ALVEOLAR BONE ITS RELEVANCE IN PROSTHODONTICS

Welcome message from author
This document is posted to help you gain knowledge. Please leave a comment to let me know what you think about it! Share it to your friends and learn new things together.
Transcript

ALVEOLAR BONE ITS
RELEVANCE IN PROSTHODONTICS

CONTENT
Topic Page no.
Introduction 3-6
Systemic influences on alveolar bone 7
Effects of hormones 8-9
Effects of vitamins 10
Effects of drugs 10
Prosthodontic considerations of alveolar
bone in relation to
Complete denture 12
Single complete denture 12
Removable partial denture 13
Fixed partial denture. 14
Implants. 15
Combination syndrome 16-18
Conclusion 19
References 20-21
Page 2

Introduction
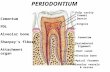
According to Glossary of prosthodontics alveolar bone is defined as
bony portion of mandible or maxilla in which roots of teeth are held by
fibers of periodontal ligament. A.R Tencate states that alveolar bone is that
portion of maxilla and mandible which forms & supports roots of teeth. It
forms when tooth erupts, to provide the osseous attachment to the forming
periodontal ligament and disappears gradually after tooth is lost.
It is extremely important to the dental practitioner, as almost all his
treatment procedures can be successful only if the bony support remains
intact. The success of complete denture, partial dentures, implants is
dependent on degree of stability that the underlying bone can maintain.
Residual Ridge Resorption
Alveolar bone has one of the highest metabolic rate, owing to nearly
continous masticatory stress applied to it through tensile forces transmitted
throught periodontal ligament.
Residual Ridge Resorption is chronic, progressive, irreversible,
cumulative, multifactorial, biomechanical disease that results from a
combination of anatomic, metabolic and mechanical determinants.
After teeth loss, alveolar bone undergoes rapid remodeling. Which
results in bone loss.
Amount of bone loss varies among individuals and depends on
- Age
- Sex
- Nutritional status
- Medical conditions
Page 3

- Original shape
- Size and location of alveolar process
Factors affecting rate at which bone is lost
Anatomical – size of ridge following extraction
- type of residual bone
- type of mucoperiosteum
- Location with in oralcavity
Metabolic - Age
-Sex
-diet
-harmonal status
Functional - Frequency, direction and amount of force applied to
ridge.
Prosthetic factor - type of denture base,
- forms and type of teeth,
- interocclusal distance.
Osteoclasts have the function of eliminating bone i.e. no longer
adapted to mechanical forces. At the site of bone formation, osteoblasts
differentiate from precursor cells of connective tissue. The mechanisms
which determine bone formation at any given site are unknown. They must
be varied and determined on a genetic and functional basis.
Osteoblasts form osteoid tissue which will be followed by
mineralization. It always lags behind production of bone matrix and
therefore in such areas a superficial layer of osteoid tissue is always seen. A
peptide called osteoclastic activating factor is found in lymphocytes and is
capable of increasing AMP and osteoclastic activity and reducing
osteoblastic activity at target site.
Page 4

The exact mechanism by which osteoclasts may act to resorb the bone
is not clear. The osteoclasts may liberate enzymes which dissolve the
organic matrix and remaining inorganic salts. May then be dissolved by
chelating agents such as EDTA, C.AMP in cells may play some role in bone
resorption.
The initiation of resorption is not completely known. It may be due
to dying or dead osteocytes that stimulate the connective tissue, resulting in
osteoclast’s in the area.
Thomas, Stahl and Pendleton consider alveolar ridge resorption as
normal biologic process that increases with age.
Bones have an intrinsic growth pattern as stated by TOWNSLEY in
1948 and it is possible that the alveolar bone may have a hereditary
resorption pattern.
- In 1971, Atewood described RRR as “MAJOR ORAL DISEASE
ENTITY” characterised by loss of oral bone after the extraction of teeth.
- The size, shape and tolerance of residual ridges provides the basis of
stability, retention, support of complete denture.
- New Feld reported “ In some of specimens studied, the trabecular pattern
was arranged in a such a way that it indicated that there was some
adaptation of structure of bones to presence of an appliance in region
near the superior surface of alveolar process”.
- Atewood reported “ A complete abscence of periosteal bone over
residual ridge in all specimens studied”.
- Clayton. F. Parkinson in 1978 stated that i) Arch width of maxilla is
less than mandible in molar region by 6 - 7 mm ii) Alveolar resorption
rate is highest in early stages of edentulism and slows with loss of bone,
longevity of edentulism and the attendant wearing dentures.
Page 5

