Decreased entorhinal cortex volumes in schizophrenia Monica Baiano a,c , Cinzia Perlini b,d , Gianluca Rambaldelli b,d , Roberto Cerini e , Nicola Dusi b,d , Marcella Bellani b,d , Giorgia Spezzapria b,d , Amelia Versace b,d , Matteo Balestrieri a,c , Roberto Pozzi Mucelli e , Michele Tansella b,d , Paolo Brambilla a,c,f, ⁎ a Department of Pathology and Clinical & Experimental Medicine, Psychiatry Section, University of Udine, Udine, Italy b Verona-Udine Brain Imaging and Neuropsychology Program, InterUniversity Center for Behavioral Neurosciences, University of Verona, Italy c Verona-Udine Brain Imaging and Neuropsychology Program, InterUniversity Center for Behavioral Neurosciences, University of Udine, Italy d Department of Medicine and Public Health, Section of Psychiatry and Clinical Psychology, University of Verona, Verona, Italy e Department of Morphological and Biomedical Sciences, Section of Radiology, G.B. Rossi Hospital, University of Verona, Verona, Italy f Scientific Institute IRCCS ‘E. Medea’, Udine, Italy Received 9 May 2007; received in revised form 22 November 2007; accepted 23 November 2007 Available online 14 January 2008 Abstract Background: The entorhinal cortex is located in the medial temporal lobe and is involved in memory and learning. Previous MRI studies reported conflicting findings in schizophrenia, showing normal or reduced entorhinal size. Objectives: To explore entorhinal cortex volumes in a large sample of patients with schizophrenia recruited from the geographically defined catchment area of South Verona (i.e. 100,000 inhabitants). We also investigated the size of hippocampus as part of the medial temporal lobe. Methods: 70 patients with schizophrenia and 77 normal controls underwent a session of MRI (TR = 2060 ms, TE = 3.9 ms, slice thickness = 1.25 mm). Entorhinal and hippocampal volumes were explored using the Brains2 software. Results: A significant group effect was found for total entorhinal cortex but not for hippocampus, with patients suffering from schizophrenia having smaller entorhinal volumes compared to normal subjects (F = 6.24, p = 0.01), particularly on the right side (F = 9.76, p = 0.002). Also, the laterality index for entorhinal cortex was higher in normal individuals than in patients with schizophrenia (F = 5.45, p = 0.02). Conclusions: Consistent with some of the previous reports, our study confirmed the presence of abnormally decreased entorhinal volumes, particularly on the right side, in a large number of patients with schizophrenia and also found altered asymmetry. This may play a major role in the psychopathology and cognitive disturbances of the disease. Future longitudinal MRI studies including high-risk subjects and drug-free, first-episode patients are crucial to further understand whether entorhinal cortex shrinkage is already present at the onset of the illness or appears as a consequence of the illness. © 2007 Elsevier B.V. All rights reserved. Keywords: Psychosis; Hippocampus; Magnetic resonance imaging; Brain imaging; Neuroimaging Available online at www.sciencedirect.com Schizophrenia Research 102 (2008) 171 – 180 www.elsevier.com/locate/schres ⁎ Corresponding author. Dipartimento di Patologia e Medicina Clinica e Sperimentale, Cattedra di Psichiatria, Policlinico Universitario, Via Colugna 50, 33100 Udine, Italy. Tel.: +39 0432 55 9494; fax: +39 0432 54 5526. E-mail address: [email protected] (P. Brambilla). 0920-9964/$ - see front matter © 2007 Elsevier B.V. All rights reserved. doi:10.1016/j.schres.2007.11.035

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Available online at www.sciencedirect.com
02 (2008) 171–180www.elsevier.com/locate/schres
Schizophrenia Research 1
Decreased entorhinal cortex volumes in schizophrenia
Monica Baiano a,c, Cinzia Perlini b,d, Gianluca Rambaldelli b,d, Roberto Cerini e,Nicola Dusi b,d, Marcella Bellani b,d, Giorgia Spezzapria b,d, Amelia Versace b,d,
Matteo Balestrieri a,c, Roberto Pozzi Mucelli e,Michele Tansella b,d, Paolo Brambilla a,c,f,⁎
a Department of Pathology and Clinical & Experimental Medicine, Psychiatry Section, University of Udine, Udine, Italyb Verona-Udine Brain Imaging and Neuropsychology Program, InterUniversity Center for Behavioral Neurosciences, University of Verona, Italyc Verona-Udine Brain Imaging and Neuropsychology Program, InterUniversity Center for Behavioral Neurosciences, University of Udine, Italy
d Department of Medicine and Public Health, Section of Psychiatry and Clinical Psychology, University of Verona, Verona, Italye Department of Morphological and Biomedical Sciences, Section of Radiology, G.B. Rossi Hospital, University of Verona, Verona, Italy
f Scientific Institute IRCCS ‘E. Medea’, Udine, Italy
Received 9 May 2007; received in revised form 22 November 2007; accepted 23 November 2007Available online 14 January 2008
Abstract
Background: The entorhinal cortex is located in the medial temporal lobe and is involved in memory and learning. Previous MRIstudies reported conflicting findings in schizophrenia, showing normal or reduced entorhinal size.Objectives: To explore entorhinal cortex volumes in a large sample of patients with schizophrenia recruited from the geographicallydefined catchment area of South Verona (i.e. 100,000 inhabitants). We also investigated the size of hippocampus as part of the medialtemporal lobe.Methods: 70 patients with schizophrenia and 77 normal controls underwent a session of MRI (TR=2060 ms, TE=3.9 ms, slicethickness=1.25 mm). Entorhinal and hippocampal volumes were explored using the Brains2 software.Results: A significant group effect was found for total entorhinal cortex but not for hippocampus, with patients suffering fromschizophrenia having smaller entorhinal volumes compared to normal subjects (F=6.24, p=0.01), particularly on the right side(F=9.76, p=0.002). Also, the laterality index for entorhinal cortex was higher in normal individuals than in patients withschizophrenia (F=5.45, p=0.02).Conclusions: Consistent with some of the previous reports, our study confirmed the presence of abnormally decreased entorhinalvolumes, particularly on the right side, in a large number of patients with schizophrenia and also found altered asymmetry. Thismay play a major role in the psychopathology and cognitive disturbances of the disease. Future longitudinal MRI studies includinghigh-risk subjects and drug-free, first-episode patients are crucial to further understand whether entorhinal cortex shrinkage isalready present at the onset of the illness or appears as a consequence of the illness.© 2007 Elsevier B.V. All rights reserved.
