BY Dr. Pratibha.C.Hullur BAMS (K.U.Dharwad) Dissertation submitted to the Rajiv Gandhi University of Health sciences, Karnataka, Bangalore in partial fulfillment of the requirements for the degree of Ayurveda Vachaspati” [M.D.] in KAYACHIKITSA GUIDE Prof. Pramod Kumar Mishra MD (Ayu), (RSU) Head of the Department Kayachikitsa DEPARTMENT OF POST GRADUATE STUDIES IN KAYACHIKITSA A.L.N.RAO MEMORIAL AYURVEDIC MEDICAL COLLEGE KOPPA - 577126 CHIKMAGALUR DISTRICT, KARNATAKA, INDIA MARCH - 2006

Amlapitta kc007 kop
Oct 19, 2014
A CLINICAL STUDY ON THE EFFECT OF SHATAVARI CHOORNA WITH ABHRAKA BHASMA IN THE MANAGEMENT OF AMLAPITTA , Pratibha.C.Hullur , PG Studies in Kayachikitsa, A.L.N. Rao Memorial Ayurvedic Medical College and P. G. Centre, Koppa.
Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

BY Dr. Pratibha.C.Hullur
BAMS (K.U.Dharwad)
Dissertation submitted to the
Rajiv Gandhi University of Health sciences, Karnataka, Bangalore
in partial fulfillment of the requirements for the degree of
Ayurveda Vachaspati” [M.D.]
in
KAYACHIKITSA
GUIDE Prof. Pramod Kumar Mishra
MD (Ayu), (RSU) Head of the Department
Kayachikitsa
DEPARTMENT OF POST GRADUATE STUDIES IN KAYACHIKITSA A.L.N.RAO MEMORIAL AYURVEDIC MEDICAL COLLEGE KOPPA - 577126
CHIKMAGALUR DISTRICT, KARNATAKA, INDIA MARCH - 2006
Ayurmitra
TAyComprehended

A.L.N.Rao Memorial Ayurvedic Medical College Koppa – 577126 Dist: Chikmagalur
Department of Post Graduate Studies in KAYACHIKITSA
I here by declare that this dissertation entitled “A CLINICAL STUDY
ON THE EFFECT OF SHATAVARI CHOORNA WITH ABHRAKA BHASMA
IN THE MANAGEMENT OF AMLAPITTA” is a bonafide and genuine
research work carried out by me under the guidance of Prof. Pramod Kumar Mishra, HOD, Department of Post Graduate
Studies in Kayachikitsa, A.L.N. Rao Memorial Ayurvedic Medical College and
P. G. Centre, Koppa.
Date:
Place: Koppa
Dr. Pratibha.C.Hullur P.G.Scholar, Dept. of Kayachikitsa, A.L.N. Rao Memorial Ayurvedic Medical College, Koppa – 577 126
Ayurmitra
TAyComprehended

A.L.N.Rao Memorial Ayurvedic Medical College Koppa – 577126 Dist: Chikmagalur
Department of Post Graduate Studies in KAYACHIKITSA
This is to certify that the dissertation entitled “A CLINICAL STUDY ON
THE EFFECT OF SHATAVARI CHOORNA WITH ABHRAKA BHASMA IN
THE MANAGEMENT OF AMLAPITTA” is a bonafide research work done by
Dr.Pratibha.C.Hullur., in partial fulfillment of the requirement for the
degree of Ayurveda Vachaspati (MD) in Kayachikitsa of Rajiv Gandhi
University of Health Sciences, Bangalore, Karnataka.
Date:
Place: Koppa
Guide:Prof. Pramod Kumar Mishra
MD (Ayu), (RSU) Head of the Department Post Graduate Studies in Kayachikista A.L.N. Rao Memorial Ayurvedic Medical College, Koppa – 577 126

A.L.N.Rao Memorial Ayurvedic Medical College Koppa – 577126 Dist: Chikmagalur
Department of Post Graduate Studies in KAYACHIKITSA
This is to certify that the dissertation entitled “A CLINICAL STUDY ON
THE EFFECT OF SHATAVARI CHOORNA WITH ABHRAKA BHASMA IN
THE MANAGEMENT OF AMLAPITTA” is a bonafide research work done by
Dr.Pratibha.C.Hullur., under the guidance of Prof. Pramod Kumar Mishra, HOD, Department of Post Graduate Studies in
Kayachikitsa, A.L.N. Rao Memorial Ayurvedic Medical College and P. G.
Centre, Koppa.
Date:
Place: Koppa
Dr.Jagadeesh Kunjal MD., (Ay).,
Principal, A.L.N.Rao Memorial Ayurvedic Medical College. Koppa –577126, Dist: Chikmagalur

COPYRIGHT
I here by declare that the Rajiv Gandhi University of Health Sciences,
Karnataka shall have the rights to preserve, use and disseminate this
dissertation in print or electronic format for academic/research purpose.
Date:
Place:
Dr.Pratibha.C.Hullur P.G.Scholar, Dept. of Kayachikitsa, A.L.N. Rao Memorial Ayurvedic Medical College, Koppa – 577 126
© Rajiv Gandhi University of Health Sciences, Karnataka

INDEX
Page No.
INTRODUCTION 1-2
Chatper – I OBJECTIVES 3
Chapter – II REVIEW OF LITERATURE
Historical Review 4-6
Nirukti,Paribhasha,Paryaya. 7-10
Anato-physiological consideration 11-18
Nidana 19-24
Samprapti 25-37
Poorvarupa 38
Rupa 39-47
Upashaya – Anupashaya 48
Vyavacheddaka Nidana 49
Sadhya asadhyata 50
Upadravas 51
Chikitsa 52-56
Pathya Apathya 57-59
Dyspepsia 60-69
Drug Review 70-79
Chapter –III METHODOLOGY
Materials and Methods 80-90
Observations 91-116
Chapter –IV RESULTS 117-132
Chapter –V DISCUSSION 133-147
Chapter –VI CONCLUSION 148-149
SUMMARY 150-152
BIBLIOGRAPHY
ANNEXURES

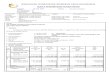
LIST OF TABLES Sl. No SUBJECT PAGE NO
1. Showing pitta guna 14
2. Guna-karma vivecana 21-22
3. Showing the lakshanas of amlapitta mentioned by different
authors
41
4. Lakshanas of Urdhvaga amlapitta 42-43
5. Showing the lakshanas of Sanila Amlapitta 44
6. Showing the lakshanas of Sakapha Amlapitta 45
7. Showing the lakshanas of Shleshmapittaja Amlapitta 46
8. Showing the lakshanas of Pittaja Amlapitta 46
9. Showing the referance of vamana and Virechana Karma in
Amlapitta
54
10. Showing Pathya apathya 57-58
11. Distinguishing between functional and organic/structural disease
of gastrointestinal tract.
66
12. Symptoms of Functional dyspepsia Comparison with Amlapitta 69
13. Showing the age wise distribution of 60 Amlapitta patients. 91
14. Showing the Sex wise distribution of 60 Amlapitta patients. 92
15. Showing the Religion wise distribution of 60 Amlapitta patients 92
16. Showing the Marital status wise distribution of 60 Amlapitta
patients
93
17. Showing the Educational status wise distribution of 60 Amlapitta
patients
94
18. Showing the socioeconomic status wise distribution of 60
Amlapitta patients
95
19. Showing the Occupational status wise distribution of 60 Amlapitta
patients
96
20. Showing the onset wise distribution of 60 Amlapitta patients 96
21. Showing the Aggravating period wise distribution of 60 Amlapitta
patients
97

22. Showing the Incidence Aggravating of symptoms due to
environmental factors in 60 Amlapitta patients
98
23. Showing the Habitat status wise distribution of 60 Amlapitta
patients
98
24. Showing the Dietary habit wise distribution of 60 Amlapitta
patients
99
25. Showing the Ahara vidhi wise distribution of 60 Amlapitta
patients
99-100
26. Showing the Type of diet wise distribution of 60 Amlapitta
patients
100
27. Shows Rasa Satmya wise distribution of 60 Amlapitta patients 101
28. Showing the Regimen wise distribution of 60 Amlapitta patients 102
29. Showing the Mental stress/strain wise distribution of 60 Amlapitta
patients
102
30. Shows incidence of Addictions in 60 Amlapitta patients 103
31. Showing the Exercise wise distribution of 60 Amlapitta patients 104
32. Shows incidence of nidra in 60 Amlapitta patients 105
33. Shows Bowel habit wise distribution of 60 Amlapitta patients 105
34. Shows Nature of stool wise distribution of 60 Amlapitta patients 106
35. Shows Type of occupation wise distribution of 60 Amlapitta
patients
107
36. Shows Nature of work wise distribution of 60 Amlapitta patients 107
37. Shows incidence of Deha prakriti in 60 Amlapitta patients 108
38. Shows Sara wise distribution of 60 Amlapitta patients 109
39. Shows Samhanana wise distribution of 60Amlapitta patients 109
40. Shows Satva wise distribution of 60 Amlapitta patients 110
41. Shows Agni wise distribution of 60 Amlapitta patients 111
42. Shows Koshta wise distribution of 60 Amlapitta patients 111
43. Shows Bala wise distribution of 60 Amlapitta patients 112
44. Shows Desha wise distribution of 60 Amlapitta patients 113
45. Shows Duration of Illness wise distribution of 60 Amlapitta 113

patients
46. Shows Samanya lakshana wise distribution of 60 Amlapitta
patients
114
47. Shows Associated symptom wise distribution of 60 Amlapitta
patients
115
48. Shows Srotodusti wise distribution of 60 Amlapitta patients 116
49. Effect of Trial drug on Main symptoms after Treatment 117
50. Effect of Trial drug on Main symptoms after follow up 117
51. Effect of Control drug on Main symptoms after Treatment 118
52. Effect of control drug on Main symptoms after follow up 119
53. Effect of Trial drug on Associated symptoms after Treatment 119
54. Effect of Trial drug on Associated symptoms after follow up 120
55. Effect of Control drug on Associated symptoms after Treatment 121
56. Effect of Control drug on Associated symptoms after follow up 122
57. Effect of Trial drug on Srotodusti after Treatment 123
58. Effect of Trial drug on Srotodusti after follow up 123
59. Effect of Control drug on Srotodusti after Treatment 124
60. Effect of control drug on Srotodusti after follow up 124
61. Total effect of Trial drug and Control drug After treatment 125
62. Total effect of Trial drug and Control drug After follow up 125
LIST OF GRAPHS Sl.No. Page No.
1. Showing the age wise distribution of 60 Amlapitta patients. 91
2. Showing the Sex wise distribution of 60 Amlapitta patients. 92
3. Showing the Religion wise distribution of 60 Amlapitta patients 93
4. Showing the Marital status wise distribution of 60 Amlapitta patients 93
5. Showing the Educational status wise distribution of 60 Amlapitta
patients
94
6. Showing the socioeconomic status wise distribution of 60 Amlapitta
patients
95

7. Showing the Occupational status wise distribution of 60 Amlapitta
patients
96
8. Showing the onset wise distribution of 60 Amlapitta patients 97
9. Showing the Aggravating period wise distribution of 60 Amlapitta
patients
97
10. Showing the Incidence Aggravating of symptoms due to
environmental factors in 60 Amlapitta patients
98
11. Showing the Habitat status wise distribution of 60 Amlapitta patients 99
12. Showing the Dietary habit wise distribution of 60 Amlapitta patients 99
13. Showing the Ahara vidhi wise distribution of 60 Amlapitta patients 100
14. Showing the Type of diet wise distribution of 60 Amlapitta patients 101
15. Shows Rasa Satmya wise distribution of 60 Amlapitta patients 101
16. Showing the Regimen wise distribution of 60 Amlapitta patients 102
17. Showing the Mental stress/strain wise distribution of 60 Amlapitta
patients
103
18. Shows incidence of Addictions in 60 Amlapitta patients 104
19. Showing the Exercise wise distribution of 60 Amlapitta patients 104
20. Shows incidence of nidra in 60 Amlapitta patients 105
21. Shows Bowel habit wise distribution of 60 Amlapitta patients 106
22. Shows Nature of stool wise distribution of 60 Amlapitta patients 106
23. Shows Type of occupation wise distribution of 60 Amlapitta patients 107
24. Shows Nature of work wise distribution of 60 Amlapitta patients 108
25. Shows incidence of Deha prakriti in 60 Amlapitta patients 108
26. Shows Sara wise distribution of 60 Amlapitta patients 109
27. Shows Samhanana wise distribution of 60Amlapitta patients 110
28. Shows Satva wise distribution of 60 Amlapitta patients 110
29. Shows Agni wise distribution of 60 Amlapitta patients 111
30. Shows Koshta wise distribution of 60 Amlapitta patients 112
31. Shows Bala wise distribution of 60 Amlapitta patients 112
32. Shows Desha wise distribution of 60 Amlapitta patients 113
33. Shows Duration of Illness wise distribution of 60 Amlapitta patients 114

34. Shows Samanya lakshana wise distribution of 60 Amlapitta patients 115
35. Shows Associated symptom wise distribution of 60 Amlapitta
patients
116
36. Shows Srotodusti wise distribution of 60 Amlapitta patients 116
37. Showing comparative effect of therapies on main symptoms after the
treatment
126
38. Showing comparative effect of therapies on main symptoms after
follow up
127
39. Showing comparative effect of therapies on associated symptoms
after the treatment
128
40. Showing comparative effect of therapies on associated symptoms
after follow up
129
41. Showing comparative effect of therapies on srotodusti after the
treatment
130
42. Showing comparative effect of therapies on srotodusti after follow
up
130
43. Showing comparative total effect of therapies after treatment 131
44. Showing comparative total effect of therapies after follow up 132
LIST OF CHARTS No. Page No.
1. Schematic Representation of Amlapitta Nidanana 20
2. Showing the classification of Nidanas of Amlapitta 24
3. Schematic Representation of Samprapti of Amlapitta 31
4. Schematic Representation of Samprapti on basis of Kriyakala 37
5. Schematic Representation of Vicious circle formed in Amlapitta 37
6. Schematic Representation of manifestation of symptoms 40
7. Schematic Representation of Classification according to different
Authors
47

ABBREVIATIONS
A.T After treatment
As.Hri Ashtanga hridaya
As.San Ashtanga sangraha
B.T Before treatment
Ba.Pr Bhava prakasha
Bh. Bhela samhita
Ch Charaka
Ch Su Charaka sutra
Chi Chikitsa sthana
D M Digestion and Metabolism
Ha Harita samhita
Kha.Sam Kashyapa samhita
Ma. Ni Madhava nidana
Ma.Kha Madhyama khanda
Ni Nidana sthana
Sha Sam Sharangadhara samhita
Sa Sharira sthana
Su Su Sushruta samhita sutra sthana
Vi Vimana Sthana
Ut Uttara Tantra
V.S Vanga sena
Y.R Yoga Ratnakara
B.R Baishajya Ratnavali
D.G Dravya Guna
O.T.P Oxford Text book of Pathology
R.R.S Rasa Ratna Sammuchaya
C.S.S Chikitsa Sara Sangraha

ABSTRACT
Amlapitta has become one of the common problems today due to the change in
lifestyle. Sophistication and a stressful life to keep pace with the fast developing world.
Amlapitta is more of a psycho somatic disorder caused due to dietetic indiscrimination
and mental stress and strain. A good member of medicines have been mentioned as the
modern medicines for the management of Amlapitta, but their merits trail.
Amlapitta is a pitta pradhana disease of the annavaha stotas caused due to
mandagni, ama and annavaha sroto dusti. It is characterized by Amlodgara, Utklesha and
Hrtkanta daha indicating the vikruthi of pachakapitta along with the kledaka kapha and
samana vayu. the patho-physiology of the Amlapitta states it to be a diseases caused due
to functional disturbance rather than organic lesion. While describing the progonosis of
Amlapitta, it has been stated that it can be cured easily if promptly treated at the earliest
with proper pathyapthya.
A larger number of yoga have been mentioned in Ayurveda in the management of
Amlapitta, among which “Shatavari Choorna” and “Abhraka Bhasma” are among the
commonly used ingredients.
In the present study an attempt is being made to understand the pathophysiology
of the diseease in principles of Ayurveda and also to control and treat the disease with a
simple herbo-mineral combination.

Objectives:
1. To evaluate the efficacy of “Shatavari Choorna” with “Abhraka Bhasma” in the
management of Amlapitta.
2. To compare the effect of “Shatavari Choorna” with Abhraka Bhasma over liquid
antacid by controlled trial.
3. Treating the disease by correcting the samprapti rather than symptoms.
4. Detailed study of disease covering classical and modern literature.
5. To establish an effective, simple herbo-mineral combination in the management
of Amlapitta.
Methodology :
Total of 64 patients who fulfilled the inclusion criteria were randomly selected for
the study. Among them 4 patients dropped out. Hence, the study was conducted on the
reaming 60 patients. The patients were randomly grouped into two groups i.e. trial group
and control group each comprising of 30 patients.
The trial group was given “Shatavari choorna” – 3 gms. and Abhraka Bhasma –
125 mg. along with gritha before meals thrice daily for a duration of 1 month.
The control group was given Syrup Gelusil – 1tsp. before meals thrice daily for a
duration of 1 month.
During this period both the groups were adviced to follow the pathyapathya
Both the groups were fallowed up for a month after the treatment.
During the treatment schedule, the various subjective signs and symptoms were
observed and recorded in the special perform made for purpose.

Interpretation of the Results:
At the end of the treatment schedule of 1 month and also the follow-up period of 1
month, the observations which were recorded were subjected to statistical analyses. It
was found that the trial group showed highly significant relief [p<0.001 to p<0.010] in
almost all the patients in their presenting complaints after treatment and highly significant
to moderately significant relief even after the fallow-up. Whereas, the control drug
showed highly significant to moderately significant relief in all the presenting complaints
after the treatment but the reccurence of symptoms was observed after follow-up.Trail
drug showed more number of improved cases,whereas the control drug showed
controlled effect in more number of cases after the follow-up
Conclusion:
1. The trial drug is more effective in the management of Amlapitta as it pacifics pitta
does Agnideepana, reduces the ama and corrects the srotodusti.
2. The trial drug provides significant relief in the management of symptoms like
Hrthdaha –Amlodgana. Utklesha, and Udarashoola even after the follow-up.
3. It also showed highly significant relief in the management of Aruchi, Avipaka,
Gurukoshtata and Adhmana after the treatment as well as after the follow-up.
4. The trial drug showed highly significant relief in the srotodusti symptoms after the
treatment as well as after the follow-up when compared to control drug.
5. The control drug does give significant and fast relief but does not show sustained
effect after follow-up and reccurence of symptoms was observed.
6. The trail drug seems to act like an antacid and pacify the symptoms.It also corrects
the agni at the same time and reduces further reccurence of the symptoms.

ACKNOWLEDGEMENT
It would be a great pleasure to acknowledge my gratitude to all those who helped me in bringing out this work. Its my great pleasure to confirm my gratitude to my teacher and uncle Dr.S.S.Hosmani. Retd. Principal Sri B.M.Kankanwadi Ayurveda Mahavidhyalaya. Belgaum. who has been my inspiration to step into the field of Ayurveda. My sincere thanks and salutation to him. I will remain grateful forever to Prof. P.K.Mishra. M.D [Ayu.] H.O.D. Dept of Kayachikitsa , A.L.N.Rao Memorial Ayurvedic College, Koppa, Post Graduate Centre, for his valuable guidance, meticulous supervision, timely advices, motivation and co-operation that he extended towards me throughout this dissertation work. I am grateful to Sri. Aroor Ramesh Rao President. Aroor Trust Koppa, for giving me a chance to pursue my post graduation studies in his esteemed institution. I am grateful to Dr. Jagdeesh Kunjal M.D [Ayu.] Principal,A.L.N.Rao Memorial Ayurvedic College, Koppa, for his help and support, both as the head of the institute and as a guide in completing his work. I am grateful to Prof.Narayana Sharma, M.D.[Ayu] Dept to Kayachiktsa , Prof. Pandey M.D [Ayu.] Dept of Rasashastra, Jamnagar, Dr. Sarshetty. M.D [Ayu.] HOD Dept of Rasa shastra, Bijapur and Dr. Prashanth. A.S. M.D [Ayu.] Prof. Department of Kaya chikitsa, Hubli for their help in my initial days of work and in preparing the base work for the present study. My sincere gratitude to Prof. D.S. Lucas, M.D [Ayu.] FRAS [London] FRAV [India], H.O.D. Department of Dravyaguna for his motivational inspiration and support. I am grateful to Dr. S.M. Shanbhag; M.B.B.S. Dr. Lalitha Bhaskar. M.D [Ayu.]; Dr. N.V. Ramesh M.D [Ayu.] A.L.N. Rao

Memorial Ayurvedic Medical College Koppa for their support in selection of the patients and during the study. I immensely thank Dr. Dinesh Kumar Mishra, Reader Dept. of Rasa shastra and Bhaishajya Kalpana for his co-operation in preparing the medicine for the trial, and also his suggestions. At this juncture, I take the opportunity to thank Mr. Mathew, Mr. Nityananda and Miss Violet, who took the pain in preparing the medicine for the trial in a short duration of time. I am thankfull to Dr. Kajrekar, M.D [Ayu] Belgaum for helping me in getting the Abhraka Bhasma prepared from his pharmacy. I am grateful to Dr. Sanjay K.S, M.D [Ayu] : Dept of Dravya guna. A.L.N. Rao Memorial Ayurvedic College Koppa, for his support in collecting the study material. I am thankful toDr. Banmali Das, M.D [Ayu] Dept. of Roga Vignana, Dr. Galib, M.D [Ayu] , Dept of Rasa Shastra and Bhaishajya Kalpana , Dr. Sridhar V, M.D [Ayu] Dept of Dravya guna, A.L.N. Rao Ayurvedic Medical College Koppa, for their timely suggestions and help. My heartfelt thanks to Dr. Prasanna Kerur M.D.[Ayu] Dept of Kayachikitsa, S.D.M. Ayurveda College, Hassan; because of whom I was able to pursue my P.G. studies. I am grateful to Dr. Mangalgi M.D [Ayu] H.O.D Dept of Kayachikitsa. Mysore and Dr. [Mrs.] Aruna. Mangalgi M.D. [Ayu] Dept of Kayachikitsa. Mysore for helping me to collect the study material and use the P.G. Library at Mysore. I am thankful to Dr. Rangesh Parmesh. M.D [Ayu] R&D. The Himalaya Drug Company for helping me to get information regarding some recent studies on the trial drug used in the study. I am thankful to Dr. T.K. Mohanta, M.D [Ayu] Ph.D and Dr. Rashmi, Rekha, Mishra, M.D. [Ayu]. Dept of Kayachikitsa A.L.N. Rao Memorial Ayurvedic Medical College for there help during my work.

I am thankful to Mrs. Jyotsna for her valuable help in conducting laboratory investigations. I am grateful to Mr. Satish H.D Librarian and Miss Triveni who helped me a lot in my reference work. I also thank Sri, Ramesh Gowda and Mrs. Jyothi for the help. I am thankful to Dr. Mahesh Desai. P.G. Dept of Shalya Tantra, Hubli Ayurveda College for his valuable support throughout my P.G studies. I am grateful to Dr. Sanjay, P.G. Dept of Kayachiksta, Mysore for his help. I express my sincere thanks and gratitude to my friend Mr. Srinivas. H.M. for his support throughout my work, and also in completing it. I would like to submit my heartfelt thanks to Mr. Sanjay K. Handur, Senior Manager, Regulatory Affairs, Himalaya Drug Company for helping me in collecting the study material and his moral support throughout my work. I express my sincere thanks and gratitude to my P.G. Classmates Dr. Ravi Ganesh; Dr. James chako; Dr. Sharat Babu; Dr. Bijayendra; Dr. Kavitha B.M.; Dr. Suja Nair; Dr. Roshy Joseph; Dr. Prashanth B.K; Dr. Vishwanath; Dr. Binu Alapat; Dr Sajeev Athani; Dr. Pradeepa; Dr. Krishna Kishore; Dr. Pankaj Prasad and Dr. Parthasarthy for their support and help in completing this work. I am thankful to my seniors Dr. Srinivas, Dr. Sujatha Tenginkai; Dr. Pradeep K.V; Dr. Christy Joseph ; Dr. Indu and also my junior P.G.’s. for their kind co-operation during my study. My heartfelt thanks to Dr. H.R. Pradeep M.D [Ayu] and his family for their moral support during my stay and also in my work. I am gratefull to Dr.Mangalagouri Rao,M.D [Ayu] and Dr.Elizebeth.P.Johan M.D[Ayu]. A.L.N. Rao Memorial Ayurvedic Medical College and my student Dr.Pratibha.Hegde for their help and moral support during my work.

I am thankful to Mr. Shreedhar Gowda and Miss.Sujaya for heir friendly help in typing, editing and speedy completion of this dissertation work. I am indebted to my parents whose blessings, affection and encouragement helped me to complete my work. I owe my salutation and thanks to them. I am grateful to my brothers for their love, support and encouragement. Finally thanks to all those people who helped me directly and indirectly to complete this work. Date :
Place : Dr. Pratibha C. Hullur.

Introduction
1
INTRODUCTION
Ayurveda is known to be one of the oldest scientific medical systems in the
world. Kayachikitsa is one of the important eight major specialties of Ayurveda which
corresponds to general medicine. Its defined as ‘antaragni chikitsa’ by Chakrapanidutta
which involves both digestive and metabolic disturbances. The therapeutic principles of
Ayurveda governing both the prevention and cure of diseases are based on this concept.
Most of the diseases arise from abnormal functioning of the digestive system.
Improper digestion results in the accumulation of undigested food which inturn becomes
the pathogen in the body, breeding toxins leading to upsetting of auto immune system.
The role of agni draws greater importance in Ayurveda, as most of the diseases are
caused by mandagni.
In this fast advancing era, the modernization has led to the advent of bad cooking,
over indulgence, anxiety and stress induced hectic unhealthy schedules. These, along
with sophistications and indiscriminate dietary habits has strong influence over the
annavaha srotas leading to various diseases among which Amlapitta is one such.
Amlapitta, being a disease of Annavaha srotar is a psycho-somatic disorder
caused due to mandagni and vitiation of pitta. i.e. pachaka pitta. This presents a group of
signs and symptoms viz Avipaka [Indigestion], Amlodgara [Acid eructation], Hrtdaha
[Heart burn], Kanta daha [Burning in throat] Utklesha [Nausea] etc. which has a startling
similarities in all most all the aspects to Non-ulcer Dyspepsia or Functional Dyspepsia.
The pathogenesis of Amlapitta involves three important factors, i.e Agnimandya,
Ama and Annavaha sratodusti. Along with these, the vitiation of pitta leading to
qualitative and quantitative increase of pachaka pitta especially in its amla and drava
guna gives rise to Amlapitta. Non-ulcer dyspepsia is a condition or disorder of G.I.T.
characterized by dyspeptic signs and symptoms seen in most of the acid-peptic disorders
with no evidence of any organic lesions.

Introduction
2
Dyspepsia is extremely prevalent, affecting up to 80% of the population at some
time, and very often no abnormality is discovered during investigations especially in
younger patients [< 40 years of age]. Hence, most of the patients fall under Non-Ulcers
dyspepsia / functional dyspepsia. Women are said to be affected twice as commonly as
men.
As proper pathogenesis is not established its termed as functional disorder and
thought to be due to mucosal or motility disorder or psychological disturbances, drugs or
habits. These factors have been highlighted in the Ayurvedic science as the prime factors
for the manifestation of Amlapitta. Hence to over come this, the trial drug Shatavari
choorna and Abhraka Bhasma with gritha was selected.
A large mumber of yogas have been mentioned in classics for the management of
Amlapitta, among which the “Shatavari Choorna” and “Abhraka Bhasma” are one of the
ingredients in these yogas. Hence, an attempt has been made in this study to assess the
efficacy of this simple, safe, easy to administer herbo mineral combination in the
management of Amlapitta.
The diagnosis of the disease Amlapitta is done on the basis of classical signs and
symptoms. Before the assessment, the signs and symptoms will be graded and scored.
Then they will be subjected to statistical analysis.
The whole study has been distributed into two major divisions –
The conceptual study : which is grouped into Literary Review and Drug Review.
The clinical study : contains Material Methods, Observations, Results,
Discussion, Conclusion, Summary and Bibliography.
The whole study is a stepping-stone to the evolution in the field of Ayurveda in
the management of Amlapitta and to provide a better, and simple herbo-mineral
combination.

Objectives
3
OBJECTIVES
1. To evaluate the efficacy of “Shatavari Choorna” with “Abhraka Bhasma” in the
management of amlapitta.
2. To compare the effect of Shatavari choorna with Abhraka Bhasma over liquid
antacid by controlled trial.
3. Treating the disease by correcting the samprapti rather than symptoms.
4. Detailed study of disease covering classical and modern literature.
5. To establish an effective, simple herbo-mineral combination in the management
of Amlapitta.
HYPOTHESIS
1. Null Hypothesis : Shatavari choorna and Abraka Bhasma with Gritha does not
have any effect in the management of patients suffering from
Amlapitta.
2. Alternative Hypothesis : Shatavari choorna and Abraka Bhasma with Gritha is
effective in the management of patients suffering from
Amlapitta.

Review of literature – Disease review
4
CHAPTER-3
REVIEW OF LITERATURE
A. DISEASE REVIEW
The chronological description of the disease Amlapitta offers a very intresting
pictures about its evolution .The review of the vedic literature shows no suggestive
evidence of Amlapitta described in vedic period , but some passing references can be
seen .
VEDIC PERIOD [from Pre- historic era to 2500 B.C]
1. In Atharvaveda the term ‘Agni’ has been described which plays an important role in
the genesis of Amlapitta
2. In Garuda purana a passing reference to this disease and its treatment is found in the
chapter of Nadivrana chikitsa
3. The term “Shoola” an important feature of Amlapitta is that mentioned in Kaushika
sutra of Atharva veda 1
SAMHITA KALA
In Charaka Samhita [1000 B.C]:
Scattered refences of Amlapitta is available .
a) While explaining about the qualities of milk it has been indicated as pathya in Pandu
roga , Amlapitta etc.2
b) Kulatha has been mentioned as chief etiological factor for Amlapitta3
c) While stating the effects caused due to excessive use of lavana rasa, there is a
mention that it provokes pitta , lohita pitta, amlapitta etc.4

Review of literature – Disease review
5
d) Amlapitta is also mentioned in the context of illeffects of vidhi virudha ahara sevana.5
e) Rajamasha is more beneficial in Amlapitta disorder.6
f) While describing grahani dosha , pathogenesis of Amlapitta has been
clearly mentioned .7
g) Mahatikthaka gritha has been indicated in Amlapitta. 8
h) While explaining the pittaja nantamja diseases the terms Dumaka
Amalaka and Vidaha have been mentioned which are seen in Amlapitta. 9
i) Indications of Kansa Haritaki also includes Amlapitta. 10
In Sushrutha Samhita :
The term Amlapitta or the desription the disease has not been mentioned in
Sushrutha samhita .
In Bhela samhita there is no any reference about this disease.
Vaghbhata has mentioned that excessive use of kulatha causes Amlapitta .11
In Harita samhita no description of Amlapitta is found.
Kashyapa samhita first describes Amlapitta as a seperate disease entity in
khilasthana 12
.and has explained its nidana , lakshana , samprapti and chikitsa
elaborately.
SANGRAHA KALA(500 B.C. to 600 B.C.)
Most of the commentaries were written during this period on various texts and
also some original texts were written.
In Baudha sarvaswa [Baudha literature] only the treatment of Amlapitta is mentiond.

