Endocrinology for Finals Dr Niru Goenka Consultant Physician in Diabetes/Endocrinology Countess of Chester NHS Foundation Trust

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Endocrinology for Finals
Dr Niru GoenkaConsultant Physician in Diabetes/Endocrinology
Countess of Chester NHS Foundation Trust

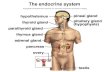
• Diabetes
• Thyroid
• Adrenal
• Pituitary
• Reproductive
• Metabolic eg. sodium, calcium etc..
The breadth of endocrinology

• Clinics and cases
• Interpretation of dynamic endocrine tests.
• www.endotext.com – completely free, well written, illustrated and fully referenced online endocrine textbook written by reputable authors.
Learning Endocrinology

1) The basic rule of any endocrine test is
“If you are trying to prove something is elevated then try and suppress it and if you are trying to prove something is deficient then try and stimulate it.”
2) Biochemistry & Dynamic tests more important than imaging (+ also usually done before imaging)
Golden Rules

• 28 year old woman• Palpitations and weight loss• TSH <0.05• Free T4 35
Edna

• Make a diagnosis• Treatment depends on underlying
condition• Graves – offer medication (50%
relapse)• Others will need definitive Rx
Thyrotoxicosis

• 18 year old woman• TATT, fatigue, lethargy, weight gain• TSH 7.5• Free T4 17
Kelly

• 18 year old woman• TATT, fatigue, lethargy, weight gain• TSH 8.1• Free T4 10
Kelly

• 18 year old woman• TATT, fatigue, lethargy, weight gain• TSH 40• Free T4 3
Kelly

• 19 year old woman• Now on 125mcg T4• Still TATT, fatigue, lethargy, weight gain• TSH 17• Free T4 14
Kelly

• 19 year old woman• on 125mcg T4 says she is taking regularly• Still TATT, fatigue, lethargy, weight gain• TSH 20• Free T4 9
Kelly

• 19 year old woman• on 250mcg T4 says she is taking regularly• Still TATT, fatigue, lethargy, weight gain• TSH 50• Free T4 2
Kelly

• 19 year old woman• Now on 150mcg T4 – taking regularly• Still TATT, fatigue, lethargy, weight gain• TSH 3.2• Free T4 19
Kelly

• Subclinical – 6-12 monthly TFTs and add small dose T4 if free T4 low/low normal and positive antibodies.
• Thyroxine may not improve all of symptoms.
• Remember non-compliance
Hypothyroidism

• 70 year old man• Fatigue and lethargy• TSH 0.03• Free T4 7
Gino

• Don’t add T4 until steroid axis sorted out – you can precipitate crisis
• Need TRH test to diagnose• Can only monitor using Free T4 as
TSH will always be low
Secondary Hypothyroidism

• 25 year old woman• fatigue, nausea, amenorrhoea and
weight gain.• Free T4 40• TSH 6.0
Jo

Thyroid hormone resistance
Thyroid hormone resistance
Inadequate response of the pituitary &/or peripheral tissues to circulating free thyroid hormones
First described 1967
Autosomal dominant, occasional sporadic cases
Mutations of exons 9 & 10 (chromosome 3) which encode the T3-binding domain of TRB gene
TSH secreting adenoma can also cause this clinical picture but would be associated with a pituitary macroadenoma

• 35 year old pharmacist• fever, sore throat, and dysphagia• Pyrexial and in AF• TSH 0.02 • T4 32
Andy

• Inflammatory thyroiditis – likely viral aetiology
• Can be difficult to differentiate from “standard” thyrotoxicosis
• Completely absent uptake on thyroid uptake scan
• Can use NSAIDs or steroids. Β-blockers for symptoms.
De Quervains Thyroiditis


Graves Opthalmopathy
May occur in the absence of clinical thyroid disease
Progress is often independent of that of thyroid disease.
Treatment Supportive (keeping the cornea moist)SteroidsDecompression if sight is threatenedAnti thyroid drugs NOT helpful-except to treat
associated thyroid disease (RAI worsens it).
Other Investigations
CT/MR orbits allows the optic nerve to be seen

• FDH and heterophile antibodies• Thyroid hormone resistance• TSH-oma• secondary hypothyroidism• T3 toxicosis• Poor compliance• Sick euthyroid syndrome• Amiodarone• Pregnancy
Weird TFTs