Keywords: Psychosis; Hippocampus; Magnetic resonance imaging; Brain imaging; Neuroimaging
⁎ Corresponding author. Dipartimento di Patologia eMedicina Clinica e Sperimentale, Cattedra di Psichiatria, PoliclinicoUniversitario, Via Colugna 50,33100 Udine, Italy. Tel.: +39 0432 55 9494; fax: +39 0432 54 5526.
E-mail address: [email protected] (P. Brambilla).
0920-9964/$ - see front matter © 2007 Elsevier B.V. All rights reserved.doi:10.1016/j.schres.2007.11.035
172 M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
1. Introduction
The human entorhinal cortex (EC) is located in therostral half of the ventromedial temporal lobe andcorresponds to the anteromedial parahippocampal gyrus(Brodmann's areas 28 and 34) (Insausti, 1998; Pruessneret al., 2002). It modulates multiple interactions betweenthe limbic structures and the neocortex. More specifi-cally, it is considered to be themost important gateway ofneocortical polysensory information to the hippocampus(Sim et al., 2006). It is crucial for memory processing(Fransén, 2005), associative learning (Fyhn et al., 2004)and spatial navigation (Charles et al., 2004; Hafting etal., 2005). Furthermore, the entorhinal projections to theamygdala provide the neural pathway for the associa-tion between olfaction, emotional states and memory(Turetsky et al., 2003). All of these higher-levelcognitive dimensions are compromised in patients withschizophrenia. As a result, it has always been believedthat the entorhinal cortex is involved in the pathophy-siology of this illness (Arnold, 1999; Arnold, 2000a,b;Lisman and Otmakhova, 2001).
Up to now, four magnetic resonance imaging (MRI)investigations have reported on reduced volumes of theentorhinal cortex in patients with schizophrenia comparedto healthy individuals (Joyal et al., 2002; Pearlson et al.,1997; Prasad et al., 2004; Turetsky et al., 2003). On thecontrary, no significant differences were found in threeother MRI studies (Kalus et al., 2005; Nasrallah et al.,1997; Sim et al., 2006). However, early onset patients hadsmaller entorhinal cortex volumes than late-onset patientsin one of these studies (Nasrallah et al., 1997). Therefore,the literature is still controversial on entorhinal cortex sizein patients suffering from schizophrenia.
Nonetheless, several post-mortem studies support therole of entorhinal cortex in schizophrenia, showing
Table 1Socio-demographic and clinical variables for normal controls and patients w
Normal controls (N=77)
Age (years) 39.97±10.92Gender (males/females) 40/37Handedness (right/non right-handed) 63/14Race CaucasianEducational level (years) 13.10±4.44Age at onset (years)Duration of illness (years)Number of hospitalizationsLifetime AP treatment (years)BPRS total scoresPositive symptomsNegative symptoms
subtle cytoarchitectural changes, such as smaller neuro-nal size (Arnold et al., 1995 and 1997) and neuronaldisplacement (Falkai et al., 2000; Jakob and Beckmann,1986, 1989, 1994). These findings indicate that theentorhinal cortex is involved in a pattern of neurodeve-lopmental abnormalities (Kovalenko et al., 2003), whichhave also been observed in animal models of schizo-phrenia (Cunningham et al., 2006; Talamini et al., 1998).Also, neurophysiologic studies suggest that the entorh-inal cortex plays a major role in the psychopathology andneuropsychology of schizophrenia (Cunningham et al.,2006). For instance, entorhinal cortex volumes werepositively correlated with psychotic symptoms, espe-cially with delusions (Prasad et al., 2004). In this regard,it has been hypothesized that the entorhinal cortex couldretrieve corrupted memories (Prasad and Keshavan,2003), consecutively processed as false conclusions by adysfunctional circuitry involving the hippocampus(Benes and Berretta, 2000; Lisman and Otmakhova,2001). Therefore, there is evidence that the cytoarchi-tecture and the function of the entorhinal cortex isimpaired in schizophrenia, potentially participating insustaining symptoms and cognitive disturbances.
In conclusion, some MRI studies exploring entorh-inal cortex size in patients suffering from schizophrenia,provided conflicting findings. In this study, we inves-tigated entorhinal cortex volumes in a large community-based population of patients with schizophrenia,representative of those living in the geographicallydefined catchment area of South Verona (100,000inhabitants), Italy. Based on previous literature, weexpected that patients suffering from schizophreniawould have decreased entorhinal cortex volumescompared to normal controls. Since the entorhinalcortex is part of the medial temporal lobe, we alsoexplored the size of hippocampus in this dataset.
