Acta Neuropathol (2007) 114:221–229 DOI 10.1007/s00401-007-0261-2 123 ORIGINAL PAPER Co-morbidity of TDP-43 proteinopathy in Lewy body related diseases Hanae Nakashima-Yasuda · Kunihiro Uryu · John Robinson · Sharon X. Xie · Howard Hurtig · John E. Duda · Steven E. Arnold · Andrew Siderowf · Murray Grossman · James B. Leverenz · Randy Woltjer · Oscar L. Lopez · Ronald Hamilton · Debby W. Tsuang · Douglas Galasko · Eliezer Masliah · JeVrey Kaye · Christopher M. Clark · Thomas J. Montine · Virginia M. -Y. Lee · John Q. Trojanowski Received: 15 May 2007 / Revised: 22 June 2007 / Accepted: 25 June 2007 / Published online: 25 July 2007 © Springer-Verlag 2007 Abstract Here, we investigated if TAR-DNA-binding protein-43 (TDP-43), the disease protein in frontotemporal lobar degeneration and ubiquitin inclusions with or without motor neuron disease as well as amyotrophic lateral sclero- sis, also formed inclusions in Lewy body (LB) disorders including Parkinson’s disease (PD) without or with demen- tia (PDD), and dementia with LBs (DLB) alone or in association with Alzheimer’s disease (AD). Immunohisto- chemical analyses of TDP-43 in clinically well character- ized and pathologically conWrmed cases of DLB + AD, PD and PDD demonstrated TDP-43 pathology in the following percentage of cases: DLB + AD = 25/80 (31.3%); PD = 5/69 (7.2%); PDD = 4/21 (19%), while DLB and normal controls exhibited no (0/10, 0%) and one cases (1/33, 3%) presenting TDP-43 pathology, respectively. SigniWcant diVerences in the prevalence of TDP-43 lesions were noted between disease versus normal brains (P < 0.001) as well as demented versus non-demented brains (P < 0.001). Sta- tistical analyses revealed a positive relationship between TDP-43 lesions and several clinical and pathological parameters in these disorders suggesting the TDP-43 pathology may have co-morbid eVects in LB diseases. This study expands the concept of TDP-43 proteinopathies by implicating TDP-43 lesions in mechanisms of neurodegen- eration in LB disorders. Hanae Nakashima-Yasuda and Kunihiro Uryu are equally contributed Wrst authors. H. Nakashima-Yasuda · K. Uryu · J. Robinson · V. M. -Y. Lee · J. Q. Trojanowski (&) Department of Pathology and Laboratory Medicine, Center for Neurodegenerative Disease Research, University of Pennsylvania School of Medicine, HUP/Maloney 3rd Floor, Philadelphia, PA 19104-4283, USA e-mail: [email protected] J. Q. Trojanowski Institute on Aging, University of Pennsylvania School of Medicine, Philadelphia, PA, USA H. Hurtig · J. E. Duda · A. Siderowf · M. Grossman · C. M. Clark Department of Neurology, University of Pennsylvania School of Medicine, Philadelphia, PA, USA S. X. Xie Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia, PA, USA S. E. Arnold Department of Psychiatry, University of Pennsylvania School of Medicine, Philadelphia, PA, USA J. E. Duda Parkinson’s Disease Research, Education and Clinical Center, Philadelphia VAMC, Philadelphia, PA, USA J. B. Leverenz · D. W. Tsuang Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA, USA J. B. Leverenz Department of Neurology, University of Washington, Seattle, WA, USA R. Woltjer · T. J. Montine Department of Pathology, University of Washington, Seattle, WA, USA J. B. Leverenz Mental Illness Research, Education, and Clinical Center, VA Puget Sound Health Care System, Seattle, WA, USA J. B. Leverenz · D. W. Tsuang Parkinson’s Disease Research, Education, and Clinical Center, VA Puget Sound Health Care System, Seattle, WA, USA

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Acta Neuropathol (2007) 114:221–229
DOI 10.1007/s00401-007-0261-2ORIGINAL PAPER
Co-morbidity of TDP-43 proteinopathy in Lewy body related diseases
Hanae Nakashima-Yasuda · Kunihiro Uryu · John Robinson · Sharon X. Xie · Howard Hurtig · John E. Duda · Steven E. Arnold · Andrew Siderowf · Murray Grossman · James B. Leverenz · Randy Woltjer · Oscar L. Lopez · Ronald Hamilton · Debby W. Tsuang · Douglas Galasko · Eliezer Masliah · JeVrey Kaye · Christopher M. Clark · Thomas J. Montine · Virginia M. -Y. Lee · John Q. Trojanowski
Received: 15 May 2007 / Revised: 22 June 2007 / Accepted: 25 June 2007 / Published online: 25 July 2007© Springer-Verlag 2007
Abstract Here, we investigated if TAR-DNA-bindingprotein-43 (TDP-43), the disease protein in frontotemporallobar degeneration and ubiquitin inclusions with or withoutmotor neuron disease as well as amyotrophic lateral sclero-sis, also formed inclusions in Lewy body (LB) disordersincluding Parkinson’s disease (PD) without or with demen-tia (PDD), and dementia with LBs (DLB) alone or inassociation with Alzheimer’s disease (AD). Immunohisto-chemical analyses of TDP-43 in clinically well character-ized and pathologically conWrmed cases of DLB + AD, PDand PDD demonstrated TDP-43 pathology in the following
percentage of cases: DLB + AD = 25/80 (31.3%); PD =5/69 (7.2%); PDD = 4/21 (19%), while DLB and normalcontrols exhibited no (0/10, 0%) and one cases (1/33, 3%)presenting TDP-43 pathology, respectively. SigniWcantdiVerences in the prevalence of TDP-43 lesions were notedbetween disease versus normal brains (P < 0.001) as wellas demented versus non-demented brains (P < 0.001). Sta-tistical analyses revealed a positive relationship betweenTDP-43 lesions and several clinical and pathologicalparameters in these disorders suggesting the TDP-43pathology may have co-morbid eVects in LB diseases. Thisstudy expands the concept of TDP-43 proteinopathies byimplicating TDP-43 lesions in mechanisms of neurodegen-eration in LB disorders.
