ofPDTCs. Our results suggest that stabilized p53 expres-sion, usually assumed as a surrogate of p53 mutationand MDM2 down-regulation, indicative of absenceof wt-p53 activity [22], correlate with Gal-3 over-expression.
Correlation between Gal-3 expression and p53mutations in TCCLs
To further evaluate the molecular bases of Gal-3 andmutant p53 co-expression observed in PDTCs andATCs in vivo, we analysed Gal-3 and p53 proteinexpressions in a subset of 12 different TCCLs, char-acterized by the presence of various known p53 muta-tions, affecting codons located in the DNA-bindingdomain (DBD) of the protein (Figure 1A, B) [23]. Gal-3 expression was high in all cell lines harbouring a p53mutation, compared to TPC-1 and K1, characterizedby wt-p53 (Figure 1A, lane 5, and Figure 3A, respec-tively). The intensity of Gal-3 expression was variable,with higher expression level observed in cells withp53 mutations affecting codon 273 (Figure 1A, lanes1, 3, 7, 8) and codon 285 (Figure 1A, lane 9). Gal-3was highly expressed in those cells in which a p53mutation simultaneously affected two distinct codons(Figure 1A, lanes 1, 2, 11, 13). Moreover, in two cell
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
70 L Lavra et al
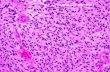
Figure 1. Positive correlation between Gal-3 expression and p53 mutation in TCCLs. (A) Immunoblots with antibodies to Gal-3and p53 on TCEs obtained from 11 thyroid carcinoma cell lines (FTC-133, C-643, 8305-C, SW-1736, TPC-1, KAT-4, ARO, FF-1,Bc-Pap and Hth-74), one hepatocarcinoma cell line (HepG2) and one osteosarcoma cell line (SAOS-2), characterized by thepresence of wt, mutated or null p53. β-Actin was used as a loading control. (B) Densitometric analysis of the intensity of Gal-3(black bars) and p53 (grey bars) bands visualized in (A). Results are expressed as relative densitometric units (rdu), measurednormalizing Gal-3 and p53 signals with the corresponding β-actin band intensity
lines totally devoid of p53 protein (Figure 1A, lanes4, 10), Gal-3 expression levels were high in the thy-roid carcinoma-derived SW-1736 cells and detectablein the osteosarcoma-derived SAOS-2 cells. In thesecases, the absence of the p53 inhibitory effect on Gal-3 expression could be responsible for such an effect.Densitometric analysis, performed on our WB experi-ments, clearly shows such positive correlation betweenp53 mutation and Gal-3 expression (Figure 2B), thusreinforcing our in vivo data.
Gain-of-function mutant p53R273H stimulates Gal-3expression
Since we detected the highest levels of Gal-3 expres-sion in cells containing p53 R273H mutant (Figure 1A,lanes 1, 7, 8, and Figure 1B), we asked whether thistype of mutation could be directly responsible forthis effect. We therefore over-expressed the mutantpLp53 R273H SP construct [19], in two p53-null cellsystems, viz. SAOS-2 and SW-1736, as well as inthe two wt-p53-carrying cells, TPC-1 and K1. Over-expression of mutant p53 in these four cell systemswas associated with an increase in Gal-3 expression
(Figure 2A–D). Conversely, over-expression of wt-p53 in SAOS-2 and SW-1736 caused a reduction inGal-3 protein expression (Figure 2A, B), in agreementwith our previously published data [19]. To confirmthe specificity of the effect of this p53 mutation onGal-3 expression, we then interfered with endogenousmutant p53 R273H expression in ARO cells. Down-regulation of mutant p53 R273H , induced by RNAi, wasresponsible for a dramatic reduction of both mRNA(see Supporting information, Figure S1) and proteinGal-3 expression levels, at 24 and 72 h, respectively,after transfection (Figure 2E).
