dmm.biologists.org 580 Introduction The prognosis for cancer patients is generally poor once cancer cells have metastasized (American Cancer Society, 2011), and metastasis is therefore a major clinical problem. Nevertheless, studies in mouse models suggest that it is an inefficient process, because the majority of disseminating cancer cells never successfully invade a distant organ but die in the vasculature (Wong et al., 2001; Chambers et al., 2002; Hunter et al., 2008; Kouros- Mehr et al., 2008). Genetic changes in the cancer cells and contributions from the microenvironment are both crucial for the establishment of metastatic lesions (Bos et al., 2009; Joyce and Pollard, 2009). The microenvironment plays a role via, for example, the production of growth factors, cytokines and proteases, and both primary and metastatic tumors can recruit host cells, such as bone- marrow-derived macrophages, to promote angiogenesis (the formation of new blood vessels from pre-existing vessels) and invasion (Joyce and Pollard, 2009). Traditionally, studies on metastasis have relied on measurements made at the end-point of the process: the establishment of micro- or macrometastasis. However, such methods do not address the dynamic aspect of the metastatic process: cells exit the primary tumor, invade the local tissue, enter blood or lymphatic vessels (a process known as ‘intravasation’), and are passively transported to the secondary site where the cells exit the vessels (a process known as ‘extravasation’) and enter the tissue (Fig. 1) (Fidler, 2003; Kim et al., 2009a). To gain insight into the dynamics of metastasis, different types of imaging technologies have been applied to animal models (Box 1). Bioluminescence imaging has been used to track luciferase- expressing cancer cells and thus to determine their ability to metastasize at the organism level. Live microscopy with expression of fluorescent proteins [e.g. green and red fluorescent proteins (GFP and RFP, respectively)] by cancer and stromal cells has provided insights into what types of behavior and cell-cell interactions differentiate metastatic and non-metastatic cancer cells (Fig. 1). Here, we review some of the most important biological insights into the process of metastasis that have been gained through different types of imaging technologies. These insights include how the cancer cells interact with their surrounding microenvironment, the stroma, which refers to all connective tissue within an organ, such as the extracellular matrix (ECM), the vasculature, the fibroblasts and the immune cells. Leaving the primary site The first step in the metastatic process is for the cancer cells to leave the primary tumor site. Live imaging has in particular provided insights into how the dynamics of the tumor-stroma interactions at the primary site contribute to metastasis. Moving through the tissue Cancer cells initiate dissemination when they breach the basement membrane (an ECM barrier consisting of e.g. laminin, type IV collagen and proteoglycans that surrounds epithelial, endothelial, muscle, fat and nerve cells). Once the cancer cell breaches the basement membrane, it comes into contact with the interstitial ECM, which is rich in fibrillar collagens. Second harmonic generation (SHG) imaging allows for visualization of fibrillar ECM proteins, primarily collagens. Because of their molecular structure, these proteins have the capacity to combine photons from light REVIEW Disease Models & Mechanisms 6, 580-593 (2013) doi:10.1242/dmm.009282 1 Cold Spring Harbor Laboratory, 1 Bungtown Road, Cold Spring Harbor, NY 11724, USA 2 Stony Brook University, Graduate Program in Genetics, 130 Life Sciences Building, Stony Brook, NY 11794, USA *Author for correspondence ([email protected]) © 2013. Published by The Company of Biologists Ltd This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial Share Alike License (http://creativecommons.org/licenses/by-nc-sa/3.0), which permits unrestricted non-commercial use, distribution and reproduction in any medium provided that the original work is properly cited and all further distributions of the work or adaptation are subject to the same Creative Commons License terms. The prognosis of metastatic cancer in patients is poor. Interfering with metastatic spread is therefore important for achieving better survival from cancer. Metastatic disease is established through a series of steps, including breaching of the basement membrane, intravasation and survival in lymphatic or blood vessels, extravasation, and growth at distant sites. Yet, although we know the steps involved in metastasis, the cellular and molecular mechanisms of dissemination and colonization of distant organs are incompletely understood. Here, we review the important insights into the metastatic process that have been gained specifically through the use of imaging technologies in murine, chicken embryo and zebrafish model systems, including high-resolution two-photon microscopy and bioluminescence. We further discuss how imaging technologies are beginning to allow researchers to address the role of regional activation of specific molecular pathways in the metastatic process. These technologies are shedding light, literally, on almost every step of the metastatic process, particularly with regards to the dynamics and plasticity of the disseminating cancer cells and the active participation of the microenvironment in the processes. Caught in the act: revealing the metastatic process by live imaging Miriam R. Fein 1,2 and Mikala Egeblad 1, * Disease Models & Mechanisms DMM

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
dmm.biologists.org580
IntroductionThe prognosis for cancer patients is generally poor once cancercells have metastasized (American Cancer Society, 2011), andmetastasis is therefore a major clinical problem. Nevertheless,studies in mouse models suggest that it is an inefficient process,because the majority of disseminating cancer cells neversuccessfully invade a distant organ but die in the vasculature (Wonget al., 2001; Chambers et al., 2002; Hunter et al., 2008; Kouros-Mehr et al., 2008). Genetic changes in the cancer cells andcontributions from the microenvironment are both crucial for theestablishment of metastatic lesions (Bos et al., 2009; Joyce andPollard, 2009). The microenvironment plays a role via, for example,the production of growth factors, cytokines and proteases, and bothprimary and metastatic tumors can recruit host cells, such as bone-marrow-derived macrophages, to promote angiogenesis (theformation of new blood vessels from pre-existing vessels) andinvasion (Joyce and Pollard, 2009).
Traditionally, studies on metastasis have relied on measurementsmade at the end-point of the process: the establishment of micro-or macrometastasis. However, such methods do not address thedynamic aspect of the metastatic process: cells exit the primarytumor, invade the local tissue, enter blood or lymphatic vessels (aprocess known as ‘intravasation’), and are passively transported tothe secondary site where the cells exit the vessels (a process known
as ‘extravasation’) and enter the tissue (Fig. 1) (Fidler, 2003; Kim etal., 2009a). To gain insight into the dynamics of metastasis, differenttypes of imaging technologies have been applied to animal models(Box 1). Bioluminescence imaging has been used to track luciferase-expressing cancer cells and thus to determine their ability tometastasize at the organism level. Live microscopy with expressionof fluorescent proteins [e.g. green and red fluorescent proteins (GFPand RFP, respectively)] by cancer and stromal cells has providedinsights into what types of behavior and cell-cell interactionsdifferentiate metastatic and non-metastatic cancer cells (Fig. 1).Here, we review some of the most important biological insightsinto the process of metastasis that have been gained throughdifferent types of imaging technologies. These insights include howthe cancer cells interact with their surrounding microenvironment,the stroma, which refers to all connective tissue within an organ,such as the extracellular matrix (ECM), the vasculature, thefibroblasts and the immune cells.
Leaving the primary siteThe first step in the metastatic process is for the cancer cells toleave the primary tumor site. Live imaging has in particularprovided insights into how the dynamics of the tumor-stromainteractions at the primary site contribute to metastasis.
Moving through the tissueCancer cells initiate dissemination when they breach the basementmembrane (an ECM barrier consisting of e.g. laminin, type IVcollagen and proteoglycans that surrounds epithelial, endothelial,muscle, fat and nerve cells). Once the cancer cell breaches thebasement membrane, it comes into contact with the interstitialECM, which is rich in fibrillar collagens. Second harmonicgeneration (SHG) imaging allows for visualization of fibrillar ECMproteins, primarily collagens. Because of their molecular structure,these proteins have the capacity to combine photons from light
REVIEW Disease Models & Mechanisms 6, 580-593 (2013) doi:10.1242/dmm.009282
1Cold Spring Harbor Laboratory, 1 Bungtown Road, Cold Spring Harbor, NY 11724,USA2Stony Brook University, Graduate Program in Genetics, 130 Life Sciences Building,Stony Brook, NY 11794, USA*Author for correspondence ([email protected])
© 2013. Published by The Company of Biologists LtdThis is an Open Access article distributed under the terms of the Creative Commons AttributionNon-Commercial Share Alike License (http://creativecommons.org/licenses/by-nc-sa/3.0), whichpermits unrestricted non-commercial use, distribution and reproduction in any medium providedthat the original work is properly cited and all further distributions of the work or adaptation aresubject to the same Creative Commons License terms.
The prognosis of metastatic cancer in patients is poor. Interfering with metastatic spread is therefore important forachieving better survival from cancer. Metastatic disease is established through a series of steps, including breaching ofthe basement membrane, intravasation and survival in lymphatic or blood vessels, extravasation, and growth at distantsites. Yet, although we know the steps involved in metastasis, the cellular and molecular mechanisms of disseminationand colonization of distant organs are incompletely understood. Here, we review the important insights into themetastatic process that have been gained specifically through the use of imaging technologies in murine, chickenembryo and zebrafish model systems, including high-resolution two-photon microscopy and bioluminescence. Wefurther discuss how imaging technologies are beginning to allow researchers to address the role of regional activationof specific molecular pathways in the metastatic process. These technologies are shedding light, literally, on almostevery step of the metastatic process, particularly with regards to the dynamics and plasticity of the disseminatingcancer cells and the active participation of the microenvironment in the processes.
Caught in the act: revealing the metastatic processby live imagingMiriam R. Fein1,2 and Mikala Egeblad1,*
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 581
Live imaging of the metastatic process REVIEW
Host cell
Tumor cell
Macrophage
T cell
NeutrophilFibroblastChemokines
Blood vessel
Lymphatic vessel
F Colonization E Extravasation
D Intravasation
C Cell migration
BA D
C
E
F
A Lymphangiogenesis B Angiogenesis
Key
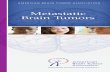
Fig. 1. Live imaging of the metastatic process. Central cartoon summarizes the metastatic stages detailed in A-F. (A)Top: blood (green) and lymphatic (red)vessels in an ear with a transplanted T241 fibrosarcoma cell line overexpressing the growth factor VEGF-C were visualized with simultaneous angiography andlymphangiography (using FITC- and TRITC-conjugated dextrans). Tumor blood and lymphatic vessels were dilated compared with normal ear (not shown). Scalebar: 850 μm. Bottom: GFP-positive T241 fibrosarcoma cells (green) in a lymphatic vessel (arrowheads; red; tetramethyl-rhodamine lymphangiography), travelingfrom the primary tumor to the cervical lymph node. Scale bar: 100 μm. Reprinted with permission (Hoshida et al., 2006). (B)Angiogenesis imaged in a dorsalskinfold window chamber by fluorescence microscopy after transplantation of GFP-labeled 4T1 mammary carcinoma cells (green) in a BALB/c mouse. Red arrowin the day 2 panel indicates an elongated cancer cell. In the day 8 panel, purple arrows point to microvessels within the tumor (localized in the marked circle),and red arrows point to dilated vasculature outside the tumor. Scale bars: 200 μm. Reprinted with permission (Li et al., 2000). (C)GFP-labeled MTLn3 mammarycarcinoma cells (green) move along collagen fibers (purple), visualized by second-harmonic generation (SHG) imaging. Arrows are pointing to carcinoma cells,and arrowheads are pointing to cell-matrix interactions. Scale bar: 25 μm. Reprinted with permission (Condeelis and Segall, 2003). (D)Intravasation of GFP-labeled MTLn3 mammary carcinoma cells (green) into a dextran-labeled blood vessel (red) imaged by multiphoton microscopy. Three cells that have crossed intothe blood vessel are yellow, indicated by arrows. Scale bar: 25 μm. Reprinted with permission (Condeelis and Segall, 2003). (E)Imaging extravasation intransgenic zebrafish embryos. Confocal image of a non-extravasating, wild-type (expressing CFP, colored blue) or extravasating and twist overexpressing (co-expressing RFP and colored red) MDA-MB-231 human breast cancer cell. Cells are shown near the intersegmental vessels (ISV) of a zebrafish embryo, inside (in)or extravasated (out) from the vessel lumen. Scale bar: 200 μm. Reprinted with permission (Stoletov et al., 2010). (F)The establishment of a micrometastasis(‘colonization’) in the liver of a BALB/c mouse. Mouse C26 colorectal carcinoma cells (cyan, expressing fluorescent Dendra2) shown by repeated imaging throughan abdominal imaging window. Fibrillar collagens (purple) are detected by SHG imaging. Scale bars: 20 μm. Reprinted with permission (Ritsma et al., 2012).
