Final Product ============================== MetaData ============================== Journal: Journal of Cancer Research and Discovery(JCRD) Article Type: Basic Research Article Title: Microbiological analysis of endotracheal aspirate and endotracheal tube cultures in mechanically ventilated patients Short Title: Microbiological ana endotracheal Authors: Zheng Chen (1 3); Xiangyu Q. Wei (3); Xuesheng Zheng (1 2); Affiliations: 1: At the same time, Pseudomonas aeruginosa, normal respiratory flora 2: But results of endotracheal tube and endotracheal 3: The main pathogens cultured in the catheter end culture Abstract: Abstract Objective To analyze the consistency of microbiological culture results between endotracheal aspirate and endotracheal tube end specimens in ICU patients with mechanical ventilation. Method From January 2017 to December 2017 a total of 81 patients undergoing mechanical ventilation in the [a] intensive care unit were continuously enrolled. The results of endotracheal tube and endotracheal aspirate cultures were recorded and analyzed. Spearman correlation analysis was used to analyze the relevance of the results of the two specimens. The consistency of the results of the two specimens was analyzed by Kappa analysis and principal component analysis. Results The main pathogens cultured in the catheter end culture and tracheal suction specimens were Acinetobacter baumannii, Pseudomonas aeruginosa, Staphylococcus aureus, and pneumonia Klebsiella. The results of spreaman analysis showed a positive correlation between the results of the two specimens [b]. At the same time, Pseudomonas aeruginosa, normal respiratory flora, Staphylococcus aureus, Klebsiella pneumoniae, and Acinetobacter baumannii were also positively correlated in both specimens [c]. Kappa analysis also showed the consistency of the microbiological culture results of the endotracheal aspirates and the end of catheters was very high [d]. The K values of Pseudomonas aeruginosa, Staphylococcus aureus, Klebsiella pneumoniae and Acinetobacter baumannii were [e], respectively. Meanwhile, the principal component analysis also showed higher similarity. Conclusion The microbiological culture results of tracheal aspiration specimens in patients with ICU mechanical ventilation are similar to those of catheter end cultures. In clinical practice, it has a high reference value as an etiological specimen. Keywords: tracheal aspirate; endotracheal tube end; mechanical ventilation; microorganism; clinical value; consistency analysis Corresponding Author: Xue-sheng Zheng Department of Neurosurgery, Xinhua Hospital, Affiliated to Shanghai Jiao Tong University School of Medicine Address: 1665 Kongjiang Road, Yangpu District, Shanghai 200092, China (PRC) Shanghai Shanghai China (PRC) Tel: 86-15001932566 Corresponding Email: [email protected]

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Final Product
============================== MetaData ============================== Journal: Journal of Cancer Research and Discovery(JCRD) Article Type: Basic Research Article Title: Microbiological analysis of endotracheal aspirate and endotracheal tube cultures in mechanically ventilated patients Short Title: Microbiological ana endotracheal Authors: Zheng Chen (1 3); Xiangyu Q. Wei (3); Xuesheng Zheng (1 2); Affiliations: 1: At the same time, Pseudomonas aeruginosa, normal respiratory flora 2: But results of endotracheal tube and endotracheal 3: The main pathogens cultured in the catheter end culture
Abstract: Abstract Objective To analyze the consistency of microbiological culture results between endotracheal aspirate and endotracheal tube end specimens in ICU patients with mechanical ventilation. Method From January 2017 to December 2017 a total of 81 patients undergoing mechanical ventilation in the[a] intensive care unit were continuously enrolled. The results of endotracheal tube and endotracheal aspirate cultures were recorded and analyzed. Spearman correlation analysis was used to analyze the relevance of the results of the twospecimens. The consistency of the results of the two specimens was analyzed by Kappa analysis and principal component analysis. Results The main pathogens cultured in the catheter end culture and tracheal suction specimens were Acinetobacter baumannii, Pseudomonas aeruginosa, Staphylococcus aureus, and pneumonia Klebsiella. The results of spreaman analysis showed a positive correlation between the results of the two specimens [b]. At the same time, Pseudomonas aeruginosa, normal respiratory flora, Staphylococcus aureus, Klebsiella pneumoniae, and Acinetobacter baumannii were also positively correlated in both specimens [c]. Kappa analysis also showed the consistency of the microbiological culture results of the endotracheal aspirates and the end ofcatheters was very high [d]. The K values of Pseudomonas aeruginosa, Staphylococcus aureus, Klebsiella pneumoniae and Acinetobacter baumannii were [e], respectively. Meanwhile, the principal component analysis also showed higher similarity. Conclusion The microbiological culture results of tracheal aspiration specimens in patients with ICU mechanical ventilation are similar to those of catheter end cultures. In clinical practice, it has a high reference value as an etiological specimen. Keywords: tracheal aspirate; endotracheal tube end; mechanical ventilation; microorganism; clinical value; consistency analysis Corresponding Author: Xue-sheng Zheng Department of Neurosurgery, Xinhua Hospital, Affiliated to Shanghai Jiao Tong University School of Medicine Address: 1665 Kongjiang Road, Yangpu District, Shanghai 200092, China (PRC) Shanghai Shanghai China (PRC) Tel: 86-15001932566 Corresponding Email: [email protected]

Final Product
Cover Letter
Dear Editor in Chief:
We would like to submit the revised manuscript entitled “FM19G11
inhibits O6-methylguanine DNA-methyltransferase expression under
both hypoxic and normoxic conditions”, which we wish to be considered
for publication in Cancer Medicine.
The authors declare no conflicts of interest.
We have reviewed the final version of the manuscript and approve it
for publication. To the best of our knowledge and belief, this manuscript
has not been published in whole or in part nor is it being considered for
publication elsewhere.
Best Regards.
Yours Sincerely,
Chao-guo You, Han-song Sheng, Chao-ran Xie, Nu Zhang, Xue-sheng Zheng

Final Product
FM19G11 is a low-toxicityinhibits O6-methylguanine
DNA-methyltransferase inhibitor expression under
both hypoxic and normoxic conditions

Final Product
Abstract:
Background: FM19G11 is a small molecular agent that inhibits hypoxia-inducible factor-1-alpha
(HIF-1α) and other signaling pathways. In this study, we characterized the modulating effects of
FM19G11 on O6-methylguanine DNA-methyltransferase (MGMT), the main regulator of
temozolomide (TMZ) resistance in glioblastomas.
Methods: This study included two MGMT-positive cell lines (GBM-XD and T98G). MGMT
promoter methylation status, mRNA abundance, and protein levels were determined before and
after FM19G11 treatment, and the roles of various signaling pathways were characterized.
Results: Under hypoxic conditions, MGMT mRNA and protein levels were significantly
downregulated by FM19G11 via the HIF-1α pathway in both GBM-XD and T98G cells. In
normoxic culture, T98G cells were strongly positive for MGMT, and MGMT expression was
substantially down-regulated by FM19G11 via the NF-κB pathway. In addition, TMZ resistance
was reversed by treatment with FM19G11. Meanwhile, FM19G11 has no cytotoxicity at its
effective dose.
Conclusions: FM19G11 could potentially be used to counteract TMZ resistance in MGMT-
positive glioblastomas.
Keywords: FM19G11; O6-methylguanin DNA-methyltransferase; glioblastoma
Abbreviation list:
O6-methylguanin DNA-methyltransferase (MGMT)
Glioblastoma (GBM)
Temozolomide (TMZ)
Overall survival (OS)