Re-introduction of wt-p53 in the context of AROcells was previously reported to be able to restore amore differentiated state (i.e. re-expression of specificthyroid markers) and to reduce their malignant pheno-type [6]. We analysed the effect of such restorationon Gal-3 expression in these cells. Transient over-expression of wt-p53 in ARO cells caused a rapidreduction of Gal-3 protein expression levels, alreadyvisible 24 h after transfection (Figure 2F). This resultis consistent with a rapid inhibitory effect of wt-p53 onGal-3 expression and is compatible with an action atthe promoter level, as previously observed [19]. These
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Gal-3 and p53 mutations in ATC 71
Figure 2. Effects of wt and mutant p53R273H on Gal-3 expression in different TCCLs. Immunoblots with antibodies to Gal-3performed on TCE from cells transiently transfected with pLXSP control, pLwtp53SP or pLp53H273SP mutant vectors on SAOS-2(A), SW-1736 (B), TPC-1 (C) and K1 (D) cells. SW-1736 cells, transfected with pLwtp53SP vector, were harvested after 48 h,while the same cells transfected with pLp53H273SP construct were harvested after 8 h. (E) ARO cells were transiently transfectedwith pSUPERretro control or pSUPER-p53 vectors. At indicated times post-transfection the cells were harvested to perform WBto analyse Gal-3 and p53 protein expression. (F) Immunoblotting kinetics of Gal-3 and p53 at the indicated times after transienttransfection of ARO cells with pLXSP control and pLwtp53SP vectors. α-Tubulin and β-actin were used as loading controls
data reinforce our results regarding a positive correla-tion between p53 mutation and Gal-3 expression. p53mutation affecting codon 273 appears to act as a gain-of-function mutation with respect to Gal-3 expression.
p53R273H-mediated Gal-3 over-expressioncorrelates with resistance to cisplatin treatment
Both p53 mutations and Gal-3 over-expression areknown to inhibit apoptosis in may different cell sys-tems [13,16]. We tried to correlate resistance to apop-tosis with p53 and Gal-3 expression in ARO cells,using K1 cells expressing wt-p53 as a control. Tothis end, we treated K1 and ARO cells with cisplatin
and we analysed cell death, by Trypan blue exclu-sion as well as induction of apoptosis by Caspase-3and PARP-1 cleavage. ARO cells proved to be resis-tant to cisplatin treatment, while apoptosis was eas-ily obtained in K1 cells. In fact, we could inducecell death in only 1.6% of ARO cells, compared to66.9% of K1 cells (Figure 3B). Induction of apop-tosis in K1 cells was accompanied by reduction ofCaspase-3 and cleavage of PARP-1 (Figure 3C). Incontrast, ARO cells showed no reduction of Caspase-3 and absence of PARP-1 cleavage (Figure 3C). Inaddition, induction of apoptosis in K1 cells corre-lated with activation of wt-p53 and down-regulation ofGal-3 protein expression, in agreement with our pre-vious data obtained using other wt-p53-carrying cell
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
72 L Lavra et al
lines [19]. Conversely, ARO cells treated with cis-platin showed a concomitant up-regulation of p53R273H
and Gal-3 protein levels (Figure 3C ). These resultssuggest that Gal-3 expression correlates with resis-tance to apoptosis in TCCLs expressing mutatedp53.
RNAi with Gal-3 expression restoreschemosensitiveness in ARO cells
On the basis of our previous observations, we tried tosensitize ARO cells to chemotherapy by stably inter-fering with their endogenous mRNA Gal-3 expres-sion levels. The two cells lines ARO–Gal3i/845
Figure 3. Effects of cisplatin treatment on Gal-3 expressionand apoptosis in TCCLs with wild-type or mutated p53R273H.(A) Immunoblots with antibodies to endogenous Gal-3 andp53 on TCEs of K1 and ARO cells. (B) Percentage of deadcells, determined by Trypan blue exclusion, in K1 and AROcells treated with 10 µg/ml cisplatin for 24 h. A result ofan experiment representative of three independent analysisis reported. (C) Immunoblots with antibodies to Gal-3, p53,Caspase-3, PARP-1 and its cleaved form (PARP-1∗) on TCEsof K1 and ARO cells described in (B). Note that a differentamount of TCEs was used for K1 (50 µg) and ARO (10 µg) tobetter demonstrate modulation of Gal-3 and p53 expression inthe two different cell systems. Vinculin was used as a loadingcontrol
and ARO–Gal3i/551, stably interfered with Gal-3expression (Figure 4A), were treated with differentdoses of cisplatin and analysed by clonogenic assay(Figure 4B, C). The results indicated that clone forma-tion was significantly reduced in both interfered cells,compared to ARO–ctr cells, transfected with the pSU-PER vector (p < 0.0005; Figure 4B, C). The effectwas more evident with low doses of cisplatin and wascorrelated to the levels of Gal-3 interference obtainedusing the two different constructs, being more evidentin ARO–Gal3i/551, which exhibits more depleted lev-els of Gal-3 protein (Figure 4A–C). Our data indicatethat the level of Gal-3 expression influences sensi-tiveness of ATC-derived TCCLs to chemotherapeutictreatment.