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org582
Live imaging of the metastatic processREVIEW
directed at them and effectively double the frequency with preciselyhalf the wavelength of the original photons, enabling imagingwithout the need for exogenous labeling. SHG is a non-linearprocess that requires high-intensity light generated by a pulsed laser,and it is therefore often combined with multi-photon microscopy(Box 1) (Campagnola and Loew, 2003). Using SHG imaging, cancercells were found to migrate more rapidly through murine tissuewhen they were in close association with collagen fibers than whenthey were not, potentially facilitated by integrin-mediatedinteractions with the fibers (Condeelis and Segall, 2003) (Fig. 1C).Furthermore, metastatic cancer cells, in contrast to non-metastaticcells, attached to and move along collagen fibers (Wang et al., 2002).The motility of cancer cells, as they move through the tissue, canalso be enhanced by tumor-associated macrophages. Indeed,imaging has shown that mammary carcinoma cells move along withmacrophages in a streaming cell movement (Roussos et al., 2011)(see supplementary material Movie 1). This can occur via aparacrine loop, in which cancer cells secrete colony-stimulatingfactor 1 (CSF-1) to attract macrophages, leading to macrophageactivation and secretion of ligands, such as epidermal growth factor,which in turn stimulates cancer cell movement (Wyckoff et al.,2004). Directional motility towards blood vessels is proposed to bean important factor in determining the rate of metastasis, becauseit leads to an increase in the number of cancer cells that canintravasate. The directional migration probably involves the release
of chemoattractants from vascular endothelial cells or theirsupporting cells (Condeelis and Segall, 2003).
Imaging studies have further revealed at least two major typesof cellular movement through the ECM: protease-dependent and-independent migration (Madsen and Sahai, 2010) (Fig. 2).Protease-dependent migration relies mainly on membrane-anchored matrix metalloproteinase (MMP) activity (Rowe andWeiss, 2008). There are 23 MMP family members expressed inhumans and they play a role in regulating tumor angiogenesis,invasiveness and metastasis by cleaving a diverse group of substrates(Kessenbrock et al., 2010). One MMP in particular, MMP14 [alsoknown as membrane-type 1 matrix metalloproteinase (MT1-MMP)], has been shown to be crucial for cell invasion andmorphogenesis in three-dimensional type I collagen matrices usedto mimic the interstitial ECM (Hotary et al., 2000; Sabeh et al.,2004). Although expression of MMP14 can confer epithelial cancercells the ability to invade, animal experiments using tissuerecombination between MMP14-proficient and -deficient cancerand stromal cells strongly suggest that MMP14 expressed bystromal cells mediates cancer cell metastasis (Szabova et al., 2008).The mechanism by which stromal MMP14 promotes invasion andmetastasis is not clear, but it is likely to involve degradation offibrillar collagen in the interstitial matrix.
MMP14 is a cell-membrane-anchored MMP, but most MMPsare secreted, commonly by stromal cells (reviewed by Kessenbrocket al., 2010). Several of these MMPs are also important for invasivebehavior, either through degradation of structural components ofthe ECM or through activation of chemokine and growth factorsthat stimulate invasion (Kessenbrock et al., 2010). Nevertheless,when synthetic MMP inhibitors were tested in the clinical setting,they had no effect on patient survival (Coussens et al., 2002). Onelikely contributing factor to this failure was that most clinical studiestested the effect of MMP inhibitors on end-stage cancer, after theestablishment of metastatic disease. Imaging experiments, however,have offered an alternative, intriguing explanation for the lack ofclinical results: when proteases are blocked, cancer cells cancompensate for the loss of protease activity by using amoeboid- ormesenchymal-type movement to disseminate into the adjacenttissue as individual cells (Friedl and Wolf, 2003; Wolf et al., 2003;Wolf et al., 2007). Thus, in the absence of proteolytic ECMbreakdown, the cells instead change their shape (Fig. 2) andtemporarily deform the ECM (not shown) (Friedl and Alexander,2011; Wolf and Friedl, 2011).
To date, most work on the function of MMPs in invasion hasbeen performed in culture on two-dimensional or three-dimensional matrices, which cannot faithfully recapitulate the fullcomplexity of the ECM or of the different cell types in tumors.However, fluorogenic MMP substrates can now be used to assessthe proteolytic activity of MMPs, as well as the efficacy of theirinhibition, in vivo, in tumors (Weissleder et al., 1999; Bremer et al.,2001; Littlepage et al., 2010). Future studies will therefore probablygive additional insights into the importance, or lack thereof, ofspecific MMPs in vivo.
Even in tumors generated from an established metastatic rodentmammary carcinoma cell line, only a small proportion (1-5%) ofcancer cells are highly motile, and the type of motility (cohesiveversus single-cell amoeboid motility) within the tumors isheterogeneous (Giampieri et al., 2009). The heterogeneity in
Box 1. Common methods in live imaging ofmetastasisBioluminescence imaging: Bioluminescence imaging is based on thedetection of light produced during enzyme-mediated oxidation of a molecularsubstrate when the enzyme (e.g. firefly, Renilla, green click beetle or red clickbeetle luciferase) is expressed as a molecular reporter. Light emission fromluciferase-catalyzed reactions can penetrate through several centimeters oftissue, and the substrate is non-toxic and has a relatively short half-life in vivo,which makes imaging internal organs over multiple sessions possible (Sadikotand Blackwell, 2005).Multiphoton microscopy: Several recent reviews discuss the advances inhigh-resolution microscopy techniques for studies of metastasis, cell division,cell death, cell migration and cell-cell communication (Condeelis andWeissleder, 2010; Beerling et al., 2011; Pittet and Weissleder, 2011). The mostcommonly used technique is multiphoton microscopy, which uses short pulsesof infrared laser light to excite fluorophores, while the emitted light is detectedusing photomultipliers. Under optimal circumstances, excited and emittedlight penetrates tissues up to 1000 μm, although 200-300 μm is a commonlimit. Labeling cells for confocal or multiphoton microscopy is accomplished byexpression of fluorescent proteins. Injectable imaging agents, e.g. fluorescentdextran, are also commonly used (Condeelis and Weissleder, 2010). Livemicroscopy techniques have been particularly useful for imaging cellularbehaviors in tumors, such as migration, intravasation, extravasation, and cell-cell or cell-ECM interactions.Bioluminescence imaging and multiphoton microscopy have vastlydifferent uses. Bioluminescence is very sensitive and does not require externalillumination in order to generate a signal, but has low resolution. In contrast,high-resolution microscopic imaging with fluorophores requires an excitationsource and can suffer from poor light penetration and problems with tissueautofluorescence. Bioluminescence is useful for tracking cell activities ornumbers in deep tissues over time spans of weeks, such as for followingchanges in metastatic burdens in lungs. In contrast, live microscopy allows forhigh-resolution analysis of cell activities, including migration or signalingresponses, during time spans of minutes to days (Prescher and Contag, 2010).
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 583
Live imaging of the metastatic process REVIEW
motility might reflect heterogeneity within the cancer cellpopulation. However, another possible explanation is that cancercell motility is influenced by factors from the microenvironmentthat are unevenly present within the tumor. Transforming growthfactor beta (TGFβ) could be one such factor; it is present in themicroenvironment and influences migratory behavior of cells.Using fluorescent reporter constructs, it was shown that cells withtransient and local activation of TGFβ signaling pathwaysdisseminate as single cells and spread through blood vessels (seesupplementary material Movies 2, 3). In contrast, collectivemigration of carcinoma cells does not rely on TGFβ, and such cells,which maintain contact with each other, move much slower andspread through the lymphatic system (Giampieri et al., 2009) (seesupplementary material Movie 4). Thus, these studies used liveimaging to directly link activation of a signaling pathway withspecific cellular and metastatic behaviors (Giampieri et al., 2009;Giampieri et al., 2010) (Fig. 3).
Interaction with the vasculature and lymphaticsMetastatic spread occurs through the blood and the lymphaticvasculature, and the structure and organization of these vesselstherefore impact the rate of metastasis (Fig. 1A,B). The tumorvasculature has an abnormal organization, structure and function
compared with the vasculature of normal tissues (Jain, 1988). Liveimaging has revealed that tumor blood vessels often are leaky, inpart due to incomplete coverage with pericytes, which arespecialized cells that wrap around endothelial structures (Jain, 2003;Fukumura and Jain, 2008). In addition, lymphatic vessels insidetumors have a compromised ability to transport fluid ormacromolecules, leading to a high interstitial fluid pressure insidetumors (Fukumura and Jain, 2008; Fukumura et al., 2010). Imagingof tumors after anti-angiogenic therapy using optical frequencydomain imaging (OFDI; see below) elegantly shows how tumorvessel structure is normalized after treatment (Vakoc et al., 2009)(see supplementary material Movie 5).
One experiment highlighting the importance of vasculature forthe metastatic process utilized an imaging window that wassurgically inserted over a mouse mammary carcinoma (Kedrin etal., 2008). This allowed for consecutive imaging over several daysand was used together with cancer cells engineered to express thephotoswitchable fluorescent protein Dendra2. Dendra2 is derivedfrom octocoral Dendronephthya sp. and it photoswitches from agreen to red fluorescent state in response to either visible blue orUV-violet light (e.g. 405 nm) (Gurskaya et al., 2006). When the sameareas were imaged at 0, 6 and 24 hours after photoswitching, therewas a marked decrease over time in the number of red,
Contact-dependent proteolysis Cell deformationA
B Ameboid movement
Fig. 2. Plasticity of cell migration: matrix metalloproteinases.(A)Protease-dependent and -independent migration. Black arrowsindicate the direction of migration. β1-integrin staining is shown in red;proteolytically digested collagen (Col2¾C) staining in green; reflectionindicates fibrillar extracellular matrix structures (white); DAPI stainingof nuclei is shown in blue. Nuclei are shown in inserts. Scale bars:10 μm. Left panel: contact-dependent proteolysis of migrating HT1080fibrosarcoma cells overexpressing the metalloproteinase MT1-MMP ina three-dimensional collagen matrix. Contact-dependent proteolysis isindicated with an open arrowhead and the proteolytic path isindicated with a black arrowhead. The nucleus has maintained itsellipsoid shape (asterisk, insert). Right panel: protease-inhibitedmigration (in the presence of a broad spectrum protease inhibitorcocktail, PI) with deformation of the cell nucleus (arrowheads). Thedeformation is clearly visible in the insert. Reprinted with permission(Wolf and Friedl, 2011). (B)Non-proteolytic migration (amoeboidmovement). GFP-expressing squamous cell carcinoma A431 cells(green) are shown moving into a collagen-rich matrix (red)surrounding a tumor (visualized with second harmonic generation).No proteolysis of the collagen fibers is seen. Arrows mark points of cellconstriction. Field of view is 150×180 μm. Yellow dotted lines outlinemoving cells; white dotted lines represent a fiber that a carcinoma cellmoves along. Time after initiation of imaging is indicated on the timeseries. Reprinted with permission (Sahai, 2007).