Final Product
Introduction
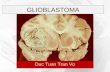
Glioblastoma (GBM) is the most common primary malignant brain tumor in adults,
accounting for approximately 39% of central nervous system neoplasms. Treatment typically
includes maximal safe resection plus post-operative adjuvant ionizing radiation and
chemotherapy with temozolomide (TMZ). In 2005, Stupp et al. reported a 2.5-month
overall survival (OS) benefit with the addition of the alkylating agent TMZ to surgery and
radiation ; thus, this treatment plan is termed Stupp’s regimen.
Although the median survival time of GBM patients receiving the Stupp regimen is only 14.6
months, it is noteworthy that patients with low O6-methylguanin DNA-methyltransferase
(MGMT) expression benefit more from TMZ chemotherapy than patients with high MGMT
expression . According to a recent study, the median OS of a low-MGMT group of GBM patients
receiving the Stupp regimen was 21.8 months, while that of a high-MGMT group was only 13.1
months .
TMZ exhibits cytotoxicity mostly by methylating the O6 position of guanine and then causing
tumor cell apoptosis. MGMT directly removes the methyl group at the O6 position of guanine and
thus reverses the cytotoxic effects of TMZ . Therefore, inhibition of MGMT expression may help
to overcome TMZ resistance in GBM .
If the MGMT promotor is methylated, the gene is silenced . Otherwise, the gene will be
expressed, and the expression efficiency is modulated by many mechanisms, including the
hypoxia-inducible factor-1-alpha (HIF-1α), NF-κB , and WNT/β-catenin pathways .
Recently, Tang et al. reported that the HIF-1α inhibitor 2-methoxyestradiol (2-ME)
downregulated MGMT expression under hypoxic conditions . However, 2-ME is highly cytotoxic,
which limits further investigation in pre-clinical settings, and it only exerts an effect under
hypoxic conditions . FM19G11 is a novel small molecule (molecular weight: 463.40 g/mol) HIF-
1α inhibitor with an effective dose in the nanomolar range, and it is very safe at concentrations
lower than 30 μM . In addition, FM19G11 modulates other signaling pathways, including mTOR
and PI3K/Akt/eNOS , when the HIF-1α pathway is inactivated under normoxic conditions.
Therefore, we hypothesized that FM19G11 suppresses MGMT expression under both hypoxic and

Final Product
normoxic conditions through different mechanisms. The present study was performed to test this
hypothesis.

Final Product
Methods
GBM cell culture: The T98G GBM cell line was provided and authenticated by the Shanghai
Institute of Biochemistry and Cell Biology, Shanghai, China. GBM-XD is a primary cell strain
derived from the surgical specimen of a patient with World Health Organization grade IV GBM
undergoing resection in accordance with a protocol approved by the Ethics Committee of our
hospital, and with prior informed consent from the patient. The culture medium was composed of
DMEM (Life Technologies/GIBCO, Carlsbad, CA, USA) and 10% fetal bovine serum (FBS; Life
Technologies/GIBCO). The cells were cultured at a density of 1 × 105 cells /ml. For normoxic
culture, the cells were incubated at 37°C with 95% air, 5% CO2, and 100% humidity. For hypoxic
culture, the cells were incubated at 37°C with 1% O2, 5% CO2, and 100% humidity.
Cell viability assay: The cytotoxic effects of TMZ (Sigma-Aldrich, St. Louis, MO, USA) and
FM19G11 (Sigma-Aldrich) were measured using the CellTiter 96 AQueous Non-Radioactive Cell
Proliferation Assay (Promega Corp., Madison, WI, USA) following the manufacturer’s protocol.
Briefly, GBM-XD and T98G cells were seeded in 96-well flat-bottom plates at 5,000 cells/well,
cultured in DMEM supplemented with 10% FBS, and then treated with TMZ and/or FM19G11, or
DMSO as a control. A mixture of 100 µl phenazine methosulfate (PMS) and 2 ml of [3-(4,5-
dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS)
reagent was freshly prepared. Next, 20 µl of MTS/PMS mix reagent was added to 100 µl of media
per well, and the cells were incubated at 37°C for 2 h. The optical density (OD) was measured at
490 nm with a spectrophotometer. Relative cell viability was expressed as the ratio of the OD of
TMZ and/or FM19G11-treated cells to the OD of control cells.
Western blotting: Cells were rinsed with phosphate-buffered saline (PBS), lysed in
radioimmunoprecipitation assay (RIPA) buffer (150 mM NaCl, 25 mM Tris [pH 7.4], 1% Triton
X-100, 0.5% sodium dodecyl sulfate [SDS], and 5 mM EDTA), and cleared by centrifugation in a
microfuge at 20,000 × g for 15 min. The protein concentration was determined using bovine
serum albumin as the standard. Equal amounts of protein were used for SDS polyacrylamide gel