Follow up question
What is the cause of his Cushings syndrome?
A Pituitary Dependent Cushing’s DiseaseB Cushing’s Syndrome secondary to adrenal adenomaC Ectopic ACTH SyndromeD Long term prednisolone for asthma




Primary hyperaldosteronism
• Most common cause of mineralocorticoid hypertension
• Most cases due to solitary adenoma (0.5-2cm)• Third of cases due to bilateral adrenal
hyperplasia• Most patients asymptomatic: may have fatigue,
weakness, thirst, polyuria, nocturia• Imaging with MR or CT• Adrenal vein sampling - to confirm or refute
unilateral disease and help predict success of unilateral adrenalectomy

Conn’s syndrome
• Needs to be considered in anyone particularly with difficult to control hypertension and hypokalaemia. Absence of hypokalaemia does not exclude diagnosis (30% normal K)
• An aldosterone/renin concentration is the screening investigation of choice
• Cutoff is >2000 (aldo in pmol/l, renin in pmol/ml/h). Most normals will have a ratio<800
• Diagnosis using postural studies (lying down – vol expansion)



Addison’s disease
• The diagnosis is Addisons disease.• Pigmentation of palmar creases and generalised
pigmentation of skin.• Most common cause of primary adrenal failure is
autoimmune adrenalitis. Other causes include TB, infiltration by tumour/amyloid, adrenal haemorrhage/infarction due to septicaemia, thromboembolic disease or coagulopathy

• Typical manifestations in Addison’s disease:– Anorexia, nausea, vomiting, weight loss,
hyperpigmentation, weakness and lassitude, low blood pressure
• Diagnosis:– Clues: hyponatraemia and hyperkalaemia, raised
urea– Low morning cortisol and raised ACTH (morning
cortisol > 400 nmol/l makes dx of adrenal insufficiency unlikely
– Diagnostic test: short synacthen test


21-hydroxylase

21-hydroxylase
11β-hydroxylase


P65GAL4 on NRE



A 45 yr old man presents with tiredness, loss of libido, loss of muscular strength, and reduced body hair and beard growth. Examination shows fine wrinkles over his face, loss of pubic hair, and bilateral testes volumes of 9 ml.
He has gynaecomastia. Visual fields are full to confrontation.
His prolactin is measured at 700 U/L (normal range 100-350)

What is the most likely diagnosis?•A Hypothyroidism•B Craniopharyngioma•C Depression•D Prolactinoma•E Non functioning pituitary adenoma
The most useful investigation is:•A Gonadotrophins and Testosterone•B Thyroid function tests•C Sex hormone binding globulin•D Testicular USS•E Pituitary MR scan

HyperprolactinaemiaPhysiological: pregnancy,
lactation, stressDrugs:
Anti-emeticsPhenothiazinesTCAs
Primary hypothyroidismPituitary tumours:
ProlactinomaGrowth hormone secreting (raised PRL in 30%)Non-functioning tumours (stalk “disconnection”)
Polycystic ovarian syndrome
Liver/renal failure“Nipple” stimulationUncommon hypothalamic/
stalk lesionsSarcoidosisHypothalamic tumoursLangerhans cell histiocytosis

Question A 15 year old girl presents with oligomenorrhoea, hirsutism, acne and weight gain (current BMI 32). She has a family history of type 2 DM.On examination she has acanthosis nigricans in both axillae and on the neck. A Glucose tolerance test shows a 2 hour plasma glucose of 9.8mmol/l.
a) What is the likely diagnosis?
A Cushing’s syndromeB Polycystic ovary syndromeC HyperprolactinaemiaD HypothyroidismE Type II diabetes
b) What treatment would you recommend?
A Reducing dietB ExerciseC InsulinD MetyraponeE KetoconazoleF DianetteG MarvelonH DexamethasoneI RoaccutaneJ DepoProvera


Answer to Question •B Polycystic Ovary syndrome
b) F Reducing diet G Exercise
Insulin Resistance Hyperandrogenism
Acanthosis Nigricans
Diagnosis - clinical featuresandrogen levelsPelvic U/S
Treatment diet and exercisemetformin, newer insulin sensitisers
oestrogens will make weight loss more difficult
High risk of glucose intolerance, dyslipidaemia and type II diabetes.
There is often a family history of type II diabetes.