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org584
Live imaging of the metastatic processREVIEW
photoswitched cancer cells in well-vascularized regions, suggestingthat the vascular environment supported the disappearance of thecancer cells through intravasation. In contrast, there were limitedchanges in the number and location of the photoswitched cells inregions without detectable vessels (Kedrin et al., 2008) (Fig. 4A).Using this photoswitch assay, neural Wiskott-Aldrich syndromeprotein (N-WASP), a protein that regulates the polymerization ofthe actin cytoskeleton, was shown to be necessary for intravasationof cancer cells (Gligorijevic et al., 2012). N-WASP is essential forthe formation of invadopodia, which are cell-membrane protrusionswith proteolytic activity, and the data therefore suggest thatlocalized proteolysis is necessary for intravasation.
Live imaging has shown that the cancer cells that intravasate arein close proximity to perivascular tumor-associated macrophages(TAMs), suggesting that these cells facilitate the breaching of thebarrier provided by either the basement membrane or the cell-cellinteractions between endothelial cells (Wyckoff et al., 2004; Wyckoffet al., 2007). The cooperation between macrophages and cancercells is clinically relevant because a higher number of foci ofinteracting cancer cells, macrophages and endothelial cells werefound in primary breast tumors of patients that developedmetastatic disease than in tumors of patients that did not (Robinsonet al., 2009). Confocal imaging in an in vitro three-dimensionalmicrofluidic model for intravasation suggests that macrophages
A
CDii Blood vessel
Biv
Primary tumor
Non-motile cells
Single-cellmotility
Loss of cell-cellcohesion
Collective cellmotility
Non-motile
Non-motile
Di
BiBii Lymph vessel
Biii Lymph node
Diii Lungs
Div
EPrimary tumor
Fig. 3. Signaling pathways in metastasis: the role of TGFβ. Model illustrating how combinations of signals within a primary tumor can direct the mode of cellmotility. (A) Non-motile, cohesively packed cells in the primary tumor (no signal). (Bi)Cells receiving pro-motility cues (such as EGF; red circles), but not TGFβ,move cohesively and collectively via the lymphatic route (Bii), and metastasize to the lymph nodes (Biii), where the signal is lost and cells become non-motile.(Biv)Image of an MTLn3E lymph node metastasis constitutively expressing myristoylated Cherry (red) and CFP (cyan) from a SMAD-dependent promoter (notexpressed by cells in the metastasis); collagen second harmonic signal is in blue. (C) High TGFβ signals (blue circles), without pro-motility cues, cause loss of cell-cell cohesion. (Di) Pro-motility cues with TGFβ together promote single-cell motility, entry into the blood (Dii), and lung metastases (Diii). (Div)Image of anMTLn3E lung metastasis constitutively expressing myristoylated Cherry (red) and CFP (cyan) from a SMAD-dependent promoter (not expressed by cells in themetastasis); collagen second harmonic signal is in blue. (E)A primary tumor originating from MTLn3E mammary carcinoma cells constitutively expressingmyristoylated Cherry (red) and CFP (cyan) from a SMAD-dependent promoter; collagen second harmonic signal is in blue. White and yellow arrows indicatemotile cells. The marked area is shown at higher magnification at 0, 4.5 and 9 minutes. Panels Biv, Div and E are reprinted with permission (Giampieri et al., 2009),and cartoons are adapted with permission from the American Association for Cancer Research (Giampieri et al., 2010).
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 585
Live imaging of the metastatic process REVIEW
0 h 6 h 24 h
t=0 bleach recovery
B Optical frequency domain imaging
E Gradient index (GRIN) lens
A Photoswitching to track cell fates
C Fluorescence recovery after photobleaching
D Fluorescence lifetime microscopy
0 hours 6 hours 24 hours
t=0 Bleach Recovery
Photoswitched cellsTumor cells
GFP–E-cadherin
Time (h/min) 0:30 3:04 8:44
Fluorescencecollection
Fig. 4. Advances in imaging technologies. (A)Photoswitching using a mammary imaging window. Tumor cells are labeled with the photoswitchable proteinDendra2. Non-photoswitched cells (green) and photoswitched cells (red) are shown at 0, 6 and 24 hours after the photoswitch in vascular microenvironments.White dotted lines indicates a vessel. The photoswitched cells adjacent to the vessel disappear quickly over time, suggesting that they leave the primary tumorthrough intravasation. Scale bar: 30 μm. Reprinted with permission (Kedrin et al., 2008). (B)Three-dimensional microscopy using optical frequency domain imaging(OFDI) compared with multiphoton microscopy. Imaging of a murine mammary adenocarcinoma tumor in a dorsal skinfold chamber using OFDI is shown (a,c,e),compared with multiphoton microscopy (b,d,f ). c-f are higher-magnification views of the corresponding areas outlined in white on panels a and b. OFDI is superiorto multiphoton for visualizing vessels in deeper regions (c,d), whereas multiphoton microscopy has better resolution of finer structures in more superficial regions(e,f ). Depth is denoted by color: yellow (superficial) to red (deep). Scale bars: 250 μm. Reprinted with permission (Vakoc et al., 2009). (C)Fluorescence recovery afterphotobleaching (FRAP). Images of FRAP experiments of GFP–E-cadherin performed at the front of a wound heal assay. Red arrows indicate cell protrusions, andwhite arrows point to the areas photobleached in the middle panel. Reprinted with permission (Timpson et al., 2009). (D)Fluorescence lifetime microscopy (FLIM)used to monitor uptake of doxorubicin, a chemotherapeutic drug, at the invasive front of a spheroid consisting of mouse mammary MMT-DC cells. Fluorescentlifetime is visualized before (left panel) and after (middle and right panels) treatment and shows a stepwise reduction of fluorescence lifetime. False-color range: 0to 3.5 ns. Scale bar: 20 μm. Reprinted with permission (Bakker et al., 2012). (E)Use of the gradient index (GRIN) lens with a multiphoton microscope. One end of theGRIN lens is positioned close to the focal plane of the objective lens of a standard multiphoton laser-scanning microscope, with the opposite end inserted insidethe animal. A piezoelectric focus control performs fine focusing without moving the GRIN lens. Reprinted with permission (Levene et al., 2004).
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org586
Live imaging of the metastatic processREVIEW
increase the permeability of the endothelial barrier throughsecretion of tumor necrosis factor-α (TNFα) (Zervantonakis et al.,2012).
Lymphatic vessels transport antigens, immune cells and fluidsfrom tissues to the lymph nodes and back to the vascular system.They lack a continuous basement membrane and this contributesto the high permeability of these vessels and probably also to themetastatic spread of cells through lymphatic vessels, a first stepin dissemination in many human cancers (Detmar and Hirakawa,2002; Oliver and Detmar, 2002). Lymph nodes activated byinflammation or tumor growth can be imaged with immuno-positron emission tomography (PET) using radiolabeledantibodies against lymphatic endothelial cell surface markers,possibly allowing for detection of lymphangiogenesis as an earlyindicator of metastasis (Mumprecht et al., 2010). Whenfluorescent dextran is injected into tissues and tumors, thelymphatic drainage can be visualized. This has enabled imagingof cancer cells within the lymphatics and of structural changesof tumor-draining lymphatic vessels. Furthermore, by combiningfluorescent dextran labeling with fluorescence photobleachingimaging, it was shown that the velocity of the lymphatic fluid thatdrains tumors was reduced compared with that of normal tissues,but total fluid volume was increased, because of an enlargedvascular diameter (Hoshida et al., 2006). A mouse model allowingdual fluorescent and bioluminescence imaging of the lymphaticvessels, through expression of reporters under the control of thepromoter for lymphatic endothelial-specific Vegfr3 (vascularendothelial growth factor receptor 3) (Martínez-Corral et al.,2012), is likely to contribute to further insights into lymphaticmetastatic spread.
Importance of angiogenesis for supporting themetastatic processBecause dissemination often occurs via blood vessels, angiogenesissupports metastasis (Weidner et al., 1991). Insights into the biologyof angiogenesis therefore contribute to our understanding ofmetastasis. It was previously thought that angiogenesis only startedafter a tumor mass reached 1 mm in diameter and hypoxiaoccurred. Using dorsal skinfold window chambers in rats or mice,the dynamics of tumor angiogenesis can be monitored for weeksby repeated intravenous injections with fluorescein isothiocyanate(FITC)-labeled dextran, allowing for assessments of how bloodvessel diameter, surface area and branching patterns change withtumor progression (Zhou et al., 2011). This method was used todetermine that modification of the normal vasculature occursalready when the tumor consists of only 60-80 cancer cells, andthat functional, new blood vessels are established as the tumorreaches about 100-300 cells (Li et al., 2000) (Fig. 1B).
Tumor hypoxia can result in activation of angiogenesis (Harris,2002). Interestingly, the ability to respond to hypoxia by theinduction of angiogenesis might be associated with metastasisspecifically to the lungs. The levels of hypoxia were tracked intumors from two subclones of the MDA-MB-231 mammarycarcinoma cell line using firefly luciferase as a reporter for theactivity of hypoxia inducible factor-1α (HIF-1α; an indicator ofhypoxia levels). Tumors from the cell line that metastasized to thelungs had a strong angiogenic response, and hypoxia levels werereduced as the tumors grew. In contrast, tumors from the cell line
that metastasized to the bone had limited angiogenesis, andhypoxia continued to increase as the tumors grew (Lu et al., 2010).
Another model system for analysis and imaging of angiogenesisis the engrafting of human carcinoma cells into the chorioallantoicmembrane (CAM) of chick embryos before the full developmentof the immune system. The CAM is highly vascularized with adense capillary network, and it rarely exceeds 100 μm in thickness,making it very amenable for the imaging of angiogenesis.Interestingly, the ability of human fibrosarcoma and prostatecancer cells to intravasate and disseminate in this model correlatedpositively with their capacity to induce angiogenesis and to recruitneutrophils (Bekes et al., 2011).
Imaging at secondary sitesImaging at secondary sites where disseminated cancer cellsextravasate and colonize can provide crucial insights into themechanisms underlying these processes. However, this is inherentlychallenging because the organs involved (e.g. brain, lung, liver, bonemarrow) are often difficult to access while maintaining survival ofthe animals. Furthermore, getting the timing right for monitoringthe establishment of secondary lesions is difficult. However, newmethods have recently opened up possibilities in real-time imagingof metastatic sites.
Live imaging of the liver – through repeated exteriorization andstabilization of the left liver lobe in the same mouse – has allowedvisualization of the progression of angiogenesis during theestablishment of colorectal liver metastases (Tanaka et al., 2012).Another, less invasive, technique was recently developed involvingthe insertion of an imaging window over abdominal organs,including the spleen, kidney, small intestine, pancreas or liver(Ritsma et al., 2012). Once inserted, the window allows forvisualization of the same site for up to 1 month. Using thistechnology, the establishment of liver metastases was found toinvolve the extravasation of single cancer cells followed by aproliferative state with high cancer-cell motility in themicrometastatic lesions and reduced motility in the larger lesions(Fig. 1F). Intriguingly, imaging showed that, when the high cancer-cell motility in the small lesions was inhibited, metastatic burdenwas reduced (Ritsma et al., 2012).
