DRUGS TO TREAT ENDOCRINE PROBLEMS
DRUGS TO TREAT ENDOCRINE PROBLEMSEndocrine System:
Regulates the following:
Reproduction
Growth
Immunity Energy
Fluid, electrolyte and acid base balance Maintains Homeostasis helps all other organs to function properly
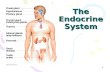
Organs of the Endocrine System:
Small ductless glands Dispersed throughout the body
Produce HORMONES
Hormones:
Chemical messengers
Secreted into the bloodstream
Carried by the blood
Bind to specific receptors of target cells to alter cellular activities
Homeostatic Feedback Mechanism:
Negative Feedback Mechanism decreases deviation from normal
Positive Feedback Mechanism increases deviation from normal
Hypothalamus:
Regulates endocrine function
Between brainstem and cerebrum
Releases hormones:
Growth Hormone Releasing Hormone
Thyrotropin Releasing Hormone
Corticotropin Releasing Hormone
Gonadotropin Releasing Hormone
Prolactin Releasing Hormone
Major Organs of the Endrocrine System:
Pituitary Gland
Thyroid Gland
Parathyroid Gland
Pancreas
Adrenal Glands
Gonads
Pineal Gland
Thymus
Pituitary Gland:
Known as the Master Gland
Pituitary hormones direct the activity of all other endocrine organs
Located below the hypothalamus
Infindibulum connects the pituitary gland to the hypothalamus
2 Regions:
Posterior Lobe
made up of nerve fibers
storage area of 2 hormones produced by the hypothalamus:
Oxytocin initiates uterine contraction
Antidiuretic Hormone (ADH) also known as
Vasopressin; stimulate reabsorption of water from the
collecting tubules
Anterior Lobe Glandular tissue produce Tropic Hormones Somatotrophs
Thyrotrophs
Carticotrophs
Lactotrophs
Gonadotrophs
Melanocyte Stimulating Hormone
Anterior Pituitary Hormones:
(
Growth Hormones:
Stimulates growth in bone and muscles
Decreased GH = Dwarfism
Increased GH = Gigantism
Increased GH in adults = Acromegaly (abnormally large hands, feet and facial features)
Thyroid Gland:
Butterfly-shaped organ located in the neck
Anterior or in front of the trachea
Secrete:
thyroid hormones (T3 and T4) - Increased oxygen consumption of most of the body cells Thyrocalcitonin regulates calciumParathyroid Gland:
4 Tiny glands embedded at the back of the thyroid
Secrete Parathyroid Hormone (PTH) important in calcium and phosphate regulation
Adrenal Glands:
Triangular glands at the top of each kidney 2 endocrine glands:
Outer adrenal cortex
Glucocorticoids
Mineralocorticoids
Androgens
Inner adrenal medulla
Catecholamines epinephrine and norepinephrine Pancreas:
Located near the duodenum of the intestines Aids in digestion
Produce hormones: regulates glucose in the body
Insulin beta cells Glucagon alpha cells Somatostatin delta cellsGonads:
Produce sex hormones regulate reproductive functions
Females gonads are called ovaries
estrogen and progesterone
Males gonads are called testes
androgens; testosterone (most important male androgen) by Leydig cellsThymus Gland:
Located posterior or behind the sternum
Regresses with age
2 major hormones: help T-lymphocytes mature (immune system) Thymosin
Thymopoietin
Pineal Gland:
Secrete and synthesize Melatonin almost entirely at night Melatonin affects the functions of the thyroid, adrenal and gonads
DRUGS FOR DIABETES MELLITUS
DIABETES MELLITUS
Chronic metabolic disorder resulting from insufficient secetion of insulin
Disorder of carbohydrate metabolism
Signs and symptoms of Diabetes Mellitus result from:
insulin insulin
Principle Sign: Sustained Hyperglycemia Polyuria
Polydipsia
Polyphagia
Ketonuria
Weight loss
May lead to:
Hypertension
Cardiac diseases
Renal failure
Neuropathy
Amputations
Impotence
stroke
TYPE 1 (IDDM)TYPE 2 (NIDDM)
Juvenile onset diabetes