Final Product
electrophoresis (SDS-PAGE). Gels were electroblotted onto nitrocellulose membranes that were
blocked for 1 h with 5% non-fat dry milk in tris-buffered saline (TBS) containing 0.1% Tween-20.
The membranes were then incubated at 4°C overnight with primary antibodies. After rinsing in
PBS, the membranes were incubated at room temperature for 1 h with peroxidase-conjugated
secondary antibodies, and then developed using the enhanced chemiluminescence (ECL) system
(Amersham Biosciences, Little Chalfont, United Kingdom). The primary antibodies used were
specific for MGMT, GAPDH, IKBα, IKKα, P65, TCF1, LEF1, -catenin, c-Myc, C-Jun, HIF-1α,
EPO, and VEGF (ABCAM, Cambridge, USA).
Real-time reverse transcription (RT)-PCR: Total RNA from GBM-XD and T98G cells was
extracted using TRIzol reagent (Invitrogen Corp., Carlsbad, CA, USA) according to the
manufacturer’s instructions. RT was carried out with 2 μg of RNA as the template in a total
volume of 20 µl with a RevertAid First Strand cDNA Synthesis Kit (Fermentas, Waltham, MA,
USA). The primer sequences for the MGMT gene were: Forward, 5'-
GTTATGAATGTAGGAGCCCTTATG-3'; and Reverse, 5'-TGACAACGGGAATGAAGTAATG-
3'. The amplicon size was 239 bp. Real-time PCR was performed with the SuperScript III OneStep
RT-PCR System (Thermo Fisher Scientific, Waltham, MA, USA), according to the manufacturer’s
instructions. The results are expressed as relative mRNA levels (mRNA level in FM19G1-treated
cells/mRNA level in untreated control cells).
Immunofluorescence staining: Tumor cells were cultured on coverslips. After the cells attached to
the slips over 24 h, FM19G11 was added to the culture media for 72 h. The cells were then fixed
with 4% formaldehyde (10 min), permeabilized with 0.1% Triton X-100 for 5 min, and blocked
with 1% BSA/10% normal goat serum for 1 h. The cells were then incubated with anti-MGMT
antibodies (Abcam, Cambridge, USA) overnight at 4°C in the dark, followed by incubation at
room temperature for 1 h with secondary antibodies (Abcam). Then, the slips were rinsed in PBST
once and in PBS twice, and mounted with DAPI mounting solution. The slips were immediately
examined under a fluorescence microscope.
Flow cytometry: T98G cells were dissociated with 0.25% trypsin to prepare a cell suspension. The

Final Product
suspension was filtered through a cell strainer to remove cell clusters. The total cell number was
then counted. The single-cell suspension was centrifuged at 600 rpm for 1–2 minutes at 4°C to
remove the supernatant. The cell pellet was then resuspended in 5 ml of DMEM supplemented
with 10% FBS. TMZ (500 μM) and/or FM19G11 (300 nM) was then added to the cells, followed
by 2 h of incubation at 37°C. The cells were then washed with cold PBS and stained with an
Annexin V-FITC/propidium iodide solution (BD Biosciences, CA, USA). The samples were
analyzed on a flow cytometer (Beckman Coulter, Brea, CA, USA) using a 488-nm excitation
wavelength.
Bisulfite sequencing PCR (BSP): Genomic DNA was extracted from GBM-XD cells using a
Genomic DNA Mini Tissue Kit (Invitrogen Corp.). Sodium bisulfite modification of 2 μg DNA
was carried out using a MethylEasy DNA Bisulfite Modification Kit (Human Genetic Signatures,
Sydney, Australia). The MGMT promoter-associated CpG island is 267 bp in length and contains
27 CpG sites. The following primer pairs were used: F, 5'-GGATATGTTGGGATAGTT-3'; and R,
5'-AAACTAAACAACACCTAAA-3'. The PCR mixture contained 1 μl of each primer, 3 μl of
bisulfite-treated DNA, 0.8 μl of Taq DNA polymerase (4 U), and 200 mM dNTPs in a final
volume of 50 μl. PCR was performed with an initial denaturation step at 98°C for 4 min followed
by 40 cycles of denaturation at 94°C for 45 s, annealing at 56°C for 45 s, and extension for 1 min
at 72°C, and a final extension at 72°C for 8 min. The PCR products were cleaned using a
ChargeSwith PCR Clean-Up Kit (Invitrogen Corp.) and cloned using pUC18-T (Sangon Biotech,
Shanghai, China). The bacterial colonies containing the recombinant plasmid were amplified, and
the plasmid was extracted. The plasmid was then sequenced. Ten clones were sequenced for each
sample.
Statistical analysis: An analysis of variance was used to analyze the cell viability assay data. The
chi-square test was used to analyze the flow cytometry data. P<0.05 was accepted as statistically
significant.

Final Product
Results
Immunocytochemistry and Western blotting showed that both GBM-XD and T98G cells were
MGMT-positive in hypoxic culture (Figures 1 and 2). After FM19G11 treatment (300 nM for 3
days), MGMT expression was significantly suppressed in both cell lines (Figures 1 and 2). In
normoxic culture, T98G cells were strongly positive for MGMT, and MGMT expression was
substantially down-regulated by FM19G11. However, MGMT expression in GBM-XD cells was
weak in normoxic culture, and the effect of FM19G11 on MGMT expression was unobservable
(Figures 1 and 2). Similarly, the mRNA levels of MGMT were significantly down-regulated by
FM19G11 treatment in hypoxic GBM-XD, hypoxic T98G, and normoxic T98G cells (Figure 3).
Since promotor methylation is the main regulator of MGMT transcription, we examined the
methylation status of the MGMT promoter and found that GBM-XD was completely
unmethylated, and that T98G was partially unmethylated, with only 1 of the 27 CpG sites
methylated. After FM19G11 treatment (300 nM for 30 days), the promoter methylation status did
not change in either cell line (Figure 4), suggesting that the effect of FM19G11 on MGMT
expression is unrelated to promotor methylation.
We next explored several signaling pathways that may be involved in the modulation of MGMT
transcription under hypoxic conditions. HIF-1α was expressed in GBM-XD and T98G cells. After
FM19G11 treatment, the levels of HIF-1α and its target genes EPO and VEGF were decreased,
and the change was similar to that of MGMT (Figure 5). For the WNT/β-catenin pathway, the β-
catenin levels remained constant in the absence or presence of FM19G11. In addition, the related
transcription factors TCF1 and LEF1 and the target genes C-JUN and C-MYC changed irregularly
after FM19G11 treatment (Figure 6). For the NF-κB pathway, we found that P65, a member of the
NF-κB family, and the regulatory molecules IKBα and IKKα were unaffected by FM19G11
(Figure 7). Taken together, we conclude that under hypoxic conditions FM19G11 inhibits
MGMT expression mainly via the HIF-1α pathway.
Under normoxic conditions, HIF-1α is inactivated, so we explored only the WNT/β-catenin and
NF-κB pathways. Again, the second messenger β-catenin remained unchanged after FM19G11
treatment, and TCF1, LEF1, C-JUN, and C-MYC changed irregularly (Figure 8). For the NF-κB

Final Product
pathway, P65 decreased dramatically after FM19G11 treatment in T98G cells in normoxic culture,
and the change was similar to that of MGMT (Figure 9). However, the regulatory molecules IKBα
and IKKα did not change. These results suggest that, under normoxic conditions, FM19G11
directly inhibits NF-κB and thus down-regulates MGMT expression.
As shown in Figure 10, the cell viability assay demonstrated that FM19G11 (300 nM for 3
days) had no cytotoxicity by itself. However, FM19G11 significantly enhanced the cytotoxicity of
TMZ (100 µM for 3 days) in hypoxic GBM-XD cells (TMZ group 0.754 ± 0.048 vs.
TMZ+FM19G11 group 0.464 ± 0.015, P<0.05), hypoxic T98G cells (TMZ group 0.498 ± 0.016
vs. TMZ+FM19G11 group 0.339 ± 0.009, P<0.05), and normoxic T98G cells (TMZ group 0.488 ±
0.012 vs TMZ+FM19G11 group 0.327 ± 0.010, P<0.05). Flow cytometry showed that the early
apoptosis percentage was 18.9% in the TMZ group and 26.6% in the TMZ+FM19G11 group
(P<0.05), while the late apoptosis percentage was 27.0% in the TMZ group and 36.8% in the
TMZ+FM19G11 group (P<0.05). These results indicate that FM19G11 significantly enhanced the
pro-apoptotic effect of TMZ, although FM19G11 did not induce apoptosis by itself (Figure 11).