ith schizophrenia
Patients with schizophrenia (N=70) Statistics p
39.99±12.09 t=0.006 0.9945/25 χ2=2.29 0.1358/12 χ2=0.03 0.87Caucasian9.66±4.08 t=4.75 b0.00126.25±9.2514.14±10.724.33±8.2012.64±10.5643.32±16.5711.06±6.1811.25±3.93
173M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
2. Methods
2.1. Subjects
Seventy patients with DSM-IV schizophrenia werestudied (Table 1). They were recruited from thegeographically defined catchment area of South Verona(i.e. 100,000 inhabitants) and were being treated by theSouth Verona Community-based Mental Health Service(CMHS) and by other clinics reporting to the SouthVerona Psychiatric Care Register (PCR) (Ammaddeoet al., 1997; Tansella and Burti, 2003). Diagnoses forschizophrenia were obtained using the Item GroupChecklist of the Schedule for Clinical Assessment inNeuropsychiatry (IGC-SCAN) (World Health Organi-zation, 1992) and confirmed by the clinical consensus oftwo staff psychiatrists. The IGC-SCAN was performedby two trained research clinical psychologists withextensive experience in the procedure. In fact, theyadministered at least 10 IGC-SCAN with a seniorinvestigator trained in SCAN, after having conductedseveral IGC-SCAN. Then, they had to work blindly andindependently of the senior investigator and achievesimilar diagnoses for at least eight out of 10 IGC-SCAN.Moreover, the psychopathological item groups com-pleted by the two raters were compared, in order todiscuss any major symptom discrepancies. We alsoensured the reliability of the IGC-SCAN diagnoses byholding regular consensus meetings with the psychia-trists treating the patients and a senior investigator. It isworth noting that the Italian version of the SCAN wasedited by our group (World Health Organization, 1996)and that our investigators attended specific trainingcourses held by official trainers in order to learn how toadminister the IGC-SCAN. Subsequently, diagnoses forschizophrenia were corroborated by the clinical con-sensus of two staff psychiatrists, according to the DSM-IV criteria. Patients with comorbid psychiatric disorders,alcohol or substance abuse within the six monthspreceding the study, history of traumatic head injurywith loss of consciousness, epilepsy or other neurolo-gical diseases were excluded. Apart from two patients,all of the participants, were receiving antipsychoticmedication at the time of imaging. More specifically, 25patients were on typical antipsychotic drugs (16 onhaloperidol, three on chlorpromazine, two on fluphena-zine, two on clotiapine , one on thioridazine, one onzuclopenthixol) and 45 on atypical antipsychoticmedication (25 on olanzapine, nine on clozapine, nineon risperidone, two on quetiapine). Patients' clinicalinformation was retrieved from psychiatric interviews,the attending psychiatrist and medical charts. Clinical
symptoms were characterized using the Brief Psychia-tric Rating Scale (BPRS 24-item version) (Ventura et al.,2000), which was administered by two trained researchclinical psychologists. The reliability for BPRS wasestablished and monitored utilizing procedures similarto the IGC-SCAN.
Seventy-seven healthy control subjects were alsorecruited (Table 1). They had no DSM-IV axis Idisorders, as determined by a modified version of theSCID-IV (non-patient version), no history of psy-chiatric disorders among first-degree relatives, nohistory of alcohol or substance abuse and no currentmajor medical illness. Typical control subjects werehospital/University staff volunteers or subjects under-going MR scans for dizziness without evidence ofcentral nervous system abnormalities on the scan, asdetermined by the neuroradiologist (R.C.). Dizzinesswas due to benign paroxysmal positional vertigo or tonon-toxic labyrinthitis. Control individuals werescanned only after a full medical history had beentaken, general neurological, otoscopic, and physicalexaminations carried out, and the patient hadcompletely recovered from the dizziness. In addition,none of the control subjects was on medication at thetime of participation in the study, including drugs fornausea or vertigo.
This research study was approved by the biomedicalEthics Committee of the Azienda Ospedaliera ofVerona. All individuals provided signed their informedconsent, after having understood all of the issuesinvolved in participation in the study.
2.2. MRI acquisition
MRI scans were acquired using a 1.5 T SiemensMagnetom Symphony Maestro Class, Syngo MR2002B. All participants were provided with earplugsto reduce acoustic noise and their head was comfortablyplaced in a head holder and held stable in order tominimize movement artefact. Initially, exploratory T1-weighted images (TR=450 ms, TE=14 ms, flipangle=90°, FOV=230×230, slice thickness=5 mm,matrix size=384×512) were obtained to verify thesubject's head position and the quality of the image. Asequence of DP/T2-weighted images were then obtained(TR=2500 ms, TE=24/121 ms, flip angle=180°,FOV=230× 230, slice thickness = 5 mm, matrixsize=410×512) according to an axial plane parallel tothe anterior–posterior commissures (AC–PC), in orderto exclude focal lesions. Subsequently, a coronal3D MPR sequence was acquired (TR=2060 ms,TE=3.9 ms, flip angle=15°, FOV=176×235, slice
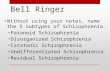
Fig. 1. Regions of interest landmarks. The frontotemporal stem was used as anterior limit; the intersection of the line along the grey–white junctionwith the medial bank of the collateral sulcus as inferolateral border; the sulcus semiannularis and the uncal cleft defined the superomedial limit; themost anterior slice in which the body of the hippocampus first became clearly visible was chosen as posterior border.
174 M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
thickness=1.25 mm, matrix size=270×512, TI=1100)to obtain 144 images covering the entire brain.
2.3. Anatomical landmarks
All imaging data was transferred to a PC workstationand analyzed using the BRAINS2 software developed atthe University of Iowa (http://www.psychiatry.uiowa.edu/mhcrc/IPLpages/BRAINS.htm).
The entorhinal cortex was traced on MRI coronalslices based on prior published methods (Bernasconiet al., 1999; Prasad et al. 2004) (Fig. 1). Thefrontotemporal stem delimited the region of interestanteriorly. The intersection of the line along the grey–white junction with the medial bank of the collateralsulcus defined the inferolateral border. The superomedialborder was defined rostrally by the sulcus semiannularisand caudally by the uncal cleft. The intersection of theline along the grey–white junction with the corticalsurface was used to improve the definition of thesestructures. The most anterior slice in which the body ofthe hippocampus first became clearly visible was chosenas the posterior limit (Bernasconi et al., 1999). It shouldbe noted that the prior methods were slightly modifiedsince the lateral geniculate body was poorly detectable inmost of our scan and therefore it was not to used as a
posterior limit. Also, the perirhinal cortex was includedin our tracing.
Hippocampus was detected on MRI coronal slices,where the corona radiata and then the ambient cisternwere used as the superior border; the white matteracted as the inferior border, and the inferior horn ofthe lateral ventricle as the lateral one (Brambilla et al.2003). Parahippocampal gyrus was not included inthe tracing.
Intracranial volume (ICV) was traced in the coronalplane, along the border of the brain and included thecerebrospinal fluid, dura mater, sinus, optic chiasma,brainstem, cerebral and cerebellar matter. The inferiorborder did not extend below the base of the cerebellum.The first and last ten slices including brain matter weretraced, then 1 slice in every 5 was traced. To validate themanual tracing of ICV performed with BRAINS2, tenrandomly selected scans were analyzed by using FSL(http://www.fmrib.ox.ac.uk/fsl/), providing an intra-class correlation coefficients (ICCs) of 0.90.