PCOSDiagnosis• Must have 2 of the following 3
manifestations:1. Irregular or absent ovulation
2. Clinical and/or biochemical signs of hyperandrogenism3. Enlarged ovaries containing at least 12 follicles each
• Other aetiologies should be excluded e.g. CAH, androgen-secreting tumours, Cushings

Hairy women(aka hisutism)
presence of xs hair
not a diagnosis
look for virilizationeg. frontal balding
deep voice muscles
clitoromegaly

Causes of Hirsutism
Ovarian Polycystic Ovary Syndrome >95%
Androgen -secreting tumours <1%
Adrenal Congenital Adrenal Hyperplasia <1%
Cushing’ s Syndrome <1%
Androgen secreting tumours <1%
Acromegaly <1%

Causes of Hirsutism
Ovarian Polycystic Ovary Syndrome >95%
Androgen -secreting tumours <1%
Adrenal Congenital Adrenal Hyperplasia <1%
Cushing’ s Syndrome <1%
Androgen secreting tumours <1%
Acromegaly <1%

Androgen production in women
PITUITARY
ACTH LH
ADRENALS OVARIES
Androstenedione/DHEA Testosterone DHT

A 54 year old man presented to A&E with collapse. A subarachnoid haemorrhage was diagnosed by CT, and he underwent clipping of a berry aneurysm.
On post op day 5 he was drowsy.
His biochemistry showed:Sodium 121Potassium 3.5Urea 2.3Spot urinary sodium 48Urine osmolarity 325 (normal range 350-1000)Plasma osmolarity 236 (normal range 278-305)
QuestionThe most likely diagnosis is•A Cerebral salt wasting•B SIADH•C Cranial diabetes insipidus•D Hypopituitarism leading to steroid deficiency•E Excess IV fluid administration

SIADHClinical featuresWater retention and
hyponatraemiaConfusion, nausea, irritability, fits
and comaMild sx when Na <125, severe
when <115mmol/lNo oedema
Diagnosis:Decreased plasma osmolality
(<270mosm/kg) with inappropriately high urine osmolality
Na excretion > 30mmol/lAbsence of hypokalaemia/low BPNormal renal/adrenal/thyroid
function
Treatment:Fluid restrictDemeclocycline
Causes:TumoursPulmonary diseaseCNS diseaseDrugs
Main differential diagnosis:
Dilutional hyponatraemia due to excess glucose/water

A 62 year old man was admitted with an extradural haematoma. He had surgical decompression, and on day 4 post op was noted to have abnormal biochemistry results.
On examination he was noted to be drowsy and was clinically dehydrated.
Sodium 121Potassium 3.4Urea 8.5Creatinine 145Spot urinary sodium 51 Urine osmolarity 270 (normal range 350-1000)Plasma osmolarity 246 (normal range 278-305)
QuestionThe most likely diagnosis is:•A SIADH•B Excess IV fluid administration•C Cerebral salt wasting•D Addisonian crisis•E Diabetes insipidus

The following results are picked up when a 35 year old woman attends for an insurance medical. She tells the doctor that her sister has also been found to have an elevated calcium.
Corrected calcium 2.8 mmol/lPhosphate 1.0 mmol/l (normal range 0.8 – 1.45)Urinary calcium excretion 2.8 mmol/24 hours (normal range 2.5 – 7.5)PTH 3 pmol/ml (normal range 0.9 - -5.4)
Question
The most likely diagnosis is•A Milk-alkali syndrome•B Malignancy•C Serum sample left standing too long•D Primary hyperparathyroidism•E Familial hypocalciuric hypercalcaemia

Primary Hyperparathyroidism
• The diagnosis is primary hyperparathyroidism (PHPT). Patients have raised serum calcium with normal or raised PTH.
• Predominantly a disease of postmenopausal women• Due to single adenoma in 85% of cases• Majority of patients asymptomatic. May have features of
hypercalcaemia or end organ damage-at baseline arrange 24 h urine calcium excretion, renal USS, DEXA scan
• Only definitive treatment option is surgery

Self-induced illness
Anorexia – hormonal changes as discussed, occasionally hyponatraemia caused by excess water drinking.
Excess exercise – gonadotrophin hormonal changes similar to anorexia. Also bradycardia.
Self-induced vomiting – hypokalaemic hypochloraemic metabolic alkalosis (similar pictures with laxative abuse and diuretic abuse).
Remember illicit drugs as a cause.