Review of literature – Disease review
6
In Ranvir Prakash a gleaming description of Amlapitta with some astrological
relations has been described .
MADHYA KALA [ 600 A.D to 1800 A.D]
Madhavakara [18th A.D] in his treatise has seperatly dealt with Amlapitta with
respect to nidana , lakshanas and bheda in 51th chapter.13
Bhavaprakasha [16 A.D]14 in the the 10th chapter and Yogaratnakara[ 17 A.D] in
Amlapitta nidana chapter have dealt in detail reagrding nidana , lakshana , samprapti
and chikitsa of Amlapitta.
Sharangadhara[14 A.D]15 has explained a few yogas usefull in Amlapitta in different
context and 3 types of Amlapitta.
Basavrajeeyam deals about the nidana , lakshana and chikitsa of Amlapitta in its
saptama prakarna.
A detailed description regarding Amlapitta chikitsa has been quoted in Chakradutta
52nd chapter.
ADHUNIKA KALA
In Bhaishajya Ratnavali [ 19th cent A.D] amlapittadhikara and Yogatarangini 64th
taranga : the nidana lakshana and chikitsa have been explained in detail .
In Rasaratna sammuchaya a detailed description of the samanya lakshanas and
treatment of Amlapitta is found.
In Sidhanta Nidana [ 20 A.D] 6th chapter a brief explainantion about nidana
samprapti , lakshana, upadrava and sadyasadhyata of Amlapitta has been explained .
Apart from these texts later subsequent authors have decribed Amlapitta as a disease
in their works.

Review of literature – Disease review
7
NIRUKTI , PARIBHASHA AND PARYAYA OF AMLAPITTA
NIRUKTI
The word Amlapitta connotes the pathological change in humour pitta found in
this disease. Literally it means that the pitta is of sour taste. An attempt has been made in
the available ayurvedic and allied literatures to define the word differently.
Etymologically the word “Amlapitta” comprises of two components i.e .“Amla”
and “ Pitta ”
The word ‘amla’ has commonly been used to express one of the six kinds of tastes
[Shabda Kalpadruma] In this present context the meaning of the amla can be taken as one
of the properties of pitta.
According to Charaka, the natural quality of pitta is said to be both Amla and
Katu 1. It may be mentioned here that the sour taste of pitta has been considered as the
physiological property of pitta 2 . The justification for the use of the word as an adjective
of pitta may be interpreted that though the physiological properties of pitta is sour,
normally it is never felt in physiological states.
Sushrutha in sutrasthana quotes that the natural quality of pitta is katu and when it
attains vidagadhata it changes into amla3 . Hence it can be interpreted that the pitta in its
nirama avastha has got katu rasa and in sama avastha it attains amla rasa.
The second component word “pitta” is derived from the dhatu ‘tap’ ie to heat or to
burn or to warm 4 . This term seems to have three meaning ie. tap santape, tap dahe and
tap aishwarye [ siddanth kaumudi]
1. Tap santape :- Refes to the generation of heat.
2. Tap dahe :- Relates to the act of burning of nutrition which is consumed .
3. Tap aishwarye :- Refers to those factors which are responsible to make one achieve
the eight folds of benefits .
These references are obtained from the Bhattaji’s “ Siddanth Kaumudi” and the
words furnish the Vyakarna version of the term pitta.

Review of literature – Disease review
8
In this present context, if from the word ‘amla’ we take its meaning as diseased,
then etymologically amlapitta may be said to be a diseased state, where the amla guna of
pitta gets augmented, and consequently in turn disturbs the doshic equilibrium of the
body especially of pitta dosha.
PARIBHASHA
Chakrapani in his commentary on charaka samhita defines amlapitta as.
“ Amlapittam cheti amlagunoundriktam pittam” 5
The augmented or increased amla guna of pitta is known as Amlapitta.
Srikantadutta in his Madhukosha vyakya defines
“ Vidahadhyamla gunaoundrikta pittam amlapittam” 6 .
That is, the pitta becomes augmented or vidagdha because of excessive increase
of amla guna of pitta and
“ Amlam vidagdham cha tat pittam amlapittam” 7
The pitta which attains amla guna and vidagdhata is called as amlapitta.
Apart from the above there are other definitions of amlapitta they are:
In Sanskrit dictionary vachaspathyam its defined as
“ Amlaya Pittam Amlapittam “ 8
Amlapitta is a disease where pitta attains sour taste. In this condition whatever is
eaten is transformed into amla rasa due to pathological pitta.
Sushrutha has also cited a reference to this fact that disorders of pitta of annavaha
srothas may lead to vidaha of food. 9
According to Sanskrit dictionary [ viswakors]
“ Amlath ajeernath yat pittam amlapittam “ 10
Amlapitta is a condition caused due to the increased sourness of pitta and
improper or ill digestion of the food. The same has been explained in Charaka where he
quotes that the impaired agni is unable to digest even the lightest food and hence the

Review of literature – Disease review
9
undigested food particles turns sour due to fermentation and leads to formation of
annavisha. This annavisha combines with pitta and produces amlapittam. 11
According to Kashyapa the vidagdha annarasa turns to shukta, this shukta annarasa is
retained in amashaya combines with the vrudda pitta and produces amlapitta. 12
According to Madhava Nidana, the amlapitta is that condition where the pitta which
has previously accumulated from its self aggravating causes gets vidagadha due to
viruddha [incompatible diets], dushta [ spoiled / state food ], amla [sour] , vidahi
[fried] and pitta provokating foods and drinks.13
These two definations to a certain extent speak of nindana and samprapti of the
disease.
PARYAYA
The paryayas (synonyms) of amlapitta signify different aspects of it. Indu15 in his
commentary on Ashtanga Sangraha has given synonyms of amlapitta as
Prameelaka
Amlapitta
Pittavisuchika
Yogaratnakara16 and Kashyapa17 have used the term pittamla and shuktata
respectively,as synonyms of amlapitta,though they have not directly stated so.
The terms Amalaka and Amleeka may be added as synonyms to the above for
they imply the important features of the disease.
Thus from the above,the following terms can be tsken as importsnt synonyms of
Amlapitta.They are;
* Prameelaka * Amlapitta * Pittavisuchika * Pittamla
* Shuktata * Amalaka * Amleeka
Prameelaka:
The pachyamana vidagdha annarasa immediately provokes pittadi doshas, there
by producing mukha vairasyat, hrtshula, sadana, continous lavana tiktamla, chardi,

Review of literature – Disease review
10
discolouration, emaciation, distaste, restlessness and watering of mouth. This states
where all symptoms is spoken of as Prameelaka18.In Ashtanga sangraha we find this term
mentioned under kaphaja vyadhis.
Amlapitta:
The implication of the term amlapitta signifies the abnormal state of pitta
especially in its amlaguna.
Pittavisuchika:
This may pertain to both the types of amlapitta. i.e. Urdhvagha and Adhoga
amlapitta where, their respective cardinal features are urdhvagha pravruthi(vamana) and
adhapravruthi (Atisara) of pitta associated with burning sensation.
Pittamla:
This term would imply the sense of the term amlapitta which is mentioned in
amlapitta chikitsa in Yogaratnakara.
Shuktata:
Shuktata is mentioned as synonym of amlapitta in Kashyapa samhitha
Khilasthana 16th chapter.
Amalaka:
It refers to one of the nanatmaja vyadhis of pitta mentioned in the context of pitta
nanatmaja vyadhis19
Amaleeka :
Means amlodgara21 and would refer to one of lakshana of samapitta.
As stated above these synonyms would refer to different aspects of the abnormal
states of pitta.
The similar symptom complex is considered as functional dyspepsia in modern
medicine, which will be discussed later.

Review of literature – Disease review
11
ANATO -PHYSIOLOGICAL CONSIDERATION OF ANNAVAHA SROTAS
To discreen the abnormal, it is necessary to thoroughly know the normal1. So, also
here the rachana and kriya sarira pertaining to the main site of pathology . i.e Annavaha
srotas is being elaborated .
Anatomical Considerations:
The Mahasrotas corresponding to the alimentary tract is immediately concerned
with the process of alimentation [ ingestion and egestion ]. Mahasrotas is also spoken of
as kosta. The term kosta has several Synonyms2 Viz
1. Mahasrotras [ the great channel ] 2. Shareer Madhya [ the middle part of the trunk]
3. Mahanimna [ the great cavity ]
4. Amapakwashaya [ the organs of preliminary and final aspects of digestion ]
In other sense, the ashayas contained in them, such as, nabhi , hridaya, pleeha ,
vrikka, basti, pureeshadhara, amashaya, uttaraguda, adhoguda , kshudrantra, sthoolantra3.
It would seem from the above that there is a mixup in the enumeration of the
anatomical and functional parts especially the kostangas which can be classified as
follows for proper understanding of the subject.
Anatomical division of Mahasrotas -
Amashaya [Stomach] , Kshudrantra ( small intestine,) Unduka [ ceacum],
Sthoolantra [ large intestine] , Uttaraguda [upper segment of the rectum] and Adhoguda [
lower segment of the rectum and anus].
Physiological or Functional Divisions of Mahasrotas :
Amashaya with its two parts Viz 4
1) Urdhwa amashaya : Also known as pachyamanashaya . (Stomach and small intestine
including duodenum]
2) Adho-amashaya : Pakwashaya (large intestine) and Pureeshadhara [ Rectum]
According to Sushrutha, the following constitute Kosta: Amashaya, Pakwashaya ,
Agnayashaya [Pachyamanashaya], Mutrashaya, Raktashaya, Hridaya, Unduka,

Review of literature – Disease review
12
Phuphusa5. This description would appear to be purely functional. According to this
view, functional division of Mahasrotas will be as following.
* Amashaya [ Stomach] * Pakwashaya [ large Intestine]
* Pachyamanshaya6 [Between Amashaya and Pakwashaya corresponding to
kshudrantara]
Sushrutha has very clearly stated that amshaya is the seat of kapha 7 where as
Charaka 8 and Vaghbhata have described amashaya, not only as the seat of kapha but also
that of pitta. This contention may be strong by the fact that the amlabhava9 attained by
the food, at the stage of amlabhavavastha during ahara pachana is due to an amlafactor10
or amlaguna of pitta11
[Pachaka Pitta] secreated by urdhwa amashaya.
Amashaya :
The word would literally translate as “ Receptacle of Ama “ The following points
of the Amashaya may be noted .
Amashaya is a matruja avayava 12
Its enumerrated amongst Ashayas 13, Kostanga 14
It can be subdivided into Urdhwa Amashaya and Adhoamashaya 15
It’s the seat of both Pitta and Kapha 16
It’s the moola of Annavaha srotas 17
Site :
Between Nabhi and Stana 18
Above the pittashaya 19
Its continuous with the Annanadi and Kshudrantra below 20
Related Structures :
* 2 Pesis are present in Amashaya 21 * Supplied by 2 Dhamanis 22
* Composed of Susira snayu 23 * Composed of Kala24

Review of literature – Disease review
13
AHARAPAKA - PRAKRUTA AND VAIKRUTA AVASTHAS
Amlapitta is a functional disorder caused due to qualitative and quantitative
derangement of pitta, which has a major role in the normal digestive process, giving rise
to clinical manifestation of the disease. Hence the proper knowledge of the prakruta
aharapaka becomes essential in order to understand the vikrutha avastha of aharapaka.
PRAKRUTA AHARAPAKA
The term paka means digestion. The different kinds of food ingested undergoes
digestion or paka by the influence of jataragni. The whole process of digestion/ paka and
absorption is influenced by factors like Ushma, Vayu. Kleda, Sneha, Kala and Samyoga
among which Ushma plays a major role1
1. USHMA :
The term ushma refers to agni comprehanding factors which participate in the
course of digestion and metabolism from the point of view of Ayurveda, pitta has been
described as agni [ fire] since it performs action like fire ie paka which refers to pachana
[digestion], dahana [burning] binnasanghata [splitting], tapana [heat production] ,
parinama [conversion ], paravritti [transformation], prakashana[illumination], ranjana or
varnakara[ complexion] and prakashana[ lustre] 2
Charaka has recorded marichi as having stated that
“ Agnireva shareere pittantargataha kupit a kupitaha shubhashubhani karoti”.3a
It is only agni which is located in pitta that gives rise to beneficial or adverse
consequences accordingly as it is in normal and abnormal state of functioning.
Sushruta himself has raised the question-‘is pitta same as agni or it is something other
than this factor?’3b further he has furnished the answer that it is identical to agni,in the

Review of literature – Disease review
14
view of the fact that such action as dahana (burning, oxidation, combustion),
pachana,(digedtion), etc.cannot occur in the body without pitta.This clarifies agni as
antaragni.
Clarifing the implication of the term “ Pittantargataha” used in above description
Chakrapani has observed that this term does not mean that the pitta of the body is
flamning fire and it only refers to the phenomenon of heat which is associated with fire. 4
The Medini and Amarkosha while explaining about functions of pitta have quoted
that the pitta has a direct bearing on the pakakramas to which ahara dravyas are subjected
resulting in their parinamana or transformation . The implication of these two aspects of
pitta vyapara are the digestion of food and its transformation into various functional and
structural factors of the body.
Pitta Guna and Karma :
The general physical characteristics and properties of pitta or agni availablefrom
the classics are listed in the table No. 1 [ Charaka 5 , Sushrutha
6 , Kashyapa and
Vaghbhata]
Table No. 1 Showing pitta guna
Colour Consistency Density
Naste Smell Other Properties
Suklareena Varjya
Sara, Laghu Katu, Amla Visra Satva
Pandu Vivarjita
Drava Vidagdha Amla
Vaigandhya Ushna
Ushna
Neela Peeta
Ishat or anatisneha
Tikta Putigandha Teekshna
The qualities such as sara , drava,ushna and teekshna may pertain to all the pittas or
agni’s of the body but is particular to pachakapitta. There is difference of opinion
regarding the rasa of the pitta .Charaka quotes that the prakruta rasa of pitta as katu and

Review of literature – Disease review
15
amla7, but Sushrutha quotes that the prakruta rasa of pitta as katu and it turns to amla to
when it attains vidagdhavastha8. The justification for the use of the word as an adjective
of pitta may be interpred that the pitta in its nirama avastha has got katu rasa and in sama
avastha it attains amla rasa.
2) VAYU :
Vayu is the controller of all the movemnets of the body .In the process of
digestion, prana vayu helps in deglutation , samana vayu stimulates the agni , promotes
digestion , assimilation and does sara kitta vibhaga . Any abnormality in the functioning
of the samana vayu leads to vaishamyata of agni and initiates the pathogenesis of the
diseases related to the GIT.
3) KLEDA :
Kleda means moisture . The kapha located in the amshaya is called Kledaka for
its moisturizing action. This along with the liquid part of the food breaks down the
compactness of food and disintigrates it to facilitate easy digestion. Emulsification of the
food is done by saliva and the liquid portion of the various digestive juices and hence
kledaka kapha can be said compared to the saliva and other various digestive juices.
4) SNEHA :
Sneha means unctousness and its the specific quality of kapha and pitta also. The
sneha which is consumed in the form of ahara brings softness to the food and also
enhances the functions of agni.
5) KALA :
Kala is also very important factor influancing the proper digestion . The time of
intake of food decides the digestion power i.e. pachakagni because agni is influenced by
three doshas: Kapha, pitta and vata in the early middle and late hours of the day. Kala
also cannotes the time taken for digestion on which the outcomes of the digestion
depends.

Review of literature – Disease review
16
6) SAMYOGA :
The cordination of certain factors influence the digestion. They are food,
nature of food [Prakriti] processing [Samskara], additives[Samayoga] quantity [Rashi]
consideration of the place regarding the food as well a the user [Desha] age of the
user[Ayu] ,season and the time of eating [Kala] and following the rules of eating keeping
in consideration of one’s needs etc.
AHARAPAKA :
The process of aharapaka has got two phases i.e.
1) Prathama Paka / Prapaka 2) Vipaka
The priliminary phase of digestion or the first outcome of the paka is known as
prathamapaka . This commences from the introduction of the food into the mouth
followed by the digestion of the food in the upper part of the stomach i.e. urdhwa
amashaya which is comprehended by madhurabhava. This phase can be referred to the
digestion that takes place in the buccal cavity.
Vipaka:
Vipaka has been defined as the outcome of the action of the jataragni on the ahara
dravya which is resultant of the prathamapaka , which is to be judged from the point of
view of the taste of the end product of gastro intestinal digestion Viz. Madhura [Sweet]
Amla [Sour] and Katu [Pungent].
Vipaka ocurs in 2 phases
a) Avasthapaka [ Auring digestion]
b) Nishtapaka [ At the end of the digestion ]
Avasthapaka :
Avasthapaka refers to the changes that the ahara dravya undergoes in the kosta
under the influence of Jataragni. The avasthapaka/ aharapaka in the kosta may be stated
to proceed in the following order:

Review of literature – Disease review
17
1. Madhura Avasthapaka
2 .Amla Avasthapaka
3. Katu Avasthapaka
1] Madhura Avasthapaka :
The presence of food in the mouth is followed by the perception of its taste under
the influence of bhodaka kapha9 which is seated in the root of the tongue. The concept of
bhodaka kapha parallels with the description of saliva and its function marks the
digestion that takes place in the buccal cavity . The outcome of the action of bodhaka
kapha on food; especially that fraction of its composition which essentially is madhura in
tatse seems to be continued and complete in the upper portion of urdhwa amashaya. By
now, the insoluble madhura portion of food becomes sufficiently soluble and mixed up
with the frothy kledaka kapha i.e mucin present in the urdhwa amashaya. Here with the
help of kleda ,sneha and vayu it breaks down, becomes less complex and soft and as a
result frothy and sweet ahara rasa will be produced . Since, the ahara rasa produced is of
madhura rasa and contributes to kapha, this is called madhura avasthapaka10
.
2] Amla Avasthapaka:
At this stage ahara reaches the lower part of the amashaya .Agni i.e pachakagni
which is stimulated by samana vayu acts on it and results in the vidagdhata of the ahara
rasa, the so formed ahara rasa attains amla guna and hence the name amla avasthapaka11.
The ahara is stated to undergo amlabhava, corresponding to the conversion of insoluble
proteins into soluble protein, under the influence of pepsin in the presence of
hydrochloric acid. This synchronises with the passing down of ahara rasa which has
attained amlabhava into the lower portion of mahasrotas where achha pitta is stated to be
secreated and it comes in contact with the pittasthana 12.
The final outcome of the entire gastric digestion is the acidified chime which has
been characterized by Charaka as vidagdha13, has been interpreted by Chakrapani as
pakwa-apakwa 14 or kinchit pakwa or kinchit apakwa.Even, Sushruta, in sutrasthana

Review of literature – Disease review
18
defines vidagdha as, “Vidagdha sangnyamata amlabhavam” 15. At this stage, the food
substance remains partly digested orpartly indigested.
3] Katu Avasthapaka:
The food is subjected to further digestive events which takes place in the
bhridantra or pakwashaya.This has been described by Charaka as katubhava16 or katu
avasthapaka.The materials or digested food particles passed down from amashaya having
reached the pakwashaya being dried up by agni is rendered into lumps. During this
process the ahara rasa becomes katu in nature and vayu dosha will be nourished.
The facts furnished above are fully supported by modern physiological
contribution, as regards the process of digestion according to which the starch digestion
begun in the mouth and is continued in the stomach, which is sweet . The consistency of
the food at this stage is pasty and frothy .This step can be aptly described as
madhurbhava and the place where it occur as amashaya. Further digestion of sugar is
arrested by HCL. Then commences the protein digestion under the influence of HCL and
enzyme pepsin which results in the conversion of insoluble proteins into soluble proteins.
The gastric digestion in this stage of digestion can be appropriately described as
amlabhava and the state of the digested material as pakwapakwa. As the acidified chyme,
which is passed down in small quantities to the duodenum through the pylorus comes in
contact with the mucosa of the duodenum through the common bile duct . These findings
fully confirm the Ayurvedic version of the mechanism responsible for the production of
accha pitta 17. Subsequent digestive events take place leading to the formation of chyle.
The formation of the chyle in this manner can also be aptly described as anupaka vyapara
and bhautikagni vyapara. From here the ahara rasa is stated to be absorbed through
dhamanis to be distributed throughout the body18.

Review of literature – Disease review
19
NIDANA
The term Nidana refers to the causative factors which play an important role in
the manifestation of a disease. Nidana parivarjana forms the first and foremost step in the
treatment of any disease in general and specifically in Amlapitta, it is practically
observed fact that many of the patients can be managed only by nidana parivarjana.
It is said “the character of a man’s digestive system moulds and shapes his destiny
on this planet”1. This statement holds good as the annavaha srotas and ahara have a direct
proximity. Thus a thorough knowledge of the Nidana is imperative such that preventive
measures can be adopted.
In classics a large number of nidanas have been explained in the content of
Amlapitta. Opinion of different authors are listed in Table No. basically under two
headings.
1. Ahara sambandhi 2. Vihara sambandhi.
Apart from these the other factors which can be included under the nidana of the
amlapitta can be summed up under the following headings.
1. Manasika Hetu. 2. Anya vyadhikruta 3. Oushadha / Vaidyakruta.
Aharaja nidana:
Much stress has also been laid on the benefits of following regular timings for
Aharasevana.
Adhyasana leads to Ajirna as the previously ingested meal is yet to be digested.
Visama bhojana in the form of Akala bhojana produces Ama2 while Atita kala
bhojana suppresses the Jatharagni due to prakupita vata3.
Atimatra bhojana is also Amapradosakara4.
Ahara vidhi visesa ayatana has been explained for Svasthya raksana. Vidhityakta
bhojana hence can lead to Agnidusti5.
Langhana/upavasa produces vataprakopa that in turn has a bearing on the Agni.

Review of literature – Disease review
20
Chart No. 1 Showing the Amlapitta Nidanana
AMLAPITTA NIDANA
Ahara sambandhi Vihara Sambandhi
1. Abhojana. 1. Bhukte Bhukte snana
2. Atibhojana. 2. Bhukte Bhukte avagahana
3. Ajeerna 3. Bhukte Bhukte divaswapna
4. Amepurna 3. Vegadharana.
5. Vishamashana.
6. Adhyashana.
7. Gurubhojana.
8. Gorasa Atisevana.
9. Apalkwa Atisevana.
10. Abhishyanda atisevana.
11. Phanita atisevana.
12 Pishta atisevana.
13. Ikshurvikara atisevana.
14. Prutuka atisevana.
15. Ushna atisevana.
16. Katurasa atisevana.
17. Amla atisevana.
18. Lavana atisevana.
19. Drava atisevana.
20. Kulatha atisevana.
21. Madhya atisevana.
22. Ruksha atisevana.
23. Brishtadhanya atisevara.

Review of literature – Disease review
21
Acharya Charaka has aptly stated “Aharasambhavam vastuh rogasca
aharasambhavah6”. The Guna-karma vivecana of the Ahararupi nidana are enlisted in
Table No.2 GUNA-KARMA VIVECANA7-12
Nidana Guna-karma
A. Rasatah
Amla rasa
Katu rasa
Kashaya rasa
Tikta rasa
B. Gunatah
Usna
Tiksna
Ruksa
Sheeta
Snigdha
C.Dhanya varga
Vrihi
Sastika
Yava
Mudga
Masa
Kulattha
Adhaki
Kalaya
Nispava
Koradusa
Laghu, Ushna, Pittakapharaktakrt, Kostha vidahi,
Sithilatvam janayati, Rujakara, Ksatakara,
Dagdhakara, Laghu, Ruksa, Ushna, Vatapittakrt,
Lekhana, Snehakledasosana, Sulakari
Ruksha, Sheeta, Vatapittakrt, Lekhana, Soshana
Laghu, Ruksha, Sheeta, Kledasosana, Sulakara,
Stambhakrt
Pittavardhaka, Soshaka
Pittakrt, Lekhana
Vatakrt, Sulakara, Soshaka
Vatakaphakrt, Stambhaka
Kaphakrt
Guru, Pittakrt
Sheeta
Kashaya, Sheeta, Ruksa, Vatakaphakrt
Laghu, Ruksa, Sheeta, Kashaya, Vatakaphakrt
Guru, Snigdha, Ushna, Pittakaphakrt
Ushna, Amlavipaki, Pittakaphakrt
Vatakrt
Laghu, Ruksha, Vatakrt
Ruksha, Vistambhi
Soshana, Vatakaphakrt

Review of literature – Disease review
22
Nidana Guna-karma
Masura
Triputaka
Rajika
Tila
D.Krtanna varga
Pinyaka
Palala
Pistanna
Suskanna
Krsara
E. Mamsa varga
Anupa mamsa
Varija mamsa
F. Payah varga
Payah
Dadhi
Kilata
G. Miscellaneous
Ksara
Sura vikara
Viruddha ahara
Saskuli
Iksu
Laghu, Ruksha, Sheeta, Vatakrt
Ruksha, Vatakrt
Ushna, Tikshna, Raktapittakrt
Madhura, Tikta, Kashaya, Katu, Snigdha, Ushna,
Pittakaphakrt
Ruksha, Lekhana, Visthambhi
Gurupaki, Pittakaphakrt
Guru, Ushna, Pittakaphakrt, Vidahi
Na pakam gacchati, pindikrtam, asamklinnam,
vidahamupagacchati
Guru, Pittakaphaprada
Guru, Snigdha, Picchila, Pittakaphakrt, Agnisadakrt,
Abhisyandi
Sheeta, Snigdha, Bahala, Picchila, Kaphakrt
Amlapaki, Abhisyandi, Pittakaphakrt
Guru, Kaphakrt
Laghu, Ushna, Tikshna, Kledayati adou pascat visosayati,
Dahakrt, Vidaranakrt
Amla, Ushna, Amlavipaki, Tridosakrt, Dahakrt
Amavisakrt, Grahanigadakrt, Amlapittakrt
Guru, Kaphakrt
Sheeta, Snigdha, Kaphakrt, Vidahi (if machine pressed)
Vihara sambandhi. Nidana :
Among the viharaja nidanas. The Bhukte Bhukte snana, Bhukte Bhukte avagaha
and bhukte bhukte diwaswapna will lead to agnimandya and formation of ama. Further

Review of literature – Disease review
23
indulgence in pitta prakopake ahara and vihara will lead to the manifestation of amlapitta.
Diseases of the stomach or Jathara is said to be due to vata veghedharana and hence
amlapitta also. Physical stress, fatigue and overwork are known to augment amla type of
srava – pitta srava consequent to agnidushti.13
Manasika Nidana :
More importance is being layed on the manasika karanas in the recent times.
During emotional disturbances the food consumed in the stipulated quantity remains
undigested.14 In addition to this, these nidana are also capable of aggravating the
individual dosha like vata prakaopa by chinta, shoka, trasa; pitta prakopa due to bhaya,
krodha, ershya. These mental stress and strains may augment amla type of srava leading
to agnidushti – which in turn produces amavisha or ama resulting in the manifestation of
Amlapitta. 15
Anya Vyadhikruta :
The concept of a disease begetting another disease has been explained by the
Acharyas. Karshana due to longstanding disease is said to cause vataprakopa and hence
the agnimandya. Apart from the Jawara and Atisara being a
Jathragnimandhyajanyavikara, the agni dusthti may itself produce amlapitta when an
individual indulges into pittaprakopaka ahara vihara.
Oushadha / Vaidyakruta :
Panchakarama vyapad may cause Agnimandya leading to Amlapitta. Non-
compliance with Ashtamaha do shakara bhava also causes Agnimandya.16
Though the specific nidana for Amlapitta has been mentioned in the classics, the
individual role of the nidanas are not explained in the context of Amlapitta. Hence the
nidanas can be summed up under 4 groups depending upon their mechanism of action in
the manifestation of Amlapitta.
* Agnidushtikara Nidana. * Pittaprakopaka Nidana especially Amlagunavardhaka.
* Vataprakopaka Nidana. * Kaphaprakopaka Nidana.

Review of literature – Disease review
24

Review of literature – Disease review
25
SAMPRAPTI
The concept of samprapti in Ayurveda describes the causative mode and
development of disease as well as the evolutive process of the disease .1
Decephering the samprapti is relavent to know the modality in which the nidana
has effected the body.The body is continually threatened by a variety of Nidana . The
capacity to withstand this, lies in the soundness of the dosha and the dhatu .Any
incompelence of these intrinsic factors paves way for the development of the disease .
Samprapti covers the entire visage from the Nidana to the development and progression
of the Vyadhi.
The Samprapti of Amlapitta innvolves three important factors in the manifestation
of the clinical signs and symptoms .Hence the knowledge of these factors becomes
essential as its been quoted in the classics that “ Samprapti vighatanamewa chikitsa “ i.e.
reversal of pathogenesis is the complete treatment.
The factors involved are
1) Agni 2) Ama 3) Sroto dusti
AGNI
Nearly all diseases included under kayachikitsa are engendered due to
impairement of kayagni2.Even so, is amlapitta annavaha srotodusti which latter is due to
pakavaigunya. Pitta, one of the trinity of doshas is also spoken of as agni for the reason
that this factor in the body has been stated to perform actions similar to fire3 .
As stated elsewhere agni is generally held to be responsible for the conduct of
pakadi karma Viz, sarapaka in amashaya and pakwashaya the separation of sara4 from
kitta in the pakwashaya , augmenting the action of bhutagni5, thus renedering the
digested food fit for further chemo thermal reaction described by Chakrapani as anupaka6
after which follows the reactions in dhatu paripaka.

Review of literature – Disease review
26
The two main aspects of Agni has been envisaged by all the authotities of
ayurveda
a) Kostagni [Charaka], b) Pachakagni, Jataragni [ Sushrutha], c) Pachakapitta [Vagbhata]
Dhatwagni by all the three authorities. The former is stated to be located between
amashaya and pakwashaya 7 . This aspect of pitta or agni while performing all the
digestive fuctions described in the foregoing paragraph is also stated to lend support and
augment the functions of other pittas elsewhere in the body including the dhatvagni .
The main samhita granthas have described four satges of jatargni viz, sama,
vishma , tekshana and manda 8 . The three doshas become involved due to the operation
of different etiological factors on the body leading to reciprocal influence between them.
Sama Agni :
In the well-equilibrated state of fuctioning of tridoshas, the jataragni is also stated
to function normally. This state of its function has been described as Sama Agni. In this
state jataragni ensures complete digestion of food in scheduled time without any harm to
the body9
Vishma Agni:
An erratic state of agni arises, as a result of the influence of vata in the condition
described as vishma agni . In this condition the agni varies with periods of strong appetite
alternating with loss of appetite 10.
Teekshna Agni :
The agni in this state is excited by pitta hence it is known as teekshna agni .In this
state agni digests even large quantities of food earlier to the scheduled time 11
.
Manda Agni :
This is a state in which agni is considerably inhibited due to the dominance of
kapha dosha . In this state the agni is unable to digest and metabolise even a less quantity
of otherwise easily digestable food in scheduled time 12
.