Tracing was performed by a rater who was blind tosubjects' identity and sociodemographic and clinicalvariables. Two raters achieved high reliability (A.V,G. S.), as defined by intra-class correlation coefficients(ICCs) of 0.94 for left entorhinal cortex, 0.95 for rightentorhinal cortex and 0.97 for ICV. These volumes were
Table 2Entorhinal cortex and hippocampal volumes in normal controls and patients with schizophrenia
Volumes (cm3) Normal controls (N=77) Patients withschizophrenia (N=70)
Statistics
Mean S.D. Mean S.D. F p
Total entorhinal cortex 2.21 0.42 2.06 0.41 6.24 0.01Right entorhinal cortex 1.16 0.24 1.06 0.23 9.76 0.002Left entorhinal cortex 1.05 0.23 1.00 0.21 1.93 0.17Total hippocampus 3.52 0.64 3.51 0.69 0.53 0.47Right hippocampus 1.78 0.36 1.76 0.32 0.82 0.37Left hippocampus 1.74 0.31 1.75 0.39 0.23 0.63
ANCOVA with age, gender, and ICV as covariates was performed to compare the volumes of EC and hippocampus between patients withschizophrenia and normal controls. S.D. = standard deviation.
175M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
established by blindly tracing 10 randomly selectedscans.
2.4. Statistical analysis
All statistical analyses were conducted using theSPSS for Windows software, version 11.0 (SPSS Inc.,Chicago). A two-tailed significance level of pb0.05 wasadopted. Demographic variables were compared usingStudent's t-test and Pearson chi-square, as appropriate.An analysis of covariance (ANCOVA) using age,gender, and ICVas covariates was conducted to comparethe volumes of the entorhinal cortex and hippocampusbetween patients with schizophrenia and healthy con-trols. Pearson's correlation and partial correlation
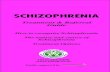
Fig. 2. Right entorhinal cortex volumes in patients with schizophrenia and norentorhinal cortex volumes than normal controls (F=9.76; p=0.002) (ANCO
analyses, which were controlled for age, were used toexamine association between age and clinical variables,respectively, and entorhinal cortex volumes.
3. Results
The two groups significantly differed for total ento-rhinal cortex volumes, with patients having smaller vol-umes than normal controls (F=6.24, p=0.01; ANCOVA,age, gender and ICV as covariates). Also, a significantgroup×hemisphere interactionwas found; indeed, patientswith schizophrenia had significantly reduced right entorh-inal cortex volumes compared to normal controls(F=9.76; p=0.002; ANCOVA, age, gender, and ICV ascovariates) (Table 2 and Fig. 2), even when education was
mal controls. Patients with schizophrenia had significantly smaller rightVA with age, gender, and ICV as covariates).
176 M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
included as a covariate (F=4.56; p=0.03; ANCOVA, age,gender, education, and ICVas covariates). Similar findingswere found when patients suffering from schizophreniawere compared separately to normal individuals fromamong the hospital/University staff (N=37) (totalvolumes: F=5.78, p= 0.02; right side: F=9.10,p=0.003; left side: F=1.92, p=0.17, respectively) or tocontrol subjects who had recovered from dizziness(N=40) (total volumes: F=3.22, p=0.07; right side:F=3.95, p=0.04; left side:F=1.42, p=0.24, respectively)(ANCOVA, age, gender and ICV as covariates). More-over, no significant differences for entorhinal cortexvolumes were found between the two groups of normalcontrols (ANCOVA, age, gender, and ICV as covariates,pN0.05).
Among normal controls, the right entorhinal cortexwas 9.5% larger than the left, being this differencestatistically significant (Student's paired t-test, t=3.45,pb0.01), even including only right-handed controls(t=2.97, p=0.004). On the contrary, in patients withschizophrenia, the volume of the right entorhinal cortexwas only 5.7% bigger than the left and this differencewas not statistically relevant (Student's paired t-test,t=1.54, p=0.13), even when only right-handed patientswere taken into account (t=1.03, p=0.31). Accordingly,the right to left entorhinal cortex volume difference(volumes of right minus left entorhinal cortex) and thelaterality index (right minus left entorhinal cortexvolumes, divided by the sum of right and left entorhinalcortex volumes) were higher in normal subjects than inpatients (F=5.87, p=0.02; F=5.45, p=0.02, respec-tively) (ANCOVA, age and gender as covariates).Considering only right-handed individuals, these differ-ences were still significant (F=7.76, p=0.006; F=7.01,p=0.009, respectively).
In contrast, no significant differences were found forhippocampal volumes between patients with schizo-phrenia and normal controls (ANCOVA, age, gender,and ICV as covariates, pN0.05; Table 2) and nolaterality effects were detected within the two groups,even when only right-handed subjects were included(Student's paired t-test, pN0.05).
There was no significant correlation between entorh-inal or hippocampal volumes and age in either patientsor control subjects (Pearson's correlation coefficient,pN0.05). Neither any significant associations werefound between volumes of entorhinal cortex orhippocampus and clinical measures (age at onset, lengthof illness, antipsychotic lifetime administration, numberof prior hospitalizations, BPRS scores) (Partial correla-tion analyses controlled for age, pN0.05). Patientstreated with typical antipsychotic drugs (N=25) did not
significantly differ in entorhinal cortex or hippocampalvolumes, bilaterally, compared to those on atypicalantipsychotic drugs (N=45) (ANCOVA, age, gender,and ICV volume as covariates, pN0.05).