- Antje. Tallgren in 1972 stated that mean reduction in lower anterior
ridge height is approximately four times as great as that of upper ridge.
- Tallgren stated that RRR
According to Atwood D.A.
Class – I – Pre extraction
Class – II – Post extraction. Immediately following exfoliaition of tooth
with, the labial and lingual alveolar process remaining
Class – III – High well rounded. The sharp edges will be rounded OFF by
the external osteoclastic activities leaving a high well rounded
residual ridge.
Class – IV – Knife edge . As resorption continues form both labial and
lingual aspects the crest of ridge becomes increasingly narrow
finally results in knife edge.
Class – V – Low well rounded. The knife edge shortens and finally
leaving
low well rounded or flat ridge.
Class – VI – Depressed . Further resorption leaving only the thin cortical
bone in lower border of body of maxilla
Page 6
1damping effect of the mucosa
Winkler observed thatRRR Anatomical factors Bone resorption factors Force factors
Time Bone formation factors Damping Effect+ +

Age changes
Age changes in alveolar bone are similar to those occurring in
remainder of skeletal system.
These include – osteoporosis
- decreased vascularity
- reduction in metabolic rate
- reduction in healing capacity
- Bone resorption may be increased or decreased and the density of
alveolar bone may increase or decrease depending on its location. There
is greater irregularity in surfaces of alveolar bone facing the PDL with
advancing age.
- Older persons is likely to have more alveolar ridge resorption than a
younger person.
- In aged, resorption is not compensated by production of bone, resulting
in senile osteoporosis. In persons over 70 yrs of age, 25% of bone may
be engaged in bone resorption.
REIFENSTEIN in 1950 stated that osteoporosis may be normal after
menopause. Alveolar ridge may show resorption in connection with
osteoporosis.
Page 7

Influence of systemic diseases
1. Protein deficiency – causes loss of alveolar bone which is the result
of inhibition of normal bone forming activity.
2. Acute starvation results in osteoporosis and reduction in height of
alveolar bone.
3. In hyperpitutarism (acromegaly) marked over growth of alveolar
bone causes increase in size of dental arch.
4. Ridge resorption is associated with hyperparathyroidism and
vonrecklinghausen’s disease due to increased bone loss.
a. Radiological findings of hyperparathyroidism are alveolar
osteoporosis with closely meshed trabeculae, widening of PDL space
and loss of laminadura.
5. Complete loss of laminadura occurs in paget’s disease, Fibrous
dysplasia, osteomalasia.
6. Diabetes mellitus shows rapid alveolar bone loss.
7. In acute, sub acute leukemia, marrow of alveolar bone exhibits
localized areas of necrosis, thrombosis of blood vessels, leukocytic
infiltration and replacement of fatty marrow with fibrous tissue.
8. In agranulocytosis, osteoporosis of alveolar bone with osteoclastic
resorption, necrosis of alveolar bone and heamorrhage in the marrow
occur.
9. Mercury intoxification leads to destruction of alveolar bone.
10. Other chemicals such as phosphorous, arsenic and chromium may
cause necrosis of alveolar bone.
11. Benzene intoxification also leads to destruction of alveolar bone.
12. Hypophoshatasia, an inherited disease causes premature loss of
alveolar bone surrounding decidous incisors by 10 months of age.
Page 8

Effect of hormones
Hormones such as androgens, estrogens and somatotropin exert a
definite influence on growing alveolar bone, but their effect on adult bone is
not clear.
- PTH has direct action on adult bone, which is responsible for
maintainence of normal blood calcium levels of 10-11 mg%
- PTH has 4 main sites of activity namely 1) kidney 2) bone 3) intestine 4)
lactating mammary gland.
- PTH is probably the most important of harmones in so far as RRR is
concerned.
- In alveolar bone PTH liberates both calcium and phosphate. When PTH
is active, calcium and phosphate ions move from alveolar bone to
plasma. But it is not known whether PTH acts directly or through
osteoclasts.
- When circulating PTH is high, it leads to osteoporosis which in turn
leads to resorption of alveolar ridge. A decrease in PTH level results in
increase formation of bone hence resorption of alveolar bone is reduced.
Calcitonin – It has antagonist action compared to PTH.
Estrogen : Estrogen deficiency causes increased bone resorption activity
where as surface of residual ridge alveolar bone in oestrogen deficiency and
its replacement therapy seem to affect the activity of residual ridge bone
remodelling at the molecular level.
Osteoporosis is predominant side effect of menopause which is due to
decrease of oestrogen production.
Page 9