Final Product
Discussion
The alkylating agent TMZ is currently the standard chemotherapy for GBM . As a prodrug, it
undergoes spontaneous decomposition in solution at a physiological pH to the reactive
intermediate 5-(3-methyl-1-triazeno)imidazole-4-carboxamide, which methylates the N7 and O6
positions of guanine and the N3 position of adenine . Among these three methylation positions, O6-
methylguanine (O6-meG) is the most important mismatch; it results in a continuous cycle of DNA
base mismatch repair with eventual strand breaks, ultimately leading to cellular apoptosis, which
is how TMZ exerts its chemotherapeutic effects .
However, if MGMT is expressed in tumor cells it will directly remove the methyl group from
O6-meG, causing the cells to become TMZ-resistant . Every methyl group removed from O6-meG
is transferred to a cysteine residue within the active site of MGMT in a stoichiometric reaction,
and this MGMT molecule is then inactivated and finally degraded. This process of destruction of
one MGMT molecule for each methyl group removed from methylguanine is termed suicide
inhibition . Therefore, TMZ cytotoxicity is theoretically determined by the ratio of MGMT to O6-
meG .
Many different agents have been tested for their ability to inhibit MGMT, with little success .
For example, TMZ itself was shown to partially deplete MGMT protein in tumors. In clinical
practice, a dose-dense TMZ regimen is applied to some recurrent MGMT-unmethylated gliomas ,
based on the idea that a high dose of TMZ would probably deplete MGMT in tumor cells via
suicide inhibition . However, these large clinical trials failed to produce an OS benefit of
increasing TMZ dose intensity . Another limitation of this strategy is that high-dose drug exposure
inevitably leads to increased side effects .
Some other chemotherapeutic agents have been tried to bypass the limitations of TMZ in
MGMT unmethylated patients, including 1,3-bis(2-chloroethyl)1-nitrosourea or 3-[(4-amino-2-
methyl-5-pyrimidinyl) methyl]-1-(2-chloroethyl)-1-nitrosourea hydrochloride. However, the
hematological side effects of these drugs are much more frequent and severe than TMZ .
Another potential method was to sensitize glioma cells to TMZ by concomitant use of the
MGMT pseudosubstrate. One potent agent is O6-BG, a pseudosubstrate inactivator of MGMT.

Final Product
This agent has been shown to reverse resistance to TMZ by decreasing MGMT protein levels in
glioma cells and animal models . However, in a clinical trial, the addition of O6-BG had little
therapeutic effect, and caused grade 4 hematological events in 48% of the patients, halting further
attempts to use this concomitant therapy .
Taken together, the above mentioned agents have a common drawback; namely, severe side
effects, which limits further study. Therefore, it is necessary to search for new agents to suppress
MGMT expression, especially ones with low cytotoxicity.
FM19G11 is a small molecule agent with a molecular weight of only 463.40 g/mol . In this
study, we showed that under hypoxic conditions, FM19G11 significantly inhibited MGMT
expression in GBM cells by modulating the HIF-1α pathway. However, under normoxic
conditions, when the HIF-1α pathway was inactivated, FM19G11 inhibited MGMT expression by
modulating the NF-κB pathway. Since there are considerable oxygen concentration gradients in
the lungs and across the capillaries and tumor tissues, the oxygen levels in the tumor should be
lower than that in the air, which is defined as “normoxic condition” in this in vitro study.
Therefore, under the in vivo micro-environments, HIF-1α pathway may play a more important
role than the NF-κB pathway.
Our findings reveal that FM19G11 by itself was not cytotoxic at its effective dose (300 nM for
3 days), implying that this agent is safe for future clinical use. Whenbut when FM19G11 was
given concomitantly with TMZ, it strongly enhanced the pro-apoptotic effect of TMZ. Therefore,
FM1911 could be a candidate for future pre-clinical testing to counteract TMZ resistance in
MGMT-positive glioblastomas. There is a concern that unselective MGMT inhibition is likely to
make the normal tissues, for example, the hematopoietic tissues, more vulnerable to the
cytotoxicity of TMZ, and this might be a major reason for the failure of the above-mentioned
clinical trials. But since the malignant tumor tissue is generally in hypoxic state (Tang et al.
2016), and the MGMT-inhibition effect of FM19G11 majorly relies on the hypoxia-inducible
factor-1-alpha pathway, we think FM19G11 probably preferentially inhibit MGMT activity in
tumor than in the normal tissues. This indirect MGMT-inhibition strategy may be better tolerable
for the body.
Although both TMZ and FM19G11 are from Sigma-Aldrich, the authors declared that there is
no conflict of interest.

Final Product

Final Product
References
Belanich M et al. (1996) Intracellular Localization and intercellular heterogeneity of the human DNA
repair protein O(6)-methylguanine-DNA methyltransferase Cancer chemotherapy and
pharmacology 37:547-555
Dahlrot RH et al. (2017) Prognostic value of O-6-methylguanine-DNA methyltransferase (MGMT)
protein expression in glioblastoma excluding nontumour cells from the analysis
Neuropathology and applied neurobiology doi:10.1111/nan.12415
El Assar M et al. (2015) FM19G11 reverses endothelial dysfunction in rat and human arteries through
stimulation of the PI3K/Akt/eNOS pathway, independently of mTOR/HIF-1alpha activation
British journal of pharmacology 172:1277-1291 doi:10.1111/bph.12993
Fu D, Calvo JA, Samson LD (2012) Balancing repair and tolerance of DNA damage caused by
alkylating agents Nature reviews Cancer 12:104-120 doi:10.1038/nrc3185
Gilbert MR et al. (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized
phase III clinical trial Journal of clinical oncology : official journal of the American Society of
Clinical Oncology 31:4085-4091 doi:10.1200/JCO.2013.49.6968
Hegi ME et al. (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma The New
England journal of medicine 352:997-1003 doi:10.1056/NEJMoa043331
Hegi ME et al. (2008) Correlation of O6-methylguanine methyltransferase (MGMT) promoter
methylation with clinical outcomes in glioblastoma and clinical strategies to modulate MGMT
activity Journal of clinical oncology : official journal of the American Society of Clinical
Oncology 26:4189-4199 doi:10.1200/JCO.2007.11.5964
Kaloshi G et al. (2010) Nitrosourea-based chemotherapy for low grade gliomas failing initial treatment
with temozolomide Journal of neuro-oncology 100:439-441 doi:10.1007/s11060-010-0197-6
Kreklau EL, Liu N, Li Z, Cornetta K, Erickson LC (2001) Comparison of single- versus double-bolus
treatments of O(6)-benzylguanine for depletion of O(6)-methylguanine DNA
methyltransferase (MGMT) activity in vivo: development of a novel fluorometric
oligonucleotide assay for measurement of MGMT activity The Journal of pharmacology and
experimental therapeutics 297:524-530
Lan F, Yang Y, Han J, Wu Q, Yu H, Yue X (2016) Sulforaphane reverses chemo-resistance to
temozolomide in glioblastoma cells by NF-kappaB-dependent pathway downregulating
MGMT expression International journal of oncology 48:559-568 doi:10.3892/ijo.2015.3271
Moreno-Manzano V et al. (2010) FM19G11, a new hypoxia-inducible factor (HIF) modulator, affects
stem cell differentiation status The Journal of biological chemistry 285:1333-1342
doi:10.1074/jbc.M109.008326
Nagane M (2015) Dose-dense temozolomide: is it still promising? Neurologia medico-chirurgica

