AmericanNurseToday.com July 2017 American Nurse Today 25 A T ST . JOSEPH’S Hospital and Health Center in Syra- cuse, NY, we’re committed to providing a safe, com- fortable, caring environment for our patients. We be- lieve all patients deserve to be cared for in the most humane way possible to preserve their dignity and in- dividual rights. This means ensuring our patients’ physical safety, including preventing injuries from falls, during a hospital stay. Central to our fall prevention program is the hos- pital’s patient safety care bundle. We found that bundling (standardizing) fall prevention practices prevents more falls than nonbundling or variable ap- proaches. We also learned that involving all unit and house-wide staff in this approach inspires greater buy-in and participation and fosters best practices. Our bundling journey St. Joseph’s didn’t always use bundling to prevent falls. Our journey began in 2010 when I was asked to lead a task force to review and revise the hospital’s fall prevention program. After reviewing many articles in the nursing literature, our task force decided to take different concepts that proved effective and combine them into the bundled approach. All clinical and nonclinical staff were taught how to use the new bundle. Rapid-cycle piloting in select care areas was implemented. Following a process and outcome review and revision of the bundling ap- proach, full implementation followed throughout our facilities. St. Joseph’s bundled approach to fall pre- vention includes safety huddles, hourly rounding, use of the Morse scale, individual care plans, and post-fall debriefings. Safety huddle: To consistently identify patient safety needs for all shifts, each unit has a safety com- ponent as part of its shift-change huddle. The safety huddle must be documented on a form designed by the unit. Hourly rounding: Nurses round on patients hourly. The RN uses a consistent, caring conversation, which starts with an introduction, such as, “Mrs. Jones, I’m Marty, your nurse, and I’m here to check on you.” Un- less necessary, sleeping patients aren’t awakened. Rounds are documented in the electronic documenta- tion system. The RN admitting new patients explains that hourly rounding is done to anticipate their needs and ensure their safety. Morse scale: The Morse fall scale assessment tool, Fall prevention safety bundle: Collaboration leads to fewer falls By Marty Pond, MS, RN-BC–Gerontology NICHE Coordinator and Falls Chairperson, St. Joseph’s Hospital and Health Center, Syracuse, New York As told to Janet Boivin, BSN, RN A man in his late 80s was admitted to the medical-surgical unit after several falls at home, including one that re- sulted in a hip fracture. He had a uri- nary tract infection (UTI) and was con- fused and sleep deprived. His family reported that he’d fallen many times at home. Our challenge was to keep him safe while treating his UTI and giv- ing him the rest he needed to get well. The patient’s admitting nurse eval- uated him with a Morse scale of more than 85, so a magnet indicat- ing this designation was placed on his door and every shift was notified of his fall risk every day. In addition to the door magnet, our interven- tions included a bed alarm when the patient was in bed, a chair alarm, hip protectors to add extra protec- tion if he fell, and floor mats* on each side of the bed. As a result of our interventions, the patient got much-needed rest, his UTI resolved, his cognition im- proved, and he was able to return home. We gave the hip protectors to the family for use at home. *Manufactured by Posey Case study