Although the osteoporotic change of maxilla – mandible occur elderly
patients in a fashion similar to that of metacarpal bone and vertebral bone.
NISHIMURA et al. reported that, although bone height showed no
differences, the knife edge morphologic features of mandibular residual
ridge was statistically associated with osteoporotic changes in 2nd vertebrate
bone.
Effects of vitamins on alveolar bone :
1. Hypervitaminosis D- causes generalized resorption changes in bone
including alveolar bone.
2. Avitaminosis D causes decreased concentration of blood phosphate
and retarded calcification.
3. Chronic hypervitaminosis A- WEINMANN & SICHER in 1955
noted that above condition leads to bone resorption in supporting
bone of the alveolar process in those regions most subject to stress.
4. Hypovitaminosis A- leads to overall bone growth retardation and in
later stages endochondral bone growth ceases entirely.
5. Hypovitaminosis C leads to SCURVY. It causes failure of collagen
production in bone. Production of osteoid is deficient and hence
calcification is restricted. However, bone resorption continues and
eventually bone becomes thin and fragile, which is prone for fracture.
It is characterized by decreased activity of fibroblasts, osteoblasts,
odontoblasts, which ultimately effects collagen production.
Page 10

EFFECT OF DRUGS
A generalised decrease in alveolar bone mass is associated with
chronic corticosteroid therapy, anticonvulsant therapy, long term high dose
heparin therapy and alcoholism.
PROSTHODONTIC CONSIDERATIONS OF ALVEOLAR BONE :
In relation to complete denture :
Alveolar bone is the basic support for the complete dentures. It
provides most of the vertical support. After loss of teeth, re-constructive
process leads generally to loss of bone in the area and the formation of
compact lamellae at surface.
Histologically, socket is filled with immature bone by the end of 2nd
month. But there is some quantitative loss when healing is uneventful; when
primary clot fails to form. The denuded bone necrotizes and is elminated by
resorption. This loss in quantity during healing after extraction is one of the
reasons – awaiting period of 6 weeks to 2 months is advocated prior to
placement of dentures.
Another reason is to allow the immature bone to replace the young
connective tissue.
Continuous presence of dentures is capable of exerting pressure of
sufficient intensity to produce resorption. This is true in mandibular arch,
since gravity exerts a steady pull on denture. A complete denture is
potentially capable of exerting steady pressure that can interrupt the blood
supply. For this season the dentures should be removed at least for 8 hours a
day.
Page 11

“WEINMAN – SICHER” reported that “whether intermittent
pressure is tolerated or even beneficial or whether it too leads to loss of
bone depends entirely on its affects on blood circulation.
Boucher stated that “ prominent alveolar ridges with parallel buccal
and lingual walls may also provide significant retention by increasing
surface area between denture and mucosa there by maximizing interfacial
and atmospheric forces.
Factors that influence the form and size of supporting bone include.
1) Original size and consistency.
2) Person’s general health.
3) Forces developed by surrounding musculature.
4) Severity and location of periodontal disease.
5) Surgery at time of extraction.
6) Relative length of time different parts of jaws have been
edentulous.
K. W. Tyson, J. C. Mcford stated that in case of flat ridges
1. Their should be increased free way space by 2 – 3 mm
2. Impression should cover as much area as possible
3. Peripheral form of polished denture should be in hormone with
buccinator muscle.
Ashman stated that ridge preservation can be done by
1. Advanced extraction therapy (AET)
In this after extraction introduction of synthetic graft in to the
socket was done followed by suturing. He observed that their was
not change in height and width of the bone
2. Replacement therapy – An alloplast graft was placed in an
extraction socket, or in combination with titanium threaded
implant immediately after extraction
Page 12

RESORPTION PATTERN
Single complete dentures :
In upper jaw the premaxillary area is frequently subjected to more
resorption when the patient is wearing a complete denture which occludes
with natural anterior lower teeth.
If magnitude of major force of occlusion is great i.e., no partial
denture fitted, the alveolar bone will be resorbed in that area, leaving a soft
flabby ridge of tender inflamed tissue.
Even when free end saddle partial denture, has been fitted, it is
inevitable that once any resorption has taken place, the major forces of
occlusion will again be thrust on the anterior teeth to be dissipated in upper
jaw through the premaxillary edentulous ridge.
However carefully the complete denture for upper and lower ridges
are made with occlusal forces concentrated in posterior region rather than
anterior bringing the teeth in to occlusion will often thrust upper denture
upward and forward on unstable, tender premaxillary tissues. This is one of
the most irrevocable injuries done to mouth by dentures.
Page 13