4. Discussion
Our study confirmed the presence of abnormallydecreased entorhinal cortex volumes in schizophrenia,particularly on the right side (p=0.002). This is consistentwith the findings of four previous reports which foundsmaller entorhinal volumes in patients with schizophreniawhen compared to healthy controls (Pearlson et al., 1997;Turetsky et al., 2003), even in neuroleptic–naive first-episode patients (Joyal et al. 2002; Prasad et al., 2004).Also, microstructural impairments of entorihnal cortexhave been found in schizophrenia even in presence of nonsignificantly decreased volumes (Kalus et al. 2005). Ingeneral, neurodevelopmental disturbances, such as prun-ing and apoptotic mechanisms (Glantz et al., 2006;Pantelis et al., 2005), together with environmental stressfactors (Cooper, 2005; Danese, 2006; Keshavan et al.,2005), may lead to progressive neuronal loss of theentorhinal cortex. Particularly, as proposed by Kalus et al.(2005, 2006), alterations of entorhinal cortexmay result indisturbances in the perforant pathway, a large entorhinalefferent fiber tract to the limbic system crucial forcognition. Interestingly, altered expression of specificmicrotubule proteins have been found in entorhinal cortexin schizophrenia and may in part sustain decreased size(Arnold et al., 1991; Rioux et al., 2003). This mayultimately result in cytoarchitectural and cytoskeletalabnormalities of entorhinal cortex and impaired signaltransduction. However, preserved entorhinal cortexvolumes were found in another three studies (Kaluset al., 2005; Nasrallah et al., 1997; Sim et al., 2006).Discrepancies between our report and studies showingnormal entorhinal cortex volumes in schizophreniamay inpart be explained by the small sample size of these studies(N=15 in Kalus et al., 2005; N=19 in Sim et al., 2006).Also, our patients were older and more chronicallyaffected than those included in Kalus et al. (2005) (meanage: 32.27±10.67 with 3.17±3.82 years of illness) andNasrallah et al. (1997) (mean age: 32.6±7.1 year-old with9.8±6.1 years of illness). Other methodological issues,such as different tracing techniques should be considered,since different anatomical landmarks were used by thesethree negative studies (Kalus et al., 2005; Nasrallah et al.,1997; Sim et al., 2006). Furthermore, a slice thickness of5 mm were used in the study by Nasrallah et al. (1997).
Interestingly, a laterality effect was found in thenormal group, but not in individuals suffering from
177M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
schizophrenia, with the right-sided volumes beingsignificantly higher than the left-sided ones, aspreviously reported in human studies (Bernasconiet al., 1999; Pruessner et al., 2002). In general, thedevelopment of structural brain asymmetry is con-sidered the root of hemispheric independence/dom-inance and cerebral functional lateralization, whichhas been found to be reduced in patients sufferingfrom schizophrenia (Bilder et al., 1994; Crow et al.,1989; DeLisi et al., 1997; Falkai et al., 1995).Possibly, abnormal entorhinal lateralization duringbrain development may play a crucial role insustaining the cognitive disturbances of the disorder(Talamini et al., 1998).
In regard to hippocampus, this study did not find anyvolume abnormalities in schizophrenia using a region ofinterest (ROI) technique. The literature is somewhatcontroversial, with most of the previous structural MRIstudies showing hippocampal volume decreases (Vela-koulis et al., 2006; Weiss et al., 2005) and somereporting no differences (Staal et al., 2000) in patientswith schizophrenia compared to healthy controls.Interestingly , post-mortem studies documented thathippocampal neurons' number (Walker et al., 2002;Weinberger, 1999) and density (Arnold et al., 1995;Harrison, 1999) are not significantly altered in schizo-phrenia. This suggests that hippocampal changes inschizophrenia may be related to local disturbances ofcytoarchitecture organization (Harrison, 2004;Heckersand Konradi, 2002). Indeed, these alterations are notvisualized by conventional volumetric methods alone(as performed in this study) because they may notnecessarily affect hippocampal volumes. Consistently,subtle shape deformities and microstructural tissuealterations have been found by high dimensional brainmapping and diffusion imaging studies (Csernanskyet al., 2002; Kalus et al., 2004). Therefore, the usage ofadvanced MR techniques and post-processing proce-dures will be of great help to further clarify the role ofhippocampus for the pathophysiology of the disease.However, it should be noted that meta-analyses of MRIstudies showed significant reductions of hippocampusin schizophrenia, particularly in first-episode patients(Nelson et al., 1998; Steen et al., 2006; Vita et al., 2006),whereas we mainly investigated chronic patients withlong-term antipsychotic maintenance. To this regard, ithas been suggested by human and animal studies thatantipsychotic drugs have neuroprotective effects onhippocampus (Bastianetto et al., 2006; Jarskog et al.,2000; McClure et al., 2006; Pillai and Mahadik, 2006),which may in part explain the findings of preservedhippocampal volumes in our patient population.
There are some limitations to this study. Firstly, ourpatient sample was mostly composed of chronicallymedicated subjects. Thus it is not completely clearwhether entorhinal cortex atrophy preceded the onset ofthe illness or appeared subsequently as a result of thecourse of the illness or psychotropic treatment. However,the length of the illness or the lifetime administration ofantipsychotic drugs did not significantly affect entorhinalvolumes, suggesting that entorhinal cortex abnormalitiesmay not be related to illness or medication, as shown byprevious studies (Kalus et al., 2005; Sim et al., 2006). Inaddition, compared to previous MRI studies we recruiteda relatively larger number of subjects matching schizo-phrenia and control individuals well, and thus providingadequate statistical power. Secondly, part of our controlgroup was selected from individuals undergoing MRscanning for dizziness, which may represent a methodo-logical limitation. However, they were fully recovered atthe time of imaging and showed no evidence of centralnervous system abnormalities on the scan. Moreover,when patients with schizophrenia were comparedseparately to the two groups of controls, the findingswere still consistent and similar entorhinal cortexvolumes were found in normal individuals recruitedfrom among the hospital/University staff and those whohad recovered from a dizzy spell.
In conclusion, our study, consistent with some of theprevious reports, confirmed the presence of abnormallydecreased entorhinal cortex volumes, particularly on theright side, in a very large sample of patients recruitedfrom the geographically defined catchment area of SouthVerona (i.e. 100,000 inhabitants). Entorhinal cortexabnormalities may play a major role in the psychopathol-ogy and cognitive disturbances of the disorder. Futurelongitudinal MRI studies including large samples ofhigh-risk subjects and drug-free first-episode patients willbe crucial to further understand whether entorhinal cortexshrinkage is already present at the onset of the illness orappears as a consequence of illness course.