Discussion
ATC is a rare but aggressive form of cancer thataccounts for <2% of all thyroid malignancies [26,27].The results of surgical resection, chemotherapy andradiotherapy, alone or in combination, are not effec-tive and patients usually die within 6–12 months [28].This clinical behaviour and outcome is dramaticallydifferent from that observed in WDTCs, which usu-ally grow and progress slowly, rarely metastatize andare characterized by a good or very good prognosis.These differences are generally referred to the pres-ence of mutations in the p53 tumour suppressor gene,encountered in the majority of ATCs but only rarelyin WDTCs [29]. In both PDTCs and ATCs, prog-nosis is negatively affected by p53 mutations, whichcontribute actively to tumour maintenance, spreadingand increased resistance to conventional anticancertreatments [13,14,29].
We found p53 expression in approximately half ofthe PDTCs examined and in almost all ATCs that alsoover-expressed Gal-3. In addition, we found good cor-relation between MDM2 down-regulation, indicativeof the absence of wt-p53 activity [22], and Gal-3over-expression, especially among ATCs. In fact, adown-regulation of Gal-3 expression was observed in5/8 p53-positive samples that were also characterizedby MDM2 nuclear expression, indicative of a retainedphysiological activity of p53 on the MDM2 promoter[22] (Table 3). However, we found that Gal-3 wasup-regulated in four tumour samples that containeda wt-p53 (Table 2A). We cannot exclude, in suchcases, the occurrence of other p53-independent Gal-3-activating mechanisms, or lack of wt-p53 activationdue to mutation or deletion of p53-activating fac-tors. Mutant p53 is known to up-regulate many genesinvolved in cell proliferation, apoptosis and cell cycleregulation [30], and in some of them, such as c-myc[31], ABCB1 (multi-drug resistance, MDR) [32] andGal-3 (present study), an opposite effect exerted bywt and mutant p53 on the same gene can be demon-strated. The correlation between Gal-3 expression andp53 mutation is reinforced by the occurrence of Gal-3
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Gal-3 and p53 mutations in ATC 73
Figure 4. Effects of Gal-3 down-regulation by RNAi on chemosensitivenes in ARO cells. (A) Immunoblots with antibodies toGal-3 on TCEs of ARO interferred with Gal-3 expression by stable transfection with pSUPER–Gal3–845 (ARO-Gal-3i/845) andpSUPER–Gal3–551(ARO-Gal-3i/551) vectors as well as with pSUPER control vector (ARO–ctr). β-Actin was used as a loadingcontrol. (B, C) Two clones of ARO cells, stably interfered with Gal-3 expression (ARO-Gal-3i/845 and ARO-Gal-3i/551), wereplated in duplicate along with their control (ARO–ctr) and treated with the indicated doses of cisplatin. The clones formed werestained 10 days later with crystal violet (C) and counted (B). In (B) is plotted the number of clones formed as mean ± SD of threeindependent experiments. p < 0.0005 for ARO–ctr versus ARO-Gal-3i/845 and ARO-Gal-3i/551 in all treatments; a significantdifference (p < 0.05) was also found between the two interfered clones
over-expression in cell lines derived from WDTCs, butcharacterized by the presence of mutations in the p53gene (Figure 1A, lanes 1, 3, 11, 13) [23] and by thelower Gal-3 expression levels in WDTC-derived TPC-1 and K1, which contain a wt-p53 (Figure 1, lane 5,and Figure 3A). Finally, over-expression of the mostfrequently reported p53 mutation (p53 R273H ) [33] inboth TPC-1 and K1 cells caused a further increaseof Gal-3 expression, suggesting a dominant effect ofp53 R273H on endogenous wt-p53 (Figure 2C, D).
