trendsinmenshealth.com Trends in Urology & Men’s Health ❘ November/December 2019 ❙ 19 New approaches ● D upuytren’s disease is an idiopathic myofibroblastic disease of connective tissue characterised by multiple, painless subcutaneous nodules, convalescing to palpable cords along lines of tension. It most commonly affects the hands, usually the fourth and/or fifth digit, leading to a fixed flexion deformity, or contracture. The disease often follows a progressive course, eventually leading to finger dysfunction and the need for surgical or medical intervention. The term ‘Viking disease’ was coined as a consequence of its common presentation in northern European men. 1 It is very common in its mild form – present in 4% of the UK population and 6% of the USA population. 2 A study by Gudmundsson et al among the Icelandic population showed a prevalence in men of 19.2%, with only 4.4% in women. 3 This is a higher gender bias than has often been quoted, with a male prevalence usually twice as high as female. 4 The disease becomes much more frequent in the elderly population, increasing to a prevalence at around 20%, although few cases will be severe enough to warrant active treatment. 4 The highest incidence rate is in parts of Scandinavia, where up to 30% of adults over 60 years old are affected. 5 Among non-white populations the disease is much rarer. In a review of world literature, by 1994 only 23 cases of Dupuytren’s disease had been documented in the black population, usually with a milder presentation than in patients of Caucasian origin. 6 The same discrepancy is true for Chinese patients, with Liu et al reporting a case series of 41 patients of Chinese origin who presented with symptoms of Dupuytren’s disease from 1970–88, 35 of which required surgery. 7 Aetiology and pathophysiology Although idiopathic, recent research has shown a possible autosomal dominant inheritance pattern coupled with androgen receptor overexpression within the nodules, perhaps accounting for its prevalence in men. 8 Studies in identical twins and DNA microarray analysis have mapped a gene to the long arm of chromosome 16 in one family, while MafB (a fibroblast oncogene) seems to be upregulated exclusively in diseased patients. 8,9 Diabetes is commonly associated with Dupuytren’s disease, with a prevalence Dupuytren’s disease: is surgery still the best option? Oliver Ralph, Foundation Doctor, University College London Hospital; Nikita Shroff, Foundation Doctor, The Royal London Hospital, Barts Health NHS Trust Dupuytren’s disease can have a significant impact on the daily lives of patients. Traditionally, treatment focused on surgical correction, but advances in rheumatic pharmacology and surgical techniques have opened up a wider scope of management options. Here the authors give a background of the disease and its treatment, while providing evidence for a link with Peyronie’s disease. Figure 1. Image shows advanced disease, nodules have coalesced to form a cord with an accompanying contracture deformity. Image used under a Creative Commons licence, no alterations were made 30

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

trendsinmenshealth.com Trends in Urology & Men’s Health ❘ November/December 2019 ❙ 19
New approaches ●
Dupuytren’s disease is an idiopathic myofibroblastic disease of
connective tissue characterised by multiple, painless subcutaneous nodules, convalescing to palpable cords along lines of tension. It most commonly affects the hands, usually the fourth and/or fifth digit, leading to a fixed flexion deformity, or contracture. The disease often follows a progressive course, eventually leading to finger dysfunction and the need for surgical or medical intervention. The term ‘Viking disease’ was coined as a consequence of its common presentation in northern European men.1 It is very common in its mild form – present in 4% of the UK population and 6% of the USA population.2 A study by Gudmundsson et al among the Icelandic population showed a prevalence in men of 19.2%, with only 4.4% in women.3 This is a higher gender bias than has often
been quoted, with a male prevalence usually twice as high as female.4
The disease becomes much more frequent in the elderly population, increasing to a prevalence at around 20%, although few cases will be severe enough to warrant active treatment.4 The highest incidence rate is in parts of Scandinavia, where up to 30% of adults over 60 years old are affected.5 Among non-white populations the disease is much rarer. In a review of world literature, by 1994 only 23 cases of Dupuytren’s disease had been documented in the black population, usually with a milder presentation than in patients of Caucasian origin.6 The same discrepancy is true for Chinese patients, with Liu et al reporting a case