Many mouse models of cancer develop metastasis in the lung,but this organ is particularly challenging to image for severalreasons. The alveolar structure of the lung causes a high degree oflight scattering and, in addition, the movement of the lung duringcardiorespiratory cycles makes imaging difficult (Wagner, 1969).A thoracic window has been developed, which allows imaging forseveral hours, but not days or weeks, under physiological gasexchange and blood flow. The surface of the lung adheres to thewindow loosely with 20-25 mmHg reversible vacuum, allowingnormal ventilation and physiological blood flow with limited tissuemovement in the imaging field. This system has been used to imageimmune surveillance during lung injury in mice (Looney et al.,2011), and it should be possible to also apply it to study lungmetastasis in vivo.
Homing to distant organsIt was reported as far back as 1889, by Stephen Paget, thatmetastases primarily develop in certain organs, and he thereforeproposed that the organ environment influenced metastasis
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 587
Live imaging of the metastatic process REVIEW
[reprinted in 1989 (Paget, 1989)], the so-called ‘seed and soil’hypothesis. However, the question of how this preference isestablished is still not fully understood, although factors intrinsicto the cancer cells as well as factors contributed by the specificmicroenvironment of different tissues have been identified (Nguyenet al., 2009; Chaffer and Weinberg, 2011). A microenvironmentalhoming factor in the bone marrow is stromal cell derived factor 1(SDF-1; also known as CXCL12), a potent chemoattractant for cellsexpressing the CXCR4 chemokine receptor. Several cancer cell lineswere imaged homing to specific regions of the bone marrowendothelium, and disruption of the interaction between SDF-1 andCXCR4 blocked homing of cancer cells to these regions (Sipkinset al., 2005).
In vivo studies in mouse models have shown that VEGFR1-expressing bone-marrow-derived hematopoietic progenitor cellshome to sites of future metastases before the arrival of cancer cells(Kaplan et al., 2005). One potential function of such cells could beto enhance the survival of the disseminating cells. Bioluminescenceimaging has shown that expression of vascular cell adhesionmolecule 1 (VCAM-1) in breast cancer cells increases their abilityto colonize the lung. The VCAM-1-expressing cancer cells werefound to interact with macrophages through α4 integrins and thisin turn activated a phosphoinositide-3-kinase-dependent survivalpathway (Chen et al., 2011a).
A role for another myeloid-derived cell type, the neutrophils, indetermining the site of metastasis was suggested in a disseminationmodel in zebrafish. Zebrafish embryos are optically transparentwith an immature immune system that allows forxenotransplantation of fluorescently labeled human cancer cells.Human cells can also be transplanted to adult, chemically immune-suppressed animals (Stoletov et al., 2007; Stoletov and Klemke,2008). Intravital imaging showed that, although cancer cellsdisseminated to multiple locations within the embryo, they wereonly able to extravasate and establish micrometastatic lesions atsites of physiologically high neutrophil transmigration into thetissue (He et al., 2012). Imaging further suggested that theneutrophils aided the invasive process into the tissue by modulatingthe collagen matrix (He et al., 2012). Intriguingly, the observationin the zebrafish embryo model contrasts with findings from micethat propose that metastasis to the lung is inhibited by neutrophils,as shown by bioluminescent imaging (Granot et al., 2011). Theseconflicting results could reflect species differences. However, it isalso possible that pro- and anti-metastatic effects of neutrophilsrepresent different activation stages of the cells (Fridlender andAlbelda, 2012), because neutrophils can promote intravasation inmice (Bekes et al., 2011).
ExtravasationZebrafish embryos have also been useful for high-resolutionimaging of the process of extravasation. It was found that cancercells do not damage or induce vascular leakage at the site ofextravasation, as previously thought, but instead arrest in thecapillaries and induce local vessel remodeling. The ability of cancercells to successfully extravasate is associated with their ability toadhere to the endothelium and migrate along the vascular wall.Time-lapse imaging has shown an increased number of endothelialcells and a thickening of the vascular cell wall surrounding thearrested cancer cells, as well as remodeling of the cell junctions at
the site of extravasation. The expression of Twist, a gene involvedin epithelial-to-mesenchymal transition (EMT), increased theintravascular migration and extravasation through the vessel wallof the cancer cells (Stoletov et al., 2010) (Fig. 1E; see supplementarymaterial Movie 6).
Myeloid-derived cells have been linked to increased metastasisand extravasation. Using an ex vivo intact whole lung imagingapproach, in which the lung is dissected and placed in a speciallydesigned chamber with artificial ventilation, it was shown thatcancer cell extravasation is reduced when monocyte recruitmentis blocked with a chemokine (C-C motif ) ligand 2 (CCL2)neutralizing antibody (Qian et al., 2011).
Dormancy and establishment of metastatic lesionsCancer can recur years after initial treatment or removal of theprimary tumor, providing clinical evidence that some metastaticcancer cells are dormant at distant sites for long periods of time(Aguirre-Ghiso, 2007; McGowan et al., 2009). However, it is notclear what factors regulate whether the cells stay dormant oreventually start proliferating. The primary tumor might participatein the regulation of distant dormancy: an acceleration of growthof the metastatic lesions after resection of the primary tumor hasbeen reported in mouse models of both hepatic and lung cancer(Qadri et al., 2005; Kollmar et al., 2006). It is possible that this is areflection of the ability of disseminating cancer cells to home backto the primary tumor (so-called ‘self-seeding’) (Comen et al.,2011): when the primary tumor is removed it no longer acts as a‘sink’ for disseminating cells, which might instead start to growelsewhere. Nevertheless, retrospective studies of human patientswith end-stage breast cancer show that long-term survival isimproved by resection of the primary tumor as compared withthose who did not undergo surgery (Fields et al., 2007; Zhang andYang, 2009).
Imaging can contribute to the understanding of the process ofdormancy and reactivation. Mammary carcinoma cells, whichoccasionally form liver metastases after a long latency, were loadedwith fluorescent nanospheres to trace the dilution of the dye, whichoccurs with cell division. Solitary cells with strong nanospheresignal were found up to 11 weeks after injection, indicating thesurvival of non-dividing, dormant cells (Naumov et al., 2002).Dormancy of cancer cells that have disseminated to the brain hasbeen suggested by the use of a highly sensitive magnetic resonanceimaging (MRI) technique to track cancer cells labeled with micron-sized iron oxide particles. In this model, most of the cancer cellsthat arrive at the brain disappear, but a small subset (1.5%) go onto form metastases, and a slightly larger proportion (4.5%) persistas undivided, single cells, which might represent a population ofdormant cells (Heyn et al., 2006). These types of studies using long-lasting labeling have the potential to uncover the types of cells orenvironmental factors involved in reactivation after dormancy.
Long-term fluorescent imaging of the brain can be performedin rats and mice by using cranial imaging windows (Yuan et al.,1994). Using such windows, the fate of individual metastasizingcancer cells was followed from minutes to months after intra-arterial injection of the cells. Four crucial steps of metastasisformation in the brain were identified: arrest at blood vessels,extravasation, the requirement for the cells to be in a perivascularposition in order to advance to micro- or macrometastases and,
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org588
Live imaging of the metastatic processREVIEW
finally, angiogenesis or co-option of preexisting microvasculature.Interestingly, treatment with the angiogenesis-inhibiting antibodyto VEGF (bevacizumab) induced long-term dormancy of humanlung carcinoma cells, highlighting that angiogenesis is alsoimportant at the secondary site (Kienast et al., 2010).
Bioluminescent imaging is commonly used for non-invasivemonitoring of the establishment of metastatic lesions. For example,the importance of Src activity for late-onset experimental bonemetastasis of breast cancer cells was shown by comparing theoutgrowth of bone lesions arising from cancer cells stablyexpressing luciferase and either SRC shRNA or a control shRNAconstruct (Zhang et al., 2009). Bioluminescent imaging was alsoused to show that increased expression of vascular cell adhesionmolecule 1 (VCAM-1) is important for expansion of dormantmicrometastases to overt bone metastasis (Lu et al., 2011).Metastatic lesions, as identified by bioluminescence imaging, werefurther subjected to two-photon imaging after preparation for exvivo bone explant cultures. VCAM-1 can bind to integrin α4β1 onosteoclast progenitors, and imaging of the explant cultures showedthat the velocity of cells of the monocytic lineage, probablyosteoclast progenitors, was increased when the cultures weretreated with an antibody against VCAM-1, probably owing to theinhibition of VCAM-1-mediated cell-cell adhesion. This suggestedthat recruitment of osteoclasts to dormant micrometastasesthrough upregulated VCAM-1 expression had taken place in vivoand triggered the expansion of the lesions (Lu et al., 2011).
Current limitationsLive imaging in mice, rats, chick embryos and zebrafish hasprovided insights into cancer metastasis at almost every stage ofthe process. Yet, there are limitations to these technologies, asdiscussed below, some of which could be addressed throughfurther technical developments.
Imaging of the metastatic process has mostly been performedfor tumors of superficial organs (e.g. skin and breast), and it is notclear whether this is representative of the process in organs thatare less accessible to imaging, such as pancreas, colon and ovary.Although there have been promising studies on imaging tumorsin pancreas and liver (McElroy et al., 2008; Ritsma et al., 2012;Tanaka et al., 2012), as described above, additional protocols areneeded for imaging internal organs, and particularly to imagedeeper in the tumors. In the brain, this has been achieved usinggradient index (GRIN) lenses for deep brain imaging, up to about1.5 mm below the surface of the cortex. GRIN lenses have a negativegradient in the refractive index of glass from the center of the lensto the outside edge to bend and focus light, and they are capableof resolving optical sections relatively far from the surface of thelens (Levene et al., 2004) (Fig. 4E). Imaging with such lenses might,however, lead to compression of the tissue in front of the lens,resulting in bleeding and tissue edema. Nevertheless, the use ofGRIN lenses in imaging probes seems to be a very promisingapproach for intravital imaging of internal organs (Kim et al., 2012).Other approaches are to use a small-diameter (e.g. 1.2 mm)microprobe ‘stick’ objective lens, which has been used to imageovarian cancer within the abdominal cavity in a mouse model(Williams et al., 2010), or to use fiber optic microprobes insteadof objective lenses (e.g. Lin et al., 2008). For imaging of internalorgans, tissue motion due to respiration and heartbeat can be very
limiting. Techniques to reduce motion artifacts include puttingpressure on the organ’s surface (Toiyama et al., 2010), or using amicrostage device to stabilize the organ (Cao et al., 2012).
The use of live imaging to gain insight into the biologicalprocesses of metastasis has exclusively been done in modelorganisms. However, it is unclear how well these models mimicthe metastatic process in humans. In vivo microscopy in humansis still largely in the early stages, but various microscopic techniqueshave clinical potential, e.g. for the identification of suspicious tissueregions for biopsy collection (Liu et al., 2011). Confocalendomicroscopes have been used in the clinical setting withinjection of non-targeted fluorescein to identify areas of mucosaldysplasia in the esophagus (Johnson et al., 2012). Targeted imagingusing an integrin-avβ3-directed near-infrared (NIR) fluorescentprobe could potentially be used to guide surgical resection of livermetastatic lesions in colon cancer, because colon cancer cells andtumor vasculature express integrin avβ3, whereas normal liver tissuedoes not. However, so far this method has only been validated inrodent cancer models (Hutteman et al., 2011). It might also befeasible to use imaging without contrast probes to identifypathological tissue changes by using fiber optic probes with Fouriertransform infrared spectroscopy, a technology that can detectvibrations in chemical bonds (Mackanos and Contag, 2010). Thistechnology can potentially distinguish normal from diseased tissuebecause the signal will differ between regions with differentmolecular compositions.