The effects of the gain-of-function mutant p53 R273H
on tumour cell lines have already been reported andare usually associated with the acquisition of more
aggressive behaviour [34,35]. Recently, we analysedthe effects of wt-p53 on Gal-3 expression in other cellsystems, such as RKO and MEF, upon wt-p53 RNAiand p53 gene knock-out. respectively [19]. Theseexperiments demonstrated that the absence of p53 didnot allow Gal-3 to be down-regulated, thus result-ing in decrease of apoptosis. We hypothesized thatGal-3 over-expression, induced by mutant p53, couldbe associated with resistance to apoptosis induced bychemotherapy. ARO cells are generally more resis-tant to chemotherapy induced by either drugs orUV radiation. Indeed, we could not induce apop-tosis in these cells, measured both as PARP-1 and
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
74 L Lavra et al
Caspase-3 cleavages (Figure 3). This chemoresistantstate was associated with high level of Gal-3 expres-sion that further increases upon treatment with cis-platin. Moreover, down-regulation of Gal-3 by RNAiin ARO cells was sufficient to restore chemosensitiv-ity to cisplatin. These observations demonstrate thatGal-3 over-expression is correlated to resistance toapoptosis in human ATCs, as previously observedin other tumour cell lines [36–39]. Further experi-ments are needed to test chemosensitivity using newchemotherapic drugs such as gemcitabine, vinorelbineand paclitaxel that have proved to be active in ATCs[40].
In conclusion, we demonstrate that in ATC Gal-3 expression is up-regulated by gain-of-function p53mutation, and is responsible for chemoresistance ofthese cells. Therefore, Gal-3 plays a relevant role in themalignant behaviour of ATC and may be considered anew target for the design of novel diagnostic [41] aswell as therapeutic approaches to this aggressive formof thyroid tumour.
Acknowledgements
We are particularly grateful to F. Orlandi and M. Papotti forproviding some of the ATCs analysed. LL and CR are recipientsof fellowships from Fondazione Italiana per la Ricerca sulCancro (FIRC). This study was funded by Compagnia di SanPaolo, Progetto Oncologia 2002-2006, Turin, Italy, and by theItalian Association for Cancer Research (AIRC).
Supporting information
Supporting information may be found in the onlineversion of this article.
References
1. Wyllie FS, Haughton MF, Blaydes JP, Schlumberger M, Wynford-Thomas D. Evasion of p53-mediated growth control occurs bythree alternative mechanisms in transformed thyroid epithelialcells. Oncogene 1995;10:49–59.
2. Dobashi Y, Sakamoto A, Sugimura H, Mernyei M, Mori M,Oyama T, et al. Over-expression of p53 as a possible prognosticfactor in human thyroid carcinoma. Am J Surg Pathol1993;17:375–381.
3. Fagin JA, Matsuo K, Karmaker A, Chen DL, Tang S-H, Koef-fler HP. High prevalence of mutations of the p53 gene inpoorly differentiated human thyroid carcinomas. J Clin Invest1993;91:179–184.
4. Takeuchi Y, Daa T, Kashima K, Yokoyama S, Nakayama I,Noguchi S. Mutations of p53 in thyroid carcinoma with an insularcomponent. Thyroid 1999;9:377–381.
5. Ito Y, Seyama T, Mizuno T, Tsuyama N, Hayashi T, Hayashi Y,et al. Unique association of p53 mutations with undifferentiatedbut not with differentiated carcinomas of the thyroid gland. CancerRes 1992;52:1369–1371.
6. Moretti F, Farsetti A, Soddu S, Misiti S, Crescenzi M, Filetti S,et al. p53 Re-expression inhibits proliferation and restoresdifferentiation of human thyroid anaplastic carcinoma cells.Oncogene 1997;14:729–740.
7. Nagayama Y, Yokoi H, Takeda K, Hasegawa M, Nishihara E,Namba H, et al. Adenovirus-mediated tumor suppressor p53 gene
therapy for anaplastic thyroid carcinoma in vitro and in vivo. JClin Endocrinol Metab 2000;85:4081–4086.
