Antifungal Drugs Infectious diseases caused by fungi are called mycoses, and they are often chronic in nature. Fungal infectious occur due to : 1- Abuse of broad spectrum antibiotics 2- Decrease in the patient immunity

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript
Antifungal Drugs
Infectious diseases caused by fungi are called
mycoses, and they are often chronic in nature.
Fungal infectious occur due to :
1- Abuse of broad spectrum antibiotics
2- Decrease in the patient immunity
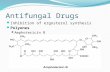
They have rigid cell walls composed
largely of a polymer of N-
acetylglucosamine rather than
peptidoglycan (a characteristic component
of most bacterial cell walls).
The fungal cell membrane contains
ergosterol rather than the cholesterol found
in mammalian membranes.
These chemical characteristics are useful in
targeting chemotherapeutic agents against
fungal infections
Types of fungal infections
1. Superficial : Affect skin – mucous membrane. e.g.
Tinea versicolor
Dermatophytes : Fungi that affectkeratin layer of skin, hair, nail. e.g. tineapedis ,ring worm infection
Candidiasis : Yeast-like, oral thrush,vulvo-vaginitis , nail infections.
2- Deep infections
Affect internal organs as : lung ,heart ,
brain leading to pneumonia ,
endocarditis , meningitis.
Classification of Antifungal Drugs
1- Antifungal Antibiotics :
Griseofulvin
Polyene macrolide : Amphotericin- B &
Nystatin
2- Synthetic :
Azoles :
A) Imidazoles : Ketoconazole , Miconazole
B) Triazoles : Fluconazole , Itraconazole
Synthetic Antifungal ( contin…)
Flucytosine
Squalene epoxidase inhibitors :
e.g.Terbinafine & Naftifine.
Classification According to Route of
Administration
Systemic :
Griseofulvin , Amphotericin- B , Ketoconazole ,Fluconazole , Terbinafine.
Topical
In candidiasis :
Imidazoles : Ketoconazole , Miconazole.
Triazoles : Terconazole.
Polyene macrolides : Nystatin , Amphotericin-B
Gentian violet : Has antifungal & antibacterial.
In Dermatophytes :
Squalene epoxidase inhibitors : Terbinafine &
Naftifine.
Tolnaftate.
White field ointment : 11% Benzoic acid &
6% Salicylic acid .
Castellani paint.
Amphotericin B
Amphotericin A & B are antifungal
antibiotics.
Amphotericin A is not used clinically.
It is a natural polyene macrolide
(polyene = many double bonds )
(macrolide = containing a large lactone ring )
Pharmacokinetics Poorly absorbed orally , is effective for fungal
infection of gastrointestinal tract.
For systemic infections given as slow I.V.I.
Highly bound to plasma protein .
Poorly crossing BBB.
Metabolized in liver
Excreted slowly in urine over a period ofseveral days.
Half-life 16 days.
Mechanism of action
It is a selective fungicidal drug.
Disrupt fungal cell membrane by binding to
ergosterol , so alters the permeability of the
cell membrane leading to leakage of
intracellular ions & macromolecules (cell
death ).
Resistance to amphotericin B
If ergosterol binding is impaired either by :
Decreasing the membrane concentration of
ergosterol.
Or by modifying the sterol target molecule.
Adverse Effects
1- Immediate reactions (Infusion –related toxicity).
Fever, muscle spasm, vomiting, headache, hypotension.
Can be avoided by:
A. Slowing the infusion
B. Decreasing the daily dose
C.Premedication with antipyretics, antihistamincs orcorticosteroids.
D. A test dose.
2- Slower toxicity
Most serious is renal toxicity (nearly in all
patients ).
Hypokalemia
Hypomagnesaemia
Impaired liver functions
Thrombocytopenia
Anemia
Clinical uses
Has a broad spectrum of activity & fungicidal action.
The drug of choice for life-threatening mycotic
infections.
For induction regimen for serious fungal infection.
Also, for chronic therapy & preventive therapy of
relapse.
In cancer patients with neutropenia who remain
febrile on broad –spectrum antibiotics.
Routes of Administration
1- Slow I.V.I. For systemic fungal disease.