Hanae Nakashima-Yasuda and Kunihiro Uryu are equally contributed Wrst authors.
H. Nakashima-Yasuda · K. Uryu · J. Robinson · V. M. -Y. Lee · J. Q. Trojanowski (&)Department of Pathology and Laboratory Medicine, Center for Neurodegenerative Disease Research, University of Pennsylvania School of Medicine, HUP/Maloney 3rd Floor, Philadelphia, PA 19104-4283, USAe-mail: [email protected]
J. Q. TrojanowskiInstitute on Aging, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
H. Hurtig · J. E. Duda · A. Siderowf · M. Grossman · C. M. ClarkDepartment of Neurology, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
S. X. XieDepartment of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
S. E. ArnoldDepartment of Psychiatry, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
J. E. DudaParkinson’s Disease Research, Education and Clinical Center, Philadelphia VAMC, Philadelphia, PA, USA
J. B. Leverenz · D. W. TsuangDepartment of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA, USA
J. B. LeverenzDepartment of Neurology, University of Washington, Seattle, WA, USA
R. Woltjer · T. J. MontineDepartment of Pathology, University of Washington, Seattle, WA, USA
J. B. LeverenzMental Illness Research, Education, and Clinical Center, VA Puget Sound Health Care System, Seattle, WA, USA
J. B. Leverenz · D. W. TsuangParkinson’s Disease Research, Education, and Clinical Center, VA Puget Sound Health Care System, Seattle, WA, USA
123
222 Acta Neuropathol (2007) 114:221–229
Keywords Frontotemporal lobar degeneration · TDP-43 · Dementia with Lewy bodies · Parkinson’s disease
Introduction
Neurodegenerative diseases are characterized by intracellu-lar and extracellular protein aggregates in the central ner-vous system and many of these disorders are classiWed asdisease speciWc proteinopathies as exempliWed by tauopa-thies, �-synucleinopathies, polyglutamine repeat diseases,prion protein diseases [8] and the newly recognized groupof disorders known as TAR-DNA-binding protein-43(TDP-43) proteinopathies [22]. These proteinopathies mayshare common disease mechanisms linked to pathologicalconformational changes, post-translational modiWcations,or cell localization of speciWc proteins that become insolu-ble leading to the formation of abnormal protein aggregatesor inclusions. Understanding how these pathological pro-teins contribute to mechanisms of neurodegenerative dis-eases will open up new avenues for better diagnostics andtherapeutics for these disorders.
Frontotemporal lobar degeneration (FTLD) is a clinically,genetically and pathologically heterogeneous group of disor-ders that is the second most common cause of dementia afterAlzheimer’s disease (AD) in individuals <65 years of age.Frontotemporal lobar degeneration with ubiquitin-positive(FTLD-U), tau-negative inclusions is the most commonpathologic form of FTLD [9]. Recently, TDP-43, a nuclearprotein implicated in exon skipping and transcription regula-tion [3, 4, 21], was identiWed as the major pathological pro-tein in inclusions of sporadic and familial FTLD-U with andwithout motor neuron disease (MND) as well as in amyo-trophic lateral sclerosis (ALS) [22]. This initial observationwas rapidly conWrmed and extended [2, 5, 6, 13, 16, 18].Together, these reports suggest a mechanistic link between
FTLD-U and ALS, which may represent diVerent clinicalmanifestations of neurodegenerative diseases referred tonow as TDP-43 proteinopathies.
Although AD is characterized by pathologically Wbrillartau and �-amyloid lesions, >50% of AD brains contain Wla-mentous �-synuclein inclusions, and a subgroup of ADcases may be diagnosed with concomitant Parkinson’s dis-ease (PD) or dementia with Lewy bodies (DLB) [19]. Simi-larly, DLB commonly co-occurs with AD. Since a recentstudy showed that TDP-43 pathology occurs in »30% of allAD brains [1], we investigated the prevalence of TDP-43pathology in clinically well characterized and pathologi-cally conWrmed cases of Lewy body (LB) disease includingDLB, DLB + AD, PD without and with dementia (PDD).We report the variable presence of TDP-43 pathology inthese LB disorders thereby expanding the concept of TDP-43 proteinopathies.