8. Soddu S, Sacchi A. p53 : prospects for cancer gene therapy.Cytokines Cell Mol Ther 1998;4:177–185.
9. Gurnani M, Lipari P, Dell J, Shi B, Nielsen LL. Adenovirus-mediated p53 gene therapy has greater efficacy when combinedwith chemotherapy against human head and neck, ovarian,prostate, and breast cancer. Cancer Chemother Pharmacol1999;44:143–151.
10. Wang Y, Blandino G, Oren M, Givol D. Induced p53 expressionin lung cancer cell line promotes cell senescence and differentiallymodifies the cytotoxicity of anti-cancer drugs. Oncogene1998;17:1923–1930.
11. Nishizaki M, Fujiwara T, Tanida T, Hizuta A, Nishimori H,Tokino T, et al. Recombinant adenovirus expressing wild-type p53is antiangiogenic: a proposed mechanism for bystander effect. ClinCancer Res 1999;5:1015–1023.
12. Komarova EA, Diatchenko L, Rokhlin OW, Hill JE, Wang ZJ,Krivokrysenko VI, et al. Stress-induced secretion of growthinhibitors: a novel tumor suppressor function of p53. Oncogene1998;17:1089–1096.
13. Blandino G, Levine AJ, Oren M. Mutant p53 gain of function:differential effects of different p53 mutants on resistance ofcultured cells to chemotherapy. Oncogene 1999;18:477–485.
14. Sigal A, Rotter V. Oncogenic mutations of the p53 tumorsuppressor: the demons of the guardian of the genome. CancerRes 2000;60:6788–6793.
15. Bossi G, Lapi E, Strano S, Rinaldo C, Blandino G, Sacchi A.Mutant p53 gain of function: reduction of tumor malignancyof human cancer cell lines through abrogation of mutant p53expression. Oncogene 2006;25:304–309.
16. Nangia-Makker P, Nakahara S, Hogan V, Raz A. Galectin-3 inapoptosis, a novel therapeutic target. J Bioenerg Biomembr2007;39:79–84.
17. Bartolazzi A, Gasbarri A, Papotti M, Bussolati G, Lucante T,Khan A, et al. Thyroid Cancer Study Group: application of animmunodiagnostic method for improving preoperative diagnosisof nodular thyroid lesions. Lancet 2001;357:1644–1650.
18. Bartolazzi A, Orlandi F, Saggiorato E, Volante M, Arecco F,Rossetto R, et al. Galectin 3-expression analysis in the surgicalselection of follicular thyroid nodules with indeterminate fine-needle aspiration cytology: a prospective multicentre study. LancetOncol 2008;9:543–549.
19. Cecchinelli B, Lavra L, Rinaldo C, Iacovelli S, Gurtner A,Gasbarri A, et al. Repression of the antiapoptotic moleculegalectin-3 by homeodomain-interacting protein kinase 2-activatedp53 is required for p53-induced apoptosis. Mol Cell Biol2006;26:4746–4757.
20. Li Volsi VA, Albores-SaAvedra J, Asa SL, Baloch ZW, Sobrinho-Simoes M, Wenig B, et al. Tumours of thyroid and parathyroid.In WHO Classification of Tumours: Pathology and Genetics ofTumours of Endocrine Organs, vol 8, DeLellis RA, Lloyd RV,Heitz PU, Eng C (eds). World Health Organization (WHO):Geneva/IARC: Lyon, 2004; 49–100.
21. Volante M, Collini P, Nikiforov YE, Sakamoto A, Kakudo K,Katoh R, et al. Poorly differentiated thyroid carcinoma: theTurin proposal for the use of uniform diagnostic criteriaand an algorithmic diagnostic approach. Am J Surg Pathol2007;31:1256–1264.
22. Nenutil R, Smardova J, Pavlova S, Hanzelkova Z, Muller P,Fabian P, et al. Discriminating functional and non-functional p53in human tumours by p53 and MDM2 immunohistochemistry. JPathol 2005;207:251–259.
23. Frasca F, Vella V, Aloisi A, Mandarino A, Mazzon E, Vigneri R,et al. p73 tumor-suppressor activity is impaired in human thyroidcancer. Cancer Res 2003;63:5829–5837.