series of 41 patients of Chinese origin who presented with symptoms of Dupuytren’s disease from 1970–88, 35 of which required surgery.7
Aetiology and pathophysiologyAlthough idiopathic, recent research has shown a possible autosomal dominant inheritance pattern coupled with androgen receptor overexpression within the nodules, perhaps accounting for its prevalence in men.8 Studies in identical twins and DNA microarray analysis have mapped a gene to the long arm of chromosome 16 in one family, while MafB (a fibroblast oncogene) seems to be upregulated exclusively in diseased patients.8,9 Diabetes is commonly associated with Dupuytren’s disease, with a prevalence
Dupuytren’s disease: is surgery still the best option?Oliver Ralph, Foundation Doctor, University College London Hospital; Nikita Shroff, Foundation Doctor, The Royal London Hospital, Barts Health NHS Trust
Dupuytren’s disease can have a significant impact on the daily lives of patients. Traditionally, treatment focused on surgical correction, but advances in rheumatic pharmacology and surgical techniques have opened up a wider scope of management options. Here the authors give a background of the disease and its treatment, while providing evidence for a link with Peyronie’s disease.
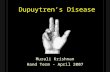
Figure 1. Image shows advanced disease, nodules have coalesced to form a cord with an accompanying contracture deformity. Image used under a Creative Commons licence, no alterations were made30

trendsinmenshealth.com20 ❙ Trends in Urology & Men’s Health ❘ November/December 2019
● New approaches
up to 33%, although patients tend to have a more indolent progression.10 The mechanism of the association with smoking and diabetes is unclear, but it is thought that pockets of ischaemia brought about via microvascular disease may induce fibroblastic differentiation in both cases.11
Other associations include alcohol and trauma, with the former possibly confounding data for the latter. However, it should be noted that such associations remain controversial, often due to the complete lack of alcohol intake in many patients, but also because of the conflicting literature.12 An interesting association is that of epilepsy, with large cohort studies having investigated the finding of reduced disease burden on discontinuation of epilepsy treatment but failing to provide direct evidence for a link with epilepsy itself.13 As a result, current thinking is that there is no direct link between the two, but that anti-epileptic medication may be responsible for disease flares.
Diagnosis and physical examDupuytren’s disease is diagnosed based on clinical history and physical exam findings, with very little role for ultrasound or other forms of imaging. Patients often report difficulty putting on gloves or putting their hands in pockets due to the deformity. The diagnosis itself has three grades, based on the type of fibrosis seen as well as the presence of contracture: Grade 1 represents a thickened palmar aponeurosis with nodules present; Grade 2 has tendinous cords (see Figure 1); and Grade 3 is characterised by the presence of a contracture.1 The contracture itself can be subcategorised into stages depending on the angle of deformity, ranging from stage 0 (no contracture) to stage 4 (>135°).14
A hard, indurated subcutaneous palmar nodule, located just proximal to the fourth or fifth metacarpophalangeal joint, is usually the initial sign of disease. After nodule formation, skin
changes such as tethering, pitting and thickening occur, followed by the appearance of multiple nodules that convalesce into subcutaneous, peritendinous cords in the palmar aponeurosis. As the disease continues to progress contractures develop, usually of the fourth finger, leading to a fixed flexion deformity that is often first noticed when a patient complains of difficulty in extending their finger. The degree of contraction deformity is proportional to the severity of the disease. Dupuytren’s diathesis is a form of disease that presents in younger men with a more severe course, often with systemic fascial fibrosis, and shows a strong autosomal dominant inheritance pattern.8 It usually affects both hands and is associated with Ledderhose disease of the plantar fascia and Peyronie’s disease of the penis.5 Garrod nodes, also known as knuckle pads, are seen both in the diathesis and in severe idiopathic disease, and represent fibrotic skin lesions over the dorsal surfaces of the proximal interphalangeal joints. The table top Hueston test is a simple method to help diagnosis, which is positive if the patient is unable to flatten their hand on a table. A positive test represents an indication for treatment.
