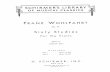
Epidemiology – Cohort studies I Epidemiology – Cohort studies I March 2010 March 2010 Jan Wohlfahrt Jan Wohlfahrt Afdeling for Epidemiologisk Forskning Afdeling for Epidemiologisk Forskning Statens Serum Institut Statens Serum Institut

Epidemiology – Cohort studies I March 2010 Jan Wohlfahrt Afdeling for Epidemiologisk Forskning Statens Serum Institut.
Dec 28, 2015
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Epidemiology – Cohort studies IEpidemiology – Cohort studies I
March 2010March 2010
Jan WohlfahrtJan WohlfahrtAfdeling for Epidemiologisk ForskningAfdeling for Epidemiologisk Forskning
Statens Serum InstitutStatens Serum Institut
EPIDEMIOLOGYEPIDEMIOLOGY
COHORT STUDIES ICOHORT STUDIES I
March 2009 (modified)March 2009 (modified)
Søren FriisSøren FriisInstitut for Epidemiologisk KræftforskningInstitut for Epidemiologisk Kræftforskning
Kræftens BekæmpelseKræftens Bekæmpelse
”While the individual man is an insoluble puzzle, in the
aggregate he becomes a mathematical certainty. You
can, for example, never foretell what any one man will
do, but you can say with precision what an average
number will be up to”
Arthur Conan Doyle
Sherlock Holmes: The Sign of four
Ideal study of a causal effectIdeal study of a causal effect
”The experience of exposed people is compared
with their experience when not exposed, while
everything else is held constant”
Kenneth Rothman, Modern Epidemiology, 1998
Assignment of exposure
Non-experimentalstudies
Randomised/intervention
trials
Sampling accordingto exposure status
Sampling according to outcome status
Cohort studies
Case-control studies
Yes No
no yes
Analytic epidemiological studies Analytic epidemiological studies
Experimental studies
Non-experimentalstudies
Random allocation
Community intervention
trials
Cohort studiesCohort studies
Classical definitionClassical definition
”The delineation of a group of persons who are distinguished in some specific way from the majority of the population and observation of them for long enough to allow any unusual morbidity or mortality to be recognised”
Richard Doll 1964
Cohort studiesCohort studies
Recent definitionRecent definition
Experiments Randomised clinical trials
two (or multiple)-arm, cross-over
Field trials intervention on single-person level
Community intervention trials intervention on community level
Non-experimental cohort studies
Past Present Future
Identify study subjects and assess exposure characteristics
Follow-up
Population at risk
Exposed
Non-exposed
Udfald
+
-+
-
Censored
Censored
Population at riskPopulation at risk
Individuals at risk of developing the outcome(s) of interest Basis for computation of measures of diseases frequency and effect
measures
Classified according to exposure characteristics At baseline During follow-up
Censoring at First outcome (typically) Death Migration Upper age limit, if age restriction Other criteria, e.g. exposure shift
CohortCohort
”Any designated group of individuals who are followed or traced over a period of time” Kenneth Rothman, Modern Epidemiology, 1998
Can be divided into closed and open populations
Closed and Open PopulationsClosed and Open Populations
Closed population
A population that adds no new members over time
Open/dynamic population
A population that may gain members over time or lose members who are still alive e.g. drug users within a specific observation period
Closed populationClosed population
limitationslimitations
Loss to follow-up (censoring)
Decreasing cohort size
Aging of cohort members
Depletion of susceptibles
Selection of the exposed populationSelection of the exposed population
General population Diet, Cancer & Health cohort, Danish Cancer Society
Individuals aged 50 to 64 years, follow-up from 1994 (n 57,000)
Occupational exposure groups Nurses Health Study, USA
Nurses aged 30 to 55 years, follow-up from 1976 (n 120,000)
Exposure ”Special exposure groups”
Ex.: Workers at the Thule base, Epileptics at Dianalund, individuals exposed to thorotrast
Drug users
Registers General Practice Research Database, UK Danish health and administrative registers
Selection of the comparison groupSelection of the comparison group
Ideally identical to the exposed group with respect to all other factors that may be related to the disease except the outcome(s) under study
”Internal” comparison general population/large occupational cohort frequent exposure
”External” comparison
General population (rates) Standardised incidence rate ratio (SIR) Standardised mortality rate ratio (SMR)
Data sourcesData sources
Exposure Existing data
registers medical records bio-banks
Questionnaires interview self-administered
Ad hoc measurements clinical parametes
biological samples
Outcome Registers
Clinical examination
Information from study subjects interview
questionnaire