Materials and methods
Case selection and pathological assessment
Fixed, paraYn-embedded 6 �m thick sections of brainsincluding hippocampus and entorhinal cortex sectionsfrom all autopsied enrolled patients were obtained fromWve NIA-funded AD Centers (University of Washington,Seattle, WA, USA; University of Pittsburgh, Pittsburgh,PA, USA; University of California San Diego, San Diego,CA, USA; Oregon Health & Sciences University, Port-land, OR, USA; University of Pennsylvania, Philadelphia,PA, USA) to screen for TDP-43 positive lesions sincethese regions are consistently aVected in TDP-43 protein-opathies [2]. All cases were diagnosed by trained neuropa-thologists in accordance with published guidelines for AD[28], DLB [19], PD [10] and diVerent pathological vari-ants of FTLD [20]. Each disease group was deWned as fol-lows: for the DLB + AD group cases had a high andintermediate likelihood for both DLB [19] and AD criteria[28], for the DLB group cases had a high and intermediatelikelihood for DLB criteria [19] and no or low likelihoodfor AD [28]. Furthermore PD cases were diagnosed basedon Gelb et al. [10]. PDD cases are pathologically similarto DLB, however, motor impairment preceded in PDD byat least 1 year [19]. Aged matched normal cases wereselected for non-disease control. A total of 213 cases wereexamined including: DLB + AD (n = 80), DLB (n = 10),PD (n = 69), PDD (n = 21) and normal controls (n = 33).Several previously published FTLD-U cases representingsubtypes 1, 2 and 3 of FTLD-U were used as positive con-trols. Demographics of the patients, including diagnoses,age at onset, age at death disease duration and gender areindicated in Table 1.
O. L. LopezDepartment of Neurology, University of Pittsburgh, Pittsburgh, PA, USA
R. HamiltonDepartment of Pathology, University of Pittsburgh, Pittsburgh, PA, USA
D. Galasko · E. MasliahDepartment of Neuroscience, University of California-San Diego, San Diego, CA, USA
E. MasliahDepartment of Pathology, University of California-San Diego, San Diego, CA, USA
J. KayeDepartment of Neurology, Oregon Health & Sciences University, Portland, OR, USA
123
Acta Neuropathol (2007) 114:221–229 223
To investigate hippocampal cell loss in cornu ammonis(CA), subiculum and entorhinal cortex, we scored neuron lossand gliosis from 0 to 3 as described previously [31]. BrieXy,stage 0 indicated neither cell loss nor gliosis, stage1 indicatedno cell loss but gliosis, stage 2 had mild to moderate cell losswith gliosis and stage 3 showed prominent neuron loss andgliosis based on evaluation of H and E stained sections.
Immunohistochemical evaluation
Sections of brain including hippocampus and entorhinalcortex from all cases were screened by immunohistochem-istry (IHC) for TDP-43 positive pathological inclusions.IHC was performed as described previously using the avi-din–biotin complex detection system (Vector Laboratories,Burlingame, CA, USA) and 3,3-diaminobenzidine as chro-mogen [25]. Antigen retrieval included pretreatment bymicrowaving in 10 mmol/l citrate buVer as described else-where [22, 23]. Antibodies used in this study were rabbitpolyclonal anti-TDP-43 antibodies (1:4,500 Protein, TechGroup, Chicago, IL, USA), rabbit polyclonal anti-ubiquitinantibodies (1:2,000, DAKO, Glostrup, Denmark) mouseanti-ubiquitin monoclonal antibodies (MAb1510, 1:40,000,Chemicon International Inc., Temecula, CA, USA), mouseanti-nitrated alpha-synuclein (MAb syn303, 1:4,000) [7],mouse anti-phosphorylated tau (MAb PHF1, 1:2,000, a giftfrom Dr P. Davies). Negative and positive controls for IHCstudies were performed as reported [14]. Neuropathologicaland IHC examination was done by three individuals (HNY,JR and KU) independently and together using a triple-headteaching microscope (Nikon Eclipse 50i, Tokyo, Japan).Photographs were captured using a digital camera (Olym-pus DP71, Tokyo, Japan) connected with a microscope(Olympus BX51 microscope, Tokyo, Japan).
Double staining
Double Xuorescent IHC (DFIHC) was performed asdescribed previously [30] by co-incubation of brain sec-tions with two primary antibodies, one raised in mice(ubiquitin, tau or �-synuclein) and the other in rabbits(TDP-43), followed co-incubation with secondary anti-mouse and anti-rabbit antibodies conjugated to Alexa Fluor
488 (Invitrogen Corporation, Carlsbad, CA, USA) andAlexa Fluor 594 (Invitrogen) [30], and Wnally treatment forblocking autoXuorescence [24]. These sections were cov-erslipped using Vectorshield mounting medium (VectorLaboratories, Burlingame, CA, USA) with 4,6-diamino-2-phenylindole (1 �g/ml). Negative and positive controls forDFIHC studies were performed as reported [14]. Analysisof the DFIHC was performed with an Olympus BX51microscope (Tokyo, Japan) and photographs were capturedusing a digital camera (Olympus DP71, Tokyo, Japan).
Statistic analyses
For statistical analysis, the degree of cell loss in each casewas categorized as being either insigniWcant (0 and 1) orsigniWcant (2 and 3). Furthermore, to analyze the relation-ship between frequency of TDP-43 pathology and stage ofAD pathology all cases were categorized into one of fourstages based on Braak and Braak staging as follow;none = no neuroWbrillary tangles (NFTs), low = I–II,intermediate = III–IV and severe = V–VI.