Less invasive treatmentOptions for less invasive treatment are percutaneous needle fasciotomy, percutaneous aponeurotomy with lipografting and collagenase Clostridium histolyticum (CCH; Xiapex) injection. In patients with <30° of contracture and no proximal interphalangeal joint involvement, needle fasciotomy is often the preferred treatment. Under local anaesthetic a needle is used to manipulate the cord until it can be broken with forced extension of the digit, producing the characteristic ‘snap’. Its key advantages are that it is minimally invasive, fast, produces minimal scarring, has quick recovery
times and can be repeated as necessary. However, as tissue is not removed recurrence rates are over 50%, with one 2003 study indicating recurrence rates as high as 85% after five years.15 Additionally, haematomas and neurovascular injury are possible because it is a blind procedure, perhaps indicating the concurrent use of ultrasound to minimise this risk.16 Percutaneous fasciotomy is an alternative to needle fasciotomy despite sharing many similarities, including risk of recurrence.17 The difference here is the use of a scalpel to disrupt the fibrosis, which means an operating room is needed. In 2010, the Food and Drug Administration approved the use of CCH for the treatment of Dupuytren’s disease as it was found to be more effective than placebo.18 CCH acts as a peptidase, breaking peptide bonds in mature collagen.19 The use of injections as an alternative to needle and surgical treatment has been evaluated in double-blind randomised controlled trials, showing efficacy and a low side-effect profile. Results show up to 87% of patients had restored finger extension after one to three injections over four to six weeks.20
The technique for its use is straightforward, using a needle to insert CCH in a proximal to distal fashion along the fibrous cords. The patient then returns the next day for gentle manipulation of the finger in which the cord is extended to the point of rupture. Common side-effects are limited but may extend to swelling, pruritus and painful lymphadenopathy, with a few reported cases of tendon rupture and complex regional pain syndrome.21
More invasive treatment A segmental fasciotomy represents a compromise between the less invasive needle fasciotomy and the more invasive open fasciotomy. In this procedure, multiple small incisions are made in the palm and small segments of fibrotic tissue are removed to achieve discontinuity in the cords. It is

trendsinmenshealth.com Trends in Urology & Men’s Health ❘ November/December 2019 ❙ 21
New approaches ●
often performed for patients who have a contracture just exceeding 30° and/or proximal interphalangeal joint involvement. Although recurrence rates are lower than with needle fasciotomy, they remain significant at 20–35%.22
Although total fasciotomy was the standard of care throughout the 20th century it has since fallen out of favour, along with radiation therapy, in preference for an open partial fasciotomy approach. Indications for this surgery are the same as a segmental fasciotomy (patients with a more severe >30° contracture) and recurrence rates are the lowest of any treatment option at 15%.23 The procedure involves a Brunner or longitudinal zigzag incision (see Figure 2), opening the hand to remove any diseased tissue without removing healthy fascia, differentiating the procedure from a total fasciotomy. Neurovascular structures deep to diseased fascia must be identified before a proximal to distal resection and, if the cord extends into the phalanx, the radial and ulnar digital arteries must also be isolated. Wound closure is done via primary closure or skin grafting from the
elbow, depending on the presence of skin involvement, and splinting is initiated in the immediate postoperative period, which is then followed by hand flexion exercises.