• Diabetes
• Thyroid
• Adrenal
• Pituitary
• Reproductive
• Metabolic eg. sodium, calcium etc..
The breadth of endocrinology

A 37-year-old woman presents with a three year history of oligomenorrhoea and more recently amenorrhoea. She underwent a normal menarche, and had a successful pregnancy aged 26 years. She smokes 20 cigarettes a day.
Over the last year she had gained one stone in weight, however, she felt this was related to giving up running because of pain in her leg and in hip. On examination she was noted to have excessive facial and body hair. BP 160/100 mmHg. The recent death of husband has led her being treated for clinical depression

Sodium 144 Potassium 3.5 Urea 6.5 Creatinine 78
LH 2 U/LFSH 1 U/LOestradiol 120 pmol/LTestosterone 3.9 nmol/L (normal range 0.5-3)
0900 ACTH 70 ng/L (normal range <10–80 ng/L)
Overnight (1 mg) dexamethasone suppression test0900 cortisol 150 nmol/l
High dose dexamethasone suppression test (2 mg dexamethasone 6 hourly for 48 hours)0900 day 0 cortisol 650 nmol /l0900 day 2 cortisol 40 nmol/l
MRI scan pituitary fossa NAD

QuestionWhat is the most likely diagnosis?•A Pituitary dependent Cushing's disease•B Pseudo Cushing's disease•C Polycystic ovarian syndrome•D Cortisol producing adrenal adenoma•E Ectopic ACTH secretion
QuestionSuggest a diagnostic investigation•A CT scan of the adrenals•B Transvaginal ultrasound scan•C Inferior petrosal sinus sampling•D Spiral CT of thorax•E Metyrapone test
QuestionWhat is the most likely cause of her hip and back pain?•A Metastatic lesions in lumbar spine•B Slipped femoral epiphysis•C Osteoporosis of spine•D Metastatic deposits in hip•E Crush fractures of the lumbar vertebrae
Question 21What medical therapy could be useful?•A Metyrapone •B Fluconazole•C Dianette•D Spironolactone•E Metformin

A 40 year old woman presents with malaise and weigh loss. She has not had a period for 5 years
Investigations revealed:Hb 12.1 g/dlWCC 5.7 x 109/L Plts 167 x 109/L Na 118 mmol/lK 4.0 mmol/lUrea 3.4 mmol/lHCO3 20 mmol/l
Question 36What is the most likely underlying diagnosis?� A hyperthyroidism� B hyperprolactinaemia� C Addison’s Disease� D panhypopituitarism� E syndrome of inappropriate ADH secretion

A 47 year old lady attends her GP’s surgery for HRT. Her periods had stopped 4 years ago. She had noticed that over the past few years her hands had increased in size. She was currently on no medication.
Physical examination revealed coarsened features, spade like hands and the presence of a minimally enlarged goitre. Her blood pressure was 150/85 mmHg.
Further Investigations revealed FBC, U&Es, calcium, LFTs, Glucose were normal.LH, FSH – normal. Low oestradiol, normal progesteroneTFTs – normalProlactin - normal

Oral Glucose Tolerance Test
Time Glucose GH0 5.7 6030 8.1 7060 10.2 80120 6.6 88
Insulin stress test
Time Glucose Cortisol0 5.5 40030 1.7 850

QuestionComment on the glucose tolerance test with regard to the glucose response� A normal response� B diagnostic of diabetes� C diagnostic of impaired glucose tolerance� D diagnostic of an insulinoma� E inconclusive
QuestionComment on the glucose tolerance test with regard to the growth hormone response� A normal result� B compatible with a diagnosis of acromegaly� C diagnostic of growth hormone deficiency� D abnormal due to underlying physical illness� E inconclusive
QuestionComment on the insulin stress test with regard to the glucose response� A demonstrates insulin resistance� B insufficiently low glucose level� C inconclusive� D adequate level of hypoglycaemia� E compatible with a diagnosis of ectopic insulin secretion

Question 31Comment on the insulin stress test with regard to the cortisol response� A demonstrates adrenal insufficiency� B normal� C demonstrates underlying Cushing’s syndrome� D suggestive of panhypopituitarism� E suggestive of ectopic ACTH production
Question 33What is the most likely cause for her amenorrhoea?� A underlying malignancy� B hyperprolactinaemia� C post menopausal� D pituitary failure� E weight loss secondary to underlying malignancy� F ovarian failure� G Cushing’s syndrome

Thank you
Related Documents