Statistic analyses were performed by a statistician (SXX)in the University of Pennsylvania AD Center. Two sample t-test was used to compare the mean values of age at onset ageat death and duration between TDP-43 positive and TDP-43negative groups within each disease category. Fisher’s exacttest was used to compare the extent of neuron loss betweenTDP-43 positive and TDP-43 negative groups within eachdisease category, to compare the proportion of TDP-43 posi-tive patients between demented versus non-demented aswell as between disease versus normal, and to examine theassociation between AD stage and TDP pathology. Analyseswere performed using SAS software (version 9.1, SAS Insti-tute Inc, Cary, NC, USA). All Statistical tests were two-sided. Statistical signiWcance was set at the 0.05 level.
Results
Distribution of TDP-43 pathology
TAR-DNA-binding protein-43 IHC was performed on hip-pocampal and entorhinal cortical sections of the brains
Table 1 Demographics of LB related disease cases examined in this study
Patients(n)
Age at onset (years)
Age at death (years)
Disease duration (years)
Gender—male:female% (n)
Dementia groupa 111 67.7 § 8.8 77.9 § 7.1 10.2 § 5.6 64.0:36.0 (71:40)
DLB + AD 80 68.8 § 7.9 78.3 § 7.1 9.4 § 4.3 57.5:42.5 (46:34)
DLB 10 67.0 § 3.2 75.8 § 3.3 8.7 § 3.5 90.0:10.0 (9:1)
PDD 21 63.6 § 12.5 77.6 § 8.4 14.2 § 8.6 76.2:23.8 (16:5)
PD 69 59.3 § 12.6 75.3 § 9.9 15.8 § 7.2 69.6:30.4 (48:21)
Normal 33 n/a 75.5 § 12.1 n/a 42.4:57.6 (14:19)
a Dementia group represents all patients from DLB + AD, DLB and PDD disease categories
123
224 Acta Neuropathol (2007) 114:221–229
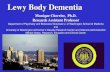
from patients with various LB related neurodegenerativediseases, including DLB + AD, DLB, PDD and PD as wellas the brains of normal control patients to assay for the sig-nature lesions of FTLD-U, i.e., ubiquitin and TDP-43 posi-tive inclusion since one or both of these regions always areaVected in TDP-43 proteinopathies [2, 9, 19]. ConWrmedFTLD-U cases, including Type-1, Type-2 and Type-3based on previously deWned categories of Sampathu et al.[25] (corresponding to Type-2, Type-3 and Type-1, respec-tively, of Mackenzie et al [17]) were analyzed. TDP-43IHC revealed the ubiquitous distribution of normal TDP-43nuclear staining in neurons of all brains. We also observedthe presence of TDP-43 positive inclusions with variablefrequency in selected neurons of the brains of a subset ofLB disease patients. The distribution patterns and morpho-logical proWles of pathology in these brains matched theoriginal description of TDP-43 pathology in FTLD-U/MND cases [22] (Fig. 1). All positive cases possessed neu-ronal perinuclear cytoplasm inclusions (NCIs) of granularcells in the dentate gyrus (Figs. 1, 2b–d). TDP-43 positiveLB disorder brains showed simultaneous existence of inclu-sions in the dentate gyrus and entorhinal cortex, with only afew cases presenting CA1-4 inclusions in the hippocampus.In addition, short and thin neuritic threads and/or perinu-
clear inclusions were observed to a lesser extent (Fig. 2a, f).The majority (»95%) of these TDP-43 positive LB disor-der brains exhibited NCIs and short neuritic threads in thesuperWcial layers of entorhinal cortex (Fig. 2a, e–g) [22,25], while few of these cases (»5%) showed the presenceof NCIs devoid of threads. Rare neurons with NFT-likeproWle contained focal TDP-43 positive staining (Fig. 2h).The majority of TDP-43 positive LB disorder cases werecategorized as Type-3 (Fig. 2a) and the few cases showingNCIs devoid of threads were categorized as Type-2. Therewere no cases categorized as Type-1. In addition, sectionsof hippocampus and entorhinal cortex from the normal con-trol group did not show any TDP-43 inclusions with theexception of a normal 98-year-old individual whose brainexhibited a number of TDP-43 positive threads in the CAregion, but no TDP-43 positive NCIs. Notably, no neuronalintranuclear inclusions (NIIs) were seen in any of the brainsexamined here.
Co-localization of TDP-43, ubiquitin, tau and �-synuclein
Co-localization of pathological TDP-43 with ubiquitin, tauor �-synuclein positive inclusions was examined byDFIHC. Ubiquitinated TDP-43 was readily observable.
Fig. 1 TAR-DNA-binding pro-tein-43 IHC photomicrographs illustrate TDP-43 positive patho-logical inclusions in dentate gyrus granular cells in various disease brains; a FTLD-U, b nor-mal control, c DLB + AD, d DLB, e PD and f PDD. The brains of subset patients from all LB disease groups, except DLB, demonstrated TDP-43 immuno-reactive inclusions in granular neurons of the dentate gyrus. The scale bar = 50 �m in all images
123
Acta Neuropathol (2007) 114:221–229 225
Pathological cytoplasmic and neuritic TDP-43 preciselyco-localized with ubiquitin as detected by Xuorescent immuno-reactivity. Normal nuclear TDP-43 staining was not associ-ated with ubiquitin staining (Fig. 3a–f). In contrast, taupositive NFTs and threads in disease brains were devoid ofTDP-43 positivity (Fig. 3h–m), but NFTs occasionally
were associated with reduced nuclear TDP-43 staining(Fig. 3k–m), suggesting cell death or degeneration, andvery rare NFTs showed association with cytoplasmic TDP-43 positive staining. (Fig. 3n–p).