A link with Peyronie’s diseasePeyronie’s disease is a connective tissue disorder characterised by the formation of localised fibrous plaques leading to pain, deformity and erectile dysfunction. Both Dupuytren’s and Peyronie’s disease are thought to share some pathophysiology, and they show clear epidemiological similarities. Like Dupuytren’s, Peyronie’s disease appears to be far more common in European populations, with 77.6% of sufferers being Caucasian, and a much lower rate in patients of African and Asian descent at 19.4%.24 Also, like Dupuytren’s disease, diabetes seems to be a potential risk factor for Peyronie’s disease.25 There is growing evidence of a direct link between the two conditions based on patients that present with symptoms of both Dupuytren’s and Peyronie’s disease. Current literature indicates that a patient with Dupuytren’s disease has a 3–15% risk of also
developing symptoms of Peyronie’s disease.26 Nugteren et al showed that in a cohort of 415 men with known Peyronie’s disease, 21% also showed signs of Dupuytren’s disease on examination.27 In cases of established Peyronie’s disease, a literature review indicated up to a 58.8% chance of coexisting, undiagnosed Dupuytren’s disease.28
Perhaps the most significant reason for demonstrating a possible association between Peyronie’s and Dupuytren’s disease is in accurately describing an increased risk of cancer from baseline in these two conditions. In a 2017 retrospective cohort study by Pastuszak et al, a sample of 48 423 men with Peyronie’s disease, 1 177 428 with erectile dysfunction, and 484 230 controls were identified. From these groups a statistically significant increase in cancer risk was seen with all cancer subtypes for men with Peyronie’s disease, as compared with erectile dysfunction patients or the controls (hazard ratio 1.10, 95% CI 1.06–1.14).29 What is clear is that both a clinical and genetic link may exist between Peyronie’s disease and Dupuytren’s disease. This is likely due to a possible shared pathogenesis, which, in turn, allows for the logical consideration that cancer may also be more common in patients with Dupuytren’s disease. Pastuszak makes it clear that longitudinal studies of patients with these connective tissue diseases are necessary to further characterise the risk of malignancy, and to guide screening.29
ConclusionThe aetiology of Dupuytren’s disease is currently unknown and diagnosis is made on clinical grounds alone, with management looking at reducing deformity once symptoms set in. Although Dupuytren’s disease was once a significant surgical diagnosis, recent advances in technique and an understanding of the disease prognosis have led to the development of less invasive techniques such as
Figure 2. A typical zigzag incision pattern in a patient immediately post-open partial fasciotomy. Image used under a Creative Commons licence31

trendsinmenshealth.com22 ❙ Trends in Urology & Men’s Health ❘ November/December 2019
● New approaches
percutaneous needle fasciotomy, percutaneous aponeurotomy with lipografting and CCH. Although effective, these new treatments continue to exhibit higher rates of disease recurrence than a traditional total fasciotomy and so there is clearly some way to go. An interesting final point is that similarities in treatment between Peyronie’s and Dupuytren’s disease may shed light on a possible unifying underlying aetiology.
Declaration of interests: none declared.
References1. Hart MG, Hooper G. Clinical associations of Dupuytren’s disease. Postgrad Med J 2005;81:425–8.2. Hueston JT. Dupuytren’s contracture. Curr Orthop 1988;2:173–8.3. Gudmundsson KG, Arngrimsson R, Jonsson T. Eighteen years follow-up study of the clinical manifestations and progression of Dupuytren’s disease. Scand J Rheumatol 2001;30:31–4.4. Early PF. Population studies in Dupuytren’s contracture. J Bone Joint Surg 1962;44:602–13.5 US National Library of Medicine. Genetics Home Reference. Dupuytren contracture (https://ghr.nlm.nih.gov/condition/dupuytren-contracture; accessed 19 August 2019).6. Mitra A, Goldstein RY. Dupuytren’s contracture in the black population: a review. Ann Plast Surg 1994;32:619–22.7. Liu Y, Chen WY. Dupuytren’s disease amongst the Chinese in Taiwan. J Hand Surg [Am] 1991;16(5):779–86.8. Hu FZ, Nystrom A, Ahmed A, et al. Mapping of an autosomal dominant gene for Dupuytren’s contracture to chromosome 16q in a Swedish family. Clin Genet 2005;68:424–9.