Review of literature – Disease review
27
Out of these the sama agni is considered as the samanya condition of the agni and
the rest three as the vaishamya condition.
The vaishamyata of agni leads to improper digestion due to vridhi or kshaya of
agni in their guna, praman and karma . In mandagni the food will be apakwa .In case of
teekshnagni it will be dagdhapaka and pakwapakwa in case of vishamagni .All these lead
to specific type of ajeerna leading to formation of Ama, one of the important cause for
the further vitiation of the Annavaha srotas and manifestation of the disease Amlapitta.
AMA
All the diseases, studied under the heading of Kayachikitsa are stated to have
their origin in amadosha. Amadosha or amavisha, both as acute and subacute or chronic
conditions appear to be related to the gastro-intestinal as well as metabolic disturbances
developed due to the impairement of agni which is sited in amashaya i.e.antaragni or
better still agnidushti.Ama has been defined as a condition in which the first dhatu
namely, rasa dhatu is not properly formed due to the lowered strength of Ushma(agni) 13
and in this state the food ingested becomes dushta. According to Vagabhata the impaired
vatadi doshas become mixed up with one another leading to the formation of amadhosha
very much like the production of visha from the spoiled kodrava14.
The general outlook of the two descriptions of ama would appear to be that in
absence of or due to the inhibition of kayagni the ingested food is not properly
digested.Products that arise out of such an impaired digestion is retained in the amashaya
and they undergo such changes to yield toxic substances-‘Visha roopataam yati’ which
are known as amarasa .
The etiological factors of amadosha as described by Charaka and Sushruta15
range
from dietetic indiscretions including errors of nutrition to emotional tensions of different
kinds.

Review of literature – Disease review
28
Ama Lakshanas:
The indulgence of the above mentioned etiological factors may lead to the
formation of ama in the amashaya which travels throughout the body and produces
symptoms like:
1.Srotorodha 2.Bala bramsha 3.Gourava 4.Anilamoodata 5.Alasya
6.Apakti 7.Nishteeva 8.Malasanga 9.Aruchi 10.Klama16
The ama wich is situated in amashaya produces symptoms related to kosta or
when they are traveling throughout the body, they produce sarvadaihika laxanas. When
ama co-exists along with the vrudha dosha then this condition is known as sama or sama
dosha. So, before going to amlapitta nidana,it is very important to note the sama and
samapitta conditions.
Sama:
The term sama refers to undigested,crude,not sufficiently prepared or matured (a
morbid state of humour)17
In various refrences sama is defind as “Sahamena samaha”18
i.e. the substances associated with ama are known as sama.(As.Su by Arunadutta)
Samadosha:
The sama doshas can be defined as condition in which the doshas, dhatus and
malas get vitiated and permeated with th ama.it is the cause for all the diseases.19
Hemadri commenting on this says
“Samairdoshair dhatubir malaischa janita roga api sama uchyate”20
The ama which combines with dosha,dhatu and malas is called as sama doshas,
sama dhatus and sama malas respectively. When vata, pitta and kapha doshas mixes up
with amadosha, then it is called samavata,samapitta and samakapha respectively.
In Amlapitta the mandagni leads to the formation of amarasa which gets retained
in the amashaya and combines with the deranged pitta giving rise to clinical
manifestation of the disease . The lakshanas of samapittas are stated as;
Durgandha, harita ,Shyava , amla , sthira ,guru , amlaka, uraha kanta daha.

Review of literature – Disease review
29
SROTODUSTI
The samprapti of amlapitta is also the study of srotas and the study of same both
at the physiological and pathological levels. Pathological events are stated to have their
origin at the level of srotamsi as mentioned in the classics21. Charaka quotes that the
ahara rasa is continuosly circulated throughout the body being propelled by vyana vayu.
If ahararasa accumulates in any part of the body due to pathological involvement of the
srotases i.e. khavaigunyaath , abnormal changes are initiated .Dhoshas in such a
condition become localised and initiate the process of disease in their places i.e.
karotivikritim tatra.
The srotas involved in Amlapitta is annavaha srotas. Annavaha srotas was
discussed in connection with pitta srava in urdhwa amashaya during amlabhava or
avasthapaka , in the process of ahara pachana .It is due to this sroto vaigunya that
amlapitta is engendred. Srotovaigunya can be either functional or structural .The former
is due to aggravation of doshas and the latter due to sroto dusti.
Due to annavaha sroto dusti the prakupita pittadosha having accumulated and
expanded , spreads to amashaya to lodge there22 . Further, it gets exacerabated by vidahi
and other pittaprakopa factors impairing the agni . In this condition, food is tormented to
vidagdha to assume amlabhava. It is pointed that vidagdha annarasa which assumes
amlabhava is an abnormal state in the process of digestion and this abnormality would
appear to be due to the amlaguno udrikta pitta or excess amla type of srava. It can be
obviously inferred that, this is resulted as to the atipravruti prakara of dushti in the
sookshma srotases of annavaha srotas .
The responsible dushya i.e. rasa gets vidagdha by amla factor assuming shuktata.
This shukta rasa which retains in amashaya23 is resultant of amadosha .This may refer to
sanga type of sroto dusti .Since, one of the distinct classification of this disease viz
urdhwaga amlapitta and tikta amla vamana a symptom would speak of the direction

Review of literature – Disease review
30
against the normal physiological course. Vimarga gamana type of dusti can also be
referred in this condition.
On summing up, the following dusti prakaras of annavaha srotas would apper in
this disease
1. Atipravrutti 2. Sanga 3. Vimargagamana
Samprapti can be clearly studied under the folloing headings
1. Samanya and Vishesha samprapti 2. Samprapti ghatakani
3. Kriyakala samprapti
Samanya Samprapti :
Samanya refers to “ Similitude “ . Thus the samanya samprapti establishes a
common relationship .The samanya samprapti of a disease indicates the basic
pathogenesis uninfluenced by secondary factors and that remains the same in all the
stages of vyadhi . The samprapti of Amlapitta has been put forth in the following
manner.
Due to nidana sevana vatadi doshas become aggravated and affects the agni to
produced jataragni mandhya , which in turn leads to the vidagdhata of the consumed
ahara .This vidagdha amarasa combines with the vitiated pitta and undergoes shuktapaka
in amashaya. In this stage, if the person involves in ahithakara ahara and vihara it
becomes more vitiated due to vidagdha pitta and produces amlapitta24
.
Pitta which is already sanchita; due to its self aggravating factors further attains
vidagdhata due to virudha,dushta,amla ,vidahi and pittaprakopaka ahara and vihara and
changes into amlarasa.25
The first samprapti as told by Kashyapa stresses on all the tridoshas being
responsible for agnimandya singly or all together leading to formation of ama rasa .The
so formed amarasa gets retained in the amashaya leading to formation of annavisha
which combines with the vitiated pitta and undergoes shuktatva resulting in the
manifestation of the Amlapitta , if the person indulges himself further into ahitakara ahara
vihara.

Review of literature – Disease review
31
Madhavakara has especially emphasised on the derangement of the pitta and the
pittaprakopaka ahara - vihara in the manifestation of the Amlapitta and the conversion of
the ahara rasa into amla rasa . This clearly indicates that the composition of pitta turned
abnormal. From the above information the manifestation of the Amlapitta can be putforth
as follows;
1) Due to the pitta prakopaka nidana sevana especially amlaguna vardhaka ahara , the
amlaguna of pitta increases and its known as vidagdha pitta, which leads to
agnimandya i.e. jataragni mandyata
2) In such a condition if one indulges in vatakara or kaphakara or both vata and
kaphakara nidanas then it contributes to agnimandya.
3) Due to the vidagdha pitta and jataragnimandya the ahara rasa undergoes shuktapaka
in the amashaya.
4) Further if one indulges in more nidanakara ahara and vihara it leads to more shuktatva
leading to clinical manifestation of the disease Amlapitta.
From this it can be inferred that there is a functional derangement of pachana karma.
Samprapti of Amlapitta is stated in Fig.No.
Chart no. 3 Showing the Samprapti of Amlapitta Pittaprakopaka nidana Vata or kapha or vatakapha Prakopaka nidana with pitta Prakopaka nidana Amlaguna vriddhi in pitta Vata or kapha or vatakapha Vidagdha pitta Agnimandya
Vidagdha anna Shukta paka Amlapitta

Review of literature – Disease review
32
Implication of the term SHUKTATVA :
The term shuktatva refers to sourness. Charaka while describing the second
avasthapaka has used term amlapaka which refers to the outcome of the normal digestive
reactions that occurs in the amashaya due to pittasrava 26. It should be noted that even
though shuktapaka 27 and vidagdhapaka yields substances which are also amla has not
been mentioned in the context of normal gastric digestion. From this it can be inferred
that the latter term relates to the outcome of abnormal digestive reactions which yield
pittasrava having excess amlarasa or guna..
Amadosha in which the food attains shuktatva obviously relates to the
fermentation brought about by various factors which latter have become active due to
pavakavaigunya [impairment of agni ]. This is annavisha. This may abnormally increase
the amlaguna of pitta resulting in amlapitta.
Kashyapa28 illustrates the same with an analogy viz as the formed curd turns sour
assuming inspissated form on adding kshera, so also the rasadhatu responsible dushy in
this condition assumes vidagdha attaining shuktatva by excess of amlatype of srava, due
to over indulgence in aggravating factor.This augments the amlagunoudriktam pittam i.e.
Amlapitta.
VISHESHA SAMPRAPTI
The vishista samprapti indicates the various transformations and intricacies in the
doshic involvement. Its studied under five headings
* Sankhya Samprapti * Vidhi Samprapti
* Vikalpa Samprapti * Pradhanya Samprapti
* Bala -kala Samprapti
Some of these like Pradhanya, vikalpa samprapti are subject to alterations during
the course of the disease and from individual to individual.

Review of literature – Disease review
33
Sankhya Samprapti:
As the name indicates , the enumeration of the disease is done under this heading
On the basis of pravruti 2 types 29
On the basis of Doshas 3 types30
4 types31
On the basis of sandhyasadhyuta 2 types 32
Vidhi Samprapti :
This is final version of the sankhya samprapti
Pravruti bhedena 33 :
1) Urdhwaga amlapitta 2) Adhoga Amlapitta
Tridosha bhedena 34
1. Vatika 2. Pitta 3. Kaphaja
1. Vata Kaphaja 2. Sleshma Pittaja
3. Sanila 4. Kaphanugata
Sadhyasadhayata 35 :
Sadhya Naveena ; Proper pathya sevana in purana
Asadhya Purana
Bala and Kala Samprapti :
The occurance and/or intensity of the symptoms are subject to the influence of the
secondary factors that can mould it.
Diuranal Variations :
As it is a pittapradhana vyadhi , occurrence or the intensity of the symptoms is
mainly seen in madhyadina and madhyaratri.
Variation in accordance with Aharakala :
Pitta is predominant in the amlavasthapaka of the ahara and as such, the
symptoms occur in the jiryamana avastha of Ahara

Review of literature – Disease review
34
SAMPRAPTI GHATAKANI
Dosa : Pitta - Pachakapitta [ Pradhana ]
Vata : Samana Vayu
Kapha : Kledaka Kapha
Dusya : Rasa
Agni : Jataragni
Ama : Jataragni Janya ama
Srotas : Annavaha, Rasavaha
Srotodusti Prakara : Sanga, Vimargagamana , Atipravruti
Udbhavasthana : Amashaya
Adhistana : Amashaya.
Sancharasthana : Annavaha Srotas
Vyaktasthana : Amashya
Rogamarga : Abhyantara
SAMPRAPTI ACCORDING TO KRIYAKALA
The concept of Kriyakala describes the mode and satges of development of
disease. Significance of kriyakala lies in timely intervention to arrest the disease process.
The recognition with respect to kriyakala becomes easier in cases of diseases pertaining
to Annavaha srotas , as the lasksanas are very evident.
The various stages and changes involved in Amlapitta. From the inception to
manifestation represents an evolution process. The evolutive process of the disease is
based on the description of dosha kriya kalas furnished by sushrutha.
I) Sanchaya : [ The stage of accumulation]
The term sanchaya means accumulation of dosas in its own place. The initial
insult to the body by the nidana results in accumulation of the dosas in their own sites.
According to Madhava , pitta dosha is main causative factor , where as according
to Kashyapa, the vata and kapha doshas are also associated factors in Amlapitta .

Review of literature – Disease review
35
Sanchaya of doshas can either occur individually, in pairs or all together . This
stage is characterized by vague and ill-defined symptomatology . The lakshana if
identifiable would be ‘stabdhapurna koshtata’ in vata sanchaya , ‘mandoshmata’ in
pittasanchaya and ‘angagourava’ and ‘alasya’ in kaphasanchaya. 36
An overall feature of this stage is stated to be an aversion towards similar nidana
and attraction towards contraries. 37
The symptoms of agnidusti may also be evident.
II) Prakopa [ The stage of Provocation ] :-
“ Kopasthu Unmargagamita “ 38 Further, indulgence in nidana leads to further
vitiation of the dosha. Its stated to be the condition in which the doshas having previously
accumulated and stagnated in its own sites, become swollen or excited.
This may occur under two circumstances such as :
* Chaya purvaka prakopa * Achaya purvaka prakopa
Chaya purvaka prakopa is a condition which suceeds the previous stage of
sanchaya due to continued inception of the dosha vardhaka ahara and vihara.
As Amlapitta is pitta predominant disease the paittika lakshanas become
pronounced due to pitta provocating factors in particular. In the case of agnidusti, the
apakwa ahara rasa may start to undergo vidagdhata and shuktata. Achaya purvaka
prakopavastha without the previous accumulation of doshas/ sanchaya, where in it is
referred to as Unabhava39. This is in subject to the strength of the nidana , specially in
manasika karanas and aganthuja karanas this kind of prakopa can be observed.
III) Prasara : [ The stage of pervation of vitiation process]
The vitiated doshas unable to contain themselves in svasthana spill out into other
sthanas too. In addition the combining of doshas with each other , thus potentiating the
samprapti is the main feature of this avastha. In Amlapitta the prakupita pitta dosha
remains quiescent , retaining as it40 was in amashaya and exacerbate to cause vidagdha,
due to vidahi and pitta provoking factors. In addition, the ama/ shuktarasa produced in the
earlier avastha mingles with dosha producing sama dosha . The prasara is mediated via

Review of literature – Disease review
36
rasarakta dhatu by vyana vayu . The laxanas of pitta are predominant as its pradhana in
amlapitta.
IV) Sthanasamsraya : [ The stage of location]
The dosa dushya sammurchana is an integral part of the disease and occurs in this
avastha. This stage obviously represents the prodromal phase or purvarupa. The site of
sthanasamshraya may have a pre-existing khavaigunyata or it may occur simultaneously.
In Amlapiita, the sthanasamshraya is in the annavaha srotas, amashaya in particular . The
prakupita pitta gets lodged in the amashya and marks the beginning of disturbance there.
The vidagdha ahara rasa attains amlabhava/shuktatva and mixes with the vitiated pitta
and vitiates the rasavaha srotas, leading to dosha dushya sammurchana. Purvarupaof
Amlapitta has not been described.
V) Vyakta : [The stage of manifestation]
Vyakta is the stage of manifestation of actual disease condition, which is the
result of dosha dushya sammurchana. In this stage, Amlapitta gets fully manifested and
differentiated in doshic varieties depending upon the predominant dosha. The clinical
signs and symptoms become evident.
VI) Bheda :
Depending on the extrinsic and intrinsic nidana the disease process is modified to
exhibit the lakshanas based on the dominant dosha. The disease worsens and upadrava
may manifest in this avastha. Upekshana of this avastha leads to upadravas such as jwara,
atisara, parinamashoola and annadravashoola.
A vicious cycle is formed in Amlapitta which is represented by the schematic
diagram in the Fig.No. The pachakapitta gets vrudh due to pittaprakopaka nidanas in its
amlaguna and dravatwa leading to agnimandya, which in turn leads to avipaka. The
apakwa ahara rasa undergoes vidagdhata giving rise to ama which leads to rasa dusti. The
rasa dusti inturn causes agnimandya and the cycle continues as long as one indulges in
the nidanakara bhavas.

Review of literature – Disease review
37
Chart no. 4 Samprapti on basis of Kriyakala Nidana
Amaraja Viharaja Manasika Agantuka
Sanchaya and Prakopa Agnidusti
Pitta sanchaya Ajirna apachana Amotpatti Prakopa Suktatwa
Prasara
Sthana Shuktamlata Vidagdhajirna Sanchaya
Vyakta Pitta amavisha Sammurchana
Amlapitta
Bheda
Urdhwaga Adhoga
Sitapitta Upadrava Udarda Kotha Annadrava shoola Parinama shoola Chart no. 5 Vicious circle formed in Amlapitta Pachaka pitta Ati Amlata Ati Dravata Rasa Avipaka Ama Vidagdhata
Hetu
Agnimandya

Review of literature – Disease review
38
POORVA RUPA
Poorvarupa are the promonitary symptoms, which appears before the
manifestation of the main symptoms of the disease. The purvarupas are those that preceed
the actual manifestation of the disease1. The vitiated doshas at the stage of
sthanasamshraya will manifest the signs and symptoms of forthcoming disease2. They are
the indications of the impending disease 3.
According to Madhavkara they are of two kinds4.
1. Samanya: [General] 2. Vishista [Specific]
Samanya purvarupas are the ones, which indicate the disease to some extent
without giving any indication of the dosha derangement.
Vishista purvarupas are the ones which give an idea of the doshas also in addition
to idea of the disease.
Samanya purvarapas generally disappear before the onset of the disease whereas
vishista purvarupas are likely to continue after the actual manifestation of the disease.
According to Chakrapani purvarupas are of two kinds5.
Vyakta laxanas – manifested or visible
Avyakta laxanas – Unmanifested or invisible
In Amlapitta, purvarupas are not evident as they probably belong to the latter
category. Even if they are present it is not possible to recognize them, as minor function
of doshas are common events. Hence no purvarupas have been mentioned for amlapitta in
the classics.
In Amlapitta samprapti, the agnimandya and pittavriddhi are the important
factors; hence the laxanas due to these may manifest in milder forms or show variations
in accordance with the doshic variations. Aruchi , avipaka , chardi, utklesha and hrillasa
are produced due to agnimandya[ama] and karadaha, charanadaha, angadaha, ushanata
etc. denote the sarvadhaihika pitta prakopa.

Review of literature – Disease review
39
RUPA
The rupas are the charecteristic manifestation of the clinical features which
appears during the cause of the disease 1. Its defined as the clear manifestation of the
prodromal symptoms itself is called as rupa 2. The word rupa indicates the signs and
symptoms by which a disease is identified 3
The clinical features or rupa of the Amlapitta can be described under following
headings.
* Pratyatma lakshanas * Samanya lakshanas
Lakshanas due to the pravritti of doshas
* Urdhwaga Amlapitta * Adhoga Amlapitta
* Vishista Lakshanas
Specific lakshanas due to doshas involved
Pratyatma lakshanas :
The word atma lakshana denotes the cardinal features of the disease. From the
name itself it is evident that Amlapitta is a pitta predominant disease caused due to the
vitiation of pitta. Shuktapaka is a peculiar stage of samprapti. Hence, the lakshanas
produced by shuktapaka mainly amloudgara, haritdaha, kukshidaha, and kantadaha are
taken as pratyatma lakshanas of Amlapitta.
Samanya Lakshanas:
The lakshanas caused due to the other factors involved in samprapti ghatakas is
known as samnya lakshanas .
In Amlapitta the symptoms caused due to agnimandya[formation of ama]
sarvadaihika pitta prakopa and rasa kshaya as a result of shuktapaka are considered as
samanya lakshanas.

Review of literature – Disease review
40
The lakshanas caused are as follows
Agnimandya [Ama formation] - Avipaka. Aruchi, Chardi, Utkesha, Hrillasa, Gourava etc
Rasakshaya - Klama, brahma
Sarvadaihika pitta prakopa - Karadaha, Charanadaha,Angadaha,Ushnata etc.
The Schematic diagram showing the manifestation of the symptoms is presented in fig.
Chart no. 6 Showing the manifestation of symptoms Pittaprakopaka nidana sevana Vata or kapha or vatakapha Prakopaka nidana + pitta Prakopaka nidana sevana Lakshanas Lakshanas Karadaha Aruchi Charanadaha Avipaka Angadaha etc. Chardi Utklesha Hrillasa Rasakshaya lakshanas Lakshanas Klama, Bhrama etc. Amloudgara, hritdaha Kukshidaha, kantadaha.
Pitta vriddhi Agnimandya
Shuktapaka

Review of literature – Disease review
41
The samanya lakshanas of the Amlapitta mentioned by different authors are listed in
Table No.3. Showing the lakshanas of amlapitta mentioned by different authors
Sl.No Lakshanas Ka M.K B.M Y.R V.S
1. Amlodgara (Acid eructation) - + + + +
2. Tiktodgara (Bitter eructation) - + + + +
3. Kantavidaha
(Burning sensation in throat)
+ + + + +
4. Urovidaha (Chest burn) + - - - -
5. Kukshidaha (Abdominal burning) - + + + +
6. Utklesha (Nausea) - + + + +
7. Amloutklesha
(Nausea with the sour taste)
+ - - - -
8. Avipaka (Indigestion) - + + + +
9. Hritdaha (Heart burn) - + + + +
10. Gurukoshtata + - - - -
11. Udaradhmana + - - - -
12. Antrakujana
(Gurgling sound in the intestine)
+ - - - -
13. Vitbheda(Loose bowels) + - - - -
14. Aruchi (Anorexia) + - - - -
15. Klama (Fatigue without exertion) - + + + +
16. Gourava (Heaviness) - + + + +
17. Angasada (Bodyache) + - - - -
18. Romaharsha + - - - -
19. Shiroruja (Headache) + - - - +
According to madhavakara, amlapitta has been classified under two headings viz
Urdhwaga Amlapitta and Adhoga Amlapitta 5

Review of literature – Disease review
42
This is mainly based on the location of doshas and their subsequent urdhvaga and
adhoga pravritti. These lakshanas may be seen along with the samanya lakshanas of
Amlapitta.
The term ‘kadachith’ used by Madhavakara while envisaging lakshanas of these
two distinct varities as interpreted by Srikantadutta as “ Nasarva Kalam” 6 can be taken
as ; that all lakshanas of these varities not necessarily be present always or they will be
exhibited rarely or occasionally as the case may be.
Urdhwaga Amlapitta:
In this type the dosas tend to have urdhwagati hence features like hritkantadaha,
kukshidaha, utklesha, chardi are predominant. These features of urdvaga Amlapitta
mentioned by different authores are listed in Table No
Table No.4 Lakshanas of Urdhvaga amlapitta
Sl.No. Lakshanas Y.R7 B.M8 V.S9 M.K 1. Vantam haritam + + + + 2. Vantam peetma + + + + 3. Vantam Neelam + + + + 4. Vantam Krishnam + + + + 5. Vantam Arunam + + + + 6. Vantam Raktam + + + + 7. Vantam ateevamlam + + + + 8. Vantam mamasodakabham + + + + 9. Vantam Atipichilam + + + + 10. Vantam + + + + 11. Shleshmanugatam + + + + 12. Vantam rasena vividham + + + + 13. Vantam bhukte vidagdhe Tiktavami + + + + 14. Vantam bhukte vidagdhe amlavami + + + + 15. Vantam abhukte tiktavami + + + + 16. Vantam abhukte amlavami + + + + 17. Tiktoudgara + + + +

Review of literature – Disease review
43
18. Amloudgara + + + + 19. Hritdaha + + + + 20. Kantadaha + + + + 21. Kukshidaha + + + + 22. Karadaha + + + + 23. Charanadaha + + + + 24. Ushnata + + + + 25. Aruchi + + + + 26. Jwara + + + + 27. Kandu + + + + 28. Mandala + + + + 29. Pidaka + + + +
Adhoga Amlapitta :
In this type the doshas tend to have Adhpravrtti and the features related to that are
predominant the features of Adhoga Amlapitta mentioned by different authors are
Trishna, Daha, Murcha, Bhrama, Moha, Hrillasa, Kotha, Analasada, Harsha, Sweda and
Angapeetata
Sanila amlapitta:
The aggravated pitta and vata which are situated in amashaya leads to abnormal digestion
i.e. agnimandya which results in shuktapaka. In this condition along with earlier
mentioned factors,vata contributes for the manifeststion of symptoms.
Vaikrita pitta + Vaikrita vata ------------------------ agnimandya
(samanavata) (Abnormal digestion)
shuktapaka Sanila amlapitta lakshanas.

Review of literature – Disease review
44
The symptoms of this type of amlapitta mentioned by Kashyapa10 and Madhavakara are
listed in the table no.
Table No.5 Showing the lakshanas of Sanila Amlapitta
Sl. No.
Lakshanas Ka M.K. B.M. Y.R. V.S.
1 Tamodarshana - + + + +
2 Sheeta + + + + +
3 Gatravasada + + + + +
4 Murcha - + + + +
5 Kampa - + + + +
6 Chimichimitva - + + + +
7 Pralapa - + + + +
8 Vibhrama - + + + +
9 Vimoha - + + + +
10 Harsha - + + + +
11 Jrimbha + - - - -
12 Upashaya Shigdhoupashaya + - - - -
Sakapha Amlapitta:
In this vaikrita pitta and kapha which are situated in amashaya results in
agnimandya and produces shuktapaka. In this condition along with the above said factors
kapha contributes to the manifestation of symptoms.
Vaikrita pitta + Vaikrita kapha ------------------------ agnimandya
(kledaka kapha) (Abnormal digestion)
shuktapaka Sakapha amlapitta laxanas.
The symptoms of this type of amlapitta mentioned by Kashyapa11 and Madhavakara are
listed in the table no.

Review of literature – Disease review
45
Table No. 6 Showing the lakshanas of Sakapha Amlapitta
Sl. No.
Lakshanas
Ka M.K. B.M. Y.R. V.S
1 Kaphashteevana - + + + +
2 Vamana - + + + +
3 Aruchi - + + + +
4 Sleshmaliptasya - + + + +
5 Gourava + + + + +
6 Jadata - + + + +
7 Sheetatva - + + + +
8 Balasada - + + + +
9 Angasada - + + + +
10 Kandu - + + + +
11 Nidra - + + + +
12 Chardi + + + + +
Sanilakapha Amlapitta:
In this vaikrita kapha and vata located in amashaya along with vaikrita pitta
results in agnimandya and produces shuktapaka. In this condition along with the above
said factors vata and kapha contributes to the manifestation of symptoms.
Vaikrita pitta + Vaikrita vata and kapha ---------------- agnimandya
shuktapaka Sanila kapha amlapitta laxanas.
Shleshma pittaja Amlapitta:
This variety of amlapitta is mentioned in Madhava nidana.The laxanas are
mentioned in table no. . here the dominance of pitta and kapha dosha are observed and
features are similar to urdhvaga amlapitta.12

Review of literature – Disease review
46
Table No.7 Showing the lakshanas of Shleshmapittaja Amlapitta
Sl. No.
Lakshanas
Ka M.K. B.M. Y.R. V.S
1 Shiroruk - + + + + 2 Praseka - + + + + 3 Chardi - + + + + 4 Tiktoudgara - + + + + 5 Amloudgara - + + + + 6 Katukoudgara - + + + + 7 Kantadaha - + + + + 8 Kukshidaha - + + + + 9 Aalasya - + + + + 10 Murcha - + + + + 11 Bhrama - + + + + 12 Upashya
Rukshoupashaya Ushnoupashaya
- -
+ +
+ +
+ +
+ +
Pittaja Amlapitta:
When only vaikrita pitta is sited in amashaya without vitiated kapha and vata
which produces agnimandya results in shuktsa kapha. The laxanas produced are
predominantly of pitta dosha.
Vaikrita pitta + prakrita vata and kapha ---------------- agnimandya
shuktapaka Pittaja amlapitta laxanas
The symptoms of this type of amlapitta mentioned by Kashyapa13 are listed in the table
no.
Table No.8 Showing the lakshanas of Pittaja Amlapitta
Sl. No.
Lakshanas
Ka M.K. B.M. Y.R. V.S
1 Bhrama + - - - - 2 Vidaha + - - - - 3 Upashaya
Rukshoupashaya Ushnoupashaya
+ +
- -
- -
- -
- -

Review of literature – Disease review
47
BHEDA
Many authors clearly draft regarding the classification of Amlapitta
According to Madavakara, amlapitta has been classified under two headings
based on location of doshas their subsequent urdhavaga and adhoga pravritti Viz.
* Urdhwaga Amlapitta 1 * Adhoga Amlapitta
Again from the point of view of doshas samsarga Madhavakara, Bhavamishra and
others2 amlapitta has been classified under four headings viz.
* Sanila * Sakapha * Sanilakapha * Shleshma pittaja
According to kashyapa, the classification is absed on the dosha responsible for Amlapitta,
The classification is as follows 3
* Vataja * Pittaja * Kaphaja
Chart No. 7. Classification according to different Authors
Amlapitta
1. Urdhwaga 2. Adhoga
1.Sanila 2.Sakapha 3.Sanilakapha 4.Sleshmapitta
1.Vataja 2.Pittaja 3.Kaphaja

Review of literature – Disease review
48
UPASHAYA ANUPASHAYA
Upashaya is one of the therapeutic measures adopted for confirming the
diagnosis. The medicine or food or the external therapies which gives relief is called as
upashaya and the one which worsens the condition is known as Anupashaya. Charaka
says that.
“ Ghudalingam vyadhim upshaya anupashayaabhyam pareeksheta” 1
i.e An unmanifested or obscure disease may be investigated by upashaya and
anupashaya. The Upashaya are of two types 2
Viparita [ Oppossite to hetu, Vyadhi or both]
Viparitarthakari [ similar to hetu, Vyadhi or both]
Here in Amlapitta, Kashyapa explains about upashaya of vataja, pittaja and kaphaja
varieties as fallows: 3
Vataja Amlapitta : Snigdha ahara
Pittaja Amlapitta : Swadu sheeta ahara
Kaphaja Amlapitta : Ruksha ushna ahara
The anupashayas of amlapitta are not described in the classics. But however the
causative factors themselves may be taken as anuspshayas,especially amla, katu vidahi
and other pitta provoking factors.

Review of literature – Disease review
49
VYAVACHEDAKA NIDANA
Amlapitta is a functional disorder which has to be differentiated from other
diseases having similar features. The conditions from which it has to be differentiated are
as follows;
1. Vidagdajeerna 2. Pittaja shula
3. Parinama shula. 4. Annadrava shula.
1) Vidagdajeerna :
Vidagdhajeerna is mainly caused due to pitta dosha. Bhrama, murcha , amlodgara,
sweda , daha, pittaja vividharuja are the lakshanas of vidagdajeerna among which certain
symptoms are similar to Amlapitta. The difference between these two are only in its
chronicity and its course.
2) Pittaja Shula:
Teevrashula, trishna, mutradaha, sweda, murcha, bhrama, chosha are the
symptoms which are aggravated by pittaprakopaka ahara, madhyadina, madyaratri and
ahara pachyamana kala. It is a ekdoshaja vyadhi where as amlapitta is a tridoshaja
vyadhi. The intensity of shula is very severe in pittaja shula and so varies from mild to
moderate in Amlapitta. Swadya; sheeta ahara, snigdha sheetopchara factors relieves the
pain in pittaja shula.
3) Parinama Shula :
This is shula pradhana vyadhi associated with adhmana, vibandha, atopa, trishna,
atisweda lakshanas. The shula relieves by intake of food, after the digestion and after
vamana.
4) Annadrava Shula :
In this condition shula is continuously present and relieved only after vamana
From the above all the diseases though mimic amlapitta in some of the
symptoms,they differ from the etiological point of view,samprapti and classification.