The majority of TDP-43 perinuclear aggregates were notco-localized with �-synuclein staining (Fig. 3q–s), but rare
Fig. 2 Distribution pattern and morphology of TDP-43 pathology inthe entorhinal cortex from LB disease brains. Most TDP-43 positivecases (»95%) exhibited TDP-43 stained threads and/or perinuclearcytoplasmic inclusions in the entorhinal cortex (a, e–h) and the dentategyrus (b–d). These photomicrographs exemplify the morphological
features of the TDP-43 pathology in the LB disease brains examinedhere; DLB + AD (a–c, e–g), PDD (d). A NFT-like proWle with focalTDP-43 immunoreactivity was seen on rare occasions (h). The scalebar = 30 �m in all images
123
226 Acta Neuropathol (2007) 114:221–229
dystrophic neurites showed co-existing of �-synuclein andTDP-43 pathology (Fig. 3t–v), which may reXect accumu-lation of these proteins due to blocked transport in theaVected processes.
Cell loss in hippocampus
The relationship of cell loss and TDP-43 pathology in eachgroup was assessed and summarized as follow: DLB + AD
Fig. 3 Double label IHC in DLB + AD brains to examine co-localiza-tion of ubiquitin, tau, �-synuclein and TDP-43. Both dense cytoplas-mic (a–c) and skine-like (d–f) TDP-43 positive inclusions were shownto co-localize with ubiquitin. Tau positive NFTs were almost alwaysTDP-43 negative (h–j, k–m), but some neurons showed tau and TDP-
43 positive inclusions that co-existed in the same cell without co-local-izing with each other (n–p). The majority of �-synuclein pathology isTDP-43 negative (q–s), but rarely there was co-localization of TDP-43with �-synuclein positive threads (t–v). The scale bar = 30 �m in allimages
123
Acta Neuropathol (2007) 114:221–229 227
with TDP-43 positive = 15/25 (60%), DLB + AD withTDP-43 negative = 13/55 (23.6%), DLB with TDP-43negative = 1/10 (10%), PDD with TDP-43 positive = 2/4(50%), PDD with TDP-43 negative = 0/17 (0%), PD withTDP-43 positive = 0/5 (0%), PD with TDP-43 negative =0/64 (0%), normal control with TDP-43 positive = 0/1 (0%)and normal control with TDP-43 negative = 1/32 (3.1%).
Statistical analysis
The prevalence of TDP-43 positive cases varied amongthese LB disorders as follows: DLB + AD = 25/80 (31.3%),DLB = 0/10 (0%), PD = 5/69 (7.2%), PDD = 4/21 (19%)and normal control = 1/33 (3%). SigniWcant diVerenceswere noted between demented group (DLB + AD, DLB,PDD) and non-demented group (normal control and PD)(P < 0.02) as well as disease group and normal controlgroup (P < 0.001) with respect to the presence of TDP-43pathology. Examination of the co-relationship between theprevalence of TDP-43 inclusions and the LB disordersillustrated that there was no single factor associated withTDP-43 proteinopathy. Nonetheless, in the dementiapatients as an entire group and in the PDD group alone,average age at death in the TDP-43 positive patients wassigniWcantly higher. Further, in the entire dementia patientsgroup alone, the percentage of males in the TDP-43positive cases was signiWcantly lower than in the TDP-43negative cases. There was no statistical diVerence with
respect to age at onset and duration of disease betweenTDP-43 positive and TDP-43 negative patients in AD/DLB, PDD, PD as well as dementia group in total. Therewere statistically signiWcant relationship between neuronloss and TDP-43 positive inclusions in entire dementia(P < 0.0001), DLB + AD (P < 0.01) and PDD (P < 0.05)groups (Table 2). DLB + AD cases indicated positive rela-tionship between ratio of TDP-43 occurrence and fre-quency of AD pathology. More speciWcally, as thefrequency of AD pathology increased, as indicated byBraak and Braak stage, the ratio of TDP-43 pathologicalinvolvement increased as follows: none = 6/106 (5.7%),low = 3/18 (16.7%), intermediate = 8/51 (15.7%) andsevere = 18/38 (47.4%). The severer Braak and Braak stagebecomes, the higher TDP-43 pathogenesis occurs(P < 0.0001).