2- Intrathecal for fungal C.N.S. infections.
3- Topical drops & direct subconjunctival
injection for Mycotic corneal ulcers & keratitis.
3- Local injection into the joint in fungal arthritis.
4- Bladder irrigation in Candiduria.
Liposomal preparations of
amphotericin B
Amphotericin B is packaged in a lipid-
associated delivery system to reduce binding to
human cell membrane , so reducing :
A. Nephrotoxicity
B. Infusion toxicity
Also, more effective
More expensive
Nystatin
It is a polyene macrolide ,similar in structure
& mechanism to amphotericin B.
Too toxic for systemic use.
Used only topically.
It is available as creams, ointment ,
suppositories & other preparations.
Not significantly absorbed from skin, mucous
membrane, GIT .
Clinical uses
Prevent or treat superficial candidiasis of
mouth, esophagus, intestinal tract.
Vaginal candidiasis
Can be used in combination with antibacterial
agents & corticosteroids.
Azoles
A group of synthetic fungistatic agents with a
broad spectrum of activity .
They have antibacterial , antiprotozoal
anthelminthic & antifungal activity .
Mechanism of Action
1-Inhibit the fungal cytochrome P450 enzyme, (α-
demethylase) which is responsible for converting
lanosterol to ergosterol ( the main sterol in fungal
cell membrane ).
2- Inhibition of mitochondrial cytochrome
oxidase leading to accumulation of peroxides that
cause autodigestion of the fungus.
3- Imidazoles may alter RNA& DNA metabolism.
Imidazoles
Ketoconazole
Miconazole
Clotrimazole
They lack selectivity ,they inhibit human
gonadal and steroid synthesis leading to
decrease testosterone & cortisol production.
Also, inhibit human P-450 hepatic enzyme.
Ketoconazole
Well absorbed orally .
Bioavailability is decreased with antacids, H2
blockers , proton pump inhibitors & food .
Cola drinks improve absorption in patients
with achlorhydria.
Half-life increases with the dose , it is (7-8 hrs).
Clinical uses
Used topically or systematic (oral route only )
to treat :
1- Oral & vaginal candidiasis.
2- Dermatophytosis.
3- Systemic mycoses.
Adverse Effects
Nausea, vomiting ,anorexia
Hepatotoxic
Inhibits human P 450 enzymes
Inhibits adrenal & gonadal steroids leading to:
Menstrual irregularities
Loss of libido
Impotence
Gynaecomastia in males
Contraindications & Drug interactions
Contraindicated in :
Prgnancy, lactation ,hepatic dysfunction
Interact with enzyme inhibitors , enzyme
inducers.
H2 blockers & antacids decrease its absorption
Triazoles
Fluconazole
Itraconazole
Voriconazole
They are :
Selective
Resistant to degradation
Causing less endocrine disturbance
Itraconazole
Lacks endocrine side effects
Has a broad spectrum activity
Given orally & IV
Food increases its absorption
Metabolized in liver to active metabolite
Highly lipid soluble ,well distributed to bone,
sputum ,adipose tissues.
Can not cross BBB
Itraconazole (cont.)
Half-life 30-40 hours
Used orally in dermatophytosis & vulvo-vaginal candidiasis.
IV only in serious infections.
Effective in AIDS-associated histoplasmosis
Side effects :
Nausea, vomiting, hypokalemia, hypertension, edema, inhibits the metabolism of many drugs as oral anticoagulants.
Fluconazole
Water soluble
Completely absorbed from GIT
Excellent bioavailability after oraladministration
Bioavailability is not affected by food orgastric PH
Concentrated in plasma is same by oral or IV route
Has the least effect on hepatic microsomalenzymes
Fluconazole (cont.)
Drug interactions are less common
Penetrates well BBB so, it is the drug of choice
of cryptococcal meningitis
Safely given in patients receiving bone marrow
transplants (reducing fungal infections)
Excreted mainly through kidney
Half-life 25-30 hours
Resistance is not a problem
Clinical uses
Candidiasis
( is effective in all forms of mucocutaneous
candidiasis)
Cryptococcus meningitis
Histoplasmosis, blastomycosis, , ring worm.