Review of literature – Disease review
50
SADHYASADHYATA
The ayurvedic manuscripts bear the descrption regarding the prgnostic states or
sadhyasadhyata of the disease. Before going to the treatment, the prognosis as to the
curability[sadhya] or incurable [asadhya] and also whether it is easily curable[ sukh-
sadhya] or curable with difficulty [ krichrasadhya] or curable as long as treatment is
given [yapya] should be estimated.
Charaka says, ” A disease in its early stage is easily curable but when advanced is
cured with quite difficulty or even becomes asadhya” 1Incurable diseases never become
curable while curable diseases may pass into stage of incurability on account of the short
comings in any of the four basic therapeutic factors or as the result of destiny.
Madhavakara 2 states that , if Amlapitta is in its early satge is curable with
efforts. If it becomes chronic it becomes yapya. In chronic cases and of persons with
recent origin indulging in apathya ahara vihara it becomes krischrasadhya[curable with
difficulty] . If amlapitta is accompanied with the upadravas[complications], then becomes
asdhya [incurable].
Kashyapa has stated that in case if the patient develops upadravas along with
dhatukshaya then it becomes asadhya[incurable] 3
Hence the early diagnosis and prompt treatment of nava ao taruna amlapitta would not
procreed to obtain chronicity and produce complications.

Review of literature – Disease review
51
UPADRAVA
The occurance of another disease in the wake of primary disease, as a
complication or sequele is termed as upadrava1 and is meant as rogauttarakalaja,
rogashraya and roghaeva. The upadhrava of the disease corresponds to the intensity of
severity or chronicity of the disease.
Kashyapa in khilasthana2 describes upadravas of amlapitta as follows:
Jwara
Atisara
Pandutva
Shula
Shotha
Aruchi
Bhrama
According to Gananath Sen
Sheetapitta
Udarda
Kandu
Kotha
Mandala
Vicharchika
Visphota
Pidaka
Amashaya Kshata
Grahani Kshata

Review of literature – Disease review
52
CHIKITSA
The basic principle of treatment of any disease is nidana parivarjana1 and
samprapti vighatana2. Nidana parivarjana has a vital role in management of any disease
and is very important in case of amlapitta, which is explained in the context of
pathyapathya.
Different measuers have been explained by many authores of our classics for the
purpose of Samprapti vighatana. Kashayapa, Bhavamishra and yogaratnakara have
mentioned the line of treatment of Amlapitta as vamana,virechana and shamana theropy3.
In Bhaishajya ratnavali and Chakradutta there is a mention of vamana, virechana,
anuvasana basti and asthapana basti in the context of treatment of Amlapitta 4. Other than
this Rakthamokshana is mentioned by Vangasena and Yogartnakara5. The individual role
of these measures in the management of amlapitta is described below.
Vamana and Virechana :
The main objective of treatment in amashayotha vikaras including amlapitta is to
expell the doshas from nearest route. i.e. by vamana and virechana, if there is
bahudoshavastha and the patient is fit for these procedures. The general principle is to do
vamana, if the doshas are sited in urdhwa amashaya, and to do virechana if the doshas are
sited in adho amashaya. Probably in this aspect Bhavamishra has advised vamana in
urdhwaga amlapitta and virechana in adhoga amlapitta6. Rest of the authors have advised
vamana followed by virechana 7 . This seema to be ideal as Indu opines that vamana is a
must before virechana, because if virechana is performed without vaman it may come out
through the mouth after mixing with shleshma and proper virechana does not takes place.

Review of literature – Disease review
53
Even if it takes place the sleshma does achachdana of grahani and produces angagourava
and pravahika. 8
Virechana is needed in Amlapitta as the main dosha involved in Amlapitta is pitta
and virechana is the ideal treatment for elimination of pitta 9 and it also expells the
shesha doshas, that remains in amashaya after the vamana therapy . The vamana and
virechana yogas mentioned in the context of amlapitta chikitsa are listed below.
Vaman Yogas:
1. A decoction prepared out of the leaves of patola vasa nimbatwak mixed with
madanaphala, saindhava lavana and honey is advocated 10
2. Another decoction prepared out of above-mentioned drugs except vasa 11
3. Lavana jala, warm milk , ikshu rasa, water prepared with honey or tiktha dravyas are
beneficial for the purpose12
4. Kashayapa gives gritha prepration for the same purpose. The following dravayas viz
patola patra, triphalatwak measuring ardhaphala, trayamana, rohini, nimba, yasti
measuring karshamatra, masoora measuring phaladwayam has to be mixed well
together in a morter. These should be boiled in post with one adaka water to reduce it
to one eighth [1/8 part]. Then this is mixed with one khudava quantity of gritha and
boiled again to reduce it to half prastha; this residual quantity measuring half prastha
should be administered which should be neither too hot nor too cold. This produces
vamana quietly and abolishes amlapitta of long duration 13.
Virechana Yogas :

Review of literature – Disease review
54
1. Decoction prepared out of triphala kwath mixed with trivrit churna and honey is
advocated.14
2. A decoction prepared out of triphala, trayamana, katuka rohini, trivrit, measuring
ardhaphala and trivrit half the quantity of all. This is advocated for virechana karma15
Vamana & Virechana karma in amlapitta chikitsa mentioned by different authors
are listed below.
Table No 9 Showing the referance of vamana and Virechana Karma in Amlapitta
Authors Vamana Virechana
Kashyapa Samhitha + +
Yogaratnakara + +
Bhaishajya Ratnavali + +
Chakradutta + +
Bhavaprakasha + +
Basavarajeeyam + +
Basti:
After the above measures bastikarma has to be done to cleanse the residual
morbid matters. The necessity of basti does not usually arise unless vata is predominent.
Anurvasana basti is the usual procedure followed before going for asthapana basti16The
asthapana basti has proven benefit in Amlapitta which has attained chronicity and also in
vata predominent amlapitta.
Raktamokshana:
The necessity of raktamokshana arises when the doshas do not subside by other
measures. Vangasena & Yogartnakara observes this as a last measure restored to cleanse
the unabated dosha by other measures. This is beneficial in Amlapitta associated with
kota etc. synchronizing with raktadusti.17

Review of literature – Disease review
55
SHAMANA
Shamana is defined as which does not results into elimination of doshas neither
does it vitiates nor disturbs the normal balance of dhosas but results in correction of the
imbalanced doshas i.e. it bring them to normal state.
Generally the medicines used for the pittaja disorder consists of tikta, madhura,
kashaya rasa, sheekta veerya and madhuravipaka dravyas.
In Amlapitta the pitta is in the state of samavastha. Here ama co-exists along with
vridhpitta.Hence, the dravyas which have both the properties of ama pachana and pitta
shaman should be used. Therefore tikta rasa pradhana dravyas are indicated.
In Sushrutha samhita while dealing with the pittatisara Dalhana expresses his
doubt that how can tikta rasa dravyas be used as pachanas. Then the clarsifies that, even
in jwaratisara, tikta pachanas have been indicated. In jwara samanya chikitsa, langhana,
swedana tikta rasa pradhana yavagus are used for the purpose of pachana karma in the
condition of apkawa doshas in taruna jwara.
Above mentioned both refernaces show that tiktarasa is more useful in sama.
Which also applies for samapitta condition because in Charaka samhita, while dealing
with the treatment of raktarasha he has told that tikta rasa is usefull in improving the
agni[Deepnartha] and pachana of doshas [doshanam panchanatham] and in Ashtanga
hridaya, arsha chikitsa he has given a similar opinion.19
All these refrences suggests that tikta rasa drugs should be used in samapitta
conditions and hence in amlapitta too.
Even for the purpose of deepana and pachana which has to be performed prior to
vamana, only tikta rasa pradhana dravyas have to be used and even for vamana virechana
tiktarasa pradhana yogas have been mentioned.
Mainly tikta rasa , laghu ,snigdha guna, katu or madhura vipaka , seta veerya
drugs have been mentioned by the acharyas.
The yogas mentioned by acharyas for the shamana of the Amlapitta are as
follows:

Review of literature – Disease review
56
SINGLE DRUGS20
Herbal Drugs:
Patola Patra, Nimba, Bhunimba, Amalaki, Guduchi, Yastimadhu, Dhanyak,
Narikela, Haritaki, Vasa, Parpataka, Shunti, Katuki, Shatavari
Jangama Drugs:
Shankha, Mukta, Cow’s Ghee, Cow’s Milk
Parthiva Drugs :
Abhraka, Gairika, Tamra, Louha, Mandura, Rajata
Compound drug Preprations :
Kwatha:
Bhunimbadi, Guduchyadi, Patoladi, Vasadidashanga, Phalatrikadi, Dashanga,
Shringbera
Churna:
Panchanimbadi, Avipattikara, Trikatukadi, Eladi Choorna
Vati / Gutika :
Panchanana Gutika, Phaniyabhakta Gutika, Shankhavati, Drakshadi Gutika,
Kshudavati
Khanda/ Modaka:
Kushmanda Khanda, Narikela Khanda, Soubhagyashunti, Pippali Khanda,
Amlapittantak Modaka, Gudadi Modaka, Khanda Amalaki
Gritha:
Shatavari, Drakshadi, Panchatikta, Narayan, Vasa, Tiktaka
Rasaousahadis:
Amlapittanka Louha, Lilavilasa Rasa, SoothshekaraRasa, Amlapittantaka Rasa,
Dhatri louha, Pravala Pisti, Mukta Pisti

Review of literature – Disease review
57
PATHYAPATHYA
“ The doctor of the future will give no medicine but will interest their patients in
the case of the human frame in diet and in the cause and prevention of disease”
- Thomas Edison
The diet, drugs or regimen which are condusive to the body and mind do not
produce any adverse effects are considered as wholesome and the opposite ones as
unwholesome.1
Pathyapathya plays an important role in the prevention and causation of disease
respectively.Some diseases in their intial stages can just be treated by following the
pathya and even any treatment procedure followed for a particular disease is not complete
unless the patient strictly follows the diet regimen.
Pathyapathya attains more significance in the disease of the Annavaha srotas as
this is amongst the first to be affected by the aharaja nidanas. Along with this due
importance should also be paid to the viharaja and manasika nidana.
The pathya and apathya of Amlapitta as mentioned in Ayurvedic texts as follows.
Table No. 10 Showing Pathya apathya5
Sl.No. Food Stuffs Pathya Apathya
1. Cereals Rice [old], Wheat, Barley
Rice within one year of harvest
2. Pulses Green Gram Black gram, Horse gram, Red gram, Sesamum
3. Vegetables Bitter guard,Snake gourd, Carrot, Ashgourd, drumstick leaves
Potato, garlic, chilli sweat potato

Review of literature – Disease review
58
4. Seasoning Corriander, turmeric, Malabar, Tamarind
5. Fruits Gooseberry, grapes[dry], Kadali,pineapple, orange,Robexta fruit
Lemon , grapes, plantain , Sour fruits
6. Food Addatives
Sugar, Honey,Boiled & cooled water
Curd, buttermilk, goats milk, jaggery, oil, tea , coffee, alcohol, dhanyamla
7. Type of food Sweat, bitter, astringent , subsiding kapha and pitta
Sour, pungent, salty, oily Aggravating pitta dosha Incompatible, difficult to digest
8. Food Prepartaion
Mamsa rasa, lajapeya, Mastu, lassy, saktu
Pickles, fried items, baked items , pishtanna, biscuits, cake , carbonated drinks,
9. Non veg Jangala mamsa fishes
10. Activities Adequate rest, sleep and Exercise
Strenous labour, exposure to hot sun, fire, suppression of natural urges
11. Emotions Happiness, Satisfaction
Anxiety, worry , grief tension, Jealousy
12. Complaints Dadima, pippali, guduchi satwa, shatavari, kapitha, karkola
As a guideline for selection of food and method of consumption, Astavidha ahara
visesayatana and Aharavidhividhana are explained respectively.
A. Astavidha ahara visesayatana2:
1. Prakrti 2. Karana
3. Samyoga 4. Rasi
5. Kala 6. Upayoga samstha
7. Desa 8. Upayokta

Review of literature – Disease review
59
B. Ahara Vidhi Vidhana 3 :
These have been explained for the healthy and the diseased.
1. Usnamasniyat 2. Snigdhanamasniyat
3. Matravadasniyat 4. Jirne asniyat
5. Viryaviruddhamasniyat 6. Iste deshe, ista sarvopakaranam
7. Nati drutam, nati vilambitam 8. Ajalpannahasan tanmana bhunjita
9. Atmanamabhisamiksya bhunjita
The following are also to be avoided 4 :
Samasana: Combination of pathya and apathya ahara
Adhyasana: Eating repeatedly
Amatrasana: Unwholesome quantity
Visamasana: Eating prior to or after regular mealtimes
All the above factors have a bearing on the efficacy of the Jatharagni and thus on
the Aharapaacana. Hence, one should observe the above regimen at every
mealtime for the maintenance of health.

Review of literature – Disease review
60
DYSPEPSIA
Dyspepsia [Indigestion] is a collective term for any symptoms thought to original
from the upper gastrointestinal tract1.
From a clinical point of view the most common of disordered gastric emptying is
Dyspepsia. [Greek: “Dys” means bad and “peptin” means to digest]2. Understanding this
term is key to interpreting the literature in this area but, unfortunately, definations vary.
In Harrison’s medicine it is considered as a word equivalent to indigestion and
referred to a set of vague upper abdominal symptoms like heart burn, belching, epigastric
pain /discomfort, anorexia, nausea and excessive abdominal symptoms associated with
intake of foods. A clear-cut diagnosis may not be possible clinically, and investigations
may also be normal. In fact when clinical features are sharp enough for a reasonable
diagnosis the term dyspepsia is not used.3
More than half of all dyspeptic patients do not have any organic disease, however
much we investigate. These patients may have aggravation of symptoms during
emotional upset. Hence, it is called “functional dyspepsia” or nervous dyspepsia.
Dyspepsia means pain or any discomfortable symptoms associated with the
function of digestion [Thomson – 1963]. Variation of digestion produce symptoms of
many sorts, often not at all directly connected with the taking of food together with
leisurely eating of meals by those accustomed to hurry. Frequently suffices to cure
indigestion of longstanding.
Edward and Coghill [1968] have reported when no cause for the dyspepsia was
apparent the condition is described as Non-Ulcer dyspepsia [NUD]

Review of literature – Disease review
61
Causes of Dyspepsia4:
Upper GIT Disorders
Other GIT Disorders
Systemic Diseases
Drugs
Others
Functional [Non-Ulcer dyspepsia and IBS]
Peptic Ulcer. Acute Gastritis Gall stones Motility disorders
[Oesophageal spasm]
Hepatic diseases [Hepatitis, Metastases]
Pancreatic diseases [Cancer, Chronic Pancreatitis]
Colonic carcinoma.
Renal failure
Hyper-Calcaemia
NSAID’s Iron and
potassium supplements.
Corticosteroids. Digoxin
Alcohol Psychological
[e.g anxiety, depression]
Functional / Non-Ulcer Dyspepsia : 5
Frequently however a clear etiologic explanation for the patients complaint of
symptoms cannot be established and descriptive designations are applied.
a) Non-Ulcer Dyspepsia:
This is defined as chronic dyspepsia [pain/upper abdominal discomfort] with no
evidence of organic disease on investigation. i.e, Ulcer like symptoms with no
evidence of ulcer.
b) Functional dyspepsia:
When clinical evaluation fails to reveal any explanation for indigestion then its
known as functional dyspepsia. The term is interchangeable with Non-ulcer
dyspepsia. This is mainly due to some forms of stress, such as
* Nervous * Physical stress * Alimentary stress
c) Flatulent Dyspepsia:
When Belching, abdominal distension and early satiety are predominant.
d) Dysmotility like Dyspepsia:
Same as flatulent dyspepsia.

Review of literature – Disease review
62
e) Acid-Dyspepsia:
Is due to the presence of an excessive amount of hydro-chloric acid or acid salts in the
gastric juice. Commonly seen in young patients of sedentary occupation, who eat
irregularly as to time and amount of food and who are in the habit of bolting their
meals.
f) Nervous Dyspepsia :
Occurs in those who are exposed to psychological stress. The symptoms being more
or less like functional dyspepsia. The diagnosis turns on the absence of evidence of
organic disease and the elicitation of psychological factors.
g) Fermentive Dyspepsia:
Arises in connection with the dilatation of stomach due to some obstruction at its exit,
in consequence of which food is retained, ferments and distends the organ giving rise
to the symptoms.
h) Acute dyspepsia:
Sometimes occurs in people who ordinarily digest food with comfort and still more
frequently in persons of weak digestive powers.
In all these conditions there is no evidence of any sort of organic disease on
investigation and are termed as synonyms of Non-Ulcer Dyspepsia / Functional
Dyspepsia.
Non-Ulcer Dyspepsia:/Functional Dyspepsia:
Non-Ulcer dyspepsia refers to symptoms that suggest a diagnosis of peptic ulcer
despite the documented absence of an ulcer by endoscope or barium x-ray studies and
other demonstrable organic disorder [bilary tract disease] or evidence of irritable bowel
syndrome.6
The term Non-ulcer dyspepsia was coined by True Love [1972].

Review of literature – Disease review
63
Jone and Pollak [1945] have mentioned that half of all the patients with gastric
symptoms do not suffer from peptic ulcer, and in majority of these patients its impossible
to make any form of diagnosis.
Incidence:7
Usually seen in young patients [<40yrs]
Women affected twice as commonly as men.
Twice as common as peptic ulcer affecting 20%-30% of populllation.
Etiology of NUD : 8
1. Covers a spectrum of
a) Mucosal Disorders
b) Motility Disorders.
c) Psychiatric Disorders.
Etiology and Pathogeneses :
All though the precise etiology of NUD is unknown, several candidate factors are
considered here.
a. Gastric acid. b. Motility.
c. Chronic gastritis d. H-pylori Infection.
e. Psychological factors and stress. f. Diet, habits and drugs.
a) Gastric Acid
Certainly the clinical features of NUD are reminiscent of those in actual peptic
ulcer patients. Nevertheless, despite years of study, the relationship of acid to ulcer-type
pain remains unclear. On the other hand most studies indicate that acid secretion is
normal in patents was NUD9.
In general therefore, acid does not appear to play a pivotal role in the
pathogenesis of Non-Ulcer Dyspepsia.

Review of literature – Disease review
64
b) Motility
The literature on the association of Non-Ulcer Dyspepsia with gastric dysmotility
is confusing, but some studies do point to delayed emptying of liquids or solids. The
timing and variability of symptoms make this area difficult to study with current methods
between 25%-50% of patients with Non-Ulcer Dyspepsia have postprandial and antral
hypomotality. 50% experience abdominal discomfort in response to ballon distension at
volumes lower than those provoke pain in healthy controls, suggesting visceral
hypersensitivity.
c) Chronic gastritis
Chronic gastritis [Round cell infiltration of the mucosa] is a common condition
whose prevalence increases with age. It would appear, however that many patients with
this finding are asymptomatic and that symptoms cannot be correlated with the degree of
inflammation10. Relation between non-ulcer dyspepsia and deuodenitis /duodenal ulcer
has not been demonstrated11.
d) Helicobacter pylori:
H-pylori is a short spiral shaped, micro-aeroplilic gram negative bacillus which is
found primarily in the deep portions of the mucus gel layer. that coats the gastroduodenal
mucosa, but does not invade the mucosa. Role of H-pylori and associated chronic
gastritis in causing dyspeptic symptoms in persons without peptic ulcers is unknown and
there is no convincing evidence that H-pylori accounts for the symptoms in NUD11b.Role
of H-pylori eradication remains controversial.
e) Psychological factors and stress:
Stress anxiety and depression are considered as the causative factors for
functional dyspepsia 12. Stress has been known since the experiments of William to effect
gastric function and secretion.

Review of literature – Disease review
65
f) Diet :
Excessive consumption of coffee, tobacco cola, hot spicy foods, citrus, irregular
eating all favour the manifestation of the disease entity, many patent relate their
symptoms to meals in general, and fatly food in particular.13
g) Habits:
Chiefly alcohol and smoking contribute to the disease. There is less evidence to
relate it to NUD.14
h) Drugs :
Chronic usage of NSAID’s such as aspirin, ibubrufen, indomethacin, salicylates
and also steroids are found to induce Non-Ulcer-dyspepsia.15
Clinical presentation: 16
1. Abdominal pain. 2. Acid Erructations.
3. Anorexia. 4. Heartburn [pyrosis]
5. Nausea. 6. Vomiting
7. Water brash. 8. Flatulence / Bloating / Gaseousness.
9. Abdominal discomfort / Fullness. 10. Constipation /Diarrhoea.
11. Food Intolerance. 12. Early satiety.
The Non-ulcer dyspepsia usually presents with dyspeptic symptoms or ulcer like
symptoms or symptoms suggestive of IBS.
Symptoms may appear disproportionate to clinical well being. But morning
symptoms are characteristic.
Psyehological symptoms may be seen sometimes like depressive illness.

Review of literature – Disease review
66
Diagnostic Approach:17
The patients presenting with dyspepsia may have any of the conditions related to
upper gastro-intestinal tract. Hence the following approach has to adopted.
1. A detailed history and physical examination.
2. Upper G.I.T. Endoscopy. [In Elderly]
3. Barrium- Meal X-ray [In Elderly]
The distinguishing features between functional and organic /structural dyspepsia
of gastrointestinal tract are given in the table No.
Table No 11 Distinguishing between functional and organic/structural disease of
gastrointestinal tract.18
Function Organic Neoplastic Inflammatory Symptoms : Weight loss None Common Sometimes Diarrhoea Day time only
Nocturnal Day and Night
Blood loss None
Frequent Frequent
Fever None
Rate Frequent
Pain Cramping, relieved by defecation
Minor to severe May be localized, may be severe
Bowelhabit [diarrhoea/constipation]
Alternating Diarrhoea/constipation pellet like stools
Constipation (Rarely dianhoea)
Diarrhoea or Normal
Laboratory tests Hematocrit Normal Often decereased May be decreased W.B.C. count Normal Usually normal Often elevated Erythrocyte Sedimentation rate Normal Usually
increased Usually increased
Investigations :
1. Routine Urine Examination.
2. Routine Blood Examination.
3. Stool Examination.

Review of literature – Disease review
67
4. Endoscopy if necessary. [especially in pts. Of age>55 yr.]
Management and therapy: 19
Drug treatment is not especially successful, and merits trail.
1. Avoidance of factors responsible for worsening the conditions such as stress, foods
medications etc.
2. Life – style modifications
3. Assurance and counseling with patients associated with an identifiable cause of
psychological factors.
4. Antacids are sometimes helpful
5. H2 – Receptor antagonists may be helpful in night pain or heartburn
6. Prokinetic drugs such as metaclopromide may be given before meals.
Diet 20:
The diet recommended in functional dyspepsia are,
1. Avoiding foods known to excerbate symptoms.
2. Frequent small meals, low in fat.
3. Avoid tea, coffee, chocolate and carbonated drinks.
4. Avoid regular and decaffeinated coffee.
5. Avoid heavy use of alcohol.
6. Avoid smoking.
7. Avoid aspirin containg compounds and NSAID’s etc.
8. Avoid activities causing more mental and physical stress/ strain.
9. Adequate physical exercises and adoption of relaxation technique like yoga,
meditation etc.
Discussion on disease review:
Amlapitta is defined as a pitta pradhana vyadhi caused due to the quantitative and
qualitative derangement of pitta.Its the out come of digestive disturbance due to faulty
food and regimen.The pathogenesis of amlapitta clearly states it to be a functional

Review of literature – Disease review
68
disturbance rather than an organic disturbance.Amlapitta is characterized by utklesha
(nausea), amlodgara (acid erructations), hrtdaha (heart burn), kantadaha (burning
sensation in the throat), vamana (vomiting),udarashula (abdominal pain), avipaka
(indigestion), klama (fatigue), gourava (heaviness in the body), vitbheda
(constipation/loose stools), adhmana (abdominal fullness), etc.All tese signs and
symptoms are broadly termed as Indigestion or Dyspepsia in the modern medicine.As,
Amlapitta is a functional disorder we can compare it to Functional dyspepsia or Non
ulcer Dyspepsia.
An attempt is being made to draw a paralance between Amlapitta and Non ulcer
Dyspepsia.
A clear description of etiology of Non ulcer Dyspepsia has not been stated, but some
factors like; Nervous(psychological factors,viz fear, anxiety, depression etc.),
Physical stress(long hours of working,walking etc.), Alimentary stress(faulty eating
habits,spicy food,badly cooked food,drugs etc) have been said to be pre disposing
factors.These have been highlighted in Amlapitta as the nidana of the disease.
Non ulcer Dyspepsia is said to be more comman in middle age (< 40yrs.) and more
common especially in women.The same can be seen to be quoted in Ayurveda stating
it to be pitta pradhana kala in the life of an individual.
A clear pathogenesis of Non ulcer Dyspepsia is not found,but its stated to be
characterized by dyspeptic signs and symptoms with no any organic lesions anywhere
in the G.I.T. This clearly specifies it to be a functional disorder and so also in
amlapitta there is no mention of any organic lesion in the pathogenesis.

Review of literature – Disease review
69
Different descriptive terms are used for Functional dyspepsia/ Non ulcer Dyspepsia
viz Fermentive dyspepsia, Flatulent dyspepsia, Nervous dyspepsia, Acid dyspepsia,
Dysmotility like dyspepsia etc. on the basis of the predominant symptom as given by
the patient.These can be to some extent said to be due to the involvement
/predominant of a particular dosha leading to those signs and symptoms,i.e. it can be
compared to doshic varieties explained in Ayurveda.
The signs and symptoms of Non ulcer Dyspepsia more aptly ressemble to that of
amlapitta than any other disorders of the G.I.T.
As Non ulcer Dyspepsia is a fuctional disorder there are no diagnostic signs and only
history will often suggest the diagnosis.Even in amlapitta no diagnostic signs are
present ,only the signs and symptoms suggestive of the deranged pitta along with vata
and kapha are seen.
Non ulcer Dyspepsia is said to show considerable relief with proper diet and regimen
and avoidance of the causative factors. In amlapitta ,more stress has been laid on the
pathyapathya and nidana parivarjana in the management of amlapitta.Its also stated
that with proper pathya itself the Amlapitta can be managed.
Table No.12. Symptoms of Functional dyspepsia Comparison with Amlapitta
1 Kukshidaha - Epigastric pain 2 Kantadaha - Retrosternal burning 3 Hritdaha - Heartburn 4 Udgara [amla or tikta - Belching 5 Utklesha - Nausea 6 Chardi - Vomiting 7 Aruchi - Anorexia 8 Avipaka - Indigestion 9 Antrakujana - Barborygmus 10 Udaradhmana - Flatulence, Abdominal distension, bloating 11 Vidbheda - Change in bowel habits

Review of literature – Drug review
70
B. DRUG REVIEW
SHATAVARI
Botanical name : Asparagus racemosus Willd.
Famlily : Liliaceae
Classical name : Shatavari
Sanskrit name : Shatavari, Shatamuli, Shatavirya, Bahusuta, Atirasa,
Kula : Rasona Kula
Gana : Madhuraskandha. Balya. Vayasthapana1 [Charaka ]
Vidarigandhadi, Kantakapanchamoola, Pittashamana2. [Sushruta]
English name : Wild Asparagus.
Description3 :
Scandent climber, tall climbing, excessively branched, prickly under shrub. Roots
tuberous; prickles 0.6-1.5 cm, straight or recurved, cladodes 2.5 cm, curved. Terete,
spreading in tufts of 2-6, channeled beneath. Flowers in recemes. Fruit a berry, pea-like,
red when ripe; fruit containing seeds 1-2.
Drug Morphology :
The drug comprises of dried tuberous succulent roots which arise adventitiously
from the root stock. Its cylindrical in the middle, tapered towards the ends and brown in
colour. Surface of the fresh roots are easily removable and cover glistening material
inside. The drugs are entire roots or longitudinally broken pieces, surface of dried roots
exhibit deep irregular longitudinal furrows and minute transverse wrinkles due to
shrinkage during drying. The drug is hard. However, it breaks with a short fracture. The
drug has no odour and has slightly mucilaginous taste which leaves bitterish blend after
chewing for few minutes.

Review of literature – Drug review
71
Varieties :
1. Shatavari [Asparagus racemosus Willd]
2. Mahashatavari [Asparagus sarmentosa]
Pharmaco dynamics :
Rasa : Madhura, tikta.
Guna : Guru, snigdha.
Virya : Sheeta.
Doshakarma : Tridoshagna.
Chemical Composition :
• Shatavari contains large amount of saccharine matter and mucilage.
• The plant contains 4 saponins i.e shatavarin I-IV.
• Tubers contain rhamnose, glucose, sarsapogenin, sitosterol, glycosides and
carbohydrates.
• Flower contains qurcetin, rutin and hyperoside.
• Leaves contain disosgenin.
• Mature fruit contains glycosides, sitosterol, sigmasterol
In fresh tubers :
Water soluble ingredient 52.5 %
Fibre : 33.3 % Water :9 %
Water soluble ingredients contain :
Sugar : 7 % Mucilagenous principle : 6 %
Volatile Oil : 52.4 % Ash : 4 %
Karma :
Effect on Dosha : Tridoshagna, Pittashamaka.
Effect on Dhalus : Balya ; Rasayana ; Shukrajanana; Vrshya;
Stanyajanana; Garbhaposhaka; Raktaja vikaras;
Medhya; Nadibalya.

Review of literature – Drug review
72
Effect on Mala : Grahi ; Mutrala.
Effect on other organs : Shulahara; Vednaasthapana; Eye; Stomach; Gall
bladder; Liver; and cardia.
Rogagnata :
Shukrakshaya; Garbhasrava ; Chalitagarbha ; Rakta pradara ; Sveta pradara ;
Stanyakshaya ; Dourbalya ; Dhatukshaya ; Mutrakrucchra ; Kshayaroga ; Drishtimandya
Amlapitta ; Sula , Arsha ; Vatavyadhi ; Siroroga ; Apasmara ; Moorcha ; Grahani.
Therapeutic Uses :
The drug shatavari is alternative, anti-diarrhoeal anit-dysentric; anti-spasmodic;
aphrodisiac; astringent; cardiac tonic; carminative; demulcent; diuretic; glactagogue;
nervine tonic; nutritive; ophthalmic; strengthening and tonic.
It is also used in blood diseases, pulmonary complaints, rheumatism; scanty urine
and seminal weakness. The roots are also utilized for medicated oils, used for nervous
and rheumatic disorders.
It is much used in kshaya, atisara, rakta and amatisara, apasmara [epilepsy],
haemophilic disorders and shotha.
The roots of drug are exploited for use in several preprations belonging to group
of classical formulations; Viz: Eladya modakam. Guduchyadi modakam; Trayodashanga
guggulu; Shatavari guda; Shatavaryadi gritha; Shatmulyadi louha; Shatavari manduram;
Shatavari pakam; Shatavari panaka; Phala gritha; Anu taila ; Narayan taila etc.
Medicinal preprations are incorporated in content of the management of different
diseases.
Parts used : Tubers.
Dose :
Juice 10-20 ml.
Decoction 50-100 ml.
Powder 3-6 gms.

Review of literature – Drug review
73
ABHRAKA BHASMA
ABHRAKA
Abhraka is one among Maharasa and the first one in the series. It’s a double
silicate of Magnesium and Aluminium with sodium or potassium. There are different
kinds of mica and they vary from the chemical stand point. The micas are silicates of
varying composition of Aluminum and Potassium, containing hydroxil, magnesium, iron,
sodium, lithium, fluorine. The silica content varies between 33-55 %
Types4 :
Based on colour Abhraka is of four types.
1. Shwetha. 2. Peetha.
3. Raktha. 4. Krushna.
Krshna Abhraka is said to posses roganashaka property. And among the krushna
veriety vajra abhraka is said to be shreshta5 as it allievates the diseases and has got
rasayana property.
In this study the vajra abhraka of krushna variety is used for the prepration of
abhraka bhasma.
Shodhana6:
The shodhana of Abhraka was made by heating it and dipping in Triphala kashaya
for 7 times and Dhanyabhraka was prepared as per the procedure told in Rasa Ratna
sammuchaya.
Marana :
Around 64 maraka ganas have been explained in the text.
For this study, the Abhraka Bhasma is prepared by triturating it with Kasamarda
swarasa7 and subjected to puta for 30 times. The bhasma becomes nischandra within 10
putas, but to increase its therapeutic value 30 putas were given.