Discussion
The current study revealed TDP-43 inclusions in LB disor-ders and the burden of this TDP-43 pathology varied sig-niWcantly among the disorders studied here including DLB+ AD, pure PD and PDD. This study is signiWcant because
it expands the deWnition of TDP-43 proteinopathies. SinceNeumann et al. [22] initially described TDP-43 as a majorubiquitinated component of FTLD-U and sporadic ALSinclusions, there has been rapid conWrmation and extension
Table 2 TAR-DNA-binding protein-43 pathology in LB related diseases and relationship with variable factors
Comparisons of gender and hippocampal cell loss between TDP-43 positive group and TDP-43 negative group were done through Fisher’s exacttest within each disease category; comparisons of age at onset, age at death and duration of disease between TDP-43 positive group and TDP-43negative group were done through two-sample t-test within each disease category
M male, F female, sd standard deviationa Dementia group represents all patients from DLB + AD, DLB and PDD disease categoriesb SigniWcant diVerence between TDP-43 positive group and TDP-43 negative group for the factor under study (P < 0.05)c SigniWcant diVerence between TDP-43 positive group and TDP-43 negative group for the factor under study (P < 0.01)d CS neuron loss was scored (0, 1+, 2+, 3+) according to neuropathological standards; while signiWcant cell loss was deWned as 2+ or 3+
TDP-43 pathology
Ratio of pathology % (n)
Gender Age at onset Age at death Duration of disease Hippocampal cell lossd
% (M:F) P value mean § sd P-value mean § sd P-value Mean § sd P-value % P-value
Dementia groupa
+ 26.0 (29) 44.8:55.2 0.023b 70.1 § 6.7 0.09 80.5 § 6.5 0.024b 10.4 § 6.4 0.86 58.6 <0.0001c
¡ 74.0 (82) 70.7:29.3 66.8 § 9.3 77.0 § 7.1 10.2 § 5.3 17.1
DLB + AD + 31.3 (25) 40.0:60.0 0.050 69.6 § 6.7 0.56 79.4 § 6.0 0.34 9.8 § 5.6 0.58 60.0 0.0024c
¡ 68.7 (55) 65.5:34.5 68.5 § 8.4 77.8 § 7.5 9.2 § 3.7 23.6
DLB + 0.0 (0) n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
¡ 100.0 (10) 90.0:10.0 67.0 § 3.2 75.8 § 3.3 8.7 § 3.5 10.0
PDD + 19.0 (4) 75.0:25.0 1.00 73.3 § 7.4 0.08 87.0 § 5.6 0.0086c 13.8 § 9.8 0.91 50.0 0.028b
¡ 81.0 (17) 76.5:23.5 61.1 § 12.4 75.4 § 7.4 14.3 § 8.6 0.0
PD + 7.2 (5) 100.0:0.0 0.31 67.6 § 7.3 0.13 83.6 § 7.7 0.051 16.0 § 6.0 0.94 0.0 n/a
¡ 92.8 (64) 67.2:32.8 58.7 § 10.6 74.7 § 9.8 15.8 § 7.3 0.0
Normal + 3.0 (1) 100.0:0.0 0.42 n/a n/a 98.00 0.06 n/a n/a 0.0 1.00
¡ 97.0 (32) 40.6:59.4 n/a 74.8 § 11.6 n/a 3.1
123
228 Acta Neuropathol (2007) 114:221–229
of these Wndings [5, 6, 17, 27] including evidence thatTDP-43 proteinopathy underlies most or all FTLD-Ucaused by progranulin gene mutations [16, 26], at leastsome cases of Guam parkinsonism–dementia complex [13],and many cases of AD with and without prominent hippo-campal sclerosis [1, 2].
Here we extended these observations further to deWnethe prevalence of TDP-43 pathology in LB disorders andshow that the morphology and distribution pattern of ubiqu-itin and TDP-43 positive inclusions in LB diseases are sim-ilar to those reported by Sampathu et al. and Neuman et al.in FTLD-U brains [22, 25]. Further, as in these and otherreports, neurons with cytoplasmic TDP-43 inclusionsshowed a loss of normal nuclear TDP-43 staining consis-tent with a loss of TDP-43 nuclear function in aVected neu-rons. There are some noticeable diVerences in histologicalcharacteristics of the pathology, however, between LB dis-eases and FTLD-U, since LB diseases showed more TDP-43 positive NCI than threads, and we did not detect anyNIIs in the LB diseases examined here, in addition, sincethe distribution of these pathologies was conWned mostly tothe superWcial layers of cortex, DLB + AD and PD/PDDconforms largely to Type-3 TDP-43 pathology.
The Wndings here also emphasize the complexity of neu-rodegenerative diseases including LB disorders due to thefrequent co-occurrence of diverse pathologies in the samepatient. This is best exempliWed here by DLB + ADwherein 31.3% (25/80) of these cases had concomitantTDP-43 proteinopathy. Furthermore there was signiWcantpositive correlation between tau pathology burden and fre-quency of TDP-43 pathology occurrence in DLB + ADgroup. While the basis for this remains to be explained,there is evidence that tau and �-synuclein can promote theWbrillization of each other in vitro [11] and that the misfold-ing and aggregation of a disease protein may disrupt normalcellular mechanisms thereby predisposing other proteins toaggregate [12]. These mechanistic considerations notwith-standing, growing evidence underlines the importance ofrecognizing the frequent overlap of the pathological andclinical features of patients with tauopathies and �-synuc-leinopathies [15, 29]. Clearly, further clinico-pathologicalstudies are needed to translate these new observations into abetter understanding of the signiWcance of the added burdenof TDP-43 pathology to the cognitive and motor impair-ments in DLB + AD, PD and PDD. Indeed a recent study ofthe burden of TDP-43 pathology in AD with and withouthippocampal sclerosis [1] showed that overall »30% of ADpatients develop an associated TDP-43 proteinopathy. Inthe current study as well, positive correlation between cellloss in the hippocampus and TDP-43 pathogenesis wasseen. Thus, the extent to which AD pathology versus �-syn-uclein lesions drive the accumulation of TDP-43 pathologyin DLB + AD remains to be determined, but the study by
Amador-Ortiz et al. [14] may signify that AD rather thanLB pathology is the more dominant risk factor for TDP-43proteinopathy. The impact of this Wnding on the clinicalmanifestations of dementia and the prodromal dementiarequires better understanding since this could be importantin the early detection of dementia and eVorts to developbetter diagnostics and therapeutics for neurological disor-ders with dementia.