Not effective in aspergillosis
Side effects
Nausea, vomiting, headache, skin rash ,
diarrhea, abdominal pain , reversible alopecia.
Hepatic failure may lead to death
Highly teratogenic ( as other azoles)
Inhibit P450 cytochrome
No endocrine side effects
Voriconazole
A broad spectrum antifungal agent
Given orally or IV
High oral bioavailability
Penetrates tissues well including CSF
Inhibit P450
Used for the treatment of invasive aspergillosis
& serious infections.
Reversible visual disturbances
Flucytosine
Synthetic pyrimidine antimetabolite (cytotoxic
drug ) often given in combination with
amphotericin B & itraconazole.
Systemic fungistatic
Mechanism of action
Converted within the fungal cell to 5-
fluorouracil (Not in human cell ), that inhibits
thymidylate synthetase enzyme that inhibits
DNA synthesis.
(Amphotericin B increases cell permeability ,
allowing more 5-FC to penetrate the cell, they
are synergistic).
Phrmacokinetics
Rapidly & well absorbed orally
Widely distributed including CSF.
Mainly excreted unchanged through kidney
Half-life 3-6 hours
Clinical uses
Severe deep fungal infections as in meningitis
Generally given with amphotericin B
For cryptococcal meningitis in AIDS patients
Adverse Effects
Nausea, vomiting , diarrhea, severe
enterocolitis
Reversible neutropenia, thrombocytopenia,
bone marrow depression
Alopecia
Elevation in hepatic enzymes
Caspofungin
Inhibits the synthesis of fungal cell wall by
inhibiting the synthesis of β(1,3)-D-glucan,
leading to lysis & cell death.
Given by IV route only
Highly bound to plasma proteins
Half-life 9-11 hours
Slowly metabolized by hydrolysis & N-
acetylation.
Elimination is nearly equal between the
urinary & fecal routes.
Clinical uses
Effective in aspergillus & candida infections.
Second line for those who have failed or
cannot tolerate amphotericin B or
itraconazole.
Adverse effects :
Nausea, vomiting
Flushing (release of histamine from mast cells)
Very expensive
Griseofulvin
Fungistatic, has a narrow spectrum
Given orally (Absorption increases with fattymeal )
Half-life 26 hours
Taken selectively by newly formed skin &concentrated in the keratin.
Induces cytochrome P450 enzymes
Should be given for 2-6weeks for skin & hairinfections to allow replacement of infectedkeratin by the resistant structure
Griseofulvin(cont.)
Inhibits fungal mitosis by interfering with microtubule function
Used to treat dermatophyte infections ( ring worm of skin, hair, nails ).
Highly effective in athlete,s foot.
Ineffective topically.
Not effective in subcutaneous or deep mycosis.
Adverse effects ;
Peripheral neuritis, mental confusion, fatigue, vertigo,GIT upset, enzyme inducer, blurred vision.
Increases alcohol intoxication.
TOLNAFTATE
Effective in most cutaneous mycosis.
Ineffective against Candida.
Used in tinea pedis ( cure rate 80% ).
Used as cream, gel, powder, topical solution.
Applied twice daily.
NAFTIFINE
Broad spectrum fungicidal .
Available as cream or gel.
Effective for treatment of tinea cruris.
TERBINAFINE
Drug of choice for treating dermatophytes (onychomycoses).
Better tolerated ,needs shorter duration of therapy.
Inhibits fungal squalene epoxidase, decreases
The synthesis of ergosterol .(Accumulation of squalene ,which is toxic to the organism causing death of fungal cell).
Fungicidal ,its activity is limited to candida
albicans & dermatophytes.
Effective for treatment of onychomycoses
6 weeks for finger nail infection & 12 weeks
for toe nail infections .
Well absorbed orally , bioavailability
decreases due to first pass metabolism in liver.
Highly protein binding
Accumulates in skin , nails, fat.
Severely hepatotoxic, liver failure even death.
Accumulate in breast milk , should not be
given to nursing mother.
GIT upset (diarrhea, dyspepsia, nausea )
Taste & visual disturbance.
Related Documents