Common Hospital Infections

Antibiotics
May 25, 2015
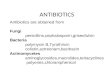
Antibiotics
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

Common Hospital Infections

Fever
• Its 1am and the nurse on Lakeside 65 just called you because Mrs. Price has a T of 101.5 . . . What do you do?

What is the definition of a fever?• Textbook
– Elevation in the body’s thermoregulatory set point
• In the different IDSA guidelines dealing with fever– T >101 at any timepoint– T >100.4 for greater than one hour
• Use your judgement

Fever
1) Assess the patient- As always this is #1 when you are called
about a patient- What are they in for?- Have they been febrile?- What do they look like?
- Are there any symptoms consistent with infection or non-infectious causes of fever (which are?)

Non-infectious causes of fever
• Venous thromboembolism
• Medications
• Transfusion reaction
• Neuroleptic malignant syndrome
• Connective tissue disease
• Malignancy
• Just drank hot coffee

Fever
2) Orders
Blood cultures
Urinalysis, urine culture
Chest x-ray

Sepsis
• Documented or suspected infection plus
• Systemic Inflammatory Response Syndrome (2 of the following 4)– Pyrexia or hypothermia- T >38C or <36C– Tachycardia- HR >90– Respiratory- RR >20 or PaCO2 <32mmHg– WBC- Total >12,000, <4000 or Bands >10%
Keep in mind that many clinical scenarios can produce 2 of 4 SIRS criteria

Hypotension
• Systolic BP <90mmHg or
• Systolic BP reduced >40mmHg from baseline

Types of sepsis
• Severe sepsis- sepsis associated with organ dysfunction, hypoperfusion, or hypotension
• Septic shock- Sepsis with hypotension, despite adequate fluid resuscitation, along with the presence of perfusion abnormalities- lactic acidosis, oliguria, mental status change

Treatment
• Antibiotics – Targeted at known organism or empiric
treatment
• Early goal directed therapy

Sepsis- Early goal directed therapy

Sepsis considerations
• Corticosteroids– “given only to adult septic shock patients after
it has been confirmed that their blood pressure is poorly responsive to fluid resuscitation and vasopressor therapy”
• Activated Protein C (Xigris)– APACHE II >25– Talk with your fellow

Your clinic patient is . . .
• 44 yo female h/o HTN who complains of 2 days of dysuria and subjective fever
• On exam T is 99.7, HR 68, BP 120/64
• Abdominal exam with suprapubic tenderness

UTI risk
• Females– Atrophic vaginal mucosa with altered flora– Use of diaphragms and spermaticides– Foley catheter
• Males– Stricture or obstruction of the urethra (e.g.
BPH)– Foley catheter

Etiology of UTI
• Uncomplicated– E. coli- 85% of females with uncomplicated
infection– Staph. Saprophyticus
• Recurrent– Enterococci (faecium and faecalis)– Klebsiella– Proteus

UTI pathogenesis
• Introduction of bacteria into the urinary bladder
• Incomplete emptying of the bladder (as little as 10mL of residual)
• Fast reproduction time of many of the bacteria that cause UTI (e.g. E. coli which reproduces in 20 minutes)

Urinalysis
• Leukocyte esterase- test for esterase which is released from leukocytes
• Nitrite- produced when bacteria convert nitrates to nitrites
• WBC- pyuria is defined as . . .– >5WBC per HPF in women – >2WBC per HPF in men
• Bacteruria- different for clinical scenario– The presence of bacteria in male urine should always
be considered abnormal– Females- >10^5 per HPF (100,000)

Complicated UTI
• Abnormal anatomy- residual urine, neurogenic bladder, BPH
• Foreign bodies- Catheters, Calculi, Tumors
• Vesicoureteral reflux
• Diabetes

Uncomplicated UTI treatment
• Oral– Bactrim– Nitrofurantoin– Augmentin– Cephalosporin– Fluoroquinolone
• IV– Cephalosporin- ceftriaxone– Fluoroquinolone

• 54 yo male h/o HTN, DM who presents with raised erythematous lesion on right leg and subjective fevers.
• T 99.7 HR 86 RR 16 BP 140/90

Soft tissue infections
• Cellulitis– Erythematous lesions with less clear line of
demarcation compared to erysipelas– Involves deeper dermis and subcutaneous fat
• Erysipelas– raised above the level of surrounding skin,
and there is a clear line of demarcation between involved and uninvolved tissue
– Involves upper dermis and superficial lymphatics

Treatment of routine cellulitis
• MRSA coverage?
• Beta-lactam– Often in hospital would use Unasyn– Consider Pseudomonas coverage for
diabetics (Piperacillin-tazobactam)
• PCN allergic– Consider fluoroquinolone

When is cellulitis not cellulitis?
• Myositis
• Osteomyelitis

When is cellulitis not cellulitis?
• Toxic appearance to patient
• Pain out of proportion to exam
• Quickly spreading infection
• Presence of crepitation
• Bullae formation

Risk of necrotizing fasciitis- score >6 is suggestive and score >8 is
highly predictive• Serum C-reactive protein ≥150 mg/L (4 points) • White blood cell count 15,000 to 25,000/microL (1 point) or
>25,000/microL (2 points) • Hemoglobin 11.0 to 13.5 g/dL (1 point) or ≤11 g/dL (2 points) • Serum sodium less than 135 meq/L (2 points) • Serum creatinine greater than 1.6 mg/dL (141 mmol/L) (2 points) • Serum glucose greater than 180 mg/dL (10 mmol/L) (1 point) • A total score ≥6 should raise the suspicion for necrotizing fasciitis
while a score ≥8 was highly predictive (>75 percent). Among the patients with necrotizing fasciitis, 75 to 80 percent had a score ≥8, while only 7 to 10 percent had a score less than 6. Thus, the score is only useful when severe soft tissue infection is strongly suspected.