Role of the funding sourceThis work was partly supported by grants from the American
Psychiatric Institute for Research and Education (APIRE/AstraZenecaYoung Minds in Psychiatry Award), the Italian Ministry for Education,Universities and Research (PRIN n. 2005068874), the StartCupVeneto 2007 to Dr. Brambilla and by a grant from the Veneto Region,Italy, (159/03, DGRV n. 4087). None of these funding agencies hadany further role in the study design; in the collection, analysis andinterpretation of data; in the writing of the report, and in the decision tosubmit the paper for publication.
ContributorsMonica Baiano managed the literature searches and wrote themanuscript draft.
178 M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
Cinzia Perlini coordinated patient and control recruitment and scaleadministration.Gianluca Rambaldelli managed MRI data post-processing.Roberto Cerini and Roberto Pozzi Mucelli collected MRI data.Marcella Bellani and Nicola Dusi recruited patients.Giorgia Spezzapria traced the entorhinal cortex.Amelia Versace supervised the entorhinal cortex tracing.Matteo Balestrieri and Michele Tansella supervised subject recruitment.Paolo Brambilla designed the study, wrote the protocol, undertook thestatistical analyses, and wrote the final version of the manuscript.
All authors contributed to and have approved the final manuscript.
Conflict of interestNo authors of this manuscript have fees and grants from,
employment by, consultancy for, shared ownership in, or any closerelationship with, an organization whose interests, financial orotherwise, may by affected by the publication of the paper.
AcknowledgementsWe thank Dr Konasale Prasad for his very helpful comments on the
earlier versions of this manuscript and all subjects who participated.This work was partly supported by grants from the American
Psychiatric Institute for Research and Education (APIRE YoungMindsin Psychiatry Award), the Italian Ministry for University and Research(PRIN n. 2005068874), the StartCup Veneto 2007 to Dr. Brambilla andby a grant from the Veneto Region, Italy, (159/03, DGRV n. 4087).
References
Ammadeo, F., Beecham, J., Bonizzato, P., Fenyo, A., Knapp, M.,Tansella, M., 1997. The use of a case register o evaluate the cost ofpsychiatric care. Acta Psychiatr. Scand. 95, 189–198.
Arnold, O.H., 1999. Schizophrenia—a disturbance of signal interactionbetween the entorhinal cortex and the dentate gyrus? The contribu-tion of experimental dibenamine psychosis to the pathogenesis ofschizophrenia: a hypothesis. Neuropsychobiology 40, 21–32.
Arnold, S.E., 2000a. Cellular and molecular neuropathology of theparahippocampal region in schizophrenia. Ann. N.Y. Acad. Sci.911, 275–292.
Arnold, S.E., 2000b. Hippocampal pathology. In: Harrison, P.J., Roberts,G.W. (Eds.), The Neuropathology of Schizophrenia. Progress andInterpretation. Oxford University Press, Oxford, pp. 57–80.
Arnold, S.E., Lee, V.M., Gur, R.E., Trojanowski, J.Q., 1991. Abnormalexpression of two microtubule-associated proteins (MAP2 andMAP5) in specific subfields of the hippocampal formation inschizophrenia. Proc. Natl. Acad. Sci. U. S. A. 88, 10850–10854.
Arnold, S.E., Franz, B.R., Gur, R.C., Gur, R.E., Shapiro, R.M.,Moberg, P.J., Trojanowski, J.Q., 1995. Smaller neuron size inschizophrenia in hippocampal subfields that mediate cortical–hippocampal interactions. Am. J. Psychiatry 152, 738–748.
Arnold, S.E., Ruscheinsky, D.D., Han, L.Y., 1997. Further evidence ofabnormal cytoarchitecture of the entorhinal cortex in schizophreniausing spatial point pattern analyses. Biol. Psychiatry 42, 639–647.
Bastianetto, S., Danik, M., Mennicken, F., Williams, S., Quirion, R.,2006. Prototypical antipsychotic drugs protect hippocampalneuronal cultures against cell death induced by growth mediumdeprivation. BMC Neuroscience 7, 28.
Benes, F.M., Berretta, S., 2000. Amygdalo–entorhinal inputs to thehippocampal formation in relation to schizophrenia. Ann. N.Y.Acad. Sci. 911, 293–304.
Bernasconi, N., Bernasconi, A., Andermann, F., Dubeau, F., Feindel,W., Reutens, D.C., 1999. Entorhinal cortex in temporal lobeepilepsy: a quantitative MRI study. Neurology 52, 1870–1876.
Bilder, R.M., Wu, H., Bogerts, B., Bogerts, B., Degreef, G., Ashtari,M., Alvir, J.M., Snyder, P.J., Lieberman, J.A., 1994. Absence ofregional hemispheric volume asymmetries in first-episode schizo-phrenia. Am. J. Psychiatry 151, 1437–1447.
Brambilla, P., Harenski, K., Nicoletti, M., Mallinger, A.G., Frank, E.,Kupfer, D.J., Keshavan, M.S., Soares, J.C., 2003. MRI investiga-tion of temporal lobe structures in bipolar patients. J. Psychiatr.Res. 37, 287–295.
Csernansky, J.G., Wang, L., Jones, D., Rastogi-Cruz, D., Posener, J.A.,Heydebrand, G., Miller, J.P., Miller, M.I., 2002. Hippocampaldeformities in schizophrenia characterized by high dimensionalbrain mapping. Am. J. Psychiatry 159, 2000–2006.
Charles, D.P., Browning, P.G.F., Gaffan, D., 2004. Entorhinal cortexcontributes to object-in-place scene memory. Eur. J. Neurosci. 20,3157–3164.
Cooper, B., 2005. Schizophrenia, social class and immigrant status: theepidemiological evidence. Epidemiol. Psychiatr. Soc. 14, 137–144.
Crow, T.J., Ball, J., Bloom, S.R., Brown, R., Bruton, C.J., Colter, N.,Frith, C.D., Johnstone, E.C., Owens, D.G., Roberts, G.W., 1989.Schizophrenia as an anomaly of development of cerebral asymmetry.A postmortem study and a proposal concerning the genetic basis ofthe disease. Arch. Gen. Psychiatry 46, 1145–1150.