Information from next-of-kin
Mortality data
Cohort studiesCohort studies
Can examine multiple effects of a
single exposure rare exposures
Exposures with certainty precede outcomes (if prospective)
Allows direct measurement of incidence (IR, IP) of outcomes
Can elucidate temporal relationship between exposure and outcome
Allow study subjects to contribute person-time to multiple exposure categories
Biological material can be collected prior to outcome
If prospective, minimizes bias in the ascertainment of exposure
AdvantagesAdvantages
Cohort studiesCohort studies
Is inefficient for the evaluation of rare diseases
If prospective, can be very expensive and time consuming
If retrospective, requires the availability of adequate records for both exposure and outcome
If prospective, cannot provide quick answers
If retrospective, precise classification of exposure and outcome may be difficult
Validity of the results can be seriously affected by losses to follow-up
DisadvantagesDisadvantages
Historical cohort studies
Comparison with general population (rates)
Nested case-control studies
Register studies
Cohort studiesCohort studies
Methods for reduction of costs and time Methods for reduction of costs and time
Register studies in DKRegister studies in DK
Frank L. Science 2000;287: 2398-9Frank L. Science 2000;287: 2398-9
Register studies in DKRegister studies in DK
CPR Register
National Death Files
National Hospital Register
Birth Register
Prescription Databases
IDA Register(socioeconomic
variables)
Cancer Registry
Register studiesRegister studies
Registers are highly valuable data sources, BUT
Difficulties in interpretation due to incomplete data on competing risk factors
Life-style factors, socioeconomic factors, comorbidity, medical treatment
Other potential biases
Misclassification, non-compliance, etc.
Measures of disease frequencyMeasures of disease frequency
Definitions
What is the case? What is the study period?What is the population at risk?
Measures of disease frequency, summaryMeasures of disease frequency, summary
Incidence proportion (IP) Proportion of population that develops the outcome of interest during a
specified time Can be measured only in closed populations ”Average risk” for a population
Incidence rate (IR) Number of new cases of the outcome of interest divided by the amount of
person-time in the base population Can be measured in both open and closed populations Most often restricted to include a maximum of one event per person
Prevalence proportion (PP) Proportion of population that has the outcome of interest at given instant
IP+ = a/a+b IP- = c/c+d
RR = IP+/IP-
Attributable risk (AR) = IP+ - IP-
Attributable proportion (AP) = AR/IP+ = (RR-1)/RR
Effect measures in cohort studiesEffect measures in cohort studies
Incidence proportion Incidence proportion
ConditionsConditions
All persons should be followed-up from start of study (t0) until end of study with respect to the outcome(s) of interest
Problems: Open/dynamic population (t0?)
Competing risks of death Censoring
Is usually not directly observable, solution:
Computation of incidence rates
Relation between rate (IR) og risk (IP)
IP = 1 - exp(-IR x t) (IR constant)
IP = 1 - exp(- IRí x tí ) (IR variable)
IR small and/or short t:
IP IR x t
Person-time in study
cases
cases
Non-exposed
Exposed
Problem: Exposure status changes over time (episodical, sporadical)
Solution: Allow persons to contribute person-time to multiple exposure categories
Time dimensionTime dimension
Calendar time
1970
19901975 1980 1985 1995
Age
30
35
40
45
50
55
Y
X
Non-X
Contribution f rom the two study subjects
Exp. to drug X Non-exp. to drug X
Age PY Disease Y PY Disease Y
30-34 y 0 0 5 0
35-39 y 5 0 5 0
40-44 y 10 0 0 0
45-49 y 8 1 0 0
50-54 y 0 0 5 0
”Crude” 23 1 15 0
30-year-old man is enrolled in a cohort study of drug X in relation to disease Y in 1970 and followed free of Y through 1995
35-year-old man is enrolled in 1970 and followed until occurrence of Y in 1983
Person-time in study
cases
cases
Non-exposed
Exposed
Incidence rate = cases / person-time
Incidens Rate Ratio (IRR) = IR+ / IR-
A
PYC
PY
Cases Person-time
Exp
osu
re
Yes
No
A = Exposed cases
C = Non-exposed cases
Effect measures in cohort studiesEffect measures in cohort studies
IR+ = a/PY+
IR- = c/PY-
Incidence rate ratio (IRR) = IR+/IR-
Incidence rate difference = IRD (≈AR) = IR+ - IR-
AP = IRD/IR+ = (IR+-IR-)/IR+ = (IRR-1)/IRR
Effect measures in cohort studiesEffect measures in cohort studies
”Relative risk” vs. incidence rate ratio
Given IP IR x t (IR small)
”Relative risk” is equivalent with the ratio of two incidence
rates when the disease is rare
2
1
2
1
2
1
IRIR
tIRtIR
IPIP
Indirect Standardisation
Do more outcomes occur in the studied population than would be expected if the risk prevailing was the same as in the general population?