New directionsTracking cancer cells using live imaging has been valuable fordetermining how cancer cells move throughout the metastaticprocess. Now, new technologies are set to push the field beyondthe observation of movement of cells with, for example, approachesthat allow for the manipulation of signaling pathways in cells inreal-time in the live tissue using techniques such as photoactivation(reviewed by Timpson et al., 2011).
Primary tumors are heterogeneous, but it is generally believedthat metastases originate from a single cell of the primary tumor,as suggested by single-cell sequencing of a primary breast tumorand its liver metastasis (Navin et al., 2011). Indeed, in experimentalmodels, metastatic lesions have a clonal origin, as based on analysisof karyotypes (Fidler and Kripke, 1977; Fidler and Talmadge, 1986),or lentiviral integration sites (Winslow et al., 2011). Heterogeneityin cellular invasive behavior in primary tumors is often reported(e.g. Giampieri et al., 2009; Pinner et al., 2009). Combining liveimaging with methods to trace cancer cell lineage, for examplethrough fluorescent-based lineage-tracking techniques (Snippertet al., 2010; Schepers et al., 2012), might enable a deeperunderstanding of how heterogeneity contributes to metastasis.
EMT is a highly conserved cellular program known to play a rolein processes such as mesoderm formation, neural crestdevelopment and heart valve development. During embryogenesis,the process is reversible and mesenchymal cells can revert back toan epithelial cell state, for example during the formation of thenephron in the developing kidney (Yang and Weinberg, 2008). Ithas been suggested that, in order for cancer cells to metastasize,they must undergo EMT and acquire mesenchymal traits (Hardyet al., 2010; Wells et al., 2011). It has also been proposed that areverse EMT, mesenchymal-to-epithelial transition (MET), is
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 589
Live imaging of the metastatic process REVIEW
necessary to enable metastatic colonization, which might requirere-expression of epithelial genes and downregulation ofmesenchymal genes (Chao et al., 2011). Imaging could potentiallybe employed to address the dynamics of EMT and MET in vivoand determine the importance of cellular plasticity in metastasis.One study has taken advantage of the correlation betweenpigmentation and differentiation of melanoma cells: lessdifferentiated cells with a low level of pigmentation (resembling anEMT-like state) were migratory at the primary site and theyintravasated, whereas differentiated and pigmented cells did not.Interestingly, the cells that had established themselves at thesecondary site had high levels of pigmentation, suggesting re-differentiation (an MET-like process) (Pinner et al., 2009).Phototoxicity might have contributed to the reduced cell migrationof the pigmented cells, because pigmented cells absorb pulsed laserlight more strongly than non-pigmented cells. Nevertheless, thestudy illustrates how imaging can be employed to understand thelink between the differentiation state of cancer cells and invasivebehavior.
Intravital imaging has been combined with technologies forgenomic level analysis of the metastatic pathway only to a limiteddegree. Genes involved in invasive behavior were identified by liveimaging of cells migrating towards a microneedle containingchemoattractants (including EGF) followed by analysis of geneexpression profiles of cells collected in the needles (Wyckoff et al.,2000; Wang et al., 2003; Wang et al., 2005). Such approaches couldnow be further developed to link cellular behavior in vivo with amolecular level analysis, because single-cell genomic level analysishas become feasible (Navin et al., 2011).
The use of imaging techniques to determine the status ofsignaling activities within single cells is well established in cellculture settings and has great potential for in vivo imaging, althoughit is at this point still largely in its infancy. Adaptation of thesetechniques for in vivo imaging will be useful to gain insights intothe dynamics of signaling activity and its relationship withmetastatic cellular behavior. However, this has so far beenchallenging because the ratio of signal-to-noise often is reduced invivo, in part due to scattering and absorption of light in the livetissue (e.g. Handmaker, 1975; Cuccia et al., 2009). Furthermore,maintaining tissue viability and stability is also more difficult thanfor cell culture systems, where more optimal imaging conditionscan easily be achieved.
Techniques for molecular level imaging that have been adaptedfrom the cell culture setting and applied in vivo include fluorescencerecovery after photobleaching (FRAP). With this technique,fluorescently tagged fusion proteins are used to track changes inprotein mobility after photobleaching, the photochemicaldestruction of fluorophores (Fig. 4C). In vivo, this was used to showthat the mobility of E-cadherin in cell membranes is lower inmigratory cells than in stationary cells, and that inhibition ofmigration, through inhibition of Src, FAK or β1-integrin, reducescollective cell movement and increases E-cadherin membranemobility (Serrels et al., 2009; Canel et al., 2010). These studies showthe potential for using FRAP to understand how activation ofspecific signaling pathways influences cell migration, an importantcomponent of the metastatic process, in vivo.
To monitor the activation stage of signaling molecules in realtime, including the activation of Rho-family GTPases, fluorescence
resonance energy transfer (FRET) is a valuable technique. FRET isthe transfer of emission energy from one fluorophore to another,resulting in excitation of the latter. FRET only occurs when the twomolecules are in close proximity and it is therefore useful forstudying molecular interactions in live cells (Timpson et al., 2009).Through imaging of brain slice cultures, FRET biosensors for Rho-family GTPase activity were used to show that glioblastoma cellsthat invade along blood vessels with a single pseudopodium at theleading edge of the cell have high levels of Rac1 and Cdc42 andlow levels of RhoA activities. In contrast, slower movingglioblastoma cells within the brain parenchyma had multiplepseudopodia, and low Rac1 and Cdc42 and high RhoA activities(Hirata et al., 2012). Many other FRET biosensors have beendeveloped, including those that label protein conformationalchanges, post-translational modifications and second messengers(Sabouri-Ghomi et al., 2008), but these have not been used to anylarge extent in studies on metastasis.
Fluorophores are not just characterized by their excitation andemission spectra, but also by their unique lifetime. Fluorescentlifetime imaging microscopy (FLIM) measures the exponentialdecay in emission after the excitation of a fluorescent probe. Thefactors affecting the fluorescence lifetime include: changes in pH,temperature, ion intensity, hydrophobic properties, oxygenconcentration, molecular binding and molecular interaction byenergy transfer when two proteins approach each other (Ishikawa-Ankerhold et al., 2012). FLIM can therefore be used to provideinsights into the microenvironment surrounding a fluorescenceprobe. FLIM has recently been employed in vivo in tumors fordetection of both FRET and naturally fluorescent metabolites suchas FAD and NADH (Provenzano et al., 2009; McGinty et al., 2011;Bakker et al., 2012) (Fig. 4D). Because detection of FAD and NADHdoes not require the addition of exogenous labels, it has potentialfor use in human studies.
Nanoparticles have also been adapted for live imaging studies.They are often defined as particles ranging from 1 to 100 nm indiameter, but broadly can encompass particles up to 1000 nm indiameter (Bharali et al., 2009). Integrin lymphocyte function-associated antigen-1 (LFA-1) is an important adhesion moleculefor the interactions occurring between leukocytes and theendothelium of inflamed tissues and tumors. Super paramagneticiron oxide nanoparticles labeled with fluorescent dyes andconjugated to the I domain of LFA-1 have been used forfluorescent and MRI detection of the vasculature of tumors (Chen et al., 2011b). The design of the nanoparticles allowedvisualization of sites of inflamed vasculature by these two differenttechniques.
A triple-modality nanoparticle has enabled detection of mouseglioblastoma with MRI and intraoperative detection of tumormargins with photoacoustic and Raman imaging, resulting inaccurate tumor resection (Kircher et al., 2012). Both photoacousticand Raman imaging are technologies with great potential for liveanimal imaging. Photoacoustic imaging uses light pulses to excitemolecular imaging agents, causing thermal expansion that producesultrasound waves recorded by an ultrasound transducer (Yang etal., 2012). An advantage is that it can provide images of biologicaltissue at a greater depth than conventional optical imaging. Ramanimaging relies on detecting the so-called Raman scattering effectand allows for highly specific and sensitive detection when used
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org590
Live imaging of the metastatic processREVIEW
with surface-enhanced Raman scattering contrast agents (Keren etal., 2008).
Quantum dots are small (about 10 nm in diameter) fluorescentnanoparticles that provide a good method for long-term fluorescenttracing of cells in the body because they are chemically inert, brightand photostable. They have been used to track the delivery ofmicrospheres and migration of bone-marrow-derived cells totumors (Stroh et al., 2005). They have also been used to label tumorvessels and to visualize vascular leakage (Stroh et al., 2005; Kim etal., 2009b). Quantum dots conjugated to RGB peptides, which bindto integrin αvβ3, have been used to demonstrate heterogeneity inboth vascularity and extravasation between tumor models (Smithet al., 2010).
Optical frequency domain imaging (OFDI) is another emergingimaging technique for live animal imaging. It is based on opticalcoherence tomography (OCT), which is analogous to ultrasoundbut measures the echo time delay and magnitude of light ratherthan sound (Fujimoto, 2003). A focused laser beam scans the tissuesample while the reflected optical signals are recorded and compiledin real-time. Vessels can be detected without the use of anyexogenous contrast agents because contrast is derived fromcirculating red blood cells. Post-processing imaging analysis is usedto provide three-dimensional images and quantitative analysis(Vakoc et al., 2005; Vakoc et al., 2009). OFDI reportedly has apenetration depth of up to 2-3 mm into tissue, which exceeds thatof multi-photon microscopy. It enables imaging of wide fields ofview and has been used to visualize vascular morphology overmultiple sessions within tumors (Vakoc et al., 2009) (Fig. 4B). OFDIwas recently combined with near-infrared imaging foratherosclerotic plaque microstructure imaging using an intra-arterial catheter. This approach could detect microscopic changesassociated with plaque formation in live rabbits and is underdevelopment for use in human patients (Yoo et al., 2011).
ConclusionsVisualizing cancer and stromal cells in real-time has been crucialfor understanding cellular mechanisms of metastasis: how cellsmove from primary to secondary sites, seed and proliferate in theirnew environment. In vivo studies using confocal or two-photonmicroscopy have shown that: (1) cancer cells migrate towardschemoattractants; (2) cancer cells can migrate as single cells, insingle-cell files or collectively; (3) both protease-dependent and -independent cancer cell migration can lead to dissemination; (4)the vasculature undergoes dynamic changes; (5) macrophages andinvadopodia promote intravasation; (6) extravasation of cancer cellsis related to expression of EMT-regulating transcription factors;and (7) specific microenvironmental factors are necessary forhoming of cancer cells.
Two overall themes have emerged from imaging experiments:they have pointed to the crucial role of the tumormicroenvironment (e.g. ECM, vasculature, macrophages,fibroblasts and neutrophils) in the metastatic process, and they havehelped to visualize the dynamics of cellular movements as well asthe signaling pathways involved in these processes. The dynamicsof tumor-stroma interactions and cellular behavior required for thevarious stages of metastasis could not have been revealed by anyother means. Thus, insights from live imaging could ultimately shedlight on how to effectively treat cancer metastasis.
ACKNOWLEDGEMENTSWe thank Charles Camarda for generating the cartoons in Fig. 1, Elvin Wagenblastfor critical comments on the manuscript, and the authors and journals thatcontributed images and movies to this review.
COMPETING INTERESTSThe authors declare that they do not have any competing or financial interests.
AUTHOR CONTRIBUTIONSM.R.F. and M.E. wrote the text. M.R.F. designed the figures.
FUNDINGThis work was supported by funds (to M.E.) from the National Cancer Institute(U01 CA141451), Long Island 2 Day Walk to Fight Breast Cancer, ManhassetWomen’s Coalition Against Breast Cancer, Islip Breast Cancer Coalition, and GlenCove Cares.