Review of literature – Drug review
74
Properties :
Colour : Brick Red Colour.
Guna : Laghu, snigdha.
Rasa : Madhura Kashaya.
Vipaka : Madhura.
Veerya : Sheeta.
Doshagnatha : Tridoshagna .
Karma :
Balya, Rasayana, Medhya, Deepana, Pachana, Anulomana, Sthanya vardhaka,
Jwaragna,.Shonitha sthapana. Dhatuvardhaka., Yogavahi.
Indications :
Kasa, Shwasa, Pandu, Kshaya, Parinamashoola, Amlapitta, Grahani, Arsha,
Bhrama, Sheetapitta, Prameha, Mutrakruchra, Agnimandya, Hrudroga, Vatavyadhi.
Anupana :
Anupana for some of the diseases have been mentioned in the texts. Depending
upon the disease appropriate anupana should be selected.
Chemical Composition :
Analytical report of Abhraka Bhasma.
Silica [SiO2] - 36.01 % Allumina [Al2O3] - 27.57%
Ferric Oxide [Fe2O3] - 12.78% Potash [K2O] - 13.17 %
Lime [CaO] - 5.03 % Soda [Na2O] - 3.06 %
Magnesia [MgO] - 1.92 % Chloride. - 0.09 %
Phosphate. - Faint trace Moisture - 0.37 %

Review of literature – Drug review
75
GRITHA
Gritha is not only included in the Gorasavarga, but it is also used as the best
remedy for pitta disorders and vata pitta disorder8. Gritha is best among all sneha
dravyas9 used internally. It is the sneha par-excellence because of its remarkable property
to assimilate the properties of other substances when added to it. With its own qualities
intact, it has the capacity to transform itself, so as to imbibe the qualities of the
substances added to it.
Though gritha has properties contrary to those of pitta, yet it is agnideepana.
Increase intellect, memory, strengthens eyesight and increases shukra dhatu10.
Gritha because of its sheha quality alleviates the vata and due to its sheeta veerya
alleviates pitta, even though kapha possesses qualities homologous to ghee, the latter
when mixed up with drugs possessing opposite qualities alleviates the former.
Gritha has different actions when licked and when swallowed. For e.g when
licked its pittashamaka. Whereas when swallowed it pacifies vata.
Cows gritha is considered as the best one11.
Meeting point 33-37° C.
Contains more of oxygen than any other oils.
Varga : Gorasa, Ghrita, Ksheera, Suvarnadi.
Rasa : Madhura 12
Vipaka : Madhura13
Guna : Snigdha, Guru
Veerya : Sheeta14
Doshagnata : Pittahara
Vata pitta hara.

Review of literature – Drug review
76
Karma :
Medhya, Deepaneeya, Snehana, Anulomana, Hrudya, Vrushya, Garbhasthapana,
Jwaragana, Daha prashamana, Balya, Bruhana, Rasayana, Chakshushya, Varnya,
Vayasthapana.
Rogagnata :
Karshya; Daurbalya, Udavarta, Gulma, Kasa, Raktapitta, Jeernajwara, Anaha,
Shula.
Problable mode of action of the Trial drug :
Amlapitta is a pitta pradhana vyadhyi caused due to agnimandya. The three
important factors leading to the pathogenesis of the disease are agnimandya, ama and
srotodushti. Pitta is the pradhana dosha which singly or along with samana vayu and
kledaka kapha causes agnimandya, which leads to the formation of ama which combines
with the vrudh pitta (due to its own causes) leading to amavisha which turns to suktatva.
This further vitiates the pitta leading to Amlapitta.
To overcome this condition, the medication used should be such that it increases
the agni, reduces the ama and pacifies the pitta. Along with these, the drug should be able
to correct the vitiated dosha involved. i.e. vata and kapha. So the selection of the drug
plays a vital role in the management of Amlapitta. A large number of yogas have been
explained in the classics for the management of Amlapitta, among which “Shatavari
choorna” and Abhraka Bhasma” are one of the commonly used ingredients. This study
aims at assessing the efficacy of this simple, herbo-mineral combination in the
management of Amlapitta.
A potent Amlapitta medication should possess tikta madhura rasa, madhura
vipaka and sheeta veerya to pacify the pitta and also vata. It should also possess agni
deepana property as agnimandya is the main causative factor in the pathogenesis of
Amlapitta.

Review of literature – Drug review
77
In a drug combination the drug acts combindly to give the desired effect. This is
called as the synergetic action of the combination.
In this context, the Shatavari choorna and Abhraka Bhasma along with gritha acts
combinedly to bring about a synergetic effect in management of the Amlapitta and reduce
its recurrence rate in long run.
Shatavari choorna :
Shatavari choorna due to its madhura rasa, madhura vipaka and sheeta veerya
helps to pacify the pitta and hence relieves bilous dyspepsia. Due to its deepana property
it helps to stimulate the agni and thereby reduce the agnimandya and promote appetite.
Because of its tikta rasa it has got stomachic action and reduces the pain. It also has got
soothing and demulcent action over the mucosal lining of the G.I.T. Because the balya
and rasayana effect of the drug helps in increasing the strength and general condition.
The adaptogenic activity of shatavari helps in reducing the stress and increasing
endurance and sustaining capacity.
Abhraka Bhasma :
Abhraka bhasma due to its tridoshagna property, pacifies all the doshas. Because
of its madhura rasa, madhura vipaka and sheeta veerya it specifically acts on pitta and
pacifies it. Based on experimental studies it is found to be more effective in Amlapitta,
Anemia which are caused due to pitta vitiation. Its possess high antacid property and
hence found to be very effective in Amlapitta due to its anti-dotal property. The deepana
property of the drug helps in stimulating the agni and reducing the ama. The rasayana and
balya properties indicate that the drug acts as a bioavailability enhancer and helps in
correcting the srotodusti.

Review of literature – Drug review
78
Gritha :
Gritha because of madhura rasa and sheeta veerya pacifies the pitta and sneha
guna alleviates vata. Its deepana property helps in promating agni and thus reducing the
ama. Its yogavahi guna helps in potentiating the gunas of the shatavari choorna and
abhraka bhasma and acts synergetically. It has cooling and softening affect over the
mucosal lining of the G.I.T. Gritha is said to have pitta shamaka property when licked.
Herbo-mineral compounds act as bio-catalyst, for biological energy conservation
and for signal transduction. [Ghosal.S. 1996] and thus rasayana.
Cakradutta has given emphasis on the utility of juice of rhizomes of Satavari
(Asparagus racemosus, Fam.: Liliaceae) in Daha and Sula (Cakr. 26: 28).
Maheswari and Chaturvedi (1977) have reported significant fall in free and total
acidity of gastric juice of albino rats with Satavari choorna.
In a clinical study, Singh et al. (1985) observed Shatavari mandura showed a
tendency to decrease acid-pepsin secretion, significant decrease in cell shedding and
increase in mucin secretion indicating its predominant effect on mucosal defensive
factors in deudonal ulcer. Direct healing effect was proposed probably by enhancement
of mucosal barrier, prolongation of life span of mucosal cells or cytoprotection.
LIQUID ANTACID
ANTACIDS
Antacids remain an effective therapy relieve the symptoms of Non-ulcer
dyspepsia.
Gastric antacids are substance which on injection act by neutralizing HCL
secreted by gastric parietal cells thus devoting the gastric pH. They produce symptomatic
relief of pain partly by reducing the acidity and partly by the consequent relief of muscle
spasm. Reduction in acidity inhibits the action of pepsin. It also increases the tone of the

Review of literature – Drug review
79
oesophago –gastric sphincter and reduces the reflex of the acid, gastric contents into the
oesophagas.21
Mechanism of Action:
These drugs act as weak bases. They raise the gastric pH above 4.
The antacid used for the study is Syrup-Gelusid which is a combination of
Magnesium trisilicate and Aluminium Hydroxide.
Aluminium and Magnesium Containing Antacids :
Antacids such as magnesium carbonate, hydroxide and trisilicates and aluminium
glycinate and hydroxide, being relatively insoluble in water, are long acting if retained in
the stomach. Magnesium salts increase intestinal motility, where as Aluminium decreases
it; thus antacids containing former tend to be laxative whereas those containing latter may
be constipating.A right balance of aluminium and magnesium compounds can be used so
as not to significantly change bowel function.
Sodium-bi-carbonate is a systemic antacid and not usually the antacid of choice,
especially if it has to be administered for a long period.
Advantages of Antacid combinations 22:
a) Fast [Mag.hydrox] and slow [Alum-hydrox] acting components yield promp] as well
as sustained effect.
b) Mag. Salts are laxative while Alum. Salts are constipating.Combination may annual
each others action and bowel movement each others action and bowel movement may
be least affected.
c) Gastric emptying is least affected.
d) Dose of individual components is reduced and systemic toxicity is minimized.

Methodology
80
MATERIALS AND METHODS
Samprapti vighatana forms, the basis of any chikitsa. Amlapitta is caused due to
the vitiation of pitta, and agnimandya leading to formation of ama or annavisha which
attains shuktatva leading to the clinical manifestation of the disease entity. Many number
of yoga’s have been mentioned in the classics for the treatment and management of
Amlapitta of which “Shatavari Choorna” and “Abhraka Bhasma” are also among the
most commonly used ingredients in these yoga’s. Hence an attempt has been made in this
study to assess the efficacy of this simple herbo mineral combination in the management
of Amlapitta.
Shatavari choorna and Abhraka Bhasma both are tridoshagna, madhura rasa
pradhana madhura vipaka, sheeta veerya and have deepana property which helps in
pacifying the pitta and correcting the agnimandya.
Materials :
1. Abhraka Bhasma
2. Shatavari choorna
3. Gritha for Anupana
Method of Preparation of Shatavari choorna:
Dry tubers of shatavari was procured from dealers and were properly identified
with the help of the Botanist and faculty members of Dravya guna department.
The drug was cleaned and dried in sun to remove the moisture the drug was
pounded to coarse powder and then made into a fine powder with help of a pulverizer.
The choorna thus obtained was filtered through a cloth to get a fine powder and then
packed in an air tight container.

Methodology
81
Method of preparation of Abhraka Bhasma:
The layers of Krishna abhraka was separated and subjected to shodhana by
heating it to red hot and dipping in triphala kashya for 7 times. Then Dhanyabhraka was
prepared as per the procedure described in Rasa Ratna sammuchaya. The so formed
dhanyabhraka was subjected to marana process by triturating it with kasa marda swaras
and giving puta. This was repeated for 30 times, though the bhasma became nischandra
by 10 putas in order to increase its therapeutic value the finished product and was packed
in an air tight container.
A air tight pack of 7 days medication of shatavari choorna [63gm.] along with
Abhraka Bharma [2.625gm.] was made after mixing the both thoroughly and given to the
patient at each visit the patient was asked to take 3/4th tsp. of the choorna mixing with
little of gritha to make it in the form of leha thrice daily 10-15 mins. before meals.
Form of administration of medicine : Choorna.
Dose of Medicine : 3 gms of shatavari choorna
+
125mg of Abhraka Bhasma.
Anupana : Gritha [little quantity] to mix the choorna to make it
like leha.
Time and Duration : 10-15 mins before meals thrice daily for a month.
METHODOLOGY
Objectives :
1. To evaluate the efficacy of “Shatavari Choorna” with “Abhraka Bhasma” in the
management of amlapitta.
2. To compare the effect of Shatavari choorna with Abhraka Bhasma over liquid
antacid by controlled trial.
3. Treating the disease by correcting the samprapti rather than symptoms.

Methodology
82
4. Detailed study of disease covering classical and modern literature.
5. To establish an effective, simple herbo-mineral combination in the management
of Amlapitta.
Source of data:
The patients of either sex diagnosed as Amlapitta on the basis of classical features
were randomly selected from the OPD and IPD of A.L.N.Rao Memorial Ayurvedic
Medical College Hospital, Koppa and associated hospitals.
Sampling Method:
Total 64 diagnosed cases of Amlapitta were selected at random from clinical
survey of patients attending the IPD and OPD of A.L.N.Rao Memorial Ayurvedic
Medical College Hospital, Koppa and associated hospitals.
A complete history including the general body condition of the patient was
assessed and few bio-chemical investigations were done to rule out systemic illness and
other complications and were selected only after found fulfilling the diagnostic as well as
inclusive criteria. There after the patients were registered and treated as outpatients for
the present study with the help of the case proforma specially designed for the study.
Criteria for selection of the patients :
Diagnostic Criteria:
The patients presenting with the following subjective signs and symptoms with
one or more associated symptoms and investigations were selected for the study.
1. Utklesha.
2. Hrithdaha.
3. Kantadaha.
4. Amlodgara.

Methodology
83
5. Vanti.
6. Udara shoola.
7. Normal hematocrit, White Bllod cell. Count and erythrouyte sedimentation rate.
8. Normal urine free from sugar, albumin and microbes
9. Normal stool with no ova and cysts.
10. Endoscopy if necessary to rule out ulcers.
Inclusion Criteria :
Patients fulfilling the following conditions were included for the study.
1. Patients presenting with pratyatma laxanas of Amlapitta like utklesha
[Nausea].Hrithdaha [heart burn], Kantadaha [Burning sensation in throat],
Amlodgara [acid erructations], Vanti [Vomiting] and Udara shoola [pain in
abdomen with or without other laxanas like Aruchi, Adhamana, Kalama etc.
2. Patients of either sex between 18-50 years of age.
3. A minimum history of 3 months were selected.
Exclusion Criteria :
Patients presenting with the below mentioned conditions were excluded from the
study.
1. Patients below 18yrs and above 50yrs of age.
2. Subjects suffering from acute-gastro intestinal disorders like.
i. Peptic ulcers.
ii. Duodenal ulcers.
iii. Panceratic and Hepatic diseases.
iv. Motility disorders.

Methodology
84
v. Inflammatory Bowel Disease.
3. Lactating and pregnant women.
4. Any other severe complicating systemic illness.
Research Design:
It is a randomized single single blind control study where liquid antacid i.e.
Syrup. Gelusil is control drug and Shatavari choorna and Abhraka Bhasma with gritha is
the trial drug.
Selection of the patients :
After the diagnosis as on the above parameters, the patients selected were
assigned into two groups of 30 patients each.
Trail group received Shatavari choorna - 3gms + Abhraka Bhasma – 125 mg
With Gritha thrice daily before meals.
Duration 1 month.
Control group, received Syrup. Gelusil 1 tsp thrice daily before meals.
Duration 1 month.
Total number of patients registered for study : 64.
Total number of patients in Trial Group : 32.
No. of patients completed the treatment in Trial Group : 30.
No. of patients discontinued the treatment in Trial Group : 2.
Total number of patients in Control Group : 32.
No. of patients completed the treatment in Control Group : 30.
No. of patients who discontinued the treatment in Control Group : 2.

Methodology
85
Investigations :
The following investigations were carried out on mandatory basis for each patient
before starting the treatment in order to rule out general condition, systemic illness and
other complications and also to fulfill the diagnostic as well as inclusive criteria.
a) Blood investigations - Hb%
E.S.R.
T.C. & D.C.
b) Urine investigations - Albumin.
Sugar.
Microscopic.
c) Stool Examination - Ova & Cyst.
d) Endoscopy - If necessary.
Interventions :
Trial group – Drugs : Shatavari choorna – 3 gms. + Abhraka Bhasma – 125 mg.
- Anupana : Gritha.
- Duration : Thrice daily before meals for 1month.
Control group - Drug : Syrup Gelusil.. 1 Tsp thrice daily
before meals
- Duration : 1 month
Follow up - : 1 month.
The follow up was done once a week during the treatment and there after for a
duration of 1 month for both the groups.
During this period the patient was advised to follow the pathyapthya.
Assessment of Response :

Methodology
86
The assessment of response of patients were made on the basis of improvements
observed in the following subjective parameters.
I. Cardinal complaints :
1. Ulklesha [Nausea] 2. Hrthdaha [Heart Burn]
3. Kanta daha [Burning in throat] 4. Amlodgena [Acid Erructation]
5. Vanti [Vomiting] 6. Udara shoola [Abdominal pain]
II. Associated complaints :
1. Avipaka 2. Klama. 3. Tiktodgara.
4. Gourava. 5. Aruchi. 6. Gurukoshtata.
7. Adhmana. 8. Antrakujana. 9. Sirashula.
Criteria of Assessment :
The following criteria were adopted to assess the results at the end of the
treatment schedule.
1. Improvement in the cardinal signs and symptoms of the disease on the basis of
symptom score.
2. Improvement in the associated signs and symptoms of the disease on the basis of
symptom score.
3. Improvements in dusti score of Annavaha, Rasavaha and Pureeshavaha srotas.
Scoring of cardinal symptoms:
1. Utklesha : [Nausea]
Severity of utklesha is scored as fallows.
Grade 3 : Frequent with vomiting.

Methodology
87
Grade 2 : Frequent but no vomiting.
Grade 1 : Occasionally only on consumption of faulty diet.
Grade 0 : No utklesha.
2. Amlodgara : [Acid Erructation]
Severity of Amlodgara is scored as fallows :
Grade 3 : Continuous throughout the day.
Grade 2 : Occurs on consuming food stuffs.
Grade 1 : Occasional; only on consuming sour or spicy food.
Grade 0 : No Amlodgara.
3. Hrithdaha : [Heart burn]
Severity of Hrithdaha is scored as follows.
Grade 3 : Continuous burning, throughout the day.
Grade 2 : Occurs on consuming food stuffs.
Grade 1 : Occasional; only on consuming sour and spicy food.
Grade 0 : No Hrithdaha.
4. Kantadaha : [Burning sensation in throat]
Severity of Kantadaha is scored as fallows.
Grade 3 : Continuous throughout the day.
Grade 2 : Occurs on consuming food stuffs.
Grade 1 : Occasional; only on consuming spicy or sour food.
Grade 0 : No Kantadaha.
5. Vamana : [Vomiting]
Severity of vamana is scored as fallows

Methodology
88
Grade 3 : Frequently.
Grade 2 : Occurs only in early morning.
Grade 1 : Rarely
Grade 0 : No Vamana.
6. Udara Shoola : [Pain Abdomen]
Severity of Udarashoola is scored as fallows
Grade 3 : Severe pain, disturbing daily routine.
Grade 2 : Moderate pain enough to take medical advice.
Grade 1 : Mild pain or dull aching pain.
Grade 0 : No Pain.
Associated symptoms :
The severity of associated symptoms are scored with following rating method.
Grade 0 : Normal. Grade 1 : Mild.
Grade 2 : Moderate. Grade 3 : Severe.
I. The patients with mild associated symptoms are defined as those with one or more
of the following.
1. Symptoms occur less than twice in a week or when exposed to causative factors.
2. Presence of symptoms for few hours, does not interfere with daily routine,
occasionally feeling of inconvenience during routine work.
3. Nausea may be present but vomiting is rare.
II. The patients with moderate associated symptoms are defined as those with one or
more of the following.
1. Presence of symptoms 2 to 4 times in a week.
2. The symptoms present during day and night does interfere, but doesn’t prohibit
work performance and other activities.

Methodology
89
3. Occasional presence of vomiting.
III. The patients with severe Amlapitta are defined as those with one or more of the
following.
1. Continuous presence of symptoms.
2. Symptoms develop during the day as well as in night.
3. Frequent vomiting.
Scoring of Sroto dusti :
Amlapitta being a disease involving mainly Annavaha, Rasavaha and
Pureeshavaha srotas, the sroto dusti lakshanas of these srotas are assessed and scoring of
the sroto dusti is done as follows:
1. Annavaha srotas :
Severity of Annavaha sroto dusti is scored as follows:
Grade 3 : All the symptoms.
Grade 2 : Chardi along with any 1 or 2 symptoms.
Grade 1 : Only Aruchi and Avipaka.
Grade 0 : No symptoms.
Rasavaha srotas :
Severity of Rasavaha sroto dusti are scored as follows :
Grade 3 : All the symptoms.
Grade 2 : Presence of 5 - 8 symptoms.
Grade 1 : Presence of 3 - 4 symptoms.
Grade 0 : No symptoms.
Pureeshavaha srotas :
Severity of Pureeshavaha sroto dusti are scored as follows.
Grade 3 : All the symptoms.
Grade 2 : Presence of 3 - 5 symptoms.
Grade 1 :Presence of 2 Symptoms.
Grade 0 : No symptoms.

Methodology
90
Statistical analysis :
Mean, Percentage, Standard Deviation, Standard Error, ‘t’ value and ‘p’ value
were calculated.
Paired ‘t’ test was used for calculating the ‘t’ value in the paired data.
Assessment of overall effect of therapy :
The overall effect of the therapy was assessed as stated below.
1. Patients in whom there was 100% relief in all signs and symptoms with no recurrence
was considered as cured. [cases]
2. Patients in whom there was relief in signs and symptoms my more than 75% with no
recurrence was considered be marked improvement. [cases]
3. Patients in whom there was relief in signs and symptoms by more than 50% with
recurrence of signs and symptoms in milder form was considered to be improved.
[cases]
4. Patients in whom there was relief in signs and symptoms by more than 25% with
recurrence of signs and symptoms in moderate form was considered be controlled.
5. Patients in whom there was less than 25% relief in signs and symptoms and
recurrence of all the signs and symptoms in severe form was considered to be
unchanged].

Methodology
91
0
2
4
6
8
10
12
18-25 26-33 43-41 42-50
Trail GroupControl Group
OBSERVATIONS
In the present study total 64 patients of Amlapitta were registered. Out of which
60 patients completed the course of treatment in both the groups i.e. 30 patients in each
group and remaining 4 patients discontinued the treatment. The biostatistical observations
and total effect of the treatment is presented on findings of 60 patients (30 in each group)
only.
Incidence of Age
Table no. 13 Showing the age wise distribution of 60 Amlapitta patients.
Sl.
No. Age (in yrs.)
Trial
Group %
Control
Group % Total %
01 18-25 3 10 6 20 9 15
02 26-33 12 40 9 30 21 35
03 34-41 9 30 9 30 18 30
04 42-50 6 20 6 20 12 20
Majority of patients belongs to age group of 26-33 yrs. i.e. 35% followed by 30% in the
age group 34-41 yrs; 20% in 42-50yrs age group while 15% were in the 18-25 yrs age
groups.
Graph no. 1 Showing the age wise distribution of 60 Amlapitta patients.

Methodology
92
0
5
10
15
20
1 2
MaleFemale
Incidence of Sex
Table no. 14 Showing the Sex wise distribution of 60 Amlapitta patients.
Sl
No Sex Trial Group %
Control
Group % Total %
01 Male 12 40 15 25 25 45
02 Female 18 60 15 25 33 55
55% of the patients in the study were females while 45% were males.
Graph no. 2 Showing the Sex wise distribution of 60 Amlapitta patients.
Incidence of Religion
Table no. 15 Showing the Religion wise distribution of 60 Amlapitta patients.
Sl.
No Religion Trial Group %
Control
Group % Total %
01 Hindu 15 25 18 60 33 55
02 Muslim 9 30 6 20 15 25
03 Christian 6 20 6 20 12 20
Amongst the patients registered for the study 55% were Hindus, followed by 25%
Muslims and 20% were Christians.

Methodology
93
0
2
4
6
8
10
12
14
16
18
Married Unmarried Widow/Widower
Divorcee
Trial GroupControl Group
0
2
4
6
8
10
12
14
16
18
Hindu Muslim Christian
Trial GroupControl Group
Graph no. 3 Showing the Religion wise distribution of 60 Amlapitta patients.
Incidence of Marital status
Table no. 16 Showing the Marital status wise distribution of 60 Amlapitta patients.
Sl.
No. Status
Trial
Group %
Control
Group % Total %
01 Married 12 40 18 60 30 50
02 Unmarried 15 50 9 30 24 40
03 Widow/ Widower 3 10 0 0 3 5
04 Divorcee 0 0 3 10 3 5
50% of the patients were married , 40% were not married, 5% of them were divorcee. and
5% were widow/widower.
Graph no. 4 Showing the Marital status wise distribution of 60 Amlapitta patients.

Methodology
94
Une
duca
ted
Prim
ary
scho
ol
Mid
dle
scho
ol
Hig
h sc
hool
Gra
duat
e
Trial roupControl Group
Incidence of Educational status
Table no. 17 Showing the Educational status wise distribution of 60 Amlapitta
patients.
Sl.
No. Education
Trial
Group %
Control
Group % Total %
01 Uneducated 9 30 6 20 15 25
02 Primary school 3 10 3 0 6 10
03 Middle school 0 0 6 20 6 10
04 High school 9 30 6 20 15 25
05 Graduate 9 30 9 30 18 30
30% of the patients were graduates, 25% were uneducated, 25% were educated up
to high school, 10% up to middle school and 10% up to primary school.
Graph no. 5 Showing the Educational status distribution of 60 Amlapitta patients.

Methodology
95
0
2
4
6
8
10
12
14
16
Very poor Poor Lr. Middle Middle Ur. Middle Rich
Trial Group
Control Group
Incidence of Socioeconomic status
Table no. 18 Showing the socioeconomic status wise distribution of 60 Amlapitta
patients.
Sl.
No Strata
Trial
Group %
Control
Group % Total %
01 Very poor 3 10 0 0 3 5
02 Poor 6 20 3 10 9 15
03 Lr. Middle 6 20 9 30 15 25
04 Middle 9 30 15 50 24 40
05 Ur. Middle 3 10 3 10 6 10
06 Rich 3 10 0 0 3 5
40% of the patients belonged to the middle class. 25% representation was seen in middle
class. 15% belonged to poor class, 10% belonged to upper middle class, and 5% were
from the very poor and rich class each.
Graph no. 6 Showing the Socioeconomic status wise distribution of 60 Amlapitta
patients.

Methodology
96
05
10152025303540
Student Housewife
Labour Business Services
Trial groupControl group
Incidence of Occupational status
Table no. 19 Showing the Occupational status wise distribution of 60 Amlapitta
patients.
Sl,
No Occupation
Trial
Group %
Control
Group % Total %
01 Student 3 10 - 0 3 5
02 House wife 12 40 9 30 21 35
03 Labour 6 20 6 20 12 20
04 Business 6 10 12 40 18 30
05 Service 3 10 3 10 6 10
35% of the patients were house wives followed by 30% belonged to business
class. 20% to labour class; 10% to service and 5% of them were students.
Graph No. 7 Showing the Occupational status wise distribution of 60 Amlapitta
patients.
Incidence of Onset
Table No. 20 Showing the onset wise distribution of 60 Amlapitta patients.
Sl,
No
Onset
Trial
Group %
Control
Group % Total %
01 Sudden 12 40 15 50 27 45
02 Gradual 18 60 15 50 23 55
Table shows that 55% of patients presented gradual onset while 45% presented sudden
onset.

Methodology
97
010
2030
4050
60
Sudden Gradual
Trial groupControl group
0
10
20
30
40
50
Mid-day Mid-Night Morning
Trial groupControl group
Graph No. 8 Showing the onset wise distribution of 60 Amlapitta patients.
Incidence of Aggravating Period
Table No 21 Showing the Aggravating period wise distribution of 60 Amlapitta
patients
Sl, No
Aggravating Period
Trial Group % Control
Group % Total %
01 Mid-day 15 50 12 40 27 40
02 Mid-Night 3 10 3 10 6 10
03 Morning 12 40 15 50 27 40
40% of patients presented with aggravation of symptoms in Mid-day;40% in the
morning and10% in Mid-night
Graph No. 9 Showing the Aggravating Period wise distribution of 60 Amlapitta
patients.

Methodology
98
0
10
20
30
40
50
60
Rainy Autumn Summer Winter
Trial groupControl group
Incidence of Aggravation due to Environmental Factor
Table No 22 Showing the Incidence Aggravating of symptoms due to
environmental factors in 60 Amlapitta patients
Sl, No
Environmental Factor
Trial Group % Control
Group % Total %
01 Rainy 15 50 18 60 33 55 02 Autumn 03 10 03 10 06 10 03 Summer 09 30 09 30 18 30 04 Winter 3 10 0 0 3 5
55% patients showed aggravation of symptoms in rainy season;followed by 30%
insummer;10% in autumn and 5% in winter season
Graph No.10 Showing the Incidence Aggravating Of symptoms due to
environmental factors in 60 Amlapitta patients
Incidence of Habitat
Table no. 23 Showing the Habitat status wise distribution of 60 Amlapitta patients.
Sl.
No. Habitat Trial Group %
Control
Group % Total %
01 Urban 9 30 12 40 21 35
02 Rural 21 70 18 60 39 65
65% of the patients were from rural populace while 35% were from urban populace.

Methodology
99
0
5
10
15
20
25
Urban Rural
Trial GroupControl Group
0
5
10
15
20
25
Trial Group Control Group
Vegetarian
Mixed
Graph no. 11 Showing the Habitat wise distribution of 60 Amlapitta patients.
Incidence of Dietary habit
Table no. 24 Showing the Dietary habit wise distribution of 60 Amlapitta patients.
Sl.
No Diet
Trial
Group %
Control
Group % Total %
01 Vegetarian 9 30 12 40 21 35
02 Mixed 21 70 18 60 39 65
65% of the patients were consuming mixed diet, while 35% were strict vegetarians.
Graph no. 12 Showing the Dietary habit wise distribution of 60 Amlapitta patients.
Incidence of Ahara vidhi
Table no.25 Showing the Ahara vidhi wise distribution of 60 Amlapitta patients.
Sl. No. Ahara vidhi Trial
Group % Control Group % Total %
01 Samasana 9 30 6 20 15 25 02 Visamasana 18 60 21 70 39 65 03 Adhyasana 3 10 6 20 9 15

Methodology
100
0
5
10
15
20
25
Samasana Visamasana Adhyasana Anashana Pramitasana Viruddhasana
Trial Group
Control Group
04 Anashana 0 0 0 0 0 0 05 Pramitasana 9 30 6 20 15 25 06 Viruddhasana 6 20 9 30 15 25
65% of the patients gave a history of Visamasana, 25% each gave history of Samasana,
Viruddhasana and Pramitasana and 15% of Adhyasana.
Graph no. 13 Showing the Ahara vidhi wise distribution of 60 Amlapitta patients.
Type Of Diet Table No. 26 Showing the Type of diet wise distribution of 60 Amlapitta patients.
Sl, No
Type Of Diet
Trial Group % Control
Group % Total %
01 Viruddhanna 9 30 6 20 15 25 02 Pittaprakopaka 9 30 12 40 21 35 03 Vidahianna 3 10 3 10 6 10 04 Amlarasapradhana 6 20 6 20 12 20 05 Abhishyandhi 3 10 0 0 3 5 06 Atibhojana 0 0 3 10 3 5
35% of patients were used to pittaprakopaka ahara; while 25% were used to
Virudhanna; 20% were used to amlarasapradhana; 10% to vidahianna and 5% to
atibhojana.