Develops during childhood and adolescents
Signs and symptoms are abrupt
Destruction of pancreatic beta cells which is responsible for insulin synthesis
Autoimmune disorder
Cause: COXSACKIE INFECTION Adult onset diabetes
Almost always with obesity
No ketoacidosis
Insulin may be normal and sometimes increased
Insulin not proportionate to plasma glucose level
Release of insulin is delayed
Peak output of insulin is abnormal
Cause: Familial association
Delayed Insulin Release/Subnormal Peak Output
Resistance of liver, muscles, adipose tissues to insulin
Causes:
receptor binding
number of receptors
receptor responsiveness
Leads to: Destruction of pancreatic beta cells
insulin production
Short term complications of Diabetes Mellitus:
Hyperglycemia when insulin dosage is - when allowed to persist will lead to KETOACIDOSIS
Hypoglycemia when insulin dosage is
Long term complications of Diabetes Mellitus:
Macrovascular Disease Hypertension due to atherosclerosis; from a combination of hyperglycemia
Cardiac diseases and altered lipid metabolism
Stroke
Microvascular Disease
Microangiopathy
basement membrane of capillaries thicken causing a bloodflow
Destruction of small blood vessels cause kidney damage and blindness
(proportionate to the degree and duration of hyperglycemia)
Retinopathy caused by damage to retinal capillaries
Microaneurysms
Scarring and Proliferation
Causes local ischemia
Overgrowth of new capillaries vision
kill retinal cells
Accelerated by:
Hypertension
Hyperglycemia
smoking
Nephropathy
Proteinuria
glomerular filtration rate
arterial blood pressure
Common cause of end stage renal disease requires dialysis or kidney transplant
Increase incidence in Type 1 than in Type 2
Treatment:
ACEI delay the onset of overt nephropathy and retard ARBS progression of nephropathy
Neuropathy begins early but usually symptoms are absent for years; related to sustained hyperglycemia Tingling sensation in the fingers and toes
Pain
Suppression of reflexes
Loss of sensation
Amputations because of severe nerve damage
Impotence caused by combination of blood vessel injury and neuropathy
Gastroparesis injury to the autonomic nerves that control GI motility
Nausea
Vomiting
Delayed gastric emptying
Abdominal distention secondary to atony
DOC: Metoclopramide (Reglan)
Diabetes and Pregnancy:
Disappears after delivery Contributing Factors:
Placenta produce HPL (anti-insulin enzyme) on the 18th -20th week AOG Production of cortisol that promotes hyperglycemia (3X during pregnancy)
blood glucose level (hyperglycemia) from the maternal blood that pass through
the placenta to the fetal circulation
Hyperglycemia of the mother will stimulate the production of fetal insulin which
causes adverse effects to the fetus
Management:
Blood glucose level must be monitored 6-7X daily
C-section as soon as fetus is matured to be delivered (fetal death usually occurs
near term)
Insulin administration
Diet
Diagnosing Diabetes:
Must be tested in 2 separate days and both must reveal (+) results. Any of the 2 tests may be employed:
Fasting Plasma Glucose (FPG)
8 hrs after the last meal
Normal Value: 60-110 mg/dl
Casual Plasma Glucose Test
Blood is drawn anytime
Fasting not required
200 mg/dl and is (+) of DM but must exhibit signs and symptoms
Oral Glucose Tolerance Test (OGTT)
DM is suspected but FPG and Casual Plasma Glucose is not definite
Give oral glucose load of 75 grams Anhydrous Glucose and measure plasma
glucose 2 hrs later
200 mg/dl and = (+) DM
Not used for routine screening
Treatment:
Diet
Proper diet balance because Type 1 individuals are thin
Carbohydrates 60 to 70% of daily energy intake
Proteins 15 to 20%
space evenly
Polysaturated fats 10%
throughout
Saturated fats -