Electrocardiogram (ECG) A 90 year old female is brought to the emergency room in pulseless arrest. You immediately initiate CPR and intubate the patient. When the patient is placed on the monitor, you hold compressions and obtain the following rhythm strip. The patient still has no pulse. The rhythm strip below shows which of the following: 1) Atrial fibrillation 2) Ventricular Fibrillation 3) Torsade de pointes 4) Sinus Tachycardia 5) None of the above Explanation The correct answer is choice C. Torsades de pointes is a type of ventricular tachycardia characterized by a crescendo-decrescendo morphology of QRS complexes. It quickly degenerates to ventricular fibrillation and should be treated immediately. Treatment may include CPR, IV magnesium, and defibrillation. Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Electrocardiogram (ECG) A 90 year old female is brought to the emergency room in pulseless arrest. You immediately initiate CPR and intubate the patient. When
the patient is placed on the monitor, you hold compressions and obtain the following rhythm strip. The patient still has no pulse.
The rhythm strip below shows which of the following:
1) Atrial fibrillation 2) Ventricular Fibrillation 3) Torsade de pointes 4) Sinus Tachycardia 5) None of the above
Explanation
The correct answer is choice C.
Torsades de pointes is a type of ventricular tachycardia characterized by a crescendo-decrescendo morphology of QRS complexes. It quickly degenerates to ventricular fibrillation and should be treated immediately. Treatment may include CPR, IV magnesium, and defibrillation.
Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.

Ventricular fibrillation (choice B) is a pulseless rhythm characterized by irregular and disorganized activity on the rhythm strip.
Sinus tachcyardia (choice D) is a regular, rapid, narrow complex tachycardia.
A 53 year old diabetic female presents to the emergency department complaining of several hours of dyspnea. She has a past medical
history of hypertension and high cholesterol. You order a chest X-ray and an ECG.
The electrocardiogram below shows which of the following:

1) Type II heart block 2) Complete heart block 3) Anterior Myocardial Infarction 4) Inferior myocardial infarction 5) None of the above
Explanation
The correct answer is choice D.

This ECG demonstrates ST elevation in inferior leads (III and AVF) with reciprocal changes (ST depression) in leads I and AVL. An ST elevation myocardial infarction is an indication for emergency reperfusion therapy, either with a thrombolytic like tPA or angioplasty.
A 2nd degree, type II heart block (choice A) is characterized by a prolonged, fixed PR interval with intermittent dropped beats. These can often progress to a complete heart block.
A complete heart block (choice B) is also known as AV dissociation, and is characterized by the atria and ventricles each beating on their own intrinsic, uncoordinated rhythms.
An anterior MI (choice C) will demonstrate ischemic changes in anterior prechordial leads (V1-3, not shown in this ECG).
A 58 year old male with a past medical history of hypertension presents to your office for an annual physical. You order a screening ECG
as part of his visit and obtain the following.
The electrocardiogram shows which of the following findings:
1) Atrial fibrillation
2) Left ventricular hypertrophy (LVH)
3) Right Ventricular hypertrophy (RVH)
4) Ventricular tachycardia
5) Acute pericarditis

Explanation

The correct answer is choice B.
Left ventricular hypertrophy is a common finding in patients with long histories of hypertension, caused by cardiac muscle against a high afterload. ECG findings include left axis deviation and R or S waves greater than 20 mm in any limb leads among other diagnostic criteria.
Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.
Right ventricular hypertrophy (choice C) will cause right axis deviation.
Ventricular tachycardia (choice D) is an unstable tachy arrhythmia characterized by wide complex, ventricular originating beats.
Acute pericarditis (choice E) is an inflammatory condition of the pericardium causing PR depression and diffuse ST elevation.
A 50 year old male presents to your cardiology office for an evaluation. He was sent by his primary doctor for ECG changes noted over the past one year. You order a repeat ECG in your office. The electrocardiogram below shows which of the following:
1) Left Bundle Branch Block 2) Right Bundle Branch Block 3) Left Anterior Fascicular Block 4) Right Bundle Branch Block & Left Anterior Fascicular Block 5) Right Bundle Branch Block & Left Posterior Fascicular Block

The correct answer is choice C. A left anterior fascicular block is characterized by a left axis deviation, Q-R in I and AVL, and R-S in inferior leads (II, III, and AVF). The QRS duration is usually normal.

A left bundle branch block (choice A) is characterized by a wide complex, Q-S morphology in lead V1. A right bundle branch block (choice B) is characterized by a R-S-R-prime morphology in V1 and a slurred upstroke of the S wave in V6. A left posterior fascicular block (choice E) is characterized by an extreme right axis deviation. A 75 year old gentleman is admitted via ambulance to the emergency department. He gives a 4 hour history of vague upper abdominal discomfort. There is no radiation. He also complains of feeling dizzy. Relevant past medical history includes: an abdominal aortic aneurysm repair/stenting performed 3 months previously via percutaneous technique. He tells you he was admitted 2 weeks ago for 2 days of observation as follow up ultrasound scan had revealed a small leak at the site of repair. He has never been treated for ischaemic heart disease. On examination he is fully conscious and alert. Heart rate is 60 bpm regular and BP is 90/68. Heart sounds one and two are present and normal in character. There are no additional heart sounds or murmurs. Auscultation of the chest is clear. His left femoral pulse is very difficult to palpate. You perform an ECG. The electrocardiogram below shows which of the following:

1) Acute Anteroseptal Myocardial Infarction 2) Complete heart block 3) Acute pericarditis 4) Infero-posterior myocardial infarction 5) Acute Inferior myocardial infarction
The correct answer is choice D. Inferior-posterior myocardial infarction is the correct answer. This is a typical case of inferior infarction associated with posterior wall infarction. We can see on the EKG that there is ST segment elevation in leads II, III, and aVF. Because a 12-lead EKG looks primarily at the front of the heart, no leads show an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, a secondary R wave (R) in V1 or V2, and wide slurred S waves in leads I, V5, and V6. ST segment depression and T wave inversion in the right precordial leads are seen in this trace ECG. Acute Anteroseptal Myocardial Infarction (choice A) is not the correct answer. ST elevation and tall peaked T waves are not seen in the chest leads V1 to V4 and no q waves have appeared in this trace ECG. Complete heart block (choice B) is not the correct answer. In third degree block, there is complete failure of conduction between the atria and ventricles, with complete independence of atrial and ventricular contractions. The P waves bear no relation to the QRS complexes and usually proceed at a faster rate. In this trace, we can recognize the P wave followed by QRS complex. Acute pericarditis (choice C) is not the correct answer as the history and the age of patient is not suggestive for acute pericarditis plus the ECG finding not showing the diffuse pattern of pericarditis especially in V1, 2, 3, 4 and V5. A 40 year old male with a history of aortic stenosis presents to your office for an annual physical. You order blood work and an ECG. The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Left atrial enlargement 3) Mobitz II heart block 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice B. Left atrial enlargement occurs as a result of mitral valve disease, aortic valve disease, or long standing hypertension. It is characterized by a widened QRS complex, often with a biphasic appearance. Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex. A mobitz II (2nd Degree) heart block (choice C) is characterized by a fixed prolonged PR interval with intermittent skipped beats.

Right atrial enlargement (choice D) is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension. A 58 year old male with a history of pulmonary hypertension presents to your office as a new patient. You order his annual blood work and a screening ECG for your records. The electrocardiogram below shows which of the following:
1) Right Ventricular Hypertrophy 2) Left axis deviation

3) Mobitz II heart block 4) Right atrial enlargement 5) None of the above
The correct answer is choice A Right ventricular hypertrophy occurs in the setting of right heart strain, e.g. pulmonary hypertension. It is characterized by a rightward axis, seen in this ECG, and an R wave in AVR. Left axis deviation (choice B) is characterized by positive deflection in lead I and negative deflection in AVF. A 2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats. Right atrial enlargement (choice D) is characterized by increase height of the P wave. A 50 year old male with a history of a prior heart attack presents to the emergency room complaining of 1 hour of chest discomfort. He states that his symptoms resolved en route to the hospital and he feels fine. You order an ECG. The electrocardiogram below shows which of the following:

1) RBBB 2) LBBB 3) Left anterior hemiblock 4) right anterior hemiblock 5) None of the above
The correct answer is choice A.

This ECG demonstrates a right bundle branch block (RBBB), which is characterized by a wide complex, rabbit ear appearance of the QRS complex in V1, the so-called R-S-R-prime morphology. A left bundle branch block (LBBB) (choice B) is characterized by a wide QRS complex and ST segment abnormalities. In the setting of chest pain, a new LBBB requires emergency reperfusion therapy with a thrombolytic like tPA or an emergency angioplasty. Hemiblocks (choices C and D) are incomplete branch blocks and have narrow QRS complexes. A 63 year old female presents to your primary care office for an annual physical. She has a history of poorly controlled hypertension. You order blood work and a screening ECG. The electrocardiogram below shows which of the following:

1) left ventricular hypertrophy 2) Left atrial enlargement 3) Right ventricular hypertrophy 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice A.

Left ventricular hypertrophy is a common consequence of poorly controlled hypertension. The left ventricle's cardiac muscle changes in response to increased afterload. It is characterized by multiple ECG changes, principally increasing height of QRS complexes. Left atrial enlargement (choice B) occurs as a result of mitral valve disease, aortic valve disease, or long standing hypertension. It is characterized by a widened QRS complex, often with a biphasic appearance. Right ventricular hypertrophy (choice C) is characterized by a right axis deviation. Right atrial enlargement (choice D) is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension. A 70 year old male with a significant cardiac history presents to the emergency department complaining of one week of weakness and lethargy. His pulse is 40 in triage so you order immediate cardiac monitoring. The rhythm strip below shows which of the following:
1) Atrial fibrillation 2) Torsades des pointes 3) Mobitz II heart block 4) Complete (third degree) heart block 5) Acute pericarditis
The correct answer is choice D.

This rhythm strip shows a complete heart block. Also known as "AV dissociation," the atria and ventricles are beating on separate fixed rhythms and atrial beats are not conducted to the ventricles. Complete heart block is associated with life threatening bradycardia and requires emergent pacemaker placement. Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes. Torsades des pointes (choice B) is a type of ventricular tachycardia that is associated with long QT syndrome, hypokalemia, and hypomagnesemia. It often degrades to ventricular fibrillation. Torsades des pointes appears as a crescendo, decrescendo of the QRS complex heights over several beats. 2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats. Acute pericarditis (choice E) is an inflammatory condition of the pericardium causing PR depression and diffuse ST elevation. The electrocardiogram below shows which of the following:

1) LAD and LAE 2) RAD and RAE 3) LAE and LVH 4) LAE and RAE 5) RAD and LAE
The correct answer is choice B. RAD and RAE are the correct choices. In this case we need to know how to recognise the cardiac axis and the atrium chamber enlargement on the ECG trace. The cardiac axis refers to the mean direction of the wave of ventricular depolarisation in the vertical plane, measured from a zero reference point. Several methods can be used to calculate the cardiac axis, though occasionally it can prove extremely difficult to determine. The simplest method is by inspection of leads I, II, and III. as we can see in the ( hexaxial diagram), each lead’s view of the heart in the vertical plane. The cardiac axis may lie anywhere between 180 and − 180°. The normal range for the cardiac axis is between − 30° and 90°. An axis lying beyond − 30° is termed left axis deviation, whereas an axis > 90° is termed right axis deviation. And in the ECG trace above the QRS complexes in leads I, II, and III is pointing positive above the line so it's Right axis deviation. The second issue in this ECG strip is how to recognise the Rt. Atrium enlargement RAE, Simply we look to the P wave, and (P waves are usually most prominently seen in leads II). Right atrial hypertrophy or dilatation is associated with tall P waves in the anterior and inferior leads, though the overall duration of the P wave is not usually prolonged. A tall P wave (height >2.5 mm) in leads II, III, and aVF is known as the P pulmonale.

LAE and LVH (choice C) is not the correct answer. A pronounced notch with a peak-to-peak interval of > 1 mm(0.04 s) is usually pathological, and is seen in association with a left atrial abnormality or enlargement —for example, in mitral stenosis. In this ECG we can see clear tall P wave. For the Left ventricular hypertrophy Voltage criteria in Limb leads, we can see R wave in lead 1 plus S wave in lead III >25 mm, R wave in lead aVL >11 mm, R wave in lead aVF >20 mm,S wave in lead aVR >14 mm, and in the Precordial leads we can see R wave in leads V4, V5, or V6 > 26 mm, wave in leads V5 or 6 plus S wave in lead V1 > 35 mm, Largest R wave plus largest S wave in precordial leads > 45 mm. The Non-voltage criteria areDelayed ventricular activation time >0.05 s in leads V5 or V6 >0.05 s, ST segment depression and T wave inversion in the left precordial leads and none of these can be seen in the trace. LAD and LAE (choice A), LAE and RAE (choice D), and RAD and LAE (choice E) are not the correct answers as it has been explained above.

A 50 year old male presents to your office for medical clearance prior to a wrist surgery he has scheduled for next week. You order blood work and an ECG. The electrocardiogram below shows which of the following:

1) Right bundle branch block 2) Acute inferior wall myocardial infarction with reciprocal depression in the lateral leads 3) Left bundle branch block 4) Left anterior hemiblock 5) None of the above
The correct answer is choice A.
This patient has a right bundle branch block, which occurs when cardiac conduction is delayed over the right branch of the bundle of His. Characteristic ECG findings include a wide QRS complex with a rabbit ears appearance of V1-V2, and a terminal R wave in V5-V6.
An acute inferior wall MI (choice B) is characterized by ischemic changes (e.g. ST elevation) in inferior leads (AVF, II, and III).