Methodology
101
0
10
20
30
40
Viruddhanna Pit t aprakopaka Vidahianna Amlarasapradhana Abhishyandhi At ibhojana
Trial group
Control group
0
5
10
15
20
25
Madhura Amla Lavana Katu
Trial Group
Control Group
Graph No.14 Showing the Type of diet wise distribution of 60 Amlapitta patients.
Incidence of Rasa satmya
Table no. 27 Shows Rasa Satmya wise distribution of 60 Amlapitta patients
Sl. No. Rasa Trial Group %
Control
Group % Total %
01 Madhura 9 30 6 20 15 25
02 Amla 12 40 9 30 21 35
03 Lavana 9 30 9 30 18 30
04 Katu 18 60 21 70 39 60
60% of the patients showed Katu rasa satmyata, 30% were Lavana rasa satmya, 35%
were Amla rasa satmya and 25% were Madhura rasa satmya.
Graph no. 15 Shows Rasa Satmya wise distribution of 60 Amlapitta patients

Methodology
102
0
10
20
30
40
Diw asw apna Vegadharana Avagahana Atapasevana
Trial group
Control group
Incidence of Regimen
Table no. 28 Showing the Regimen wise distribution of 60 Amlapitta patients.
Sl,
No
Regimen
Trial
Group %
Control
Group % Total %
01 Diwaswapna 6 20 3 10 9 15
02 Vegadharana 9 30 6 20 15 25
03 Avagahana 6 20 12 40 18 30
04 Atapasevana 9 30 9 30 18 30
Above table shows 30% of patients gave a history of atapasevana; 30% of
avagahana; 25% of vegadharana and remaining 15% of diwaswpna.
Graph no. 16 Showing the Regimen wise distribution of 60 Amlapitta patients.
Incidence of Mental stress\strain
Table no. 29 Showing the Mental stress/strain wise distribution of 60 Amlapitta
patients.
Sl. No Mental stress Trial
Group % Control Group % Total %
01 Present 18 60 21 70 39 70
02 Absent 12 40 9 30 21 30
70% of the patients gave a history of mental stress while 30% did not have any mental
stress.

Methodology
103
0
5
10
15
20
25
Trial Group Control Group
PresentAbsent
Graph no.17 Showing the Mental stress/strain wise distribution of 60 Amlapitta
patients.
Incidence of Addictions
Table no.30 Shows incidence of Addictions in 60 Amlapitta patients
Sl. No. Habits Trial
Group % Control Group % Total %
01 Tea/Coffee 21 70 18 60 39 65
02 Smoking 9 30 6 20 15 25
03 Alcohol 3 10 6 20 9 15
04 Tobacco 0 0 3 10 3 5
05 Cool drinks 3 10 6 20 9 15
06 NSAID’s 6 20 6 20 12 20
07 None 3 0 0 0 3 5
65% of the patients gave a history of regular consumption of tea/coffee, 25% were
addicted to smoking, 20% of the patients had history of consumption of NSAID’s,15% of
patients were addicted to alcohol and cool-drinks,5% of them had no addictions.

Methodology
104
0
5
10
15
20
25
Tea/
Cof
fee
Smok
ing
Alco
hol
Toba
cco
Coo
l drin
ks
NSA
ID’s
Non
e
Trial Group
Control Group
0
2
4
6
8
10
12
Regular Irregular Occasional Only RoutineWork
Trial Group
Control Group
Graph no. 18 Shows incidence of Addictions in 60 Amlapitta patients
Incidence of Exercise
Table No. 31 Showing the Exercise wise distribution of 60 Amlapitta patients.
Sl, No Exercise Trial
Group % Control Group % Total %
01 Regular 3 10 0 0 3 5
02 Irregular 6 20 9 30 15 25
03 Occasional 9 30 12 40 21 35
04 Only Routine
Work 12 40 9 30 21 35
Table shows that 35% of the patients did only routine work; 35% of patients only
occasional exercise; 25% did irregular exercise and only 5% did regular exercise.
Graph No.19 Showing the Exercise wise distribution of 60 Amlapitta patients.

Methodology
105
0
2
4
6
8
10
12
14
16
18
Sound Irregular Disturbed Delayed
Trial GroupControl Group
Incidence of Nidra
Table no.32 Shows incidence of nidra in 60 Amlapitta patients
Sl. No Nidra Trial
Group % Control Group % Total %
01 Sound 6 20 3 10 9 15
02 Irregular 6 20 6 20 12 20
03 Disturbed 9 30 18 60 27 45
04 Delayed 9 30 9 30 18 30
45% of the patients complained of disturbed sleep,while 30% of delayed sleep 20% of
irregular sleep and15% of no such complaints.
Graph no. 20 Shows incidence of nidra in 60 Amlapitta patients
Incidence of Bowel Habit
Table no. 33 Shows Bowel habit wise distribution of 60 Amlapitta patients
Sl, No
Bowel Habit
Trial Group % Control
Group % Total %
01 Regular 6 20 3 10 9 15
02 Irregular 9 30 9 20 18 30
03 Constipation 15 50 18 60 33 55
Above table shows 55% of patients had constipation; 30% had irregular bowel
habit and 15% had regular bowel habit
Graph No. 21 Shows Bowel habit wise distribution of 60 Amlapitta patients

Methodology
106
0
10
20
30
40
50
60
Regular Irregular Constipation
Trial groupControl group
0
2
4
6
8
10
12
14
16
18
Loose Soft Constipated
Trial Group
Control Group
Incidence of Nature of Stool
Table No. 34 Shows Nature of stool wise distribution of 60 Amlapitta patients
Sl, No Nature Of Stool Trial
Group % Control Group % Total %
01 Loose 3 10 6 20 9 15
02 Soft 12 40 6 20 18 30
03 Constipated 15 50 18 60 33 55
Majority of the patients i.e.55% complained of constipated stool; 30% of soft
stool and remaining 15% of loose stools.
Graph No. 22 Shows Nature of stool wise distribution of 60 Amlapitta patients

Methodology
107
0
2
4
6
8
10
12
14
16
18
Heavy Moderate Sedentary
Trial GroupControl Group
Incidence of Type of occupation
Table No.35 Shows Type of occupation wise distribution of 60 Amlapitta patients
Sl. No. Degree of work Trial
Group % Control Group % Total %
01 Heavy 9 30 3 10 12 20
02 Moderate 15 50 18 60 33 55
03 Sedentary 6 20 9 30 15 25
55% had moderate degree of work, 20% were heavy workers, 25% while were sedentary.
Graph No.23 Shows Type of occupation wise distribution of 60 Amlapitta patients
Incidence of Nature Of Work
Table No.36 Shows Nature of work wise distribution of 60 Amlapitta patients
Sl, No
Nature Of Work
Trial Group % Control
Group % Total %
01 Physical 15 50 18 60 33 55
02 Mental 15 50 12 40 27 45
55% of the patients were in physical nature of work, while 45% in mental nature
of work.

Methodology
108
010
2030
4050
60
Physical Mental
Trial groupControl group
0
2
4
6
8
10
12
14
16
18
Vata pittala Pittakaphala Vatakaphala
Trial GroupControl Group
Graph No. 24 Shows Nature of work wise distribution of 60 Amlapitta patients
Incidence of Deha prakrti
Table no. 37 Shows incidence of Deha prakriti in 60 Amlapitta patients
Sl. No. Prakrti Trial
Group % Control Group % Total %
01 Vata pittala 18 60 12 40 30 50
02 Pittakaphala 12 40 12 40 24 40
03 Vatakaphala 0 0 6 20 6 10
Amongst the patients, 50% were of Vatapittala prakrti, 40% of Pittakaphala and 10% of
Vatakaphala.
Graph no. 25 Shows incidence of Deha prakrati in 60 Amlapitta patients

Methodology
109
0
2
4
6
8
10
12
14
16
18
Tvak Mamsa Asthi Majja
Trial Group
Control Group
Incidence of Sara
Table no.38 Shows Sara wise distribution of 60 Amlapitta patients
Sl.No. Sara Trial Group % Control
Group % Total %
01 Tvak 9 30 6 20 15 25
02 Mamsa 15 50 18 60 33 55
03 Asthi 6 20 3 10 9 15
04 Majja 0 0 3 10 3 5
55% of the patients were of Mamsa sara, 25% were of Tvak sara while 15% were Asthi
sara and 5% were Majja sara.
Graph no. 26 Shows Sara wise distribution of 60 Amlapitta patients
Incidence of Samhanana
Table no. 39 Shows Samhanana wise distribution of 60Amlapitta patients
Sl. No. Samhanana Trial
Group % Control Group % Total %
01 Pravara 12 40 6 20 18 30
02 Madhyama 18 60 21 70 39 65
03 Avara 0 0 3 10 3 5
65% of the patients were of Madhyama samhanana followed by 30% of Pravara and 5%
of Avara samhanana.

Methodology
110
0
5
10
15
20
25
Pravara Madhyama Avara
Trial GroupControl Group
0
2
4
6
8
10
12
14
16
18
Pravara Madhyama Avara
Trial Group
Control Group
Graph no. 27 Shows Samhanana wise distribution of 60Amlapitta patients
Incidence of Satva
Table no. 40 Shows Satva wise distribution of 60 Amlapitta patients
Sl. No Satva Trial
Group % Control Group % Total %
01 Pravara 3 10 6 20 9 15
02 Madhyama 18 60 18 60 36 60
03 Avara 9 30 6 20 15 25
60% of the patients were of Madhyama satva, 25% of Avara satva and 15% of Pravara
satva.
Graph no. 28 Shows Satva wise distribution of 60 Amlapitta patients

Methodology
111
0
5
10
15
20
25
Tiksna Visama Manda Sama
Trial GroupControl Group
Incidence of Agni
Table no. 41 Shows Agni wise distribution of 60 Amlapitta patients
Sl.No Agni Trial Group % Control
Group % Total %
01 Tiksna 3 10 3 10 6 10
02 Visama 6 20 9 30 15 25
03 Manda 21 70 18 60 39 65
04 Sama 0 0 0 0 0 0
65% of the patients suffered from Mandagni while 25% had Visamagni,and10% of them
had tikshanagni.
Graph no.29 Shows Agni wise distribution of 60 Amlapitta patients
Incidence of Koshta
Table No. 42 Shows Koshta wise distribution of 60 Amlapitta patients
Sl, No
Koshta
Trial Group % Control
Group % Total %
01 Mrudu 09 30 9 30 18 30
02 Madhyama 12 40 15 50 27 45
03 Krura 9 30 6 20 15 25
45% of the patients had madhyama koshta followed by 30% of mrudu koshta and
25% had krura koshta.
Graph No.30 Shows Koshta wise distribution of 60 Amlapitta patients

Methodology
112
0
10
20
30
40
50
Mrudu Madhyama Krura
Trial groupControl group
0
5
10
15
20
25
Pravara Madhyama Avara
Trial GroupControl Group
Incidence of Bala
Table no.43 Shows Bala wise distribution of 60 Amlapitta patients
Sl. No Bala Trial
Group % Control Group % Total %
01 Pravara 6 20 15 50 24 30
02 Madhyama 24 80 15 50 39 70
03 Avara 0 0 0 0 0 0
Pravara bala patients were 70% while 30% were of Madhyama bala.
Graph no. 31 Shows Bala wise distribution of 60 Amlapitta patients

Methodology
113
010203040506070
Anoopa Jangala Sadharana
Trial groupControl group
Incidence of Desha
Table no. 44 Shows Desha wise distribution of 60 Amlapitta patients
Sl. No Desha
Trial
Group % Control Group % Total %
01 Anoopa 21 70 15 50 36 55
02 Jangala 9 30 12 40 24 40
03 Sadharana 0 0 3 10 3 5
Table shows 55% of patients were from anoopa desha; 40% from jangala and 5%
from sadharana desha.
Graph No. 32 Shows Desha wise distribution of 60 Amlapitta patients
Incidence of Duration of illness
Table no.45 Shows Duration of Illness wise distribution of 60 Amlapitta patients
Sl.
No.
Duration Trial
Group
% Control
Group
% Total %
01 > 6 mths. 6 20 3 10 9 15
02 7-12 mths 12 40 6 20 18 30
03 13-18 mths 3 10 15 50 18 30
04 19-24 mths 6 20 3 10 9 15
05 25-30 mths 3 10 0 0 3 5
06 31-36 mths 0 0 3 10 3 5

Methodology
114
0
2
4
6
8
10
12
14
16
> 6 mths. 7-12 mths 13-18mths
19-24mths
25-30mths
31-36mths
Trial GroupControl Group
30% gave a history of 7mths to 12 mths and 13mths to 18mths of illness each, 15% had
suffered for less than 6mths, 5% had the illness for 25mths to30mths and 31mths
to36mths each.
Graph no.33 Shows Duration of Illness wise distribution of 60 Amlapitta patients
Incidence of Samanya laksana
Table no.46 Shows Samanya lakshana wise distribution of 60 Amlapitta patients
Sl. No. Laksana Trial
Group % Control Group % Total %
01 Utklesha 27 95 25 83 52 87 02 Amlodgara 27 95 23 77 50 83 03 Hrtdaha 27 95 22 73 49 81 04 Kanthadaha 18 60 24 80 42 70 05 Udarashoola 24 80 24 80 48 80 06 Vanti 16 53 23 77 39 65
The most prominent feature was that of Utklesa (Nausea) and was seen in all most
all the patients in both the groups i.e87%; Amloudgara(acid erructations) was present in
83% of the patients, Hrtdaha (Burning in cheste) in 81%;Udara shoola (pain in abdomen)
in 80%;kantadaha(Burning in throat) in 70% and 60% of patients presented vanti.All the
patients gave a history of aggravation of symptoms following consumption of specific
foods and regimen.

Methodology
115
0102030405060708090
100
Utkle
sha
Am
lodg
ara
Hrtd
aha
Kant
hada
ha
Udar
asho
ola
Van
ti
Trial group
Control group
Graph No. 34 Shows Samanya lakshana wise distribution of 60 Amlapitta patients
Incidence of Associated symptoms
Table no.47 Shows Associated symptom wise distribution of 60 Amlapitta patients
Sl. No Laksana Trial
Group % Control Group % Total %
01 Avipaka 21 70 15 50 36 60 02 Klama 14 47 14 47 28 47 03 Tiktodgara 13 43 16 53 29 48 04 Gourava 16 53 12 40 28 47 05 Aruchi 18 60 16 53 34 57 06 Gurukoshtatha 17 57 13 43 30 50 07 Adhamana 19 63 16 53 35 58 08 Antrakujana 8 27 16 53 24 40 09 Sirasula 14 47 17 57 31 52
60% of the patients complained of avipaka; 58% of patients complained of adhamana;
57% of aruchi; 52% of sirasula; 50% of gurukoshtatha; 48% of tiktodgara; 47% of klama
and gourava each and 40% of patient complained of antrakujana.

Methodology
116
0
5
10
15
20
25
Avip
aka
Klam
a
Tikt
odga
ra
Gou
rava
Aruc
hi
Gur
ukos
htat
ha
Adha
man
a
Antra
kuja
na
Sira
sula
Trial Group
Control Group
0
10
20
30
40
Annavaha Rasavaha Pureeshavaha
Trial group
Control group
Graph No. 35 Shows Associated symptom wise distribution of 60 Amlapitta patients
Incidence of Srotodusti
Table no. 48 Shows Srotodusti wise distribution of 60 Amlapitta patients
Sl. No Srotas Trial
Group % Control Group % Total %
01 Annavaha 12 40 9 30 21 35
02 Rasavaha 9 30 12 40 21 35
03 Pureeshavaha 9 30 9 30 18 30
35% of the patients had annavaha srotodusti and rasavaha srotodusti lakshanas each and
30% of the patients had pureeshavaha srotodusti lakshanas.
Graph No.36 Shows Srotodusti wise distribution of 60 Amlapitta patients

Results
117
RESULTS Effect of Trial drug on Main symptoms:
Table no. 49 Effect of Trial drug on Main symptoms after Treatment
Mean Lakshana BT AT BT-AT
% SD (±)
SE (±)
t P Remarks
Utklesha 1.44 0.852 0.598 59.85 0.500 0.096 6.143 <0.001 HS
Amlodgara 2.07 1.270 0.730 73.07 0.567 0.111 7.19 <0.001 HS
Hrtdaha 1.92 1.111 0.727 72.77 0.483 0.093 8.750 <0.001 HS
Kanthadaha 1.55 0.944 0.611 61.66 0.501 0.118 5.168 <0.001 HS
Udarashoola 2.125 1.375 0.625 62.50 0.516 0.137 3.872 <0.001 HS
Vanti 1.562 1.062 0.500 50.00 0.675 0.129 5.437 <0.001 HS
The trial drug provided highly significant relief(p<0.001) in all the symptoms
especially in management of amlodgara and hrtdaha by 73.07% and 72.77%
respectively.
The other symptoms also showed highly significant relief i.e.utklesha kantadaha,
udarashoola and vamana by 59.85%,61.11%,62.5% and 50% respectively.
An overall highly significant result was observed in the main symptoms after the
treatment.
Effect of Trial drug on Main symptoms:
Table no. 50 Effect of Trial drug on Main symptoms after follow up
Mean Lakshana BT AFU BT-AFU
% SD (±) SE (±) t P Remarks
Utklesha 1.44 1.19 0.259 25.92 0.446 0.085 2.908 <0.010 MS
Amlodgara 2.07 1.63 0.407 40.74 0.577 0.111 3.996 <0.001 HS
Hrtdaha 1.92 1.58 0.333 33.33 0.480 0.092 3.601 <0.010 MS
Kanthadaha 1.55 1.273 0.277 27.77 0.460 0.108 2.549 <0.050 Mi. S
Udarashoola 2.125 1.584 0.541 54.16 0.508 0.103 5.207 <0.001 HS
Vanti 1.562 1.187 0.375 37.50 0.500 0.125 3.000 <0.01 MS

Results
118
The trial drug provided highly significant relief(p<0.001) in the management of
especially udarashoola and amlodgara by 54.16% and 40.74% respectively even after the
follow up.
The drug provided moderately significant relief(p<0.010) in the management of hrtdaha,
vamana and utklesha by 33.33%, 37.5% and 25.92% respectively.
It provided mild significant relief(p<0.050) in the management of kantadaha by 27.77%.
Effect of Control drug on Main symptoms:
Table no.51 Effect of Control drug on Main symptoms after Treatment
Mean Lakshana BT AT BT-
AT
% SD (±)
SE (±)
t P Remarks
Utklesha 1.72 1.20 0.52 52.00 0.509 0.101 5.099 <0.001 HS
Amlodgara 1.52 0.956 0.565 56.52 0.506 0.105 5.345 <0.001 HS
Hrtdaha 1.54 1.06 0.50 50.00 0.500 0.106 4.690 <0.001 HS
Kanthadaha 1.33 0.875 0.458 45.80 0.508 0.103 4.408 <0.001 HS
Udarashoola 1.50 0.772 0.75 75.00 0.607 0.129 5.249 <0.001 HS
Vanti 1.78 1.086 0.695 69.50 0.634 0.132 6.043 <0.001 HS
The control drug provided highly significant relief( p<0.001) in all the symptoms
especially in management of udarashoola and vamana by 75% and 69.50% respectively.
The other symptoms like utklesha, amlodgara, hrtdaha, and kantadaha also showed highly
significant relief by 52%, 56.52%, 50% and 45.8% respectively.

Results
119
Effect of control drug on Main symptoms:
Table no. 52 Effect of control drug on Main symptoms after follow up
Mean Lakshana BT AFU BT-
AFU
% SD(±) SE(±) t P Remarks
Utklesha 1.72 1.48 0.24 24.00 0.435 0.087 2.752 <0.020 MS
Amlodgara 1.52 1.217 0.304 30.43 0.470 0.098 3.098 <0.010 MS
Hrtdaha 1.54 1.22 0.318 31.81 0.476 0.101 3.128 <0.010 MS
Kanthadaha 1.33 0.96 0.32 32.00 0.476 0.095 3.360 <0.010 MS
Udarashoola 1.50 1.12 0.375 37.50 0.499 0.101 3.714 <0.010 MS
Vanti 1.78 1.47 0.347 34.78 0.486 0.101 3.417 <0.010 MS
The control drug provided moderately significant relief(p<0.010) in the management of
amlodgara, hrtdaha, kantadaha,vamana and udarashoola by 30.43%, 31.85%, 32%,
34.78% and 37.5.% respectively. It provided moderately significant relief (p<0.020) in
the management of utklesha by 24%.
Effect of Trial drug on Associated symptoms:
Table no. 53 Effect of Trial drug on Associated symptoms after Treatment
Mean Lakshana BT AT BT-
AT
% SD (±)
SE (±)
t P Remarks
Avipaka 1.761 0.809 0.952 95.23 0.316 0.069 14.49 <0.001 HS
Klama 1.428 0.174 0.714 71.42 0.662 0.177 4.836 <0.001 HS
Tiktodgara 1.230 0.615 0.615 61.53 0.506 0.140 4.37 <0.001 HS
Gourava 1.312 0.750 0.562 56.25 0.512 0.128 4.38 <0.001 HS
Aruchi 1.388 0.833 0.555 55.55 0.607 0.143 4.265 <0.001 HS
Gurukoshtatha 1.411 0.823 0.588 58.82 0.685 0.166 4.237 <0.001 HS
Adhamana 1.473 0.684 0.789 78.94 0.567 0.130 6.871 <0.001 HS
Antrakujana 1.125 0.375 0.750 75.00 0.462 0.163 4.582 <0.001 HS
Sirasula 1.500 0.858 0.642 64.20 0.633 0.169 3.792 <0.001 HS

Results
120
The trial drug provided a highly significant relief(p<0.001) in the management of
avipaka, adhamana, antrakujana, klama, tiktodgara, gurukoshtata, gourava and aruchi by
95.323%; 78.94%; 75%; 71.42%; 61.53% 58.82% 56.25% and 55.55% respectively.
The trial drug provided moderately significant relief(p<0.010) in the management of
shiroruja by 64.2%.
Effect of Trial drug on Associated symptoms:
Table no. 54 Effect of Trial drug on Associated symptoms after follow up
Mean Lakshana BT AFU BT-
AFU
% SD(±) SE(±) t P Remarks
Avipaka 1.761 1.237 0.523 52.38 0.511 0.111 4.656 <0.001 HS
Klama 1.428 1.070 0.357 35.71 0.497 0.132 2.686 <0.050 Mi.S
Tiktodgara 1.230 0.768 0.461 46.15 0.660 0.183 2.938 <0.020 MS
Gourava 1.312 0.937 0.375 37.50 0.500 0.125 3.000 <0.010 MS
Aruchi 1.388 0.888 0.500 50.00 0.511 0.120 3.684 <0.001 HS
Gurukoshtatha 1.411 0.881 0.529 52.94 0.701 0.170 3.800 <0.001 HS
Adhamana 1.473 1.052 0.421 42.10 0.611 0.140 3.370 <0.010 MS
Antrakujana 1.125 0.750 0.375 37.50 0.517 0.182 2.049 >0.050 NS
Sirasula 1.500 1.215 0.285 28.50 0.468 0.125 2.274 <0.020 MS
The trial drug provided a highly significant relief(p<0.001)in the management of avipaka,
aruchi and gurukoshtata by 52.38%, 5 0% and 52.94% respectively after follow up.
The Trial drug provided moderately significant relief(p<0.010) in the management of
adhmana and gourava by 42.10% and 37.5% respectively.
The Trial drug provided moderately significant relief(p<0.020) in the management of
tiktodgara and shiroruja by 46.15% and 28.5% respectively.

Results
121
The Trial drug provided mild significant relief (p<0.050) in the management of
klama by 35.17%.
The Trial drug provided no significant relief (p>0.050) in the management of
antrakujana by 37.5%.
Effect of Control drug on Associated symptoms:
Table no. 55 Effect of Control drug on Associated symptoms after Treatment
Mean Lakshana BT AT BT-
AT
% SD(±) SE(±) t P Remarks
Avipaka 1.530 0.860 0.666 66.66 0.487 0.125 5.286 <0.001 HS
Klama 1.280 0.780 0.500 50.00 0.518 0.138 3.605 <0.010 MS
Tiktodgara 1.187 0.687 0.500 50.00 0.516 0.129 3.872 <0.001 HS
Gourava 1.166 0.583 0.583 58.30 0.514 0.148 3.922 <0.001 HS
Aruchi 1.312 0.625 0.687 68.75 0.478 0.119 5.744 <0.001 HS
Gurukoshtatha 1.230 0.769 0.461 46.10 0.518 0.143 3.203 <0.010 MS
Adhamana 1.437 0.937 0.500 50.00 0.516 0.129 3.872 <0.001 HS
Antrakujana 1.000 0.700 0.300 30.00 0.483 0.152 1.963 >0.050 NS
Sirasula 1.470 0.764 0.705 70.58 0.469 0.113 6.189 <0.001 HS
The control drug provided highly significant relief (p<0.001) in the management
of shiroruja, aruchi, avipaka, gourava, tiktodgara and adhmana by 70.58%, 68.75%,
66.66%, 58.30%, 50% and 15% respectively.
The control drug provided moderately significant relief (p<0.010) in the
management of klama and gurukostata by 50% and 46.10% respectively.
The control drug provided no significant relief (p>0.050) in the management of
antrakujana by 30%.

Results
122
Effect of Control drug on Associated symptoms:
Table no. 56 Effect of Control drug on Associated symptoms after follow up
Mean Lakshana BT AFU BT-
AFU
% SD(±) SE(±) t P Remarks
Avipaka 1.530 1.197 0.333 33.33 0.487 0.125 2.643 <0.020 MS
Klama 1.280 1.066 0.214 21.42 0.425 0.113 1.880 >0.050 NS
Tiktodgara 1.187 0.937 0.250 25.00 0.447 0.111 2.230 <0.050 MS
Gourava 1.166 1.000 0.166 16.66 0.389 0.112 1.482 >0.050 NS
Aruchi 1.312 1.124 0.187 18.75 0.403 0.100 1.860 >0.050 NS
Gurukoshtatha 1.230 1.154 0.760 07.60 0.277 0.076 0.988 <0.001 HS
Adhamana 1.437 1.312 0.125 12.50 0.341 0.085 1.463 >0.050 NS
Antrakujana 1.000 0.900 0.100 10.00 0.316 0.100 1.000 >0.050 NS
Sirasula 1.470 1.352 0.117 11.76 0.332 0.080 1.460 >0.050 NS
The control drug provided highly significant relief (p<0.001) in the management
of gurukostata by 7.6% after follow up.
The control drug provided moderately significant relief (p<0.020) in the
management of avipaka by 33.33% after follow up.
The control drug provided mild significant relief (p<0.050) in the management of
tiktodgara by 25% after follow up.
The control drug provided no significant relief (p>0.050) in the management of
klama, gourava, aruchi, adhmana, antrakujana and shiroruja by 21.42%, 16.16%, 18.15%,
12.5%, 10% and 11.76% respectively after follow up.

Results
123
Effect of Trial drug on Srotodusti:
Table no. 57 Effect of Trial drug on Srotodusti after Treatment
Mean Srotas BT AT BT-
AT
% SD(±) SE(±) T P Remarks
Annavaha 1.633 0.766 0.866 86.66 0.490 0.089 10.795 <0.001 HS
Rasavaha 1.933 1.100 0.833 83.33 0.520 0.095 9.811 <0.001 HS
Pureeshavaha 1.615 0.884 0.730 73.07 0.688 0.134 6.837 <0.001 HS
The Trial drug provided highly significant relief (p<0.001) in the management of
annavaha srotodusti, rasavaha srotodusti and pureeshavaha srotodusti by 86.66%,
83.33%and 73.07% respectively.
In total the effect of trial drug on the srotodusti involved in the amlapitta is highly
significant.
Effect of Trial drug on Srotodusti:
Table no. 58 Effect of Trial drug on Srotodusti after follow up
Mean Srotas BT AFU BT-AFU
% SD(±) SE(±) t P Remarks
Annavaha 1.633 1.067 0.566 56.66 0.773 0.141 5.421 <0.001 HS
Rasavaha 1.933 1.466 0.466 46.66 0.678 0.123 4.566 <0.001 HS
Pureeshavaha 1.615 0.999 0.615 61.33 0.496 0.097 6.320 <0.001 HS
The Trial drug provided highly significant relief (p<0.001) in the management of
annavaha srotodusti, rasavaha srotodusti and pureeshavaha srotodusti by 56.66%, 46.66%
and 61.53% respectively.

Results
124
Effect of Control drug on Srotodusti:
Table no. 59 Effect of Control drug on Srotodusti after Treatment
Mean Srotas BT AT BT-
AT
% SD(±) SE(±) t P Remarks
Annavaha 1.733 1.200 0.533 53.33 0.568 0.103 5.454 <0.001 HS
Rasavaha 1.866 1.100 0.766 76.66 0.718 0.131 7.875 <0.001 HS
Pureeshavaha 1.586 1.034 0.551 55.17 0.568 0.105 5.555 <0.001 HS
The control drug provided highly significant relief (p<0.001) in the management
of annavaha srotodusti, rasavaha srotodusti and pureeshavaha srotodusti by 53.33%,
76.66%and 55.17% respectively.
Effect of control drug on Srotodusti:
Table no. 60 Effect of control drug on Srotodusti after follow up
Mean Srotas BT AFU BT-
AFU
% SD(±) SE(±) t P Remarks
Annavaha 1.733 1.633 0.100 10.00 0.434 0.079 1.677 >0.050 NS
Rasavaha 1.866 1.732 0.133 13.33 0.345 0.063 2.106 <0.050 Mi.S
Pureeshavaha 1.586 1.448 0.137 13.79 0.724 0.134 0.765 >0.050 NS
The control drug provided mild significant relief (p<0.050) in the management of
rasavaha srotodusti by 13.33%.
The control drug provided no significant relief (p>0.050) in the management of
annavaha srotodusti and pureeshavaha srotodusti by 10% and 13.79% respectively.

Results
125
Total effect of Trial drug and Control drug After treatment:
Table no.61
Trial drug Control drug Results No. of patients % No. of patients %
Complete relief 00 00 00 00 Marked improvement 11 36.66 4 13.33 Improved 14 46.66 15 50.00 Controlled 5 16.66 11 36.66 Unchanged 00 00 00 00
In the trial group 46.66% of patients showed improved effect where in there was
50% to 75% relief in the symptoms. 36.66% of the patients showed marked improvement
in the condition by more than 75% relief. 16.66% of the patients showed control effect of
the drug by 25% to 50% of the result in the symptoms.
In the control group 50% of patients showed improved effect where in there was
50% to 75% relief in the symptoms. 36.66% of the patients showed control effect in the
condition by 25% to 50%% relief. 13.33% of the patients showed marked improvement
in the condition by more than 75% relief in the symptoms.
Total effect of Trial drug and Control drug After follow up:
Table no.62
Trial drug Control drug Results No. of patients % No. of patients %
Complete relief 00 00 00 00 Marked improvement 02 6.66 00 00 Improved 10 33.33 4 13.33 Controlled 17 56.66 22 73.33 Unchanged 1 3.33 4 13.33
After the follow up in the trial group 56.66% of patients showed controlled effect
where in there was 25% to 50% relief in the symptoms. 33.33% of the patients showed
improved effect by 50% to 75% relief. 6.66% of the patients showed marked

Results
126
0
20
40
60
80
Utk
lesh
a
Am
lodg
ara
Hrtd
aha
Kan
thad
aha
Uda
rash
oola
Van
tiTrial drug
Control drug
improvement in the condition by more than 75% relief. Only 3.33% of patients showed
no change in any of the complaints.
After the follow up in the control group 73.33% of patients showed controlled
effect where in there was 25% to 50% relief in the symptoms. 13.33% of the patients
showed improved effect by 50% to 75% relief. 13.33% of the patients showed no change
in any of the complaints.
Graph No.37
Showing comparative effect of therapies on main symptoms after the treatment
The trial drug showed highly significant relief (p<0.001) in all the symptoms
especially amlogdara and hritdaha by 78.07% and 72.77% respectively. While the control
drug also showed highly significant in all the symptoms especially in udarashoola and
vamana by 75% and 69.05% respectively.
Though there was highly significant relief in all the other symptoms also. But in
trial group the percentage of relief was higher when compared to the control group.