SUPPLEMENTARY MATERIALSupplementary material for this article is available athttp://dmm.biologists.org/lookup/suppl/doi:10.1242/dmm.009282/-/DC1
REFERENCESAguirre-Ghiso, J. A. (2007). Models, mechanisms and clinical evidence for cancer
dormancy. Nat. Rev. Cancer 7, 834-846.American Cancer Society (2011). Cancer Facts and Figures 2011. Atlanta, GA: American
Cancer Society.Bakker, G. J., Andresen, V., Hoffman, R. M. and Friedl, P. (2012). Fluorescence
lifetime microscopy of tumor cell invasion, drug delivery, and cytotoxicity. MethodsEnzymol. 504, 109-125.
Beerling, E., Ritsma, L., Vrisekoop, N., Derksen, P. W. and van Rheenen, J. (2011).Intravital microscopy: new insights into metastasis of tumors. J. Cell Sci. 124, 299-310.
Bekes, E. M., Schweighofer, B., Kupriyanova, T. A., Zajac, E., Ardi, V. C., Quigley, J.P. and Deryugina, E. I. (2011). Tumor-recruited neutrophils and neutrophil TIMP-free MMP-9 regulate coordinately the levels of tumor angiogenesis and efficiency ofmalignant cell intravasation. Am. J. Pathol. 179, 1455-1470.
Bharali, D. J., Khalil, M., Gurbuz, M., Simone, T. M. and Mousa, S. A. (2009).Nanoparticles and cancer therapy: a concise review with emphasis on dendrimers.Int. J. Nanomedicine 4, 1-7.
Bos, P. D., Zhang, X. H., Nadal, C., Shu, W., Gomis, R. R., Nguyen, D. X., Minn, A. J.,van de Vijver, M. J., Gerald, W. L., Foekens, J. A. et al. (2009). Genes that mediatebreast cancer metastasis to the brain. Nature 459, 1005-1009.
Bremer, C., Tung, C. H. and Weissleder, R. (2001). In vivo molecular target assessmentof matrix metalloproteinase inhibition. Nat. Med. 7, 743-748.
Campagnola, P. J. and Loew, L. M. (2003). Second-harmonic imaging microscopy forvisualizing biomolecular arrays in cells, tissues and organisms. Nat. Biotechnol. 21,1356-1360.
Canel, M., Serrels, A., Miller, D., Timpson, P., Serrels, B., Frame, M. C. and Brunton,V. G. (2010). Quantitative in vivo imaging of the effects of inhibiting integrinsignaling via Src and FAK on cancer cell movement: effects on E-cadherin dynamics.Cancer Res. 70, 9413-9422.
Cao, L., Kobayakawa, S., Yoshiki, A. and Abe, K. (2012). High resolution intravitalimaging of subcellular structures of mouse abdominal organs using a microstagedevice. PLoS ONE 7, e33876.
Chaffer, C. L. and Weinberg, R. A. (2011). A perspective on cancer cell metastasis.Science 331, 1559-1564.
Chambers, A. F., Groom, A. C. and MacDonald, I. C. (2002). Dissemination andgrowth of cancer cells in metastatic sites. Nat. Rev. Cancer 2, 563-572.
Chao, Y., Wu, Q., Acquafondata, M., Dhir, R. and Wells, A. (2011). Partialmesenchymal to epithelial reverting transition in breast and prostate cancermetastases. Cancer Microenviron. 5, 19-28.
Chen, Q., Zhang, X. H. and Massagué, J. (2011a). Macrophage binding to receptorVCAM-1 transmits survival signals in breast cancer cells that invade the lungs. CancerCell 20, 538-549.
Chen, X., Wong, R., Khalidov, I., Wang, A. Y., Leelawattanachai, J., Wang, Y. andJin, M. M. (2011b). Inflamed leukocyte-mimetic nanoparticles for molecular imagingof inflammation. Biomaterials 32, 7651-7661.
Comen, E., Norton, L. and Massague, J. (2011). Clinical implications of cancer self-seeding. Nat. Rev. Clin. Oncol. 8, 369-377.
Condeelis, J. and Segall, J. E. (2003). Intravital imaging of cell movement in tumours.Nat. Rev. Cancer 3, 921-930.
Condeelis, J. and Weissleder, R. (2010). In vivo imaging in cancer. Cold Spring Harb.Perspect. Biol. 2, a003848.
Coussens, L. M., Fingleton, B. and Matrisian, L. M. (2002). Matrix metalloproteinaseinhibitors and cancer: trials and tribulations. Science 295, 2387-2392.
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 591
Live imaging of the metastatic process REVIEW
Cuccia, D. J., Bevilacqua, F., Durkin, A. J., Ayers, F. R. and Tromberg, B. J. (2009).Quantitation and mapping of tissue optical properties using modulated imaging. J.
Biomed. Opt. 14, 024012.Detmar, M. and Hirakawa, S. (2002). The formation of lymphatic vessels and its
importance in the setting of malignancy. J. Exp. Med. 196, 713-718.Fidler, I. J. (2003). The pathogenesis of cancer metastasis: the ‘seed and soil’
hypothesis revisited. Nat. Rev. Cancer 3, 453-458.Fidler, I. J. and Kripke, M. L. (1977). Metastasis results from preexisting variant cells
within a malignant tumor. Science 197, 893-895.Fidler, I. J. and Talmadge, J. E. (1986). Evidence that intravenously derived murine
pulmonary melanoma metastases can originate from the expansion of a singletumor cell. Cancer Res. 46, 5167-5171.
Fields, R. C., Jeffe, D. B., Trinkaus, K., Zhang, Q., Arthur, C., Aft, R., Dietz, J. R.,Eberlein, T. J., Gillanders, W. E. and Margenthaler, J. A. (2007). Surgical resectionof the primary tumor is associated with increased long-term survival in patients withstage IV breast cancer after controlling for site of metastasis. Ann. Surg. Oncol. 14,3345-3351.
Fridlender, Z. G. and Albelda, S. M. (2012). Tumor-associated neutrophils: friend orfoe? Carcinogenesis 33, 949-955.
Friedl, P. and Alexander, S. (2011). Cancer invasion and the microenvironment:plasticity and reciprocity. Cell 147, 992-1009.
Friedl, P. and Wolf, K. (2003). Tumour-cell invasion and migration: diversity andescape mechanisms. Nat. Rev. Cancer 3, 362-374.
Fujimoto, J. G. (2003). Optical coherence tomography for ultrahigh resolution in vivoimaging. Nat. Biotechnol. 21, 1361-1367.
Fukumura, D. and Jain, R. K. (2008). Imaging angiogenesis and themicroenvironment. APMIS 116, 695-715.
Fukumura, D., Duda, D. G., Munn, L. L. and Jain, R. K. (2010). Tumormicrovasculature and microenvironment: novel insights through intravital imagingin pre-clinical models. Microcirculation 17, 206-225.
Giampieri, S., Manning, C., Hooper, S., Jones, L., Hill, C. S. and Sahai, E. (2009).Localized and reversible TGFbeta signalling switches breast cancer cells fromcohesive to single cell motility. Nat. Cell Biol. 11, 1287-1296.
Giampieri, S., Pinner, S. and Sahai, E. (2010). Intravital imaging illuminatestransforming growth factor beta signaling switches during metastasis. Cancer Res.
70, 3435-3439.Gligorijevic, B., Wyckoff, J., Yamaguchi, H., Wang, Y., Roussos, E. T. and Condeelis,
J. (2012). N-WASP-mediated invadopodium formation is involved in intravasationand lung metastasis of mammary tumors. J. Cell Sci. 125, 724-734.
Granot, Z., Henke, E., Comen, E. A., King, T. A., Norton, L. and Benezra, R. (2011).Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell
20, 300-314.Gurskaya, N. G., Verkhusha, V. V., Shcheglov, A. S., Staroverov, D. B., Chepurnykh,
T. V., Fradkov, A. F., Lukyanov, S. and Lukyanov, K. A. (2006). Engineering of amonomeric green-to-red photoactivatable fluorescent protein induced by blue light.Nat. Biotechnol. 24, 461-465.
Handmaker, H. (1975). Nuclear medicine in the evaluation of the patient withjaundice. JAMA 231, 1172-1176.
Hardy, K. M., Booth, B. W., Hendrix, M. J., Salomon, D. S. and Strizzi, L. (2010).ErbB/EGF signaling and EMT in mammary development and breast cancer. J.
Mammary Gland Biol. Neoplasia 15, 191-199.Harris, A. L. (2002). Hypoxia – a key regulatory factor in tumour growth. Nat. Rev.
Cancer 2, 38-47.He, S., Lamers, G. E., Beenakker, J. W., Cui, C., Ghotra, V. P., Danen, E. H., Meijer, A.
H., Spaink, H. P. and Snaar-Jagalska, B. E. (2012). Neutrophil-mediatedexperimental metastasis is enhanced by VEGFR inhibition in a zebrafish xenograftmodel. J. Pathol. 227, 431-445.
Heyn, C., Ronald, J. A., Ramadan, S. S., Snir, J. A., Barry, A. M., MacKenzie, L. T.,Mikulis, D. J., Palmieri, D., Bronder, J. L., Steeg, P. S. et al. (2006). In vivo MRI ofcancer cell fate at the single-cell level in a mouse model of breast cancer metastasisto the brain. Magn. Reson. Med. 56, 1001-1010.
Hirata, E., Yukinaga, H., Kamioka, Y., Arakawa, Y., Miyamoto, S., Okada, T., Sahai,E. and Matsuda, M. (2012). In vivo fluorescence resonance energy transfer imagingreveals differential activation of Rho-family GTPases in glioblastoma cell invasion. J.
Cell Sci. 125, 858-868.Hoshida, T., Isaka, N., Hagendoorn, J., di Tomaso, E., Chen, Y. L., Pytowski, B.,
Fukumura, D., Padera, T. P. and Jain, R. K. (2006). Imaging steps of lymphaticmetastasis reveals that vascular endothelial growth factor-C increases metastasis byincreasing delivery of cancer cells to lymph nodes: therapeutic implications. Cancer
Res. 66, 8065-8075.Hotary, K., Allen, E., Punturieri, A., Yana, I. and Weiss, S. J. (2000). Regulation of cell
invasion and morphogenesis in a three-dimensional type I collagen matrix bymembrane-type matrix metalloproteinases 1, 2, and 3. J. Cell Biol. 149, 1309-1323.
Hunter, K. W., Crawford, N. P. and Alsarraj, J. (2008). Mechanisms of metastasis.Breast Cancer Res. 10 Suppl. 1, S2.
Hutteman, M., Mieog, J. S., van der Vorst, J. R., Dijkstra, J., Kuppen, P. J., van derLaan, A. M., Tanke, H. J., Kaijzel, E. L., Que, I., van de Velde, C. J. et al. (2011).Intraoperative near-infrared fluorescence imaging of colorectal metastases targetingintegrin α(v)β(3) expression in a syngeneic rat model. Eur. J. Surg. Oncol. 37, 252-257.
Ishikawa-Ankerhold, H. C., Ankerhold, R. and Drummen, G. P. (2012). Advancedfluorescence microscopy techniques – FRAP, FLIP, FLAP, FRET and FLIM. Molecules 17,4047-4132.
Jain, R. K. (1988). Determinants of tumor blood flow: a review. Cancer Res. 48, 2641-2658.
Jain, R. K. (2003). Molecular regulation of vessel maturation. Nat. Med. 9, 685-693.Johnson, E. A., De Lee, R., Agni, R., Pfau, P., Reichelderfer, M. and Gopal, D. V.
(2012). Probe-based confocal laser endomicroscopy to guide real-time endoscopictherapy in Barrett’s esophagus with dysplasia. Case Rep. Gastroenterol. 6, 285-292.