A left bundle branch block (choice C) is characterized by a wide complex with ST segment abnormalities.
A left anterior hemiblock (choice D) is a block of part of the left bundle branch, characterized by left axis deviation, normal QRS complex width, among other findings.
The electrocardiogram below shows which of the following:
1) Anteroseptal MI 2) Anterior MI 3) Posterior MI 4) Posterolateral MI 5) Right ventricular MI
The correct choice is A.
We use a 12-lead EKG to pinpoint the site were the coronary artery might be occluded. EKG changes indicative of an MI are found only in the leads that look directly at the site of the infarction, and the waveforms provide valuable information to guide treatment. When interpreting 12-lead EKGs, it's helpful to think of the leads as groups, or sister leads, based on the area of the heart that they "see". Lead V2, V3, and V4 see the anterior wall of the left ventricle. Lead V1 is the septal lead. Leads I, aVL, V5, and V6 look at the lateral wall. Leads II, III, and aVF see the inferior wall of the left ventricle. The aVR lead is of limited use for recognizing an MI. For this trace ECG, ST segment elevation in leads V1 – V4 represents an anteroseptal MI because the zone of injury includes the anterior wall and the anterior

portion of the septal wall.
Anterior MI (choice B) is not the correct answer. An anterior wall MI is caused by occlusion of the left anterior descending coronary artery (LAD). You'll see ST segment elevation in leads V2 – V4. Muscle damage is seen in the anterior wall of the left ventricle. The higher or more proximal the occlusion, the more muscle damage there is.
Posterior MI (choice C), Posterolateral MI (choice D), Right ventricular MI (choice E) are not the correct answers. An inferior wall MI is usually due to occlusion of the right coronary artery (RCA), with muscle damage in the right ventricle and the posterior and inferior left ventricle. This is seen on the EKG as ST segment elevation in leads II, III, and aVF. Up to half of all inferior wall MIs are associated with an occlusion of the proximal portion of the RCA, which can lead to significant damage to the right ventricle. Infarction of the posterior wall of the LV, like an MI of the right ventricle, is uncommon. The posterior wall generally has a dual blood supply from the RCA and the circumflex artery. Because a 12-lead EKG looks primarily at the front of the heart, no leads face an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall.
Posterior wall MI is best confirmed by ST segment elevation in leads V7 – V9, which are tracings from electrodes placed on the patient's back in the fifth intercostal space beginning at the left posterior axillary line. Damage to the right ventricle is best seen on the EKG by placing electrodes on the right side of the chest in a position that mirrors the location of leads V1 – V6 on the left side of the chest. In this mirror image position, the leads are identified as V1R – V6R. Right ventricular MI is seen as ST segment elevation of 1 mm or more in leads V3R – V6R, particularly in V4R.
A 59 year old female diabetic presents to the emergency department with a 2 hour history of chest tightness and shortness of breath.
You order an ECG and supplemental oxygen.
The electrocardiogram below shows which of the following:

1) RBBB 2) LBBB 3) Left anterior hemiblock 4) Right anterior hemiblock 5) None of the above
The correct answer is choice B.
This ECG demonstrates a left bundle branch block (LBBB), characterized by a wide QRS complex and ST segment abnormalities. In the

setting of chest pain, a new LBBB requires emergency reperfusion therapy with a thrombolytic like tPA or an emergency angioplasty.
A right bundle branch block (RBBB) (choice A) is characterized by a rabbit ear appearance of the QRS complex in V1, the so-called R-S-R-prime morphology.
Hemiblocks (choices C and D) are incomplete branch blocks and have narrow QRS complexes.
A 25 year old male basketball player presents to your office after sustaining blunt traumatic injury to his chest during a game. His chest
X-Ray is negative for rib fractures or pneumothorax. You order an ECG.
The electrocardiogram below shows which of the following:

1) Left Ventricular Hypertrophy 2) Right axis deviation 3) Mobitz II heart block 4) Right atrial enlargement 5) None of the above

The correct answer is choice B.
Right axis deviation is common in patients with posterior heart blocks, and can also be seen in patients who are tall or have situs inversus. It is characterized by a negative deflection in lead I and a positive deflection in AVF.
Left ventricular hypertrophy (choice A) is characterized by large heights of QRS complexes in anterior prechordial leads.
A 2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
Right atrial enlargement (choice D) is characterized by increase height of the P wave.
The electrocardiogram below shows which of the following:

1. 3rd degree AV Block
2. Sinus rhythm
3. LVH (left ventricular hypertrophy)
4. Ventricular Pacing
1) 1, 2, and 3 only 2) 1 and 4 3) 2 and 4 only 4) 4 only 5) all are correct
The correct answer is choice B.
In third degree block, there is complete failure of conduction between the atria and ventricles, with complete independence of atrial and ventricular contractions as seen in this strip ECG. The P waves bear no relation to the QRS complexes and usually proceed at a faster rate as seen in the second ECG trace. Complete heart block is caused by a conduction block at the level of the AV node, the bundle of His, or the bundle-branch Purkinje system. In most cases (approximately 61%), the block occurs below the His bundle. Block within the AV node

accounts for approximately one fifth of all cases, while block within the His bundle accounts for slightly less than one fifth of all cases. Duration of the escape QRS complex depends on the site of the block and the site of the escape rhythm pacemaker. Pacemakers above the His bundle produce a narrow QRS complex escape rhythm, while those at or below the His bundle produce a wide QRS complex.
When the block is at the level of the AV node, the escape rhythm generally arises from a junctional pacemaker with a rate of 45-60 beats per minute. Patients with a junctional pacemaker frequently are hemodynamically stable and their heart rate increases in response to exercise and atropine. When the block is below the AV node, the escape rhythm arises from the His bundle or the bundle-branch Purkinje system at rates less than 45 beats per minute. These patients generally are hemodynamically unstable and their heart rate is unresponsive to exercise and atropine. It is clear here that there is Pacing spikes in this strip ECG.
In order to calculate if there is voltage criteria for LVH (left ventricular hypertrophy) we need to measure the depth of the S in V1 is measured and added to the height of the R in V6 her in this strip ECG we cannot. We have only V1 Lead so it is not possible to calculate voltage criteria for LVH.
Normal sinus rhythm criteria are: The P wave is upright in leads I and II, each P wave is usually followed by a QRS complex, the heart rate is 60-99 beats/min. As in the first strip the P wave is not normal upright, each P wave is usually followed by a QRS complex which we cannot see it here, the heart rate is around 35 beats/min, however after the capture we can see the features of normal sinus, but in this strip there is also spike for the pacemaker so it is not a normal sinus rhythm.
Choices A, C, D, and E, are not the correct answers, as has been mentioned above.
A 60 year old male with no past medical history presents to the emergency department complaining of palpitations and chest pain. On
arrival his pulse is approximately 130 beats per minute and irregularly irregular. You order a ECG and diagnose the patient with atrial
fibrillation.
All of the following ECG findings accurately describes this condition except?
1) P-R interval will be shorter

2) QRS interval will be maintained 3) There will be more QRS complexes than P waves 4) The T wave will be present 5) Discrete P waves are absent
The correct answer is choice C.
Atrial fibrillation occurs when disorganized and electrical impulses, originating from the atria, irregularly conduct through the AV node to produce ventricular contractions. The AV node limits the number of impulses that can proceed to the ventricles, so the ECG demonstrates more P waves (atrial impulses) than QRS complexes (ventricular contractions). The ventricular rate is typically irregular.
The P-R interval (choice A), is not a relevant interval that can be analyzed in the setting of atrial fibrillation given the high number of unconducted atrial impulses present.
The QRS interval (choice B) is usually maintained since it is determined by the path of the electrical impulse distal to the AV node. So there will ultimately be fewer QRS complexes compared with P waves, not the opposite (choice C).
After ventricular contraction, the ventricles will repolarize as usual, causing a T wave (choice D).
Discrete P waves (choice E) are absent; instead, undulating fibrillatory (f) waves are present.

The accompanying 12-lead electrocardiogram is taken form an 80 year old man seen in the ER with abdominal pain.

Which of the following is correct:
1) the underlying rhythm is atrial fibrillation 2) the wide QRS complex is due to left bundle branch block 3) the wide QRS complex is due to left bundle branch block 4) the patient needs to be assessed for the requirement of anticoagulation 5) magnetic resonance imaging (MRI) is contraindicated in the investigations of the patient
The correct answer is choice B.
Wide QRS complex is due to left bundle branch block is the correct answer. This ECG represents a left bundle branch block which most commonly is caused by coronary artery disease, hypertensive heart disease, or dilated cardiomyopathy. It is unusual for left bundle branch block to exist in the absence of organic disease. The left bundle branch is supplied by both the anterior descending artery (a branch of the left coronary artery) and the right coronary artery. Thus patients who develop left bundle branch block, generally have extensive disease.
This type of block is seen in 2-4% of patients with acute myocardial infarction and is usually associated with an anterior infarction. The diagnostic criteria for left bundle branch block include: QRS duration of >0.12 s; broad monophasic R wave in leads 1, V5, and V6; Absence of Q waves in leads V5 and V6; Displacement of ST segment and T wave in an opposite direction to the dominant deflection of

the QRS complex (appropriate discordance); Poor R wave progression in the chest leads; RS complex, rather than monophasic complex, in leads V5 and V6 and Left axis deviation which is clearly seen in this strip. Also in this ECG, we see a wide QRS complex.
Choice A is not the correct answer. Atrial fibrillation is caused by multiple re-entrant circuits or ―wavelets‖ of activation sweeping around the atrial myocardium. These are often triggered by rapid firing foci. Atrial fibrillation is seen on the ECG as a wavy, irregular baseline made up of f (fibrillation) waves, and there is no recognised P wave can be seen especially in lead 2.
Cardiac pacing with the capture at 70 beats per minute (choice C) is not the correct answer. It is clear in this ECG there are no Pacing spikes.
Patient needs to be assessed for the requirement of anticoagulation (choice D) is not the correct answer. With the lack of information and full history, it is difficult to diagnose this patient as having a new onset of MI, however this possibilty is still there with ST elevation of more than 1mm.
Magnetic resonance imaging (MRI) is contraindicated in the investigations of the patient (choice E) is not the correct answer. Absolute Contraindications for the MRI are: electronically, magnetically, and mechanically activated implants, ferromagnetic or electronically operated active devices like automatic cardioverter defibrillators, cardiac pacemakers, metallic splinters in the eye, and ferromagnetic haemostatic clips in the central nervous system. The above ECG shows no pacemaker spike plus there is no history given to make an MRI contraindicated for this patient.
A 48 year old male is brought to the emergency department after passing out at home. He arguing with his wife when he suddenly
collapsed. He regained consciousness a few minutes later and is currently without complaints. You order blood work and an ECG. His
ECG shows sinus rhythm, no obvious ischemic changes, and a corrected QT (QTc) interval of 500 ms.
What other ECG sign would indicate a high risk for a cardiac event?
1) T-wave alternans 2) U wave development

3) Peaked T waves 4) Osborne waves 5) Left posterior fascicular block
The correct answer is choice A.
The presence of T wave alternans is a significant risk factor for sudden cardiac death. It refers to a periodic change in the vector and amplitude of sequential T waves. It can be measured using the naked eye or with the use of a "microvolt T wave alternans" device. This test is used to risk stratify patients and determine who needs an implantable defibrillator.
A U wave (choice B) can be a normal finding between the T and P waves, but is often associated with hypokalemia.
Peaked T waves (choice C) are associated with hyperkalemia and may be found in the early stages of a myocardial infarction.
Osborne waves (choice D) have been described in patients with hypothermia, and are positive deflections which occur at the "J point," at the beginning of the ST segment.
A Left posterior fascicular block (choice E) is a partial block of the left bundle branch and is characterized by extreme right axis deviation.
A thirty year old male presents to the emergency department with a chief complaint of chest pain. He also complains of several days of
cough. He states that the pain is worse when he takes a deep breath. You order an ECG as part of his initial work up.

The electrocardiogram below shows which of the following conditions:
1) Atrial fibrillation 2) Torsades des pointes 3) Mobitz II heart block 4) Ventricular tachycardia 5) Acute pericarditis
The correct answer is choice E.
This ECG shows signs of pericarditis, with diffuse ST elevations and PR depressions.
Pericarditis is an inflammatory process of the pericardium and often presents with chest pain, often relieved by leaning forward. It can occur related to an infection, malignancy, following an MI, or it can be idiopathic in nature.

Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.
Torsades des pointes (choice B) is a type of ventricular tachycardia that is associated with long QT syndrome, hypokalemia, and hypomagnesemia. It often degrades to ventricular fibrillation. Torsades des pointes appears as a crescendo, decrescendo of the QRS complex heights over several beats.
2nd Degree Mobitz II heart block (choice C) occurs when certain beats are dropped in the absence of PR shortening after the dropped beat. The PR interval will remain fixed, unlike a 2nd degree type I heart block.
Ventricular tachycardia (choice D) is a wide complex tachycardia, it is a life threatening arrhythmia that requires cardioversion if symptomatic.
A 70 year old male presents to the emergency room with signs of impending respiratory failure. You sedate and intubate him, then place
him on a mechanical respiratory. You order a chest X-ray, labs, and an ECG.