Estimation of expected number of outcomes Number of person-years at risk x incidence rate
PYage,period,sex x incidenceage,period,sex
Observed number/expected number ≈ RR
Standardised incidence ratio (SIR)
Effect measures in cohort studiesEffect measures in cohort studies
Calendar time
SIR = Observed number of outcomes/ expected number of outcomes
= Obs/IRpop x PYexp
= (Obs/PYexp) / IRpop
= IRexp / IRpop
≈ IRexp / IR0
= IRR (RR)
Relevant exposure?Relevant exposure?
Ex Ex Ex
ExExEx
Ex Ex Ex
1-3 days?
10-15 days?
100-150 days?
Ex Ex Ex years?
NSAID cohort studyNSAID cohort study
Population: Saskatchewan – province in Canada with appr. 1.1 mill. inhabitants
A study of the association between use of NSAIDs and risk of gastrointestinal (GI) bleeding included all 228,392 individuals who had redeemed one og more prescriptions for NSAIDs. The study subjects were followed during the period 1982-1986 for hospitalization due to upper GI bleeding
From the paper: .. Entered our cohort upon the first receipt of a prescription for diclofenac, indomethacin, naproxen, piroxicam or sulindac. Person-time contributed by this person continued until the earliest of: 1) hospitalization due to UGB, 2) death, 3) departure from Saskatchewan or 4) end of study
Note!: No control group of ’non-exposed’
Garcia Rodriguez et al. NSAIDs and GI-hospitalizations in Saskatchewan: A cohort study. Epidemiology 1992;3:337-42
Current user Recent past user Old past user Non-user
Day 0 30 60 150
Day 0 30 30 30 30 60
The person time of the study subjects was categorized according to time since last prescription
Current user Current user Current user Recent past userCurrent user
# 1
# 2
1.Rx 4.Rx3.Rx2.Rx
1. Rx
Current user Recent past user Old past user Nonuser
Person 1 30 30 90 >90 Person 2 120 30 - -
Modified from Garcia Rodriguez et al. NSAIDS and GI-hospitalizations in Saskatchewan: A cohort study. Epidemiology 1992;3:337-42
I ncidence rate ratios of GI -hospitalisations of NSAI D users
Current users Recent past users Old past users (0-30 days) (30-60 days) (60-150 days)
Diclofenac 3.9 2.2 1.3
I ndomethacin 4.0 1.7 1.4
Naproxen 3.8 2.3 1.4
Nonusers
1.0
Absolute vs. relative disease measuresAbsolute vs. relative disease measures
Avoid confusing measures of frequency with
measures of association (effect measures)
Ex:
A RR=10 is described as a high risk, or a population for whom RR=10 is said to be at higher risk than a population in which RR=5
A RR=10 may be described as a high relative risk
Risk of deep vein thrombosis (DVT)Risk of deep vein thrombosis (DVT)Third vs. second generation oral contraceptives Third vs. second generation oral contraceptives
RR 1.7 (1.4-1.7)
AR 1.5 per 10 000 person-years
Mortality of DVT 3%
Kemmeren et al. BMJ 2001; 323: 131-4
Vioxx (rofecoxib) and cardiovascular diseaseVioxx (rofecoxib) and cardiovascular disease
APPROVe trialAPPROVe trial
2,586 patients randomised to rofecoxib (Vioxx) (25 mg daily; n=1287) or placebo (n=1299) during a 3-year study period
1.50 CVE per 100 py (46 events; 3,059 py) vs. 0.78 CVE per 100 py (26 events; 3,327 py)
RR = 1.92 (1.19-3.11)
AR 72 pr. 10 000 py
Bresalier et al. N Engl J Med 2005; 352: 1092-1102
Attributable proportionsAttributable proportions
What proportion of the disease among the exposed is attributable to the exposure (APexp)?