Results
127
0102030405060
Utk
lesh
a
Am
lodg
ara
Hrtd
aha
Kan
thad
aha
Uda
rash
oola
Van
ti
Trial drug
Control drug
Graph No.38
Showing comparative effect of therapies on main symptoms after follow up
In the trial drug after follow up there was highly significant relief (p<0.001) in
udarashoola and amlogdara by 54.16% and 40.74% respectively; where as in the control
group it showed moderate significant relief by 37.5% and 30.43% respectively.
In hritdaha, vamana and utklesha, the trial group showed moderately significant
relief 33.33%, 37.5% and 25.92% respectively; where as in the control group it showed it
showed same result by 31.81%, 34.78% and 24% respectively.
In kantadaha the trial drug showed mild significant relief by 27.77%, where as
control drug provided moderately significant relief by 32%.

Results
128
020406080
100
Avi
paka
Klam
a
Tikt
odga
ra
Gou
rava
Aru
chi
Gur
ukos
htat
ha
Adh
aman
a
Ant
raku
jana
Sira
sula
Trial drug
Conrol drug
Graph No.39
Showing comparative effect of therapies on associated symptoms after the treatment
The trial drug showed highly significant relief in avipaka, adhmana, tiktodgara,
gourava and aruchi by 95.23%, 78.94%, 61.53%, 56.25% and 55.5% respectively. Where
as in the control group also showed the same result in these symptoms by 68.75%, 50%,
58.30%, 66.66% and 50% respectively.
In klama and gurukostata the trial drug showed highly significant relief by
71.42% and 61.52% respectively; where as in control group showed moderately
significant relief by 50% and 46.10% respectively.
In shiroruja the trial group showed moderately significant relief by 64.2%, where
as in control group it provided highly significant relief by 70.58%.
In antrakujana the trial group showed highly significant relief by 75%, where as
the control group showed no relief.

Results
129
0102030405060
Avi
paka
Klam
a
Tikt
odga
ra
Gou
rava
Aru
chi
Gur
ukos
htat
ha
Adh
aman
a
Ant
raku
jana
Sira
sula
Trial drug
Control drug
Graph No.40
Showing comparative effect of therapies on associated symptoms after follow up
In gurukostata there was highly significant relief by 52.94% in trial group, where
as in control group also showed same result by 7.6%.
In avipaka there was highly significant relief in the trial group by 52.38%, where
as in control group there was moderately significant relief by 33.33%.
In aruchi there was highly significant relief in the trial group by 50%, where as in
control group there was no significant relief by 18.15%.
In tiktodgara there was moderately significant relief in the trial group by 46.15%,
where as in control group there was mild significant relief by 25%.
In klama there was mild significant relief in the trial group by 35.71%, where as
in control group there was no significant change.
In adhmana and gourava there was moderately significant relief in the trial group
by 42.10% and 37.5% respectively, where as in control group there was no significant
change.
There was no significant change in antrakujana in both the groups.

Results
130
0
20
40
60
80
100
Annavaha Rasavaha Pureeshavaha
Trial drugControl drug
0
20
40
60
80
Annavaha Rasavaha Pureeshavaha
Trial drugControl drug
Graph No.41
Showing comparative effect of therapies on srotodusti after the treatment
In annavaha srotodusti, rasavaha srotodusti and pureeshavaha srotodusti the trial
group showed highly significant relief by 86.66%, 83.33% and 73.07% respectively.
Where as in control group also showed the same result by 53.33%, 76.66% and 55.17%
respectively.
Graph No.42
Showing comparative effect of therapies on srotodusti after follow up

Results
131
0
10
20
30
40
50
Com
plet
ere
lief
Mar
ked
impr
ovem
ent
Impr
oved
Cont
rolle
d
Unch
ange
d
Trial drug
Control drug
After follow up also there was highly significant relief in annavaha srotodusti,
rasavaha srotodusti and pureeshavaha srotodusti in trial group by 56.66%, 46.66% and
61.53% respectively. Where as in control group there was mild significant relief in
rasavaha srotodusti by 13.33%, but no significant change in annavaha srotodusti and
pureeshavaha srotodusti.
Graph No.43
Showing comparative total effect of therapies after treatment
The trial drug group was found to be more effective than the control drug group
after the treatment.
In the trial group 36.66% of the patients showed marked improved, while only
13.33% of patients showed the same in control group.
The trial group showed 46.66% of the patients with improved effect, where as
50% of patients in control group with same effect.
The trial group showed 16.66% of the patients with controlled effect, where as
36.66% of patients in control group with same effect.
The trial group showed unchanged cases where as the control group showed
unchanged effect in 3.33% of patients.

Results
132
01020304050607080
Com
plet
ere
lief
Mar
ked
impr
ovem
ent
Impr
oved
Cont
rolle
d
Unch
ange
d
Trial drug
Control drug
Graph No.44
Showing comparative total effect of therapies after follow up
After follow up the trial drug group was found to be more effective than the
control group.
The trial group showed 6.66% of patients with marked improved where as in the
control group there was no such improvement.
The trial group showed 33.33% of patients with improved effect where as in the
control group it was 13.33%.
The trial group showed 56.66% of patients with controlled effect where as in the
control group it was 73.33%.
The trial group showed 3.33% of patients with unchanged effect where as in the
control group it was 13.33%.
From the above it can be observed that the trial drug showed maximum cases to
be markedly improved, improved and no unchanged cases, where as the control group
showed maximum cases to be improved and having control effect after the treatment.
Even after follow up the trial group shows maximum cases to be markedly
improved and improved when compared to control group. The trial group also shows
minimal cases to be unchanged when compared to control group after follow up.
The control group shows maximum cases to be controlled than in the trial group,
but the improved and markedly improved cases are found to be more in trial group.
Hence it can be concluded that the trial drug provided better result than the control drug.

Discussion
133
DISCUSSION
Amlapitta is a psycho-somatic disease of annavaha srotas mainly caused due to
indulgence in faulty diet and regimen. It presents a group of signs and symptoms viz.,
avipaka, amlodgara, hrtdaha, kantadaha utklesha, vamana, udaarashoola, adhmana
vitbheda etc. which are more commonly termed as dyspeptic signs in the modern
medicine.
Amlapitta is stated to be a disorder manifested due to agnimandya leading to the
formation of ama. Inturn the ama combining with the vrudhpitta leads to the formation of
amavisha which turns into shuktapaka and manifests clinically. This disorder is stated to
be caused due to dusti occurring in the annavaha srotas first and involving the rasavaha
and pureeshavaha srotas. From the samprapti explained it is clear that Amlapitta is the
result of functional disturbance of the annavaha srotas, especially during the
amlaavastapaka where in the food in taken turns to shuktapaka due to agnimandya and
ama. This can be compared to non ulcer dyspepsia or functional dyspepsia in the modern
medicine as most of the symptoms seen in Amlapitta are similar to it and more over non-
ulcer dyspepsia is said to be characterized by dyspeptic signs caused due to functional
disturbance with no organic lesions any where in GIT.
Amlapitta is most commonest disease met with in general practice requiring an
adequate and proper management as it hampers the daily routine of an individual.
Madhavakara states that Amlapitta is a condition which and when promptly
treated along with proper diet and regimen can be easily cured. If it is neglected and one
indulgence himself in apathya ahara vihara it becomes kastasadhya.

Discussion
134
The patients of Amlapitta were randomly selected irrespective of sex fulfilling the
inclusion and exclusion criteria. Freshly diagnosed cases and cases of recent origin were
selected for the study. The main symptoms of the disease were graded and scored for the
assessment. Along with this the associated symptoms and srotodusti were also graded and
scored for the assessment. The cases with chronic and acute onset were ruled out for
ulcers before including into the study by Endoscopy. The general condition of the patient
was also assessed by detailed history and routine bio-chemical investigations for other
diseases so as to fulfill the inclusion criteria. The patients were grouped randomly and
controlled study was carried out. Patients under the trial group received Shatavari churna
-3gms and Abhraka bhasma 125mg along with litte ghrita before meals thrice daily for 1
month and the patients under control group received Syrup Gelusil 1 tsp. thrice daily
before meals for 1 month. The result was assessed by statistical analysis of the symptoms
that was graded and scored.
Nidanatmaka aspect of the disease:
Age:
Most of the patients belonged to age group of 26-33 yrs of age followed by 34-41
yrs of age group. This findings shows a very similar statistics about prevalence of non-
ulcer dyspepsia in the middle age group.
Sex :
Majority of the patients were females which is similar to the incidence of Non-
Ulcer dyspepsia described in modern medicine.
3] Religion :
The disease incidence was quite more in Hindus this may be due to the demographic
cause or distribution of the patients.

Discussion
135
4] Marital status :
More of the married individuals showed the presence of the disease. As this
condition is more common in the middle age group, the presence of Amlapitta is more in
the married group. The life is more stressfull during the middle age due to greater
responsibilities both physically and mentally; which becomes one of the cause for the
manifestation of the amlapitta.
5] Educational Status :
Amlapitta was found to be more in graduates and the people who had completed
higher secondary schooling. In this phase the mental stress and strain is found to be more
along with improper food habits which becomes the causative factor for the clinical
manifestation of the disease.
6] Occupational status :
The disease incidence was found to be highest in house wives followed by
businessmen which indicated the sedentary life style and food habits which are more in
these individuals to be the causative factors.
7] Diet :
a) Type: The incidence of mixed diet was more ; which highlights that intake of
excessive fatty and spicy foods leads to the manifestation of the disease.
b) Habit :Majority of the patients were accustomed to vishama shana [untimely
intake of food] which is also the cause for the manifestation of the disease.
c) Nature of diet :Majority of the patients had pittaprakopaka ahara, amla rasa
pradhana, and virudhanna which are also the cause for the vriddhi of pitta leading to the
manifestation of the disease.

Discussion
136
8] Socio – Economic status :
More number of patients belonged to middle class which especially states the
stressfull physical and mental condition and faulty diet which may be the cause for the
disease.
9] Addictions :
Majority of the patients were addicted to coffee and tea followed by smoking and
NSAID’s , which are also considered as one of the causative factors in modern medicine
for Non-ulcer dyspepsia.
10] Habitat :
Majority of the patients belonged to the rural area which indicates the improper
dietic habits and regimen leading to Amlapitta.
11] Aggravating period :
The i `ncidence of aggravation of the symptoms was found to be more during
mid-day and morning hours which indicates the pittaprakopaka and increase ama avastha
phases respectively giving rise to the symptoms.
12] Influence of environmental factors :
The incidence of aggravation of the symptoms was found to be higher in rainy
season which indicates that the pittaprakopaka kala is one of the causative factor.
13] Psychological factors : The incidence of mental stress or strain was found to be
more in the majority of patient which clearly indicates that psychological factor has
greater influence over the manifestation of the disease.
14] Regimen :
Majority of the patients gave a history of atapsevana, avagahana which are said to
the causative factors influencing pitta leading to the disease entity.
15 Rasa- satmya :

Discussion
137
The disease incidence was found to be more in the patients with katu-rasa satmya
and Amla-rasa-satmya, which has been stated to be the cause for the manifestation of the
disease.
16] Prakruti :
The disease incidence was found to be highest in pitta-vataja prakruti indicating
that the prakruti also has influence over the manifestation of the disease.
17] Sara :
Majority of the patients belonged to mamsa sara and twak sara individuals.
18] Samhanana :
Majority of the patients belonged to madhyama samhanana.
19] Satva :
Majority of the patients belonged to madhyama satva.
20] Agni :
Majority of the patients having mandagni showed the higher incidence of the
disease which indicates the pathogeness of the diesese.
21] Koshta :
The incidence of the disease was found to be higher in madhyama koshta people,
indicating the vata-pitta influence in the manifestation of the disease.
22] Desha :
The incidence of the disease was found to be higher in the subjects belonging to
Anoopa pradesha which is said to be having influence over the pitta and its aggravation
leading to the disease.
23] Bala :
Majority of the patients of the present study had madhyama bala and pravara bala,
indicating the loss of bala due to improper digestion and assimilation of nourishment.
24] Exercise :

Discussion
138
The incidence of the disease was found to be more in people who did only routine
work and occasional exercise, indicating the sedentary or less physical work leading to
agnimandya and hence the disease.
25] Bowel Habit :
The incidence of the disease is high in the patients with constipation and irregular
bowel habit which indicates the influence of vata and pitas over the pureeshavaha srotas.
26] Past Illness :
Majority of the patients gave a history of agnimandya and ajeerna which are the
important factors involved in the samprapti of the disease.
Effect of therapies on Utklesha [Nausea]:
In trial group 95% of patients presented with mild to severe degree of utlklesha
[Nausea] and showed highly significant relief by59.85% after treatment and moderately
significant relief even after follow-up by 25.92%
The control drug group showed highly significant relief by 52% after treatment
and moderately significant relief even after follow-up by 24%.
This indicates that the trial drug has better effect on the symptom utklesha.
The Shatavari choorna and Abhraka Bhasma both are tridoshagna and have
madhura rasa, madhura vipaka and sheeta veerya which will pacity the pitta which is the
cause for utklesha along with vriddh kapha. The tikta rasa of the shatavari choorna will
pacity the kapha, which is anubandha dosha in this symptom.
Effect of therapies on Amlodgara [Acid Erructations]:
In trial group 95% of patients presented with mild to severe degree of
Amlodgara [Acid erructations] and showed highly significant relief by 73.07% after the
treatment and even after follow-up also it showed highly significant relief by 40.74%.
The control drug group showed highly significant relief by 56.52% after treatment
and moderately significant relief by 30.43% after the follow up.

Discussion
139
This indicates that the trial drug has better effect on the amlodgara.
The madhura and tikta rasa of Shatavari choorna and madhura rasa of Abhraka
Bhasma and madhura vipaka and sheeta veerya of both the drug pacify the pitta and
reduces the udrikta pitta which is cause for amlodgara. As both drugs have deepana
property they increase the agni and reduce the ama.
Effect of therapies on Hrthdaha [Heart burn]:
Hrthdaha or in other words known as pysosis is caused due to the reflux of the
pitta in to the upper part of the G.I.T. This was assessed by grading and scoring the
symptom.
In trial group 95% of patients presented with mild to severe degree of hrtdatha
[Burning behind the sternum] and showed highly significant relief by 72.77% after the
treatment and after follow-up showed moderately significant relief by 33.33%.
In the control group 73% of patients presented with mild to severe degree of
hrtdaha and showed highly significant relief by 50% and after follow-up showed
moderately significant relief by 31.81%.
This clearly indicates that the trial drug is more effective than the control drug
over Hrtdaha.
Shatavari choorna and Abhraka bhasma both due to their madhura rasa, madhura
vipaka and sheeta veerya pacify the pitta and reduces the daha produced in the
hrtpradesha. Shatavari choorna due to its demulscent property reduces the burning
sensation.
Effect of therapies on Kantdaha : [Burning sensation in the throat]:
This symptom is often associated with the Hrtdaha. Due to the regurgitation of the
gastric contents into the mouth.
In trial group 60% of patients presented with mild to severe degree of kantdaha
and showed highly significant relief by 61.11% after the treatment and mild significant
relief by 27.77% after follow-up.

Discussion
140
In control group 80% of patients presented with mild to moderate degree of
kantadaha and showed highly significant relief by 45.8% after the treatment and
moderately significant relief by 32% after follow-up. This indicates that the trial drug is
better after the treatment where as the control drug showed a sustained relief even after
follow-up.
Shatavari choorna due to its demulscent action decreased the kantadaha and due
to its madhura rasa, madhura vipaka and sheeta veerya along with the same of the
Abhraka Bhasma reduced the daha by pacifying the pitta.
Effect of therapies on Vamana : [Vomiting]:
Vamana occuss due to the co-mixture of ama along with pitta and its regurgitation
into the upper part of the G.I.T. by vata. The symptom was graded and scored for the
purpose of assessment.
In trial group 53% of patients presented with mild to severe degree of vamana
[vomiting] and showed highly significant relief by 50% after the treatment and
moderately significant relief by 25.92% after the follow-up.
In control group 77% of patients presented with mild to severe degree of vamana
and showed highly significant relief by 69.50% after treatment and moderately significant
relief by 34.78% after follow-up.
This indicates that the control drug had better effect over vamana than trial drug.
The trial drug Shatavari choorna and Abhraka Bhasma, especially helps in
pacifying the pitta and due to its deepana property reduces ama.
Effect of therapies on Udara shoola : [Abdominal pain]:
The pain is characteristic of vata and hence its seen when pitta is associated with vata.
In trial group 80% of patients presented with mild to severe degree of udara
shoola [Abdominal pain] and showed highly significant relief by 62.5% after the
treatment and the same relief by 54.16% even after the follow-up.

Discussion
141
In control group 80% of patients presented with mild to severe degree of udara
shoola and showed highly significant relief by 75% after the treatment and moderately
significant relief by 37.5% even after the follow-up.
Though the control drug showed a greater percentage of relief than the trial drug
after the treatment the trial drug had a greater and sustained effect after follow-up.
Shatavari choorna due to its vata pitta shamana property and Abhraka Bhasma
due to its tridoshagna property pacifies both vata and pitta and reduces the pain. Shatavari
choorna is said to have stomachic action due to its bitter taste. Along with this it has
demulscent, and anti-spasmodic action.
Effect of therapies on Avipaka : [Indigestion] :
In trial group 70% of patients presented with mild to severe degree of Avipaka
and showed highly significant relief by 95.23% after the treatment and even after the
follow-up by 52.38%.
In control group 50% of patients presented with the Avipaka and showed highly
significant relief by 66.66% after the treatment and moderately significant relief by
33.33% after follow-up.
This indicates that the trial drug has better effect over Avipaka than the control
drug.
Shatavari choorna, Abhraka Bhasma and Gritha, due to their deepana property
increases the agni and reduce the avipaka. Gritha due to its sneha guna pacifies the vata
and stimulates the Jataragni.
Effect of therapies on Klama : [Fatigue]
In trial group 47% of patients presented with klama which varied from mild to
severe degree and showed highly significant relief by 71.42% after the treatment and
mild significant relief by 35.71% after the follow-up.

Discussion
142
In control group 47% of patients presented with klama which varied from mild to
severe degree and showed moderately significant relief by 50% after the treatment and no
significant relief by 21.42% after the follow-up.
This indicates that the trial drug is more effective over klama than the control
drug.
Both Shatavari choorna and Abhraka Bhasma due to thir madhura rasa, madhura
vipaka and sheeta veerya pacify the pitta and due to their deepana property reduce the
ama, and hence reduces the klama. Which is seen due to ama and pitta.
Effect of therapies on Tiktodgara :
In trial group 43% of patients presented with tiktodgara which varied from mild
to severe degree and showed highly significant by 61.53% after the treatment and
moderately significant relief by 46.15% after the follow-up.
In control group 53% patients presented with tiktodgara and showed highly
significant relief by 50% after treatment and mild significant relief by 25% after
followup.
The trial drug had better effect over the Tiktodgara than control drug.
The trial drug due to its madhura rasa, madhura vipkaka and sheeta veerya
pacified the pitta and reduced the Tiktodgara.
Effect of therapies on Gourava :
In trial group 53% of patients presented with mild to severe degree of Gourava
and showed a highly significant relief by 56.25 % after treatment and showed moderately
significant relief by 37.5 % after follow up.
In control group 40% of patients presented with mild to severe Gourava and
showed a highly significant relief by 66.66% after the treatment but no relief after follow
up by 16.16%.
From this it indicates the trial drug is more effective than the control drug even after
follow-up.

Discussion
143
The trial drugs due to their deepana property increased the jataragni and helped to
reduce the ama which is cause for the Gourava.
Effect of therapies on Aruchi : [Anorexia]:
Aruchi is mainly due to ama caused by agnimandya, which is one among
sampraptighatakas of this disease.
In trial group 60% of patients presented with mild to severe Aruchi [Anorexia]
and showed highly significant relief by 55.55% after the treatement and showed the same
result by 50% even after the follow up.
In control group 53% of patients presented with mild to severe Aruchi and
showed highly significant relief by 68.75% after the treatment and no relief after the
follow-up by 18.15%
This indicates that the control drug showed better results after treatment compared
to trial drug. But the trial drug showed better results after follow up.
The trial drug because of its deepana property increased jataragni and reduced
ama and in turn the Aruchi.
Effect of therapies on Gurukoshtata : [Abdominal discomfort]
Gurukoshtatha is mainly caused due to ama. Agnimandya is main cause of ama
which is one among the sampraptighatakas.
In trial group 57% of patients presented with mild to severe degree of guru
koshtata and showed highly significant relief by 58.82% after the treatment and eve after
the follow up the same effect by 52.94%.
In control group 43% of patients presented with mild to severe degree of
gurukoshtata and showed moderately significant relief by 46.10% after the treatment and
highly significant relief by 7.6% after follow up.

Discussion
144
This indicates that trial drug is more effective as it showed sustained effect even
after follow-up, where as the control drug showed the good effect after follow-up, but
only in small percentage of subjects.
The trial drug mainly because of its deepana property increase jataragni and helps
in reducing the ama and hence the gurukoshtata also,but takes time for reduction of the
ama.
Effect of therapies on Adhmana : [Abdominal Distension]
Ajeerna causes accumulation of vata in disacordance with pitta to produce
Adhmana.
In trial group 63% of patients presented with mild to severe degree of Adhmana
and showed highly significant relied by 78.94%, after the treatment and moderately
significant relief by 42.10% after the follow-up.
In control group 53% of patients presented with mild to severe degree of
Adhmana and showed highly significant relief by 50% after the treatment and no relief
after the follow-up by 12.5%.
This indicates that the trial drug had better effect over Adhmana than control
drug.
Shatavari choorna and Gritha because of their vata-pitta shamaka property
pacified vata and pitta and hence reduced ajeerna and in turn Adhmana.
Effect of therapies on Antrakujana :
Antrakujana is mainly caused due to vata vrudhi. In trial group 27% of patients
presented with mild to severe degree of Anrakujana and showed highly significant relief
by 75% after the treatment and no significant relief after follow-up by 37.5%.

Discussion
145
In control group 53% of patients presented with mild to severe degree of
Antrakujana and showed no significant relief after the treatment and follow-up by 30%
and10% respectively.
This indicates that the trial drug has better effect than the control drug over
Antrakujana.
Shatavari choorna due to its property of vata-pitta shamana pacified the vata and
pitta and gritha due to its sneha guna pacified the vata and reduced Antrakujana.
Effect of therapies on Shiroruja : [Headache]
In trial – group 47% of patients presented with mild to severe degree of shiroruja
[Headache] and showed moderately significant relief by 64.2% after the treatment and
the same result after follow up by 28.5%
In control group 57% of patients presented with mild to severe degree of
shiroruja and showed highly significant relief by 70.58% after the treatment and no
significant relief after the follow-up by 11.76%
This indicates that trial drug has better effect than the control drug over shiroruja.
Shatavari choorna and Gritha due to their vata-pitta shyamaka property pacified vata and
pitta and reduced shiroruja.
Effect of therapies on Rasavaha srotodusti :
In trial group 40% of patients presented with mild to severe degree of resavaha
srotodusti and showed highly significant relief by 83.33% after the treatment and the
same result even after the follow-up by 46.66%.

Discussion
146
In control group 30% of patients presented with mild to severe degree of
rasavaha srotodusti and showed highly significant relief by 76.66% after the treatment
and mild significant relef by 13.33%.
This indicates that the trial drug is more effective than the control drug.
Shatavari choorna and Abhraka bhasma due to their madhura rasa,madhura vipaka and
sheeta veerya pacify the pitta and vata and due to their deepana property reduce the ama
by increasing the agni and thus correct the srotodusti.
Effect of therapies over Annavaha Srotodusti :
In trial group 30% of patients presented with mild to severe degree of Annavaha
sratodusti and showed highly significant relief by 86.66% after treatment and the some
effect even after follow-up by 56.66%.
In control group 40% of patients presented with mild to severe degree of
Annavaha srotodusti and showed highly significant relief by 53.33% after treatment and
no significant relief after follow-up.
This indicates that the trial drug is more effective than the control drug.
The deepana property of the trial drug influences the agni and as a result there
may be reduction in features of annavaha srotodusti..
Effect of therapies on pureeshavaha srotodusti.
In the trial drug 30% of patients present with mild to severe degree of
pureeshavaha srotodusti and showed highly significant relief by 73.07% after the
treatment and the same effect even after the follow up by 61.53%.

Discussion
147
In the control drug 30% of patients presented with mild to severe degree of
pureeshavaha srotodusti and showed highly significant relief after follow-up by 13.79%.
This indicates the trial drug had better effect than the control drug over
pureeshavaha srotodusti.
The vata pitta shamaka property of the trial drug counteracted the vata-pitta dushti
and hence lead to the reduction in the dusti of pureeshavaha srotas.
Total effect of therapies:
The trial drug showed maximum cases to be markedly improved, improved and
no unchanged cases, where as the control group showed maximum cases to be improved
and having control effect after the treatment.
Even after follow up the trial group shows maximum cases to be markedly
improved and improved when compared to control group. The trial group also shows
minimal cases to be unchanged when compared to control group after follow up.
The control group shows maximum cases to be controlled than in the trial group,
but the improved and markedly improved cases are found to be more in trial group.
Hence it can be concluded that the trial drug provided better result than the control drug.

Conclusion
148
CONCLUSION
The work entitled “A clinical study on the effect of Shatavari choorna with Abhraka
Bhasma in the management of Amlapitta” draws out following conclusions.
1. Amlapitta is a psycho-somatic disorder, where psychological factors play an equally
important factor along with the dietary indiscretions.
2. Amlodgara, Hrtdaha and Utklesha are inevitable manifestations of Amlapitta.
3. Pitta is the pradhana dosha, but the predominance/ aggravation of vata causes
undarashoola along with other Amlapitta symptoms, as such its not found in all
patients.
4. Agnimandya, Ama and Srotodusti are the prime factors in the manifestation of the
Amlapitta, the same can be considered in the manifestation of Non-Ulcer-Dyspepsia.
5. Amlapitta is a functional disorder caused due to the vikruti in the amlavastha paka
during the processes of digestion and involves no organic lesions as the pathogenesis
does not specify.
6. Poorvarupa of the Amlapitta has not been stated in the classics but most of the
patients give a history of Ajeerna and Agnimandya which can be considered as
poorvarupa or pre-disposing factors of Amlapitta.
7. Amlapitta if becomes chronic and the vitiation of the doshas lead to other conditions
like annadravashoola, parinama shoola etc.
8. Jwara, Atisara, Grahani, the upadravas of the Amlapitta states that severity of
agnidushti.
9. Its observed that most of the patients present mainly the urdhwaga amlapitta laxanas
along with samanya lakshanas.

Conclusion
149
10. Pathyapthya plays definate role in the management of Amlapitta.
11. The overall effect of the trial drug with proper diet and regimen was more significant
and better than the effect of the control drug after treatment and even follow-up.
12. The trial drug showed marked improvement in the srotodusti especially in the
annavaha srotodusti and pureeshavaha srotodusti after the follow-up also.
13. The standard drug showed significant relief in the symptoms during the treatment, but
during the follow-up, the recurrence rate was high.
14. Abhraka Bhasma acts as an Antacid and helps in neutralizing the HCl and thus giving
an instant relief.
15. Abhraka Bhasma and Shatavari choorna along with Gritha act synergistically to bring
about quick and better effect in the management of Amlapitta, than an liquid antacid.
16. No any side effects or adverse effects were observed during the study.
17. To get still more precise data the study must be carried out over a larger population
with more number of patients. The total duration of the study was only 2 months. In 2
months its not possible to evaluate all the effects and adverse effect if any of drug.. A
long term study must be conducted to know the effect of the drug in long – run.
18. Similar studies can be under taken by taking single drugs or simple combinations of
one or two herbal and mineral drugs to assess their efficacy in management of
Amlapitta.
19. As shodhana treatment gives better results, it will be ideal to follow shamana after
shodhana therapy.

Summary
150
SUMMARY
The dissertation titled “A clinical study on the effect of Shatavari choorna with
Abhraka Bahasma in the management of Amlapitta” compraises of different topics
discussed under these headings.
1. Introduction :
This comprises of the introduction to the Ayurveda, its aim and objectives and the
importance of kayachikitsa with respect to Angi. It also includes brief introduction of the
disease Amlapitta, along with its incidence, prevalence, pathology, and its paralance with
functional / Non-Ulcer Dyspepsia, in the modern medicine. The aim of the study and
selection of the drug has been putforth.
2. Objectives :
The main aim and objectives of the study has been mentioned along with the
hypothesis under this heading.
3. Review of the literature :
This section includes the collection of all the available data regarding the
etymology, definition, classification- nidana, poorvarupa, rupa, samprapti, sadhya
asadhyata, upadravas, and chikitsa along with pathyapataya of the disease Amlapitta. It
also includes a detailed description of the Dyspepsia, highlighting functional / Non-Ulcer
Dyspepsia in the modern medicine to draw its paralance to Amlapitta.
4. Materials and methods :
Clinical study :
Under this heading a detailed description of clinical study with specific reference
to patients, grouping, selection, inclusion and exclusion criteria, protocol criteria for

Summary
151
assessments of signs and symptoms, dose, duration, distribution of patients etc. of the
present study has been discussed.
5. Results :
Total of 32 patients in each group were selected for the present study and only 30
patients from each group continued the full course of the therapy.
Results of clinical study :
The results obtained after 30 days of treatment and 30 days of follow-up are
discussed under this heading. The scoring of the important features of Amlapitta before
and after the treatment and also follow-up are tabulated and percentage of improvement
is noted. The grading of the improvement is done and analyzed statistically with students
‘t’ test. The total relief obtained after the treatment schedule was recorded as:
1. Completely cured 2. Marked improvement
3. Improved 4. Controlled and
5. Unchanged.
The same was recorded even after the follow-up.
In present study no patients of either group got completely cured.
The trial group showed 36.66 % patients markedly relieved. 46.66 % of patients
to be improved, and 16.66 % of patients to be controlled. While the standard group
showed 13.33 % be markedly improved, 50 % of patients to be improved, 36.66 % of
patients to be controlled. After the follow up the trail drug showed more number of
patients to be markedly improved and improved in comparison with the control drug.
The percentage of controlled and unchanged were found to be more in the control group.

Summary
152
Thus the trial group showed better and significant result when compared to
controlled group.
6. Discussion :
Under this the nidanatmaka study and results obtained from this study have been
described. The probable mode of action of the trial drug Shatavari choorna,
Abhraka Bhasma and also gritha in the management of Amlapitta has been
discussed.
7. Conclusion :
In this chapter conclusion drawn from the above study has been highlighted along
with the limitation of the study and the scope for further improvisation.