The electrocardiogram below shows which of the following:
1) Atrial fibrillation
2) Tachycardia
3) Mobitz II heart block
4) Right axis deviation
5) None of the above
The correct answer is choice D.
This ECG demonstrates bradycardia and right axis deviation. Right axis deviation occurs in the setting of right ventricular hypertrophy and is characterized by a negative deflection in lead I and a positive deflection in AVF.
Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS

complex.
This ECG shows bradycardia, not tachycardia (choice B).
A 2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A 45 year old male presents to your office complaining of intermittent palpitations. He states that he sometimes feels like his heartbeat is
irregular and beating too fast. He states he currently feels fine. He has a history of a "mild" heart attack three year ago. You place him
on a cardiac monitor and obtain the rhythm strip below.
Which of the following is the correct diagnosis?
1) Atrial fibrillation 2) Torsades des pointes 3) Atrial flutter 4) Ventricular tachycardia 5) Acute pericarditis
The correct answer is choice A.
Atrial fibrillation occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of

QRS complexes.
Torsades des pointes (choice B) is a type of ventricular tachycardia that is associated with long QT syndrome, hypokalemia, and hypomagnesemia. It often degrades to ventricular fibrillation. Torsades des pointes appears as a crescendo, decrescendo of the QRS complex heights over several beats.
Atrial flutter (choice C) is a nodal reentry arrhythmia characterized by tachycardia and a sawtooth pattern on ECG.
Ventricular tachycardia (choice D) is a wide complex tachycardia, it is a life threatening arrhythmia that requires cardioversion if symptomatic.
Acute pericarditis (choice E) is an inflammatory condition of the pericardium causing PR depression and diffuse ST elevation.
A 50 year old male with a history of uncontrolled hypertension presents to your primary care office for a physical exam. His blood
pressure is 160//95. You order screening blood work and an ECG. His ECG shows left ventricular hypertrophy and left atrial enlargement.
In left atrial enlargement, the P wave has which of the following patterns:
1) Increases in amplitude. 2) Increases in duration 3) Increases in both amplitude and duration 4) Shows terminal P negativity in lead I 5) None of the above
The correct answer is choice B.
Left atrial enlargement is characterized by increased P wave duration, greater than 0.12 s, and a notched P wave. It can also have a biphasic P with a terminal negative deflection in V1. Left atrial enlargement is caused by hereditary factors or left sided heart strain, e.g.

hypertension.
Increased amplitude of P (choice A) is associated with right atrial enlargement.
Terminal P negativity (choice C) occurs in V1, not I.
A 55 year old man presents to the emergency department complaining of 1/2 hour of chest pain which began while he was shovelling

snow. He has a history of diet controlled hypercholesterolemia and was told he may have early diabetes, but he currently takes no
medications. His ECG on arrival shows ST elevations in anterior prechordial leads (v1, v2, and v3).
What is the most appropriate treatment protocol to follow for this patient?
1) Administer aspirin and admit for serial cardiac enzymes 2) Administer aspirin and heparin and admit for serial cardiac enzymes 3) Administer aspirin and heparin, and obtain cardiology consult for coronary angiography tomorrow morning. 4) Emergency reperfusion with a thrombolytic medication or via percutaneous cardiac intervention 5) Obtain serial ECG's and discharge with outpatient cardiology follow up
The correct answer is choice D.
The ST segment lies between the QRS complex and T wave in an ECG and occurs during systolic contraction of cardiac muscle. There are several causes of ST elevation, but in the setting of chest pain the most important differential diagnosis is myocardial ischemia/infarction (MI)
ST elevation during a heart attack occurs as a result of cardiac muscle inflammation and damage, often as a result of the total occlusion of a coronary artery. ST elevation or a new left bundle branch block, in the correct clinical setting, are indications for emergency reperfusion therapy. This can be achieved pharmacologically, with a thrombolytic drug like tPA, or by an interventional cardiologist performing an emergency angioplasty (aka percutaneous coronary intervention). These interventions should be performed without delay because "time is tissue!"
Aspirin and heparin (choices A,B, and C) are helpful treatment options which can be initiated in the emergency department, but this patient meets criteria for an ST elevation myocardial infarction and thus requires immediate reperfusion. This cannot wait until the next morning (choice C) or several days for an outpatient follow up (choice E).
A 60 year old male with a history of coronary artery disease presents to your office for medical clearance prior to an outpatient surgical
procedure. You order blood work and a screening ECG.

The electrocardiogram below shows which of the following:
1) Left Bundle Branch Block
2) Right Bundle Branch Block
3) Left Anterior Fascicular Block
4) Right Bundle Branch Block & Left Anterior Fascicular Block
5) Right Bundle Branch Block & Left Posterior Fascicular Block
The correct answer is choice D.
A right bundle branch block can co-exist with a left anterior fascicular block. A right bundle branch block (choice B) is characterized by a R-S-R-prime morphology in V1 and a slurred upstroke of the S wave in V6. A left anterior fascicular block (choice C) is characterized by a left axis deviation, Q-R in I and AVL, and R-S in inferior leads (II, III, and AVF).
A left bundle branch block (choice A) is characterized by a wide complex, Q-S morphology in lead V1.

A left posterior fascicular block (choice E) is characterized by an extreme right axis deviation.
A 55 year old female with a history of poorly controlled diabetes and hypertension presents to the emergency room complaining of 2 hours
of substernal chest pain. You order a stat ECG.
The electrocardiogram below shows which of the following:
1) Atrial fibrillation 2) Acute inferior wall myocardial infarction with reciprocal changes 3) Mobitz II heart block 4) Left anterior hemiblock 5) None of the above
The correct answer is choice B.

This patient is having an inferior wall MI based on the ST elevation noted in leads II, III, and AVF. Reciprocal changes are noted in AVL and AVR. This patient requires immediate treatment with aspirin, oxygen, heparin, and may be a candidate for thrombolysis with tPA or emergency angiography depending on the resources available.
Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.
2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A left anterior hemiblock (choice D) involves a conduction delay along the anterior fascicle of the left bundle branch, causing a left axis deviation among other changes. Unlike a left bundle branch block, this will produce narrow complex QRS complexes.
A 30 year old male with a history of renal failure and severe hypertension presents to the emergency department complaining of malaise
and palpitations. He was scheduled for dialysis yesterday but he did not go because he was feeling sick. You order blood work and an
ECG.

The electrocardiogram below shows evidence of which of the following electrolyte abnormalities:
1) Hypercalcemia 2) Hyperkalemia 3) Hypocalcemia 4) Hypokalemia 5) None of the above
The correct answer is choice B.
This ECG shows evidence of hyperkalemia, with peaked T waves and QRS complex widening. Severe hyperkalemia can progress to cause a complete heart block, ventricular fibrillation, or asystole. Hyperkalemia is a common problem in patients with renal failure. Emergency

treatment involves intravenous calcium, kayexalate, a combination of dextrose and insulin to cause an intracellular shift of K ions, and in severe cases dialysis.
Hypercalcemia (choice A) causes ST depression, short QT interval, and bradycardia.
Hypocalcemia (choice C) causes a long QT interval.
Hypokalemia (choice D) causes flat T waves, long QT interval, and U waves.
With mild to moderate hyperkalemia, there is reduction of the size of the P wave and development of peaked T waves. Severe hyperkalemia results in a widening of the QRS complex, and the EKG complex can evolve to a sinusoidal shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. Also, (as noted above), hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex.
Summary of Treatment Options:
The medications that treat hyperkalemia are meant to stabilize heart function, promote the movement of potassium from the bloodstream back into the cells, and encourage the excretion of excess potassium. Hemodialysis is the most reliable tool for removing potassium from the body in patients with kidney failure. Drug Therapies include:

Calcium Chloride or Gluconate -- minimizes the effects of hyperkalemia on the heart
Insulin -- promotes potassium shift from blood to cells
Sodium bicarbonate -- promotes potassium shift from blood to cells
Beta agonists -- promote potassium shift from blood to cells
Diuretics -- cause potassium excretion from kidneys
Binding resins -- promote potassium and sodium exchange in the gastrointestinal system
A 50 year old male with poorly controlled hypertension presents to the emergency department complaining of weakness, dizziness, and
headache. His blood pressure in triage is 190/110. You order an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Left ventricular enlargement 3) Mobitz II heart block 4) Right ventricular Enlargement 5) None of the above
The correct answer is choice B.

Left ventricular hypertrophy is a common consequence of poorly controlled hypertension. The left ventricle's cardiac muscle changes in response to increased afterload. It is characterized by multiple ECG changes, principally increasing height of QRS complexes and a left axis deviation.
Atrial fibrillation (choice A) occurs when numerous atrial beats occur and are irregularly conducted through to the ventricles, so there will be multiple P waves for every single QRS complex.
A 2nd Degree, Mobitz II heart block (choice C) is characterized by a prolonged PR interval with periodically dropped beats.
Right ventricular enlargement (choice D) is characterized by a right axis deviation.
A 28 old female prison inmate is brought to the emergency room after intentionally overdosing on an unknown medication smuggled into
her cell. She is agitated and uncooperative and requires sedation. You order labs and an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Acute inferior wall myocardial infarction with reciprocal depression in the lateral leads 3) Mobitz II heart block 4) Prolonged QT intervalc 5) None of the above
The correct answer is choice D.
The patient shows evidence of a prolonged QT interval, which is a common side effect of antipsychotic medication overdose. The QTc (corrected QT interval) is calculated by taking the QT interval and dividing it by the square root of the RR interval. If it is greater than 480 msec it is considered prolonged. A prolonged QT interval can also be visually estimated if the T wave is more than halfway between the intervening QRS complexes.
Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.

An inferior MI (choice B) will show ischemic changes in inferior leads, e.g. leads II and AVF.
A 2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A 30 year old male with a history of end stage renal disease on dialysis presents to the emergency department complaining of fatigue and
body aches. He states he missed his last dialysis treatment because of a scheduling conflict. You suspect hyperkalemia and order an
ECG.
All of the following are the ECG features of severe hyperkalemia except:
1) Peaked T waves 2) Presence of U waves 3) Sine wave pattern 4) Loss of P waves 5) Wide QRS complex
The correct answer is choice B.
Hyperkalemia is a common and life threatening condition in patients with end stage renal disease since potassium is regulated primarily by urinary excretion. Common ECG findings in hyperkalemia include peaked T waves, QRS widening, flat P waves, and eventually a sine wave (which is indicative of imminent ventricular fibrillation).
Hyperkalemia with ECG changes warrants immediate therapy with IV glucose and insulin, oral kayexelate, albuterol, and IV calcium.
U waves (choice B), are commonly associated with hypokalemia.
A 45 year old female presents to the emergency room complaining of three days of shortness of breath. She is a non-smoker and has no

past medical history. You order a chest x-ray and an ECG. Her x-ray is normal, but her ECG shows an incomplete right bundle branch
block and an S1Q3T3 pattern.
S1Q3T3 pattern in an ECG is classically described which of the following conditions:
1) Pulmonary hypertension 2) Acute inferior wall MI 3) Hypokalemia 4) Hypocalcemia 5) Pulmonary embolism
The correct answer is choice E. A pulmonary embolism occurs when a peripheral blood clot from the venous system travels to the pulmonary vasculature, causing an blood flow obstruction and ventilation/perfusion mismatch. It is a life threatening emergency associated with sudden death. ECG changes are associated with the right heart strain caused by the pulmonary vasculature blockage. ECG changes in a PE most commonly include tachycardia, and an incomplete right bundle branch block. The classic finding of the S1Q3T3, S wave in lead I, Q in lead III, and inverted T in lead III, has become synonymous with a PE, although it is rarely present in practice. Pulmonary hypertension (choice A) will cause right ventricular hypertrophy and a right axis deviation. An acute inferior wall MI (choice B) will demonstrate ischemic changes in inferior limb leads (II, III, and AVF). Hypokalemia (choice C) is associated with flat T waves, a U wave, and a prolonged QT interval. Hypocalcemia (choice D) is associated with narrow QRS, QT prolongation, T wave flattening, and a short PR interval. You are working a busy shift in the emergency department when the triage nurse brings you an ECG. He asks if the patient can wait in the waiting room for a while. The ECG has a sinus rhythm, a regular rate, a regular axis, but numerous leads demonstrate ST depressions and abnormally shaped T waves. You tell the nurse to bring the patient back. Which of the following conditions is usually associated with primary ST-T wave abnormalities?
1) Left anterior fasicular block

2) Premature ventricular contractions 3) Wolff Parkinson White syndrome 4) Electrolyte abnormalities 5) Left posterior fascicular block
The correct answer is choice D.
ST segment and T wave abnormalities can be caused by a variety of conditions, many of which are life threatening. These include ischemia, electrolyte abnormalities, drug toxicity, hyperventilation syndrome, and cardiac conduction abnormalities.
A left anterior fascicular block (choice A) is characterized by a left axis deviation, a QR pattern in leads I and AVL, and an RS pattern in leads II, III, and AVF.
Premature ventricular contractions (choice B) are periodic ventricular beats which will appear on an ECG as an intermittent wide complex QRS deflection without a preceding P wave.
Wolff Parkinson White syndrome (choice C) is a pre-excitation condition caused by an accessory pathway, and is characterized by a slurred upstroke of the R wave (the delta wave).
A left posterior fascicular block (choice E) is a partial left bundle branch block characterized by extreme right axis deviation.
You are handed an ECG from your triage nurse. She points to a waveform between the T and P waves and asks if it is evident of atrial
fibrillation. You review the rate and wave morphology and decide that it is a U wave.
Normal U waves are usually best seen in which of the following leads?
1) I 2) V1,V2

3) II, III, and aVF 4) aVL or aVR 5) I and II
The correct answer is choice B.
U waves are rarely seen on an ECG. They are thought to be "after depolarizations" that occur and interrupt the repolarization phase (T-P segment). They are associated with tachycardia, hypokalemia, hypercalcemia, thyrotoxicosis, and intracranial hemorrhage. The U wave is an additional deflection which occurs following the T wave. U waves can also be normal in an ECG, and are best seen in right prechordial leads (V1 or V2).

A 64 year old man with heart failure takes 80 mg of furosemide per day. He presents to the emergency room a few weeks after running
out of his potassium supplement, and complains of muscle cramps and fatigue. You suspect hypokalemia and order blood work and an
ECG.
Which of the following ECG changes are associated with hypokalemia:
1) Short P-R interval 2) U wave appearance 3) Short Q-T interval 4) Widened QRS

5) Flattened P waves The correct answer is choice B.
Hypokalemia is suspected in this patient because furosemide increases the urinary excretion of potassium. Symptoms of hyokalemia include fatigue, malaise, body aches, and constipation.
ECG changes include a flat T wave, QT prolongation, and prominent U waves.
QRS prolongation (choice D) is associated with hyperkalemia.
Short PR and QT and a flat P (choices A, C, and D) are associated with hyperkalemia.

A 70 year old female is brought to the emergency department complaining of dyspnea. She has a history of hypertension, congestive
heart failure, and chronic obstructive lung disease. On examination her vital signs are: 97.0 deg F (36.1 deg C), pulse 119 beats per
minute, respiratory rate 28 breaths per minute, and blood pressure 137/88. Her neck veins are distended, her cardiac exam is tachycardic
but regular, her lung exam shows rales at both bases. You order a chest x-ray and an ECG.
Her ECG reveals which of the following?
1) Atrial fibrillation 2) Left anterior fascicular block 3) Acute posterior wall infarction

4) Right axis deviation 5) Left posterior facsicular block
The correct answer is choice B.
A left anterior fascicular block a conduction delay caused by damage to the anterior fascicle of the left bundle branch. It is characterized by a left axis deviation, a QR pattern in left limb leads, and a RS pattern in inferior limb leads. It is often associated with acute anterior or inferior wall myocardial infarctions, hypertensive heart disease, and cardiomyopathy.
Atrial fibrillation (choice A) describes the condition of multiple atrial beats (P waves) intermittently and irregularly conducting to fewer ventricular response beats (QRS complexes).
A posterior wall infarction (choice C) is characterized by subtle ischemic changes in anterior prechordial leads. When suspected, a posterior ECG should be obtained.