Final Product
55:38-49 doi:10.2176/nmc.ra.2014-0277
Penas-Prado M et al. (2015) Randomized phase II adjuvant factorial study of dose-dense temozolomide
alone and in combination with isotretinoin, celecoxib, and/or thalidomide for glioblastoma
Neuro-oncology 17:266-273 doi:10.1093/neuonc/nou155
Quinn JA et al. (2009) Phase II trial of temozolomide plus o6-benzylguanine in adults with recurrent,
temozolomide-resistant malignant glioma Journal of clinical oncology : official journal of the
American Society of Clinical Oncology 27:1262-1267 doi:10.1200/JCO.2008.18.8417
Rodriguez-Jimenez FJ, Moreno-Manzano V, Mateos-Gregorio P, Royo I, Erceg S, Murguia JR,
Sanchez-Puelles JM (2010) FM19G11: A new modulator of HIF that links mTOR activation
with the DNA damage checkpoint pathways Cell cycle 9:2803-2813
doi:10.4161/cc.9.14.12184
Shirai K, Chakravarti A (2011) Towards personalized therapy for patients with glioblastoma Expert
review of anticancer therapy 11:1935-1944 doi:10.1586/era.11.103
Stupp R et al. (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma The
New England journal of medicine 352:987-996 doi:10.1056/NEJMoa043330
Tang JH et al. (2016) Downregulation of HIF-1a sensitizes U251 glioma cells to the temozolomide
(TMZ) treatment Experimental cell research 343:148-158 doi:10.1016/j.yexcr.2016.04.011
Terasaki M, Tokutomi T, Shigemori M (2009) Salvage therapy with temozolomide for recurrent or
progressive high-grade gliomas refractory to ACNU [1-(4-amino-2-methyl-5-pyrimidynyl)
methyl-3-(2-chloroethyl)-3-nitrosourea hydrochloride] Molecular medicine reports 2:417-421
doi:10.3892/mmr_00000115
van Nifterik KA et al. (2010) Absence of the MGMT protein as well as methylation of the MGMT
promoter predict the sensitivity for temozolomide British journal of cancer 103:29-35
doi:10.1038/sj.bjc.6605712
Weller M, Stupp R, Reifenberger G, Brandes AA, van den Bent MJ, Wick W, Hegi ME (2010) MGMT
promoter methylation in malignant gliomas: ready for personalized medicine? Nature reviews
Neurology 6:39-51 doi:10.1038/nrneurol.2009.197
Wickstrom M et al. (2015) Wnt/beta-catenin pathway regulates MGMT gene expression in cancer and
inhibition of Wnt signalling prevents chemoresistance Nature communications 6:8904
doi:10.1038/ncomms9904

Final Product
Figure legends
Figure 1: Western blotting. Both GBM-XD and T98G cells were positive for MGMT in hypoxic
culture. After FM19G11 treatment (300 nM for 3 days), MGMT expression was significantly
suppressed in both cell lines. In normoxic culture, T98G cells were strongly positive for MGMT,
and MGMT expression was substantially down-regulated by FM19G11. However, MGMT
expression in GBM-XD cells was weak, and the effect of FM19G11 on MGMT expression was
unobservable.
Figure 2: Immunocytochemistry. Both GBM-XD and T98G cells were positive for MGMT in
hypoxic culture. MGMT expression was significantly suppressed in both cell lines by FM19G11.
In normoxic culture, T98G cells were strongly positive for MGMT, and MGMT expression was
substantially down-regulated by FM19G11. However, GMT expression in GBM-XD cells was
weak in normoxic culture.
Figure 3: RT-PCR. The mRNA levels of MGMT were significantly down-regulated by FM19G11
treatment in hypoxic GBM-XD, hypoxic T98G, and normoxic T98G cells.
Figure 4: BSP. The GBM-XD promotor was completely unmethylated, and T98G promotor had
only one CpG site methylated. After FM19G11 treatment (300 nM for 30 days), the promoter
methylation status did not change in either cell line.
Figure 5: Under hypoxic conditions, HIF-1α was expressed in both GBM-XD and T98G cells.
After FM19G11 treatment, the levels of HIF-1α and its target genes EPO and VEGF were
decreased, and the change was similar to that of MGMT.
Figure 6: Under hypoxic conditions, the β-catenin levels remained constant in the absence or
presence of FM19G11. In addition, the related transcription factors TCF1 and LEF1 and the target
genes C-JUN and C-MYC changed irregularly after FM19G11 treatment.
Figure 7: Under hypoxic conditions, P65, a member of the NF-κB family, and the regulatory
molecules IKBα and IKKα were unaffected by FM19G11.
Figure 8: Under normoxic conditions, β-catenin remained unchanged after FM19G11 treatment,
while TCF1, LEF1, C-JUN, and C-MYC changed irregularly.
Figure 9: Under normoxic conditions, P65 decreased dramatically after the FM19G11 treatment of
T98G cells, and the change was similar to that of MGMT. However, the regulatory molecules
IKBα and IKKα did not change accordingly.