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

AmericanNurseToday.com July 2017 American Nurse Today 25
AT ST. JOSEPH’S Hospital and Health Center in Syra-cuse, NY, we’re committed to providing a safe, com-fortable, caring environment for our patients. We be-lieve all patients deserve to be cared for in the mosthumane way possible to preserve their dignity and in-dividual rights. This means ensuring our patients’physical safety, including preventing injuries from falls,during a hospital stay.
Central to our fall prevention program is the hos-pital’s patient safety care bundle. We found thatbundling (standardizing) fall prevention practicesprevents more falls than nonbundling or variable ap-proaches. We also learned that involving all unit andhouse-wide staff in this approach inspires greaterbuy-in and participation and fosters best practices.
Our bundling journeySt. Joseph’s didn’t always use bundling to preventfalls. Our journey began in 2010 when I was asked tolead a task force to review and revise the hospital’sfall prevention program. After reviewing many articlesin the nursing literature, our task force decided totake different concepts that proved effective andcombine them into the bundled approach.
All clinical and nonclinical staff were taught how touse the new bundle. Rapid-cycle piloting in selectcare areas was implemented. Following a process andoutcome review and revision of the bundling ap-proach, full implementation followed throughout ourfacilities. St. Joseph’s bundled approach to fall pre-vention includes safety huddles, hourly rounding, useof the Morse scale, individual care plans, and post-falldebriefings.
Safety huddle: To consistently identify patientsafety needs for all shifts, each unit has a safety com-ponent as part of its shift-change huddle. The safetyhuddle must be documented on a form designed bythe unit.
Hourly rounding: Nurses round on patients hourly.The RN uses a consistent, caring conversation, whichstarts with an introduction, such as, “Mrs. Jones, I’mMarty, your nurse, and I’m here to check on you.” Un-less necessary, sleeping patients aren’t awakened.Rounds are documented in the electronic documenta-tion system. The RN admitting new patients explainsthat hourly rounding is done to anticipate their needsand ensure their safety.
Morse scale: The Morse fall scale assessment tool,
Fall prevention safety bundle: Collaboration leads to fewer falls
By Marty Pond, MS, RN-BC–GerontologyNICHE Coordinator and Falls Chairperson, St. Joseph’s Hospital and Health Center, Syracuse, New York
As told to Janet Boivin, BSN, RN
A man in his late 80s was admitted tothe medical-surgical unit after severalfalls at home, including one that re-sulted in a hip fracture. He had a uri-nary tract infection (UTI) and was con-fused and sleep deprived. His familyreported that he’d fallen many timesat home. Our challenge was to keephim safe while treating his UTI and giv-ing him the rest he needed to get well.
The patient’s admitting nurse eval-uated him with a Morse scale ofmore than 85, so a magnet indicat-ing this designation was placed onhis door and every shift was notifiedof his fall risk every day. In additionto the door magnet, our interven-tions included a bed alarm when thepatient was in bed, a chair alarm,hip protectors to add extra protec-
tion if he fell, and floor mats* oneach side of the bed.
As a result of our interventions,the patient got much-needed rest,his UTI resolved, his cognition im-proved, and he was able to returnhome. We gave the hip protectorsto the family for use at home.
*Manufactured by Posey
Case study

26 American Nurse Today Volume 12, Number 7 AmericanNurseToday.com
which is individualized for each patient, assesses forthe following measures:• history of falls• secondary diagnosis• ambulatory aid• I.V.s/normal saline lock• gait/transfer• mental status.
According to St. Joseph’s fall prevention protocol,the Morse scale is used upon admission of every in-patient 14 and older, once during every day shift,when a patient’s level of care changes, upon transfer,and after a fall.
Individualized care interventions: The followinginterventions are implemented based on individualpatient needs:• Falls that take place while the patient is hospital-
ized are documented on the plan of care under theMorse scale section. When physical therapy ormedication review is requested, it’s documented inthe plan of care under the safety and activity sec-tion and communicated during handoff.
• Nurses have the option to ask for a gerontology review, which includes consultation with an expertgerontology RN and a pharmacist, and a physicaltherapy screen.
• Door signs or door magnets alerting staff to thepatient’s risk of falls must be used when the pa-tient’s Morse scale score is ≥ 85 (considered highrisk), when staff believe the patient is at risk offalling despite a lower fall assessment score, andwhen patients have an epidural infusion untilthey’re able to ambulate independently.
• Bed exit and chair alarms* must be used for pa-tients who overestimate or forget their limitations
and for those with an impaired gait transfer (asdocumented in the Morse assessment). Patientswith bed exit alarms also must have a chair alarmwhen out of bed. Any patient with a bed exitalarm, chair alarm, or door magnet is not to be leftalone on the commode or in the bathroom.Post-fall defusing: Immediately after a fall, we hold
a debriefing with the staff involved with the patient’scare. At the debriefing, similar to the huddle concept,we review and discuss the event to help formulate acollaborative approach for immediate care, treatment,and review and prevention of potential future falls.
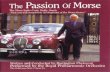
Practice implications Since our implementation of the bundled approach tofall prevention, we have seen a decrease in the num-ber of falls and a reduction in the severity of injurywhen falls do occur. (See Reduction in falls.) Perhapsmost important, though, is that an all-staff approachto quality care inspires greater buy-in and participa-tion, which fosters best-practice outcomes.
*Manufactured by Posey
Editor’s note: This is one in a series of recurring case studies describing success stories in preventing falls and injuriesfrom falls. The series is brought to you by Posey (http://www.posey.com). Watch for the next case study in the Sep-tember issue of American Nurse Today.
Reduction in annual fallsSt. Joseph’s Hospital and Health Center has reduced falls by 30.23%since implementing a fall reduction program in 2011.
500
400
300
200
100
0 2011 2012 2013 2014 2015 2016
420 388 336 326 310 293
30%decline
Dat
a fro
m N
atio
nal D
atab
ase
of N
ursi
ng Q
ualit
y In
dica
tors
®
Related Documents