Treatment of necrotizing fasciitis
• Stat surgical consult for debridement
• Clindamycin or metronidazoleplus
• Beta-lactam/beta-lactamase inhibitor or 3rd gen cephalosporin or carbapenem or fluoroquinolone or aminoglycoside

The DACR paged you and the report is . . .
• 73 yo male h/o CHF, CKD, CAD who presents with fever, productive cough x 2 days.
• On exam, the patient is febrile to 101. You note that the patient has mildly labored breathing with RR of 28, HR 106. Has crackles at the right lower lung field.
• Labs- WBC 13.5 Hct 34 Plt 175 Na 134 BUN 35
• What do you think?• What studies would you like?

Initial investigation
• CXR• Sputum culture• Blood culture• Consider ABG if respiratory distress or hypoxia
• None of the above should delay antibiotic treatment and guidelines dictate that antibiotics should be given within four hours of initial encounter

Clinical manifestations- Signs and Symptoms
• Cough- 90%• Dyspnea- 66%• Sputum production-
60% • Pleuritic chest pain-
50%• Subjective fever• Nonspecific
symptoms
• Temp>37C- 78%• Crackles- 78%• Confusion- 30%• Consolidation- 29%

Epidemiology
• Risk factors for CAP– Older age– COPD– Renal Insufficiency– Congestive Heart Disease– CAD– Diabetes– Malignancy– Chronic Neurologic Disease– Chronic Liver Disease

Pneumonia- Etiology
“The clinical features of community-acquired pneumonia cannot be reliably used to
establish the etiologic diagnosis of pneumonia with adequate sensitivity and
specificity”- IDSA guidelines on Community Acquired Pneumonia

CAP- Etiology
• The bugs . . . – Strep. Pneumoniae– Mycoplasma pneumoniae– Haemophilus influenza– Chlamydia pneumoniae– Respiratory viruses

Risk stratificationThe PORT score
• Usually prior to you seeing the patient
• May or may not be documented

Pneumonia Severity Index- PORT Score

Fine, M. J. et al. N Engl J Med 1997;336:243-250
Applying the PORT score

PORT in our patient
Age 73
CHF 10
CKD 10
BUN 20
Total= 113 PORT score

PORT Categories and mortality
• Class I- age <50, no comorbidities– 0.1% mortality
• Class II- <70– 0.6% mortality
• Class III- 71-90– 0.9 % mortality
• Class IV- 91-130– 9.3% mortality
• Class V- >130– 27% mortality

CAP- Initial empiric treatment
• Respiratory fluoroquinolone (e.g. moxifloxacin)
Or . . .
• Macrolide (e.g. azithromycin) + beta-lactam (usually ceftriaxone)

CAP- special considerationsLegionella
• Legionella risk (relative risk in parentheses)– Glucocorticoids or Cushing’s disease (2-5)– Cytotoxic chemo (5)– Cigarette smoking (2-5)– Diabetes (2)– Male gender (>2)– Age >50 (>2)– AIDS (40)– Renal failure requiring dialysis (20)– Lung or hematologic cancer (7-20)
• Diagnostics- urine legionella antigen• Treatment- Erythromycin or tetracycline (usually
doxycycline)

CAP- special considerationsAspiration pneumonia
• Risk– Think of patients with loss of consciousness
(seizures, alcoholics), patients with neurological impairment
• The bugs– Gram-negative enteric pathogens– Mouth anaerobes
• Treatment for the hospitalized patient– Piperacillin/tazobactam 3.375g q6H– Imipenem 500mg q6H– Clindamycin 900mg IV q8H plus ciprofloxacin 400mg
q12H or Aztrenoam 1-2g q8H

The DACR paged you and the report is . . .
• 83 yo male with h/o CKD, COPD, Alzheimer’s who presents from nursing home with mental status change.
• T 102 HR 135 BP 86/40 RR 40
• On exam you find that patient has lower lobe rhonchi.
• How is this different from your other patient with pneumonia?