Cunningham, M.O., Hunt, J., Middleton, S., LeBeau, F.E.N., Gillies,M.G., Davies, C.H., Maycox, P.R., Whittington, A., Racca, C.,2006. Region-specific reduction in entorhinal gamma oscilla-tions and parvoalbumin-immunoreactive neurons in animalmodels of psychiatric illness. J. Neurosci. 26, 2767–2776.
Danese, A., 2006. A public health genetic approach for schizophrenia.Epidemiol. Psychiatr. Soc. 15, 185–193.
DeLisi, L.E., Sakuma, M., Kushner, M., Finer, D.L., Hoff, A.L.,Crow, T.J., 1997. Anomalous cerebral asymmetry and languageprocessing in schizophrenia. Schizophr. Bull. 23, 255–271.
Falkai, P., Bogerts, B., Schneider, T., Greve, B., Pfeiffer, U., Pilz, K.,Gonsiorzcyk, C., Majtenyi, C., Ovary, I., 1995. Disturbed planumtemporale asymmetry in schizophrenia. A quantitative post-mortem study. Schizophr. Res. 14, 161–176.
Falkai, P., Schneider-Axmann, T., Honer, W.G., 2000. Entorhinal cortexpre-alpha cell clusters in schizophrenia. Quantitative evidence of adevelopmental abnormality. Biol. Psychiatry 47, 937–943.
Fransén, E., 2005. Functional role of entorhinal cortex in workingmemory processing. Neural Networks 18, 1141–1149.
Fyhn,M.,Molden, S.,Witter,M.P.,Moser, E.I.,Moser,M.B., 2004. Spatialrepresentation in the entorhinal cortex. Science 305, 1258–1264.
Glantz, L.A., Gilmore, J.H., Lieberman, J.A., Jarskog, L.F., 2006.Apoptotic mechanisms and synaptic pathology of schizophrenia.Schizophr. Res. 81, 47–63.
Hafting, T., Fyhn, M., Molden, S., Moser, M.B., Moser, E.I., 2005.Microstructure of a spatial map in the entorhinal cortex. Nature436, 801–806.
Harrison, P.J., 1999. The neuropathology of schizophrenia. Acritical review of the data and their interpretation. Brain 122,593–624.
Harrison, P.J., 2004. The hippocampus in schizophrenia: a review ofthe neuropathological evidence and its pathophysiological impli-cations. Psychoparmacology 174, 151–162.
Heckers, S., Konradi, C., 2002. Hippocampal neurons in schizo-phrenia. J. Neural. Transm. 109, 891–905.
Insausti, R., Juottonen, K., Soininen, H., Insausti, A.M., Partanen, K.,Vainio, P., Laakso, M.P., Pitkänen, A., 1998. MR volumetric
179M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
analysis of the human entorhinal, perirhinal, and temporopolarcortices. Am. J. Neuroradiol. 19, 659–671.
Jakob, H., Beckmann, H., 1986. Prenatal developmental disturbancesin the limbic allocortex in schizophrenics. J. Neural Transm. 65,303–326.
Jakob, H., Beckmann, H., 1989. Gross and histological criteria fordevelopmental disorders in brains of schizophrenics. J. R. Soc.Med. 82, 466–469.
Jakob, H., Beckmann, H., 1994. Circumscribed malformation andnerve cell alterations in the entorhinal cortex of schizophrenics.Pathogenetic and clinical aspects. J. Neural Transm. Gen. Sect. 98,83–106.
Jarskog, L.F., Gilmore, J.H., Selinger, E.S., Lieberman, J.A., 2000.Cortical bcl-2 protein expression and apoptotic regulation inschizophrenia. Biol. Psychiatry 48, 641–650.
Joyal, C.C., Laakso, M.P., Tiihonen, J., Syvälathi, E., Vilkman, H.,Laakso, A., Alakare, B., Räkköläinen, V., Salokangas, R.K.R.,Hietala, J., 2002. A volumetric MRI study of the entorhinal cortexin first episode neuroleptic–naïve schizophrenia. Biol. Psychiatry51, 1005–1007.
Kalus, P., Buri, C., Slotboom, J., Gralla, J., Remonda, L., Dierks, T.,Strik, W.K., Schroth, G., Kiefer, C., 2004. Volumetry and diffusiontensor imaging of hippocampal subregions in schizophrenia.Neuroreport 15, 867–871.
Kalus, P., Slotboom, J., Gallinat, J., Federspiel, A., Gralla, J.,Remonda, L., Strik, W.K., Schroth, G., Kiefer, C., 2005. Newevidence for involvement of the entorhinal region in schizo-phrenia: a combined MRI volumetric and DTI study. Neuroimage24, 1122–1129.
Kalus, P., Slotboom, J., Gallinat, J.,Mahlberg, R., Cattapan-Ludewig,K.,Wiest, R., Nyffeler, T., Buri, C., Federspiel, A., Kunz, D.,Schroth, G., Kiefer, C., 2006. Examining the gateway to thelimbic system with diffusion tensor imaging: the perforantpathway in dementia. Neuroimage 30, 713–720.
Keshavan,M.S., Diwadkar, V., Rosenberg, D.R., 2005. Developmentalbiomarkers in schizophrenia and other psychiatric disorders:common origins, different trajectories. Epidemiol. Psychiatr. Soc.14, 188–193.
Kovalenko, S., Bergmann, A., Schneider-Axmann, T., Ovary, I.,Majtenyi, K., Havas, L., Honer, W.G., Bogerts, B., Falkai, P., 2003.Regio entorhinalis in schizophrenia: more evidence for migrationaldisturbances and suggestions for new biological hypothesis.Pharmacopsychiatry 36 (Suppl. 3) , 158–161.
Lisman, J.E., Otmakhova, N.A., 2001. Storage, recall, and noveltydetection of sequences by the hippocampus: elaborating onSOCRATIC model to account for normal and aberrant effects ofdopamine. Hippocampus 11, 551–568.
McClure, R.K., Phillips, I., Jazayerli, R., Barnett, A., Coppola, R.,Weinberger, D.R., 2006. Regional change morphometry inschizophrenia associated with antipsychotic treatment. Psych.Res.: Neuroimaging 148, 121–132.