Right axis deviation (choice D) would be present with a negative deflection in lead I and a positive deflection in lead AVF.
A left posterior fascicular block (choice E) is characterized by an extreme right axis deviation.
You are working in the emergency department when one of your residents hands you the ECG of a patient that she was assessing. What is the rhythm in the lead tracing shown below:
1) first-degree heart block 2) second degree heart block 3) third degree heart block 4) premature ventriclular beats 5) premature atrial beats
The correct answer is Choice B
Second-degree heart block, or second-degree atrioventricular (AV) block, refers to a disorder of the cardiac conduction system in which some atrial impulses are not conducted to the ventricles. Second-degree AV block is composed of 2 types: Mobitz I or Wenckebach block, and Mobitz II. Type 1 second-degree heart block is considered a more benign entity than type 2 second-degree heart block. The PR interval gradually increase untill there is a drop beat.
Mobitz type I block is caused by conduction delay in the AV node in 70% of patients and by conduction delay in the His-Purkinje system in the remaining 30%. The presence of a narrow QRS complex suggests the site of the delay is more likely to be in the AV node. PR interval measures the total duration of periventricular depolarization from the begining of P wave to the begining of QRS complex. Type 1

second degree heart block usually indicates :
1. Myocarditis
2. Digitalis excess
3. A precursor of complete atrioventricular block in the setting of acute infarction
4. Healthy young adults with excess vagal tone can show type 1 second degree heart block

First-degree heart block (choice A) indicate constant PR segment prolongation more than 200 msec.
Third degree heart block (choice C) means complete dissociation between the P wave (atrial contraction) and the QRS (ventricular contraction). P wave rates usually will be around 70 per min while the ventricular rhythm will be around 40 beats per min.
Premature ventriclular beats (choice D) indicate an abnormally wide bizzare QRS usually originating from the ventricular conduction system.

Premature atrial beats (choice E) indicates premature atrial depolarization. The QRS looks like all other supraventricular QRS complexes.
The electrocardiogram below shows which of the following:
1) LAE 2) RAE 3) LVH with strain 4) Right axis deviation 5) Acute Myocardial infarction
The correct answer is choice C.
LVH with strain is the correct answer. In this ECG, we can clearly see the left ventricular hypertrophy based on the voltage criteria in the limb leads. We can see R wave in lead 1 plus S wave in lead III >25 mm, R wave in lead aVL >11 mm, R wave in lead aVF >20 mm, S wave in lead aVR >14 mm, and in the precordial leads we can see R wave in leads V4, V5, or V6 > 26 mm, wave in leads V5 or V6 plus S wave in lead V1 > 35 mm, Largest R wave plus largest S wave in precordial leads > 45 mm. The Non-voltage criteria are delayed ventricular activation time >0.05 s in leads V5 or V6, ST segment depression and T wave inversion in the left precordial leads.

LAE choice A is not the correct answer. A pronounced notch with a peak-to-peak interval of > 1 mm (0.04 s) is usually pathological, and is seen in association with a left atrial abnormality or enlargement and it is not present in this trace ECG.
RAE choice B is not the correct answer. Simply we look to the P wave (P waves are usually most prominently seen in leads II). Right atrial hypertrophy or dilatation is associated with tall P waves in the anterior and inferior leads, but in this trace, it has normal P waves.
Right axis deviation (choice D) is not the correct answer. The normal range for the cardiac axis is between − 30° and 90°. An axis lying beyond − 30° is termed left axis deviation, whereas an axis > 90° is termed right axis deviation. In the ECG trace above, the QRS complexes in leads I, II, and with the direction of lead III, the pattern is Left axis deviation not RAD.
Acute myocardial infarction choice E is not the correct answer. There is no ST segment elevation in this ECG.
A 70 year old male patient with a history of coronary artery disease and renal insufficiency presents to the emergency room complaining
of fatigue and weakness for several days. His daily medications include furosemide, digoxin, and aspirin. You order blood work and an
ECG. You receive a call from the laboratory reporting that his potassium level is 7.0. You look at his ECG and note peaked T waves and
digoxin effect.
Which of the following treatments for hyperkalemia is contraindicated in this patient?
1) IV insulin 2) IV dextrose 3) Dialysis 4) IV calcium 5) None of the above are contraindicated
The correct answer is choice D.
In the setting of possible digoxin toxicity, IV calcium should not be administered as a treatment for hyperkalemia. Digoxin works by increasing the intracellular availability of calcium, so administering IV calcium might worsen the effects of digoxin toxicity. Some studies

have recommended using IV magnesium as a cardiac muscle stabilizer in the place of calcium when digoxin toxicity is suspected.
Other standard therapies for hyperkalemia should nevertheless be administered as soon as possible. These include IV insulin and dextrose, and oral kayexelate. This patient may benefit from dialysis as well.
Cardiac effects:
tall, peaked T wave in precordial leads
widened QRS complex
prolonged P-R interval
decreased amplitude and disappearance of P wave
sine wave (blending of QRS into T wave)
ventricular arrhythmias

cardiac arrest
Neuromuscular effects:
vague muscular weakness (usually first sign)
flaccid muscle paralysis (first noticed in the legs, later in the trunk and arms, facial and respiration muscles affected last; muscles supplied by cranial nerves are usually spared)
paresthesias of the face, tongue, feet and hands are common and are the result of stimulation of pain receptors
central nervous system is not affected,patient often remains alert and apprehensive in spite of other changes until cardiac arrest occurs
Gastrointestinal effects:
nausea

intermittent intestinal colic or diarrhea
Laboratory data:
serum potassium >5.5 mmol/L
often associated with acidosis
Table 2: review of treatment options for Hyperkalemia

A 40 year old homeless female presents to brought to the emergency room by paramedics after being found unconscious on the street.
You recognize her as a regular patient with renal failure who is noncompliant with her medications and often skips her dialysis sessions.
You suspect a severe electrolyte abnormality and order blood work and an ECG.
All of the following are ECG characteristics of hyperkalemia except:
1) Lengthened P-R interval 2) Shortening of the Q-T interval 3) Broad–based (> 0.20 sec) peaked T wave 4) Widened QRS 5) Flattened P waves
The correct answer is choice B.
Hyperkalemia is a common and life threatening condition in patients with renal failure. Potassium is usually excreted by the kidneys, so patients who skip needed dialysis can precipitate a build up of this electrolyte.

ECG findings in hyperkalemia include peaked T waves, QRS widening, PR lengthening, and flat P waves.
Emergency treatment includes insulin, IV dextrose, albuterol, kayexelate, IV calcium, and dialysis.
Short QT interval (choice B) is associated with hypokalemia.

The electrocardiogram below shows which of the following:
1) Inferior MI 2) Posterior MI 3) Inferoposterior MI 4) Anterior MI 5) Non-Q wave MI
The correct answer is choice C.
Inferoposterior MI. An inferior wall MI is usually due to occlusion of the right coronary artery (RCA), with muscle damage in the right ventricle and the posterior and inferior left ventricle. This is seen on the EKG as ST segment elevation in leads II, III, and aVF. Up to half of all inferior wall MIs are associated with an occlusion of the proximal portion of the RCA, which can lead to significant damage to the right ventricle. The posterior wall generally has a dual blood supply from the RCA and the circumflex artery. Because a 12-lead EKG looks primarily at the front of the heart, no leads face an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall
Inferior MI (choice A) is not the correct answer. Inferior MI On the EKG is ST segment elevation in leads II, III, and aVF. Acute inferior MI with right-sided leads reflecting RV involvement. The limb leads demonstrate STE in the inferior leads (lead III > lead II), together with reciprocal STD in lead aVL >lead I all suggesting RCA occlusion. The precordial leads are actually leads V1R–V6R, or right-sided leads.

Posterior MI (choice B). Posterior wall MI is best confirmed by ST segment elevation in leads V7 – V9, which are tracings from electrodes placed on the patient's back in the fifth intercostal space beginning at the left posterior axillary line. Infarction of the posterior wall of the LV, like an MI of the right ventricle, is uncommon. The posterior wall generally has a dual blood supply from the RCA and the circumflex artery. Because a 12-lead EKG looks primarily at the front of the heart, no leads face an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall
Anterior MI (choice D) is not the correct answer. An anterior wall MI is caused by occlusion of the left anterior descending coronary artery (LAD). You'll see ST segment elevation in leads V2 – V4. Muscle damage is seen in the anterior wall of the left ventricle. The higher or more proximal the occlusion, the more muscle damage there is. An MI caused by occlusion of the left main (LM) coronary artery—the short vessel above the bifurcation of the LAD and the circumflex artery—is characterized by ST segment elevation in leads V1 – V6 and represents a large amount of muscle damage.
Non-Q wave MI (choice E) is not the correct answer. Non-Q wave MIs can be difficult to diagnose. But unless patients receive treatment, they typically extend the area of infarct, and end up with a Q wave MI.
A 45 year old male smoker presents to your primary care office for a physical exam. He has a strong family history of heart disease but
denies any personal history of chest pain or shortness of breath. You order blood work and an ECG.
The electrocardiogram below shows which of the following:

1) Right Bundle Branch Block 2) Left Bundle Branch Block 3) Left anterior hemiblock 4) Right anterior hemiblock 5) None of the above
The correct answer is choice A.
This patient has a right bundle branch block, which occurs when cardiac conduction is delayed over the right branch of the bundle of His. Characteristic ECG findings include a wide QRS complex with a rabbit ears appearance of V1-V2, and a terminal R wave in V5-V6. This

patient warrants a more thorough cardiac evaluation given this finding.
A left bundle branch block (choice B) is characterized by a wide complex with ST segment abnormalities.
A left anterior hemiblock (choice C) is a block of part of the left bundle branch, characterized by left axis deviation, normal QRS complex width, among other findings. A right hemiblock (choice D) will similarly show a normal QRS interval.
This ECG shows an example of right bundle branch block.
What other abnormality is present?
1) RBBB with primary ST-T wave abnormalities 2) Secondary ST-T wave changes 3) Anterolateral MI 4) LVH 5) RVH
The correct answer is choice A
RBBB with primary ST-T wave abnormalities is the correct pattern. In this trace, we can see the Diagnostic criteria for right bundle branch block; QRS duration >0.12 s, A secondary R wave (R) in V1 or V2, Wide slurred S wave in leads I, V5, and V6 and Associated features; ST

segment depression and T wave inversion in the right precordial leads. The right precordial leads have a prominent and late R wave, and the left precordial and limb leads have a terminal S wave. These terminal deflections are wide and slurred. Abnormal ventricular depolarisation is associated with secondary repolarisation changes giving rise to changes in the ST-T waves in the right chest leads.
Secondary ST-T wave changes (choice B) is not the correct answer. In the Secondary ST-T wave changes they will be a symmetrical, non specific ST changes and the ST-T waves will keep changing with exercise testing and with forced hyperventilation at rest.
Anterolateral MI (choice C) is not the correct answer. Antero-lateral Infarction changes of Acute MI are seen in all the anterior chest leads, from V1 through V6. Here we cannot see the ST elevation involved in the Antero-lateral leads; instead it is ST wave depression or ST-T wave abnormalities (ischemia) involved the Antero-lateral leads.
LVH (choice D) is not the correct answer. In Left ventricular hypertrophy, the depth of the S in V1 is measured and added to the height of the R in V6; the total is >35 mm to say It is LVH. And here it is less than 35 mm in this trace.
RVH (choice E) is not the correct answer. Normally R in V1 is <S in the same lead. If R height is found to be >S depth in lead V1, it meets the voltage criteria for RVH in Lead V1. Also an ECG with right ventricular hypertrophy shows a right axis deviation on the ECG, but here we can see this is a normal cardiac axis.
An 80 year old male with a history of hypertension presents to the emergency room complaining of chest pain. His only medication is a
beta blocker which he takes twice a day. You order an ECG.
What is the heart rate of the following ECG:

1) 50 2) 60 3) 70 4) 80 5) 90
The correct answer is choice B
There are several ways to calculate the rate on an ECG. The most simple way is to memorize the following sequence: 300, 150, 100, 75, 60, 50. Then count the number of big boxes between two QRS complexes, counting down using these numbers. If there are three big boxes between the QRS complexes for example, then the rate is 100. In this case, there are less than 5 big boxes, so the rate is between 50 and 75.
Another method is to count the number of QRS complexes over 6 seconds (30 big boxes) and multiply the number by 10. This method

works well when the rate is irregular.
A 92 year old female presents to the emergency department in respiratory distress. You intubate her, place her on mechanical ventilation,
and order a chest X-ray and and ECG. Her chest X-ray reveals a large left sided pneumonia.
The electrocardiogram below shows which of the following:
1) 1st Degree AV Block 2) Type I 2nd Degree AV Block 3) Type II 2nd Degree AV Block 4) 3rd Degree AV Block 5) None of the above
The correct answer is choice A.
A 1st degree AV block is characterized by a prolonged PR interval with no dropped beats. The normal PR interval is 120 to 200 msec long, or about one large box wide. The PR interval is measured between the start of the P wave and the start of the QRS complex.
A 2nd degree AV block is characterized by a prolonged PR interval and dropped beats. A type I 2nd degree AV block (choice B) has a PR interval that becomes more prolonged with each beat, then resets after a dropped beat. A type II 2nd degree heart block (choice C) has a fixed PR interval and intermittent dropped beats.
A 3rd degree, or complete, AV block (choice D) is characterized by complete AV dissociation, so the atria and ventricles each beat on their own independent rates.
A 60 year old male with no past medical history presents to the emergency department complaining of chest pain. He works for the

hospital, and his symptoms started while he was shoveling snow in front of the ambulance entrance and few minutes ago.
In an acute MI, which ECG finding is usually the first to appear?
1) Q wave 2) Hyperacute T wave 3) T wave inversion 4) ST segment elevation 5) None of the above
The correct answer is choice B.
The first sign of myocardial ischemia, although it is non-specific, is an increased amplitude of T waves. Peaked T waves also occur in the setting of Hyperkalemia, so it is hypothesized that the ischemia causes localized hyperkalemia leading to the repolarization abnormality. Hyperacute T waves in the setting of chest pain warrants frequent repeat ECG's to look for dynamic changes more specific of an ischemic process.
T wave changes and ST segment elevation or depression (choices C and D) occur next and are more specific for infarction.
Q waves (choice A) are late findings of infarction.