Joyce, J. A. and Pollard, J. W. (2009). Microenvironmental regulation of metastasis.Nat. Rev. Cancer 9, 239-252.
Kaplan, R. N., Riba, R. D., Zacharoulis, S., Bramley, A. H., Vincent, L., Costa, C.,MacDonald, D. D., Jin, D. K., Shido, K., Kerns, S. A. et al. (2005). VEGFR1-positivehaematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature
438, 820-827.Kedrin, D., Gligorijevic, B., Wyckoff, J., Verkhusha, V. V., Condeelis, J., Segall, J. E.
and van Rheenen, J. (2008). Intravital imaging of metastatic behavior through amammary imaging window. Nat. Methods 5, 1019-1021.
Keren, S., Zavaleta, C., Cheng, Z., de la Zerda, A., Gheysens, O. and Gambhir, S. S.(2008). Noninvasive molecular imaging of small living subjects using Ramanspectroscopy. Proc. Natl. Acad. Sci. USA 105, 5844-5849.
Kessenbrock, K., Plaks, V. and Werb, Z. (2010). Matrix metalloproteinases: regulatorsof the tumor microenvironment. Cell 141, 52-67.
Kienast, Y., von Baumgarten, L., Fuhrmann, M., Klinkert, W. E., Goldbrunner, R.,Herms, J. and Winkler, F. (2010). Real-time imaging reveals the single steps of brainmetastasis formation. Nat. Med. 16, 116-122.
Kim, M. Y., Oskarsson, T., Acharyya, S., Nguyen, D. X., Zhang, X. H., Norton, L. andMassagué, J. (2009a). Tumor self-seeding by circulating cancer cells. Cell 139, 1315-1326.
Kim, J. V., Kang, S. S., Dustin, M. L. and McGavern, D. B. (2009b). Myelomonocyticcell recruitment causes fatal CNS vascular injury during acute viral meningitis. Nature
457, 191-195. Kim, J. K., Lee, W. M., Kim, P., Choi, M., Jung, K., Kim, S. and Yun, S. H. (2012).
Fabrication and operation of GRIN probes for in vivo fluorescence cellular imaging ofinternal organs in small animals. Nat. Protoc. 7, 1456-1469.
Kircher, M. F., de la Zerda, A., Jokerst, J. V., Zavaleta, C. L., Kempen, P. J., Mittra, E.,Pitter, K., Huang, R., Campos, C., Habte, F. et al. (2012). A brain tumor molecularimaging strategy using a new triple-modality MRI-photoacoustic-Ramannanoparticle. Nat. Med. 18, 829-834.
Kollmar, O., Menger, M. D. and Schilling, M. K. (2006). Macrophage inflammatoryprotein-2 contributes to liver resection-induced acceleration of hepatic metastatictumor growth. World J. Gastroenterol. 12, 858-867.
Kouros-Mehr, H., Bechis, S. K., Slorach, E. M., Littlepage, L. E., Egeblad, M., Ewald,A. J., Pai, S. Y., Ho, I. C. and Werb, Z. (2008). GATA-3 links tumor differentiation anddissemination in a luminal breast cancer model. Cancer Cell 13, 141-152.
Levene, M. J., Dombeck, D. A., Kasischke, K. A., Molloy, R. P. and Webb, W. W.(2004). In vivo multiphoton microscopy of deep brain tissue. J. Neurophysiol. 91,1908-1912.
Li, C. Y., Shan, S., Huang, Q., Braun, R. D., Lanzen, J., Hu, K., Lin, P. and Dewhirst,M. W. (2000). Initial stages of tumor cell-induced angiogenesis: evaluation via skinwindow chambers in rodent models. J. Natl. Cancer Inst. 92, 143-147.
Lin, K. Y., Maricevich, M., Bardeesy, N., Weissleder, R. and Mahmood, U. (2008). Invivo quantitative microvasculature phenotype imaging of healthy and malignanttissues using a fiber-optic confocal laser microprobe. Transl. Oncol. 1, 84-94.
Littlepage, L. E., Sternlicht, M. D., Rougier, N., Phillips, J., Gallo, E., Yu, Y., Williams,K., Brenot, A., Gordon, J. I. and Werb, Z. (2010). Matrix metalloproteinasescontribute distinct roles in neuroendocrine prostate carcinogenesis, metastasis, andangiogenesis progression. Cancer Res. 70, 2224-2234.
Liu, J. T., Loewke, N. O., Mandella, M. J., Levenson, R. M., Crawford, J. M. andContag, C. H. (2011). Point-of-care pathology with miniature microscopes. Anal. Cell
Pathol. (Amst.) 34, 81-98.Looney, M. R., Thornton, E. E., Sen, D., Lamm, W. J., Glenny, R. W. and Krummel,
M. F. (2011). Stabilized imaging of immune surveillance in the mouse lung. Nat.
Methods 8, 91-96.Lu, X., Yan, C. H., Yuan, M., Wei, Y., Hu, G. and Kang, Y. (2010). In vivo dynamics and
distinct functions of hypoxia in primary tumor growth and organotropic metastasisof breast cancer. Cancer Res. 70, 3905-3914.
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
dmm.biologists.org592
Live imaging of the metastatic processREVIEW
Lu, X., Mu, E., Wei, Y., Riethdorf, S., Yang, Q., Yuan, M., Yan, J., Hua, Y., Tiede, B. J.,Lu, X. et al. (2011). VCAM-1 promotes osteolytic expansion of indolent bonemicrometastasis of breast cancer by engaging α4β1-positive osteoclast progenitors.Cancer Cell 20, 701-714.
Mackanos, M. A. and Contag, C. H. (2010). Fiber-optic probes enable cancerdetection with FTIR spectroscopy. Trends Biotechnol. 28, 317-323.
Madsen, C. D. and Sahai, E. (2010). Cancer dissemination – lessons from leukocytes.Dev. Cell 19, 13-26.
Martínez-Corral, I., Olmeda, D., Diéguez-Hurtado, R., Tammela, T., Alitalo, K. andOrtega, S. (2012). In vivo imaging of lymphatic vessels in development, woundhealing, inflammation, and tumor metastasis. Proc. Natl. Acad. Sci. USA 109, 6223-6228.
McElroy, M., Kaushal, S., Bouvet, M. and Hoffman, R. M. (2008). Color-codedimaging of splenocyte-pancreatic cancer cell interactions in the tumormicroenvironment. Cell Cycle 7, 2916-2921.
McGinty, J., Stuckey, D. W., Soloviev, V. Y., Laine, R., Wylezinska-Arridge, M., Wells,D. J., Arridge, S. R., French, P. M., Hajnal, J. V. and Sardini, A. (2011). In vivofluorescence lifetime tomography of a FRET probe expressed in mouse. Biomed. Opt.Express 2, 1907-1917.
McGowan, P. M., Kirstein, J. M. and Chambers, A. F. (2009). Micrometastatic diseaseand metastatic outgrowth: clinical issues and experimental approaches. Future Oncol.5, 1083-1098.
Mumprecht, V., Honer, M., Vigl, B., Proulx, S. T., Trachsel, E., Kaspar, M., Banziger-Tobler, N. E., Schibli, R., Neri, D. and Detmar, M. (2010). In vivo imaging ofinflammation- and tumor-induced lymph node lymphangiogenesis by immuno-positron emission tomography. Cancer Res. 70, 8842-8851.
Naumov, G. N., MacDonald, I. C., Weinmeister, P. M., Kerkvliet, N., Nadkarni, K. V.,Wilson, S. M., Morris, V. L., Groom, A. C. and Chambers, A. F. (2002). Persistenceof solitary mammary carcinoma cells in a secondary site: a possible contributor todormancy. Cancer Res. 62, 2162-2168.
Navin, N., Kendall, J., Troge, J., Andrews, P., Rodgers, L., McIndoo, J., Cook, K.,Stepansky, A., Levy, D., Esposito, D. et al. (2011). Tumour evolution inferred bysingle-cell sequencing. Nature 472, 90-94.
Nguyen, D. X., Bos, P. D. and Massagué, J. (2009). Metastasis: from dissemination toorgan-specific colonization. Nat. Rev. Cancer 9, 274-284.
Oliver, G. and Detmar, M. (2002). The rediscovery of the lymphatic system: old andnew insights into the development and biological function of the lymphaticvasculature. Genes Dev. 16, 773-783.
Paget, S. (1989). The distribution of secondary growths in cancer of the breast. 1889.Cancer Metastasis Rev. 8, 98-101.
Pinner, S., Jordan, P., Sharrock, K., Bazley, L., Collinson, L., Marais, R., Bonvin, E.,Goding, C. and Sahai, E. (2009). Intravital imaging reveals transient changes inpigment production and Brn2 expression during metastatic melanomadissemination. Cancer Res. 69, 7969-7977.
Pittet, M. J. and Weissleder, R. (2011). Intravital imaging. Cell 147, 983-991.Prescher, J. A. and Contag, C. H. (2010). Guided by the light: visualizing biomolecular
processes in living animals with bioluminescence. Curr. Opin. Chem. Biol. 14, 80-89.Provenzano, P. P., Eliceiri, K. W. and Keely, P. J. (2009). Multiphoton microscopy and
fluorescence lifetime imaging microscopy (FLIM) to monitor metastasis and thetumor microenvironment. Clin. Exp. Metastasis 26, 357-370.
Qadri, S. S., Wang, J. H., Coffey, J. C., Alam, M., O’Donnell, A., Aherne, T. andRedmond, H. P. (2005). Can surgery for cancer accelerate the progression ofsecondary tumors within residual minimal disease at both local and systemic levels?Ann. Thorac. Surg. 80, 1046-1050.
Qian, B. Z., Li, J., Zhang, H., Kitamura, T., Zhang, J., Campion, L. R., Kaiser, E. A.,Snyder, L. A. and Pollard, J. W. (2011). CCL2 recruits inflammatory monocytes tofacilitate breast-tumour metastasis. Nature 475, 222-225.
Ritsma, L., Steller, E. J., Beerling, E., Loomans, C. J., Zomer, A., Gerlach, C.,Vrisekoop, N., Seinstra, D., van Gurp, L., Schafer, R. et al. (2012). Intravitalmicroscopy through an abdominal imaging window reveals a pre-micrometastasisstage during liver metastasis. Sci. Transl. Med. 4, 158ra145.
Robinson, B. D., Sica, G. L., Liu, Y. F., Rohan, T. E., Gertler, F. B., Condeelis, J. S. andJones, J. G. (2009). Tumor microenvironment of metastasis in human breastcarcinoma: a potential prognostic marker linked to hematogenous dissemination.Clin. Cancer Res. 15, 2433-2441.
Roussos, E. T., Balsamo, M., Alford, S. K., Wyckoff, J. B., Gligorijevic, B., Wang, Y.,Pozzuto, M., Stobezki, R., Goswami, S., Segall, J. E. et al. (2011). Mena invasive(MenaINV) promotes multicellular streaming motility and transendothelial migrationin a mouse model of breast cancer. J. Cell Sci. 124, 2120-2131.
Rowe, R. G. and Weiss, S. J. (2008). Breaching the basement membrane: who, whenand how? Trends Cell Biol. 18, 560-574.
Sabeh, F., Ota, I., Holmbeck, K., Birkedal-Hansen, H., Soloway, P., Balbin, M.,Lopez-Otin, C., Shapiro, S., Inada, M., Krane, S. et al. (2004). Tumor cell trafficthrough the extracellular matrix is controlled by the membrane-anchoredcollagenase MT1-MMP. J. Cell Biol. 167, 769-781.