Acknowledgments We thank colleagues for technical support andadvice in the Center for Neurodegenerative Disease Research. Wethank the families of patients whose generosity made this research pos-sible. This work was supported by grants from the National Institutesof Health (AG-09215, AG-10124, AG-17586). V.M.-Y.L. is the JohnH. Ware III Professor of Alzheimer’s disease research; and J.Q.T. isthe William Maul Measey-Truman G. Schnabel Jr, Professor of Geri-atric Medicine and Gerontology.
References
1. Amador-Ortiz C, Lin WL, Ahmed Z, Personett D, Davies P, DuaraR, GraV-Radford NR, Hutton ML, Dickson DW (2007) TDP-43immunoreactivity in hippocampal sclerosis and Alzheimer's dis-ease. Ann Neurol 61:435–445
2. Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H,Mann D, Tsuchiya K, Yoshida M, Hashizume Y, Oda T (2006)TDP-43 is a component of ubiquitin-positive tau-negative inclu-sions in frontotemporal lobar degeneration and amyotrophic later-al sclerosis. Biochem Biophys Res Commun 351:602–611
3. Buratti E, Dork T, Zuccato E, Pagani F, Romano M, Baralle FE(2001) Nuclear factor TDP-43 and SR proteins promote in vitroand in vivo CFTR exon 9 skipping. EMBO J 20:1774–1784
4. Buratti E, Brindisi A, Pagani F, Baralle FE (2004) Nuclear factorTDP-43 binds to the polymorphic TG repeats in CFTR intron 8and causes skipping of exon 9: a functional link with diseasepenetrance. Am J Hum Genet 74:1322–1325
5. Cairns NJ, Neumann M, Bigio EH, Holm IE, Troost D, HatanpaaKJ, Foong C, White CL III, Schneider JA, Kretzschmar HA, Cart-er D, Paulsmeyer K, Strider J, Gitcho M, Goate AM, Morris JC,Mishra M, Kwong LK, Stieber A, Xu Y, Forman MS, TrojanowskiJQ, Lee VM-Y, Mackenzie IR (2007) TDP-43 in Familial andSporadic Frontotemporal Lobar Degeneration with UbiquitinInclusions. Am J Pathol 171:227–240
6. Davidson Y, Kelley T, Mackenzie IR, Pickering-Brown S, Du PD,Neary D, Snowden JS, Mann DM (2007) Ubiquitinated pathologicallesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol (Berl) 113:521–533
7. Duda JE, Giasson BI, Mabon ME, Lee VM-Y, Trojanowski JQ(2002) Novel antibodies to synuclein show abundant striatalpathology in Lewy body diseases. Ann Neurol 52:205–210
8. Forman MS, Trojanowski JQ, Lee VM-Y (2004) Neurodegenera-tive diseases: a decade of discoveries paves the way for therapeuticbreakthroughs. Nat Med 10:1055–1063
9. Forman MS, Farmer J, Johnson JK, Clark CM, Arnold SE, CoslettHB, Chatterjee A, Hurtig HI, Karlawish JH, Rosen HJ, Van DV,Lee VM-Y, Miller BL, Trojanowski JQ, Grossman M (2006)Frontotemporal dementia: clinicopathological correlations. AnnNeurol 59:952–962
10. Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkin-son disease. Arch Neurol 56:33–39
11. Giasson BI, Forman MS, Higuchi M, Golbe LI, Graves CL,Kotzbauer PT, Trojanowski JQ, Lee VM-Y (2003) Initiation and
123
Acta Neuropathol (2007) 114:221–229 229
synergistic Wbrillization of tau and alpha-synuclein. Science300:636–640
12. Gidalevitz T, Ben Zvi A, Ho KH, Brignull HR, Morimoto RI(2006) Progressive disruption of cellular protein folding in modelsof polyglutamine diseases. Science 311:1471–1474
13. Hasegawa M, Arai T, Akiyama H, Nonaka T, Mori H, HashimotoT, Yamazaki M, Oyanagi K (2007) TDP-43 is deposited in theGuam parkinsonism-dementia complex brains. Brain 130:1386–1394
14. Horiguchi T, Uryu K, Giasson BI, Ischiropoulos H, LightFoot R,Bellmann C, Richter-Landsberg C, Lee VM-Y, Trojanowski JQ(2003) Nitration of tau protein is linked to neurodegeneration intauopathies. Am J Pathol 163:1021–1031
15. Lee VM-Y, Giasson BI, Trojanowski JQ (2004) More than justtwo peas in a pod: common amyloidogenic properties of tau andalpha-synuclein in neurodegenerative diseases. Trends Neurosci27:129–134
16. Leverenz JB, Yu CE, Montine TJ, Steinbart E, Bekris LM, Zabe-tian C, Kwong LK, Lee VM-Y, Schellenberg GD, Bird TD (2007)A novel progranulin mutation associated with variable clinicalpresentation and tau, TDP43 and alpha-synuclein pathology. Brain130:1360–1374
17. Mackenzie IR, Baborie A, Pickering-Brown S, Du PD, Jaros E,Perry RH, Neary D, Snowden JS, Mann DM (2006) Heterogeneityof ubiquitin pathology in frontotemporal lobar degeneration: clas-siWcation and relation to clinical phenotype. Acta Neuropathol(Berl) 112:539–549