REFERENCES
HISTORICAL GLIMPSES
1. Atharva veda kaushika sutra 31/7
2. Ch.Su.1/110.
3. Ch.Su. 25/40
4. Ch.Su. 26/43
5. Ch.Su 26/103
6. Ch.Su 12/52
7. Ch.Chi.15/47
8. Ch.Chi 7/148
9. Ch. Su. 20/14
10. Ch.Chi.12/52
11. Ash.San.Su.13/3
12. Kh.Sam.Khi.16
13. Ma.Ni.51
14. Bha.Pra.Ma.Kha.10
15. Sha.Sam.pra.Kha.1

NIRUKTI
1. Ch.Su 1/60
2. Ch.Su 1/60 ; Ch . Su 20/ 15 ; Kh . Su 27/38
3. Su. Su 21/1
4. Siddantha Kaumudi
5. Ch.Chi. 15/47 ; Chakrapani
6. M.Ni. 51/ Srikantadutta
7. M.Ni. 51/ Srikantadutta
8. Sanskrit dictionary Vachaspathyam [ P.333]
9. Su.Su. 46 / 504
10. Ch.Chi. 15/10
11. Sanskrit Dictionary Viswakor
12. Ch.Chi 15/10 Ckakrapani
13. Ka.Khi 16/7.8.9
14. M.Ni . 51/1
15. Ash. San 20/16 Indutika
16. Yogaratnakara, uttarardha Amlapitta Chikitsa/3
17. Kh.Khi . 16/42-43
18. Ash.San. Su. 20/16 Indutika
19. Ash. San. Su. 20/16
20. Ash.San.Su. 20/16 Indutika
21. Su.Su. 42/10 Dalhana

ANATO PHYSIOLOGY
1. Ch. Chi. 15/3 Chakrapani
2. Ch.Su . 11/48
3. Ch. Sha 7/10
4. Ch.Su. 20/8 Chakrapani
5. Su.Chi.2/11-12
6. Su Su.21/10 ;Su. Ut.40/169
7. Su.Su.21/13
8. Ch.Su.20/8 ;Ash.Hr.Su.12/2
9. Ch.Chi. !5/10
10. Ash.Hr.Su.12/10-12
11. Ch.Chi.5/9
12. Ch.Sha.3/6
13. Su.Sha.5/8
14. Ch.Sha.7/10
15. Ch.Su. 20/8 Chakrapani
16. Ch.Su. 20/8
17. Ch.Su. 5/8
18. Ch.Vi. 2/17
19. Su.Su. 21/12
20. D.M

21. Su.Su.4/37
22. Su.Sha.9/7
23. Su.Sha.5/32
24. D.M
AHARAPAKA
1. Ch.Sha6/14
2. Ch.Su 12/11
3. Ch.Su.12/11
4. Ch.Su.12/11 Chakrapani
5. Ch.Su.1/60
6. Su.Su.20/15
7. Ch.Su.1/60
8. Su.Su.21
9. Su.Su.21/13
10. Ch.Chi.15/9
11. Ch.Chi.15/9
12. Ch.Chi 15/10
13. Ch.Chi 15/10
14. Ch.Chi 15/10 Chakrapani
15. Su.Su.46/502
16. Ch.Chi.15/9 Chakrapani
17. Ch.Chi.15/9
18. Ch.Sha.2/18

NIDHANA :
1. PP. Ch. 36
2. Ch. Vi. 2/8
3. Su.Su.46/473
4. Su.Su.46/473
5. Ch.Chi.15/41-44
6. Ch. Su. 28/45
7. Ch. Su. 26
8. Ch. Su. 27
9. D.G. Vol – I
10. Su.Su.46
11. Su.Su.45
12. Bh. Pr. 9
13. O.T.P. Ch. 15
14. O.T.P. Ch. 15
15. Ch. Vi. 2/8
16. Ch. Si. 12/56

SAMPRAPTI
1. Ma.Ni. 1/8
2. Ash. Hr. Ni. 12/5 ;Ch. Chi. 13/9
3. Ash. Hr Su. 12/11
4. Ash. Hr Su. 12/11
5. Ch. Chi. 15/39
6. 6. Ch. Chi. 15/9-11 Chakrapani
7. Ash. Hr Su. 15/10
8. Ash. Hr Su. 3/74 ;Su.Su. 35/20
9. Ch. Chi. 15/51 ; Ch. Vi. 6/12 ; Su.Su. 35/20 ; Ash. Hr. Sa. 3/74
10. Ch. Chi. 15/50 ; Su.Su. 35/20 ; Ash. Hr. Sa. 3/75
11. Ch. Chi. 15/50 ; Su.Su. 35/20 ; Ash. Hr. Sa. 3/76
12. Ash. Hr. Sa. 12/11
13. Ash. Hr. Su. 13/25
14. Ash. Hr Su. 13/26
15. Ch. Chi. 15/42-43 ; Su.Su. 46/535
16. Ash. Hr. Su. 13/23-24
17. Moniere Williams
18. Ash. Hr. Su. 13/27 Arunadutta
19. Ash. Hr. Su. 13/27
20. Ash. Hr. Su. 13/27 Hemadri

21. Ch. Chi. 15/37 ; Su.Su. 24/10
22. Su.Su. 46/497
23. Kha. Khi. 16/8
24. Kha. Khi. 16/7-9
25. Ma. Ni. 51/1
26. Ch. Su. 26/40
27. Ch. Chi. 15/44 Chakrapani.
28. Kha. Khi. 16/10-11
29. Ma. Ni. 51/3
30. Kha. Khi. 16/16-17
31. Ma. Ni. 51/3 ; Bha.Pra.Ma.Kha ; Y.R
32. Kha. Khi. 16/49
33. Ma. Ni. 51/3
34. Ma. Ni. 51/3 ; Kha. Khi. 16/16-17
35. Kha. Khi. 16/49
36. Su. Su. 21/18
37. Ash. Hr. Su. 12/22
38. Su. Su. 21/25
39. SLS
40. Su. Su. 21/30

POORVARUPA
1. Ch.Ni 1/8
2. Ch.Ni.1/8 Chakrapani
3. Madhukosha Vyakhya
4. Madhukosha Vyakhya
5. Ch Ni 1/8
RUPA
1. Ch. Ni. 1/9
2. Ash. Hr. 1
3. Ash. Hr. Su. 1; Ma. Ni. Vijayarakshita teeka
4. Ma. Ni. 51
5. Ma. Ni. 51
6. Ma. Ni. 51
7. Ma. Ni. 51/4-6
8. Yogaratnakara amlapitta chikitsa /4
9. Bha. Pra. Ma. Kha. 10/3
10. Bha. Pra. Ma. Kha. 10/8 ;Kha. Khi. 16/16 ; Ma. Ni. 51/4 ; Yogaratnakara
11. amlapitta chikitsa /8
12. Ma. Ni. 51/10 ; ;Kha. Khi. 16/16
13. Ma. Ni. 51/11
14. Kha. Khi. 16/16

BHEDA
1. Ma.Ni. 51/3
2. Ma.Ni. 51/3
3. Kha.Khi. 16/16-17
4. UPASHAYA
5. Ch. Vi. 4
6. Ch. Vi. 1/20
7. Kha. Khi. 16/16
SADYAASADYATA
1. Ch. Ni. 5/15
2. Ma. Ni. 51/7
3. Kha. Khi. 16/49
UPADRAVA
1. Ch.Chi. 21/40
2. Kha. Khi. 16/49
CHIKITSA
3. Kha. Khi. 16/42
4. Ash. San. Ni. 2/4 Indu teeka
5. Kha. Khi. 16/ ; Bha. Pra. Ma. Kha. 10/ ;Yogaratnakara amlapitta chikitsa.
6. Bhaishajya ratnavali 56/ ;Chakradutta Ch. 52/
7. Va. Se. 59/21
8. Bha. Pra. Ma. Kha. 10/13

9. Kha. Khi. 16/
10. Ash . Hr. Su. 1/25 Indu Teeka
11. Ash. Hr. Su. 1/25
12. Va. Se. 62/13
13. Bha. Pra. Ma. Kha. 10/13
14. Kha. Khi. 16/ 31
15. Kha. Khi. 16/ 33-36
16. Bha. Pra. Ma. Kha. 10/13
17. Kha. Khi. 16/ 31-32
18. V. M. 33/1
19. Va. Se. 62/21
20. Ch. Chi. 3/142 ;Su. Ut. 40/60 Dalhana ;Ash. Hr. Chi. 1/21
21. Ch. Chi. 14/182
22. Kha. Khi. 16 ; Chakradutta Ch. 52 ; Bha. Pra. Ma. Kha. 10 ; B.Ratnavali 56 ;
Y.R
23. C.S.S ; R.R.S ; Vaidya Jeevana ; Rasaidriya Sangra
PATHYA APATHYA
1. Ch..Su.25/45
2. Ch. Vi 1/21
3. Ch. Vi 1/24
4. Ch. Vi 1/24-6-8
5. Anita Varghees etal. [2000]

DYSPEPSIA
1. Davidson’s principles and practice of medicine. Ch. 17
2. Medical Dictionary
3. Principal of Internal Medicine by Harrison.
4. Davidson’s principles and practice of Medicine. Ch 17.
5. Davidson’s principles and practice of Medicine. Ch 17
6. Principal of Internal Medicine by Harrison
7. Davidson’s principles and practice of Medicine. Ch 17
8. Davidson’s principles and practice of Medicine. Ch 17
9. Davidson’s principles and practice of Medicine. Ch 17
10. Davidson’s principles and practice of Medicine. Ch 17
11. Principal of Internal Medicine by Harrison 11b] Principal of Internal
Medicine by Harrison part II.
12. Davidson’s principles and practice of Medicine. Ch 17
13. Davidson’s principles and practice of Medicine. Ch 17
14. Davidson’s principles and practice of Medicine. Ch 17
15. Davidson’s principles and practice of Medicine. chapter 20
16. Davidson’s principles and practice of Medicine. Ch 20
17. Davidson’s principles and practice of Medicine. Ch 17
18. Principal of Internal Medicine by Harrison
19. Davidson’s principles and practice of Medicine. Ch 17
20. 5 Minute Clinical Assist – CIMS

Drug review -
1. Ch. Su. 4
2. Su.Su. 38
3. D.G.Vol - III
4. R.R.Samu 2/9
5. R.R.Samu 2/10
6. R.R.Samu 2/16-17
7. R.R.Samu 2/22
8. Ch. Su. 13/25.
9. Ch. Su 27/231
10. Ch. Su 13/18
11. Yoga Ratnakara. Pu. Ar. Rutu charya.
12. Ch. Vi. 1
13. Yoga Ratnakara. Pu. Ar. Rutu charya.
14. Ch. Vi. 1

BIBLIOGRAPHY
1. Agnivesha; Charaka Samhita; redacted by Charaka and Dridabala with Ayurveda
Dipika commentary by Chakrapanidutta; edited by Vaidya Yadavji Trikamji
Acharya; 4th edition, 2001; published by Chaukhamba Surabharati Prakashana,
Baranasi Uttar Pradesh.
2. Anonymous; Yogaratnakara, with Vidyotini Hindi Commentary by Vaidya
Laxmipathi Shastri; 7th edition 1999; Chaukhambha Sanskrit Samsthana, Varanasi,
Uttar Pradesh.
3. Bahadur, Raja Radhakanthadeva ; shabda kalpadruma ; Reprint 1998 ; published by
Nagsharan Singh for Nag Publishers ; Delhi.
4. Bhavamishra ; Bhramashankara Shastri and sri Roopalal vaishya ; Eighth Edition,
1997 ; Chaukambha Sanskrit Bhavan, Varanasi, Uttar Pradesh.
5. Boyd, William ; Boyd’s textbook of pathology, Ed. Ritchie A-G 9th editions 1990;
published by Lea and Febiger, Philadelphia/London.
6. Chakrapanidutta ; Chakradutta [Chikitsa sura sangraha] ; 2nd edition, edited by P.V.
Sharma ; Published by Chaukambha Orientalia, Varanasi.
7. Davidson, Sir Stanley; Davidson’s Principles and Practice of Medicine Ed C.R.W.
Edwards et al ; 19th edition ; 2002 ; Chuchill Livingstone, Edinburgh.
8. Gogte V.M.; Ayurvedic Pharmacology and therapentic uses of Medicinal plants ;
Dravya Guna Vignana ; Published by Bharatiya Vidya Bhavan Mumbai ; 2000.
9. Govinda Dasa ; Bhaishajya ratnavali ; redacted by Bhishakratna Shri Brhama
Shankara Mishra with Bidyotini tika by Kaviraja Sri Ambikadutta Shastri ; editied by

Sri Rajeshwara Dutta Shastri ; 13th edition 1999 ; published by Chaukambha Sanskrit
Samsthan, Varanasi.
10. Gupta Niranjana Prasad A.B. ; Paradha Samhita with Hindi Commentary ; Published
by Khemraj Srikrishna Das, Mumbai
11. Gyanendra Pandey : Dravya Guna Vignyana Vol III ; 7th edition – 2001 ; published
by Krishnadas Academy Varanasi.
12. Harsh Mohan, Text book of pathology, edited by Harsha Mohan ; published by
Jaypee Brothers Medical publishers [p] Ltd. New Delhi 110002, India 3rd addition
1995.
13. Harrison T.R. et al ; ed- Harrison’s principles of Internal Medicine ; Vol I and II, 14th
International edition ; 1998 ; published by Mc. Graw – Hill Book Co. Singapore.
14. Kashyapa Maricha ; Kashyapa Samhita ; ed. Pandit Laxmiraja sharma, Shri Satyapala
Bhishagacharya with Vidyotini hindi vyakhya, 6th edition, 1998 ; Chaukambha
sanskrit samsthan, Varanasi, Uttar Pradesh.
15. Kaviraj Ramrakshak Pathak; Kaya Chikitsa Vol-III; 6th edition; 1993; Published by
Chaukambha Bharati Academy, Varanasi
16. Madhavakara ; Madhava Nidanam, Uttaradha with Madhukosha Vyakhya by
Vijayarakshita and Srikantadutta, Vidyotini tika by Ayurvedacharya Sri Sudarshana
shastri ; 29th edition, 1999 ; Chaukambha Sanskrit samsthan, varanasi Uttar Pradesh.
17. Mahajan B.K. ; Methods in Biostatistics, 6th edition, published by Jaypee Brothers,
Bombay.

18. Nayak Sandhya rani et al ; A clinical study on Amlapitta and its management with
patoladi kwatha [unpublished doctoral dissertation ; Uttkal University ;
Bhuvaneshwar; Orissa; 1998]
19. Prashanth A.S. et al . Randomised control trial of an Ayurvedic compound verses
liquid Antacid in Non-Ulcer Dyspepsia. [unpublished Doctoral dissertation,
Trivendrum University Kerala ; Trivendrum 1994]
20. Sandeep Kumar et.al. Role of Ubhayoto shodhana in management of urdhwaka
amlapitta [unpublished Doctoral dissertation, Mysore, RGUHS; 1999]
21. Santosh Khandal;Rasa Baishajya Kalpana Vigyana; 4th edition 2002; Published by
Publication Scheme; Jaipur.
22. Satoskar R.S and Bhandarkar S.D. ; Part II, Pharmacology and pharmaco therapeutics
; Revised 10th edition 1987, Published by Popular prakashan private Ltd. Bombay.
23. Sharangadhara, Sharangadhara samhita, Madhyama khanda; english translated edition
by Ayurveda Vidwan Prof. K.R. Srikantamurthy. Chaukambha Orientalia, Varanasi,
Uttar Pradesha.
24. Sharma Priyavat ; Dravya Guna Vignana, Vol – II and IV, reprint edition, 1999 ;
Chaukambha Bharati Academy, Varanasi, Uttar pradesh.
25. Sheshadri Vasan ; Amlapitta and its management with kamaduga rasa [unpublished
Doctoral dissertation, Mysore, 1976]
26. Siddinandan Mishra; Ayurvediya Rasashastra; 5th Edition; 1994;Published by
Chaukambha Orientalia, Varanasi
27. Sushruta, Maharshi ; Sushruta samhita with Nibandha sarasangraha commentary of
Sri Dalhana Acharya and Nyaya Chandrika Panjika of Sri Gayadasacharya ; ed. by

Vaidya Yadavji Trikamji Acharya and Narayan Ram Acharya ; Reprinted edition
1998 ; Krishnadas Academy, Varanasi, Uttar Pradesh.
28. Tripathi K.D. ; essentials of Medical pharmacology ; Published by Jaypee Brothers,
Bombay.
29. Vachaspathyam; compiled by Sri Taranath Tarka, Vachaspi Vol - I Published by
Chaukambha sanskrit series. Varanasi 1962.
30. Vagbhata ; Ashtanga Sangraha; Vol-I; English translation by
Prof.K.R.Shrikantamurthy; 2nd edition 1998; Published by Chaukambha Orientalia,
Varanasi
31. Vagbhatacharya ; Ashtanga Hridaya with commentaries sarvangasundara of
Arunadutta and Ayurveda Rasayana of Hemadri, ed. by Pandit Bhishak Acharya,
Harishastri Paradkar Akoln ; 8th edition, 2000 ; Chaukamba Orientatlia Varanasi,
Uttar Pradesh.
32. .Vagbhatacharya; Rasaratna Sammuchaya with Rasaprabha hindi commentary by
Dr.Indradev Tripati;2nd edition 2003;Published by Chaukambha Sanskrit Bhavan,
Varanasi.
33. Vangasena; Vangasena Samhita[Chikitsa Sarasangraha]; Vol-II; with english
translation by Dr.Nirmal Saxena; 1st edition 2002; Published by Chaukambha
Sanskrit Series, Varanasi.
34. Vargheese Anitha ; An evaluation of pathyapathya with regard to desha and kala
[Unpublished doctoral dissertation, Trivendrum University,Keralas,Trivendrum
2000].

Department of Kayachikitsa
A.L.N.R.M.A.Medical College, Koppa-577126
A CLINICAL STUDY ON THE EFECT OF SHATAVARI CHOORNA WITH
ABHRAKA BHASMA IN THE MANAGEMENT OF AMLAPITTA
CLINICAL PROFORMA
Patient Name: Group:
Age/Sex: .......yrs M/F Sl. No:
Religion: H/M/CH/J OPD/IPD:
Education: UE/P/M/HS/GR/ Ward/Bed No:
Marital status: M/UM/W/D D.O.A./D.O.D:
Socio Economic status: VP/P/LM/M/UM/R Diagnosis:
Occupation: HW/L/B/S/E Result:
Postal Address:
Chief Complaints Duration BT AT AFU
1. Utklesha:
2. Amlodgara
3. Hrtdaha
4. Kantadaha
5. Udarashoola
6. Vanti
Colour:
Consistency:
Contents:
Taste
II. Associated complaints:
1. Avipaka:
2. Klama
3. Tiktodgara:

4. Gourava:
5. Aruchi:
6. Gurukoshtatha
7 Adhamana
8 Antrakujana
9. Sirasula:
III. History of present illness:
A) Onset : Sudden / Gradual
B) Aggravating Period : Mid-day/Mid-night/Morning
C) Environmental factor : Rainy / Summer / Autumn / Winter
IV. History of past illness:
V. Drug History:
VI. Family History:
VII. Personal history:
1. Ahar (Diet) :
a) Virudhha Ahar : Yes / No
b) Pittaprakopaka Yes / No
c) Vidahianna Yes / No
d) Amlarasapradhana Yes / No
e) Abhishyandhi Yes / No
f) Atibhojana Yes / No
g) Nature : Veg/Mix
h) Habits: Samasana/Visamasana/Adhyasana/Anasana/Pramitasana
i) Rasapradhana: M/A/L/K/T/KS/Sarva rasa
j) Guna Pradhana: U/St/G/L/S/R/T/M
k) Supplimentary diet: Tea/coffee/Milk/cold drink

l) Water intake: Every morning, During or after lunch & dinner
Day or night .......... ltr total
2. Vihara (Regimen)
a) Diwaswapna Yes / No
b) Vegadharana Yes / No
c) Avagahana Yes / No
d) Atapasevana Yes / No
3. Manasika (Psychological factors)
Mental Stress/ Strain Present / Absent
4. Addictions: Smoking/Tobacco chewing/Alcohol/Narcotics/No habits
5. Exercise: Regular/Irregular/occasional/only routine work.
6. Sleep: Sound/Irregular/Disturbed/Delayed
Night...........Hrs Day:.........Hrs
7. Bowel: Regular/Irregular/constipation/Loose /Soft/Constipated
No.of frequency ........./times.........days
8. Micturation: Regular/Irregular ........times/day .......times/night
6. Occupational history: Sedentary/moderate/Heavy
a) Nature of work:Physical/mental
b) Time of work:Day/Night/Day Night .........Hrs
7. Social history:
Hygienic condition of residence: Poor/Moderate/Good

8. Gynacological history:
VIII. Atura Bala Pariksha:
i) Prakriti :
Sharira : V/P/K/VP/VK/PK/VPK
Manas : S/R/T
ii) Sara : Pravara /Madhayama /Avara
iii) Samhana : Pravara /Madhayama /Avara.
iv) Satva : Pravara /Madhayama /Avara
v) Satmya : Pravara /Madhayama /Avara
vi) Pramana : Height ......ft
Weight ...... Kg: (BT).......Kg:(AT)
vii) Ahara shakti :
Abhyavaharan shakti : Pravara /Madhayama /Avara
Jarana shakti : Pravara /Madhayama /Avara
Agni : Sama/Visama/Manda/Tikshna
Kostha : Mridu/Madhyama/Krura
viii) Vyayama shakti : Pravara /Madhayama /Avara
ix) Vya : Bala/Madhyama/vridda
x) Desha : A/J/S
xi) Vikrititaha : Pravara /Madhayama /Avara

IX. General Examination: BT AT
Pulse rate:
Respiration rate:
Temp:
B P:
X. Systemic Examination.
RS:
CVS:
CNS:
GIT:
Inspection:
Mouth : Stomatitis/Other/Normal
Shape : Distended/Scaphoid/Bulging of flanks/Normal
Umbilicus : Inverted/Everted/Normal
Surface : Smooth/Glossy/scar/wrinkles/Pigmentation/striae
Asymetrical Bulging : Epigastric/Hypogastric/Umbilical/lumbar/
Hypocondriac/Illiac/None
Movement : Symetrical/ Asymetrical
Pulsation : Visible/Invisible
Palpation : Superfical-Region of tenderness...............
Hyperasthesia:Present/Absent/Site...........
Muscle guard:Rigid/Normal

Liver : Palpable/Tender/Normal
Spleen : Palpable/Tender/Normal
Kidney : Palpable/Tender/Normal
Colon : Palpable/Tender/Normal
Any Other Mass : Present/Absent
Percussion:
XI. Srotas Examination:
Annavaha Srotas : Aruchi/Avipaka/Chardi/Anannabhilasha/Prakrita
Rasavaha scotas : Angasad/Praseka/Alasya/Gaurava/Bhrama
Sosha/Glani/Pandu/Asraddha/Asyavairasya
Arasagnata/Prakrita
Purishavaha srotas :
Atridrava/Atigrathita/Bahula/Alpalpa/Sasabda/Sasula
malapravritti/Prakrita
Other Srotas : Prakrita/Vaikrita
XII. Laboratory Investigations:
1.Heamatoligical: Hb%
Total count-
Differential count:
Neutrophils- Lymphocytes-
Monocytes- Basophils-
Erythrocyte Sedimentation Rate:

2. Urine: Albumin
Sugar
Microscopy
3. Stool: Ova and Cysts Present/Absent
4.Endoscopy ( If Necessary ):
5. Any Relevant Investigation :
Untoward Symptoms:
Comments:
Grading No Sign/symptom: 0 Mild : 1
Moderate : 2 Severe : 3
Signature of Guide Signature of scholar

chart no. 2 Showing the classification of Nidanas of Amlapitta NIDANAS
I. Agnidustikara II. Pittaprakopaka III. Vataprakopaka IV. Kaphaprakopaka Ahara Vihara Ahara Vihara * Abhojana * Bhukte Bhukte snana * Atibhojana * Bhukte Bhukte avagaha * Rooksha atisevana * Vegadharana * Ajeerna * Bhukte Bhukte diwaswapna * Brista atisevana * Viruddhasana * Vishamashana * Dushta bhojana Ahara Vihara Ahara Vihara * Adhyasana * Apakwa atisevana * Katurasa atisevana * Ushna desha * Snigdha atisevana Diwaswapna * Snigdha atisevana * Amlarasa atisevana * Ushna kala * Guru atisevana * Guru atisevana * Lavanarasa atisevana * Pista atisevana * Pishta atisevana * Kulatha atisevana * Gorasa atisevana * Ikshuvikara atisevana * Ushna atisevana * Panita atisevana * Gorasa atisevana * Drava atisevana * Panita atisevana * Madhya atisevana

FRUITS – Yes
Generally most
sweet fruit
FRUITS – No
Generally most sour
fruit
VEGETABLES – Yes
Generally most sweet &
bitter vegetables
VEGETABLES –
No Generally most
pungent vegetables
• Apples [sweet] • Apples [sour] • Artichoke • Beet greens
• Applesauce • Apricots [sour] • Asparagus • Beets raw
• Apricots [sweet] • Bananas • Beets [cooked] • Burdock root
• Avocado • Berries [sour] • Bitter melon • Corn [fresh]**
• Berries [sweet] • Cherries [sour] • Broccoli • Daikon radish
• Cherries [sweet] • Cranberries • Brussels sprouts • Eggplant **
• Coconut • Grapefruit • Cabbage • Garlic
• Dates • Grapes [green] • Carrots[cooked] • Green chilies
• Figs • Kiwi ** • Carrots [raw]* • Horseradish
• Grapes [red&
purple]
• Lemons
• Mangos [green]
• Cauliflower
• Celery
• Kohlrabi**
• Leeks [raw]
• Limes * • Oranges [sour] • Cilantro • Mustard greens
• Mangoes [ripe] • Peaches • Cucumber • Olives, green
• Melons • Persimmons • Dandelion greens • Onions [raw]
• Oranges [sweet] • Pineapple [sour] • Fennel [anise] • Peppers [hot]
• Papaya * • Plums [sour] • Green beans • Prickly pear
[fruit]
• Pears • Rhubarb • Jerusalem • Radishes [raw]

Artichoke
• Pineapple [sweet] • Strawberries • Kale • Spinach
[cooked]**
• Pomegranates • Tamarind • Leafy greens • Spinach [raw]
• Prunes • leeks [cooked] • Tomatoes
• Raisins • lettuce • Turnip greens
• Watermelon • Okra • Turnips
• Olives, black
• Onions [cooked]
• Parsley
• Parsnips
• Peas
• Peppers, sweet
• Potatoes, sweet &
white
LEGUMES – Yes LEGUMES – No DAIRY –Yes DAIRY – No
• Aduki beans • Miso • Butter [unsalter] • Butter [salted]
• black beans • soy sauce • cheese [soft, not
aged, unsalted]
• buttermilk
• black-eyed peas • soy sausages • cottage cheese • Cheese [hard]
• Chick peas • Tur dal • Cows milk • Sour cream

[garbanzo
beans]
• Kidney beans • Urad dal • Ghee • Yougurt [plain,
frozen or with
fruit]
• Lentils, brown
& red
• goats cheese [soft
& unsalted]
• Lima beans • goats milk
• Mung beans • ice cream
• Mung dal • yogurt [freshly
made &diluted]*
• Navy beans
• Peas [dried]
• Pinto beans
• Soy beans
• Soy Cheese
• Soy flour*
• Soy milk
• Soy powder
• Split peas
• Tempeh
• Tofu

• White beans
GRAIN –Yes GRAINS –Yes BEVERAGES –Yes BEVERAGES –Yes
• Amaranth • Bread [with
yeast]
• Almond milk • Apple cider
• Barley • Buckwheat • Aloe vera juice • Berry juice [sour]
• Cereal, dry • Corn • Apple juice • Caffeinated
• Couscous • Millet • Apricot juice • Caffeinated
beverages
• Crackers • Muesli** • Berry juice [sweet] • Carbonated drinks
• Durham flour • Oats [dry] • Black tea • Carrot juice
• Granola • Polenta ** • Carob • Cherry juice [sour]
• Oats
[cooked]
• Rice [brown]** • Chai [hot, spiced
milk]*
• Chocolate milk
• Pancakes • Rye • Cherry juice • Coffee
• Pasta • Cherry juice [sweet] • Cranberry juice
• Rice
[basmati,
white, wild]
• Cool dairy drinks • Grapefruit juice
• Rice cakes • Grain “coffee” • Iced tea
• Sago • Grape juice • Iced drinks
• Seitan [wheat • Mango juice • Lemonade

meat]
• Spelt • Miso broth* • Papaya juice
• Sprouted
wheat bread
[essene]
• Mixed veg. juice • Tomato juice
• Tapioca • Orange juice* • Sour juices
• Wheat • Peach nectar Hearb Teas:
• Wheat bran • Pomegranate juice • Ajwan
• Prune juice • Basil**
• Rice milk • Cinnamon *
• Soy milk • Clove
• Vegetable • Eucalyptus
Bouillon • Fenugreek
• Ginger [dry]
Herb Teas: • Ginseng
• Alfalfa • Hawthorne
• Bancha • Hyssop
• Barley • Juniper berry
• Blackberry • Pennyroyal
• Borage
• Burdock
• Catnip

• Chamomile
NUTS – Yes NUTS – No SEEDS – Yes SEEDS – No
• Almonds [soaked
and peeled]
• Almonds [with
skin]
• Flax • Chia
• Charole • Black walnuts • Halva • Sesame
• Coconut • Brazil nuts • Popcorn [no salt,
buttered]
• Tahini
• Cashews • Psyllium
• Filberts • Pumpkin *
• Hazelnuts • Sunflower
• Macadamia nuts
• Peanuts
• Pecans
• Pine nuts
• Pistachios
• Walnuts
OILS – Yes
For internal &
external use : [most
OILS – No SPICES – Yes SPICES – No

suitable at top of
list]
• Sun flower • Almond • Basil [fresh] • Ajwan
• Ghee • Apricot • Black pepper* • Allspice
• Canola • Corn • Caraway* • Almond extract
• Olive • Safflower • Cardamom * • Anise
• Soy • Sesame • Cinnamon • Asafetida [hing]
• Flax seed • Coriander • Basil [dry]
• Primrose • Cumin • Bay leaf
• Walnut • Curry leaves • Cayenne
• Dill • Cloves
• Fennel • Fenugreek
External use only • Ginger [fresh] • Garlic
• Mint • Ginger [dry]
• Avocado • Neem leaves* • Mace
• Coconut • Orange peel* • Marjoram
• Parsley* • Mustard seeds
• Peppermint • Nutmeg
• Saffron • Oregano
• Spearmint • Paprika
• Tarragon* • Pippali
• Turmieric • Poppy seeds

• Vanilla* • Rosemary
• Wintergreen • Sage
• Salt
• Savory
• Star anise
• Thyme
CONDIMIENTS –
Yes
CONDIMENTS –
No
SWEETENERS –
Yes
SWEETNERS –
No
• Black pepper* • Chili pepper • Barley malt • Honey ** [raw
& not
processed]
• Chutney, mango
[sweet]
• Chocolate • Fructose • White sugar **
• Coriander leaves* • Chutney, mango
[spicy]
• Fruit juice
concentrate
• Jaggary
• Dulse* • Gomasio • Maple syrup • Molasses
• Hijiki • Horseradish • Rice syrup • Molasses
• Kombu * • Kelp • Sucanat
• Lime * • Ketchup • Turbinado
• Sprouts • Mustard

• Tamari * • Lemon
• Lime pickle
• Mayonnaise
• Pickles
• Salt [in excess]
• Scallions
• Seaweed
• Soy sauce
• Vinegar
FOOD SUPPLEMENTS – Yes FOOD SUPPLEMENTS – No
• Aloe vera juice • Amino acids
• Barley green • Bee pollen**
• Brewer’s yeast • Royal jelly **
• Minerals: calcium, magnesium, zinc • Minerals: copper, iron, vitamin
A,B,B12 & C
• Spirolina
• Blue-green algae
• Vitamins D & E
Related Documents