Sabouri-Ghomi, M., Wu, Y., Hahn, K. and Danuser, G. (2008). Visualizing andquantifying adhesive signals. Curr. Opin. Cell Biol. 20, 541-550.
Sadikot, R. T. and Blackwell, T. S. (2005). Bioluminescence imaging. Proc. Am. Thorac.Soc. 2, 537-540.
Sahai, E. (2007). Illuminating the metastatic process. Nat. Rev. Cancer 7, 737-749.Schepers, A. G., Snippert, H. J., Stange, D. E., van den Born, M., van Es, J. H., van
de Wetering, M. and Clevers, H. (2012). Lineage tracing reveals Lgr5+ stem cellactivity in mouse intestinal adenomas. Science 337, 730-735.
Serrels, A., Timpson, P., Canel, M., Schwarz, J. P., Carragher, N. O., Frame, M. C.,Brunton, V. G. and Anderson, K. I. (2009). Real-time study of E-cadherin andmembrane dynamics in living animals: implications for disease modeling and drugdevelopment. Cancer Res. 69, 2714-2719.
Sipkins, D. A., Wei, X., Wu, J. W., Runnels, J. M., Côté, D., Means, T. K., Luster, A. D.,Scadden, D. T. and Lin, C. P. (2005). In vivo imaging of specialized bone marrowendothelial microdomains for tumour engraftment. Nature 435, 969-973.
Smith, B. R., Cheng, Z., De, A., Rosenberg, J. and Gambhir, S. S. (2010). Dynamicvisualization of RGD-quantum dot binding to tumor neovasculature andextravasation in multiple living mouse models using intravital microscopy. Small 6,2222-2229.
Snippert, H. J., van der Flier, L. G., Sato, T., van Es, J. H., van den Born, M., Kroon-Veenboer, C., Barker, N., Klein, A. M., van Rheenen, J., Simons, B. D. et al. (2010).Intestinal crypt homeostasis results from neutral competition betweensymmetrically dividing Lgr5 stem cells. Cell 143, 134-144.
Stoletov, K. and Klemke, R. (2008). Catch of the day: zebrafish as a human cancermodel. Oncogene 27, 4509-4520.
Stoletov, K., Montel, V., Lester, R. D., Gonias, S. L. and Klemke, R. (2007). High-resolution imaging of the dynamic tumor cell vascular interface in transparentzebrafish. Proc. Natl. Acad. Sci. USA 104, 17406-17411.
Stoletov, K., Kato, H., Zardouzian, E., Kelber, J., Yang, J., Shattil, S. and Klemke, R.(2010). Visualizing extravasation dynamics of metastatic tumor cells. J. Cell Sci. 123,2332-2341.
Stroh, M., Zimmer, J. P., Duda, D. G., Levchenko, T. S., Cohen, K. S., Brown, E. B.,Scadden, D. T., Torchilin, V. P., Bawendi, M. G., Fukumura, D. et al. (2005).Quantum dots spectrally distinguish multiple species within the tumor milieu invivo. Nat. Med. 11, 678-682.
Szabova, L., Chrysovergis, K., Yamada, S. S. and Holmbeck, K. (2008). MT1-MMP isrequired for efficient tumor dissemination in experimental metastatic disease.Oncogene 27, 3274-3281.
Tanaka, K., Morimoto, Y., Toiyama, Y., Matsushita, K., Kawamura, M., Koike, Y.,Okugawa, Y., Inoue, Y., Uchida, K., Araki, T. et al. (2012). In vivo time-courseimaging of tumor angiogenesis in colorectal liver metastases in the same living miceusing two-photon laser scanning microscopy. J. Oncol. 2012, 265487.
Timpson, P., Serrels, A., Canel, M., Frame, M. C., Brunton, V. G. and Anderson, K. I.(2009). Quantitative real-time imaging of molecular dynamics during cancer cellinvasion and metastasis in vivo. Cell Adh. Migr. 3, 351-354.
Timpson, P., McGhee, E. J. and Anderson, K. I. (2011). Imaging molecular dynamicsin vivo – from cell biology to animal models. J. Cell Sci. 124, 2877-2890.
Toiyama, Y., Mizoguchi, A., Okugawa, Y., Koike, Y., Morimoto, Y., Araki, T., Uchida,K., Tanaka, K., Nakashima, H., Hibi, M. et al. (2010). Intravital imaging of DSS-induced cecal mucosal damage in GFP-transgenic mice using two-photonmicroscopy. J. Gastroenterol. 45, 544-553.
Vakoc, B., Yun, S., de Boer, J., Tearney, G. and Bouma, B. (2005). Phase-resolvedoptical frequency domain imaging. Opt. Express 13, 5483-5493.
Vakoc, B. J., Lanning, R. M., Tyrrell, J. A., Padera, T. P., Bartlett, L. A.,Stylianopoulos, T., Munn, L. L., Tearney, G. J., Fukumura, D., Jain, R. K. et al.(2009). Three-dimensional microscopy of the tumor microenvironment in vivo usingoptical frequency domain imaging. Nat. Med. 15, 1219-1223.
Wagner, W. W., Jr (1969). Pulmonary microcirculatory observations in vivo underphysiological conditions. J. Appl. Physiol. 26, 375-377.
Wang, W., Wyckoff, J. B., Frohlich, V. C., Oleynikov, Y., Hüttelmaier, S., Zavadil, J.,Cermak, L., Bottinger, E. P., Singer, R. H., White, J. G. et al. (2002). Single cellbehavior in metastatic primary mammary tumors correlated with gene expressionpatterns revealed by molecular profiling. Cancer Res. 62, 6278-6288.
Wang, W., Wyckoff, J. B., Wang, Y., Bottinger, E. P., Segall, J. E. and Condeelis, J. S.(2003). Gene expression analysis on small numbers of invasive cells collected bychemotaxis from primary mammary tumors of the mouse. BMC Biotechnol. 3, 13.
Wang, W., Goswami, S., Sahai, E., Wyckoff, J. B., Segall, J. E. and Condeelis, J. S.(2005). Tumor cells caught in the act of invading: their strategy for enhanced cellmotility. Trends Cell Biol. 15, 138-145.
Weidner, N., Semple, J. P., Welch, W. R. and Folkman, J. (1991). Tumor angiogenesisand metastasis – correlation in invasive breast carcinoma. N. Engl. J. Med. 324, 1-8.
Weissleder, R., Tung, C. H., Mahmood, U. and Bogdanov, A., Jr (1999). In vivoimaging of tumors with protease-activated near-infrared fluorescent probes. Nat.Biotechnol. 17, 375-378.
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Disease Models & Mechanisms 593
Live imaging of the metastatic process REVIEW
Wells, A., Chao, Y. L., Grahovac, J., Wu, Q. and Lauffenburger, D. A. (2011). Epithelialand mesenchymal phenotypic switchings modulate cell motility in metastasis. Front.
Biosci. 16, 815-837.Williams, R. M., Flesken-Nikitin, A., Ellenson, L. H., Connolly, D. C., Hamilton, T. C.,
Nikitin, A. Y. and Zipfel, W. R. (2010). Strategies for high-resolution imaging ofepithelial ovarian cancer by laparoscopic nonlinear microscopy. Transl. Oncol. 3, 181-194.
Winslow, M. M., Dayton, T. L., Verhaak, R. G., Kim-Kiselak, C., Snyder, E. L.,Feldser, D. M., Hubbard, D. D., DuPage, M. J., Whittaker, C. A., Hoersch, S. et al.(2011). Suppression of lung adenocarcinoma progression by Nkx2-1. Nature 473,101-104.
Wolf, K. and Friedl, P. (2011). Extracellular matrix determinants of proteolytic and non-proteolytic cell migration. Trends Cell Biol. 21, 736-744.
Wolf, K., Mazo, I., Leung, H., Engelke, K., von Andrian, U. H., Deryugina, E. I.,Strongin, A. Y., Bröcker, E. B. and Friedl, P. (2003). Compensation mechanism intumor cell migration: mesenchymal-amoeboid transition after blocking ofpericellular proteolysis. J. Cell Biol. 160, 267-277.
Wolf, K., Wu, Y. I., Liu, Y., Geiger, J., Tam, E., Overall, C., Stack, M. S. and Friedl, P.(2007). Multi-step pericellular proteolysis controls the transition from individual tocollective cancer cell invasion. Nat. Cell Biol. 9, 893-904.
Wong, C. W., Lee, A., Shientag, L., Yu, J., Dong, Y., Kao, G., Al-Mehdi, A. B.,Bernhard, E. J. and Muschel, R. J. (2001). Apoptosis: an early event in metastaticinefficiency. Cancer Res. 61, 333-338.
Wyckoff, J. B., Jones, J. G., Condeelis, J. S. and Segall, J. E. (2000). A critical step inmetastasis: in vivo analysis of intravasation at the primary tumor. Cancer Res. 60,2504-2511.
Wyckoff, J., Wang, W., Lin, E. Y., Wang, Y., Pixley, F., Stanley, E. R., Graf, T., Pollard,J. W., Segall, J. and Condeelis, J. (2004). A paracrine loop between tumor cells and
macrophages is required for tumor cell migration in mammary tumors. Cancer Res.64, 7022-7029.
Wyckoff, J. B., Wang, Y., Lin, E. Y., Li, J. F., Goswami, S., Stanley, E. R., Segall, J. E.,Pollard, J. W. and Condeelis, J. (2007). Direct visualization of macrophage-assistedtumor cell intravasation in mammary tumors. Cancer Res. 67, 2649-2656.
Yang, J. and Weinberg, R. A. (2008). Epithelial-mesenchymal transition: at thecrossroads of development and tumor metastasis. Dev. Cell 14, 818-829.
Yang, J. M., Favazza, C., Chen, R., Yao, J., Cai, X., Maslov, K., Zhou, Q., Shung, K. K.and Wang, L. V. (2012). Simultaneous functional photoacoustic and ultrasonicendoscopy of internal organs in vivo. Nat. Med. 18, 1297-1302.
Yoo, H., Kim, J. W., Shishkov, M., Namati, E., Morse, T., Shubochkin, R., McCarthy,J. R., Ntziachristos, V., Bouma, B. E., Jaffer, F. A. et al. (2011). Intra-arterial catheterfor simultaneous microstructural and molecular imaging in vivo. Nat. Med. 17, 1680-1684.
Yuan, F., Salehi, H. A., Boucher, Y., Vasthare, U. S., Tuma, R. F. and Jain, R. K. (1994).Vascular permeability and microcirculation of gliomas and mammary carcinomastransplanted in rat and mouse cranial windows. Cancer Res. 54, 4564-4568.
Zervantonakis, I. K., Hughes-Alford, S. K., Charest, J. L., Condeelis, J. S., Gertler, F.B. and Kamm, R. D. (2012). Three-dimensional microfluidic model for tumor cellintravasation and endothelial barrier function. Proc. Natl. Acad. Sci. USA 109, 13515-13520.
Zhang, N. and Yang, Q. (2009). Primary tumor resection may improve prognosis fornonoperable advanced breast cancer. Med. Hypotheses 73, 1058-1059.
Zhang, X. H., Wang, Q., Gerald, W., Hudis, C. A., Norton, L., Smid, M., Foekens, J. A.and Massagué, J. (2009). Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell 16, 67-78.
Zhou, Z. N., Boimel, P. J. and Segall, J. E. (2011). Tumor-stroma: In vivo assays andintravital imaging to study cell migration and metastasis. Drug Discov. Today Dis.Models 8, 95-102.
Dise
ase
Mod
els &
Mec
hani
sms
D
MM
Related Documents