24. Ulivieri A, Lavra L, Dominici R, Giacomelli L, Brunetti E,Sciacca L, et al. Frizzled-1 is down-regulated in follicular thyroidtumours and modulates growth and invasiveness. J Pathol2008;215:87–96.
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Gal-3 and p53 mutations in ATC 75
25. Franken NA, Rodermond HM, Stap J, Haveman J, vanBree C. Clonogenic assay of cells in vitro. Nat Protocols2006;1:2315–2319.
26. Cornett WR, Sharma AK, Day TA, Richardson MS, Hoda RS,van Heerden JA, et al. Anaplastic thyroid carcinoma: an overview.Curr Oncol Rep 2007;9:152–158.
27. Are C, Shaha AR. Anaplastic thyroid carcinoma: biology,pathogenesis, prognostic factors, and treatment approaches. AnnSurg Oncol 2006;13:453–464.
28. Giuffrida D, Gharib H. Anaplastic thyroid carcinoma: currentdiagnosis and treatment. Ann Oncol 2000;11:1083–1089.
29. Hosal SA, Apel RL, Freeman JL, Azadian A, Rosen IB, LiVolsiVA, et al. Immunohistochemical localization of p53 in humanthyroid neoplasms: correlation with biological behavior. EndocrPathol 1997;8:21–28.
30. Strano S, Dell’Orso S, Di Agostino S, Fontemaggi G, Sacchi A,Blandino G. Mutant p53 : an oncogenic transcription factor.Oncogene 2007;26:2212–2219.
31. Frazier MW, He X, Wang J, Gu Z, Cleveland JL, Zambetti GP.Activation of c-myc gene expression by tumor-derived p53mutants requires a discrete C-terminal domain. Mol Cell Biol1998;18:3735–3743.
32. Bush JA, Li G. Cancer chemoresistance: the relationship betweenp53 and multidrug transporters. Int J Cancer 2002;98:323–330.
33. Olivier M, Eeles R, Hollstein M. The IARC TP53 database: newonline mutation analysis and recommendations to users. HumMutat 2002;19:607–614.
34. Kawamura M. The 273rd codon mutants of p53 showgrowth modulation activities not correlated with p53-specifictransactivation activity. Oncogene 1996;12:2361–2367.
35. Dong P, Tada M, Hamada JI, Nakamura A, Moriuchi T, SakuragiN. p53 dominant-negative mutant R273H promotes invasion andmigration of human endometrial cancer HHUA cells. Clin ExpMetastasis 2007;24:471–483.
36. Yoshii T, Fukumori T, Honjo Y, Inohara H, Kim HR, Raz A.Galectin-3 phosphorylation is required for its anti-apoptoticfunction and cell cycle arrest. J Biol Chem 2002;277:6852–6857.
37. Fukumori T, Oka N, Takenaka Y, Nangia-Makker P, ElsammanE, Kasai T, et al. Galectin-3 regulates mitochondrial stability andantiapoptotic function in response to anticancer drug in prostatecancer. Cancer Res 2006;66:3114–3119.
38. Oishi T, Itamochi H, Kigawa J, Kanamori Y, Shimada M, Taka-hashi M, et al. Galectin-3 may contribute to cisplatin resistancein clear cell carcinoma of the ovary. Int J Gynecol Cancer2007;17:1040–1046.
39. Johnson KD, Glinskii OV, Mossine VV, Turk JR, Mawhin-ney TP, Anthony DC, et al. Galectin-3 as a potential therapeu-tic target in tumors arising from malignant endothelia. Neoplasia2007;9:662–670.
40. Voigt W, Pickan V, Pfeiffer C, Mueller T, Simon H, Arnold D.Preclinical evaluation of ZD1839 alone or in combination withoxaliplatin in a panel of human tumor cell lines — implicationsfor clinical use. Onkologie 2005;28:482–488.
41. Bartolazzi A, D’Allesandria C, Parisella MG, Signore A, DelPrete F, Lavra L, et al. Thyroid cancer imaging in vivo bytargeting the anti-apoptotic molecule Galectin-3. Plos One2008;3:E3768.
J Pathol 2009; 218: 66–75 DOI: 10.1002/pathCopyright 2008 Pathological Society of Great Britain and Ireland. Published by John Wiley & Sons, Ltd.
Related Documents