Removable partial denture and fixed partial denture :
The radiographic interpretation aspects that are the most pertinent to
RPD & FPD construction, are those relative to prognosis of remaining teeth
used as abutments.
i) Quality of support from alveolar bone of an abutment tooth is of
primary important because the tooth will have to withstand greater
stresses loads when supporting RPD & FPD.
Abutment teeth providing total abutment support to RPD & FPD,
will have to with stand a greater load than before and especially
greater horizontal forces. It is minimized by establishing
harmonious occlusion and by distributing horizontal forces among
several teeth through the use of rigid connectors. Properly
designed tooth borne removable prosthesis should provide
bilateral stabilization against horizontal forces.
ii) Abutment teeth adjacent to distal extension bases in RPD’s are
subjected not only to vertical and horizontal forces but to torque
also because of tissue supported base. Vertical support and
stabilization against horizontal movement with rigid connectors
and just as important as they are with a tooth borne prosthesis.
In addition, abutment tooth adjacent to the extension base will be
subjected to torque in proportion to design of retainers, size of
denture base, tissue, support by base and total occlusal forces
applied.
iii) In RPD, if alveolar bone support is adequate a posterior abutment
should be retained if at all possible in reference to a tissue
supported extension base.
Page 14

iv) In case of RPD & FPD teeth with insufficient alveolar support
may be extracted if their prognosis is poor and other adjacent teeth
may be used to better advantage as abutments.
v) Radiographic interpretation also serve as an important function if
used periodically after the placement of RPD and FPD. Further
bone changes of any type suggest traumatic interference from
some source.
Radiographic observations made are
1. Alveolar bone crest resorption
2. Integrity of thickness of laminadura
3. Evidence of generalized horizontal bone loss
4. Evidence of vertical bone loss
5. Widened pdl space
6. Density of trabeculae of both arches
7. Crown and root ratio.
Ante’s law states that for fixed partial dentures the pericemental area of all
abutment teeth supporting the FPD should be equal to or greater than the
pericemental area of the teeth to be replaced.
For removable partial dentures it states that combined pericemental
area plus mucosal area should be equal to or greater than pericemental area
of missing teeth.
INDEX – AREAS are those of alveolar bone support that disclose the
reaction of bone to additional stress. The reaction of bone to additional
stress in index areas may be negative or positive. With evidence of a
supporting trabecular pattern, a heavy cortical layer and a dense lamina
Page 15

dura, or reverse response with the former, patient is said to have +ve bone
factor, meaning ability to build additional support where ever needed. With
the later patients is said to have negative bone factor meaning inability to
respond favourably to stress.
In FPD general alveolar bone levels with particular emphasis on
abutment teeth should be observed. Any widening of PDL space and loss of
intact of laminadura due to destruction of cribriform plate should always be
correlated with occlusal prematurities or occlusal trauma. An evaluation can
be made of thickness of cortical plate of alveolar bone around teeth and of
the trabeculation of bone.
Implants :
When we talk of implants in relation to alveolar bone first one should
think about OSSEOINTEGRTION. It is defined as direct structural and
functional connection between ordered, living bone and the surface of a load
carrying implant.
COMBINATION SYNDROME
Definition: The Glossary of Prosthodontic Terms defines combination
syndrome as "the characteristic features that occur when an edentulous
maxilla is opposed by natural mandibular anterior teeth, including loss of
bone from the anterior portion of the maxillary ridge, overgrowth of the
tuberosities, papillary hyperplasia of the hard palatal mucosa, extrusion of
mandibular anterior teeth, and loss of alveolar bone and ridge height beneath
the mandibular removable partial denture bases, also called anterior
hyperfunction syndrome.
Page 16

A few years later, further characteristics were added to the
combination syndrome : loss of vertical dimension of occlusion, occlusal
plane discrepancy, anterior spatial repositioning of the mandible, poor
adaptation of the prosthesis, epulis fissuratum, and periodontal changes.
However, these changes are not generally associated with combination
syndrome. (Palmquist Sigvard et al)
When natural anterior teeth are remaining in the mandible opposing a
maxillary edentulous arch results in combination syndrome. These changes
are: - (Kelly Elswarth)
i) Loss of bone from the anterior part of the maxillary ridge.
ii) Overgrowth of tuberosities
iii) Papillary hyperplasia in the hard palate.
iv) Extrusion of the lower anterior teeth.
v) The loss of bone under the partial denture base.
In spite of his emphasis on the negative role of the Mandibular RPD,
Kelly wrote: "The early loss of bone from the anterior part of the maxillary
jaw is the key to the other changes of the combination syndrome".
Dorland's illustrated Medical Dictionary defines "syndrome" as 'a set
of symptoms which occur together; the sum of signs of any morbid state; a
symptom complex". "Combination syndrome" is not included among
hundreds of syndromes listed in
the dictionary. From this review of
the literature it seems obvious that
Page 17