Final Product
Figure 10: Cell viability assay. FM19G11 (300 nM for 3 days) had no cytotoxicity by itself.
However, FM19G11 significantly enhanced the cytotoxicity of TMZ (100 µM for 3 days) in
hypoxic GBM-XD cells (TMZ group 0.754 ± 0.048 vs. TMZ+FM19G11 group 0.464 ± 0.015,
P<0.05), hypoxic T98G cells (TMZ group 0.498 ± 0.016 vs. TMZ+FM19G11 group 0.339 ±
0.009, P<0.05), and normoxic T98G cells (TMZ group 0.488 ± 0.012 vs TMZ+FM19G11 group
0.327 ± 0.010, P<0.05).
Figure 11: Flow cytometry. The early apoptosis percentage was 18.9% in the TMZ group and
26.6% in the TMZ+FM19G11 group (P<0.05), while the late apoptosis percentage was 27.0% in
the TMZ group and 36.8% in the TMZ+FM19G11 group (P<0.05). In contrast, the early and late
apoptosis percentages for the FM19G11 group did not exceed that of the control.

Final Product
微微微微微微微微微微微微微微微微微微微微微李李李 李李李李李李李李李李
李李李李李李(MVD)李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李MVD 李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李“李李
李李李李”李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微 微微微微微微微李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李(Zhong, 2003 Neurol Res)李李
李李李李李李李李李李李李李“李李李李李李李”李李李李李李李李李李李李李李李李李李李李李李李李 MVD 李李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李(Zhong & Li, 2011 Neurosurg)李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
李 1. 李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微 微微微微微微微微微微微微微微李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微微微微微微微微微微微微微微微微微微微微微微微微李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李①李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李 1李李②李李李李李李李李李李李李李李李李李李李李李李李李李李李
李李李李李李李李李李李 2李李③李李李李李李李李李李李李李李/李李李李李李李李李李李李李李李李李李李 3李李④李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李 4李李⑤李李李李李李李李李李李李李李李李李李李李李李李
李李李李李李李李李李李李李李李李李 5李李

Final Product微微微微微微微微微微微微微微微微微
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李 REZ 李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
1 2
4 5
1
2
5
4
3
3

Final Product
微微微微微微微微微微微微微微微微微微李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微微微微微微微微微微微微微微微李李李李李李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
李李2mm李李李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李 15 李李李 BTEP李BAEP 李李李李李李李李李李李李李李
李李李李李李李李李 20%李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李Zhong & Li,
2008 Neurol Res)李
微微微微微微微微微微微微微微微微微
李李李李 800 李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微微微微微微微微微微微微微微微
患患
患患 患患
患患 患患
患患 患患患
患患 患患 患患患 MRI(+)MRI(-)
患患患MVD患患
患患MVD患患 r-患,患患,患患患患
患患患患患

Final Product
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李(Zhong & Li, 2010 Acta Neurochir;
Zheng & Li, 2010 Acta Neurochir)李李李李李李李李李李李李李李李 REZ 李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李
微微微微微微微微微微微微微微微微 李李李李李李李李李李李李李李李李李李BTEP李AMR李BAEP李李李李李李李李李李李李李 ZLR 李李李李李李李李李
李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李李(Ying & Zhong, 2011 Int J
Surg)李
李1李李李李李李李李李李李李 AMR 李李李
李2李李李李李李李李李李李李 ZLR 李李李
李3李李李李李李李李李李李李李 BTEP 李李李

Final Product
Dear Dr. Zheng:
Manuscript ID CAM4-2018-01-0130 entitled "FM19G11 is a low-toxicity O6-methylguanine DNA-
methyltransferase inhibitor under both hypoxic and normoxic conditions" which you submitted to
Cancer Medicine, has been reviewed. Some revisions to your manuscript have been
recommended. Therefore, I invite you to respond to the comments appended below and revise
your manuscript.
Before submitting your revisions:
1. Prepare a response to the reviewer comments appended below in point-by-point fashion. In
order to expedite the processing of the revised manuscript, please be as specific as possible in
your response and indicate the page numbers in the manuscript where you have addressed each
comment.
2. Prepare a revised manuscript (word document), highlighting the changes you’ve made. Save
this new document on your computer as you will be asked to upload it during the revision
submission process. NOTE: Please be sure to keep in mind reviewer comments and incorporate
your responses within the manuscript. There may well be areas where you disagree; for example,
you may want to write, "A reviewer suggests that... However, I disagree because...". In any case,
please try to address all of the concerns that are raised within the manuscript as carefully and
adequately as possible in order to avoid unnecessary repetition of the revision process.
3. In addition to your revised manuscript with changes highlighted, please also save a “clean”
copy where the changes are not marked.
To submit your revised manuscript:
1. Log in by clicking on the link below
*** PLEASE NOTE: This is a two-step process. After clicking on the link, you will be directed to a
webpage to confirm. ***
https://mc.manuscriptcentral.com/cancermedicine?
URL_MASK=b4b7b616a59a4d28926796a539303eb1
OR
Log into https://mc.manuscriptcentral.com/cancermedicine and click on Author Center. Under
author resources, use the button “Click here to submit a revision”. PLEASE DO NOT SUBMIT YOUR
REVISIONS AS A NEW MANUSCRIPT.
2. Follow the on-screen instructions. First you will be asked to provide your “Response to
Decision Letter”—this is the response to reviewer comments that you prepared earlier.

Final Product
3. Click through the next few screens to verify that all previously provided information is correct.
4. File Upload: Delete any files that you will be replacing (this includes your old manuscript).
Upload your new revised manuscript file with changes highlighted, a “clean” copy of your revised
manuscript file, any replacement figures/tables, or any new files. Once this is complete, the list of
files in the “My Files” section should ONLY contain the final versions of everything. REMEMBER:
figures/tables should be in jpeg, tiff, or eps format.
5. Review and submit: please be sure to double-check everything carefully so that your
manuscript can be processed as quickly as possible.
Deadlines:
Because we are trying to facilitate timely publication of manuscripts submitted to Cancer
Medicine,your revised manuscript should be uploaded as soon as possible. If it is not possible for
you to submit your revision in 2 months, we may have to consider your paper as a new
submission. If you feel that you will be unable to submit your revision within the time allowed
please contact me to discuss the possibility of extending the revision time.
Keep up to date with Cancer Medicine's new content by signing up for the journal's email alerts
at http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)2045-
7634/homepage/get_email_alerts.htm
If you feel that your paper could benefit from English language polishing, you may wish to
consider having your paper professionally edited for English language by a service such as Wiley’s
at http://wileyeditingservices.com. Please note that while this service will greatly improve the
readability of your paper, it does not guarantee acceptance of your paper by the journal.
Once again, thank you for submitting your manuscript to Cancer Medicine and I look forward to
receiving your revision.
Sincerely,
Dr. Qingyi Wei
Editor in Chief, Cancer Medicine
Associate Editor Comments to Author:
Associate Editor
Comments to the Author:
(There are no comments.)
Reviewer(s)' Comments to Author:

Final Product
Reviewer: 1
Comments to the Author
This paper describes FM19G11 which is a low-toxicity indirect O6-methylguanine DNA
methyltransferase inhibitor. Most previous attempts at MGMT inhibition involve the use of low
molecular weight pseudo-substrates that directly and irreversibly inactivate this repair protein. It
should be noted that most of these other inhibitors are of low toxicity in the absence of
alkylation stress at the O-6 position of DNA guanine. From a technical point of view a
considerable amount of well executed experimental work has been performed and the actions of
this interesting molecule have been further characterized. The authors demonstrate a potent
down regulation of MGMT expression via the action of this agent on key signaling pathways, and I
believe this data merits publication. However, I strongly feel that the overall strategy present in
this paper needs to be revised as no strong evidence is presented to explain why this MGMT
inhibitory strategy will succeed therapeutically, when in all previous clinical attempts the
successful in vivo inhibition of MGMT has resulted in negative consequences. I believe that the
non-tumor selective inhibition of MGMT rationale expressed in this paper is fundamentally
flawed and all such agents will by their very nature reduce the therapeutic index of agents such
as temozolomide compared to temozolomide alone. To improve the therapeutic utility of
temozolomide (against MGMT expressing low responsive tumors) this molecule would need to
either exert the observed actions in a tumor cell selective manner or require some additional
mechanism to ensure selective or at least preferential tumor delivery so as not to also reduce
normal tissue MGMT activity. The tumor selectivity of guanine O-6 alkylating agents does not
appears to be due to a large toxicity differential resulting from the lesions themselves, but from
differences in the repair of these lesions by MGMT. Tumors which respond to guanine O-6
alkylating agents do so generally because they contain little or no MGMT activity relative to most
normal tissues, and it is this activity differential that accounts for the majority of their tumor
selectivity. That is, the therapeutic target is essentially the MGMT activity deficit/differential and
is only minimally dependent upon differences between normal and tumor cells in their direct
tolerance or sensitivity to the lesions themselves. Several groups initially argued that MGMT
activity simply represented a barrier preventing the persistence of tumor toxic therapeutic
lesions. Thus it was contended that inhibiting host and tumor protective MGMT activity (as you
have) would allow agents such as temozolomide to act in an unimpaired manner and their utility
would be enhanced, and extended to include the treatment of high MGMT activity tumors.
However, clinical trials have repeatedly demonstrated (as mentioned in this paper) that universal
depletion of MGMT activity (by non-tumor selective strategies) also greatly sensitizes normal
tissues as well as tumor tissues, and actually decreases the therapeutic efficacy. This is the effect
that would be expected if the activity were depended upon a MGMT activity differential. That is,
these inhibitors collapse the host/tumor MGMT activity differential upon which efficacy is based.
Therefore, without a selective action on tumor MGMT activity all universal MGMT inhibitory
strategies are expected to meet the same fate. In essence, the universal ablation of MGMT
activity converts guanine O-6 alkylating agents with selective toxicity to a subset of MGMT
deficient tumors to a universal (host and cancer cell) cytotoxin. Therefore, unless you have a
sound rationale or evidence that FM19G11 will exert the observed actions selectively, the

Final Product
potential therapeutic claims should be strongly attenuated.
An additional point that I think needs to be addressed is the actual levels of oxygen the cells
experienced in your hypoxic and normoxic experiments. The levels of oxygen in the air are not
normoxic as far as tissues are concerned. In fact they are hyperoxic as there are considerable
oxygen concentration gradients in the lungs and across capillaries. Tissue oxygen levels are
typically between 15 - 40 µM (equivalent to a gas mixture containing between ~ 1.5 – 4% oxygen
at 1 atmosphere of pressure). Hypoxic tissues contain levels 0 - 4 µM (equivalent to a gas mixture
containing between ~ 0 - 0.4% oxygen at 1 atmosphere of pressure).
Reviewer: 2
Comments to the Author
Dear editors,
thank you for letting me read this paper on FM19G11. The manuscript is well written and
important in its field. In general, I think the paper is suitable for publication.
Nevertheless I have some comments:
- The authors did not test toxicity of FM19G11. "Low toxicity" should therefore not be mentioned
in the title. Missing cytotoxicity at the effective dose does not necessarily warrant clinical safety.
Otherwise the authors have to present more data.
- Furthermore FM19G11 is not a direct inhibitor of MGMT as implied by the title. Its action is
most probably explained by HIF modulation.
both informations in the title are misleading.
The authors should comment if there is any conflict of interest since TMZ and FM19G11 are from
the same company.

Final Product

Final Product

Final Product

Final Product
FM19G11 inhibits O6-methylguanine DNA-
methyltransferase expression under both hypoxic and
normoxic conditions
Chao-guo You 1,2*, Han-song Sheng 2* , Chao-ran Xie 1,2*, Nu Zhang 2, Xue-sheng Zheng 1#
1 Department of Neurosurgery, Xinhua Hospital, Affiliated to Shanghai JiaoTong University
School of Medicine, Shanghai, China.
2 Department of Neurosurgery, The Second Affiliated Hospital of Wenzhou Medical University,
Wenzhou, Zhejiang, China.
* The first three authors (You CG, Sheng HS and Xie CR) contributed equally to this article.
# Correspondence to: Xue-sheng Zheng, Department of Neurosurgery, Xinhua Hospital, Affiliated
to Shanghai Jiao Tong University School of Medicine, 1665 Kongjiang Road, Yangpu District,
Shanghai 200092, China. Email: [email protected]. Tel: 86-21-25078005. Fax:
86-21-52357635.
Short Running Head: FM19G11 modulates MGMT expression
Conflict of interest statement: We have no conflict of interest. Although both TMZ and FM19G11
are from Sigma-Aldrich, we declare that there is no conflict of interest.
Acknowledge: This study is supported by 2 grants from the Science and Technology Commission
of Shanghai Municipality (#134119a9400 and #14DZ1930303, to Xue-sheng Zheng), 1 grant from
Shanghai Jiaotong University (#YG2015MS65, to Xue-sheng Zheng), and 1 grant from the
Science and Technology Commission of Zhejiang Province (#2016C33SA300055 , to Han-song
Sheng). The English in this document has been checked by at least two professional editors, both
native speakers of English. For a certificate, please see:
http://www.textcheck.com/certificate/oc31XF