18. Mackenzie IR, Baker M, Pickering-Brown S, Hsiung GY, Lind-holm C, Dwosh E, Gass J, Cannon A, Rademakers R, Hutton M,Feldman HH (2006) The neuropathology of frontotemporal lobardegeneration caused by mutations in the progranulin gene. Brain129:3081–3090
19. McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, FeldmanH, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H,Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B,Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G,Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, KennyRA, Korczyn A, Kosaka K, Lee VM-Y, Lees A, Litvan I, LondosE, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ,Yamada M (2005) Diagnosis and management of dementia withLewy bodies: third report of the DLB consortium. Neurology65:1863–1872
20. McKhann GM, Albert MS, Grossman M, Miller B, Dickson D,Trojanowski JQ (2001) Clinical and pathological diagnosis offrontotemporal dementia: report of the work group on frontotem-poral dementia and Pick’s disease. Arch Neurol 58:1803–1809
21. Mercado PA, Ayala YM, Romano M, Buratti E, Baralle FE (2005)Depletion of TDP 43 overrides the need for exonic and intronicsplicing enhancers in the human apoA-II gene. Nucleic Acids Res33:6000–6010
22. Neumann M, Sampathu DM, Kwong LK, Truax AC, MicsenyiMC, Chou TT, Bruce J, Schuck T, Grossman M, Clark CM,McCluskey LF, Miller BL, Masliah E, Mackenzie IR, Feldman H,Feiden W, Kretzschmar HA, Trojanowski JQ, Lee VM-Y (2006)Ubiquitinated TDP-43 in frontotemporal lobar degeneration andamyotrophic lateral sclerosis. Science 314:130–133
23. Neumann M, Mackenzie IR, Cairns NJ, Boyer PJ, MarkesberyWR, Smith CD, Taylor JP, Kretzschmar HA, Kimonis VE, For-man MS (2007) TDP-43 in the ubiquitin pathology of frontotem-poral dementia with VCP gene mutations. J Neuropathol ExpNeurol 66:152–157
24. Romijn HJ, van Uum JFM, Breedijk I, Emmering J, Radu I, PoolCW (1999) Double immunolabeling of neuropeptides in the hu-man hypothalamus as analyzed by confocal laser scanning Xuores-cence microscopy. J Histochem Cytochem 47:229–236
25. Sampathu DM, Neumann M, Kwong LK, Chou TT, Micsenyi M,Truax A, Bruce J, Grossman M, Trojanowski JQ, Lee VM-Y(2006) Pathological heterogeneity of frontotemporal lobar degen-eration with ubiquitin-positive inclusions delineated by ubiquitinimmunohistochemistry and novel monoclonal antibodies. Am JPathol 169:1343–1352
26. Seelaar H, Jurgen SH, Azmani A, Kusters B, Rosso S, Majoor-Krakauer D, de Rijik MC, Rizzu P, Brummelhuis MT, van DoornPA, Kamphorst W, Willemsen R, van Swieten JC (2007) TDP-43pathology in familial frontotemporal dementia and motor neurondisease without Progranulin mutations. Brain 130:1375–1385
27. Tan CF, Eguchi H, Tagawa A, Onodera O, Iwasaki T, Tsujino A,Nishizawa M, Kakita A, Takahashi H (2007) TDP-43 immunore-activity in neuronal inclusions in familial amyotrophic lateral scle-rosis with or without SOD1 gene mutation. Acta Neuropathol(Berl) 113:535–542
28. The National Institute of Aging, Reagan Institute Working Group(1997) Consensus recommendations for the postmortem diagnosisof Alzheimer’s disease. The National Institute on Aging, and Rea-gan Institute Working Group on diagnostic criteria for the neuro-pathological assessment of Alzheimer's disease. Neurobiol Aging18:S1–S2
29. Trojanowski JQ, Mattson MP (2003) Overview of protein aggre-gation in single, double, and triple neurodegenerative brain amy-loidoses. Neuromolecular Med 4:1–6
30. Uryu K, Richter-Landsberg C, Welch W, Sun E, Goldbaum O, Nor-ris EH, Pham CT, Yazawa I, Hilburger K, Micsenyi M, Giasson BI,Bonini NM, Lee VM-Y, Trojanowski JQ (2006) Convergence ofheat shock protein 90 with ubiquitin in Wlamentous alpha-synucleininclusions of alpha-synucleinopathies. Am J Pathol 168:947–961
31. Yokota O, Tsuchiya K, Oda T, Ishihara T, de Silva R, Lees AJ,Arai T, Uchihara T, Ishizu H, Kuroda S, Akiyama H (2006) Am-yotrophic lateral sclerosis with dementia: an autopsy case showingmany Bunina bodies, tau-positive neuronal and astrocytic plaque-like pathologies, and pallido-nigral degeneration. Acta Neuropa-thol 112:633–645
123
Related Documents