APexp = IR+-IR0 / IR+ = AR / IR+ = (RR-1)/RR
What proportion of the disease in the total study population of exposed and non-exposed individuals is attributable to the exposure (APpop)?
APpop = IRpop-IR0 / IRpop
= AR x pe / IRpop (pe = exp. prevalence in population)
= APexp x pc (pc = exp. prevalence among cases)
= [(RR-1) x pe] / [(RR-1) x pe - 1]
Attributable proportionAttributable proportionIncidence rates of head and neck cancer per 100,000 py Incidence rates of head and neck cancer per 100,000 py
Among drinking smokers, what proportion of head and neck cancer is caused by smoking?
Among drinking smokers, what proportion of head and neck cancer is caused by drinking?
”Non-smoker” ”Smoker”
”Non-drinker” 1 4
”Drinker” 3 12
Attributable proportionAttributable proportionIncidence rates of head and neck cancer per 100,000 py Incidence rates of head and neck cancer per 100,000 py
Among drinking smokers, what proportion of HNC is caused by smoking?
AP = IRD/IR+S+A = (IR+S+A-IR-S+A)/IR+S+A = (12-3)/12 = 75%
”Non-smoker” ”Smoker”
”Non-drinker” 1 4
”Drinker” 3 12
Attributable proportionAttributable proportionIncidence rates of head and neck cancer per 100,000 py Incidence rates of head and neck cancer per 100,000 py
Among drinking smokers, what proportion of HNC is caused by drinking?
AP = IRD/IR+S+A = (IR+S+A-IR+S-A)/IR+S+A = (12-4)/12 ≈ 67%
”Non-smoker” ”Smoker”
”Non-drinker” 1 4
”Drinker” 3 12
Study population N GI bleeding
NSAID users 20,000 100
Non-users of NSAID 100,000 100
In total 120,000 200
A hypothetical population consists of 20.000 users of non-steroid A hypothetical population consists of 20.000 users of non-steroid anti-inflammatory drugs (NSAIDs) og 100.000 non-users of NSAID. anti-inflammatory drugs (NSAIDs) og 100.000 non-users of NSAID. The study subjects are followed for one year for the occurrence of The study subjects are followed for one year for the occurrence of upper gastrointestinal (GI) bleedingupper gastrointestinal (GI) bleeding
Please calculate the following measures of frequency and risk:
1. Incidence rate (IR) for GI bleeding in each exposure group
2. Incidence rate ratio (IRR) for the association between NSAID and upper GI bleeding
3. Incidence rate difference (IRD≈AR) between NSAID users and non-users
4. Attributable proportion (APexp) among users of NSAIDs
5. Attributable proportion (APpop) in the total population
(Censoring in the risk population should be ignored)
Study population N GI bleeding
NSAID users 20,000 100
Non-users of NSAID 100,000 100
In total 120,000 200
IRNSAID = 100/20000 = 0.005 = 5 per 1000 person-years
IRo = 100/100000 = 0.001 = 1 per 1000 person-years
AR = IRD = IRNSAID–IRo = 5-1 = 4 per 1000 person-years
IRR = IRNSAID/IRo = 5/1 = 5
IRpop = 200/120000 = 0.00167 = 1.67 per 1000 person-years
APexp = AR/IRNSAID = 4 per 1000/5 per 1000 = 0.80 or 80%
ARpop = IRpop–IRo = 1.67 – 1 = 0.67 per 1000 person-years
APpop = ARpop /IRpop = 0.67/1.67 0.40 or 40%
Related Documents