Nasrallah, H.A., Sharma, S., Olson, S., 1997. The volume of theentorhinal cortex in schizophrenia: a controlled MRI study.Progr. Neuropsychopharmacol. Biol . Psychiatry 21,1317–1322.
Nelson, M.D., Saykin, A.J., Flashman, L.A., Riordan, H.J., 1998.Hippocampal volume reduction in schizophrenia as assessedby magnetic resonance imaging. Arch. Gen. Psychiatry 55,433–440.
Pantelis, C., Yucel, M., Wood, S.J., Velakoulis, D., Sun, D., Berger, G.,Stuart, G.W., Young, A., Phillips, L., McGorry, P.D., 2005.Structural brain imaging evidence for multiple processes at
different stages of brain development in schizophrenia. Schizophr.Bull. 31, 672–696.
Pearlson, G.D., Barta, P.E., Powers, R.E., Menon, R.R., Richards, S.S.,Aylward, E.H., Federman, E.B., Chase, G.A., Petty, R.G., Tien, A.Y.,1997. Medial and superior temporal gyral volumes and cerebralasymmetry in schizophrenia versus bipolar disorder. Biol. Psychiatry41, 1–14.
Pillai, A., Mahadik, S.P., 2006. Diffential effects of haloperidol andolanzapine on levels of vascular endothelial growth factor andangiogenesis in rat hippocampus. Schizophr. Res. 87, 48–59.
Prasad, K.M.R., Keshavan, M.S., 2003. Corrupt memory retrievalhypothesis of delusions. Proceedings of the American College ofNeuropsychopharmacology. Nashville, Tenn. ACNP, p. 117.
Prasad, K.M.R., Patel, A.R., Muddasani, S., Sweeney, J., Keshavan, M.S.,2004. The entorhinal cortex in first episode psychotic disorders: astructural magnetic resonance imaging study. Am. J. Psychiatry 161,1612–1619.
Pruessner, J.C., Kohler, S., Crane, J., Pruessner, M., Lord, C., Byrne, A.,Kabani, N., Collins, D.L., Evans, A.C., 2002. Volumetry oftemporopolar, perirhinal, entorhinal and parahippocampal cortexfrom high-resolution MRI images: considering the variability of thecollateral sulcus. Cereb. Cortex 12, 1342–1353.
Rioux, L., Nissanov, J., Lauber, K., Bilker, W.B., Arnold, S.E., 2003.Distribution of microtubule-associated protein MAP2-immunor-eactive interstitial neurons in the parahippocampal white matter insubjects with schizophrenia. Am. J. Psychiatry 160, 149–155.
Sim, K., DeWitt, I., Ditman, T., Zalesak, M., Greenhouse, I., Goff, D.,Weiss, A.P., Heckers, S., 2006. Hippocampal and parahippocampalvolumes in schizophrenia: a structural MRI study. Schizophr. Bull.32, 332–340.
Staal, W.G., Hulshoff Pol, H.E., Schnack, H.G., Hoogendoorn, M.L.,Jellema, K., Kahn, R.S., 2000. Structural brain abnormalities inpatients with schizophrenia and their healthy siblings. Am. J.Psychiatry 157, 416–421.
Steen, R.G., Mull, C., McClure, R., Hamer, R.M., Lieberman, J.A.,2006. Brain volume in first-episode schizophrenia: systematicreview and meta-analysis of magnetic resonance imaging studies.Br. J. Psychiatry 188, 510–518.
Talamini, L.M., Koch, T., Ter Horst, G.J., Korf, J., 1998. Methylazox-ymethanol acetate-induced abnormalities in the entorhinal cortexof the rat; parallels with morphological findings in schizophrenia.Brain Res. 789, 293–306.
Tansella, M., Burti, L., 2003. Integrating evaluative research andcommunity basedmental health care in Verona Italy. Br. J. Psychiatry183, 167–169.
Turetsky, B.I., Moberg, P.J., Roalf, D.R., Arnold, S.E., Gur, R.E.,2003. Decrements in volume of anterior ventromedial temporallobe and olfactory dysfunction in schizophrenia. Arch. Gen.Psychiatry 60, 1193–1200.
Velakoulis, D., Wood, S.J., Wong, M.T., McGorry, P.D., Yung, A.,Phillips, L., Brewer, W., Proffitt, T., Desmond, P., Pantelis, C.,2006. Hippocampal and amygdala volumes in according topsychosis stage and diagnosis: a magnetic resonance imagingstudy of chronic schizophrenia, first-episode psychosis, and ultra-high risk individuals. Arch. Gen. Psychiatry 63, 139–149.
Ventura, J., Nuechterlein, K.H., Subotnik, K.L., Gutkind, D., Gilbert, E.A.,2000. Symptom dimensions in recent-onset schizophrenia andmania: a principal component analysis of the 24-item BriefPsychiatric Rating Scale. Psychiatry Res. 97, 129–135.
Vita, A., De Peri, L., Silenzi, C., Dieci, M., 2006. Brain morphology infirst episode schizophrenia: a meta-analysis of quantitativemagnetic resonance imaging studies. Schizophr. Res. 82, 75–88.
180 M. Baiano et al. / Schizophrenia Research 102 (2008) 171–180
Walker, M.A., Highley, J.R., Esiri, M.M., McDonald, B., Roberts, H.C.,Evans, S.P., Crow, T.J., 2002. Estimated neuronal populations andvolumes of the hippocampus and its subfields in schizophrenia.Am. J. Psychiatry 159, 821–828.
Weinberger, D.R., 1999. Cell biology of the hippocampal formation inschizophrenia. Biol. Psychiatry 45, 395–402.
Weiss, A.P., Dewitt, I., Goff, D., Ditman, T., Heckers, S., 2005.Anterior and posterior hippocampal volumes in schizophrenia.Schizophr. Res. 73, 103–112.
World Health Organization, 1992. Schedules for Clinical Assessmentin Neuropsychiatry. WHO, Geneva.
World Health Organization, 1996. Schede di valutazione clinica inneuropsichiatria. SCAN 2.1. In: Tansella, M., Nardini, M., Serieseditors. Roma: Il Pensiero Scientifico Editore.
Related Documents