Final Product
Detailed Reply to Comments
Reviewer(s)' Comments to Author:
Reviewer: 1
Comments to the Author
This paper describes FM19G11 which is a low-toxicity indirect O6-methylguanine DNA
methyltransferase inhibitor. Most previous attempts at MGMT inhibition involve the use of low
molecular weight pseudo-substrates that directly and irreversibly inactivate this repair protein. It
should be noted that most of these other inhibitors are of low toxicity in the absence of
alkylation stress at the O-6 position of DNA guanine. From a technical point of view a
considerable amount of well executed experimental work has been performed and the actions of
this interesting molecule have been further characterized. The authors demonstrate a potent
down regulation of MGMT expression via the action of this agent on key signaling pathways, and I
believe this data merits publication. However, I strongly feel that the overall strategy present in
this paper needs to be revised as no strong evidence is presented to explain why this MGMT
inhibitory strategy will succeed therapeutically, when in all previous clinical attempts the
successful in vivo inhibition of MGMT has resulted in negative consequences.
Reply: Page 11, our statement as to the future clinical use of FM19G11 is strongly attenuated.
“Our findings reveal that FM19G11 by itself was not cytotoxic at its effective dose (300 nM for 3
days), but when FM19G11 was given concomitantly with TMZ, it strongly enhanced the pro-
apoptotic effect of TMZ. Therefore, FM1911 could be a candidate for future testing to counteract
TMZ resistance in MGMT-positive glioblastomas.” Since the in vivo glioblastoma tissue is
generally in hypoxic state (Tang et al. 2016), and the MGMT-inhibition effect of FM19G11 majorly
relies on the hypoxia-inducible factor-1-alpha pathway, we think FM19G11 probably
preferentially inhibit MGMT activity in tumor than in the normal tissues. This indirect MGMT-
inhibition strategy may be better tolerable for the body.
I believe that the non-tumor selective inhibition of MGMT rationale expressed in this paper is
fundamentally flawed and all such agents will by their very nature reduce the therapeutic index
of agents such as temozolomide compared to temozolomide alone. To improve the therapeutic
utility of temozolomide (against MGMT expressing low responsive tumors) this molecule would
need to either exert the observed actions in a tumor cell selective manner or require some
additional mechanism to ensure selective or at least preferential tumor delivery so as not to also
reduce normal tissue MGMT activity. The tumor selectivity of guanine O-6 alkylating agents does
not appears to be due to a large toxicity differential resulting from the lesions themselves, but
from differences in the repair of these lesions by MGMT. Tumors which respond to guanine O-6
alkylating agents do so generally because they contain little or no MGMT activity relative to most
normal tissues, and it is this activity differential that accounts for the majority of their tumor
selectivity. That is, the therapeutic target is essentially the MGMT activity deficit/differential and
is only minimally dependent upon differences between normal and tumor cells in their direct

Final Product
tolerance or sensitivity to the lesions themselves. Several groups initially argued that MGMT
activity simply represented a barrier preventing the persistence of tumor toxic therapeutic
lesions. Thus it was contended that inhibiting host and tumor protective MGMT activity (as you
have) would allow agents such as temozolomide to act in an unimpaired manner and their utility
would be enhanced, and extended to include the treatment of high MGMT activity tumors.
However, clinical trials have repeatedly demonstrated (as mentioned in this paper) that universal
depletion of MGMT activity (by non-tumor selective strategies) also greatly sensitizes normal
tissues as well as tumor tissues, and actually decreases the therapeutic efficacy. This is the effect
that would be expected if the activity were depended upon a MGMT activity differential. That is,
these inhibitors collapse the host/tumor MGMT activity differential upon which efficacy is based.
Therefore, without a selective action on tumor MGMT activity all universal MGMT inhibitory
strategies are expected to meet the same fate. In essence, the universal ablation of MGMT
activity converts guanine O-6 alkylating agents with selective toxicity to a subset of MGMT
deficient tumors to a universal (host and cancer cell) cytotoxin. Therefore, unless you have a
sound rationale or evidence that FM19G11 will exert the observed actions selectively, the
potential therapeutic claims should be strongly attenuated.
Reply: (1) Page 11, our statement as to the future clinical use of FM19G11 is strongly attenuated.
“Our findings reveal that FM19G11 by itself was not cytotoxic at its effective dose (300 nM for 3
days), but when FM19G11 was given concomitantly with TMZ, it strongly enhanced the pro-
apoptotic effect of TMZ. Therefore, FM1911 could be a candidate for future testing to counteract
TMZ resistance in MGMT-positive glioblastomas.” (2) Page 11. We agree with the concern that
unselective MGMT inhibition is likely to make the normal tissues more vulnerable to the
cytotoxicity of TMZ and this might be a major reason for the failure of the previous clinical trials.
But since the malignant tumor tissue is generally in hypoxic state, and the MGMT-inhibition effect
of FM19G11 majorly relies on the hypoxia-inducible factor-1-alpha pathway, we think FM19G11
probably preferentially inhibit MGMT activity in tumor than in the normal tissues.
An additional point that I think needs to be addressed is the actual levels of oxygen the cells
experienced in your hypoxic and normoxic experiments. The levels of oxygen in the air are not
normoxic as far as tissues are concerned. In fact they are hyperoxic as there are considerable
oxygen concentration gradients in the lungs and across capillaries. Tissue oxygen levels are
typically between 15 - 40 µM (equivalent to a gas mixture containing between ~ 1.5 – 4% oxygen
at 1 atmosphere of pressure). Hypoxic tissues contain levels 0 - 4 µM (equivalent to a gas mixture
containing between ~ 0 - 0.4% oxygen at 1 atmosphere of pressure).
Reply: We agree with this comment, and we discussed this difference of oxygen level between in
vivo and in vitro circumstances in Page 11.
“Since there are considerable oxygen concentration gradients in the lungs and across the
capillaries and tumor tissues, the oxygen levels in the tumor should be lower than that in the air,
which is defined as “normoxic condition” in this in vitro study. Therefore, under the in vivo micro-
environments, HIF-1α pathway may play a more important role than the NF-κB pathway. “

Final Product
Reviewer: 2
Comments to the Author
Dear editors,
thank you for letting me read this paper on FM19G11. The manuscript is well written and
important in its field. In general, I think the paper is suitable for publication.
Nevertheless I have some comments:
- The authors did not test toxicity of FM19G11. "Low toxicity" should therefore not be mentioned
in the title. Missing cytotoxicity at the effective dose does not necessarily warrant clinical safety.
Otherwise the authors have to present more data.
Reply: The title is modified as “FM19G11 inhibits O6-methylguanine DNA-methyltransferase
expression under both hypoxic and normoxic conditions”. “Low-toxicity” is removed from the
title.
- Furthermore FM19G11 is not a direct inhibitor of MGMT as implied by the title. Its action is
most probably explained by HIF modulation.
both informations in the title are misleading.
Reply: The title is modified as “FM19G11 inhibits O6-methylguanine DNA-methyltransferase
expression under both hypoxic and normoxic conditions”, so as to avoid this misleading.
The authors should comment if there is any conflict of interest since TMZ and FM19G11 are from
the same company.
Reply: Page 12. Although both TMZ and FM19G11 are from Sigma-Aldrich, the authors declared
that there is no conflict of interest.
Related Documents