9. Lee LC, Zhang AY, Chong AK, et al. Expression of a novel gene, MafB, in Dupuytren’s disease. J Hand Surg Am 2006;31(2):211–8.10. Chammas M, Bousquet P, Renard E, et al. Dupuytren’s disease, carpal tunnel syndrome, trigger finger, and diabetes mellitus. J Hand Surg Am 1995;20:109–14.11. Godtfredsen NS, Lucht H, Prescott E, et al. A prospective study linked both alcohol and tobacco to Dupuytren’s disease. J Clin Epidemiol 2004;57:858–63.12. Loos B, Puschkin V, Horch RE. 50 years experience with Dupuytren’s contracture in the Erlangen University Hospital - a retrospective analysis of 2919 operated hands from 1956 to 2006. BMC Musculoskelet Disord 2007;8:60.13. Arafa M, Noble J, Royle SG, et al. Dupuytren’s and epilepsy revisited. J Hand Surg Br 1992;17:221–4.14. Tubiana R. Evaluation of deformities in Dupuytren’s disease. Ann Chir Main 1986;5:5–11.15. van Rijssen AL, ter Linden H, Werker PMN. Five-Year Results of a Randomized Clinical Trial on Treatment in Dupuytren’s Disease. Plast Reconstr Surg 2012:129(2):469–77. 16. Cheng HS, Hung LK, Tse WL, et al. Needle aponeurotomy for Dupuytren’s contracture. J Orthop Surg (Hong Kong) 2008;16:88–90.17. Rowley DI, Couch M, Chesney RB, Norris SH. Assessment of percutaneous fasciotomy in the management of Dupuytren’s contracture. J Hand Surg Br 1984;9:163–4.18. Brazzelli M, Cruickshank M, Tassie E, et al. Collagenase clostridium histolyticum for the treatment of Dupuytren’s contracture: systematic review and economic evaluation. Health Technol Assess 2015;19(90):1–202.19. Thomas A, Bayat A. The emerging role of Clostridium histolyticum collagenase in the treatment of Dupuytren disease. Ther Clin Risk Manag 2010;6:557–72.
20. Badalamente MA, Hurst LC. Efficacy and safety of injectable mixed collagenase subtypes in the treatment of Dupuytren’s contracture. J Hand Surg Am 2007;32: 767–74.21. Hurst LC, Badalamente MA, Hentz VR, et al. Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med 2009;361:968–79.22. Rayan GM. Dupuytren disease: anatomy, pathology, presentation, and treatment. J Bone Joint Surg Am 2007;89:189–98.23. Townley WA, Baker R, Sheppard N, Grobbelaar AO. Dupuytren’s contracture unfolded. BMJ 2006;332:397–400.24. Shaw K, Puri K, Ruiz-Deya G, Hellstrom WJG. Racial considerations in the evaluation of Peyronie’s disease. J Urol 2001;165(5), suppl: 170.25. Sommer F, Schwarzer U, Wassmer G, et al. Epidemiology of Peyronie’s disease. Int J Impot Res 2002;14:379–83.26. Ling RSM. The genetic factor in Dupuytren’s disease. J Bone Joint Surg 1963;45:709.27. Nugteren HM, Nijman JM, de Jong IJ, van Driel MF. The association between Peyronie’s and Dupuytren’s disease. Int J Impot Res 2011;23:142–5.28. Lindsay MB, Schain DM, Grambsch P, et al. The incidence of Peyronie’s disease in Rochester, Minnesota, 1950 through 1984. J Urol 1991;146:1007–9.29. Pastuszak AW, Kohn TP, Eisenberg M. Increased risk of cancer among men with peyronie’s disease. Fertil Steril 2017;108(3):e39.30. Mike Tooming. Dupuytren´s Contracture on the ring finger. Wikimedia (https://commons.wikimedia.org/wiki/ File:Dupuytren %C2%B4s_Contracture_ on_the_ring_finger.jpg; accessed 4 September 2019).31. Hilton Teper. Hand Post Dupuytren-Op with Stiches. Wikimedia (https://commons.wikimedia.org/wiki/File:Hand_Post_Dupuytren-Op_with_Stiches.jpg; accessed 4 September 2019).
Related Documents