"combination syndrome" does not meet the criteria to be included in such a
list.
Prevention of Combination
Syndrome:
Try to avoid maxillary
edentulous arches with
mandibular natural teeth situation.
Authors do not advocate removal of lower anteriors, but rather to
retain the weak posterior teeth as abutments by means of endodontic
and periodontic techniques.
Endosseous implants, hemi section, root amputation can be done to
preserve lower molar.
An overlay denture on lower may avoid combination syndrome.
Surgical excision of flabby (hyperplastic) tissue, papillary hyperplasia
and enlarged tuberosities. This allows the distal end of the occlusal
plane to be raised to the proper level. (Cynthia P. Thiel et al)
Covering maximum area in lower partial denture.
Covering retromolar pad where muscle and raphe attachments
prevent or reduce resorption, and covering buccal shelf is necessary to
retard bone loss.
Page 18

conclusion
Now we all know the importance of alveolar bone in dentistry. But it is well
for us to understand the still further physiology of bone. It is especially
necessary to remember the factors such as harmones, vitamins, pressure, age
which may all or separately produce ridge resorption.
Unless until mechanism of bone resorption is understood little
progress will be made in prosthodontic therapy. When alveolar bone loss
can be controlled, it will be possible to offer the patient dentures with a
greatly increased chance of success.
Page 19

\
REFERENCES
1. Winkler Sheldon “Essentials of complete denture prosthodontics”. 2nd
Edition.
2. Sharry J.J. “Complete denture prosthodontics”, 3rd edition.
3. Bernard Levin “Impressions for complete dentures”.
4. Carl E. Mish “Contemporary Implant Dentistry”, Second Edition.
5. Ortman L.F. et al, 1992. “Bioelectric stimulation and residual ridge
resorption”. J. Prosthet. Dent; 67 : 67-71.
Page 20

6. Israel Harry 1979. “Evidence for continued apposition of adult
mandibular bone from skeletalized materials”. J. Prosthet. Dent; 41 :
101-104.
7. Atwood D.A., Coy W.A., 1971. “Clinical, cephalometric and
densitometric study of reduction of residual ridges”. J. Prosthet. Dent.,
26 : 280-295.
8. Atwood D.A., 1971. “Reduction of residual ridges : A major oral
disease entity”. J. Prosthet. Dent., 26 : 266-279.
9. Mercier Paul, Lafontant Roger, 1979. "Residual alveolar ridge atrophy:
Classification and influence of facial morphology". J. Prosthet. Dent.,
41: 90-100.
10.Baylink D.J. et al., 1974. “Systemic factors in alveolar bone loss”. J.
Prosthet. Dent., 31 : 486-505.
11.Kelsey C.C., 1971. “Alveolar bone resorption under complete denture”.
J. Prosthet. Dent., 25 : 152-161.
12.Wical K.E., Swoope C.C., 1974. “Studies of residual ridge resorption.
Part-II. The relationship of dietary calcium and phosphorus to residual
ridge resorption”. J. Prosthet. Dent; 32 : 13-22.
13.Sones American Diana et al, 1986. “Osteoporosis and mandibular bone
resorption : A prosthodontic perspective”. J. Prosthet. Dent., 56 : 732-
736.
14.Atwood Douglas Allen 1958. “A cephalometric study of the clinical
rest position of the mandible”. J. Prosthet. Dent., 8 : 698-708.
Page 21

15.Palmquist Siguard et al. 2003. “The combination syndrome : A
literature review”. J. Prosthet. Dent; 90 : 270-5.
16.Kelly Ellswarth 1972. “Changes caused by a mandibular removable
partial denture opposing a maxillary complete denture”. J. Prosthet.
Dent., 27 : 140-150.
17.Palmer C.A. 2003. “Gerodontic nutrition and dietary counseling for
prosthodontic patients”. Dent. Clin. N. Am., 47 : 355-371.
18.Wical K.E., Brussee P., 1979. “Effect of calcium and vitamin D
supplement on alveolar ridge resorption in immediate denture
patients”. J. Prosthet. Dent; 41 : 4-11.
Page 22
Related Documents