A 60 year old male presents to your primary care office for an annual physical. You order screening blood work and an ECG. His ECG
shows a broad, notched P wave in several limb leads.
Which of the following conditions are associated with a broad notched P wave?
1) Mitral stenosis
2) Acute rheumatic fever
3) Hypothyroidism
4) Hyperparathyroidism

5) Wolff Parkinson White syndrome
The correct answer is choice A.
A broad, notched P wave is indicative of left atrial enlargement. This occurs in the setting of left heart strain, usually caused by uncontrolled hypertension. Other causes include mitral stenosis, obesity, atrial fibrillation, and lung disease.
Rheumatic fever (choice B) is an inflammatory cardiac process associated with streptococcal infection. ECG manifestations include heart block and prolonged PR interval.
Hypothyroidism (choice C) can cause QT prolongation, a right bundle branch block, and low voltage.
Hyperparathyroidism (choice D) is associated with hypercalcemia, which causes a short QT interval and wide T wave.
Wolff Parkinson White syndrome (choice E) is an abnormal cardiac conduction disease characterized by the "delta" wave, a slurred upstroke of the R wave.
You are working in the emergency department when one of your residents hands you the ECG of a patient that she was assessing.
The electrocardiogram showed which of the following:

1) Atrial fibrillation 2) Acute Anterior Wall MI 3) Right Atrial Enlargement 4) Inferior Posterior Apical STEMI 5) None of the above
The correct answer is choice D
ST segment is measured at the J point (which indicate the end of the QRS complex) using the TP line to the next TP line as a reference. In this ECG, there are ST segment elevations in the Inferior leads (Leads II, III, avF), ST segmnet depression at leads V1 and V2 which indicate posterior infarction and ST segment elevation in the apical leads (leads V4-V6). '
In cases of inferior infarction, the magnitude of the sum of ST depression in leads V1 and V2 add significant independand prognostic information. The presense of ST segment elevation in apical leads V4-V6 was associated with a large infarct size and poor priognostic outcome.

Atrial fibrillation (choice A) indicates irregular irregularity rhythm on an ECG. In this ECG, the rhythm is sinus and it is regular.
Acute Anterior Wall MI (choice B) means an ST segment elevation more than 2 mm in at least 2 leads between V1 to V4.
Right Atrial Enlargement (choice C) can be diagnosed sometimes as it can lead to initial deflection of the P wave which is not the case here.

A 55 year old male presents to your office as a new patient. He has a history of hypertension and a heart attack 5 years ago. He denies
recent complaints. You order a screening ECG as part of your work up.
The electrocardiogram below shows which of the following:

1) Left bundle branch block 2) Acute inferior wall myocardial infarction with reciprocal depression in the lateral leads 3) Mobitz II block 4) Left anterior hemiblockc 5) None of the above
The correct answer is choice D.
A left anterior hemiblock involves a conduction delay along the anterior fascicle of the left bundle branch, causing a left axis deviation, a QR in lateral limb leads, and a RS in inferior limb leads. Unlike a left bundle branch block, this will produce narrow complex QRS

complexes.
A left bundle branch block (choice A) is a wide complex rhythm.
An inferior wall MI (choice B) would show ST elevation and T wave abnormalities in inferior leads (III and AVF).
2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A 45 year old male presents to the emergency department with one hour of severe substernal chest pain. He has no past medical
history. His symptoms began while he was shovelling snow. You order an ECG and place the patient on oxygen and a cardiac monitor.
The electrocardiogram below shows which of the following:

1) Right Bundle Branch Block 2) Left Bundle Branch Block 3) Left anterior hemiblock 4) Right anterior hemiblock 5) None of the above

The correct answer is choice B.
This ECG demonstrates a left bundle branch block (LBBB), characterized by a wide QRS complex and ST segment abnormalities. In the setting of chest pain, a new LBBB requires emergency reperfusion therapy with a thrombolytic like tPA or an emergency angioplasty.
A right bundle branch block (RBBB) (choice A) is characterized by a rabbit ear appearance of the QRS complex in V1, the so-called R-S-R-prime morphology.
Hemiblocks (choices C and D) are incomplete branch blocks and have narrow QRS complexes.
The electrocardiogram below shows which of the following:
1. atrial flutter
2. left bundle branch block
3. 2:1 AV Block
4. 3:2 AV Block

1) 1,2,3 only 2) 1 and 3 only 3) 2 and 4 only 4) 4 only 5) all are correct
The correct answer is Choice B.
The ECG demonstrates a regular rhythm, with P waves that appear as saw-toothed pattern, also called flutter waves. Atrial flutter is characterized by a macro re-entrant arrhythmia with regular atrial rates between 240-400 beats per minute. Since the atrioventricular (AV) node cannot conduct at the same rate as the atrial activity, one commonly sees some form of conduction block, typically 2:1, 3:1 or 4:1. This block may also be variable and cause atrial flutter to appear as an irregular rhythm. The saw-tooth wave form of atrial flutter can usually be seen in the inferior leads II, III and aVF if one looks closely. Sometimes the rapid atrial rate can be seen in V1, however Strip Rhythm for leads II is the best to recognize the flutter waves, especially if increases the heart rate or decreases the heart rate (slows pulse), brings out flutter waves. Tachycardia may or may not be present, depending on the degree of AV block associated with the atrial flutter activity.

Patients at highest risk for atrial flutter include those with long-standing hypertension, valvular heart disease (rheumatic), left ventricular hypertrophy, coronary artery disease with or without depressed left ventricular function, pericarditis, pulmonary embolism, hyperthyroidism, and diabetes. Additionally, CHF for any reason is a noted contributor to this disorder, postoperative revascularization, digitalis toxicity are also noted. Rare cause - Myotonic dystrophy in childhood. There are 2 types of AF:
Type I atrial flutter, counterclockwise rotation with 4:1 AV nodal block.
Type I atrial flutter, also known as common atrial flutter or typical atrial flutter, has an atrial rate of 240 to 350 beats/minute.
The reentrant loop circles the right atrium, passing through the cavo-tricuspid isthmus - a body of fibrous tissue in the lower atrium between the inferior vena cava, and the tricuspid valve. Type I flutter is further divided into two subtypes, known as counterclockwise atrial flutter and clockwise atrial flutter depending on the direction of current passing through the loop.
Type II flutter follows a significantly different re-entry pathway to type I flutter, and is typically faster, usually 340-350 beats/minute. Narrow complex tachycardia at a rate of 150 is atrial flutter with 2:1 block until proven otherwise, as shown in the ECG above.
The other Choices, (choice A), (choice C), (choice D) and (choice E) are not the correct answers, as mentioned above.
A 50 year old male presents to your office complaining of several months of intermittent palpitations. While waiting in your office, he

states the symptom begins again. You obtain an ECG moments later.
The ECG shows which of the following conditions:
1) atrial fibrillation 2) torsades des pointes 3) Atrial flutter 4) ventricular tachycardia 5) Acute pericarditis
The correct answer is choice C.
Atrial flutter is a nodal reentry arrhythmia which occurs when atrial tachycardia is blocked from conduction to the ventricles by the AV node, resulting in a fixed rate often around 150 beats per minute. The ECG typically shows a sawtooth pattern, depending the ratio of P waves to QRS complexes.

Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.
Torsades des pointes (choice B) is a type of ventricular tachycardia that is associated with long QT syndrome, hypokalemia, and hypomagnesemia. It often degrades to ventricular fibrillation. Torsades des pointes appears as a crescendo, decrescendo of the QRS complex heights over several beats.
Ventricular tachycardia (choice D) is a wide complex tachycardia, it is a life threatening arrhythmia that requires cardioversion if symptomatic.
Acute pericarditis (choice E) is an inflammatory condition of the pericardium causing PR depression and diffuse ST elevation.
You are working a busy shift in the emergency department when the triage nurse brings you an ECG. He asks if the patient should be
brought back right away or if they can wait in the waiting room for a while. The ECG demonstrates sinus rhythm, a rate of 90 beats per
minute, a normal axis, and several ST segment depressions in anterior leads. You tell the nurse to bring the patient in right away.
Which of the following conditions may cause ST segment depression?
1) Ischemia 2) Hyperventilation 3) Ventricular Hypertrophy 4) Hypokalemia 5) All of the above
The correct answer is choice E.
ST depressions can be caused by several conditions, many of which are life threatening. ST depressions are most commonly associated

with ischemia, but they can also be seen in hypothermia, hypokalemia, digoxin toxicity, and hyperventilation syndrome.
Hypothermia may also demonstrate osborne waves.
Hypokalemia may also demonstrate a narrow QRS complex and flat T waves.
Digoxin toxicity will have a characteristic shape of the ST segment, often compared to the moustache of the artist Salvador Dali.
Hyperventilation syndrome can also demonstrate QT prolongation, ST elevation, and T wave inversion.
An 80 year old man is admitted to the hospital because of syncope. He suffers from chronic anemia with a low hemoglobin and heart
failure. The patient felt somewhat short of breath prior to admission and suddenly was observed to loose consciousness.
The electrocardiogram is done and shows which of the following:

1) sinus bradycardia 2) The rhythm is atrial flutter 3) The rhythm is atrial fibrillation. 4) The tracing reveals an acute inferior wall infarction. 5) The rhythm is a Junctional rhythm
The correct answer is choice B.
The rhythm is atrial flutter. Atrial flutter is due to a re-entry circuit in the right atrium with secondary activation of the left atrium. This produces atrial Contractions at rate of about 300 beats/min seen on the EKG as flutter (F) waves. These are broad and appear saw-toothed and are best seen in the inferior leads and in lead V1. The ventricular rate depends on conduction through the atrioventricular node. Typically 2:1 block (atrial rate to ventricular rate) occurs; giving a ventricular rate of 150 beats/min. Identification of regular tachycardia with this rate should prompt the diagnosis of atrial flutter. The non-conducting flutter waves are often mistaken for or merged with T waves and become apparent only if the block is increased. Manoeuvres that induce transient atrioventricular block may allow identification of flutter waves. The causes of atrial flutter are similar to those of atrial fibrillation, although idiopathic atrial flutter is uncommon. It may convert into atrial fibrillation over time or, after administration of drugs such as digoxin.

Sinus bradycardia (choice A) is not the correct answer. Sinus bradycardia is common in normal individuals during Sleep and in those with high vagal tone, such as athletes and young healthy adults. The electrocardiogram shows a P wave before every QRS complex, with a normal P wave axis (that is, upright P wave in lead II). The PR interval is at least 0.12 s. The heart rate in this trace ECG is around 65 (ventricular rate), while the atrial rate is almost 300bpm.
The rhythm is atrial fibrillation (choice C) is not the correct answer. Atrial fibrillation is caused by multiple re-entrant circuits or ―wavelets‖ of activation sweeping around atrial myocardium. These are often triggered by rapid firing foci. Atrial fibrillation is seen on the ECG as a wavy, irregular baseline made up of F (fibrillation) waves, and there is no recognised P wave can be seen especially in lead 2.
The rhythm is a Junctional rhythm (choice E) is not the correct answer. Any tachyarrhythmia arising from the atria or the atrioventricular junction is a supraventricular tachycardia. In clinical practice, however, the term supraventricular tachycardia is reserved for atrial tachycardias and arrhythmias arising from the region of the atrioventricular junction as a result of a re-entry mechanism (junctional tachycardias). During sinus rhythm the electrocardiogram is normal. During the tachycardia the rhythm is regular, with narrow QRS complexes and a rate of 130-250 beats/min. Atrial conduction proceeds in a retrograde fashion producing inverted P waves in leads II, III, and aVF. However, since atrial and ventricular depolarisation often occurs simultaneously, the P waves are frequently buried in the QRS complex and may be totally obscured.
A 40 year old female presents to your primary care office for medical clearance prior to an elective podiatric surgery. You order basic
blood work and an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Acute inferior wall myocardial infarction with reciprocal depression in the lateral leads 3) Mobitz II heart block 4) Left anterior hemiblock 5) None of the above
The correct answer is choice D.
A left anterior hemiblock (choice D) involves a conduction delay along the anterior fascicle of the left bundle branch, causing a left axis deviation, a QR in lateral limb leads, and a RS in inferior limb leads. Unlike a left bundle branch block, this will produce narrow complex QRS complexes.

Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.
An inferior wall MI (choice B) would show ST elevation and T wave abnormalities in inferior leads (III and AVF).
2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A 30 year old male receives an ECG as part of a pre-operative physical exam prior to an elective surgery. The ECG reveals ST elevation of 2mm in v1 and v2. The patient has no past medical history and denies any history of chest pain. All of the following are associated with ST segment elevations except?
1) Full thickness myocardial infarction 2) Early repolarization 3) Acute pericarditis 4) Ventricular aneurysm 5) Digoxin Effect
The correct answer is choice E.
The ST segment lies between the QRS complex and T wave in an ECG and occurs during systolic contraction of cardiac muscle.
Myocardial infarction (choice A) is a dangerous cause of ST elevation and should be treated with emergency reperfusion.
Early Repolarization (choice B) is a benign process often seen in young healthy males, and it is the most likely cause of the findings in this patient. The ST elevation caused by early repolarization demonstrates a higher "j-point" at the end of the QRS complex and lacks the

"tombstone" appearance of an ST Elevation MI. Nevertheless, it can sometimes be difficult to differentiate from myocardial ischemia.
Pericarditis (choice C) is an inflammatory process involving the pericardium, and is associated with diffuse ST elevation on ECG. There are many causes of pericarditis, and a few of these require emergency treatment.
Ventricular Aneurysms (choice D) are outpouching of cardiac muscle that can form after a previous myocardial infarction. They are associated with persistent ST elevations on ECG in the absence of active myocardial ischemia.
Digoxin Effect (choice E) is associated with a shortened QT interval and ST depression with a characteristic downsloping that has often been compared the moustache of Salvador Dali.
A 60 year old male with a history of smoking and asthma presents to your primary care office as a new patient for an annual physical.
You order blood work and a screening ECG.
The electrocardiogram below shows which of the following:

1) left ventricular hypertrophy 2) Left atrial enlargement 3) Right ventricular hypertrophy 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice C.
Right ventricular hypertrophy occurs as a result of pulmonary hypertension. The right ventricle's cardiac muscle expands in response to

this stress, causing a right axis deviation.
Left ventricular hypertrophy (choice A) is a common consequence of poorly controlled hypertension. The left ventricle's cardiac muscle changes in response to increased afterload. It is characterized by multiple ECG changes, principally increasing height of QRS complexes.
Left atrial enlargement (choice B) occurs as a result of mitral valve disease, aortic valve disease, or long standing hypertension. It is characterized by a widened QRS complex, often with a biphasic appearance. Right atrial enlargement (choice D) is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension.
A 70 year old male with a history of poorly controlled hypertension presents to the emergency department complaining of intermittent
chest pain. He is symptom free at the moment. You order an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Left atrial enlargement 3) Mobitz II heart block 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice B.
Left atrial enlargement occurs as a result of mitral valve disease, aortic valve disease, or long standing hypertension. It is characterized by

a widened QRS complex, often with a biphasic appearance.
Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.
A mobitz II (2nd Degree) heart block (choice C) is characterized by a fixed prolonged PR interval with intermittent skipped beats.
Right atrial enlargement (choice D) is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension.
A 60 year old male with an history of multiple myocardial infarctions, severe asthma, and pulmonary hypertension, presents to the
emergency department complaining of two days of dyspnea. His lungs are clear, without wheezing. You order an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Left atrial enlargement 3) Mobitz II heart block 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice D.
Right atrial enlargement is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension.

Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.
Left atrial enlargement (choice B) is characterized by widening of the P wave.
A mobitz II (2nd Degree) heart block (choice C) is characterized by a fixed prolonged PR interval with intermittent skipped beats.
A 35 year old female with a history of mitral stenosis presents to your office for a pre-operative medical clearance prior to an elective
gynecological surgery. You order blood work and a screening ECG.
The electrocardiogram below shows which of the following:
1) Left Ventricular Hypertrophy 2) Left axis deviation 3) Mobitz II heart block

4) Left atrial enlargement 5) None of the above
The correct answer is choice D.
Left atrial enlargement occurs as the atrium hypertrophies following strain, hypertension, or atrial fibrillation. It is characterized by a prolonged P wave, often with a notch.
Left ventricular hypertrophy (choice A) is characterized by large QRS complex height in prechordial leads.
Left axis deviation (choice B) is characterized by negative deflection in inferior ECG limb leads (e.g. AVF), and positive deflection in left sided limb leads (lead I).
2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
A 78 year old female presents to the emergency department complaining of chest tightness and dyspnea. She has a past medical history
of hypertension and osteoporosis, and she resides in a rehabilitation facility since she had her right hip replaced last week. On arrival she
is afebrile, tachycardic with a pulse of 115 beats per minute, and normotensive. You request an ECG and chest X-Ray.
All of the following regarding ECG changes in acute pulmonary thromboembolism are commonexcept:
1) Sinus tachycardia is the most common ECG finding 2) Righ Bundle Branch Block (RBBB) has been documented 3) Atrial fibrillation may be seen 4) The S1 Q3 T3 pattern 5) T wave inversion in anterior prechordial leads may be seen The correct answer is choice D.

A pulmonary embolism (PE) is a life threatening condition that occurs when a clot, usually from a deep vein thrombosis (DVT) from a lower extremity, blocks a terminal branch of the pulmonary artery in the lungs. Symptoms of a PE include chest pain, hemoptysis, syncope, dyspnea, and palpitations.
Risk factors for a PE are based on Virchow's triad of hypercoagulability and include smoking, hormone therapy (including oral contraception), recent immobilization, pregnancy, and genetic hypercoagulation disorders.
The most common ECG finding in a patient with a PE is sinus tachycardia (choice A), but an ECG can also be normal in these patients.
Other ECG findings include a right bundle branch block (RBBB) (choice B), atrial fibrillation (choice C), and T wave inversion (choice E).
Although the S1 Q3 T3 finding (choice D), caused by right heart strain is often associated with the condition, it is present in less than 20% of documented pulmonary embolisms. It is therefore not a common ECG finding.
A 90 year old female presents to the emergency department complaining of chest pain and weakness for several hours. Paramedics
report that she had periods of bradycardia en route. You order a stat ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Torsades des pointes 3) Mobitz II heart block 4) Complete (third degree) heart block 5) Acute pericarditis
The correct answer is choice D
This ECG shows a complete heart block. Also known as "AV dissociation," the atria and ventricles are beating on separate fixed rhythms and atrial beats are not conducted to the ventricles. Complete heart block is associated with life threatening bradycardia and requires emergent pacemaker placement.
Atrial fibrillation (choice A) occurs when atrial beats only intermittently conduct through the AV node causing a narrow complex ventricular beat. The pulse rhythm will be irregularly irregular and the ECG will demonstrate multiple P waves for every QRS complex, and variable heights of QRS complexes.

Torsades des pointes (choice B) is a type of ventricular tachycardia that is associated with long QT syndrome, hypokalemia, and hypomagnesemia. It often degrades to ventricular fibrillation. Torsades des pointes appears as a crescendo, decrescendo of the QRS complex heights over several beats.
2nd Degree Mobitz II block (choice C) is a heart block characterized by a fixed prolonged PR interval and periodic dropped beats.
Acute pericarditis (choice E) is an inflammatory condition of the pericardium causing PR depression and diffuse ST elevation.
A 52 year old woman with history of severe hyperparathyroidism presents to the emergency department with severe abdominal pain and
malaise. You suspect hypercalcemia and order blood work and an ECG.
All of the following ECG changes are associated with hypercalcemia except:
1) QRS interval may lengthen 2) PR interval is shortened 3) Shortening of the Q-T interval 4) T waves may flatten or invert 5) Variable degree of heart block may develop
The correct answer is choice B.
Hypercalcemia may produce ECG abnormalities related to altered trans-membrane potentials that affect conduction time. QT interval shortening is common, and, in some cases, the PR interval is prolonged. At very high levels, the QRS interval may lengthen, T waves may flatten or invert, and a variable degree of heart block may develop. Digoxin effects are amplified.
Hypercalcemia is caused by

Primary hyperparathyroidism (main outpatient cause)
Malignancy: PTHrP, osteolytic, calcitriol (main inpatient cause)
Granulomatous diseases
Drugs: milk-alkali, vitamin D, thiazides, lithium
Endocrine: hyperthyroidism, adrenal insufficiency
Paget’s
Immobilization
Familial hypocalciuric hypercalcemia
ESRD and tertiary hyperparathyroidism

Manifestations:
GI: constipation, PUD, pancreatitis
Renal: stones, DI, RTA (type I), tubular toxicity (nephrocalcinosis)
Cardiovascular: QT short, HTN
Myalgias, weakness
Neuro: confusion, coma
Helpful findings:
Level: higher with malignancy, rarely >11 or 12 with primary hyperparathyroidism
Serum PO4: low with humeral hypercalcemia of malignancy (PTHrP) or hyperparathyroidism

Urine calcium: high or high normal with hyperparathyroidism and malignancy, low with milk alkali (due to metabolic
alkalosis), thiazides, and FHH
Serum Cl: high in hyperparathyroidism
Treatment usually depends on the underlying cause, but often includes IV hydration, diuretics, bisphosphonates, and dialysis.

A 63-year-old man is brought to the emergency department complaining of palpitations which developed suddenly that day. He has a past
medical history of hypothyroidism and anemia. You order an ECG.
The electrocardiogram below shows which of the following:

1) Left ventricular hypertrophy by voltage 2) First degree atrio-ventricular block 3) Left anterior fascicular block 4) Complete right bundle branch block 5) None of the above
The correct answer is choice B.
This ECG demonstrates tachycardia and a 1st degree AV block, characterized by a prolonged PR interval (larger than 1 large box, or 0.20 seconds).
Left ventricular hypertrophy (choice A) is characterized by R or S waves in limb leads greater than 20mm, or in prechordial leads greater than 30mm.
A left anterior fascicular block (choice C) is characterized by a left axis deviation, QR pattern in I and AVL, and RS pattern in II, III, and

AVF.
A right bundle branch block (choice D) will have a prolonged QRS duration greater than 120 msec and usually has the classic R-S-R-prime morphology in V1 or V2.
A 75 year old male with a history of coronary artery disease presents to your primary care office for an annual physical. You order
screening blood work and an ECG.
The electrocardiogram below shows which of the following:

1) Left Bundle Branch Block 2) Right Bundle Branch Block 3) Left Anterior Fascicular Block 4) Right Bundle Branch Block & Left Anterior Fascicular Block 5) Right Bundle Branch Block & Left Posterior Fascicular Block
The correct answer is choice B.

A right bundle branch block is characterized by a R-S-R-prime morphology in V1 and a slurred upstroke of the S wave in V6.
A left bundle branch block (choice A) is characterized by a wide complex, Q-S morphology in lead V1.
A left anterior fascicular block (choices C & D) is characterized by a left axis deviation, Q-R in I and AVL, and R-S in inferior leads (II, III, and AVF). The QRS duration is usually normal.
A left posterior fascicular block (choice E) is characterized by an extreme right axis deviation.
A 56 year old woman presents to the emergency department because of chest pain. She has a history of hypercholesterolemia, migraine
headaches, obesity and hypertension. The chest discomfort does not radiate to the arms or back but seems to move in the direction of the
epigastric area.
The electrocardiogram is done and shows which of the following:

1) There are signs of acute inferior wall infarction. 2) There are signs of acute pericarditis. 3) There are signs of sinus bradycardia and first degree AV block 4) There are signs of sinus arrhythmia. 5) None of the above are true
The correct answer is choice C. There are signs of sinus bradycardia and first degree AV block. There are many stepwise approaches for diagnosis of various cardiac rhythms, one way to interpret the ECG systematically is:
Rate and Rhythm: if it is Fast or Slow. HR can be calculated by counting the number of large squares between two consecutive R waves, and dividing this number into 300. In this case it is around 60 which is bradycardic and regular as the same QRS intervals are repeatedly repeated at the same time cycle. Here the P wave is present which means sinus rhythm.

The QRS complex: is narrow within the normal range for the normal ECG.
Relationship of p to QRS: every P wave is p followed by QRS which is normal. From above, it shows that this is sinus bradycardia. First degree AV block is: prolonged PR >0.20 sec, but does not vary (fixed) and the P wave's size and shape is normal. The Rate in First-degree heart block can be seen with both sinus bradycardia and sinus tachycardia. QRS complex: narrow; ≤ 0.10 sec in absence of intraventricular conduction defect.
There are signs of acute inferior wall infarction (choice A) is not the correct answer. There are no signs of Acute Inferior Wall MI in the ECG. There is no ST elevation, upright and peaked waves in II, III and aVF.
There are signs of acute pericarditis (choice B) is not the correct answer. In pericarditis, the ST segment elevation is diffuse rather than localised, often being present in all leads except aVR and V1. The elevated ST segments are concave upwards, rather than convex upwards as seen in acute infarction. Depression of the PR segment may also be seen. Those criteria are not present in this trace ECG.
A sign of sinus arrhythmia (choice D) is not the correct answer. Sinus arrhythmia is the variation in the heart rate that occurs during inspiration and expiration. There is ―beat to beat‖ variation in the R-R interval, the rate increasing with inspiration.
A 78 year old man with advanced renal disease comes to your office with generalized fatigue, weakness and sudden onset of palpitations.
He denies chest pain but does complain of some shortness of breath. You order an immediate ECG with the results shown below.
What is the most likely diagnosis in this case:

1) Hyperkalemia 2) Hypercalcemia 3) Hypernatremia 4) Pericarditis 5) ventricular aneurysm
The correct answer is Choice A
Hyperkalemia (choice A) is the correct answer. Hyperkalemia is defined as a potassium level greater than 5.5 mEq/L.1 Ranges are as follows:
5.5-6.0 mEq/L - Mild
6.1-7.0 mEq/L - Moderate

7.0 mEq/L and greater - Severe
Hyperkalemia is an electrolyte impalance that usualluy occur in renal impairmant due to decrease potassium excretion from kidney.The first ECG sign of hyperkalemia is peaked T waves and usually appears once K level go around 6 meq/L.
The ECG shows hyperacute T wave which means the T waves become large and 'tented' with narrow base and wide QRS complex. Hyperkalemia is a common cause of electrolyte induced cardiac conduction disturbance.
Any level over 6 mEq/L can be life-threatening, depending on the clinical setting. Pseudohyperkalemia may be seen following an artificial rise in potassium values due to potassium exiting from cells immediately before and after venipuncture. This can be occur with hemolysis or prolonged use of a tourniquet. It can also be found when there is significant leukocytosis or thrombocytosis. Pseudohyperkalemia can be ruled out by checking a plasma as opposed to serum potassium level. The plasma level should be normal if pseudohyperkalemia is present.
True hyperkalemia may occur as a result of insufficient elimination, medications or excess intake. Hyperkalemia due to inadequate removal of potassium may be viewed in several ways. In renal insufficiency, potassium filtration is decreased due to a reduction in the glomerular filtration rate (GFR). Hyporeninemic hypoaldosteronism is seen in mild renal insufficiency, diabetes and patients with chronic tubulointerstitial nephritis. The lack of aldosterone leads to hyperkalemia. Aldosterone synthesis is also decreased in primary adrenal disease or Addisons disease. This should be suspected if the sodium is low or if there are orthostatic blood pressure changes. Elevated potassium levels can occur due to renal tubules being unresponsive to aldosterone. Aldosterone levels will frequently be in the normal range. This is seen with sickle cell anemia, amyloidosis and renal transplantation.
Medications can affect potassium levels, especially if the patient has renal disease or hypoaldosteronism. The percent affected ranges from 1.3 – 10%. Medications that affect potassium can be separated into four groups:

Potassium sparing diuretics
Nonsteroidal anti-inflammatory agents (NSAIDs)
ACE inhibitors
Miscellaneous
Patients can also receive a potassium load from tissue breakdown, dietary noncompliance in renal patients or intracellular potassium shifts. Tumor lysis syndrome or rhabdomyolysis can provide a high potassium load. As long as urine output is adequate and renal function is preserved, hyperkalemia usually does not occur. Exercise and trauma can lead to high potassium due to release of potassium from tissue. Shifts of potassium can also be found in acidosis or digoxin toxicity. Hemolysis is another source of potassium and in significant hemolysis acute renal failure can develop further decreasing the excretion of potassium. Red cell transfusions using older units of blood can be a significant load of potassium. This is usually only significant with a decrease in renal function. However, transfusion on hemodialysis does not require ―fresh‖ units as was once thought to be necessary for patients with end-stage renal disease.
Cardiac disturbances include sinus bradycardia, slow idioventricular rhythm, ventricular tachycardia, ventricular fibrillation, and asystole. The EKG changes seen include peaked T waves3, prolongation of PR interval, second-degree AV block, loss of p waves and intraventricular conduction defects. Lastly T wave and widened QRS complexes form a ―sine-wave‖ pattern that can precede asystole. EKG changes however do not develop in a characteristic pattern. Clinically significant arrhythmias including ventricular arrhythmias can occur at any time. The EKG is an insensitive test to identify hyperkalemia.
Hypercalcemia (choice B) causes shortening of the QT interval. Severe Hypercalcemia induces ST-segment elevation mimicking acute

myocardial infarction.
Choice C Isolated hypernatremia has no consistent effect on the ECG.
Choice D pericarditis the ECG shows diffuse ST segment changes.
Choice E Ventricular aneurysm indicate a condition that usually complicatea Acute MI. ECG shows ST segment elevation in pericordial leads V1 to V4.
Table 1: Etiologies of Hyperkalemia Summary

A 28 year old obese male presents to your cardiology office after being referred by his primary care provider. His physician was
concerned with his ECG and complaints of dyspnea on exertion.
All of the following are causes of prominent R wave in Lead V1 EXCEPT:
1) Posterior wall myocardial infarction. 2) Right bundle branch block 3) Right ventricular hypertrophy 4) Wolff-Parkinson-White Syndrome type A. 5) Wolff-Parkinson-White Syndrome type B.

The correct answer is choice E.
Wolff Parkinson White syndrome is a rare cardiac conduction abnormality caused by an accessory conduction pathway. It is usually characterized by a slurred upstroke of the QRS complex, described as the "delta wave." Type A WPW (choice D) has a predominantly positive deflection (with a tall R wave) in lead V1, while type B WPW will have a predominantly negative deflection (no tall R wave in V1).
A posterior myocardial infarction (choice A) is a rare type of heart attack that is difficult to diagnose on an ECG. It is characterized by right ventricular hypertrophy and a prominent R wave in V1.
A right bundle branch block (choice B) is characterized by a prolonged QRS interval with characteristic and prominent R-S-R-prime morphology in V1.
Right ventricular hypertrophy (choice C) is characterized by a tall R wave V1 and a right axis deviation among other findings.
A 50 year old male with a history of chronic obstructive pulmonary disease (COPD) presents to your cardiology practice with an ECG
performed at his primary care provider's office. His primary doctor requests a cardiology evaluation.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Left atrial enlargement 3) Mobitz II heart block 4) Right Atrial Enlargement 5) None of the above
The correct answer is choice D.

Right atrial enlargement is characterized by increasing height of the P wave, especially in II, III, and AVF. It can be caused by anything that puts strain on the right atrium, e.g. tricuspid valve disease and pulmonary hypertension.
Atrial fibrillation (choice A) is characterized by multiple P waves occasionally and irregularly progressing to a ventricular beat's QRS complex.
Left atrial enlargement (choice B) is characterized by widening of the P wave.
A mobitz II (2nd Degree) heart block (choice C) is characterized by a fixed prolonged PR interval with intermittent skipped beats.
A 60 year old male presents to the emergency room with a fever, cough, and chest pain. His chest X-ray reveals a pneumonia and you
initiate antibiotics. You also order blood work and an ECG.
The electrocardiogram below shows which of the following:
1) Normal rhythm 2) Second degree AV block 3) Third degree AV block 4) First degree AV block 5) None of the above
The correct answer is choice D.

A 1st degree AV block is characterized by a prolonged PR interval with no dropped beats. The normal PR interval is 120 to 200 msec long, or about one large box wide. The PR interval is measured between the start of the P wave and the start of the QRS complex.
A 2nd degree AV block (choice B) is characterized by a prolonged PR interval and dropped beats.
A 3rd degree, or complete, AV block (choice C) is characterized by complete AV dissociation, so the atria and ventricles each beat on their own independent rates.
The electrocardiogram below shows which of the following:
1) Complete heart block 2) Left bundle branch block 3) infero-posterior infarct and trifasciular block 4) Acute posterior infarct 5) 2nd degree heart block

The correct answer is choice C.
Infero-posterior infarct and trifasciular block is the correct answer. Trifascicular block is present when bifascicular block is associated with first degree heart block. If conduction in the dysfunctional fascicle also fails completely, complete heart block ensues. Bifascicular block is the combination of right bundle branch block and left anterior or posterior hemi block. The electrocardiogram shows right bundle branch block with left or right axis deviation (in this trace ECG there is left axis deviation). In summary Trifascicular block has three features:
Prolongation of the PR interval (first degree AV block)
Right bundle branch block
Either left anterior fascicular block or left posterior fascicular block
The infero-posterior infarct is characterized by ST segment elevation in leads II, III, and aVF. Because a 12-lead EKG looks primarily at the front of the heart, no leads face an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall. As we can see in this trace ECG:
Complete heart block (choice A) is not the correct answer. In third degree block, there is complete failure of conduction between the atria and ventricles, with complete independence of atrial and ventricular contractions. The P waves bear no relation to the QRS complexes and usually proceed at a faster rate. This is not the case here.

Left bundle branch block (choice B) is not the correct answer.
Acute posterior infarct choice D is not the correct answer.
2nd degree heart block (choice E) is not the correct answer. In second degree block, there is intermittent failure of conduction between the atria and ventricles. Some P waves are not followed by a QRS complex. There are 2 types of second degree block. Mobitz type I block (Wenckebach phenomenon) is usually the initial PR interval is normal but progressively lengthens with each successive beat until eventually atrioventricular transmission is blocked completely and the P wave is not followed by a QRS complex. Mobitz type II block is less common but is more likely to produce symptoms. There is intermittent failure of conduction of P waves. The PR interval is constant, though it may be normal or prolonged.
A 45 year old male with a history of hypertension and renal failure presents with palpitations and chest pain. His ECG reveals a prolonged
QT interval.
Causes of long QT Syndrome include all of the following except:
1) Hypokalaemia 2) Hypocalcaemia 3) Hypomagnesaemia 4) Hypermagnesaemia 5) Rheumatic carditis
The correct answer is choice D.
Long QT syndrome is a rare heart condition whereby the repolarization of the cardiac muscle after systole is delayed. This delay can cause life threatening arrhythmias including torsades de pointes and ventricular fibbrilation. There are many causes of long QT syndrome including medication side effects, inherited disorders, and electrolyte imbalances.

Hypokalemia (choice A) causes a prolonged QT interval, inverted T waves, and a U wave.
Hypocalcemia (choice B) causes a prolonged QT interval.
Hypomagnesaemia (choice C) causes a prolonged QT interval, flat T waves, and a prolonged PR interval.
Hypermagnesaemia (choice D) causes a short QT interval, heart blocks, peaked T waves, and QRS complex widening.
Rheumatic carditis (choice E) involves cardiac valve damage that occurs after rheumatic fever, which is caused by Group A streptococcus. ECG findings associated with this condition include long QT interval, heart blocks, and a prolonged PR interval.
A 58 year old female presents to the emergency room complaining of weakness and dizziness. You order blood work and an ECG. She
has a past medical history of coronary artery disease and multiple heart attacks in the past. She hands you a note from her cardiologist
that indicates she also has a ventricular aneurysm.
Ventricular aneurysm has which one of the following characteristic features on ECG:
1) Persistent ST segment elevation 2) Persistent ST segment depression 3) Left bundle branch block 4) Right bundle branch block 5) ALL of the above
The correct answer is choice A.

Ventricular aneurysms can cause persistent ST elevations on an ECG. Patients with undiagnosed ventricular aneurysms are often thought to be having an ST elevation MI when they are evaluated, and are often unnecessarily thrombolyzed or taken for angioplasty. They are often associated with past myocardial ischemia.
Aneurysms are not usually associated with ST depression, LBBB, or RBBB.
A 60-year-old male patient presents with a several hour history of palpitations, shortness of breath, and fatigue. The patient indicates that

his palpitations are felt as irregular heartbeats, occasionally rapid, and sometimes associated with lightheadedness. As you are
interviewing the patient, he states that it is becoming more and more difficult to breath, and now his chest hurts. The patient is placed on
a monitor and you see the following tracing.
The rhythm strip shows the following:
What is the most appropriate treatment to perform immediately.
1) IV Magnesium 2) Oral aspirin and IV heparin 3) IV Lidocaine 4) Sychronized cardioversion 5) Transcutaneous electrical pacing
The correct answer is choice D.
The ECG shows ventricular tachycardia. If the patient appears unstable in any way they will require immediate synchronized cardioversion. If he loses his pulse he will require immediate defibrillation.
Signs of instability include chest pain, shortness of breath, hypotension, and cyanosis.
IV magnesium (choice A) is indicated in cases of polymorphic ventricular tachycardia, also known as Torsades de pointes.

Asprin and heparin (choice B) are indicated in cases of suspected myocardial infarction. This patient's chest pain may be ischemic, but it is a result of hypoperfusion from the ventricular tachycardia so the malignant rhythm must be treated first.
IV antiarrhythmics (choice C) are indicated in "stable" forms of ventricular tachycardia, and amiodarone (not lidocaine) is currently a commonly used medication in this circumstance. This patient has signs of unstable tachycardia so must be cardioverted without delay.
Electrical pacing (choice E) is used for cases of symptomatic bradycardia, not tachycardia.
A 30 year old female presents to the emergency room complaining of palpitations. She denies drug use or any past medical history. You
order an ECG.
The electrocardiogram below shows which of the following:

1) 1st Degree AV Block 2) Type I 2nd Degree AV Block 3) Type II 2nd Degree AV Block 4) 3rd Degree AV Block 5) WPW Preexcitation Syndrome
The correct answer is choice E.
This ECG demonstrates Wolf Parkinson White syndrome, a rare cardiac conduction abnormality characterized by an abnormal reentry pathway that bypasses the AV node. An ECG will demonstrate the "delta wave," a slurred upstroke of the R wave. WPW is associated with sudden death as a result of malignant tachyarrhythmias that can develop as a result of the accessory conduction pathway. Nodal blocking agents like calcium channel and beta blockers should be avoided since they will inhibit the AV node, which in the case of WPW and an underlying atrial fibrillation will lead to the conduction of all atrial beats down the abnormal pathway.
A 1st degree AV block (choice A) is characterized by a fixed prolonged PR interval without any dropped beats.
A type I second degree AV block (choice B) has a PR interval that gradually prolongs until it skips a beat, then the PR interval resets to it's initial length. A type II second degree AV block (choice C) has a fixed PR interval with an intermittently skipped beat.
A 3rd Degree AV block (choice D) is also known as AV dissociation. It is characterized by the atria and ventricles beating at their own fixed and separate rates.
The electrocardiogram below shows which of the following:

1) Poor R wave progression 2) Diffuse non-specific ST-T wave changes 3) Hyperacute anteroseptal MI 4) Fully evolved anteroseptal MI 5) Left ventricular hypertrophy with strain

The correct answer is choice D.
Fully evolved anteroseptal MI is the correct choice. An anterior wall MI is caused by occlusion of the left anterior descending coronary artery (LAD). An anterior wall MI can be seen in the anterior chest leads, from V1 to V4 and it is diagnostic; if leads V1-V2 are involved, it is termed antero-septal MI. In a fully evolved antero-septal MI, the ST is still elevated and the T wave is upright in the chest leads V1 to V4 and Q waves have appeared in the same leads. This is the appearance of the above tracing.
Poor R wave progression (choice A) is not the correct answer. From V1 to V3, there is poor progression, however the R wave returns to it is normal progression in V4, V5 and V6.
Diffuse non-specific ST-T wave changes (choice B) is not the correct answer. Nonspecific ST-T wave abnormalities are very common and may be seen in any limb or precordial lead of the electrocardiogram, they may be present only in the inferior, lateral, or anterior leads. The types of abnormalities are varied and include straightening of the ST segment, ST segment depression or elevation, flattening of the T wave, or T wave inversion. It is clear here that there is symmetrical ST elevation from V1 until V4.
Hyper-acute anteroseptal MI (choice C) is not the correct answer. As further elevation occurs, the ST segment tends to become convex upwards. Serial electrocardiograms show evolving changes that tend to follow well recognised patterns. Hyper-acute T waves: T waves become more prominent, symmetrical, and pointed (―hyperacute‖). These changes in T waves are usually present for only five to 30 minutes after the onset of the infarction and are followed by ST segment changes. And the rise in the ST did not exceed 1 mm as in this case.
An 88 year old female is brought to the emergency department complaining of dyspnea. She has a history of coronary artery disease and
a myocardial infarction 2 years ago. 1 year ago she had a stroke and she has residual left sided hemiparesis. On examination, her vital
signs are: pulse 85 beats per minute, blood pressure 130/80, temperature 96.2 deg F (35.2 deg C), her pulse is irregular, and her lung
exam reveals rales in both bases. You order a chest x-ray and an ECG.
Her ECG shows which of the following:

1) Acute inferior wall infarction 2) Sinus bradycardia with PAC’s 3) Atrial fibrillation with controlled ventricular response 4) Left anterior fascicular block 5) Left posterior fascicular block
The correct answer is choice C.
This ECG demonstrates atrial fibrillation. Her ventricular rate is between 75 and 100 beats per minute, so she is not in "rapid afib," but rather in a "rate controlled afib." Atrial fibrillation may be paroxysmal (intermittent), so this diagnosis may not have been noted by any of her previous physicians. A history of untreated atrial fibrillation is a risk factor for thromboemolic events like myocardial infarctions and strokes.
An inferior wall infarction (choice A) will show ischemic changes (e.g. ST elevation or T wave abnormalities) in inferior limb leads (II, III,

AVF).
Bradycardia (choice B) is usually defined as a ventricular rate less than 60 beats per minute.
A left anterior fascicular block (choice D) is a partial left bundle branch block characterized by a normal QRS duration, left axis deviation, a QR in lateral limb leads and an RS in inferior limb leads.
A left posterior fascicular block (choice E) is a partial left bundle branch block characterized by an extreme right axis deviaiton. It is not as common as a left anterior fascicular block.
A 65 year old male with a history of a myocardial infarction 3 years ago presents to your primary care office complaining of palpitations.
You order blood work and a screening ECG.
The electrocardiogram below shows which of the following:
1) 1st Degree AV Block 2) Type I 2nd Degree AV Block 3) Type II 2nd Degree AV Block 4) 3rd Degree AV Block 5) None of the above
The correct answer is choice B.