Defining Healthcare Associated Pneumonia
• Pneumonia in someone who. . .– Has developed pneumonia after being in
hospital ≥ 2 days– Was hospitalized for ≥ 2 days in the last 90
days– Resident of nursing home or long term care
facility (e.g. SNF)– Recently received IV antibiotics,
chemotherapy or wound care in past 30 days– Attended a hospital or hemodialysis clinic

Etiology of HCAP• Think of MDR pathogens

Risks for MDR

• Common bugs– Strep pneumo and H. flu- usually cause early rather
than late infections– Staph- worry about MRSA– Gram negative bacilli
• Pseudonas aeruginosa• E. coli• Klebsiella• Acinetobacter- if you suspect this then consider ID consult
and utilize full barrier and respiratory precautions

Treating HCAP
• Empiric antibiotics should be different classes than recently prescribed antibiotics

Recommendation for empiric therapy

Empiric treatment of HAP- early onset and no known risk factors for
MDR

Empiric treatment of HAP

Recommendation for empiric therapy
• Therapy can decreased to 7 days unless the infection is proven to be Acinetobacter or Pseudomonas

The DACR paged you and the report is . . .
• 60 yo male with pancreatic cancer who received gemcitabine 8 days ago presents with fever.
• On exam, T is 101.8, HR is 94, RR is 18, BP is 128/64. Exam is largely unremarkable.
• On labs his WBC is 0.8 with % neutrophils of 50%
• What do you think?

Neutropenic fever
• Fever (single oral temperature >101 or >100.4 for greater than one hour) in patient with ANC < 500 or in patient who has ANC <1000 with suspected nadir of <500

Epidemiology of Neutropenic fever
• ½ of patients who have ANC <500 and fever have established or occult infection
• 1/5 of patients who have ANC <100 have bacteremia

Problem with neutropenia
• They may not act infected– Patient with cellulitis may not have erythema
and induration– Patient with pneumonia may be without a
radiographic infiltrate– Patient with meningitis may not have
pleocytosis in CSF– Patient with UTI may not have pyuria on
urinalysis

Initial workup
• Blood cultures
• Urine cultures
• Sputum cultures
• CXR

Etiology
• Gram positive cocci account for 60-70% of proven bacterial infection in these patients

Low risk vs. high risk

Empiric therapy for high risk patients

Antivirals
• Should be used if signs and symptoms of HSV or VZV are present to heal portal of entry for bacteria

Duration of therapy

Fever resolved in first 3-5 days

Persistent fever in first 3-5 days

Colony-stimulating factors
• Not routinely recommended for therapy
• Consider in patients who are severely ill or who have documented bacterial infection, persistent neutropenia and are not responding to antimicrobial therapy

Uh-oh
• Your patient that you are treating for HAP begins to have profuse, watery diarrhea!

C. Diff Infection
• Clostridium difficileClostridium difficile is the most common is the most common infectious cause of healthcare associated infectious cause of healthcare associated diarrhea in the United Statesdiarrhea in the United States– 3.4 to 8.4 cases per 1000 admissions

Suspect C. diff
• What do you order?– C. diff toxin assay from 3 separate stools– Fecal leukocytes

Spectrum of diseaseSpectrum of disease• Asymptomatic carrier stateAsymptomatic carrier state
– 3% of healthy adults3% of healthy adults– 16-35% of hospitalized patients 16-35% of hospitalized patients
• Antibiotic associated diarrheaAntibiotic associated diarrhea– Accounts for 10-25% of casesAccounts for 10-25% of cases
• Colitis without pseudomembrane formationColitis without pseudomembrane formation– 60-75% of antibiotic associated colitis60-75% of antibiotic associated colitis
• Pseudomembranous colitisPseudomembranous colitis– 90-100% of antibiotic associated pseudomembanous colitis90-100% of antibiotic associated pseudomembanous colitis
• Fulminant colitis- 1-3% of patientsFulminant colitis- 1-3% of patients– May lead to ileus, toxic megacolon, perforation and deathMay lead to ileus, toxic megacolon, perforation and death

Pathogenesis- 3 hit theoryPathogenesis- 3 hit theoryFrom Cohen and PowderlyFrom Cohen and Powderly
Figure 44.1 The pathogenesis model for hospital-acquired Clostridium difficile -associated diarrhea (CDAD).]

Risk factors associated with Risk factors associated with Clostridium difficileClostridium difficile
Risk factor Comments
Specific antibiotics -Clindamycin -3rd generation cephalosporins -Fluoroquinolones
Cefazolin OR=3.5Levofloxacin OR=2.1
Increasing age OR=2.8 for age >71
Use of proton pump inhibitor OR=2.1
Gastrointestinal surgery OR=7.9
Length of stay >7 days OR=2.3
Feeding via NG tube OR=2.8
Admission to intensive care unit

Treatment of clostridium difficileTreatment of clostridium difficile
• Stop offending antibioticStop offending antibiotic– Leads to resolution in 15-23% of patientsLeads to resolution in 15-23% of patients
• Antibiotics - similar efficacy with resolution in Antibiotics - similar efficacy with resolution in approximately 93% of patientsapproximately 93% of patients– Oral metronidazole 500mg TIDOral metronidazole 500mg TID– Oral vancomycin 125mg QID as second line Oral vancomycin 125mg QID as second line
treatmenttreatment• Avoid anti-motility agentsAvoid anti-motility agents
– Leads to ileus and toxic megacolon formationLeads to ileus and toxic megacolon formation• Supportive measuresSupportive measures

THE END
Related Documents