A 2nd degree AV block is characterized by a prolonged PR interval and dropped beats. A type I 2nd degree AV block has a PR interval that becomes more prolonged with each beat, then resets after a dropped beat. A type II 2nd degree heart block (choice C) has a fixed PR interval and intermittent dropped beats. The type II 2nd degree block is considered more unstable since it can progress to a 3rd degree heart block without warning.
A 1st degree AV block is characterized by a prolonged PR interval with no dropped beats. The normal PR interval is 120 to 200 msec long, or about one large box wide. The PR interval is measured between the start of the P wave and the start of the QRS complex.
A 3rd degree, or complete, AV block (choice D) is characterized by complete AV dissociation, so the atria and ventricles each beat on their own independent rates.
A 45 year old male smoker presents to the emergency room complaining of one hour of crushing, substernal chest pain. He has a past
medical history of uncontrolled diabetes and hypertension. You order an ECG.
The electrocardiogram below shows which of the following:

1) Atrial fibrillation 2) Acute Anterior Wall MI 3) Acute Inferior Wall MI 4) \Right Atrial Enlargement 5) None of the above
The correct answer is choice B.
This ECG demonstrates ST elevation in anterior prechordial leads, V1-3 with reciprocal changes (ST depression) in inferior limb leads (II, III, and AVF). An ST elevation myocardial infarction is an indication for emergency reperfusion therapy, either with a thrombolytic like tPA or with angioplasty.
Atrial fibrillation (choice A) is an irregularly irregular rate with multiple P waves for every QRS complex.
An inferior wall MI (choice c) will demonstrate ST elevation or other ischemic changes primarily in inferior limb leads (II, III, and AVF).

Right atrial enlargement (choice D) will demonstrate an increased height of the P wave.
A 60 year old male presents to your primary care office complaining of one month of intermittent palpitations. He has no known medical
problems and does not take any medications. You order blood work and a screening ECG.
The electrocardiogram below shows which of the following:
1) 1st Degree AV Block 2) Type I 2nd Degree AV Block 3) Type II 2nd Degree AV Block 4) 3rd Degree AV Block 5) None of the above
The correct answer is choice C.
A 2nd degree AV block is characterized by a prolonged PR interval and dropped beats. A type I 2nd degree AV block (choice B) has a PR interval that becomes more prolonged with each beat, then resets after a dropped beat. A type II 2nd degree heart block (choice C) has a fixed PR interval and intermittent dropped beats. The type II 2nd degree block is considered more unstable since it can progress to a 3rd

degree block without warning.
A 1st degree AV block (choice A) is characterized by a prolonged PR interval with no dropped beats. The normal PR interval is 120 to 200 msec long, or about one large box wide. The PR interval is measured between the start of the P wave and the start of the QRS complex.
A 3rd degree, or complete, AV block (choice D) is characterized by complete AV dissociation, so the atria and ventricles each beat on their own independent rates.
A 35 year old pregnant female presents to the emergency room brought in by ambulance after an unwitnessed cardiac arrest. As per a
family member, she has no past medical history but was complaining of mild chest pain and dyspnea for several days. Given the patient
history, you suspect a pulmonary embolism.
A pulmonary embolism usually presents with any of the following electrocardiogram manifestations EXCEPT:
1) Sinus tachycardia 2) S1Q3T3 pattern 3) T-wave inversion 4) Left bundle branch block 5) Right bundle branch block
The correct answer is choice D.
A pulmonary embolism (PE) is a life threatening condition that occurs when a clot, usually from a deep vein thrombosis (DVT) from a lower extremity, blocks a terminal branch of the pulmonary artery in the lungs. Symptoms of a PE include chest pain, hemoptysis, syncope, dyspnea, and palpitations. A massive pulmonary embolism can cause sudden death.
Risk factors for a PE are based on Virchow's triad of hypercoagulability and include smoking, hormone therapy (including oral

contraception), recent immobilization, pregnancy, and genetic hypercoagulation disorders.
The most common ECG finding in a patient with a PE is sinus tachycardia (choice A), but an ECG can also be normal in these patients.
Other ECG findings include a right bundle branch block (RBBB) (choice E) and T wave inversion (choice C).
Although the S1 Q3 T3 finding (choice B), caused by right heart strain often associated with the condition, is associated with the disease, it is present in less than 20% of documented pulmonary embolisms.
Left bundle branch block (choice D) is an unlikely finding in a patient with a massive pulmonary embolism.
The electrocardiogram below shows which of the following:

1) sinus rhythm with a recent Q-wave anterior wall myocardial infaraction 2) sinus rhythm with incomplete left bundle branch block 3) sinus rhythm with acute inferior myocardial infarction 4) Bifascicular Block (RBBB + LAFB) 5) complete left bundle branch block
The correct answer is choice D.
Bifascicular Block (RBBB + LAFB) is the correct choice. Bifascicular block is the combination of right bundle branch block and left anterior or posterior hemiblock. The ECG trace shows a right bundle branch block with left axis deviation. Right bundle branch block with left anterior hemiblock is the commonest type of bifascicular block. This tracing shows a sinus rhythm at 100/minute. The PR interval is 180 ms. The QRS interval duration of 260 ms indicates a conduction defect. There is an M shaped QRS complex (rSR' variant) in leads V1 to V3. In addition there are S waves in leads I, aVL, V5 and V6. There are also prominent S waves proceeded and small R waves in II, III and aVF . The QRS also has a left axis deviation. These findings indicate the presence of a bifascicular block, right bundle branch and left anterior hemiblock.

Sinus rhythm with a recent Q-wave anterior wall myocardial infaraction (choice A) is not the correct answer. In this trace, there is no development of Pathological Q waves. As the acute myocardial infarction evolves, changes to the QRS complex include loss of R wave height and the development of pathological Q waves. Both of these changes develop as a result of the loss of viable myocardium beneath the recording electrode, and the Q waves are the only firm electrocardiographic evidence of myocardial necrosis. Q waves may develop within one to two hours of the onset of symptoms of acute myocardial infarction, though often they take 12 hours and occasionally up to 24 hours to appear. When there is extensive myocardial infarction, Q waves act as a permanent marker of necrosis. With more localized infarction, the scar tissue may contract during the healing process, reducing the size of the electrically inert area and causing the disappearance of the Q waves.
A 40 year old male presents to your cardiology office complaining of one month of intermittent chest pain. He was told by several
physicians that his ECG was "normal." You order an ECG.
The electrocardiogram below shows which of the following:

1) RBBB 2) LBBB 3) Left anterior hemiblock 4) Right anterior hemiblock 5) None of the above

The correct answer is choice C.
A left anterior hemiblock is a left branch block affecting only the anterior fascicle of the bundle. It is characterized by a narrow complex QRS, left axis deviation, QR in I and AVL, and RS in II, III, and AVF.
A right bundle branch block (RBBB) (choice A) is characterized by a wide complex, rabbit ear appearance of the QRS complex in V1, the so-called R-S-R-prime morphology.
A left bundle branch block (LBBB) (choice B) is characterized by a wide QRS complex and ST segment abnormalities. In the setting of chest pain, a new LBBB requires emergency reperfusion therapy with a thrombolytic like tPA or an emergency angioplasty.
A right anterior hemiblock (choice C) is not a commonly used term since the right bundle branch consists of only one fascicle.
A 50 year old male presents to your primary care office. He has no past medical history. He states that over the past one month, he has
felt mild discomfort in his chest for a few moments at a time. You order an ECG and notice several Q waves.
What can help to differentiate between the normal septal Q wave and a pathologic Q wave?
1) The width 2) The height 3) Both width and height 4) The QRS axis 5) ECG leads involved
The correct answer is choice E.
Leftward regions of the heart will produce an initial negative deviation on an ECG, producing a "septal" Q wave that is not indicative of

ischemia. Leads I, AVF, and V5-6 are associated with normal septal Q waves.
Pathologic Q waves are found in II, III, AVF (can be septal), and anterior prechordial leads (V1-4).
The height of the Q (choice B) may indicate likelihood of ischemia, but location is the most important differentiating factor.
The axis (choice D) will not help to differentiate Q wave origin.

A 35 year old female presents to your office complaining of several years of intermittent palpitations. Although she has not felt the
palpitations for several days, her older brother died suddenly of "unknown causes" several years ago and she is nervous that her
palpitations may be dangerous. Her ECG in your office demonstrates a QTc of 550 mSec, consistent with a diagnosis of long QT
syndrome.
Causes of long QT Syndrome include all of the followings except:
1) Inherited Syndromes 2) Hypokalemia 3) Hypercalcemia

4) Rheumatic carditis 5) Class Ic and III antiarrhythmics
The correct answer is choice C.
Long QT syndrome is a rare heart condition whereby the repolarization of the cardiac muscle after systole is delayed. This delay can cause life threatening arrhythmias including torsades de pointes and ventricular fibrillation. There are many causes of long QT syndrome including medication side effects, inherited disorders, and electrolyte imbalances.
Inherited syndromes (choice A) can cause prolonged QT syndrome via genetic abnormalities related to cardiac muscle ion channels.
Hypokalemia (choice B) is associated with prolongation of the QT interval, inverted T waves, and U waves.
Hypercalcemia (choice C) is associated with a short QT interval, not a long QT interval.
Rheumatic carditis (choice D) involves cardiac valve damage that occurs after rheumatic fever, which is caused by Group A streptococcus. ECG findings associated with this condition include long QT interval, heart blocks, and a prolonged PR interval.
Drugs (choice E) that cause long QT syndrome include antibiotics, antihistamines, antipsychotics, and antiarrhythmics .
Table 1: Classification of antiarrhythmic drug actions

The electrocardiogram below shows which of the following:

1) Inferior MI with RBBB 2) Posterior MI with LBBB 3) Inferoposterior MI 4) Inferoposterior MI with RBBB 5) None of the above
The correct answer is choice D.
Inferoposterior MI with RBBB is the correct choice. An inferior wall MI is usually due to occlusion of the right coronary artery (RCA). This is seen on the EKG as ST segment elevation in leads II, III, and aVF. Because a 12-lead EKG looks primarily at the front of the heart, no leads face an infarction in the posterior wall. But an injury in this area is indicated on EKG by what are called reciprocal changes—ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall as seen in this ECG, and the sign of RBBB the QRS duration >0.12 s, a secondary R wave (R) in V1 or V2, and wide slurred S wave in leads I, V5, and V6. Some times you will find associated features with RBBB and ST segment depression and T wave inversion in the right precordial leads as seen in this trace ECG.
Inferior MI with RBBB (choice A), Inferoposterior MI (choice C) and none of the above (choice E) are not the correct answers. In this EKG, mild ST segment elevation in leads II, III, and aVF and RBBB are seen and this indicates Inferior MI with RBBB. However we can also see, ST segment depression accompanied by tall, upright R waves and tall, symmetrical T waves in leads V1 - V3, which are the leads that face the anterior wall which means Posterior MI with RBBB as well.

Posterior MI with LBBB (choice B) is not the correct answer. As diagnosis criteria for (left bundle branch block) LBBB includes:
QRS duration of >0.12 s.
Broad monophasic R wave in leads 1, V5, and V6.
Absence of Q waves in leads V5 and V6.
Associated features; Displacement of ST segment and T wave in an opposite direction to the dominant deflection of the QRS complex (appropriate discordance), Poor R wave progression in the chest leads, RS complex, rather than monophasic complex, in leads V5 and V6.
A patient with a history of pulmonary hypertension and cardiomegaly presents to your cardiology office for an annual exam. His ECG
shows a right axis deviation and you suspect right ventricular hypertrophy.
When interpreting an ECG, right ventricular hypertrophy (RVH) can mimic which of the following conditions?
1) Left Bundle Branch Block 2) AV block 3) True posterior Infarction 4) Left anterior fascicular block 5) Left posterior fascicular block
The correct answer is choice C.

A posterior MI is often confused with right ventricular hypertrophy. Both will have tall R waves in right sided leads. RVH will have a concurrent right axis deviation. A posterior MI will have tall R waves in V1 and V2 without right axis deviation. If your suspicion is high for a posterior MI, consider doing a posterior ECG.
A left bundle branch block (choice A) has a characteristic wide QRS morphology with diffuse ST segment abnormalities.
An AV block (choice C) is a block of the atrial beat's conduction to the ventricles.
A left anterior fascicular block (choice D) and left posterior fascicular block are partial bundle branch blocks, usually with a narrow complexes and without ischemic characteristics.
Related Documents




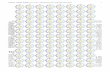
![ECG(ELECTROCARDIOGRAM) [Autosaved] new1.ppt](https://static.cupdf.com/doc/110x72/577cdafc1a28ab9e78a70e87/ecgelectrocardiogram-autosaved-new1ppt.jpg)






